Abstract
Background
Individuals with 22q11.2 deletion syndrome (22q11.2DS) have an elevated risk for schizophrenia, which increases with history of childhood anxiety. Altered hippocampal morphology is a common neuroanatomical feature of 22q11.2DS and idiopathic schizophrenia. Relating hippocampal structure in children with 22q11.2DS to anxiety and impaired cognitive ability could lead to hippocampus-based characterization of psychosis-proneness in this at-risk population.
Methods
We measured hippocampal volume using a semiautomated approach on MRIs collected from typically developing children and children with 22q11.2DS. We then analyzed hippocampal morphology with Localized Components Analysis. We tested the modulating roles of diagnostic group, hippocampal volume, sex and age on local hippocampal shape components. Lastly, volume and shape components were tested as covariates of IQ and anxiety.
Results
We included 48 typically developing children and 69 children with 22q11.2DS in our study. Hippocampal volume was reduced bilaterally in children with 22q11.2DS, and these children showed greater variation in the shape of the anterior hippocampus than typically developing children. Children with 22q11.2DS had greater inward deformation of the anterior hippocampus than typically developing children. Greater inward deformation of the anterior hippocampus was associated with greater severity of anxiety, specifically fear of physical injury, within the 22q11.2DS group.
Limitations
Shape alterations are not specific to hippocampal subfields.
Conclusion
Alterations in the structure of the anterior hippocampus likely affect function and may impact limbic circuitry. We suggest these alterations potentially contribute to anxiety symptoms in individuals with 22q11.2DS through modulatory pathways. Altered hippocampal morphology may be uniquely linked to anxiety risk factors for schizophrenia, which could be a powerful neuroanatomical marker of schizophrenia risk and hence protection.
Introduction
Chromosome 22q11.2 deletion syndrome (22q11.2DS), which occurs in 1–2 of every 4000 live births,1,2 is caused by a hemizygous microdeletion within the long arm of chromosome 22. The syndrome presents with a highly variable phenotype. Phenotypic variability germane to our study is the elevated prevalence of mood, attention and psychiatric disorders in children with 22q11.2DS.3,4 Notably, schizophrenia is reported in approximately 30% of adults with 22q11.2DS, which makes 22q11.2DS the third highest genetic cause of schizophrenia behind having an identical twin (50%) or 2 parents with schizophrenia (40%).5 22q11.2DS is unique in facilitating prospective developmental study of risk factors for schizophrenia because individuals carrying chromosome 22q11.2 deletions are typically identified early in life, before psychosis symptoms emerge. Therefore, characterizing intermediate phenotypes and potential biomarkers is critical to identify those at greater risk and which interventions may be effective in changing the course of development.
Idiopathic schizophrenia and 22q11.2DS have a number of phenotypes in common at varying rates.4,6,7 These include shared genetic (e.g., COMT genotypes8), neural (e.g., enlarged cavum septum pellucidum and lateral ventricles9,10) and cognitive (e.g., impaired executive11–14 and attentional functions15–18) traits. Major neuranatomical features of 22q11.2DS and schizophrenia centrally involve the hippocampus. Indeed, evidence from mouse models of 22q11.2DS implicates altered cytoarchitecture, neurogenesis, neurophysiology and connectivity of the hippocampus.19–22 In human brain imaging studies, reduction in hippocampal volume is a replicated finding in neuroimaging studies of schizophrenia23,24 and is thought to be a critical component of the neuropathological basis of the disorder.25 Reduced hippocampal volumes are also frequently reported in 22q11.2DS among other anomalies in a globally hypoplasic brain.26 Given these commonalities, it is reasonable to hypothesize that hippocampal analyses are critical to understanding the emergence of psychosis in 22q11.2DS. To date, multiple groups have identified predictive neuroanatomical markers of schizophrenia-related symptomology in individuals with 22q11.2DS, such as reduced hippocampal volume27–29 and declining prefrontal grey matter.30,31 Thus, the characterization of hippocampal morphology associated with elevated risk of schizophrenia development calls for more in-depth investigation.
In children and adolescents with 22q11.2DS, rates of true psychotic disorders are very low (i.e., below 10%).3,4 However, prodromal, attenuated, or subclinical symptoms of psychosis are highly prevalent in adolescents with 22q11.2DS, with rates of 45%–90% depending on the criteria used.32–34 This further indicates how enriched this population is for what is now referred to as “psychosis-proneness.” However, the factors that mediate the likelihood of conversion from psychosis-proneness to full psychotic disorder remain unclear and are a major focus of current research. Several recent longitudinal studies have shown that, aside from declines in verbal IQ and attention disorders,6,34,35 one of the strongest predictors of future psychosis in individuals with 22q11.2DS is the presence of a pre-existing anxiety disorder in childhood.34,36 Importantly, Angkustsiri and colleagues37 have demonstrated that greater anxiety, but not lower IQ, levels strongly predicted lower adaptive function in children with 22q11.2DS. Of interest is whether the hippocampus may be a component of the neural circuitry contributing to anxiety and the associated risk of schizophrenia. In the present study, we investigated potential associations between hippocampal anatomy, anxiety and IQ in children and adolescents with 22q11.2DS.
Thus far, volumetric and voxel-based morphology image analyses have primarily been used to detect anomalies in human hippocampal size in individuals with 22q11.2DS.38 When represented in 3-dimensional space, hippocampal volume and shape can be assessed at high resolution using a variety of methods. One validated method is localized components analysis (LoCA), which is a dimension reduction approach to shape analysis that outputs concise and spatially cohesive representations of the variance in structure across a sample.39 The results of LoCA may reflect localized reductions or expansions in volume or dysmorphic features since the hippocampi have been globally scaled to a common graph space. In the context of the hippocampus, results may represent abnormal hippocampal subfields, malrotation, altered folding of the hippocampal head, or deviated position of the hippocampal tail. Shape variation may reflect differences in the neuroanatomical organization of the hippocampus caused by developmental course, post-natal synaptic plasticity, or integrity of long and short pathways.40 Such analyses are critically important in 22q11.2DS since, to our knowledge, there has been no significant study to date of postmortem brain tissue that would allow testing of such hypotheses. Therefore, we propose that subregions of the hippocampus already identified as a major neuroanatomical feature of idiopathic schizophrenia, such as the CA1 subfield,7,41 may also be altered in children who have 22q11.2DS and, thus, an elevated risk of schizophrenia and persistent anxiety.
Given the absence of available postmortem tissue of 22q11.2DS brains, in vivo MRI may be the best tool with which to visualize the local hippocampal anatomy. Thus, using a semiautomated segmentation method, we measured hippocampal volume in children with 22q11.2DS and typically developing children and adolescents. We then used LoCA to identify where the hippocampus is disproportionately affected by the disorder. Finally, we investigated the associations between these shape metrics and both anxiety and IQ scores in children with 22q11.2DS.
Methods
Participants
We recruited children and adolescents with 22q11.2DS as well as typically developing controls to participate in the study. We obtained informed assent and consent was obtained from all participants and their guardians before enrolling the children in the study. Diagnosis of chromosome 22q11.2 deletion was confirmed using fluorescent in situ hybridization (FISH) or a similar genetic test. Parents provided all genetic test data as part of the screening process. The Institutional Review Board of University of California Davis Medical Center approved all protocols.
