Abstract
Objective
The Hepatitis Testing and Linkage to Care (HepTLC) initiative promoted viral hepatitis B and hepatitis C screening, posttest counseling, and linkage to care at 34 U.S. sites from 2012 to 2014. Through the HepTLC initiative, the Minnesota Department of Health (MDH) and clinic partners began conducting linkage-to-care activities with hepatitis B-positive refugees in October 2012. This intervention provided culturally appropriate support to link refugees to follow-up care for hepatitis B.
Methods
MDH refugee health and viral hepatitis surveillance programs, along with clinics that screened newly arrived refugees in Hennepin and Ramsey counties in Minnesota, collaborated on the project, which took place from October 1, 2012, through September 30, 2014. Bilingual care navigators contacted refugees to provide education, make appointments, and arrange transportation. We compared the linkage-to-care rate for participants with the rates for refugees screened the year before project launch using a two-sample test of proportions.
Results
In the year preceding the project (October 2011 through September 2012), 87 newly arrived refugees had a positive hepatitis B surface antigen (HBsAg) test. Fifty-six (64%) refugees received follow-up care, 12 (14%) refugees did not receive follow-up care, and 19 (22%) refugees could not be located and had no record of follow-up care. During the project, 174 HBsAg-positive, newly arrived refugees were screened. Of those 174 refugees, 162 (93%) received follow-up care, seven (4%) did not receive follow-up care, and five (3%) could not be located and had no record of follow-up care. The one-year linkage-to-care rate for project participants (93%) was significantly higher than the rate for refugees screened the previous year (64%) (p<0.001).
Conclusion
In the context of a strong screening and surveillance infrastructure, a simple intervention improved the linkage-to-care rate for HBsAg-positive refugees.
Chronic infection with hepatitis B virus (HBV) is a serious health concern for foreign-born U.S. residents. Among cases of chronic HBV infection reported to the Centers for Disease Control and Prevention (CDC) from 2001 to 2010 with known country of origin, about 90% of these individuals were born outside the United States.1 An estimated 1.3 million foreign-born individuals were living with chronic HBV infection in the United States in 2009.2
In Minnesota, 4,197 newly identified chronic HBV infections were reported to the Minnesota Department of Health (MDH) viral hepatitis surveillance program from 2009 to 2013. Of those infected, 2,364 (56%) were known to be foreign-born. Among chronic HBV infection cases reported to MDH, the most common risk factor was being born outside the United States.3
Individuals chronically infected with HBV are at increased risk for developing liver disease.4 Globally, an estimated 30% of cirrhosis cases and 53% of hepatocellular carcinoma cases—the most common type of primary liver cancer—are associated with chronic HBV infection.5 Regular monitoring of individuals with chronic HBV infection allows earlier detection of cirrhosis and potentially better outcomes for patients.6
A lack of familiarity with the U.S. health-care system, language barriers, and cultural and economic factors may prevent refugees with chronic HBV infection from understanding the implications of their infection and accessing ongoing care. Refugees diagnosed with chronic HBV infection at their initial screening may go years without follow-up care.7 Staff members and resources dedicated to culturally, linguistically competent linkage-to-care activities for refugees are needed.
REFUGEES IN MINNESOTA
Minnesota is home to diverse, thriving refugee communities, and the 9,877 primary refugees (i.e., those who resettle directly in Minnesota) who resettled in Minnesota from 2009 to 2013 came from 56 countries on five continents. The majority arrived from Burma (40%) and Somalia (29%).8
Many of Minnesota's refugees come from HBV-endemic countries, and chronic HBV infection is an important health issue for these refugee communities. Upon arrival in the United States, all refugees are encouraged to complete an initial health assessment. Of the 9,877 primary refugees arriving in Minnesota from 2009 to 2013, 9,591 were eligible for this assessment (i.e., residing in Minnesota and able to be located at the time of their assessment, which takes place within 90 days of their arrival in the United States). Of these, 9,485 (99%) completed screening. Among those screened, 9,342 (98%) were tested for hepatitis B surface antigen (HBsAg), 556 (6%) of whom tested positive, including 8% of refugees from Southeast Asia.8
MDH Refugee Health Program (RHP) and local partners
The MDH RHP is responsible for maintaining a public health infrastructure to control communicable diseases among refugees newly arrived in Minnesota. MDH depends on collaboration with local public health departments to ensure timely completion of the initial refugee health assessment, including HBV screening.
