Abstract
Objective
Without medical intervention, about one-quarter of the 1.4–2.2 million Americans chronically infected with the hepatitis B virus (HBV) will die of HBV-associated conditions, including liver failure and hepatocellular carcinoma. We report on a program in Sacramento County, California, that offered HBV screening to at-risk adults, referred infected individuals to care, and vaccinated uninfected adults who were susceptible to HBV infection (i.e., individuals who tested negative for hepatitis B surface antigen and who were never vaccinated against HBV).
Methods
We engaged organizations linked to Chinese, Hmong, Korean, and Vietnamese communities to cosponsor HBV screenings of Asian Americans as part of the Hepatitis Testing and Linkage to Care initiative, which promoted viral hepatitis B and hepatitis C screening, posttest counseling, and linkage to care at 34 U.S. sites. We held 28 hepatitis B community screening events throughout Sacramento County, California, in collaboration with these groups from September 2012 to September 2013.
Results
We screened 1,004 Asian American adults (i.e., 283 Koreans, 242 Chinese, 233 Vietnamese, 223 Hmong, and 23 people from other Asian communities) for HBV, of whom 98% were foreign born and 87% had a language preference other than English. Of the 76 participants who tested positive for HBV (31 Hmong, 23 Vietnamese, 17 Chinese, two Koreans, and three from other Asian communities), we provided posttest counseling to 51 participants.
Conclusion
By collaborating with community groups and addressing barriers to screening, we highlighted the importance of disaggregating chronic HBV infection rates by Asian ethnicity and sex vs. aggregated Asian American rates. Future HBV screening initiatives should target Hmong and Vietnamese men.
Globally, hepatitis B virus (HBV) infection is the primary cause of cancer after tobacco use.1 Currently, an estimated two billion people (i.e., one in three of the world's population) have been infected with HBV during their lifetime, making it one of the most common and serious infections in the world.2 Of the two billion people worldwide ever infected with HBV, 400 million are chronically infected with HBV and, in the absence of intervention, an estimated 15%–25% of people with chronic infection will die of HBV-associated complications, including cirrhosis and hepatocellular carcinoma.3 Although the overall prevalence of chronic HBV infection in the United States is low (i.e., <1%), the number of HBV-infected people has risen in recent years because of an increasing number of immigrants from HBV-endemic areas (defined as hepatitis B surface antigen [HBsAg] prevalence ≥2%), including parts of East and Southeast Asia, the Pacific Islands, and Africa.4 The disproportionately elevated prevalence of chronic HBV in people from these countries is associated with substantial health disparities.2,5 For example, among U.S. populations, Asian Americans/Pacific Islanders have the highest rates of liver cancer (up to 7.2 times higher than non-Hispanic white people),6 with rates expected to increase in the coming years because this population has experienced the highest percentage increase in population growth for every decade since 1970.7
As part of the Hepatitis Testing and Linkage to Care (HepTLC) initiative, which promoted viral hepatitis B and hepatitis C screening, posttest counseling, and linkage to care at 34 U.S. sites, the University of California, Davis (UC Davis) received funding for HBV testing of foreign-born people in Sacramento, California, from September 2012 to September 2013. The program's two goals were to (1) test at least 1,000 foreign-born adult Asian Americans who had not been previously serologically tested for HBV and (2) counsel at least 90% of the people testing positive for HBsAg. We report our findings and discuss the importance of testing this population for HBV.
METHODS
The HepTLC initiative targeted foreign-born people from HBV-endemic countries; eligibility was limited to programs serving populations in the 50 geographic areas with the highest number of foreign-born people from Asia and Africa, as documented in the 2006–2010 American Community Survey.8
In Sacramento County, the majority of foreign-born people originating from HBV-endemic countries are from East Asia (e.g., China and Korea) and Southeast Asia (e.g., Vietnam and Laos). Our program focused on four Asian American ethnic populations—Chinese, Hmong, Korean, and Vietnamese—because their countries of origin have intermediate-to-high HBV endemicity and because they are the largest Asian American groups residing in the county.