Behavioural assessments
Standardized intelligence assessments were conducted for both the typically developing children and those with 22q11.2DS. Most individuals were evaluated using the Wechsler Intelligence Scale for Children, Fourth Edition (WISC-IV) and the remainder were evaluated using the Wechsler Abbreviated Scale of Intelligence (WASI), Leiter-R or Kaufman Assessment Battery for Children, Second Edition (KABC-II). For the WISC-IV, index scores (verbal comprehension, processing speed, working memory, and perceptual reasoning) were also provided.
Ratings of anxiety symptoms were determined using the Spence Children’s Anxiety Scale Parent Version. Scores per subscale were converted to t-scores and log-transformed before performing statistical analyses to achieve normal distribution for linear models. Subscales were fear of physical injury, separation anxiety, social phobia, panic and agoraphobia, obsession–compulsion and generalized anxiety.
MRI acquisition protocol
All participants were scanned at the Imaging Research Center at the University of California at Davis Medical Center on a 3 T Siemens MAGNETOM Trio scanner with A Tim operating system. A 32-channel head coil was used to acquire T1-weighted, diffusion weighted and echo planar blood oxygen level–dependent (BOLD) images. In this experiment, only the T1-weighted images were used. The 3-dimensional magnetization-prepared rapid gradient-echo T1-weighted sequence with isotropic voxel dimensions parameters were as follows: sagittal plane of acquisition, 192 slices, slice thickness 0.9 mm, number of excitations = 1, repetition time 2200 ms, echo time 4.37 ms, inversion time 1100 ms, flip angle 7°, field of view 230 × 230 mm, matrix 256 × 256, bandwidth 260 Hz/pixel.
Hippocampus segmentation
The hippocampus was defined along its central axis, from the anterior head to the posterior tail, and included the hippocampus proper and hippocampal complex subregions extending to the medial surface of the cortex.42 All hippocampi were segmented using a semiautomated method previously validated on rhesus monkey brains.43 Briefly, landmarks were placed at regular locations on the participant image. Then the pediatric template was diffeomorphically registered to each participant image, which also had the landmarks and a complete manual segmentation of the hippocampus. The hippocampus label was applied to each participant image as an approximation of the hippocampus segmentation. Then a learning-based segmentation correction method compared the approximate segmentation to a set of manual segmentations to adjust the label. The mean DICE coefficients between the manual and SegAdapter hippocampal segmentations were 0.8352 ± 0.089. The detailed protocol is described in Appendix 1, available at jpn.ca. The brain masks generated in this image-processing pipeline were used to calculate total brain volume.
Localized components analysis
The LoCA methodology used in the present study was validated and applied in previous work39,44,45 (Fig. 1). Parameters were optimized for the characteristics of the data set and are detailed in Appendix 1. Briefly, radial meshes were generated from each participant’s volumetric segmentations and aligned to each other after linear scaling so that the radial distance at each vector could be compared among participants and to remove global differences in volume. We analyzed the variance of radial distance using principal components analysis, which generates basis vectors and individual participant coefficients for each basis vector. The normalized mean coefficient for each participant was input for statistical analyses. We conducted LoCA processing independently for the 22q11.2DS and typically developing groups (22q11.2DS–TD) combined and for and the 22q11.2DS group alone.
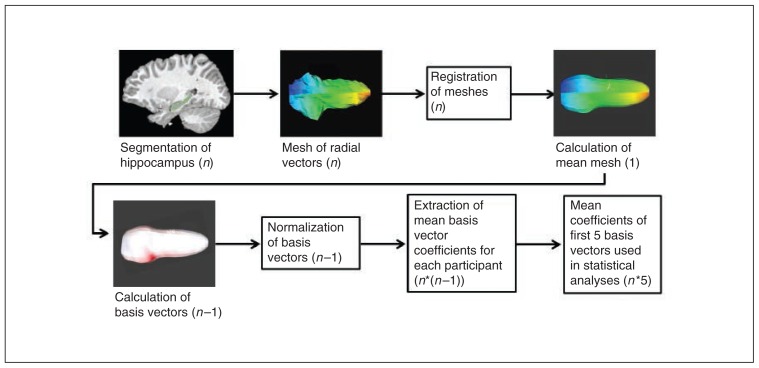
Fig. 1.
Localized components analysis (LoCA) processing steps. Each hippocampus volumetric segmentation in a sample (n) is converted to a radial mesh and oriented along the central axis. Then the meshes are registered to a common graph space where a mean mesh is created for 1:1 correspondence of vectors. Principal components analysis of the radial distances produces the basis vectors, which are then normalized by the maximum radial distance. The other output of LoCA is the individual participant coefficients for each basis vector. Only the first 5 basis vectors were used as variables for analyses of variance and general linear models.
Statistical analysis
Analysis of vector-wise variance, normalization and mesh visualization was conducted in RStudio software version 0.98.501. All other statistical analyses were carried out in SPSS version 21 (IBM). We corrected the significance of each model for multiple comparisons using false discovery rate (FDR) correction.46 First, we tested the effects of total brain volume (TBV), sex, diagnostic group and age on right and left hippocampal volume with univariate analyses of variance (ANOVA) in each subset of participants (22q11.2DS–TD and 22q11.2DS group alone).
Next, we analyzed the first 5 basis vectors in each LoCA result (right and left 22q11.2DS–TD and 22q11.2DS group alone). These were selected based on reconstruction error rank and a 5% threshold for proportion of variance explained. Individually, the analyzed basis vectors explained 5%–14% of the variance in radial distance. In total, the first 5 basis vectors accounted for 35%–45% of the variance in each analysis. In each multivariate ANOVA for normalized mean coefficients of the basis vectors, we tested for the modulating roles of diagnostic group and hippocampal volume, controlling for age and sex in each test.
We used general linear models to test for nonimaging outcome variables; hippocampal volume and basis vector normalized mean coefficients were tested as predictors of IQ scores and Spence Anxiety Scale scores in children with 22q11.2DS.
Results
Participants
A total of 117 children aged 7–15 years participated in the study: 69 with 22q11.2DS and 48 typically developing children. The demographic and clinical characteristics of participants are shown in Table 1. Of the standardized intelligence assessments conducted, 82 children were evaluated using the WISC-IV, 33 using the WASI, 1 using the Leiter-R and 1 using the KABC-II. On all scales, IQ was significantly lower in children with 22q11.2DS than in typically developing children (p < 0.001; Table 1). Children with 22q11.2DS had higher total Spence scores than typically developing children (p < 0.001).
Table 1.
Participant demographic and clinical characteristics
| Group; mean ± SD (n)* | ||
|---|---|---|
|
|
||
| Characteristic | TD | 22q11.2DS |
| Sex, male:female | 24:24 | 37:32 |
| Age, yr | 10.65 ± 2.36 (48) | 11.32 ± 2.58 (69) |
| Full-scale IQ† | 113.8 ± 13.3 (47) | 74.9 ± 13.1 (66) |
| Verbal comprehension | 117.7 ± 14.5 (47) | 80.2 ± 13.6 (66) |
| Perceptual memory | 99.8 ± 11.7 (19) | 78.0 ± 13.5 (63) |
| Working memory | 99.8 ± 11.6 (17) | 81.6 ± 14.3 (63) |
| Processing speed | 107.7 ± 11.7 (19) | 78.5 ± 13.7 (63) |
SD = standard deviation; TD = typically developing children.