Among Minnesota's 9,485 newly arrived refugees who completed screening from 2009 to 2013, 4,734 (50%) were screened in Ramsey County, 2,742 (29%) were screened in Hennepin County, and 2,009 (21%) were screened in other counties. Ramsey County, which includes St. Paul, is the second-largest county in Minnesota, and Hennepin County, which includes Minneapolis, is the largest county in Minnesota.9
The MDH RHP provides a recommended refugee screening protocol to Minnesota counties, based on CDC guidelines.10 Counties adopt varied models for screening. Newly arriving refugees in Hennepin County receive their initial health assessment at the Hennepin County Public Health Clinic. St. Paul-Ramsey County Public Health coordinates screenings at designated private clinics for refugees arriving in Ramsey County.
MDH viral hepatitis surveillance
Refugee health and viral hepatitis surveillance activities are conducted within the same division at MDH. The MDH viral hepatitis surveillance team collects, analyzes, and disseminates data on the burden of disease from viral hepatitis in Minnesota. Surveillance for viral hepatitis in Minnesota is longstanding. A chronic disease registry has been maintained for chronic HBV infection since 1987; since 2013, viral hepatitis data have been integrated into the Minnesota Electronic Disease Surveillance System (MEDSS). Demographic, laboratory, clinical, and risk-factor data are collected, as available.
Surveillance staff members evaluate all reports and perform triage for follow-up. Women of childbearing age with HBV infection are referred to the perinatal hepatitis B program for investigation. Suspected acute cases are investigated through a telephone call with the health-care provider to confirm the case and gather demographic and risk-factor information. People <30 years of age with hepatitis B are investigated using acute hepatitis protocols to identify recent infection.
Need for enhanced linkage to care
Supported by the Prevention and Public Health Fund and supplemental funds, the Hepatitis Testing and Linkage to Care (HepTLC) initiative promoted viral hepatitis B and hepatitis C screening, posttest counseling, and linkage to care at 34 U.S. sites from 2012 through 2014. MDH and its local partners have achieved a high HBV screening rate among newly arriving refugees and maintained a strong viral hepatitis surveillance system. Prior to the HepTLC initiative, however, MDH and local public health agencies did not have the capacity to ensure that HBV-infected refugees were linked to primary or specialty care following initial testing. MDH and local public health agencies recommended that screening providers refer patients to follow-up care, but lacked the resources to monitor whether or not referrals were being made, facilitate linkage to care, or track outcomes. We describe and analyze the results of activities in Minnesota's two largest counties to link refugees to medical care for chronic HBV infection.
METHODS
The HepTLC initiative
The HepTLC initiative ran from October 1, 2012, through September 30, 2014. MDH identified the initiative's target population as primary refugees who were screened for HBV infection in their initial health assessment in Hennepin and Ramsey counties. From 2009 to 2013, 67% of Ramsey County refugee arrivals were Burmese and 60% of Hennepin County refugee arrivals were Somali.8
Because HBV screening was already routinely conducted during refugees' initial health assessment and paid for by Minnesota's Medicaid program, MDH requested funding solely for linkage-to-care activities. Refugees with positive HBsAg tests who agreed to participate in the project received linkage-to-care assistance.
For the HepTLC initiative, we defined linkage to care as attending one HBV-directed medical appointment following initial HBV testing. For refugees in Minnesota, the initial refugee health assessment generally consists of two appointments: one for receiving HBsAg testing and one for receiving test results. Our team considered a participant linked to care if he or she received HBV-related care at some point after the second assessment visit. We defined care as HBV-related follow-up testing, monitoring (e.g., a liver ultrasound), or discussion.
