Abstract
Objective
Hepatitis B virus (HBV) infection continues to be a public health threat in the United States. As many as 2.2 million people are infected, approximately 70% of whom are foreign-born, and fewer than one-third are aware of their infection. We launched an HBV testing and linkage-to-care initiative among foreign-born people.
Methods
As part of the Hepatitis Testing and Linkage to Care (HepTLC) initiative, which promoted viral hepatitis B and hepatitis C screening, posttest counseling, and linkage to care at 34 U.S. sites, nine U.S. programs in seven states conducted HBV screening from October 2012 to September 2014. The nine programs partnered with health-care centers and community-based organizations to recruit foreign-born people recommended for HBV testing. We assessed patient characteristics, region of origin, risk factors, hepatitis B surface antigen (HBsAg) status, and referral to medical care.
Results
Of 23,144 participants tested for HBV, 1,317 (5.7%) were HBsAg positive. Of these, the median age was 47 years, 1,205 (91%) had at least one risk factor for HBV infection, 1,117 (85%) received posttest counseling, 1,098 (83%) were referred to care, and 606 (46%) attended a first medical appointment. The proportion of HBsAg-positive participants by region of origin included Africa (10%, 206/2,129), Western Pacific (6%, 616/9,673), Eastern Mediterranean (5%, 174/3,337), Southeast Asia (5%, 191/3,891), South America (2%, 6/252), Eastern Europe (2%, 6/262), and North America (1%, 17/1,936).
Conclusion
Community-based HBV testing initiatives can identify substantial numbers of people with chronic HBV infection, inform them of their infection status, and provide posttest counseling and linkage to care. However, strategies are needed to improve linkage to HBV-directed medical care for foreign-born individuals living with chronic HBV infection.
As many as 2.2 million people are living with chronic hepatitis B virus (HBV) infection in the United States, and about 70% are foreign-born.1,2 The majority of foreign-born people living with chronic HBV infection in the United States are from Asia and Africa, or other regions where HBV infection prevalence is ≥2%.1 In the absence of medical intervention, about 25% of people living with chronic HBV infection will die prematurely from cirrhosis or liver cancer.3 Acute HBV infection is usually asymptomatic, and the risk of progression to chronic HBV infection is 90% among those infected before 1 year of age, 20%–50% among those infected at 1–5 years of age, and <5% among those infected as adults.2,4
Although HBV infection is a vaccine-preventable disease, many foreign-born people from countries with elevated HBV prevalence were not vaccinated, because hepatitis B vaccine was not introduced into routine childhood immunization programs until relatively recently.5 As of 2013, 93 countries have introduced the hepatitis B birth dose vaccine.6 As a result, many foreign-born people acquired HBV infection early in childhood, before introduction of the vaccine, and now have chronic HBV infection.1,7 During 2004–2008, an estimated 54,000 people with HBV infection immigrated to the United States.7 As many as 66% of people with chronic HBV infection are unaware they are infected.8,9 Since 2008, the Centers for Disease Control and Prevention (CDC) has recommended hepatitis B testing with the hepatitis B surface antigen (HBsAg) test for at-risk people, including those born in regions with intermediate-to-high HBsAg prevalence (≥2%), U.S.-born people not vaccinated as infants whose parents were born in regions with high HBsAg prevalence (≥8%), household contacts or sexual partners of people with hepatitis B, men who have sex with men, injection drug users, human immunodeficiency virus (HIV)-positive people, and pregnant women.2 A recent CDC study indicated that more than half of racial/ethnic minority groups who meet CDC criteria for screening are not tested for HBV, and only one-third of HBsAg-positive individuals receive specialty care.10
To mitigate viral hepatitis-associated morbidity and mortality, the U.S. Department of Health and Human Services developed the Action Plan for the Prevention, Care, and Treatment of Viral Hepatitis in 2011, which included measures to reduce health disparities among populations affected by hepatitis B. The action plan called for resources to expand community-based programs that provide hepatitis B testing and immunization services for foreign-born populations.8 CDC and the U.S. Preventive Services Task Force recommend HBV testing of all foreign-born people from countries with HBsAg prevalence ≥2%, referral of infected people to care, and referral of close contacts for testing and immunization.2,11 Identifying foreign-born people with chronic HBV infection and linking them to care is a public health priority.