Unless indicated otherwise.
IQ score significantly lower in the 22q11.2DS group (p < 0.001).
Hippocampal volume reduced in 22q11.2DS compared with typical development
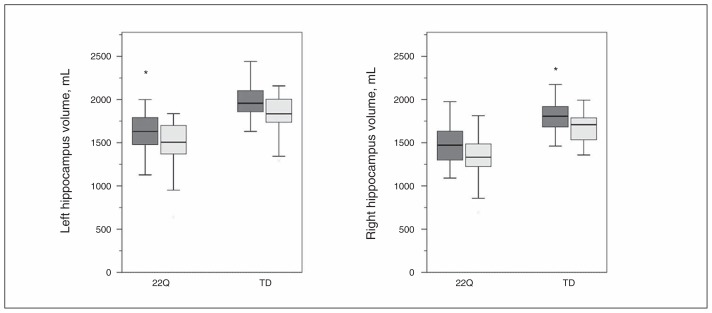
We tested for covariates of hippocampal volume across all children and found that right and left hippocampal volume was lower in children with 22q11.2DS (p < 0.001) by approximately 355 mm3 (Fig. 2) after controlling for sex, age and TBV. We found that 39% of the right and 23% of the left hippocampal volume in children with 22q11.2DS was below 2 standard deviations of the mean hippocampal volume in typically developing children. While sex and age were not significant predictors in the model, hippocampal volume positively covaried with TBV (p < 0.001). In follow-up tests within each diagnostic group, hippocampal volume was significantly associated with TBV on the left (p = 0.002) and right (p < 0.001) in the 22q11.2DS group and on the right (p < 0.001) in the typically developing group. Furthermore, TBV was significantly lower in children with 22q11.2DS than in typically developing children (p < 0.001) by approximately 84 cm3.
Fig. 2.
Hippocampus volume was smaller in male (dark grey) and female (light grey) 22q11.2DS (22Q) groups than in the typically developing (TD) group on the left (p < 0.05) and right (p < 0.01). Male hippocampi were larger than female hippocampi in the 22Q (p < 0.001) and TD (p < 0.001) groups. *Outlier data points.
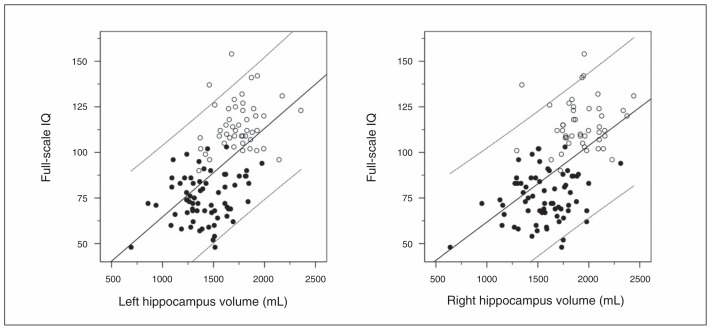
Next, we tested hippocampal volume as a predictor of full scale IQ and subscales across the entire sample in a linear regression model (Fig. 3). Right and left hippocampal volumes significantly predicted full-scale IQ when all children were analyzed (left: R2 = 0.300, p < 0.001; right: R2 = 0.337, p < 0.001). When controlling for sex, age, type of IQ test (p < 0.001, WASI > WISC-IV) and TBV, hippocampal volume still significantly covaried with full-scale IQ (left: p < 0.001; right: p < 0.001). Although TBV was significantly lower in children with 22q11.2DS than in typically developing children, TBV was not a significant parameter in the multipredictor model. Left and right hippocampal volumes significantly predicted scores on all subscales (all p < 0.05), although these were available only for a subset of participants (Table 1). Although IQ was positively associated with hippocampal volume (left: R2 = 0.299; right: R2 = 0.346), this may have been confounded by diagnosis, as children with 22q11.2DS on average had lower IQ and smaller hippocampi than typically developing children. Therefore, we tested the association within each diagnostic group. Neither the left nor the right hippocampal volume significantly covaried with full-scale IQ in typically developing children (Fig. 3). In children with 22q11.2DS, hippocampal volume tended to covary with IQ (right: p = 0.05; left: p = 0.033), but this effect did not survive in multipredictor models.
Fig. 3.
Full-scale IQ was predicted by left or right hippocampal volume across all children with a wide range of scores. Plots show linear regressions for all children (left: R2 = 0.346; right: R2 = 0.299) and within diagnostic groups (typically developing children, left: R2 = 0.041; typically developing children, right: R2 = 0.016; 22q11.2DS, left: R2 = 0.049; 22q11.2DS, right: R2 = 0.047). Typically developing children are shown in open circles; children with 22q11.2DS are shown in closed circles.
We tested whether left or right hippocampal volume covaried with anxiety in children with 22q11.2DS and found that hemispheric hippocampal volume predicted total Spence Anxiety Scale score, such that a smaller volume was associated with a higher score (left: p = 0.041; right: p = 0.045). Hippocampal volume did not significantly covary with any of the Spence Anxiety Scale subscales.
Anterior hippocampal shape altered in 22q11.2DS compared with typical development
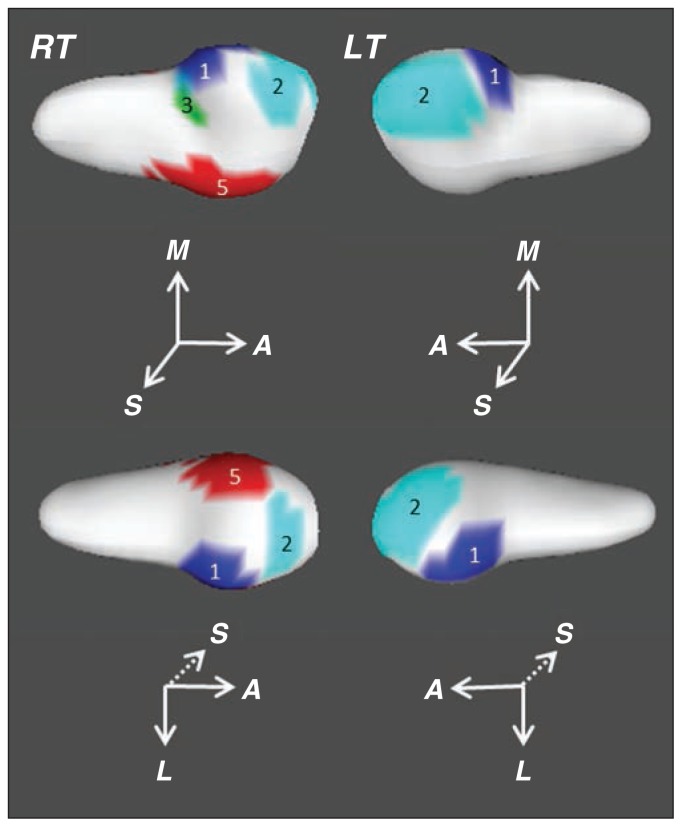
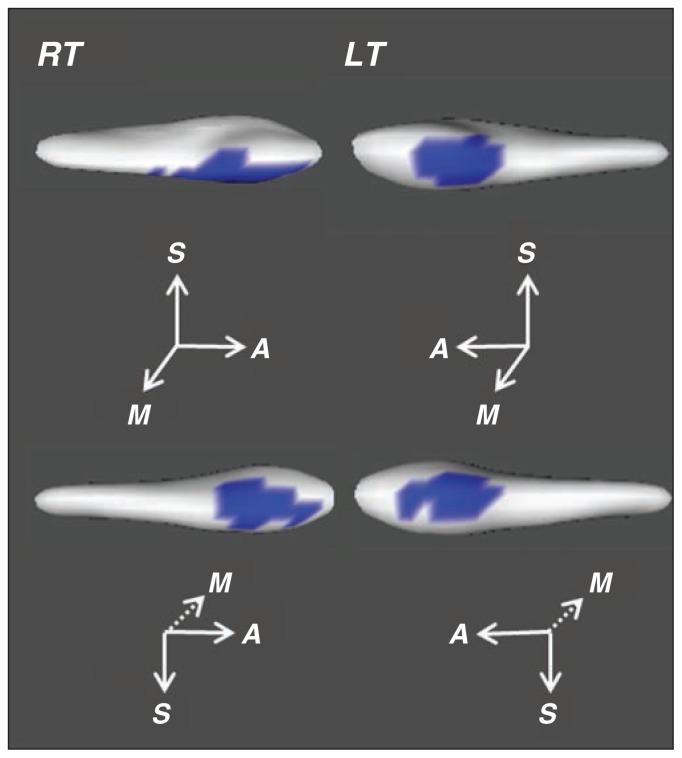
In the analysis of 22q11.2DS and typically developing groups combined, LoCA output resulted in consistent alterations in the anterior hippocampus (defined by uncal apex landmark; Fig. 4). In both hemispheres, basis vectors V.1 and V.2 were adjacent to each other with peak localizations in the anterior hippocampus near the transition to the posterior hippocampus. On the right, vector V.3 was medial to V.1 at the transition between the head and body. The peak localization of the right vector V.4 covered the hippocampal tail. The right vector V.5 had 2 peak localizations. One ran along the inferior surface of the anterior hippocampus and the most anterior aspect of the posterior hippocampus. The other region centred over the superior-lateral aspect of the anterior hippocampus. On the left, vectors V.3 and V.5 were distributed over the whole hippocampal surface without clear localizations. In contrast, on the left V.4 appeared as a patchy band around the anterior to posterior transition of the hippocampus.