MDH hired two undergraduate students as bilingual care navigators—one fluent in Somali and English, the other in Karen and English—for the HepTLC initiative. Karen and Somali are two of the most common languages spoken by refugees arriving in Minnesota in recent years.8 A graduate student handled the project's day-to-day operations. The MDH international health coordinator supervised the student workers. Epidemiologists in refugee health and viral hepatitis surveillance provided data-related support.
The bilingual care navigators played a central role in linking participating refugees to care. After a refugee agreed to participate in the project, the navigators provided culturally appropriate education in the participant's native language in person or by telephone (using a telephone interpreter service when necessary). The education script covered basic facts about hepatitis B and its transmission and emphasized the need for ongoing monitoring and care. To gauge participants' understanding, the care navigators asked comprehension questions such as, “What are some ways hepatitis B can be transmitted from person to person?” and “Why is seeing your health-care provider regularly for follow-up care important?” The MDH team developed the script with sensitivity toward the refugee patient population—acknowledging, for example, that many of these individuals were likely infected perinatally.
With guidance from screening providers, the care navigators made primary or specialty care appointments for participants. They arranged free transportation through each refugee's clinic or medical plan, or through a taxi fund set up for the project. They made reminder and follow-up calls to ensure that patients attended their appointments. Navigators also identified barriers that kept refugees from care and worked with other MDH staff members and partners to address those challenges.
The linkage-to-care model was implemented differently in Ramsey and Hennepin counties. In Ramsey County, four private clinics conducted nearly all of the refugee health screenings: the HealthPartners Center for International Health, HealthEast Roselawn Clinic, HealthEast Roseville Clinic, and University of Minnesota Physicians Bethesda Clinic. Clinics notified MDH of newly screened, HBsAg-positive refugees by submitting the HepTLC data form designed by CDC and modified by MDH. In many cases, the clinician referred the patient to primary care, often in-house, or to specialty care. Screening clinics, which provided referral and upcoming appointment information to MDH, commonly scheduled follow-up appointments for project participants in Ramsey County.
The Hennepin County Public Health Clinic conducted all screenings for newly arrived refugees residing in Hennepin County. The clinic notified MDH in advance of each HBsAg-positive refugee's second assessment appointment. One of the care navigators met with the refugee at that appointment to provide education and schedule a follow-up appointment.
MDH met with local public health and clinic partners periodically during the HepTLC initiative: first to request their participation and plan for implementation, and later to discuss challenges and successful strategies in reporting eligible patients to MDH and contributing to their linkage to care. These meetings gave the team a chance to problem-solve and make procedural adjustments to meet project objectives.
Data sources and analysis
During the HepTLC initiative, data from multiple sources were used to identify potential participants, track outcomes, and report demographic data and results to CDC. Screening and demographic data were obtained from HepTLC forms submitted to MDH by screening clinics, MEDSS, and the MDH RHP database, the Electronic System for Health Assessment of Refugees (eSHARE). The MDH RHP developed eSHARE in 2004 to house domestic health screening data and immunization history. Now Internet-based, eSHARE allows remote data entry from screening sites. Data quality mechanisms and standard reports are built into the system, which has been shared with and adapted by several other states. The HepTLC initiative gave rise to enhanced data sharing between the RHP and the viral hepatitis surveillance program. Project participants and clinics were contacted for data on follow-up care. MDH reported data to CDC using HepTLC EvaluationWeb®, an online data management system.11
To assess the impact of the HepTLC initiative, we compared the linkage-to-care rate for project participants with the linkage-to-care rate for HBsAg-positive refugees screened in Hennepin and Ramsey counties in the year preceding the project (i.e., October 2011 through September 2012). We looked at linkage to care within one year of a refugee's initial screening date. For use in our analysis, CDC provided an official HepTLC dataset on project participants as reported by MDH during the project. This dataset included all participating refugees with initial HBV testing dates from October 1, 2012, through June 28, 2014.