As part of the Hepatitis Testing and Linkage to Care (HepTLC) initiative, which promoted viral hepatitis B and hepatitis C screening, posttest counseling, and linkage to care at 34 U.S. sites from October 2012 through September 2014, CDC awarded funds to several programs. Preliminary results from October 2012 through March 2014 in three programs conducting hepatitis B screening identified 310 of 4,727 participants tested (7%) as HBsAg positive, 203 (66%) of whom had documented attendance at medical visits to which they were referred.12 We report final HBV testing and linkage-to-care results from all programs participating in the hepatitis B screening portion of the HepTLC initiative.
METHODS
CDC funded nine programs to conduct hepatitis B screening, posttest counseling, and linkage to care for HBsAg-positive individuals from October 2012 through September 2014. The programs were located in Chicago, Illinois; Columbus, Ohio; Jacksonville, Florida; Minneapolis-St. Paul, Minnesota; New York, New York; Portland, Oregon; Sacramento, California; San Diego, California; and San Francisco, California. Each program focused testing efforts on foreign-born people (some of whom were refugees) ≥18 years of age from countries with HBV infection prevalence ≥2% (i.e., African and Asian countries). To recruit foreign-born people for testing, the programs conducted outreach efforts through community-based organizations and partnered with medical providers (i.e., primary care providers and/or specialists) who conducted testing.
Programs tested participants for HBsAg and antibody to hepatitis B core antigen (anti-HBc) in community or clinical settings. Hepatitis B surface antibody testing was not performed. Programs were required to document whether or not participants received their HBV test results and, for those who tested HBsAg positive, whether or not they received posttest counseling and referral to care. Some programs initiated patient navigation processes (i.e., individualized efforts to help patients access and receive health-care services to increase the number of people who follow up on referrals and receive recommended care). Data regarding attendance at scheduled medical visits were based on self-report. Programs were also required to document the number of HBsAg-positive participants reported to state and local health department surveillance systems within six months of diagnosis. Data from these programs were entered into EvaluationWeb®, an Internet-based data management system.13 Performance evaluations were distributed to each program monthly.
Demographic characteristics, including sex, age, birth year, race/ethnicity, and birth country, were collected. Risk-factor data were obtained through voluntary participant response to a questionnaire that asked if the participant had a history of injection drug use, was a man who has had sex with a man or transgender male, was a household contact or sexual partner of a person known to be infected with HBV, had multiple sexual partners, or was positive for HIV. Health insurance status and self-reported immunization history for hepatitis A/B were also collected.
We calculated the proportions of participants tested for HBsAg and anti-HBc, testing HBsAg positive, and receiving test results. For HBsAg-positive participants, we also assessed linkage-to-care indicators, which we defined as the proportion who received posttest counseling, were referred to medical care, and had a self-reported medical visit. We also assessed the number of HBsAg-positive results reported to state and local health department surveillance systems for each program. We stratified the results for HBsAg-positive participants by country of origin and further categorized participants by region of origin based on the World Health Organization world region classification.14 We further divided the Pan-American region into North America (including Central American countries) and South America. Because HBV infection prevalence varies within Europe,1 we divided this region into Western Europe and Eastern Europe using the World Bank regional classification.15 All analyses were conducted using Pearson's c2 test, with p<0.05 considered significant. We used SAS® version 9.3 for all analyses.16
RESULTS
Of 23,144 participants tested for HBV at nine U.S. programs, 1,317 (6%) were HBsAg-positive (Table 1). Of 20,507 participants with both HBsAg and anti-HBc test results available, 8,409 (41%) had evidence of past infection (i.e., HBsAg negative, anti-HBc positive). Of 12,411 participants with available data on hepatitis immunization, 4,566 (37%) reported receiving any hepatitis vaccine. Of 694 HBsAg-positive participants with hepatitis immunization information, 158 (23%) reported receiving any hepatitis vaccine. Of 19,882 participants with documented health insurance status, 12,441 (62%) had insurance, of which 8,124 (65%) was public insurance, 3,427 (28%) was private insurance, and 890 (7%) was unknown. Of 1,118 HBsAg-positive participants who reported their health insurance status, 633 (57%) reported having health insurance.
Table 1.