Fig. 4.
Basis vectors localized to the anterior hippocampus in the analysis of 22q11.2DS and typically developing groups. These regions demonstrated the greatest localized variation in radial distance in the sample. The right side shows the average right hippocampal mesh with superior and inferior views with overlaid basis vectors at a threshold of 50%. The left side shows the respective views for the left hippocampus. The vectors (V) are shown in the following colours: V.1 = dark blue, V.2 = light blue, V.3 = green, V.5 = red.
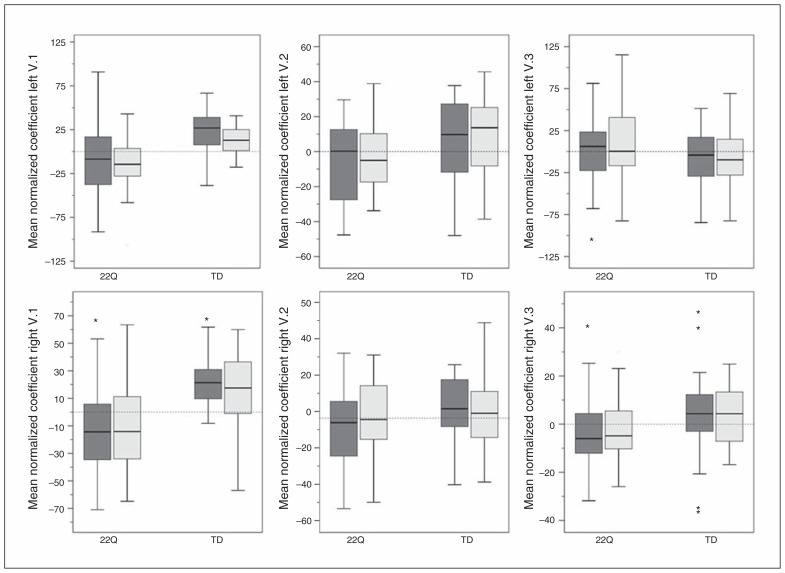
We compared the normalized mean coefficients for each basis vector between the groups, controlling for age and sex (Fig. 5). Children with 22q11.2DS showed greater inward deformation than typically developing children at vectors V.1 (partial variance explained [PVE] = 13.76%, p < 0.001) and V.3 on the right (PVE = 8.76%, p = 0.037) and V.1 (PVE = 12.26%, p < 0.001) and V.2 on the left (PVE = 6.27%, p = 0.021). Age and sex did not have a significant effect on any of the basis vector coefficients. In multivariate analyses with multiple comparison correction, only the right and left vector V.1 association with diagnostic group remained significant.
Fig. 5.
The mean coefficient for the first 3 basis vectors show the effect of diagnostic group (males = dark grey, females = light grey). The mean coefficients were smaller in the 22q11.2DS (22Q) group at vectors V.1 (p < 0.001) and V.2 (p < 0.05) on the left and vectors V.1 (p < 0.001) and V.3 (p < 0.05) on the right. None of the basis vectors were associated with age or sex. TD = typically developing group. *Outlier data points (> 1.5 × the interquartile range).
Right hippocampal volume did not significantly covary with mean coefficients for any of the right basis vectors. When age and sex were included in the left hippocampal models, hippocampal volume significantly covaried with vectors V.1 (p = 0.033) and V.5 (p = 0.022), but this did not survive multiple comparison correction. As the left vector V.5 covered the entire hippocampal surface, the positive effect of volume suggested that greater volume was predictive of larger radial distances globally. For the left vector V.1, lesser hippocampal volume predicted shorter radial distances over the focal regions of the anterior hippocampus.
Anterior hippocampal shape predicts fear of physical injury score in children with 22q11.2DS
We analyzed the LoCA output from the 22q11.2DS group alone to identify where hippocampal shape differed within the population. Strikingly, the regions of greatest variance localized to the anterior hippocampus (right V.1: p < 0.001; left V.1: p < 0.001; Fig. 6). This corresponded with the localization of the basis vectors showing an effect of diagnostic group in the combined LoCA result. The right vector V.2 was positioned over the medial-anterior aspect of the anterior hippocampus and was not associated with age, sex or hippocampal volume. The right and left basis vectors 3–5 did not have precise spatial localization to the anterior hippocampus; rather, they spread over much of the hippocampal surface.
Fig. 6.
Medial and lateral views of vector V.1 on the 22q11.2DS group mean hippocampal mesh. The region along the ventral surface of the anterior hippocampus was positively associated with hippocampal volume (i.e., more positive mean coefficient covaried with greater volume; right V.1: p < 0.001; left V.1: p < 0.001).
Hippocampal volume was positively associated with all 5 basis vectors on the left (p < 0.05) and all except V.3 on the right (p < 0.05). This pattern suggests that smaller hippocampi show greater hippocampal shape alterations. Finally, we tested the predictive value of within-group 22q11.2DS basis vector coefficients for anxiety symptomology and IQ. Models for full-scale IQ and subscales did not show a significant effect of hippocampal shape. On the other hand, right and left basis vector coefficients of the anterior hippocampus did covary with Spence Anxiety Scale scores.