Data on refugees screened from October 1, 2011, to September 30, 2012—the year preceding the project—came from eSHARE. To ascertain linkage-to-care outcomes for HBsAg-positive refugees screened in the year before the project as identified through eSHARE, we first checked their records in MEDSS. We considered an individual linked to care if HBV testing within one year of initial screening (excluding the second assessment appointment) was recorded in MEDSS. For refugees with no follow-up HBV testing data in MEDSS, we called the screening clinic to ask if the patient had received HBV-directed care in the year following screening. We also asked clinics about referrals for specialty care or records of HBV-related care from other clinics. We called any other medical facilities mentioned by the clinics.
If the screening clinic—and any other relevant clinic—reported no HBV-directed follow-up care, an MDH bilingual care navigator called the patient. We obtained patient telephone numbers from MEDSS, resettlement agencies, and clinics, as necessary. The care navigators used a script similar to the one developed for the HepTLC initiative, requesting the refugee's participation and providing education about hepatitis B. Navigators also asked participants if they had attended a clinic for hepatitis B care. The most important information to obtain was the name of any clinic the refugee had attended since his or her screening date or other details to help identify the clinic, such as its location or the provider's name. We called clinics mentioned by participants regardless of whether, and in what time frame, the refugee reported receiving HBV-related care. The final step in ascertaining linkage-to-care outcomes for refugees screened in the year preceding the HepTLC initiative was calling clinics following participants' reports of care.
We compiled demographic data (e.g., sex, age, and country of origin), vaccination history, and HBsAg test results for project participants and refugees screened in the year preceding the project. We then compared rates of linkage to care within one year for project participants and refugees screened the preceding year, overall and for each county, using two-sample tests of proportions with a significance level of a=0.05. Analyses were conducted using Stata® release 13.12
RESULTS
In the year preceding the HepTLC initiative, 1,399 refugees received HBsAg testing as part of the initial health screening in Hennepin and Ramsey counties. Eighty-seven (6%) of these refugees were HBsAg positive (Table). All of the refugees contacted agreed to speak with MDH.
Table.
Characteristics of newly arriving refugees screened for hepatitis B virus during the Hepatitis Testing and Linkage to Care (HepTLC) initiativea (October 2012 through June 2014) and in the preceding year (October 2011 through September 2012) in Hennepin and Ramsey counties, Minnesota
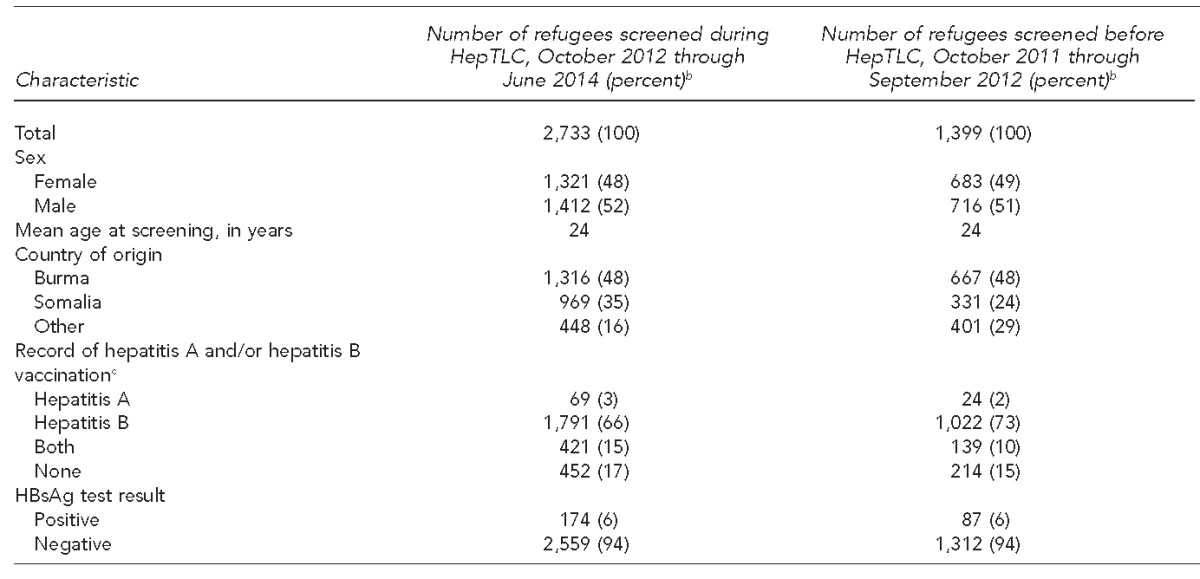
The HepTLC initiative promoted viral hepatitis B and hepatitis C screening, posttest counseling, and linkage to care at 34 U.S. sites.