Number of participants tested for hepatitis B surface antigen (HBsAg) through the Hepatitis Testing and Linkage to Care (HepTLC) initiative and percentage HBsAg-positive participants linked to care, by program, October 2012–September 2014a
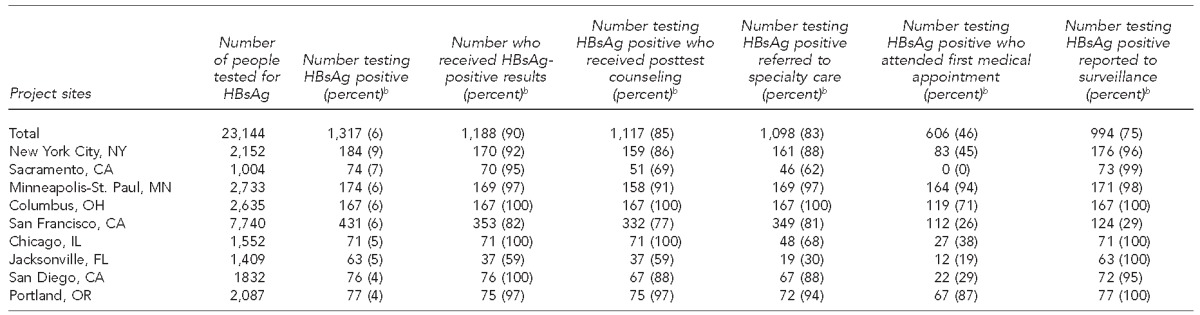
The HepTLC initiative promoted viral hepatitis B and hepatitis C screening, posttest counseling, and linkage to care at 34 U.S. sites during 2012–2014.
bPercentages are row percentages.
Of 1,317 HBsAg-positive participants, 1,188 (90%) received their test results, 1,110 (84%) received posttest counseling, and 1,065 (81%) were referred to medical care. Of those referred to care, 246 (23%) were referred to a specialist and the others were referred to primary care or another general medical facility. Six hundred six of 1,317 (46%) HBsAg-positive participants reported attendance at their first medical appointment, and equal proportions of participants with and without health insurance attended a first medical appointment (54% vs. 53%, p=0.718). Of 525 participants with documented dates for a first medical appointment, the median time from referral to medical appointment attendance was 32 days (interquartile range [IQR] = 7–42 days). Of 21,827 HBsAg-negative participants, 16,337 (75%) received their test results and 2,901 (13%) received posttest counseling. A total of 994 of 1,317 (76%) HBsAg-positive participants were reported to local or state surveillance systems (Table 1).
The median age of those tested was 49 years (IQR=31–60) and of those testing HBsAg-positive was 47 years (IQR=35–58). A higher proportion of men than women tested HBsAg-positive (7% vs. 4%, p<0.001). Significantly higher proportions of HBsAg positivity were seen among non-Hispanic black/African (11%, p<0.001) and Asian (6%, p<0.001) participants compared with non-Hispanic white participants (1%). Of note, however, the number of Asians tested for HBsAg (n=13,901) was significantly higher (p<0.001) than the number of participants tested from other racial/ethnic groups. Additionally, more participants were aged 19–64 years (n=19,546) than ≥65 years (n=3,598). Of the 23,144 participants tested for HBsAg, 20,812 (90%) were foreign-born and 19,272 (83%) were born in countries with intermediate-to-high (≥2%) HBsAg prevalence, of whom 1,130 (6%) tested HBsAg-positive. Only two (2%) of 132 participants with risk factors other than being foreign-born tested HBsAg-positive, and 112 (4%) of 3,207 participants reported no known risk factors (Table 2).
