Abstract
Although the skin production of vitamin D is initiated by ultraviolet radiation type B (UVB), the role vitamin D plays in antioxidative or pro-oxidative responses remains to be elucidated.. We have used immortalized human HaCaT keratinocytes as a model of proliferating epidermal cells to test the influence of vitamin D on cellular response to H2O2 or the anti-cancer drug, cisplatin. Incubation of keratinocytes with 1,25(OH)2D3 or its low calcemic analogues, 20(OH)D3, 21(OH)pD or calcipotriol, sensitized cells to ROS resulting in more potent inhibition of keratinocyte proliferation by H2O2 in the presence of vitamin D compounds. These results were supported by cell cycle and apoptosis analyses, and measurement of the mitochondrial transmembrane potentials (MMP), however some unique properties of individual secosteroids were observed. Furthermore, in HaCaT keratinocytes treated with H2O2, 1,25(OH)2D3, 21(OH)pD and calcipotriol stimulated the expression of SOD1 and CAT genes, but not SOD2, indicating a possible role of mitochondria in ROS-modulated cell death. 1,25(OH)2D3 also showed a short-term, protective effect on HaCaT keratinocytes, as exemplified by the inhibition of apoptosis and the maintenance of MMP. However, with prolonged incubation with H2O2 or cisplatin, 1,25(OH)2D3 caused an acceleration in the death of the keratinocytes. Therefore, we propose that lead vitamin D derivatives can protect the epidermis against neoplastic transformation secondary to oxidative or UV-induced stress through activation of vitamin D-signaling. Furthermore, our data suggest that treatment with low calcemic vitamin D analogs or the maintenance of optimal level of vitamin D by proper supplementation, can enhance the anticancer efficacy of cisplatin
Keywords: vitamin D, vitamin D analogues, keratinocytes, reactive oxygen species, oxidative stress, cisplatin
Vitamin D is a secosteroid produced in the skin via UVB-induced photolysis of 7-dehydrocholesterol (7-DHC), or obtained in limited quantities through the diet [1, 2]. Regardless of the source, vitamin D undergoes activation through two subsequent hydroxylations comprising 25-hydroxylation by CYP2R1 or CYP27A1, predominantly in the liver, followed by 1α-hydroxylation in the kidney by CYP27B1, resulting in the fully active form, 1,25(OH)2D3 (also known as calcitriol) [3]. Apart from kidneys, multiple human organs, including the skin, express CYP27B1 and have the capacity to 1α-hydroxylate 25-hydroxyvitamin D3 [4]. Moreover, the skin is the only organ equipped with all elements necessary for the synthesis, activation, and catabolism of vitamin D, as well as responding to it via the vitamin D receptor (VDR) [2, 5].
Recently, novel pathways of vitamin D metabolism and activation have been established that are initiated by CYP11A1, also known as cytochrome P450scc [6–14]. Briefly, CYP11A1 converts 7-DHC to 7-dehydropregnenolone (7-DHP) via sequential hydroxylations of 7-DHC at C-22 and C-20 followed by cleavage of its side chain [7, 12]. 7-DHP is further modified in this pathway by the classical enzymes of steroid metabolism resulting in 5,7-diene-analogues, some of which have been detected in vivo [15, 16]. In vitro studies have shown that these 5,7-dienes can be converted to the corresponding vitamin D analogues following UVB irradiation [9–11]. Several of these new derivatives, which have a short side chain compared to vitamin D3, display biological activity [6, 10, 11, 15, 17]. In contrast, CYP11A1 acts directly on vitamin D to produce hydroxyvitamin D derivatives which retain a full-length side chain, with these products being detected both in vitro [12–14, 18, 19] and in vivo [20, 21]. The hydroxyvitamin D3 metabolites produced by these pathways, including the major product, 20(OH)D3, are biologically active in both in vitro (reviewed in [8]) and in vivo [22] models. Since they are less prone to induce hypercalcemia than 1,25(OH)2D3 [23, 24], they deserve special attention as potential therapeutics for the treatment of leukemia [23], melanoma [10, 11, 25, 26] and colorectal cancer [27].
1,25(OH)2D3 may exert its effects through both genomic and non-genomic mechanisms [28]. The genomic pathway relies on binding to the intracellular vitamin D receptor (VDR), a member of the nuclear receptor superfamily [29, 30]. The binding of ligand to VDR triggers its heterodimerization with retinoid X receptor and interaction with vitamin D responsive elements (VDREs) in the promoter regions of vitamin D-regulated genes [29, 31]. It is estimated that vitamin D regulates as many as 3000 genes in the human genome [28]. In addition, 1,25(OH)2D3 may also elicit rapid responses, independent of the modulation of gene expression, associated with several signal transduction pathways which lead to production of second messengers or to modulation of the intracellular calcium concentration [2, 28]. Rapid responses to 1,25(OH)2D3 have been reported to involve plasma-membrane localized VDR [28, 32] or other receptors such as MARRSBP (1α,25(OH)2D membrane–associated rapid response steroid-binding protein), also described as PDIA3 (protein-disulfide isomerase-associated 3) and ERp57 (endoplasmic reticulum stress protein 57) [32, 33]. Most recently, retinoic acid orphan receptors (RORα and γ) have been identified as alternative receptors for D3 hydroxy-derivatives which act as reverse agonists [34].
Vitamin D exerts wide spread pleiotropic effects that are additional to its well known involvement in the regulation of calcium homeostasis [3, 35–39]. The noncalcemic effects of vitamin D include direct and indirect regulation of the cell cycle and proliferation, differentiation and apoptosis [40–45]. Therefore, it is not surprising, that vitamin D analogues are being considered for use in cancer prevention and treatment [1]. Numerous epidemiological studies and preclinical data support this proposed use [1, 46–57].
The epidermis is formed predominantly by multiple layers of keratinocytes at different stage of differentiation. This outer most part of the skin provides a protective barrier separating internal organs from the harsh outside environment [5]. Recent data indicate that biologically active forms of vitamin D3 play an important role in protection against DNA damage [21, 58, 59] and UVB-induced carcinogenesis in the epidermis [60–63]. These protective effects are also seen for the novel, CYP11A1-derived hydroxy-derivatives of vitamin D as demonstrated in human epidermal cells [21], and mouse skin in vivo [64]. Since the predominant effect of UVA irradiation, which has no effect on cutaneous vitamin D production, is to generate reactive oxygen species (ROS), active forms of vitamin D may accelerate elimination of cells with neoplastic potential induced by ROS, which would be consistent with their role as protectors of epidermal integrity [65]. Here we have documented the relationship between vitamin D and oxidative stress in human epidermal keratinocytes, and their interplay with the anticancer drug, cisplatin.
2. MATERIAL AND METHODS
Chemicals
1,25(OH)2D3, hydrogen peroxide (30%) and cisplatin were purchased from Sigma-Aldrich (Poznan, Poland). 21(OH)pD was synthesized according to the procedure described by Żmijewski et al. [11] by ProChimia Surfaces Sp. Z o.o. (Poland). 20(OH)D3 was synthesized and purified as described previously [13, 18]. Calcipotriol was a kind gift from the Pharmaceutical Research Institute (Warsaw, Poland). Other chemicals were purchased from Sigma-Aldrich (Poznan, Poland) or as indicated.
Cell culture
Human immortalized keratinocytes (HaCaT) were cultured in DMEM medium supplemented with 10% fetal bovine serum (FBS) and 1% penicillin/streptomycin. Charcoal-stripped fetal bovine serum was used for all experimental procedures where the effects of vitamin D compounds were examined in order to eliminate the influence of serum-derived vitamin D or other steroids.
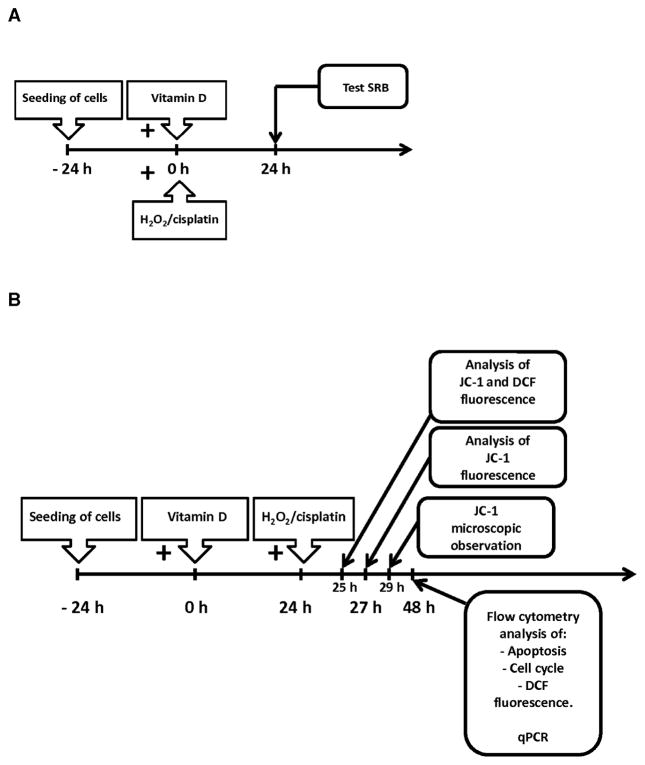
For proliferation assays, cell were seeded in 96 well plates and after 24 h were treated with hydrogen peroxide or vitamin D compounds separately or with hydrogen peroxide and selected vitamin D derivatives in pairs (Scheme 1A). All other experiments were performed according to schema 1B. Briefly, cells were preincubated for 24 h with selected secosteroids and then treated with H2O2 for an additional 24 h or as indicated.
Scheme 1.
Overview of experimental protocols for treatment of human immortalized keratinocytes (HaCaT) and their subsequent analysis. (A, SRB analysis; B, flow cytometry and real time PCR).
Proliferation assay
The SRB analysis used relies on the uptake of the negatively charged pink aminoxanthine dye, sulphorhodamine B (SRB), by basic amino acids in the cells and thus measures protein content and indirectly reflects the number of cells in the culture. Experiments were performed as described before [26]. Briefly, HaCaT keratinocytes were seeded in 96-well plates (8,000 per well), cultured for 24 h and then treated with serial dilutions of the compounds being tested for an additional 24 h (Scheme 1A). Cells were fixed with 10% trichloroacetic acid (TCA) for 1 h at 4°C. Plates were washed five times with distilled water and air-dried. Staining solution comprising 0.4% SRB in acetic acid was added to each well and after 15 min plates were washed with 1% acetic acid five times and air-dried. SRB dye was solubilized using a solution of 10 mM buffered Tris Base (pH 10.5) and absorbance measured at 570 nm using an Epoch spectrophotometer (BioTek, Winooski, USA).
Cell cycle analysis
The cell cycle was analyzed by quantification of DNA content by flow cytometry. Cells (trypsinized and cells from culture medium as well) were fixed in 70% ethanol and kept for 24 – 48 h at 4°C. Cells were treated with ribonuclease in order to remove any contaminating RNA and DNA was stained with propidium iodide (PI). Fluorescence of the PI-stained cells was measured by flow cytometry (Ex 536 nm, Em 617 nm, FACSCalibur, Becton Dickinson, Franklin Lakes, USA). Results were analyzed by CellQuest Pro Software (Becton Dickinson, Franklin Lakes, USA) and expressed as a percentage of cells with DNA content corresponding to apoptotic/necrotic cells (subG1 fraction) or cells in G1, S and G2/M phases of the cycle.
Apoptosis Assay
A PE Annexin V Apoptosis Detection Kit (Becton Dickinson 559763, Franklin Lakes, USA) was used to quantitatively determine the percentage of cells that were actively undergoing apoptosis. Briefly, after performing the experiment according to scheme B in 6 well-plates, cells were harvested, washed twice with PBS and stained according to the manufacturer’s protocol. The fluorescence of PE Annexin V and 7-AAD was measured by flow cytometry (FACSCalibur, Becton Dickinson, Franklin Lakes, USA) and data analyzed using CellQuest Pro software (Becton Dickinson, Franklin Lakes, USA).