bPercentages may not total to 100 because of rounding.
cDemographic and overseas vaccination data are from overseas medical records provided by the Centers for Disease Control and Prevention; domestic vaccination data and HBsAg test results are from refugee screening clinics. All of these data are compiled in the Electronic System for Health Assessment of Refugees (eSHARE), Minnesota's refugee health database.
HBsAg = hepatitis B surface antigen
Of the 87 HBsAg-positive individuals, 56 (64%) had been successfully linked to care and 12 (14%) had not been linked to care. Nineteen of the 87 (22%) HBsAg-positive individuals could not be located and had no HBV-related follow-up care data on record (Figure 1).
Figure 1.
Refugees screened for hepatitis B virus infection, Hennepin and Ramsey counties, Minnesota, October 2011 through September 2012
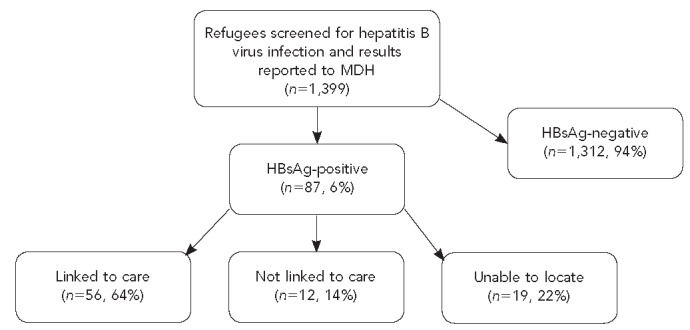
MDH = Minnesota Department of Health
HBsAg = hepatitis B surface antigen
During the HepTLC initiative, 2,733 project-eligible refugees were screened, 174 (6%) of whom were HBsAg-positive and eligible to receive linkage-to-care assistance (Table). All refugees contacted in the HepTLC period agreed to participate in the project. Among the 174 refugees contacted, 162 (93%) were successfully linked to care and seven (4%) were not (Figure 2). The seven who were not linked to care were lost to follow-up or moved out of Minnesota. Five of 174 (3%) HBsAg-positive refugees could not be reached and had no HBV-related follow-up care data on record.
Figure 2.
Refugees screened for hepatitis B virus infection during the Hepatitis Testing and Linkage to Care (HepTLC) initiative,a Hennepin and Ramsey counties, Minnesota, October 2012 through June 2014
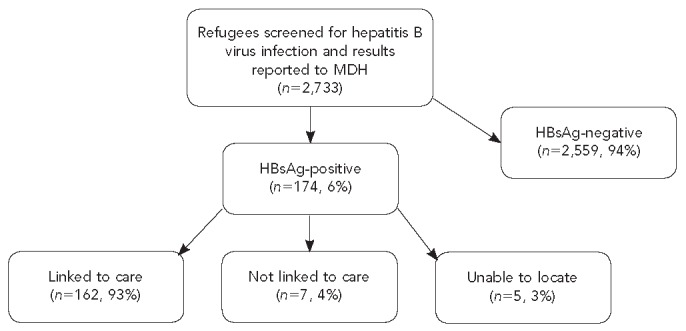
aThe HepTLC initiative promoted viral hepatitis B and hepatitis C screening, posttest counseling, and linkage to care at 34 U.S. sites.