Table 2.
Characteristics of participants tested for hepatitis B surface antigen (HBsAg) through the Hepatitis Testing and Linkage to Care (HepTLC) initiative and percentage HBsAg positive who received results, nine U.S. programs, October 2012–September 2014a
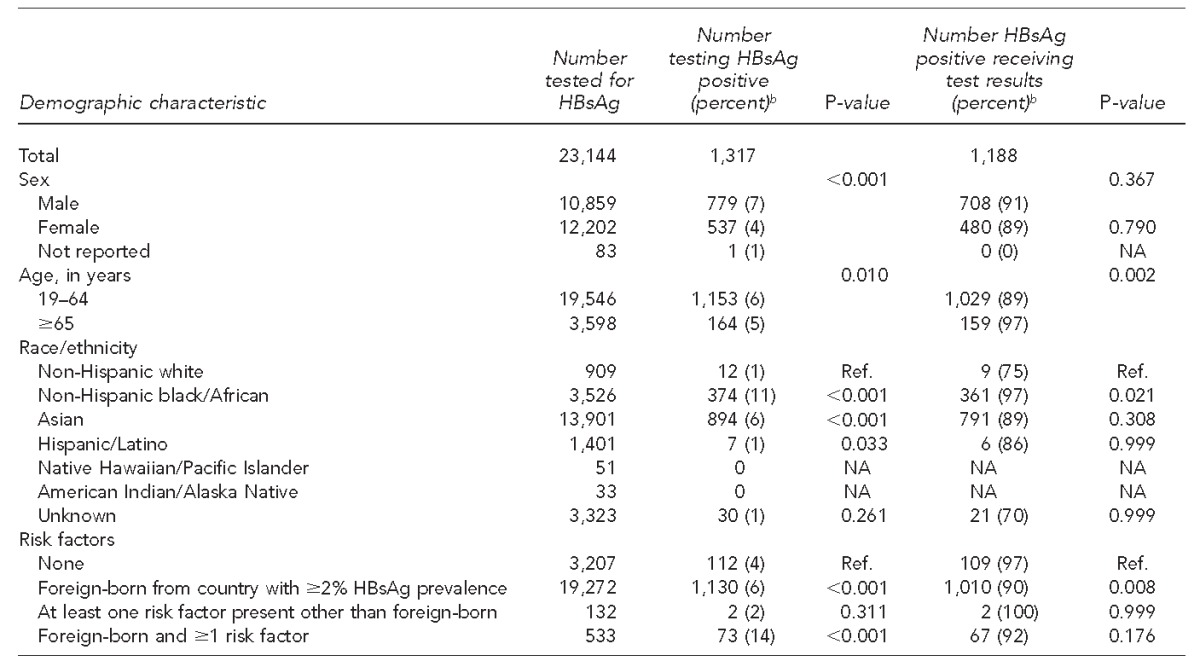
The HepTLC initiative promoted viral hepatitis B and hepatitis C screening, posttest counseling, and linkage to care at 34 U.S. sites during 2012–2014, including nine programs for hepatitis B virus testing in Chicago, Illinois; Columbus, Ohio; Jacksonville, Florida; Minneapolis-St. Paul, Minnesota; New York, New York; Portland, Oregon; Sacramento, California; San Diego, California; and San Francisco, California.
bPercentages are row percentages.
NA = not applicable
Ref. = reference group
A significantly greater proportion of men than women (49% vs. 41%, p<0.001) attended their first medical appointment. Linkage to care did not differ significantly by race/ethnicity (Table 3). Significantly more people aged 19–64 years compared with those aged ≥65 years attended their first medical appointment (50% vs. 20%, p<0.001).
Table 3.
Characteristics of participants tested for hepatitis B surface antigen (HBsAg) and percentage HBsAg-positive who were linked to care through the Hepatitis Testing and Linkage to Care (HepTLC) initiative, nine U.S. programs, October 2012–September 2014a
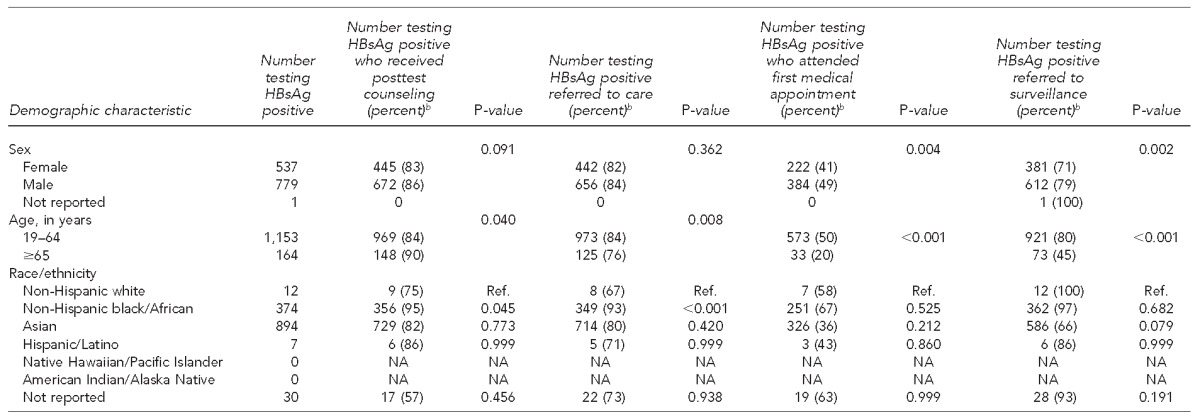
The HepTLC initiative promoted viral hepatitis B and hepatitis C screening, posttest counseling, and linkage to care at 34 U.S. sites during 2012–2014, including nine programs for hepatitis B virus testing in Chicago, Illinois; Columbus, Ohio; Jacksonville, Florida; Minneapolis-St. Paul, Minnesota; New York, New York; Portland, Oregon; Sacramento, California; San Diego, California; and San Francisco, California.
bPercentages are row percentages.