Measurement of changes in mitochondrial potential
The detection of changes in mitochondrial inner membrane electrochemical potential (Δψ) in living cells was performed using the cationic, lipophilic dye, JC-1 (5,5′,6,6′-tetrachloro-1,1′,3,3′ tetraethylbenzimidazolylcarbocyanine iodide, T-3168, Life Technologies, Carlsbad, USA). In untreated, “healthy” cells the dye accumulates in the mitochondrial matrix forming red fluorescent aggregates. After depletion of the electrochemical potential, the dye disperses throughout the cell and results in a shift from red to green fluorescence (JC-1 monomers). CCCP (carbonyl cyanide 3-chlorophenylhydrazone, C2759 Sigma, Poznan, Poland), a mitochondrial potential disrupter, was used as a control. After treatment with selected compounds (as shown in Scheme 1B and described in Results), cells were harvested and suspended in 1 ml warm PBS. CCCP solution in DMSO was added to the control tube only (2 μM final concentration) and cells incubated at 37°C for 5 min. JC-1 solution (in DMSO, 2 μM final concentration) was added to all tubes and cells were incubated at 37°C for 15 min, then centrifuged and resuspended in 500 μl of PBS. Samples were kept on ice and analyzed on the FACSCalibur flow cytometer (Becton Dickinson, Franklin Lakes, USA) using CellQuest Pro analysis software (Becton Dickinson, Franklin Lakes, USA). For microscopic observation, cells were seeded in 8-well slide chambers (Nunc Lab-Tek) and incubated as described above except that after the treatment with 1,25(OH)2D3 (100 nM, 24 h) and H2O2 (2 mM, 5 h), cells were washed with PBS and incubated in DMEM supplemented with JC-1 (2.5 μg/mL) for an additional 30 min at 37°C. Living cells were observed and photographed using the fluorescence microscope, Axiovert 200 (magnification 200x). For control experiments, 1,25(OH)2D3 and/or hydrogen peroxide treatments were omitted. For positive controls, cells were treated with CCCP at a final concentration of 2 μM for 5 min at room temperature. Images were acquired from 5–10 randomly chosen fields for each experimental condition showing nuclear cross-sections. Green and red channels were merged and the red/green ratio was shown in blue.
Detection of the production of intracellular reactive oxygen species
The intracellular production of reactive oxygen species (ROS) was measured using H2DCFDA (D399, Life Technologies, Carlsbad, USA). Cells were incubated with 100 nM 1,25(OH)2D3 for 24 h followed by exposure to 1 mM hydrogen peroxide for 1 h or 24 h (Scheme 1B). Thirty minutes before the end of the incubation, H2DCFDA was aded to a final concentration of 10 μM. Cells were washed and suspended in cold PBS. Samples were kept on ice and analyzed using the FACSCalibur flow cytometer (Becton Dickinson, Franklin Lakes, USA) using CellQuest Pro analysis software (Becton Dickinson, Franklin Lakes, USA).
Measurement of mRNA levels
The relative mRNA levels of particular genes were determined by Real-Time PCR (qPCR). Total RNA was isolated using the Total RNA Prep Plus kit (A&A Biotechnology, Gdynia, Poland), according to the manufacturer’s instructions. The concentration and quality of RNA samples were determined spectrophotometrically (Epoch BioTek, Winooski, USA). One microgram of RNA was used for reverse transcription using a RevertAid™ First Strand cDNA Synthesis Kit (Thermo Scientific, Waltham, USA). The qPCR reaction comprised 1 μL cDNA, 150 nM of each primer and Real-Time PCR Mix SYBR B (A&A Biotechnology, Gdynia, Poland) and was performed using Step One Plus (Life Technologies-Applied Biosystems, Grand Island, USA) in total volume of 20 μL. The reactions were run in duplicate and the resulting data were averaged prior to analysis with Step One Plus ver. 2.2.2. software (Life Technologies-Applied Biosystems, Grand Island, USA). The RPL37 gene was used as a control to normalize the values by the ΔΔCt quantification method.
Statistical analyses
Statistical analysis was performed using Microsoft Excel or GraphPad Prism v6.03 (GraphPad Software, San Diego, CA, USA). Data were subjected to Student’s t-test (for two groups) or one-way analysis of variance and appropriate post hoc test (the ANOVA Kruskal–Wallis test for comparison of several groups). Data are expressed as mean ± S.D. Each experiment was repeated at least three times in triplicate. Differences are shown as significant at p<0.05, p<0.01 or p<0.001, as indicated.
3. RESULTS
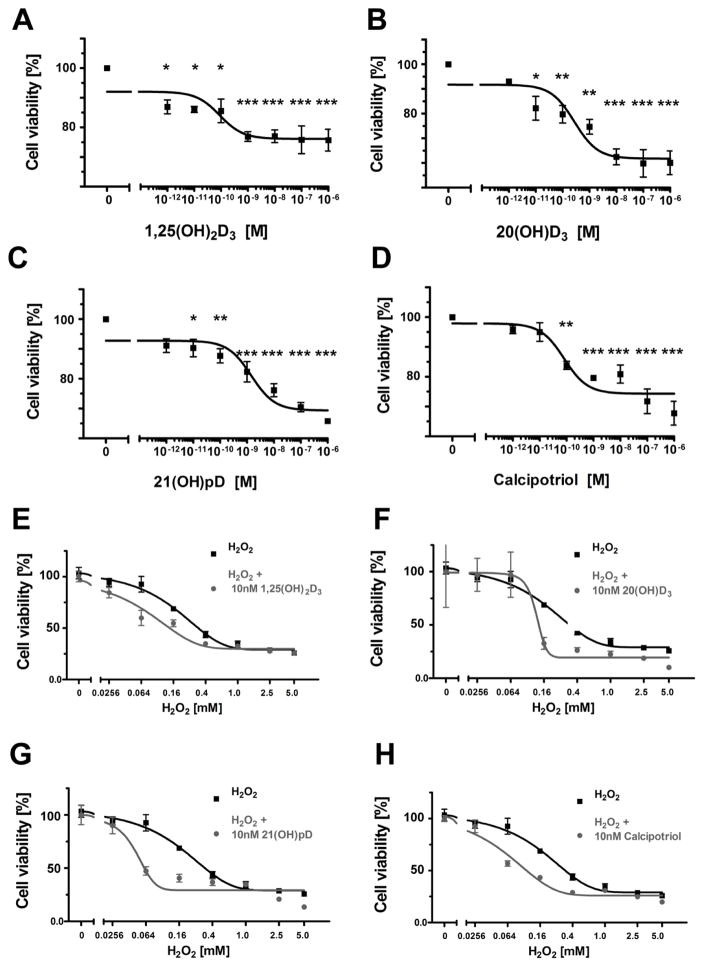
3.1. Vitamin D analogues enhance the cytotoxic effects of hydrogen peroxide on HaCaT cells
We tested the effect of the vitamin D compounds 1,25(OH)2D3, 20(OH)D3, 21(OH)pD and calcipotriol, on the sensitivity of human HaCaT keratinocytes to reactive oxygen species. As expected, these compounds [8, 19, 66] inhibited the proliferation of HaCaT keratinocytes as determined using the Sulphrodamin B assay (SRB) (Figure 1A–D). IC50 values ranged from 1.44 nM for 21(OH)pD to approximately 0.1 nM for the other secosteroids (Table 1). Hydrogen peroxide (H2O2) chosen as the agent to promote oxidative stress, inhibited the growth of HaCaT cells with an IC50 of 186 nM. 1,25(OH)2D3, 20(OH)D3, 21(OH)pD and calcipotriol decreased the IC50 observed with H2O2, thus enhancing their sensitivity to H2O2 (Figure 1E–H), with the strongest effect being seen for 21(OH)pD where the IC50 decreased 3.8 fold. (Table 1).
Figure 1.
The effect of Vitamin D compounds on the proliferation of HaCaT keratinocytes treated with hydrogen peroxide. HaCaT keratinocytes were treated with serial dilutions (10−12–10−6 M) of 1,25(OH)2D3 (A), 20(OH)D3 (B), 21(OH)pD (C) or calcipotriol (D), or were treated with serial dilutions of H2O2 (0.0256–5 mM) alone or in combination with 10 nM 1,25(OH)2D3 (E), 20(OH)D3 (F), 21(OH)pD (G) or calcipotriol (H) for 24 h (according to Scheme 1A). Data are shown as mean from three independent experiments ± S.D. Statistical significance was estimated using One–Way ANOVA and presented as *p < 0.05, **p < 0.005, ***p < 0.0005 versus control. Please note that the same curve showing the response to H2O2 alone was included into panels E – H in order to underline the effects of co-incubation with vitamin D analogues.
Table 1.
Summary of IC50 values for inhibition of proliferation of HaCaT keratinocytes. IC50 measurements were carried out as described in Figure 1.
| Compound | IC50 [nM] Secosteroid | IC50 [nM] H2O2 |
|---|---|---|
| H2O2 | - | 186 |
| 1,25(OH)2D3 | 0.089 | 72 |
| 20(OH)D3 | 0.274 | 120 |
| 21(OH)pD | 1.44 | 49 |
| Calcipotriol | 0.081 | 63 |
3.2. Preincubation of HaCaT cells with vitamin D compounds sensitizes them to hydrogen peroxide treatment
We investigated whether pretreatment with vitamin D compounds sensitize HaCaT keratinocytes to H2O2, using flow cytometry. HaCaT keratinocytes were pretreated with secosteroids (100 nM) for 24 h and then subjected to 1 mM H2O2 for an additional 24 h. To ensure that maximal stimulation was achieved, secosteroids were tested at concentrations which approximately corresponded to the concentration of 25(OH)D3 in the plasma (75–125 nM) [67]. It should be noted, however, that serum level of 1,25(OH)2D3 concentration in humans is less than 1 nM [68].
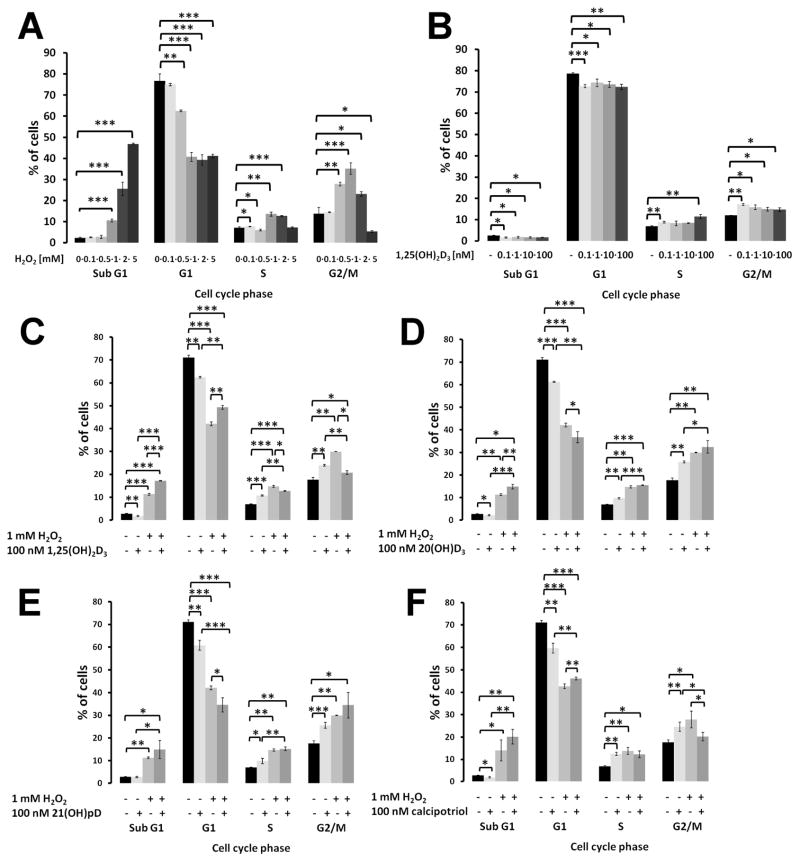
Treatment of HaCaT keratinocytes with H2O2, alone, resulted in a dose-dependent decrease in the number of cells at the G0/G1 phase and an increase in the number of SubG1 cells, indicating induction of apoptosis (Figure 2A). Interestingly, an increase in the number of cells in the G2/M phase was observed in HaCaT cells with increasing H2O2 concentrations, up to 1 mM, suggesting inhibition of the mitotic process by H2O2. 1,25(OH)2D3 had only minor effects on the distribution of HaCaT cells in the different phases of cell cycle, with a statistically significant decrease in the number of cells in the subG1 and G1 phases compared to control cells (Figure 2B).
Figure 2.
Effect of vitamin D compounds and hydrogen peroxide on the distribution of HaCaT keratinocytes through the cell cycle. HaCaT cells were treated with hydrogen peroxide (0.1 – 5 mM) (A) or with 1,25(OH)2D3 (0.1 – 100 nM) for 24 h. HaCaT keratinocytes were also preincubated with 100 nM 1,25(OH)2D3 (C), 20(OH)D3 (D), 21(OH)pD (E) or calcipotriol (F)) for 24 h, and subsequently exposed to 1 mM hydrogen peroxide for an additional 24 h (according to Scheme 1B). Cells were harvested, stained with propidium iodide and analyzed by Flow Cytometry. Data are presented as mean ± S.D. of three independent experiments carried out in triplicate. *p<0,05; **p<0,01; ***p<0,001 vs. control.