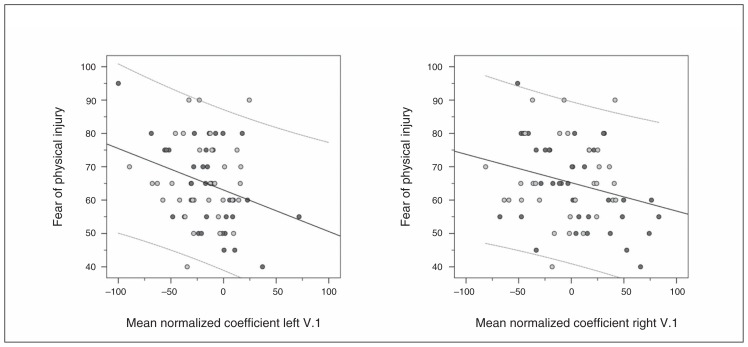
In each hemispheric model, vector V.1 mean normalized coefficients trended toward covariance with the Spence Anxiety Scale total score (right: p = 0.06; left: p = 0.05). Of the sub-scales, only fear of physical injury was significantly associated with vector V.1 mean normalized coefficients after controlling for sex and age (right: p = 0.035; left: p < 0.001; Fig. 7); however, only the left vector V.1 survived correction for multiple comparisons. Fear of physical injury was the highest subscale score in this sample and in a previous report.37 Since vector V.1 coefficients were associated with hippocampal volume, we tested multipredictor models for fear of physical injury score that included both hippocampal volume and vector V.1 with age and sex. In these models, only the left vector V.1 (p = 0.029) and age (p = 0.005) retained significant negative effects on the fear of physical injury score after multiple comparison correction. This result supported the expected age-related decline of anxiety symptoms. The association between this subscale and hippocampal shape indicated that higher scores were associated with greater inward distortion of the uncal region of the anterior hippocampus (Fig. 6).
Fig. 7.
Vector V.1 on the left and right is negatively associated with the fear of physical injury subscale score on the Spence Anxiety Scale (left: p = 0.005; right: p = 0.035). The plots show linear regressions with 95% confidence intervals. Males = dark grey, females = light grey.
In addition, the left vector V.4 coefficients negatively covaried with the total anxiety score (p = 0.025) and the separation anxiety subscale score (p = 0.002), the second highest subscale score reported here and in a previous past study.37 The peak deformation of this basis vector was adjacent to the left vector V.1 in the inferomedial and superolateral aspects of the anterior hippocampus. The areal spread of this basis vector extended posteriorly into the body of the hippocampus. We tested multipredictor models controlling for age, sex and hippocampal volume. In this model, the left vector V.4 or any other independent variable did not significantly covary with total anxiety score. In the multipredictor model for separation anxiety, the left vector V.4 did not survive as a significant covariate (p = 0.06). Rather, age showed a significant negative effect on the score, similar to the effect of age on fear of physical injury score (p = 0.002).
Discussion
The present study dissociated global hypoplasia of the hippocampus from regional distortions found in children and adolescents with 22q11.2DS. Reduced hippocampal volume covaried with broad regions along the hippocampal anterior–posterior axis. More importantly, inward deformations localized to the anterior hippocampus distinguished the hippocampi of children with 22q11.2DS from those of typically developing children. Further, hippocampal volume predicted variation in the shape of the anterior hippocampus in children with 22q11.2DS. Our results suggest that children with 22q11.2DS who have small hippocampi are more likely to have altered morphology of the anterior hippocampus. This particular variation in hippocampal shape predicted fear of physical injury anxiety score, which is 1 of the 2 strongest anxiety subtypes found in individuals with 22q11.2DS37 and is related to the anxiety disorders that appear to increase psychosis-proneness.4,34,36 Therefore, anterior hippocampus morphology may potentially serve as a sensitive neuroanatomical marker for conditions associated with greater schizophrenia risk.
Connectivity of the anterior hippocampus
Previous work has linked variance in anterior and posterior hippocampal shape and proportion to specialized function or impairments in other populations.47–49 Our understanding of the differential connectivity along the anterior–posterior axis of the hippocampus may inform how altered anterior hippocampal anatomy in individuals with 22q11.2DS may relate to anxiety symptoms. Though connectivity patterns indicate a gradient mapping, some projections are heavily weighted to the anterior regions.50 Unique to the anterior hippocampus are direct connections with the amygdala, ventromedial prefrontal cortex (vmPFC), anterior temporal lobe, insula and fusiform gyrus, which may subserve a modulatory role in the processing of emotionally salient inputs.51,52 In particular, primate uncal CA1 and prosubicular regions have direct connections to the amygdala.53 The basis vectors associated with 22q11.2DS and anxiety severity were localized to the homologous regions of the human brain.
Anterior hippocampus contribution to anxiety
Human neuroimaging studies demonstrate that the anterior hippocampus is preferentially involved in unconditioned fear, state anxiety and safety threat conditions.54 This is in contrast to the posterior hippocampus, which plays a role in fear memory55,56 and possibly trait anxiety.57
The proposed function of the anterior hippocampus in anxiety-like behaviours is to modulate input to the amygdala, which is a central component of emotionally coded memory.54 The pathway of tracts to the amygdala passes along the uncus, sharply over the region represented in vector V.1 in the present study. Parallel to this, the rodent ventral hippocampus (equivalent to the human anterior hippocampus) has disynaptic connections to the prelimbic cortex (PL, equivalent to mPFC in humans), which has reciprocal connections to the amygdala. The ventral hippocampus in rodents may modulate the input to the PL that promotes discrimination of threat via the amygdala.54,58 The smaller size of the hippocampus and altered morphology of the anterior hippocampus in humans may contribute to the neuroanatomical basis of anxiety in individuals with 22q11.2DS, particularly specific phobias.
In adults with generalized anxiety disorder or specific phobias (encompassed within the Spence fear of physical injury subscale), the amygdala and insula show an amplified coactivation under anxiety-provoking conditions.51,59 Human functional connectivity studies support the notion that the hippocampus and insula act as modulators of activity in the amygdala.51 Though functional MRI studies like these have not been conducted in children with 22q11.2DS, their results suggest that a hyperactive or dysregulated amygdala may be an element of anxiety or phobias in this population. For children with 22q11.2DS, anxiety symptoms may in part be a result of abnormal modulation by the anterior hippocampus via direct pathways and indirectly via the vmPFC. This may be additive to abnormal anatomy38,60 and hyperactivity of the amygdala. Further study of the amygdala and prefrontal structure and connectivity in the present data set would better inform this hypothesis.
Because anxiety in childhood is a strong predictor of daily living skills and functional abilities,4,37 the link we found between altered anterior hippocampus morphology and anxiety symptoms may help identify children who struggle later in development. In particular, specific phobia presents more frequently in individuals with 22q11.2DS (22% of children and 17% of adolescents) than with other types of anxiety.4 Similar rates have been reported by Antshel and colleagues,6 who found that anxiety and IQ in children independently predicted prodromal psychosis symptoms at 3-year follow-up assessment. In our sample of children aged 7–15 years, the highest Spence subscale rating was for fear of physical injury, which is consistent with both studies described. Therefore, a population with childhood anxiety will be critical for future prospective study of schizophrenia risk and protection.