MDH = Minnesota Department of Health
HBsAg = hepatitis B surface antigen
As indicated by a two-sample test of proportions, the one-year linkage-to-care rate for HepTLC initiative participants (93%) was significantly higher than the rate for HBsAg-positive refugees identified through refugee health screening in the previous year (64%) (p<0.001).
The number and percentage of HBsAg-positive refugees screened in Ramsey County who were linked to care was significantly higher in the year during the HepTLC initiative (124 of 130, 95%) than in the prior year (48 of 73, 66%) (p<0.001). The number and percentage of HBsAg-positive refugees screened in Hennepin County who were linked to care was also significantly higher in the year during the HepTLC initiative (40 of 44, 91%) than in the prior year (eight of 14, 57%) (p=0.003). Refugees participating in the HepTLC initiative were much more likely to receive follow-up care for hepatitis B within one year than refugees who did not receive this type of linkage-to-care assistance.
DISCUSSION
The bilingual care navigators were essential to the project's success. Their cultural knowledge and linguistic competence, along with their connections to public health resources, allowed them to address challenges ranging from refugees' fear and uncertainty to logistics. An appropriate referral was only the first step; refugees needed education and assistance to ensure that referrals resulted in scheduled and kept appointments. The navigators often had multiple contacts with participants to provide education, coordinate transportation, reschedule appointments, follow up, and offer support.
This intervention, which required a modest investment in hiring two undergraduate student care navigators and a graduate student to facilitate daily operations, could be adapted to any medical condition requiring health-care system navigation. It is important to note, however, that the HepTLC initiative in Minnesota was conducted in the context of a strong, multifaceted infrastructure: the MDH viral hepatitis surveillance and refugee health screening programs. Both programs rely on partnerships with local public health and private clinics. Clinics and providers demonstrated commitment and flexibility in their willingness to adapt their protocols to include HepTLC data form completion and patient referral to the MDH linkage-to-care team. Most participants in the HepTLC initiative received follow-up care from primary care providers chosen for their experience in refugee health and chronic HBV infection management. Moreover, HBV screening and care for refugees are covered by Minnesota's Medicaid program. The availability of affordable screening and care is critical to linkage-to-care endeavors.
Limitations
This study was subject to several limitations. The -HepTLC initiative took place in a major metropolitan area; linking people with chronic HBV infection to care in more rural areas may present different challenges. Also, linkage-to-care data were missing for a greater proportion of refugees from the year prior to the project, possibly introducing bias into our estimate of the difference in linkage-to-care rates. Individuals who could not be located might have been more transient and less likely to be linked to care. If they received follow-up care outside of Minnesota, however, it would not have been reported to MDH.
CONCLUSION
In the context of a strong refugee health screening and viral hepatitis surveillance infrastructure, a simple intervention improved the linkage-to-care rate among HBsAg-positive refugees in the Twin Cities. Bilingual, culturally aware staff members helped clients understand the importance of follow-up care and overcome barriers to accessing care. The success of the -HepTLC initiative demonstrated the importance of care navigators who are supported by an effective screening program and a coordinated system of data sharing. Successful linkage to care also depends on access to quality, affordable health care, which is essential to improving outcomes for people with chronic HBV infection in the United States.
Footnotes
The authors thank Claudia Miller, Paw Htoo, Abdirahman Kahiye, and Abdiwahab Shiil of the Minnesota Department of Health (MDH); Christine May and Dianne Finn of Hennepin County Public Health; Larisa Turin and Thomas Michels of -HealthPartners; Shana Sniffen, James Letts, and Kelley Jewett of HealthEast Roselawn Clinic; and David Delaney-Elsner of HealthEast Roseville Clinic.