All vitamin D compounds tested had only a slight effect on the distribution of HaCaT keratinocytes in the cell cycle with a decrease in the number of cells in the G1/G0 phase and an increase in the S and G2/M phases. Interestingly, all the secosteroids except 21(OH)pD protected cells against apoptosis as illustrated by the decrease in the subG1 fraction. Furthermore, preincubation of HaCaT keratinocytes for 24 h with 1,25(OH)2D3 or calcipotriol, prior to H2O2 treatment for 24 h, resulted in an increase in the percentage of cells in the G0/G1 phase in comparison to cells without pretreatment (7% and 3.5%, respectively; P <0.01; Figure 2, panels C and F). Curiously, pretreatment with 20(OH)D3 or 21(OH)pD had the opposite effect with the fraction of cells in the G0/G1 phase being elevated by 5% and 7.5%, respectively, compared to cells treated with hydrogen peroxide only (p <0.05; Figure 2, panels D and E). Furthermore, pretreatment with the secosteroids was accompanied by a proportional decrease in the number of cells in S and G2/M phases for 1,25(OH)2D3 and calcipotriol, and an increase for 20(OH)D3 and 21(OH)pD (Figure 2C and F). For all the secosteroids used for pretreatment, there was a trend to increase the percentage of cells in the SubG1 phase following H2O2 treatment (p <0.001 for 1,25(OH)2D3 p <0.01 for 20(OH)D3), although for 21(OH)pD and calcipotriol the effect was not statistically significant.
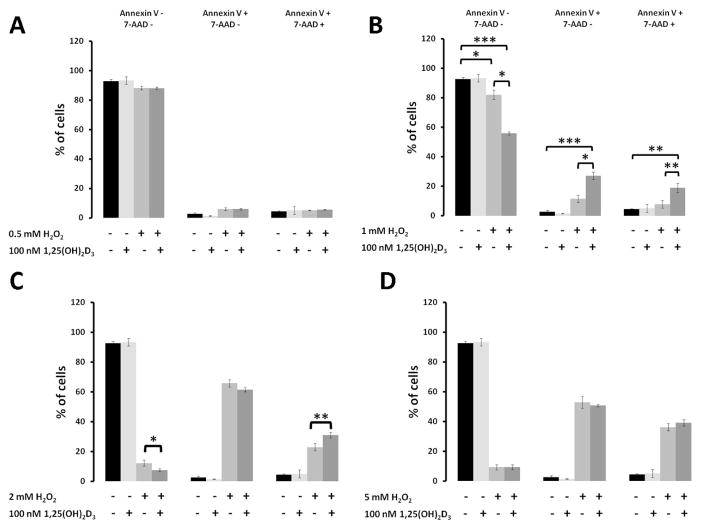
3.3. Preincubation with 1,25(OH)2D3 amplifies apoptotic and necrotic events in HaCaT cells exposed to H2O2
Preincubation of HaCaT keratinocytes with vitamin D compounds led to an increase in the percentage of cells in the SubG1 fraction following H2O2 treatment (Fig. 2). To define whether these effects are related to either necrosis or apoptosis, HaCaT keratinocytes were preincubated with secosteroids and subsequently with H2O2 (Schema 1B). Then presence of apoptotic or necrotic cells were evaluated by simultaneous staining with Annexin V and 7-AAD and flow cytometry (Figure 3). Incubation of HaCaT keratinocytes with H2O2, alone, for 24 h resulted in a dose-dependent induction of both apoptosis (Annexin V+ and 7-AAD-cells) and necrosis (Annexin V+ and 7-AAD+ cells). Apoptosis was induced at lower concentrations of H2O2 (≤1 mM) than for necrosis (2 to 5 mM). Interestingly, an amplifying effect of 1,25(OH)2D3 on the pro-apoptotic activity of hydrogen peroxide was only observed for 1 mM H2O2. While 1 mM H2O2 alone had only a limited effect on the induction of apoptosis (Annexin V+ and 7-AAD-cells), pretreatment with 100 nM 1,25(OH)2D3 effectively enhanced both apoptosis and necrosis of keratinocytes (Figure 3B). Pretreatment with 1,25(OH)2D3 stimulated necrosis, but not apoptosis, in keratinocytes treated with 2 mM H2O2 (Figure 3C) and had no effect at 5 mM H2O2 (Figure 3D). The lack of effect of 1,25(OH)2D3 on keratinocytes treated with the highest concentration of H2O2 might be explained by the fact that 5 mM H2O2, alone, was sufficient to induce cell death in the majority of keratinocytes.
Figure 3.
The effect of hydrogen peroxide on the induction of apoptosis in HaCaT keratinocytes pretreated with 1,25(OH)2D3. HaCaT cells were treated with 100 nM 1,25(OH)2D3 for 24 h and subsequently exposed to 0.5 mM (A), 1 mM (B), 2 mM (C) or 5 mM (D) hydrogen peroxide for an additional 24 h (according to Scheme 1B). Cells were harvested, stained with AnnexinV/7-Aminoactinomycin and analyzed by Flow Cytometry. Data are presented as mean ± S.D. of three independent experiments carried out in triplicate. *p<0,05; **p<0,01; ***p<0,001 vs. control.
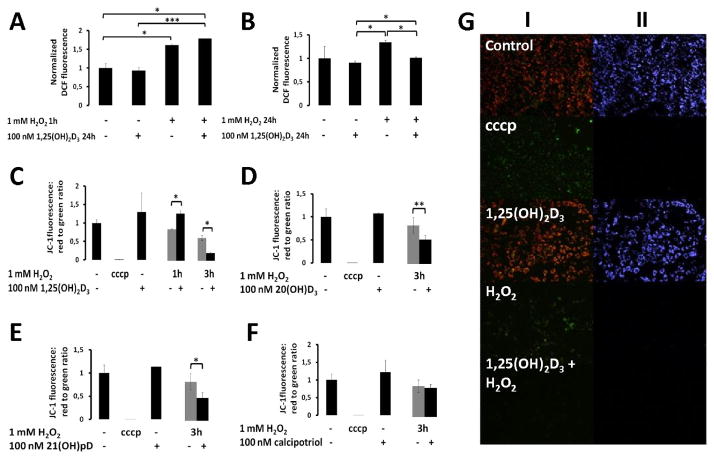
3.4. Pretreatment with vitamin D compounds affects H2O2-induced production of reactive oxygen species and changes in the mitochondrial membrane potential
Pretreatment of keratinocytes with 1,25(OH)2D3 did not significantly influence the production of reactive oxygen species (ROS), as measured by H2DCFDA (Figure 4A and B). However, preincubation of cells with the secosteroids affected ROS production after treatment with H2O2 and this effect was time dependent. Pretreatment with 1,25(OH)2D3 had no statistically significant effect on ROS production in keratinocytes treated with H2O2 for one hour. However, prolongated exposition to H2O2 (24 h treatment) resulted in a significant decrease of the ROS levels in keratinocytes pretreated with 1,25(OH)2D3 in comparison to untreated controls (Figure 4B).
Figure 4.
Effect of secosteroid preteatment on reactive oxygen levels and on mitochondrial transmembrane potential. HaCaT cells were treated with 100 nM 1,25(OH)2D3 for 24 h, and subsequently exposed to 1 mM hydrogen peroxide for 1 h (A) or for 24 h (B) (according to Scheme 1B). Cells were stained with H2DCFDA and analyzed by Flow Cytometry. HaCaT cells were also preincubated with 1,25(OH)2D3 (C), 20(OH)D3 (D), 21(OH)pD (E) or with calcipotriol (F) for 24 h followed by exposure to 1 mM hydrogen peroxide for 1 h or 3 h, then stained with JC-1 and analyzed by Flow Cytometry (according to Scheme 1B). Data are presented as mean ± S.D. of three independent experiments carried out in triplicate. *p<0,05; **p<0,01; ***p<0,001 vs. control. The image (G) shows the relative changes in mitochondrial membrane potentials which are expressed as shifts from red to green fluorescence (I) or the red to green ratio that produces blue fluorescence (II). Cells were incubated with 100 nM 1,25(OH)2D3 for 24 h and subsequently exposed to 2 mM hydrogen peroxide for 5 h (according to Scheme 1B). The positive control (cccp) was exposed to cccp for 5 min before staining with JC-1.
Previously, we reported that H2O2 treatment of human HaCaT keratinocytes resulted in a decrease in the mitochondrial membrane potential, Δψ [69]. Our initial studies on JC-1 stained cells (Δψ indicator) showed that incubation of cells with 1,25(OH)2D3 alone resulted in an increase in Δψ and, furthermore, pretreatment of cells with 1,25(OH)2D3 prevented a H2O2-triggered decrease in Δψ (Figure 4G). Next, JC1-stained cells were analysed by flow cytometry (Figure 4C–F). A protective effect of pretreatment with 1,25(OH)2D3 as relates to Δψ was observed only after a short (1 h) incubation of cells with 1 mM H2O2 (Figure 4B). However prolonged (3 h) incubation with H2O2 of 1,25(OH)2D3-pretreated keratinocytes (Figure 4C) resulted in a statistically significant decrease in the mitochondrial membrane potential, Δψ, in comparison to cells treated solely with H2O2. The 24-h preincubation with the low-calcemic vitamin D analogues, 20(OH)D3, 21(OH)pD or calcipotriol (all at 100 nM concentrations) resulted in a trend towards an elevation of Δψ, however the data did not reached statistical significance. Similar to 1,25(OH)2D3, pretreatment of cells with 20(OH)D3 or 21(OH)pD for 24 h prior to a 3 h incubation with 1 mM H2O2, decreased Δψ, whereas calcipotriol did not have a significant effect (Figure 4F).
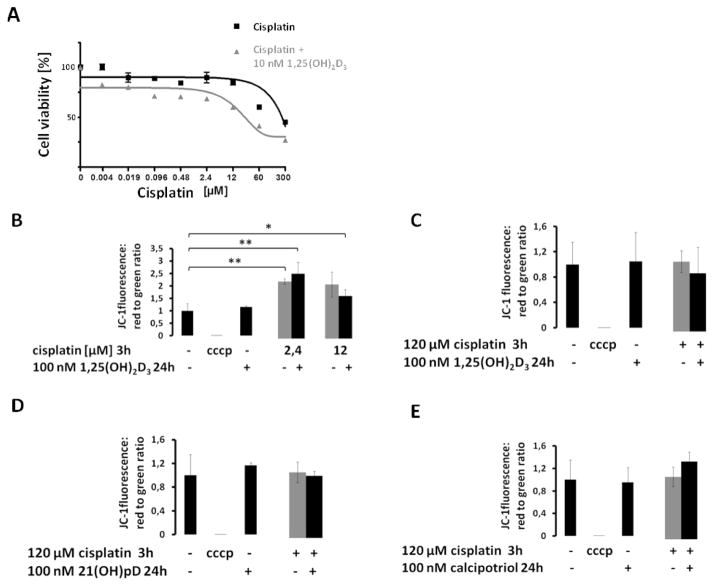
3.5. Vitamin D compounds modulate the sensitivity of keratinocytes to cisplatin
Cisplatin is a well-known anticancer drug, which in addition to its ability to intercalate with DNA, can induce production of ROS [70]. It is considered in combinational therapy of skin cancer including metastatic basal cell carcinoma [71]. Cisplatin can induce apoptosis of HaCaT cells by a hydroxyl-radical mediated mechanism [72]. Simultaneous treatment with 1,25(OH)2D3 (100 nM) and cisplatin (0.00384 to 300 μM) decreased the IC50 for the antiproliferative effect of cisplatin almost three fold (17.1 μM for cisplatin + 1,25(OH)2D3 vs 46.4 μM for cisplatin alone), as measured by the SRB assay (Figure 5A). Interestingly, cisplatin treatment did not cause a rapid induction of apoptosis. Instead, as shown by cell cycle analysis, treatment of HaCaT keratinocytes with both 12 and 120 μM cisplatin resulted in a significant decrease in the number of cells in the G1/G0 phase, which was coincidental with an increase in the proportion in the G2/M phase (Tabele 2 and 3). In addition, treatment of HaCaT keratinocytes with a high concentration of cisplatin (120 μM) resulted in an increase in the percentage of cells in the S phase of the cell cycle. Pretreatment of HaCaT keratinocytes with 1,25(OH)2D3 or calcipotriol amplified the effects of cisplatin with a significantly higher proportions of cells in the G2/M phase, and in the S phase for calcipotriol. However, the effects on the G2/M phase were not seen with the short side-chain analog, 21(OH)pD, for which only a small protective effect was observed in the S phase with the higher concentration of cisplatin (120 nM) (Table 3).
Figure 5.