Comparison to structural neuroimaging studies
The specificity of inward deformation of the anterior hippocampus, which was primarily positioned over the uncal, sub-licular and CA1 field subregions, was strikingly similar to hippocampal shape analyses of adults with schizophrenia. In contrast, a single study that directly assessed hippocampal malrotation in adults with 22q11.2DS showed very different patterns than those identified by LoCA.61 If we were to observe malrotation, or incomplete infolding of the hippocampus, we would have found differences around the lateral surfaces of the body of the hippocampus due to the narrowed morphology of a malrotated hippocampus. Rather, we found that the difference in hippocampal shape was isolated to the anterior hippocampus. Previous studies of individuals with idiopathic schizophrenia identified focal inward deformations in the anterior hippocampus bilaterally even when overall hippocampal volume was not reduced.48,62 Additionally, volumetric studies reported selective decreases in the anterior hippocampus in patients with schizophrenia.63–65 Qiu and colleagues62 took a multimodal approach and linked altered anterior hippocampus shape to reduced fornix and cingulum integrity as well as reduced functional connectivity between the anterior hippocampus and frontal regions. These complementary findings in patients with idiopathic schizophrenia and anxious youth with 22q11.2DS highlight the relevance of the hippocampus as a critical component detecting psychosis-proneness.
Two recent neuroimaging studies of 22q11.2DS that investigated associations between local anatomy and psychosis risk are relevant to the discussion of a hippocampal neuroanatomical correlate. First, a recent longitudinal study reported that greater hippocampal head volumes predicted the emergence of positive psychosis symptoms 3 years later.29 Our rather different finding showed that inward deformations localized to the inferior lateral aspects of the anterior hippocampus were predictive of anxiety severity, a risk factor for future psychosis. The divergent results between these 2 studies may be a consequence of different analytical methods and cohort characteristics. Another recent report on brain morphology in adolescents with 22q11.2DS described increased grey matter volume in the hippocampal complex, which did not predict any outcome variables.31 Rather, declining grey matter volume in the prefrontal cortex, which is another vulnerable cortical region in 22q11.2DS, predicted increased psychosis risk.66
Generally, our findings are consistent with those of structural brain image analyses in individuals with 22q11.2DS. First, we observed a mean bilateral decrease in hippocampal volume in children and adolescents with 22q11.2DS that was relatively greater than total brain volume reduction.26 Second, we found a positive association between full-scale IQ and hippocampus volume across diagnoses, yet full-scale IQ did not relate to the local anatomy of the hippocampus. Previous studies demonstrated a positive association between hippocampal volume and IQ in typically developing children67 and children with 22q11.2DS;38 however, we have not replicated such an association. The specificity of the association between the hippocampus and IQ would be better evaluated in a more comprehensive study of total and regional brain volumes as well as white matter microstructure.
Limitations
The primary limitation of our study is that we cannot discern the directionality of the association between hippocampal morphology and severity of anxiety in the children with 22q11.2DS. For example, alterations in the hippocampus may result from a common etiology influencing both anxiety risk and structural brain development. Second, our finding of a significant correlation between IQ and hippocampal volume would be strengthened by demonstrating the effect with a consistent measure of IQ across the sample, which was not possible in this study.
Conclusion
Collectively, our findings suggest that the anterior hippocampus may play a significant role in the etiology of anxiety and possibly schizophrenia risk in individuals with 22q11.2DS. The altered morphology of the anterior hippocampus in children with 22q11.2DS parallels findings in schizophrenia populations, while also predicting the most common anxiety symptoms in childhood. Additionally, IQ did not relate to the shape of the anterior hippocampus, but rather to the volume of the whole hippocampus, which helps to distinguish subtle associations of hippocampal subregions in psychological or cognitive traits. In conjunction with other known neuroanatomical correlates, the dystrophic characteristics of the hippocampus may help to elucidate subgroups within 22q11.2DS related to anxiety. This knowledge could enhance monitoring of children for the assessment of schizophrenia risk and protection.
Acknowledgements
The study was funded by National Institute of Health grant NIH R01 HD042947 (T. Simon), MIND Institute IDDRC grant 1U54HD079125 (Abbeduto), and UC Davis CTSC grant UL1 TR000002. The authors thank all the families who participated in this study and made this work possible. The authors extend sincere appreciation to Pauline Maillard for support in analyzing the data and visualizing the results, David Amaral for early guidance in the design of this study and insightful feedback on the manuscript and Danielle Harvey for statistical consultation.
Footnotes
Competing interests: None declared.
Contributors: O. Carmichael and T. Simon designed the study. N. Goodrich-Hunsaker, A. Lee, M. Hunsaker and T. Simon acquired the data, which J. Scott, N. Goodrich-Hunsaker, K. Kalish, M. Hunsaker, C. Schumann and T. Simon analyzed. J. Scott, N. Goodrich-Hunsaker and T. Simon wrote the article, which all authors reviewed and approved for publication.
References
- 1.Murphy KC, Scambler PJ. Velo-cardio-facial syndrome: a model for understanding microdeletion disorders. Cambridge: Cambridge University; 2005. [Google Scholar]
- 2.Shprintzen RJ. Velo-cardio-facial syndrome: 30 years of study. Dev Disabil Res Rev. 2008;14:3–10. doi: 10.1002/ddrr.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Green T, Gothelf D, Glaser B, et al. Psychiatric disorders and intellectual functioning throughout development in velocardiofacial (22q11.2 deletion) syndrome. J Am Acad Child Adolesc Psychiatry. 2009;48:1060–8. doi: 10.1097/CHI.0b013e3181b76683. [DOI] [PubMed] [Google Scholar]
- 4.Schneider M, Debbane M, Bassett AS, et al. Psychiatric disorders from childhood to adulthood in 22q11.2 deletion syndrome: results from the International Consortium on Brain and Behavior in 22q11.2 Deletion Syndrome. Am J Psychiatry. 2014;171:627–39. doi: 10.1176/appi.ajp.2013.13070864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murphy KC. Schizophrenia and velo-cardio-facial syndrome. Lancet. 2002;359:426–30. doi: 10.1016/S0140-6736(02)07604-3. [DOI] [PubMed] [Google Scholar]
- 6.Antshel KM, Shprintzen R, Fremont W, et al. Cognitive and psychiatric predictors to psychosis in velocardiofacial syndrome: a 3-year follow-up study. J Am Acad Child Adolesc Psychiatry. 2010;49:333–44. [PMC free article] [PubMed] [Google Scholar]