Ref. = reference group
NA = not applicable
By region of origin, the highest proportion of HBsAg-positive participants was among those born in the African and Western Pacific regions. Regarding participants with an unknown country of birth, 101 of 1,612 (6%) participants were HBsAg positive. Among cohorts from African countries of origin for which at least 10 participants were tested, most had HBsAg positivity ≥2%, including Mauritania (23%), Mali (16%), Sierra Leone (16%), Liberia (16%), Guinea (15%), Senegal (12%), Togo (10%), Burkina Faso (10%), Central African Republic (10%), Ghana (9%), Cameroon (9%), Ivory Coast (9%), Nigeria (9%), Benin (9%), the Democratic Republic of Congo (7%), Congo (7%), Gambia (5%), Ethiopia (6%), and Eritrea (3%). Asian countries of birth with the highest proportion of participants testing HBsAg positive, and with at least 10 participants being tested, included Laos (12%), Myanmar (8%), Cambodia (7%), China (7%), Vietnam (7%), Hong Kong (7%), Taiwan (6%), Mongolia (6%), Indonesia (5%), Thailand (4%), Philippines (4%), Malaysia (3%), Nepal (2%), Bangladesh (2%), North Korea (2%), and Bhutan (2%). The majority of HBsAg tests and HBsAg-positive results were among participants from the Western Pacific region (Table 4).
Table 4.
Region of origin of HBsAg-positive participants tested through the Hepatitis Testing and Linkage to Care (HepTLC) initiative, nine U.S. programs, October 2012–September 2014a
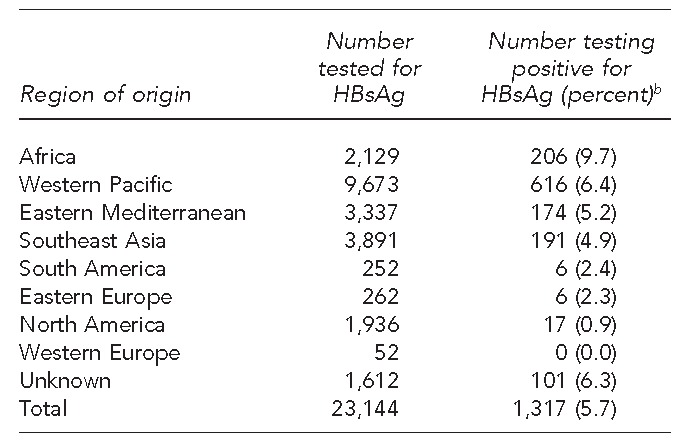
The HepTLC initiative promoted viral hepatitis B and hepatitis C screening, posttest counseling, and linkage to care at 34 U.S. sites during 2012–2014, including nine programs for hepatitis B virus testing in Chicago, Illinois; Columbus, Ohio; Jacksonville, Florida; Minneapolis-St. Paul, Minnesota; New York, New York; Portland, Oregon; Sacramento, California; San Diego, California; and San Francisco, California.
bPercentages are row percentages.
HBsAg = hepatitis B surface antigen
DISCUSSION
The HepTLC initiative demonstrated the feasibility of (1) identifying a substantial number of foreign-born individuals with chronic hepatitis B infection through focused outreach and testing and (2) providing posttest counseling and referral to care.
The models and innovations used to facilitate HBV testing varied among the nine programs but yielded noteworthy results. Educational curricula and training protocols developed and implemented with community partners likely contributed to successful recruitment. For example, the Minnesota program expanded -existing services for newly arrived and previously arriving refugees by implementing a clinic voucher referral system and an outreach referral model to target those from HBV-endemic countries for testing. Other programs incorporated educational messages and coordination of care as a routine process.
Although many foreign-born Asians have not been screened for chronic HBV infection in the United States,17–19 efforts to address disparities in testing through targeted community-based interventions have shown some success.10 A documented barrier to testing and linkage to care of Asians is poor knowledge of hepatitis B prevention; however, ethnically and linguistically targeted education and testing offered in community settings can increase testing rates.20
Correlates of successful HBV screening campaigns and subsequent linkage to care in programs participating in the HepTLC initiative included partnerships between community-based organizations and medical providers, as well as patient navigation services. Programs that leveraged culturally and linguistically matched staff members to priority groups appeared to be most beneficial for testing uptake. Many programs used the following approaches to increase testing uptake: incentives (e.g., gift cards, vaccination vouchers, bus tokens, and transportation vouchers); community radio, newspapers, and cultural events; and identifying culturally and linguistically appropriate providers.21,22 Program staff members cited patient navigation as the most critical element in ensuring that patients attended their first medical appointment. Although more than two-thirds of HBsAg-positive participants were referred to care, and several programs had high proportions of HBsAg-positive participants who attended at least a first medical appointment, we identified substantial gaps for most programs in establishing linkages to HBV-directed medical care.