The effect of vitamin D compounds on the sensitivity of HaCaT keratinocytes to cisplatin. Panel A, HaCaT keratinocytes were treated with serial dilutions of cisplatin (0.004 – 300 μM) or were exposed to 10 nM cisplatin simultaneously with 100 nM 1,25(OH)2D3 for 24 h. Cell proliferation was measured using the SRB assay. Data are represented as mean normalized absorbance (at 570 nm) from three independent experiments ± S.D. Panels B – E, cells were treated with 100 nM 1,25(OH)2D3 (B and C), 21(OH)pD (D) or calcipotriol (E) for 24 h and subsequently with 2.4 or 12 μM (B), or 120 μM cisplatin (C – E) for an additional 3 h. Cells were harvested, stained with JC-1 and Δψ analyzed by Flow Cytometry. Data are presented as mean ± S.D. of three independent experiments performed in triplicate. *p<0,05; **p<0,01 vs. control.
Tabele 3.
Effect of vitamin D compounds and cisplatin on the distribution of HaCaT keratinocytes through the cell cycle. HaCaT cells were treated with 100 nM 1,25(OH)2D3, 21(OH)pD or calcipotriol for 24 h, and subsequently exposed to 120 μM cisplatin for an additional 24 h. Cells were harvested, stained with propidium iodide and the distribution of cells in the cell cycle analyzed by Flow Cytometry. Data are presented as mean ± S.D. of three independent experiments carried out in triplicate.
| Sub G1 | G1 | S | G2/M | |
|---|---|---|---|---|
| Control | 7.16 ± 0.68 | 64.38 ± 1.32 | 9.13 ± 0.55 | 18.11 ± 1.31 |
| Cisplatin | 3.75 ± 0.46** | 46.55 ± 1.72*** | 25.33 ± 0.43*** | 23.70 ± 1.06** |
| 1,25(OH)2D3 | 3.51 ± 0.15** | 70.41 ± 0.37** | 7.47 ± 0.29** | 17.80 ± 0.43 |
| 1,25(OH)2D3 + cisplatin | 8.29 ± 0.78## | 21.62 ± 1.16**; ### | 15.97 ± 1.61**; ## | 51.26 ± 3.39***; ## |
| 21(OH)pD | 8.10 ± 1.88 | 64.17 ± 2.09 | 9.03 ± 0.13 | 18.08 ± 1.02 |
| 21(OH)pD + cisplatin | 3.56 ± 0.56** | 54.19 ± 0.35**; ### | 20.42 ± 0.20***; ### | 22.25 ± 1.11** |
| Calcipotriol | 3.54 ± 0.27** | 69.48 ± 0.87** | 8.02 ± 0.38* | 17.95 ± 0.19 |
| Calcipotriol + cisplatin | 3.27 ± 0.09** | 42.76 ± 1.03***; ## | 28.53 ± 0.72***; ## | 25.84 ± 0.95***; # |
p<0,05;
p<0,01;
p<0,001 vs. control;
- cisplatin versus cisplatin + vitamin D.
Low concentrations of cisplatin (2.4 μM and 12 μM) induced an increase in Δψ for HaCaT keratinocytes after 3 h of incubation (Figure 5B). However, treatment of HaCaT keratinocytes with a higher concentration of cisplatin (120 μM) had no effect on Δψ. Pretreatment of the cells with the secosteroids did not significantly alter Δψ following treatment with cisplatin under the experimental conditions used (Figure 5C–E).
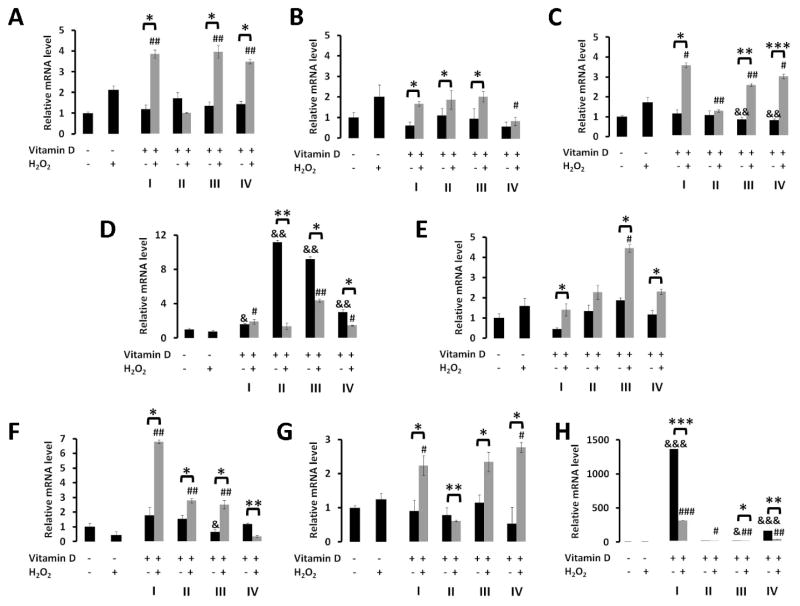
3.6. Vitamin D compounds modify the expression of genes involved in removal of ROS, following H2O2 treatment
We tested whether vitamin D compounds can modulate expression of ROS related genes including superoxide dismutase types I and II (SOD1 and SOD2), and catalase (CAT). Pretreatment of HaCaT keratinocytes with 1,25(OH)2D3, 20(OH)D3, 21(OH)pD or calcipotriol had limited effects on the mRNA levels of selected ROS related genes (SOD1, SOD2, CAT). Pretreatment with 21(OH)pD and calcipotriol resulted in a small but statistically significant decrease in catalase (CAT) gene expression (Figure 6C). As expected, treatment of HaCaT keratinocytes with 1 mM H2O2 alone resulted in an increase of SOD1, SOD2 and CAT mRNA levels (p<0.01 for SOD1, p<0,001 for SOD2, p<0,05 for CAT). Pretreatment of HaCaT keratinocytes with the vitamin D analogues (10 nM) for 24 h, prior to treatment with 1 mM H2O2, had variable effects on mRNA level of the genes under investigation. These secosteroids, except 20(OH)D3, significantly stimulated the H2O2-mediated expression of SOD1 and CAT, while 20(OH)D3 pretreatment resulted in a significant decrease in mRNA levels for these genes. Pretreatment of HaCaT keratinocytes with calcipotriol resulted in a decrease in the mRNA level for SOD2.
Figure 6.
Effects of hydrogen peroxide on SOD1(A), SOD2(B), CAT (C), VDR (D), PDIA3 (E), CYP3A4 (F), CYP27B1 (G) and CYP24A1 (H) gene expression in HaCaT keratinocytes pretreated with vitamin D compounds. HaCaT cells were incubated with 10 nM 1,25(OH)2D3 (I), 20(OH)D3 (II), 21(OH)pD (III) or calcipotriol (IV) for 24 h followed by exposure to 1 mM hydrogen peroxide for an additional 24 h. mRNA levels were masured by qPCR. Data are shown as means ± S.D of three independent experiments carried out in duplicate. *p<0,05; **p<0,01; ***p<0,001 vs. control; # - H2O2 versus H2O2 + vitamin D; & - vitamin D versus control.
3.7. The effect of preincubation of HaCaT keratinocytes with vitamin D compounds on the expression of genes related to vitamin D action or metabolism, prior to H2O2 treatment
Pretreatment of HaCaT keratinocytes with the secosteroids under study increased VDR mRNA levels, with the strongest effect (approximately 10-fold induction) being observed in cells treated with 20(OH)D3 and 21(OH)pD (Figure 6D). H2O2 treatment alone did not have a significant effect on the expression of the VDR. However, in HaCaT keratinocytes pretreated with vitamin D compounds, H2O2 caused a significant attenuation of the stimulation of VDR expression caused by the secosteroids, with the exception being for 1,25(OH)2D3.
The pretreatment of HaCaT keratinocytes with the vitamin D compounds, or treatment with 1 mM H2O2, had a marginal effect on the expression of PDIA3. However, when pretreatment with the secosteroids was followed by treatment with H2O2, statistically significant increases in mRNA levels for PDIA3 were observed. The strongest induction (4-fold increase vs controls) was observed in HaCaT keratinocytes pretreated with 21(OH)pD (Figure 6E).
Genes involved in vitamin D3 activation or metabolism (CYP27B1, CYP24A1 and CYP3A4,) were also examined [73, 74]. The preincubation with secosteroids had minimal effects on the mRNA level for CYP3A4, with only 21(OH)pD resulting in a statistically significant decrease (Figure 6F). Treatment of HaCaT keratinocytes with H2O2 (1 mM) alone resulted in a decrease in the expression of CYP3A4 (p<0.05). However, pretreatment with secosteroids other than calcipotriol, with subsequent treatment with H2O2 resulted in a marked increase in CYP3A4 expression (2 – 7 fold). Calcipotriol caused a significant decrease in the mRNA level for CYP3A4.
Preincubation with vitamin D compounds had no effect on the mRNA level for CYP27B1 (Figure 6G). However, expression of CYP27B1 was stimulated with subsequent incubation with H2O2 for 1,25(OH)2D3, 21(OH)pD and calcipotriol. In contrast, cells pretreated with 20(OH)D3 and treated with H2O2 showed a statistically significant decrease in the CYP27B1 mRNA level (Figure 6G). As expected, 1,25(OH)2D3 pretreatment alone caused a strong induction of CYP24A1 expression (Figure 6H). Subsequent treatment with H2O2 markedly attenuated this induction. The low calcemic analogues of vitamin D3, 20(OH)D3, 21(OH)pD and calcipotriol, produced a relatively small to moderate induction of CYP24A1 expression (1.5, 4 and 250 fold respectively), but as for 1,25(OH)2D3 the effect was blunted by H2O2.
4. Discussion
Current pre-clinical and clinical data strongly suggest that vitamin D can function as an anticancer agent. This is exemplified by a strong correlation between higher serum 25(OH)D3 level and decreased incidence of breast [51, 52], colon [53], lung [75], prostate [54] and skin cancer [76]. Moreover, it has been reported that active forms of vitamin D used in combined therapy enhance the effectiveness of anticancer drugs such as cisplatin [77–81], doxorubicin [82, 83], cyclophosphamide [82] or gemcitabine [83]. Interestingly, the mechanism of action of these compounds at least partially relies on generation of reactive oxygen species [70, 84–89]. However, the nature of the action of vitamin D on ROS homeostasis requires clarifications, because published papers frequently describe opposite effects [59, 90–95]. Also, while UVR induces production of both vitamin D and ROS, the effects are wavelengths-dependent with UVB on one hand transforming 7DHC to vitamin D and on the other inducing DNA damage [96–98], with UVA inducing oxidative damage [99, 100].
We observed that simultaneous addition of H2O2 and the secosteroids 1,25(OH)2D3, 20(OH)D3, 21(OH)pD or calcipotriol to HaCaT keratinocytes resulted in more potent inhibition of keratinocytes proliferation by H2O2 than seen with H2O2 alone. Similar enhancement of H2O2 cytotoxicity by 1,25(OH)2D3 in HaCaT keratinocytes has been reported previously, but at 100 nM rather than the 10 nM concentration used in our study [101]. A similar response has also been reported for 1,25(OH)2D3 and H2O2 for the breast cancer cell line, MCF-7 [102], and a colon cancer cell line [103]. Moreover, using similar experimental conditions we show that the vitamin D3 compounds caused a 3 fold reduction in the IC50 value for inhibition of cell growth by cisplatin (Figure 5A), consistent with data described for the murine leukemia cell line, WEHI-3, and the human breast cancer cell lines, MCF-7 and T47D [83]. However, the reduction in IC50 value was not as dramatic in our study (3 fold) compared to these previous studies (55 fold) which might be explained by the relatively strong resistance of HaCaT cells to cisplatin. This resistance is further reflected in the lack of stimulation of the proportion of HaCaT cells in the subG1 fraction by cisplatin (Tables 2 and 3). This is likely due to the mutation in both alleles of p53 in HaCaT cells [104, 105], since it has been shown that cells with p53 mutation or p53 silencing are resistant to cisplatin-induced apoptosis [106, 107]. Cell cycle distribution analysis showed that 24 h pretreatment of HaCaT keratinocytes with 100 nM 1,25(OH)2D3 or calcipotriol resulted in an increase in the proportion of cells in the G2/M phase of the cell cycle following incubation with 120 μM cisplatin for 24 h (Table 3). A similar effect was previously reported for 1,25(OH)2D3 with other platinum drug, carboplatin, for the prostate cancer cell line, LNCaP [108]. In the case of cisplatin we did not observe an increase in the proportion of HaCaT keratinocytes in the subG1 fraction, as observed for H2O2 treatment (Figure 2). The pretreatment of HaCaT keratinocytes with 1,25(OH)2D3 or 20(OH)D3 resulted in a further increase in the proportion of cells in the subG1 phase after subsequent treatment with H2O2 (Figure 2C and D).
Tabele 2.