- 7.Karayiorgou M, Simon TJ, Gogos JA. 22q11.2 microdeletions: linking DNA structural variation to brain dysfunction and schizophrenia. Nat Rev Neurosci. 2010;11:402–16. doi: 10.1038/nrn2841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gothelf D, Eliez S, Thompson T, et al. COMT genotype predicts longitudinal cognitive decline and psychosis in 22q11.2 deletion syndrome. Nat Neurosci. 2005;8:1500–2. doi: 10.1038/nn1572. [DOI] [PubMed] [Google Scholar]
- 9.Beaton EA, Qin Y, Nguyen V, et al. Increased incidence and size of cavum septum pellucidum in children with chromosome 22q11.2 deletion syndrome. Psychiatry Res. 2010;181:108–13. doi: 10.1016/j.pscychresns.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schmitt JE, Yi JJ, Roalf DR, et al. Incidental radiologic findings in the 22q11.2 deletion syndrome. Am J Neuroradiol. 2014;35:2186–91. doi: 10.3174/ajnr.A4003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sobin C, Kiley-Brabeck K, Karayiorgou M. Lower prepulse inhibition in children with the 22q11 deletion syndrome. Am J Psychiatry. 2005;162:1090–9. doi: 10.1176/appi.ajp.162.6.1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stoddard J, Beckett L, Simon TJ. Atypical development of the executive attention network in children with chromosome 22q11.2 deletion syndrome. J Neurodev Disord. 2011;3:76–85. doi: 10.1007/s11689-010-9070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shapiro HM, Tassone F, Choudhary NS, et al. The development of cognitive control in children with chromosome 22q11.2 deletion syndrome. Front Psychol. 2014;5:566. doi: 10.3389/fpsyg.2014.00566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bish JP, Ferrante SM, McDonald-McGinn D, et al. Maladaptive conflict monitoring as evidence for executive dysfunction in children with chromosome 22q11.2 deletion syndrome. Dev Sci. 2005;8:36–43. doi: 10.1111/j.1467-7687.2005.00391.x. [DOI] [PubMed] [Google Scholar]
- 15.Bish JP, Chiodo R, Mattei V, et al. Domain specific attentional impairments in children with chromosome 22q11.2 deletion syndrome. Brain Cogn. 2007;64:265–73. doi: 10.1016/j.bandc.2007.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Simon TJ, Bish JP, Bearden CE, et al. A multilevel analysis of cognitive dysfunction and psychopathology associated with chromosome 22q11.2 deletion syndrome in children. Dev Psychopathol. 2005;17:753–84. doi: 10.1017/S0954579405050364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sobin C, Kiley-Brabeck K, Daniels S, et al. Networks of attention in children with the 22q11 deletion syndrome. Dev Neuropsychol. 2004;26:611–26. doi: 10.1207/s15326942dn2602_5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shapiro HM, Takarae Y, Harvey DJ, et al. A cross-sectional study of the development of volitional control of spatial attention in children with chromosome 22q11.2 deletion syndrome. J Neurodev Disord. 2012;4:5. doi: 10.1186/1866-1955-4-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mukai J, Dhilla A, Drew LJ, et al. Palmitoylation-dependent neuro-developmental deficits in a mouse model of 22q11 microdeletion. Nat Neurosci. 2008;11:1302–10. doi: 10.1038/nn.2204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sigurdsson T, Stark KL, Karayiorgou M, et al. Impaired hippocampal-prefrontal synchrony in a genetic mouse model of schizophrenia. Nature. 2010;464:763–7. doi: 10.1038/nature08855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Drew LJ, Stark KL, Fenelon K, et al. Evidence for altered hippocampal function in a mouse model of the human 22q11.2 microdeletion. Mol Cell Neurosci. 2011;47:293–305. doi: 10.1016/j.mcn.2011.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ouchi Y, Banno Y, Shimizu Y, et al. Reduced adult hippocampal neurogenesis and working memory deficits in the Dgcr8-deficient mouse model of 22q11.2 deletion-associated schizophrenia can be rescued by IGF2. J Neurosci. 2013;33:9408–19. doi: 10.1523/JNEUROSCI.2700-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Steen RG, Mull C, McClure R, et al. Brain volume in first-episode schizophrenia: systematic review and meta-analysis of magnetic resonance imaging studies. Br J Psychiatry. 2006;188:510–8. doi: 10.1192/bjp.188.6.510. [DOI] [PubMed] [Google Scholar]
- 24.Vita A, De Peri L, Silenzi C, et al. Brain morphology in first-episode schizophrenia: a meta-analysis of quantitative magnetic resonance imaging studies. Schizophr Res. 2006;82:75–88. doi: 10.1016/j.schres.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 25.Shenton ME, Dickey CC, Frumin M, et al. A review of MRI findings in schizophrenia. Schizophr Res. 2001;49:1–52. doi: 10.1016/s0920-9964(01)00163-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tan GM, Arnone D, McIntosh AM, et al. Meta-analysis of magnetic resonance imaging studies in chromosome 22q11.2 deletion syndrome (velocardiofacial syndrome) Schizophr Res. 2009;115:173–81. doi: 10.1016/j.schres.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 27.Eliez S, Blasey CM. Chromosome 22q11 deletion and brain structure. Br J Psychiatry. 2001;179:270. doi: 10.1192/bjp.179.3.270. [DOI] [PubMed] [Google Scholar]
- 28.Kates WR, Miller AM, Abdulsabur N, et al. Temporal lobe anatomy and psychiatric symptoms in velocardiofacial syndrome (22q11.2 deletion syndrome) J Am Acad Child Adolesc Psychiatry. 2006;45:587–95. doi: 10.1097/01.chi.0000205704.33077.4a. [DOI] [PubMed] [Google Scholar]
- 29.Flahault A, Schaer M, Ottet MC, et al. Hippocampal volume reduction in chromosome 22q11.2 deletion syndrome (22q11.2DS): a longitudinal study of morphometry and symptomatology. Psychiatry Res. 2012;203:1–5. doi: 10.1016/j.pscychresns.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 30.Kates WR, Bansal R, Fremont W, et al. Mapping cortical morphology in youth with velocardiofacial (22q11.2 deletion) syndrome. J Am Acad Child Adolesc Psychiatry. 2011;50:272–82 e2. doi: 10.1016/j.jaac.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gothelf D, Hoeft F, Ueno T, et al. Developmental changes in multivariate neuroanatomical patterns that predict risk for psychosis in 22q11.2 deletion syndrome. J Psychiatr Res. 2011;45:322–31. doi: 10.1016/j.jpsychires.2010.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baker KD, Skuse DH. Adolescents and young adults with 22q11 deletion syndrome: psychopathology in an at-risk group. Br J Psychiatry. 2005;186:115–20. doi: 10.1192/bjp.186.2.115. [DOI] [PubMed] [Google Scholar]
- 33.Stoddard J, Niendam T, Hendren R, et al. Attenuated positive symptoms of psychosis in adolescents with chromosome 22q11.2 deletion syndrome. Schizophr Res. 2010;118:118–21. doi: 10.1016/j.schres.2009.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tang SX, Yi JJ, Calkins ME, et al. Psychiatric disorders in 22q11.2 deletion syndrome are prevalent but undertreated. Psychol Med. 2014;44:1267–77. doi: 10.1017/S0033291713001669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gothelf D, Penniman L, Gu E, et al. Developmental trajectories of brain structure in adolescents with 22q11.2 deletion syndrome: a longitudinal study. Schizophr Res. 2007;96:72–81. doi: 10.1016/j.schres.2007.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gothelf D, Schneider M, Green T, et al. Risk factors and the evolution of psychosis in 22q11.2 deletion syndrome: a longitudinal 2-site study. J Am Acad Child Adolesc Psychiatry. 2013;52:1192–203 e3. doi: 10.1016/j.jaac.2013.08.008. [DOI] [PubMed] [Google Scholar]