Activities to link refugees in Minnesota's two largest counties to medical care for chronic hepatitis B virus infection were conducted as part of the Hepatitis Testing and Linkage to Care (HepTLC) initiative, funded in part by the Prevention and Public Health Fund established through the Affordable Care Act.
MDH was funded under Category A: Early Identification and Linkage to Care for Foreign-born Persons with Hepatitis B. Partners in the project included the MDH Refugee Health Program, MDH viral hepatitis surveillance, Hennepin County Public Health Clinic, St. Paul-Ramsey County Public Health, and private clinics that screened Ramsey County refugees.
The Centers for Disease Control and Prevention determined that activities related to the HepTLC initiative were not human subjects research. Other activities described in the article were conducted within the scope of routine viral hepatitis surveillance and refugee health activities at MDH.
REFERENCES
- 1.Liu SJ, Iqbal K, Shallow S, Speers S, Rizzo E, Gerard K, et al. Characterization of chronic hepatitis B cases among foreign-born persons in six population-based surveillance sites, United States 2001–2010. J Immigr Minor Health. 2014;17:7–12. doi: 10.1007/s10903-014-0012-0. [DOI] [PubMed] [Google Scholar]
- 2.Kowdley KV, Wang CC, Welch S, Roberts H, Brosgart CL. Prevalence of chronic hepatitis B among foreign-born persons living in the United States by country of origin. Hepatology. 2012;56:422–33. doi: 10.1002/hep.24804. [DOI] [PubMed] [Google Scholar]
- 3.Minnesota Department of Health. St. Paul (MN): Minnesota Department of Health; 2014. Viral hepatitis statistics. [Google Scholar]
- 4.Iloeje UH, Yang HI, Su J, Jen CL, You SL, Chen CJ, et al. Predicting cirrhosis risk based on the level of circulating hepatitis B viral load. Gastroenterology. 2006;130:678–86. doi: 10.1053/j.gastro.2005.11.016. [DOI] [PubMed] [Google Scholar]
- 5.Perz JF, Armstrong GL, Farrington LA, Hutin YJ, Bell BP. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. J Hepatol. 2006;45:529–38. doi: 10.1016/j.jhep.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 6.Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology. 2009;50:661–2. doi: 10.1002/hep.23190. [DOI] [PubMed] [Google Scholar]
- 7.Museru OI, Vargas M, Kinyua M, Alexander KT, Franco-Paredes C, Oladele A. Hepatitis B virus infection among refugees resettled in the U.S.: high prevalence and challenges in access to health care. J Immigr Minor Health. 2010;12:823–7. doi: 10.1007/s10903-010-9335-7. [DOI] [PubMed] [Google Scholar]
- 8.Minnesota Department of Health. St. Paul (MN): Minnesota Department of Health; 2014. Refugee health statistics. Also available from: http://www.health.state.mn.us/divs/idepc/refugee/stats/index.html [cited 2014 Dec 1] [Google Scholar]
- 9.Minnesota State Demographic Center. St. Paul (MN): Minnesota State Demographic Center; 2014. Population estimates. Also available from: http://mn.gov/admin/demography/data-by-topic/population-data/our-estimates [cited 2014 Dec 1] [Google Scholar]
- 10.Centers for Disease Control and Prevention (US) Atlanta: CDC; 2014. Guidelines for the U.S. domestic medical examination for newly arriving refugees. Also available from: http://www.cdc.gov/immigrantrefugeehealth/guidelines/domestic/domestic-guidelines.html [cited 2014 Dec 1] [Google Scholar]
- 11.Luther Consulting, LLC. Carmel (IN): Luther Consulting, LLC; 2013. EvaluationWeb®: Version 5. [Google Scholar]
- 12.StataCorp. College Station (TX): StataCorp; 2013. Stata®: Release 13. [Google Scholar]