Effect of vitamin D compounds and cisplatin on the distribution of HaCaT keratinocytes through the cell cycle. HaCaT cells were treated with 100 nM 1,25(OH)2D3, 21(OH)pD or calcipotriol for 24 h, and subsequently exposed to 12 μM cisplatin for an additional 24 h. Cells were harvested, stained with propidium iodide and the distribution of cells in the cell cycle analyzed by Flow Cytometry. Data are presented as mean ± S.D. of three independent experiments carried out in triplicate.
| Sub G1 | G1 | S | G2/M | |
|---|---|---|---|---|
| Control | 3.58 ± 0.80 | 56.78 ± 0.95 | 14.88 ±0.22 | 23.19 ±1.51 |
| Cisplatin | 3.38 ±0.39 | 35.98 ± 1.59*** | 15.76 ± 0.13* | 41.16 ± 1.25*** |
| 1,25(OH)2D3 | 2.00 ±0.40* | 56.94 ± 0.99 | 14.43 ± 0.21* | 25.02 ± 0.83 |
| 1,25(OH)2D3 + cisplatin | 2.83 ± 0.30 | 32.30 ± 0.76***; # | 18.03 ± 0.28***; ### | 44.41 ± 2.06***; ### |
| 21(OH)pD | 4.25 ± 0.80 | 53.30 ± 1.01** | 16.37 ± 0.06** | 25.07 ± 0.28 |
| 21(OH)pD + cisplatin | 4.32 ± 0.05 | 38.85 ± 1.44** | 17.18 ± 0.26**; # | 38.04 ± 1.59** |
| Calcipotriol | 3.51 ± 0.55 | 55.96 ± 0.54 | 14.31 ± 0.08* | 25.08 ± 0.45 |
| Calcipotriol + cisplatin | 2.62 ± 0.28# | 30.57 ± 1.13***; ## | 17.53 ± 0.38***; ## | 47.73 ± 1.80***; ## |
p<0,05;
p<0,01;
p<0,001 vs. control;
- cisplatin versus cisplatin + vitamin D.
Interestingly, our data reveal that incubation of HaCaT keratinocytes with 1,25(OH)2D3 prevented the loss of the transmembrane mitochondrial potential, which is a sensitive indicator of the well-being of the cells, following a 1 h incubation with H2O2 (Figure 4C). Similar results were reported for cortical neurons, where pretreatment with 1,25(OH)2D3 protected them from the loss of mitochondrial transmembrane potential induced by cyanide [109]. It seems, however, that the protective effect is time-dependent, since a 3 h incubation with hydrogen peroxide resulted in a greater decrease in the mitochondrial transmembrane potential after pretreatment with 1,25(OH)2D3, 20(OH)D3 or 21(OH)pD, compared to cells without pretreatment (Figure 4C – E).
The bimodal action of secosteroids was also confirmed by flow cytometry results. 1,25(OH)2D3, 20(OH)D3 or calcipotriol treatment for 24 h decreased the proportion of HaCaT keratinocytes in the subG1 fraction, while after subsequent treatment with H2O2 there was an increase in the number of apoptotic and necrotic cells in comparison to HaCaT keratinocytes treated with H2O2 only (Figure 2). Interestingly, increased viability of cells and protection from apoptosis after treatment with secosteroids alone, was also observed in HaCaT keratinocytes by others [101, 110], as well as in human umbilical vein endothelial cells (HUVECs) [111]. Furthermore, active forms of vitamin D were shown to protect keratinocytes against UVB-induced DNA damage [112] and decrease formation of ROS in keratinocytes and melanocytes subjected to UVB irradiation [21]. Of note, in our study there was a slight decrease in the level of ROS formation in HaCaT keratinocytes after treatment with 1,25(OH)2D3 but the data did not reach statistical significance (Figure 4A and B). A similar inhibition of ROS formation by vitamin D was observed in U937 monocytes [113] and leukemia WEHI-3B cells [114]. Taken together, the results suggest a complex mechanism for the protective actions of of low calcemic vitamin D compounds in the human epidermis. Once the level of ROS exceeds the capacity of cellular defense system, active forms of vitamin D enhance the effect of prooxidants leading to cell death/apoptosis. This could eliminate cells with malignant potential.
While the vitamin D3 compounds tested had little effect by themselves on the expression of genes encoding proteins that remove ROS (SOD1, SOD2 and catalase), 1,25(OH)2D3 20(OH)pD and calcipotriol, but not 20(OH)D3, all enhanced their expression induced by H2O2. This suggests a protective role of these secosteroids against oxidative stress. On the other hand, H2O2 treatment attenuated the stimulation of VDR expression caused by 20(OH)D3, 21(OH)pD or calcipotriol (but not 1,25(OH)2D3) and stimulated the expression of PDIA3 in the presence of these secosteroids. Furthermore, pretreatment of HaCaT keratinocytes with 1,25(OH)2D3, 20(OH)D3 or 21(OH)pD (but not calcipotriol) and subsequent exposure to H2O2, resulted in elevated expression of CYP3A4 mRNA. CYP3A4 is the major cytochrome P450 isoform involved in drug metabolism, including that of some forms of vitamin D [73, 74]. Thus, the combination of active forms of vitamin D and oxidative stress would appear to enhance the ability of the cells to metabolize a range of drugs, at least in the HaCaT keratinocytes.
Our data indicate that oxidative stress and active forms of vitamin D3 (other than 20(OH)D3) together stimulate the expression of CYP27B1, the enzyme required for the formation of 1,25(OH)2D3 [73] and inhibit the expression CYP24A1, the major enzyme involved in the degradation of 1,25(OH)2D3. These effects therefore promote an increase in the level of 1,25(OH)2D3. Oxidative stress and active forms of vitamin D3 together tend to decrease the expression of VDR, but enhance the expression of PDIA3, suggesting that there is a shift away from genomic pathways of vitamin D action towards nongenomic pathways under these conditions. It appears that VDR expression may influence ROS regulation in cells as well. For instance, VDR downregulation in HIV-infected cells contributes to HIV-induced ROS generation in kidney cells and, interestingly, vitamin D administration attenuates this phenomenon [115]. This implies that the increased VDR mRNA level we observed after a 24 h incubation of HaCaT cells with all four of the secosteroids tested (Figure 6D) might be considered as an indirect antioxidative effect of these compounds.
To our knowledge this is the first report describing the interaction of low calcemic analogs (20(OH)D3, 21(OH)pD and calcipotriol), with hydrogen peroxide or cisplatin, and reveals the unique properties of the individual secosteroids tested.. Importantly, 20(OH)D3, 21(OH)pD and calcipotriol have less or no influence on calcium levels compared to 1,25(OH)2D3 [8, 23, 24, 26, 116, 117], indicating biased effects on the VDR as proposed previously [8]. For instance, of the secosteroids tested 20(OH)D3 displayed the strongest stimulation of VDR expression (Figure 6D). These differential effects might be related to the conformational change induced by specific analogues that may modify the interaction of the VDR with coactivators. Also, the nature of ligand receptor interaction can influence whether the action is primarily genomic or non-genomic. Furthermore, vitamin D analogues may bind to alternative receptors to the VDR, such as RORα or RORγ [34]. The lower activity of 21(OH)pD compared to the other secosteroids in inhibiting the growth of HaCaT keratinocytes might be attributed to its short 2C side chain, which influenced its docking to VDR [118]. The relative inability of 20(OH)D3 compared to 1,25(OH)2D3 to stimulate the expression of CYP24A1, as observed in this study, has been well documented before [8, 119]. Another example of the variation between the secosteroids tested in the present study is the inhibition of the H2O2-induced expression of catalase by 20(OH)D3, in contrast to the stimulation seen for 1,25(OH)2D3, 21(OH)pD and calcipotriol. It is therefore apparent that specific analogues may be developed for specific therapeutic applications on particular types of cells or pathways.
We used HaCaT keratinocytes as a model cell in this study because of their highly proliferative phenotype, which is characteristic for a variety of skin pathologies including psoriasis and skin cancers of epidermal origin. The low calcemic vitamin D analogues were used at concentrations corresponding to the optimal serum 25(OH)D3 level (75–125 nM) [67]. While the plasma concentration of 1,25(OH)2D3 is at least 100 times lower than that of 25(OH)D3 [120], the calculated IC50 values for secosteroids tested were actually similar to this concentration, between 0.081 and 1.44 nM for inhibition of cell proliferation. The influence of the secosteroids on the sensitivity of keratinocytes to the ROS generating drug, cisplatin, that we observed highlights the importance of maintaining an adequate serum level of 25(OH)D3 during treatment of hyperproliferative cutaneous diseases. Vitamin D deficiency is extremely common in patients with psoriasis [121] and skin cancers (see [50] for recent review). Our data indicating the enhancement of the cytotoxic activity of cisplatin by the low-calcemic vitamin D analogues, should be of practical application for cancer therapy.
Vitamin D analogs show both prooxidative and antioxidative properties Noncalcemic vitamin D derivatives enhance cytotoxic effects of H2O2 Noncalcemic vitamin D derivatives sensitize human immortalized keratinocytes to cisplatin.
Acknowledgments
The study was supported by a grant of the Polish Ministry of Science and Higher Education, Project No. N405 623238 to Michal A. Zmijewski, and in part and R21 AR066505-01A1 (A.S.).