- 37.Angkustsiri K, Leckliter I, Tartaglia N, et al. An examination of the relationship of anxiety and intelligence to adaptive functioning in children with chromosome 22q11.2 deletion syndrome. J Dev Behav Pediatr. 2012;33:713–20. doi: 10.1097/DBP.0b013e318272dd24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Deboer T, Wu Z, Lee A, et al. Hippocampal volume reduction in children with chromosome 22q11.2 deletion syndrome is associated with cognitive impairment. Behav Brain Funct. 2007;3:54. doi: 10.1186/1744-9081-3-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alcantara D, Carmichael O, Delson E, et al. Localized components analysis. Inf Process Med Imaging. 2007;20:519–31. doi: 10.1007/978-3-540-73273-0_43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim H, Mansi T, Bernasconi N. Disentangling hippocampal shape anomalies in epilepsy. Front Neurol. 2013;4:131. doi: 10.3389/fneur.2013.00131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schobel SA, Kelly MA, Corcoran CM, et al. Anterior hippocampal and orbitofrontal cortical structural brain abnormalities in association with cognitive deficits in schizophrenia. Schizophr Res. 2009;114:110–8. doi: 10.1016/j.schres.2009.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schumann CM, Hamstra J, Goodlin-Jones BL, et al. The amygdala is enlarged in children but not adolescents with autism; the hippocampus is enlarged at all ages. J Neurosci. 2004;24:6392–401. doi: 10.1523/JNEUROSCI.1297-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hunsaker MR, Amaral DG. A semi-automated pipeline for the segmentation of rhesus macaque hippocampus: validation across a wide age range. PLoS ONE. 2014;9:e89456. doi: 10.1371/journal.pone.0089456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Alcantara DA, Carmichael O, Harcourt-Smith W, et al. Exploration of shape variation using localized components analysis. IEEE Trans Pattern Anal Mach Intell. 2009;31:1510–6. doi: 10.1109/TPAMI.2008.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xie J, Alcantara D, Amenta N, et al. Spatially localized hippocampal shape analysis in late-life cognitive decline. Hippocampus. 2009;19:526–32. doi: 10.1002/hipo.20618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Benjamini YYH. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc B. 1995;57:289–300. [Google Scholar]
- 47.Maguire EA, Gadian DG, Johnsrude IS, et al. Navigation-related structural change in the hippocampi of taxi drivers. Proc Natl Acad Sci U S A. 2000;97:4398–403. doi: 10.1073/pnas.070039597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Csernansky JG, Wang L, Jones D, et al. Hippocampal deformities in schizophrenia characterized by high dimensional brain mapping. Am J Psychiatry. 2002;159:2000–6. doi: 10.1176/appi.ajp.159.12.2000. [DOI] [PubMed] [Google Scholar]
- 49.Leporé N, Shi Y, Lepore F, et al. Pattern of hippocampal shape and volume differences in blind subjects. Neuroimage. 2009;46:949–57. doi: 10.1016/j.neuroimage.2009.01.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Strange BA, Witter MP, Lein ES, et al. Functional organization of the hippocampal longitudinal axis. Nat Rev Neurosci. 2014;15:655–69. doi: 10.1038/nrn3785. [DOI] [PubMed] [Google Scholar]
- 51.Kober H, Barrett LF, Joseph J, et al. Functional grouping and cortical-subcortical interactions in emotion: a meta-analysis of neuroimaging studies. Neuroimage. 2008;42:998–1031. doi: 10.1016/j.neuroimage.2008.03.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Poppenk J, Evensmoen HR, Moscovitch M, et al. Long-axis specialization of the human hippocampus. Trends Cogn Sci. 2013;17:230–40. doi: 10.1016/j.tics.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 53.Fudge JL, deCampo DM, Becoats KT. Revisiting the hippocampal-amygdala pathway in primates: association with immature-appearing neurons. Neuroscience. 2012;212:104–19. doi: 10.1016/j.neuroscience.2012.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Adhikari A. Distributed circuits underlying anxiety. Front Behav Neurosci. 2014;8:112. doi: 10.3389/fnbeh.2014.00112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lang S, Kroll A, Lipinski SJ, et al. Context conditioning and extinction in humans: differential contribution of the hippocampus, amygdala and prefrontal cortex. Eur J Neurosci. 2009;29:823–32. doi: 10.1111/j.1460-9568.2009.06624.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pohlack ST, Nees F, Liebscher C, et al. Hippocampal but not amygdalar volume affects contextual fear conditioning in humans. Hum Brain Mapp. 2012;33:478–88. doi: 10.1002/hbm.21224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Satpute AB, Mumford JA, Naliboff BD, et al. Human anterior and posterior hippocampus respond distinctly to state and trait anxiety. Emotion. 2012;12:58–68. doi: 10.1037/a0026517. [DOI] [PubMed] [Google Scholar]
- 58.Engin E, Treit D. The role of hippocampus in anxiety: intracerebral infusion studies. Behav Pharmacol. 2007;18:365–74. doi: 10.1097/FBP.0b013e3282de7929. [DOI] [PubMed] [Google Scholar]
- 59.Etkin A, Wager TD. Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am J Psychiatry. 2007;164:1476–88. doi: 10.1176/appi.ajp.2007.07030504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Antshel KM, Aneja A, Strunge L, et al. Autistic spectrum disorders in velo-cardio facial syndrome (22q11.2 deletion) J Autism Dev Disord. 2007;37:1776–86. doi: 10.1007/s10803-006-0308-6. [DOI] [PubMed] [Google Scholar]
- 61.Andrade DM, Krings T, Chow EW, et al. Hippocampal malrotation is associated with chromosome 22q11.2 microdeletion. Can J Neurol Sci. 2013;40:652–6. doi: 10.1017/s0317167100014876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Qiu A, Tuan TA, Woon PS, et al. Hippocampal-cortical structural connectivity disruptions in schizophrenia: an integrated perspective from hippocampal shape, cortical thickness, and integrity of white matter bundles. Neuroimage. 2010;52:1181–9. doi: 10.1016/j.neuroimage.2010.05.046. [DOI] [PubMed] [Google Scholar]
- 63.Szeszko PR, Strous RD, Goldman RS, et al. Neuropsychological correlates of hippocampal volumes in patients experiencing a first episode of schizophrenia. Am J Psychiatry. 2002;159:217–26. doi: 10.1176/appi.ajp.159.2.217. [DOI] [PubMed] [Google Scholar]
- 64.Narr KL, Thompson PM, Szeszko P, et al. Regional specificity of hippocampal volume reductions in first-episode schizophrenia. Neuroimage. 2004;21:1563–75. doi: 10.1016/j.neuroimage.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 65.Weiss AP, Dewitt I, Goff D, et al. Anterior and posterior hippocampal volumes in schizophrenia. Schizophr Res. 2005;73:103–12. doi: 10.1016/j.schres.2004.05.018. [DOI] [PubMed] [Google Scholar]
- 66.Kates WR, Antshel KM, Faraone SV, et al. Neuroanatomic predictors to prodromal psychosis in velocardiofacial syndrome (22q11.2 deletion syndrome): a longitudinal study. Biol Psychiatry. 2011;69:945–52. doi: 10.1016/j.biopsych.2010.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Schumann CM, Hamstra J, Goodlin-Jones BL, et al. Hippocampal size positively correlates with verbal IQ in male children. Hippocampus. 2007;17:486–93. doi: 10.1002/hipo.20282. [DOI] [PubMed] [Google Scholar]