A frequently cited barrier was lack of sufficient resources to guide HBsAg-positive participants through the continuum of care. Through the HepTLC initiative, programs with higher proportions of HBsAg-positive participants attending their first medical appointment had been able to hire bilingual staff members from the target population to serve as translators, navigators, and educators to address logistical challenges. Implementers believe that this model was well accepted in their communities and helped to build a foundation of trust within target populations. Programs with smaller proportions of HBsAg-positive participants attending their first medical appointment noted the following challenges: cultural and linguistic barriers, limited access to medical care (e.g., insufficient numbers of providers available to conduct follow-up evaluation), lack of health insurance for many immigrants and refugees, and programs' inability to access some of the communities at risk. Future initiatives are needed to develop strategies to overcome these barriers and link individuals with chronic HBV infection to care.
People with chronic HBV infection who develop decompensated cirrhosis and hepatocellular carcinoma are frequently asymptomatic until they present with these advanced complications.23 Effective therapies exist for chronic HBV infection that substantially reduce the risk for HBV-related complications3 and, although not all people with chronic HBV infection need antiviral treatment, current management recommendations call for a thorough baseline medical examination and regular follow-up.3 Programs that test, treat, and vaccinate immigrants at risk for HBV infection are cost-effective24 and critical to reducing HBV-associated morbidity and mortality.2,25,26 Networks of outpatient primary care centers that partner with community-based organization (i.e., to increase hepatitis B awareness in the community) are most effective in linking foreign-born people with chronic HBV infection to care.27,28 Future initiatives should promote partnerships between outpatient health centers and community-based organizations.
Through the HepTLC initiative, we learned that common barriers limiting linkage to care include the cost of clinical services and a misperception among people with chronic HBV infection that no effective therapies exist. Therapies for chronic HBV infection are cost-effective and can potentially be made affordable through multiple avenues, in addition to high-quality private insurance, including pharmaceutical patient-assistance programs, public insurance (i.e., Medicare/Medicaid), and increased access to care through provisions of the Affordable Care Act.28–30 Community-based organizations may play a role in navigating individuals with chronic HBV infection through the care cascade by leveraging insurance program services and by forming strategic partnerships with providers of specialist services to help increase access for foreign-born people. In the HepTLC initiative, more than half of people with chronic HBV infection had any health insurance and only half attended their first medical appointment, which is consistent with the limitations seen in other studies examining racial/ethnic minority groups' access to follow-up care for chronic HBV infection.10 Improving patient and provider knowledge about chronic HBV infection management may improve linkage to care among foreign-born people;20 outreach strategies could include efforts to ensure that information on care and treatment options is provided to targeted populations and that providers serving these populations receive training on current professional recommendations for care.
In the HepTLC inititiave, programs in Minnesota, Columbus, and Portland attained high proportions of HBsAg-positive participants achieving linkage-to-care indicators through strategic partnerships with community-based organizations and primary care clinics that utilized patient navigators. For example, the Minnesota program's partnership with a local refugee program resulted in 90% of HBsAg-positive participants having attended their first medical appointment because patient navigators assisted with scheduling medical appointments and transportation to the medical clinic. Minnesota's approach exemplifies how dynamic partnerships among refugee programs, medical providers, and health departments can enhance a program and improve the proportion of people with chronic HBV infection who know their status and are linked to care.
Limitations
This analysis was subject to several limitations. Data regarding attendance at scheduled medical appointments were self-reported. At the time the data were finalized, many HBsAg-positive participants had pending medical appointments, so it was not possible to document their first medical appointment, which could have resulted in under-ascertainment of this variable. Although study programs were geographically diverse and targeted foreign-born participants at risk, the sample may not be representative of all foreign-born people in the United States. Lastly, although it is recommended that HBsAg-positive people be retested six months after the first test result to confirm their chronic HBV infection status,11 the design of this initiative did not facilitate retesting.
CONCLUSION
The community-based efforts to screen foreign-born people from HBV-endemic countries were effective in testing, counseling, and referring people with chronic HBV infection to medical care. However, referral to care did not necessarily result in successfully attending a first medical appointment. Outreach, counseling, and case management require extensive use of human resources; thus, strong partnerships between health centers and community-based organizations can improve efficiencies in providing these services. In this initiative, it was not possible to assess the quality of HBV-directed medical care for those who attended their first medical appointment. Future efforts might place greater emphasis on linkage to HBV-directed medical care and assessment of care quality.