Abbreviations
- 1α,25(OH)2D3
1α,25-dihydroxyvitamin D3 (calcitriol)
- 20(OH)D3
20S-hydroxyvitamin D3
- 21(OH)pD
21-hydroxypregnacalciferol
- 25(OH)D3
25-hydroxyvitamin D3 (calcifediol)
- 7-DHC
7-dehydrocholesterol (provitamin D3, cholesta-5,7-dien-3β-ol)
- 7-DHP
7-dehydropregnenolone
- CAT
catalase
- CCCP
carbonyl cyanide 3-chlorophenylhydrazone, a protonophore, a chemical inhibitor of oxidative phosphorylation
- MARRS receptor
Membrane-Associated Rapid Response to Steroid binding protein (other names: ERp57, GRp58, Pdia3)
- PDIA3
Protein disulfide-isomerase A3
- ROS
reactive oxygen species
- SOD1
superoxide dismutase 1
- SOD2
superoxide dismutase 2
- UVA/B
ultraviolet radiation A and B
- VDR
vitamin D receptor
- VDRE
vitamin D response elements
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ma Y, Trump DL, Johnson CS. Vitamin D in combination cancer treatment. J Cancer. 2010;1:101–107. doi: 10.7150/jca.1.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wierzbicka J, Piotrowska A, Zmijewski MA. The renaissance of vitamin D. Acta Biochim Pol, Poland. 2014:679–686. [PubMed]
- 3.Holick MF. Vitamin D: a d-lightful solution for health. J Investig Med. 2011;59(6):872–880. doi: 10.231/JIM.0b013e318214ea2d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adams JS, Hewison M. Extrarenal expression of the 25-hydroxyvitamin D-1-hydroxylase. Arch Biochem Biophys. 2012;523(1):95–102. doi: 10.1016/j.abb.2012.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bikle DD. Vitamin D and the skin: Physiology and pathophysiology. Rev Endocr Metab Disord. 2012;13(1):3–19. doi: 10.1007/s11154-011-9194-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Slominski A, Kim TK, Zmijewski MA, Janjetovic Z, Li W, Chen J, Kusniatsova EI, Semak I, Postlethwaite A, Miller DD, Zjawiony JK, Tuckey RC. Novel vitamin D photoproducts and their precursors in the skin. Dermatoendocrinol. 2013;5(1):7–19. doi: 10.4161/derm.23938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Slominski A, Zjawiony J, Wortsman J, Semak I, Stewart J, Pisarchik A, Sweatman T, Marcos J, Dunbar C, CTR A novel pathway for sequential transformation of 7-dehydrocholesterol and expression of the P450scc system in mammalian skin. Eur J Biochem. 2004;271(21):4178–4188. doi: 10.1111/j.1432-1033.2004.04356.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Slominski AT, Kim TK, Li W, Yi AK, Postlethwaite A, Tuckey RC. The role of CYP11A1 in the production of vitamin D metabolites and their role in the regulation of epidermal functions. J Steroid Biochem Mol Biol. 2014;144(Pt A):28–39. doi: 10.1016/j.jsbmb.2013.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zmijewski MA, Li W, Zjawiony JK, Sweatman TW, Chen J, Miller DD, Slominski AT. Synthesis and photo-conversion of androsta- and pregna-5,7-dienes to vitamin D3-like derivatives. Photochem Photobiol Sci. 2008;7(12):1570–1576. doi: 10.1039/b809005j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zmijewski MA, Li W, Zjawiony JK, Sweatman TW, Chen J, Miller DD, Slominski AT. Photo-conversion of two epimers (20R and 20S) of pregna-5,7-diene-3beta, 17alpha, 20-triol and their bioactivity in melanoma cells. Steroids. 2009;74(2):218–228. doi: 10.1016/j.steroids.2008.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zmijewski MA, Li W, Chen J, Kim TK, Zjawiony JK, Sweatman TW, Miller DD, Slominski AT. Synthesis and photochemical transformation of 3beta,21-dihydroxypregna-5,7-dien-20-one to novel secosteroids that show anti-melanoma activity. Steroids. 2011;76(1–2):193–203. doi: 10.1016/j.steroids.2010.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guryev O, Carvalho RA, Usanov S, Gilep A, Estabrook RW. A pathway for the metabolism of vitamin D3: unique hydroxylated metabolites formed during catalysis with cytochrome P450scc (CYP11A1) Proc Natl Acad Sci U S A. 2003;100(25):14754–14759. doi: 10.1073/pnas.2336107100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Slominski A, Semak I, Zjawiony J, Wortsman J, Li W, Szczesniewski A, Tuckey RC. The cytochrome P450scc system opens an alternate pathway of vitamin D3 metabolism. Febs j. 2005;272(16):4080–4090. doi: 10.1111/j.1742-4658.2005.04819.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tuckey RC, Li W, Zjawiony JK, Zmijewski MA, Nguyen MN, Sweatman T, Miller D, Slominski A. Pathways and products for the metabolism of vitamin D3 by cytochrome P450scc. Febs j. 2008;275(10):2585–2596. doi: 10.1111/j.1742-4658.2008.06406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Slominski AT, Zmijewski MA, Semak I, Sweatman T, Janjetovic Z, Li W, Zjawiony JK, Tuckey RC. Sequential metabolism of 7-dehydrocholesterol to steroidal 5,7-dienes in adrenal glands and its biological implication in the skin. PLoS One. 2009;4(2):e4309. doi: 10.1371/journal.pone.0004309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Slominski AT, Kim TK, Chen J, Nguyen MN, Li W, Yates CR, Sweatman T, Janjetovic Z, Tuckey RC. Cytochrome P450scc-dependent metabolism of 7-dehydrocholesterol in placenta and epidermal keratinocytes. Int J Biochem Cell Biol. 2012;44(11):2003–2018. doi: 10.1016/j.biocel.2012.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Slominski AT, Li W, Bhattacharya SK, Smith RA, Johnson PL, Chen J, Nelson KE, Tuckey RC, Miller D, Jiao Y, Gu W, Postlethwaite AE. Vitamin D analogs 17,20S(OH)2pD and 17,20R(OH)2pD are noncalcemic and exhibit antifibrotic activity. J Invest Dermatol, United States. 2011:1167–1169. doi: 10.1038/jid.2010.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tuckey RC, Li W, Shehabi HZ, Janjetovic Z, Nguyen MN, Kim TK, Chen J, Howell DE, Benson HA, Sweatman T, Baldisseri DM, Slominski A. Production of 22-hydroxy metabolites of vitamin d3 by cytochrome p450scc (CYP11A1) and analysis of their biological activities on skin cells. Drug Metab Dispos. 2011;39(9):1577–1588. doi: 10.1124/dmd.111.040071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Slominski AT, Li W, Kim TK, Semak I, Wang J, Zjawiony JK, Tuckey RC. Novel activities of CYP11A1 and their potential physiological significance. J Steroid Biochem Mol Biol. 2015;151:25–37. doi: 10.1016/j.jsbmb.2014.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Slominski AT, Kim TK, Shehabi HZ, Semak I, Tang EK, Nguyen MN, Benson HA, Korik E, Janjetovic Z, Chen J, Yates CR, Postlethwaite A, Li W, Tuckey RC. In vivo evidence for a novel pathway of vitamin D(3) metabolism initiated by P450scc and modified by CYP27B1. Faseb j. 2012;26(9):3901–3915. doi: 10.1096/fj.12-208975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Slominski AT, Janjetovic Z, Kim TK, Wasilewski P, Rosas S, Hanna S, Sayre RM, Dowdy JC, Li W, Tuckey RC. Novel non-calcemic secosteroids that are produced by human epidermal keratinocytes protect against solar radiation. J Steroid Biochem Mol Biol. 2015;148:52–63. doi: 10.1016/j.jsbmb.2015.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Slominski A, Janjetovic Z, Tuckey RC, Nguyen MN, Bhattacharya KG, Wang J, Li W, Jiao Y, Gu W, Brown M, Postlethwaite AE. 20S-hydroxyvitamin D3, noncalcemic product of CYP11A1 action on vitamin D3, exhibits potent antifibrogenic activity in vivo. J Clin Endocrinol Metab. 2013;98(2):E298–303. doi: 10.1210/jc.2012-3074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Slominski AT, Janjetovic Z, Fuller BE, Zmijewski MA, Tuckey RC, Nguyen MN, Sweatman T, Li W, Zjawiony J, Miller D, Chen TC, Lozanski G, Holick MF. Products of vitamin D3 or 7-dehydrocholesterol metabolism by cytochrome P450scc show anti-leukemia effects, having low or absent calcemic activity. PLoS One. 2010;5(3):e9907. doi: 10.1371/journal.pone.0009907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang J, Slominski A, Tuckey RC, Janjetovic Z, Kulkarni A, Chen J, Postlethwaite AE, Miller D, Li W. 20-hydroxyvitamin D(3) inhibits proliferation of cancer cells with high efficacy while being non-toxic. Anticancer Res. 2012;32(3):739–746. [PMC free article] [PubMed] [Google Scholar]
- 25.Slominski AT, Janjetovic Z, Kim TK, Wright AC, Grese LN, Riney SJ, Nguyen MN, Tuckey RC. Novel vitamin D hydroxyderivatives inhibit melanoma growth and show differential effects on normal melanocytes. Anticancer Res. 2012;32(9):3733–3742. [PMC free article] [PubMed] [Google Scholar]
- 26.Wasiewicz T, Szyszka P, Cichorek M, Janjetovic Z, Tuckey RC, Slominski AT, Zmijewski MA. Antitumor effects of vitamin d analogs on hamster and mouse melanoma cell lines in relation to melanin pigmentation. Int J Mol Sci. 2015;16(4):6645–6667. doi: 10.3390/ijms16046645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wierzbicka JM, Binek A, Ahrends T, Nowacka JD, Szydłowska A, Turczyk Ł, Wąsiewicz T, Wierzbicki PM, Sądej R, Tuckey RC, Slominski AT, Chybicki J, Adrych K, Kmieć Z, Żmijewski MA. Differential antitumor effects of vitamin D analogues on colorectal carcinoma in culture. Int J Oncol. 2015;47(3):1084–1096. doi: 10.3892/ijo.2015.3088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haussler MR, Jurutka PW, Mizwicki M, Norman AW. Vitamin D receptor (VDR)-mediated actions of 1alpha,25(OH)(2)vitamin D(3): genomic and non-genomic mechanisms. Best Pract Res Clin Endocrinol Metab. 2011;25(4):543–559. doi: 10.1016/j.beem.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 29.Haussler MR, Whitfield GK, Kaneko I, Haussler CA, Hsieh D, Hsieh JC, Jurutka PW. Molecular mechanisms of vitamin D action. Calcif Tissue Int. 2013;92(2):77–98. doi: 10.1007/s00223-012-9619-0. [DOI] [PubMed] [Google Scholar]
- 30.Saccone D, Asani F, Bornman L. Regulation of the vitamin D receptor gene by environment, genetics and epigenetics. Gene. 2015;561(2):171–180. doi: 10.1016/j.gene.2015.02.024. [DOI] [PubMed] [Google Scholar]
- 31.Pike JW, Meyer MB. Endocrinol Metab Clin North Am. Elsevier Inc; United States: 2010. The vitamin D receptor: new paradigms for the regulation of gene expression by 1,25-dihydroxyvitamin D(3) pp. 255–269. table of contents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nemere I, Garbi N, Hammerling G, Hintze KJ. Role of the 1,25D3-MARRS receptor in the 1,25(OH)2D3-stimulated uptake of calcium and phosphate in intestinal cells. Steroids. 2012;77(10):897–902. doi: 10.1016/j.steroids.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 33.Nemere I, Farach-Carson MC, Rohe B, Sterling TM, Norman AW, Boyan BD, Safford SE. Ribozyme knockdown functionally links a 1,25(OH)2D3 membrane binding protein (1,25D3-MARRS) and phosphate uptake in intestinal cells. Proc Natl Acad Sci U S A. 2004;101(19):7392–7397. doi: 10.1073/pnas.0402207101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Slominski AT, Kim TK, Takeda Y, Janjetovic Z, Brozyna AA, Skobowiat C, Wang J, Postlethwaite A, Li W, Tuckey RC, Jetten AM. RORalpha and ROR gamma are expressed in human skin and serve as receptors for endogenously produced noncalcemic 20-hydroxy- and 20,23-dihydroxyvitamin D. Faseb j. 2014;28(7):2775–2789. doi: 10.1096/fj.13-242040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.DeLuca HF. Overview of general physiologic features and functions of vitamin D. Am J Clin Nutr. 2004;80(6 Suppl):1689s–1696s. doi: 10.1093/ajcn/80.6.1689S. [DOI] [PubMed] [Google Scholar]
- 36.Bikle DD. Vitamin D: an ancient hormone. Exp Dermatol. 2011;20(1):7–13. doi: 10.1111/j.1600-0625.2010.01202.x. [DOI] [PubMed] [Google Scholar]
- 37.Mason RS, Sequeira VB, Gordon-Thomson C. Vitamin D: the light side of sunshine. Eur J Clin Nutr. 2011;65(9):986–993. doi: 10.1038/ejcn.2011.105. [DOI] [PubMed] [Google Scholar]
- 38.Mason RS. Vitamin D: a hormone for all seasons. Climacteric. 2011;14(2):197–203. doi: 10.3109/13697137.2010.514366. [DOI] [PubMed] [Google Scholar]