Footnotes
The authors thank the following programs for their participation in the Hepatitis Testing and Linkage to Care (HepTLC) initiative: African Services Committee in New York, New York; University of California, Davis, Davis, California; Minnesota Department of Health, Saint Paul, Minnesota; Ohio Asian American Health Coalition, Columbus, Ohio; City and County of San Francisco, San Francisco, California; Asian Health Coalition, Chicago, Illinois; University of Florida, Gainesville, Florida; University of California at San Diego, San Diego, California; and Multnomah County Health Department, Portland, Oregon. The authors thank Deborah Bedell, Margaret Patterson, and Rebecca Cabral from the Centers for Disease Control and Prevention's (CDC's) Division of Viral Hepatitis for their programmatic support throughout this initiative and input into the development of the article.
The HepTLC initiative was supported by the U.S. Department of Health and Human Services Prevention and Public Health Fund. The HepTLC initiative was a programmatic public health activity and received a non-research project determination by CDC's human subjects office. As such, institutional review board review was not required. The findings and conclusions in this article are those of the authors and do not necessarily represent the views of CDC.
REFERENCES
- 1.Kowdley KV, Wang CC, Welch S, Roberts H, Brosgart CL. Prevalence of chronic hepatitis B among foreign-born persons living in the United States by country of origin. Hepatology. 2012;56:422–33. doi: 10.1002/hep.24804. [DOI] [PubMed] [Google Scholar]
- 2.Weinbaum CM, Williams I, Mast EE, Wang SA, Finelli L, Wasley A, et al. Recommendations for identification and public health management of persons with chronic hepatitis B virus infection. MMWR Recomm Rep. 2008;57(RR-8):1–20. [PubMed] [Google Scholar]
- 3.Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology. 2009;50:661–2. doi: 10.1002/hep.23190. [DOI] [PubMed] [Google Scholar]
- 4.Stevens CE, Beasley RP, Tsui J, Lee WC. Vertical transmission of hepatitis B antigen in Taiwan. N Engl J Med. 1975;292:771–4. doi: 10.1056/NEJM197504102921503. [DOI] [PubMed] [Google Scholar]
- 5.Hepatitis B vaccines. Wkly Epidemiol Rec. 2009;84:405–19. [PubMed] [Google Scholar]
- 6.World Health Organization. Hepatitis B. July 2015 [cited 2016 Mar 17] Available from: http://www.who.int/mediacentre/factsheets/fs204/en.
- 7.Mitchell T, Armstrong GL, Hu DJ, Wasley A, Painter JA. The increasing burden of imported chronic hepatitis B—United States, 1974–2008. PLoS One. 2011;6:e27717. doi: 10.1371/journal.pone.0027717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Department of Health and Human Services (US) Rockville (MD): HHS; 2011. Combating the silent epidemic of viral hepatitis: action plan for the prevention, care, and treatment of viral hepatitis. [Google Scholar]
- 9.Lin SY, Chang ET, So SK. Why we should routinely screen Asian American adults for hepatitis B: a cross-sectional study of Asians in California. Hepatology. 2007;46:1034–40. doi: 10.1002/hep.21784. [DOI] [PubMed] [Google Scholar]
- 10.Hu DJ, Xing J, Tohme RA, Liao Y, Pollack H, Ward JW, et al. Hepatitis B testing and access to care among racial and ethnic minorities in selected communities across the United States, 2009–2010. Hepatology. 2013;58:856–62. doi: 10.1002/hep.26286. [DOI] [PubMed] [Google Scholar]
- 11.LeFevre ML U.S. Preventive Service Task Force. Screening for hepatitis B virus infection in nonpregnant adolescents and adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;161:58–66. doi: 10.7326/M14-1018. [DOI] [PubMed] [Google Scholar]
- 12.Beckett GA, Ramirez G, Vanderhoff A, Nichols K, Chute SM, Wyles DL, et al. Early identification and linkage to care of persons with chronic hepatitis B virus infection—three U.S. sites, 2012–2014. MMWR Morb Mortal Wkly Rep. 2014;63(18):399–401. [PMC free article] [PubMed] [Google Scholar]
- 13.Luther Consulting LLC. Carmel (IN): Luther Consulting LLC; 2013. EvaluationWeb®: Version 5. [Google Scholar]
- 14.World Health Organization. Definition of region groupings [cited 2016 Mar 17] Available from: http://www.who.int/healthinfo/global_burden_disease/definition_regions/en.
- 15.The World Bank. Countries [cited 2016 Mar 17] Available from: http://www.worldbank.org/en/country.
- 16.SAS Institute, Inc. Cary (NC): SAS Institute, Inc.; 2010. SAS®: Version 9.3. [Google Scholar]
- 17.Coronado GD, Taylor VM, Tu SP, Yasui Y, Acorda E, Woodall E, et al. Correlates of hepatitis B testing among Chinese Americans. J Community Health. 2007;32:379–90. doi: 10.1007/s10900-007-9060-x. [DOI] [PubMed] [Google Scholar]
- 18.Shiau R, Bove F, Henne J, Zola J, Fang T, Fernyak S. Using survey results regarding hepatitis B knowledge, community awareness and testing behavior among Asians to improve the San Francisco Hep B Free campaign. J Community Health. 2012;37:350–64. doi: 10.1007/s10900-011-9452-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taylor VM, Talbot J, Do HH, Liu Q, Yasui Y, Jackson JC, et al. Hepatitis B knowledge and practices among Cambodian Americans. Asian Pac J Cancer Prev. 2011;12:957–61. [PMC free article] [PubMed] [Google Scholar]
- 20.Nishimura A, Shiono P, Stier D, Shallow S, Sanchez M, Huang S. Knowledge of hepatitis B risk factors and prevention practices among individuals chronically infected with hepatitis B in San Francisco, California. J Community Health. 2012;37:153–8. doi: 10.1007/s10900-011-9430-2. [DOI] [PubMed] [Google Scholar]
- 21.Perumalswami PV, Factor SH, Kapelusznik L, Friedman SL, Pan CQ, Chang C, et al. Hepatitis Outreach Network: a practical strategy for hepatitis screening with linkage to care in foreign-born communities. J Hepatol. 2013;58:890–7. doi: 10.1016/j.jhep.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 22.Xu JJ, Tien C, Chang M, Rhee J, Tien A, Bae HS, et al. Demographic and serological characteristics of Asian Americans with hepatitis B infection diagnosed at community screenings. J Viral Hepat. 2013;20:575–81. doi: 10.1111/jvh.12073. [DOI] [PubMed] [Google Scholar]
- 23.Fattovich G, Bortolotti F, Donato F. Natural history of chronic hepatitis B: special emphasis on disease progression and prognostic factors. J Hepatol. 2008;48:335–52. doi: 10.1016/j.jhep.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 24.Wong WW, Woo G, Jenny Heathcote E, Krahn M. Cost effectiveness of screening immigrants for hepatitis B. Liver Int. 2011;31:1179–90. doi: 10.1111/j.1478-3231.2011.02559.x. [DOI] [PubMed] [Google Scholar]
- 25.Mast EE, Margolis HS, Fiore AE, Brink EW, Goldstein ST, Wang SA, et al. A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP) part 1: immunization of infants, children, and adolescents [published erratum appears in MMWR Morb Mortal Wkly Rep 2006;55(6):158-9 and MMWR Morb Mortal Wkly Rep 2007;56(48):1267] MMWR Recomm Rep. 2005;54(RR-16):1–31. [PubMed] [Google Scholar]
- 26.Mast EE, Weinbaum CM, Fiore AE, Alter MJ, Bell BP, Finelli L, et al. A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP) part II: immunization of adults [published erratum appears in MMWR Morb Mortal Wkly Rep 2007;56(42):1114] MMWR Recomm Rep. 2006;55(RR-16):1–33. [PubMed] [Google Scholar]
- 27.Bailey MB, Shiau R, Zola J, Fernyak SE, Fang T, So SK, et al. San Francisco Hep B Free: a grassroots community coalition to prevent hepatitis B and liver cancer. J Community Health. 2011;36:538–51. doi: 10.1007/s10900-010-9339-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rein DB, Lesesne SB, Smith BD, Weinbaum CM. Models of community-based hepatitis B surface antigen screening programs in the U.S. and their estimated outcomes and costs. Public Health Rep. 2011;126:560–7. doi: 10.1177/003335491112600412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eckman MH, Kaiser TE, Sherman KE. The cost-effectiveness of screening for chronic hepatitis B infection in the United States. Clin Infect Dis. 2011;52:1294–306. doi: 10.1093/cid/cir199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Post SE, Sodhi NK, Peng CH, Wan K, Pollack HJ. A simulation shows that early treatment of chronic hepatitis B infection can cut deaths and be cost-effective [published erratum appears in Health Aff (Millwood) 2011;30:538] Health Aff (Millwood) 2011;30:340–8. doi: 10.1377/hlthaff.2008.0905. [DOI] [PMC free article] [PubMed] [Google Scholar]