- 39.Pike JW, Zella LA, Meyer MB, Fretz JA, Kim S. Molecular actions of 1,25-dihydroxyvitamin D3 on genes involved in calcium homeostasis. J Bone Miner Res. 2007;22(Suppl 2):V16–19. doi: 10.1359/jbmr.07s207. [DOI] [PubMed] [Google Scholar]
- 40.Samuel S, Sitrin MD. Vitamin D’s role in cell proliferation and differentiation. Nutr Rev. 2008;66(10 Suppl 2):S116–124. doi: 10.1111/j.1753-4887.2008.00094.x. [DOI] [PubMed] [Google Scholar]
- 41.Bikle DD. Vitamin D regulated keratinocyte differentiation. J Cell Biochem. 2004;92(3):436–444. doi: 10.1002/jcb.20095. [DOI] [PubMed] [Google Scholar]
- 42.Bikle DD, Oda Y, Xie Z. Calcium and 1,25(OH)2D: interacting drivers of epidermal differentiation. J Steroid Biochem Mol Biol. 2004;89–90(1–5):355–360. doi: 10.1016/j.jsbmb.2004.03.020. [DOI] [PubMed] [Google Scholar]
- 43.Diaz L, Diaz-Munoz M, Garcia-Gaytan AC, Mendez I. Mechanistic Effects of Calcitriol in Cancer Biology. Nutrients. 2015;7(6):5020–5050. doi: 10.3390/nu7065020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kubis AM, Piwowar A. The new insight on the regulatory role of the vitamin D3 in metabolic pathways characteristic for cancerogenesis and neurodegenerative diseases. Ageing Res Rev. 2015 doi: 10.1016/j.arr.2015.07.008. [DOI] [PubMed] [Google Scholar]
- 45.Sergeev IN. Vitamin D-mediated apoptosis in cancer and obesity. Horm Mol Biol Clin Investig. 2014;20(2):43–49. doi: 10.1515/hmbci-2014-0035. [DOI] [PubMed] [Google Scholar]
- 46.Ness RA, Miller DD, Li W. The role of vitamin D in cancer prevention. Chin J Nat Med. 2015;13(7):481–497. doi: 10.1016/S1875-5364(15)30043-1. [DOI] [PubMed] [Google Scholar]
- 47.Krishnan AV, Swami S, Feldman D. Equivalent anticancer activities of dietary vitamin D and calcitriol in an animal model of breast cancer: importance of mammary CYP27B1 for treatment and prevention. J Steroid Biochem Mol Biol. 2013;136:289–295. doi: 10.1016/j.jsbmb.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Morris HA. Vitamin D activities for health outcomes. Ann Lab Med. 2014;34(3):181–186. doi: 10.3343/alm.2014.34.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mitchell D. The relationship between vitamin D and cancer. Clin J Oncol Nurs. 2011;15(5):557–560. doi: 10.1188/11.CJON.557-560. [DOI] [PubMed] [Google Scholar]
- 50.Yin L, Ordonez-Mena JM, Chen T, Schottker B, Arndt V, Brenner H. Circulating 25-hydroxyvitamin D serum concentration and total cancer incidence and mortality: a systematic review and meta-analysis. Prev Med. 2013;57(6):753–764. doi: 10.1016/j.ypmed.2013.08.026. [DOI] [PubMed] [Google Scholar]
- 51.Welsh J, Wietzke JA, Zinser GM, Byrne B, Smith K, Narvaez CJ. Vitamin D-3 receptor as a target for breast cancer prevention. J Nutr. 2003;133(7 Suppl):2425s–2433s. doi: 10.1093/jn/133.7.2425S. [DOI] [PubMed] [Google Scholar]
- 52.Mehta RG, Hussain EA, Mehta RR, Das Gupta TK. Chemoprevention of mammary carcinogenesis by 1alpha-hydroxyvitamin D5, a synthetic analog of Vitamin D. Mutat Res. 2003;523–524:253–264. doi: 10.1016/s0027-5107(02)00341-x. [DOI] [PubMed] [Google Scholar]
- 53.Lamprecht SA, Lipkin M. Chemoprevention of colon cancer by calcium, vitamin D and folate: molecular mechanisms. Nat Rev Cancer. 2003;3(8):601–614. doi: 10.1038/nrc1144. [DOI] [PubMed] [Google Scholar]
- 54.Krishnan AV, Peehl DM, Feldman D. The role of vitamin D in prostate cancer. Recent Results Cancer Res. 2003;164:205–221. doi: 10.1007/978-3-642-55580-0_15. [DOI] [PubMed] [Google Scholar]
- 55.Bolland MJ, Grey A, Gamble GD, Reid IR. Calcium and vitamin D supplements and health outcomes: a reanalysis of the Women’s Health Initiative (WHI) limited-access data set. Am J Clin Nutr. 2011;94(4):1144–1149. doi: 10.3945/ajcn.111.015032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Grant WB. Relation between prediagnostic serum 25-hydroxyvitamin D level and incidence of breast, colorectal, and other cancers. J Photochem Photobiol B. 2010;101(2):130–136. doi: 10.1016/j.jphotobiol.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 57.Grant WB. 25-hydroxyvitamin D and breast cancer, colorectal cancer, and colorectal adenomas: case-control versus nested case-control studies. Anticancer Res. 2015;35(2):1153–1160. [PubMed] [Google Scholar]
- 58.Gordon-Thomson C, Gupta R, Tongkao-on W, Ryan A, Halliday GM, Mason RS. 1α,25 dihydroxyvitamin D3 enhances cellular defences against UV-induced oxidative and other forms of DNA damage in skin. Photochem Photobiol Sci. 2012;11(12):1837–1847. doi: 10.1039/c2pp25202c. [DOI] [PubMed] [Google Scholar]
- 59.Fedirko V, Bostick RM, Long Q, Flanders WD, McCullough ML, Sidelnikov E, Daniel CR, Rutherford RE, Shaukat A. Effects of supplemental vitamin D and calcium on oxidative DNA damage marker in normal colorectal mucosa: a randomized clinical trial. Cancer Epidemiol Biomarkers Prev. 2010;19(1):280–291. doi: 10.1158/1055-9965.EPI-09-0448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jiang YJ, Teichert AE, Fong F, Oda Y, Bikle DD. 1alpha,25(OH)2-dihydroxyvitamin D3/VDR protects the skin from UVB-induced tumor formation by interacting with the beta-catenin pathway. J Steroid Biochem Mol Biol. 2013;136:229–232. doi: 10.1016/j.jsbmb.2012.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dixon KM, Deo SS, Wong G, Slater M, Norman AW, Bishop JE, Posner GH, Ishizuka S, Halliday GM, Reeve VE, Mason RS. Skin cancer prevention: a possible role of 1,25dihydroxyvitamin D3 and its analogs. J Steroid Biochem Mol Biol. 2005;97(1–2):137–143. doi: 10.1016/j.jsbmb.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 62.De Haes P, Garmyn M, Degreef H, Vantieghem K, Bouillon R, Segaert S. 1,25-Dihydroxyvitamin D3 inhibits ultraviolet B-induced apoptosis, Jun kinase activation, and interleukin-6 production in primary human keratinocytes. J Cell Biochem. 2003;89(4):663–673. doi: 10.1002/jcb.10540. [DOI] [PubMed] [Google Scholar]
- 63.Wong G, Gupta R, Dixon KM, Deo SS, Choong SM, Halliday GM, Bishop JE, Ishizuka S, Norman AW, Posner GH, Mason RS. 1,25-Dihydroxyvitamin D and three low-calcemic analogs decrease UV-induced DNA damage via the rapid response pathway. J Steroid Biochem Mol Biol. 2004;89–90(1–5):567–570. doi: 10.1016/j.jsbmb.2004.03.072. [DOI] [PubMed] [Google Scholar]
- 64.Tongkao-On W, Carter S, Reeve VE, Dixon KM, Gordon-Thomson C, Halliday GM, Tuckey RC, Mason RS. CYP11A1 in skin: an alternative route to photoprotection by vitamin D compounds. J Steroid Biochem Mol Biol. 2015;148:72–78. doi: 10.1016/j.jsbmb.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 65.Slominski AT, Manna PR, Tuckey RC. On the role of skin in the regulation of local and systemic steroidogenic activities. Steroids. 2015 doi: 10.1016/j.steroids.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zbytek B, Janjetovic Z, Tuckey RC, Zmijewski MA, Sweatman TW, Jones E, Nguyen MN, Slominski AT. 20-hydroxyvitamin D3, a product of vitamin D3 hydroxylation by cytochrome P450scc, stimulates keratinocyte differentiation. Journal of Investigative Dermatology. 2008;128(9):2271–2280. doi: 10.1038/jid.2008.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Płudowski P, Karczmarewicz E, Bayer M, Carter G, Chlebna-Sokół D, Czech-Kowalska J, Dębski R, Decsi T, Dobrzańska A, Franek E, Głuszko P, Grant WB, Holick MF, Yankovskaya L, Konstantynowicz J, Książyk JB, Księżopolska-Orłowska K, Lewiński A, Litwin M, Lohner S, Lorenc RS, Lukaszkiewicz J, Marcinowska-Suchowierska E, Milewicz A, Misiorowski W, Nowicki M, Povoroznyuk V, Rozentryt P, Rudenka E, Shoenfeld Y, Socha P, Solnica B, Szalecki M, Tałałaj M, Varbiro S, Żmijewski MA. Practical guidelines for the supplementation of vitamin D and the treatment of deficits in Central Europe - recommended vitamin D intakes in the general population and groups at risk of vitamin D deficiency. Endokrynol Pol. 2013;64(4):319–327. doi: 10.5603/ep.2013.0012. [DOI] [PubMed] [Google Scholar]
- 68.Rockett KA, Brookes R, Udalova I, Vidal V, Hill AV, Kwiatkowski D. 1,25-Dihydroxyvitamin D3 induces nitric oxide synthase and suppresses growth of Mycobacterium tuberculosis in a human macrophage-like cell line. Infect Immun. 1998;66(11):5314–5321. doi: 10.1128/iai.66.11.5314-5321.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fischer TW, Zmijewski MA, Wortsman J, Slominski A. Melatonin maintains mitochondrial membrane potential and attenuates activation of initiator (casp-9) and effector caspases (casp-3/casp-7) and PARP in UVR-exposed HaCaT keratinocytes. Journal of Pineal Research. 2008;44(4):397–407. doi: 10.1111/j.1600-079X.2007.00542.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Marullo R, Werner E, Degtyareva N, Moore B, Altavilla G, Ramalingam SS, Doetsch PW. Cisplatin induces a mitochondrial-ROS response that contributes to cytotoxicity depending on mitochondrial redox status and bioenergetic functions. PLoS One. 2013;8(11):e81162. doi: 10.1371/journal.pone.0081162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mehta KS, Mahajan VK, Chauhan PS, Sharma AL, Sharma V, Abhinav C, Khatri G, Prabha N, Sharma S, Negi M. Metastatic Basal cell carcinoma: a biological continuum of Basal cell carcinoma? Case Rep Dermatol Med. 2012;2012:157187. doi: 10.1155/2012/157187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Luanpitpong S, Nimmannit U, Chanvorachote P, Leonard SS, Pongrakhananon V, Wang L, Rojanasakul Y. Hydroxyl radical mediates cisplatin-induced apoptosis in human hair follicle dermal papilla cells and keratinocytes through Bcl-2-dependent mechanism. Apoptosis. 2011;16(8):769–782. doi: 10.1007/s10495-011-0609-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Schuster I. Cytochromes P450 are essential players in the vitamin D signaling system. Biochim Biophys Acta. 2011;1814(1):186–199. doi: 10.1016/j.bbapap.2010.06.022. [DOI] [PubMed] [Google Scholar]
- 74.Xu Y, Hashizume T, Shuhart MC, Davis CL, Nelson WL, Sakaki T, Kalhorn TF, Watkins PB, Schuetz EG, Thummel KE. Intestinal and hepatic CYP3A4 catalyze hydroxylation of 1alpha,25-dihydroxyvitamin D(3): implications for drug-induced osteomalacia. Mol Pharmacol. 2006;69(1):56–65. doi: 10.1124/mol.105.017392. [DOI] [PubMed] [Google Scholar]
- 75.Nakagawa K, Kawaura A, Kato S, Takeda E, Okano T. 1 alpha,25-Dihydroxyvitamin D(3) is a preventive factor in the metastasis of lung cancer. Carcinogenesis. 2005;26(2):429–440. doi: 10.1093/carcin/bgh332. [DOI] [PubMed] [Google Scholar]
- 76.Ingraham BA, Bragdon B, Nohe A. Molecular basis of the potential of vitamin D to prevent cancer. Curr Med Res Opin. 2008;24(1):139–149. doi: 10.1185/030079908x253519. [DOI] [PubMed] [Google Scholar]
- 77.Light BW, Yu WD, McElwain MC, Russell DM, Trump DL, Johnson CS. Potentiation of cisplatin antitumor activity using a vitamin D analogue in a murine squamous cell carcinoma model system. Cancer Res. 1997;57(17):3759–3764. [PubMed] [Google Scholar]
- 78.Hershberger PA, McGuire TF, Yu WD, Zuhowski EG, Schellens JH, Egorin MJ, Trump DL, Johnson CS. Cisplatin potentiates 1,25-dihydroxyvitamin D3-induced apoptosis in association with increased mitogen-activated protein kinase kinase kinase 1 (MEKK-1) expression. Mol Cancer Ther. 2002;1(10):821–829. [PubMed] [Google Scholar]
- 79.Wietrzyk J, Pelczynska M, Madej J, Dzimira S, Kusnierczyk H, Kutner A, Szelejewski W, Opolski A. Toxicity and antineoplastic effect of (24R)-1,24-dihydroxyvitamin D3 (PRI-2191) Steroids. 2004;69(10):629–635. doi: 10.1016/j.steroids.2004.05.015. [DOI] [PubMed] [Google Scholar]
- 80.Ma Y, Yu WD, Trump DL, Johnson CS. 1,25D3 enhances antitumor activity of gemcitabine and cisplatin in human bladder cancer models. Cancer. 2010;116(13):3294–3303. doi: 10.1002/cncr.25059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rassnick KM, Muindi JR, Johnson CS, Balkman CE, Ramnath N, Yu WD, Engler KL, Page RL, Trump DL. In vitro and in vivo evaluation of combined calcitriol and cisplatin in dogs with spontaneously occurring tumors. Cancer Chemother Pharmacol. 2008;62(5):881–891. doi: 10.1007/s00280-008-0678-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wietrzyk J, Nevozhay D, Filip B, Milczarek M, Kutner A. The antitumor effect of lowered doses of cytostatics combined with new analogs of vitamin D in mice. Anticancer Res. 2007;27(5a):3387–3398. [PubMed] [Google Scholar]
- 83.Pelczynska M, Switalska M, Maciejewska M, Jaroszewicz I, Kutner A, Opolski A. Antiproliferative activity of vitamin D compounds in combination with cytostatics. Anticancer Res. 2006;26(4a):2701–2705. [PubMed] [Google Scholar]
- 84.Mondal J, Bishayee K, Panigrahi AK, Khuda-Bukhsh AR. Low doses of ethanolic extract of Boldo (Peumus boldus) can ameliorate toxicity generated by cisplatin in normal liver cells of mice in vivo and in WRL-68 cells in vitro, but not in cancer cells in vivo or in vitro. J Integr Med. 2014;12(5):425–438. doi: 10.1016/S2095-4964(14)60045-5. [DOI] [PubMed] [Google Scholar]
- 85.Kikkawa YS, Nakagawa T, Taniguchi M, Ito J. Hydrogen protects auditory hair cells from cisplatin-induced free radicals. Neurosci Lett. 2014;579:125–129. doi: 10.1016/j.neulet.2014.07.025. [DOI] [PubMed] [Google Scholar]
- 86.Szwed M, Jozwiak Z. Genotoxic effect of doxorubicin-transferrin conjugate on human leukemia cells. Mutat Res Genet Toxicol Environ Mutagen. 2014;771:53–63. doi: 10.1016/j.mrgentox.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 87.Szwed M, Kania KD, Jozwiak Z. Molecular damage caused by generation of reactive oxygen species in the redox cycle of doxorubicin-transferrin conjugate in human leukemia cell lines. Leuk Lymphoma. 2014:1–9. doi: 10.3109/10428194.2014.955022. [DOI] [PubMed] [Google Scholar]
- 88.Roy SS, Chakraborty P, Bhattacharya S. Intervention in cyclophosphamide induced oxidative stress and DNA damage by a flavonyl-thiazolidinedione based organoselenocyanate and evaluation of its efficacy during adjuvant therapy in tumor bearing mice. Eur J Med Chem. 2014;73:195–209. doi: 10.1016/j.ejmech.2013.12.015. [DOI] [PubMed] [Google Scholar]
- 89.Arora S, Bhardwaj A, Singh S, Srivastava SK, McClellan S, Nirodi CS, Piazza GA, Grizzle WE, Owen LB, Singh AP. An undesired effect of chemotherapy: gemcitabine promotes pancreatic cancer cell invasiveness through reactive oxygen species-dependent, nuclear factor kappaB- and hypoxia-inducible factor 1alpha-mediated up-regulation of CXCR4. J Biol Chem. 2013;288(29):21197–21207. doi: 10.1074/jbc.M113.484576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Koren R, Hadari-Naor I, Zuck E, Rotem C, Liberman UA, Ravid A. Vitamin D is a prooxidant in breast cancer cells. Cancer Res. 2001;61(4):1439–1444. [PubMed] [Google Scholar]
- 91.Ravid A, Rocker D, Machlenkin A, Rotem C, Hochman A, Kessler-Icekson G, Liberman UA, Koren R. 1,25-Dihydroxyvitamin D3 enhances the susceptibility of breast cancer cells to doxorubicin-induced oxidative damage. Cancer Res. 1999;59(4):862–867. [PubMed] [Google Scholar]
- 92.Somjen D, Katzburg S, Knoll E, Sharon O, Posner GH, Stern N. Vitamin D analogs induce lipoxygenase mRNA expression and activity as well as reactive oxygen species (ROS) production in human bone cells. J Steroid Biochem Mol Biol. 2010;121(1–2):265–267. doi: 10.1016/j.jsbmb.2010.03.047. [DOI] [PubMed] [Google Scholar]
- 93.Bao BY, Ting HJ, Hsu JW, Lee YF. Protective role of 1 alpha, 25-dihydroxyvitamin D3 against oxidative stress in nonmalignant human prostate epithelial cells. Int J Cancer. 2008;122(12):2699–2706. doi: 10.1002/ijc.23460. [DOI] [PubMed] [Google Scholar]
- 94.Hamden K, Carreau S, Jamoussi K, Miladi S, Lajmi S, Aloulou D, Ayadi F, Elfeki A. 1Alpha,25 dihydroxyvitamin D3: therapeutic and preventive effects against oxidative stress, hepatic, pancreatic and renal injury in alloxan-induced diabetes in rats. J Nutr Sci Vitaminol (Tokyo) 2009;55(3):215–222. doi: 10.3177/jnsv.55.215. [DOI] [PubMed] [Google Scholar]
- 95.Eftekhari MH, Akbarzadeh M, Dabbaghmanesh MH, Hassanzadeh J. The effect of calcitriol on lipid profile and oxidative stress in hyperlipidemic patients with type 2 diabetes mellitus. ARYA Atheroscler. 2014;10(2):82–88. [PMC free article] [PubMed] [Google Scholar]
- 96.Bikle DD. The vitamin D receptor: a tumor suppressor in skin. Discov Med. 2011;11(56):7–17. [PMC free article] [PubMed] [Google Scholar]
- 97.Reichrath J, Rass K. Ultraviolet damage, DNA repair and vitamin D in nonmelanoma skin cancer and in malignant melanoma: an update. Adv Exp Med Biol. 2014;810:208–233. doi: 10.1007/978-1-4939-0437-2_12. [DOI] [PubMed] [Google Scholar]
- 98.Grant WB. Update on evidence that support a role of solar ultraviolet-B irradiance in reducing cancer risk. Anticancer Agents Med Chem. 2013;13(1):140–146. [PubMed] [Google Scholar]
- 99.Aroun A, Zhong JL, Tyrrell RM, Pourzand C. Iron, oxidative stress and the example of solar ultraviolet A radiation. Photochem Photobiol Sci. 2012;11(1):118–134. doi: 10.1039/c1pp05204g. [DOI] [PubMed] [Google Scholar]
- 100.Burke KE. Photoaging: the role of oxidative stress. G Ital Dermatol Venereol. 2010;145(4):445–459. [PubMed] [Google Scholar]
- 101.Diker-Cohen T, Koren R, Ravid A. Programmed cell death of stressed keratinocytes and its inhibition by vitamin D: the role of death and survival signaling pathways. Apoptosis. 2006;11(4):519–534. doi: 10.1007/s10495-006-5115-1. [DOI] [PubMed] [Google Scholar]
- 102.Weitsman GE, Koren R, Zuck E, Rotem C, Liberman UA, Ravid A. Vitamin D sensitizes breast cancer cells to the action of H2O2: mitochondria as a convergence point in the death pathway. Free Radic Biol Med. 2005;39(2):266–278. doi: 10.1016/j.freeradbiomed.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 103.Koren R, Wacksberg S, Weitsman GE, Ravid A. Calcitriol sensitizes colon cancer cells to H2O2-induced cytotoxicity while inhibiting caspase activation. J Steroid Biochem Mol Biol. 2006;101(2–3):151–160. doi: 10.1016/j.jsbmb.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 104.Lehman TA, Modali R, Boukamp P, Stanek J, Bennett WP, Welsh JA, Metcalf RA, Stampfer MR, Fusenig N, Rogan EM, et al. p53 mutations in human immortalized epithelial cell lines. Carcinogenesis. 1993;14(5):833–839. doi: 10.1093/carcin/14.5.833. [DOI] [PubMed] [Google Scholar]
- 105.Herbert KJ, Cook AL, Snow ET. SIRT1 inhibition restores apoptotic sensitivity in p53-mutated human keratinocytes. Toxicol Appl Pharmacol. 2014;277(3):288–297. doi: 10.1016/j.taap.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 106.Gumulec J, Balvan J, Sztalmachova M, Raudenska M, Dvorakova V, Knopfova L, Polanska H, Hudcova K, Ruttkay-Nedecky B, Babula P, Adam V, Kizek R, Stiborova M, Masarik M. Cisplatin-resistant prostate cancer model: Differences in antioxidant system, apoptosis and cell cycle. Int J Oncol. 2014;44(3):923–933. doi: 10.3892/ijo.2013.2223. [DOI] [PubMed] [Google Scholar]
- 107.di Pietro A, Koster R, Boersma-van Eck W, Dam WA, Mulder NH, Gietema JA, de Vries EG, de Jong S. Pro- and anti-apoptotic effects of p53 in cisplatin-treated human testicular cancer are cell context-dependent. Cell Cycle. 2012;11(24):4552–4562. doi: 10.4161/cc.22803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Moffatt KA, Johannes WU, Miller GJ. 1Alpha,25dihydroxyvitamin D3 and platinum drugs act synergistically to inhibit the growth of prostate cancer cell lines. Clin Cancer Res. 1999;5(3):695–703. [PubMed] [Google Scholar]
- 109.Li L, Prabhakaran K, Zhang X, Zhang L, Liu H, Borowitz JL, Isom GE. 1Alpha,25-dihydroxyvitamin D3 attenuates cyanide-induced neurotoxicity by inhibiting uncoupling protein-2 upregulation. J Neurosci Res. 2008;86(6):1397–1408. doi: 10.1002/jnr.21596. [DOI] [PubMed] [Google Scholar]
- 110.Diker-Cohen T, Koren R, Liberman UA, Ravid A. Vitamin D protects keratinocytes from apoptosis induced by osmotic shock, oxidative stress, and tumor necrosis factor. Ann N Y Acad Sci. 2003;1010:350–353. doi: 10.1196/annals.1299.064. [DOI] [PubMed] [Google Scholar]
- 111.Uberti F, Lattuada D, Morsanuto V, Nava U, Bolis G, Vacca G, Squarzanti DF, Cisari C, Molinari C. Vitamin D protects human endothelial cells from oxidative stress through the autophagic and survival pathways. J Clin Endocrinol Metab. 2014;99(4):1367–1374. doi: 10.1210/jc.2013-2103. [DOI] [PubMed] [Google Scholar]
- 112.De Haes P, Garmyn M, Verstuyf A, De Clercq P, Vandewalle M, Degreef H, Vantieghem K, Bouillon R, Segaert S. 1,25-Dihydroxyvitamin D3 and analogues protect primary human keratinocytes against UVB-induced DNA damage. J Photochem Photobiol B. 2005;78(2):141–148. doi: 10.1016/j.jphotobiol.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 113.Jain SK, Micinski D. Vitamin D upregulates glutamate cysteine ligase and glutathione reductase, and GSH formation, and decreases ROS and MCP-1 and IL-8 secretion in high-glucose exposed U937 monocytes. Biochem Biophys Res Commun. 2013;437(1):7–11. doi: 10.1016/j.bbrc.2013.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Shabtay A, Sharabani H, Barvish Z, Kafka M, Amichay D, Levy J, Sharoni Y, Uskokovic MR, Studzinski GP, Danilenko M. Synergistic antileukemic activity of carnosic acid-rich rosemary extract and the 19-nor Gemini vitamin D analogue in a mouse model of systemic acute myeloid leukemia. Oncology. 2008;75(3–4):203–214. doi: 10.1159/000163849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Salhan D, Husain M, Subrati A, Goyal R, Singh T, Rai P, Malhotra A, Singhal PC. HIV-induced kidney cell injury: role of ROS-induced downregulated vitamin D receptor. Am J Physiol Renal Physiol. 2012;303(4):F503–514. doi: 10.1152/ajprenal.00170.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Chen J, Wang J, Kim TK, Tieu EW, Tang EK, Lin Z, Kovacic D, Miller DD, Postlethwaite A, Tuckey RC, Slominski AT, Li W. Novel vitamin D analogs as potential therapeutics: metabolism, toxicity profiling, and antiproliferative activity. Anticancer Res. 2014;34(5):2153–2163. [PMC free article] [PubMed] [Google Scholar]
- 117.Slominski AT, Kim TK, Janjetovic Z, Tuckey RC, Bieniek R, Yue J, Li W, Chen J, Nguyen MN, Tang EK, Miller D, Chen TC, Holick M. 20-Hydroxyvitamin D2 is a noncalcemic analog of vitamin D with potent antiproliferative and prodifferentiation activities in normal and malignant cells. Am J Physiol Cell Physiol. 2011;300(3):C526–541. doi: 10.1152/ajpcell.00203.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kim TK, Wang J, Janjetovic Z, Chen J, Tuckey RC, Nguyen MN, Tang EK, Miller D, Li W, Slominski AT. Correlation between secosteroid-induced vitamin D receptor activity in melanoma cells and computer-modeled receptor binding strength. Mol Cell Endocrinol. 2012;361(1–2):143–152. doi: 10.1016/j.mce.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zbytek B, Janjetovic Z, Tuckey RC, Zmijewski MA, Sweatman TW, Jones E, Nguyen MN, Slominski AT. 20-Hydroxyvitamin D3, a product of vitamin D3 hydroxylation by cytochrome P450scc, stimulates keratinocyte differentiation. J Invest Dermatol. 2008;128(9):2271–2280. doi: 10.1038/jid.2008.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Souberbielle JC, Cavalier E, Delanaye P, Massart C, Brailly-Tabard S, Cormier C, Borderie D, Benachi A, Chanson P. Serum calcitriol concentrations measured with a new direct automated assay in a large population of adult healthy subjects and in various clinical situations. Clin Chim Acta. 2015;451(Pt B):149–153. doi: 10.1016/j.cca.2015.09.021. [DOI] [PubMed] [Google Scholar]
- 121.Gisondi P, Rossini M, Di Cesare A, Idolazzi L, Farina S, Beltrami G, Peris K, Girolomoni G. Vitamin D status in patients with chronic plaque psoriasis. Br J Dermatol. 2012;166(3):505–510. doi: 10.1111/j.1365-2133.2011.10699.x. [DOI] [PubMed] [Google Scholar]