To reach the Chinese community, we collaborated with the UC Davis-sponsored, student-run Paul Hom Asian Clinic, which serves predominantly Chinese people, to organize and host HBV screening events. We reviewed patient medical records to identify and call patients who had not been previously screened. Paul Hom Asian Clinic staff member and volunteers also promoted the HBV screening events during clinic hours, at community events, and at health fairs.
To reach the Hmong community, we partnered with the Hmong Women's Heritage Association in Sacramento, a community-based organization serving the Hmong population with whom we have collaborated since 2003. Our joint accomplishments have included offering navigation services (i.e., transportation, translation, scheduling, and attending examinations) for Papanicolau testing for Hmong women with limited English proficiency9 and demonstrating the effectiveness of Hmong bilingual lay health workers in increasing HBV screening compared with control conditions in a randomized, controlled community study.10
To reach the Korean community, we recruited a Korean community leader who is a pharmacist specializing in oncology and is familiar with the program's importance. The pharmacist also convened the Shalom Korean cancer support group that worked with Korean churches to host screening events.
To reach the Vietnamese community, we worked with another UC Davis-sponsored, student-run medical clinic, the Vietnamese Cancer Awareness Research and Education Society, and a student club from a local pharmacy school (i.e., the California Northstate University-Cancer Awareness Research and Education Society). Similar to the Paul Hom Asian Clinic, we also identified and recruited Vietnamese Cancer Awareness Research and Education Society patients by reviewing all patient medical records. The two student organizations promoted screenings through community events, by posting flyers in the community, and by advertising in the local Vietnamese newspapers.
Our community partners provided translation support for all aspects of the program, from consent for HBV testing to explaining test results to participants. Screenings were held in convenient venues that were familiar to each ethnic group (e.g., Paul Hom Asian Clinic, Vietnamese Cancer Awareness Research and Education Society, Hmong Women's Heritage -Association office, or Korean churches). Transportation to and from the screening event was offered to those who could not travel to these locations.
From September 2012 to September 2013, we held 28 community hepatitis B screening events throughout Sacramento County with the aforementioned institutions. We used linguistically specific and culturally appropriate project materials for Hmong, Korean, and Vietnamese based on previously developed materials. The Chinese-language materials were based on materials from the San Francisco Hep B Free initiative, a grassroots community coalition to prevent hepatitis B and liver cancer.11 UC Davis Translation Services translated all educational materials into the four languages of our target populations, and our respective partners verified their correctness and cultural appropriateness. Materials included a consent form, an eligibility form, an intake form, advertising material (e.g., flyers, radio announcement scripts, and telephone recruitment scripts), and a participant test result letter. Our partners provided feedback on developed materials and in-language translation during screening events and counseling sessions. Participants received three hepatitis B serologic tests: HBsAg, hepatitis B surface antibody (anti-HBs), and hepatitis B core antibody (anti-HBc).
Eligibility
Those eligible for HBV screening had to be (1) a resident of Sacramento County, (2) ≥18 years of age, (3) self-reported as never having been serologically tested for hepatitis B, and (4) born in or had a parent born in an HBV-endemic country.4 Participants completed a brief questionnaire with their sociodemographic characteristics (e.g., age, sex, Asian ethnicity). Participants provided contact information so they could receive their test results. All laboratory tests were conducted at the UC Davis Medical Center Clinical Laboratory.
Follow-up
Once the research manager received the laboratory test results, the medical director characterized the test result pattern into one of the following categories:12
Susceptible: HBsAg negative, anti-HBc negative, and anti-HBs negative
Immune because of natural infection: HBsAg negative, anti-HBc positive, and anti-HBs positive
Immune because of HBV vaccine: HBsAg negative, anti-HBc negative, and anti-HBs positive
Chronically infected: HBsAg positive, anti-HBc positive, and anti-HBs negative
Interpretation unclear: HBsAg negative, anti-HBc positive, and anti-HBs negative (Note: This serological pattern may occur in the presence of (1) resolved infection, (2) false-positive anti-HBc, (3) low-level chronic infection, and (4) resolving acute infection.)
All participants received an in-language telephone call and a mailed letter detailing their test results based on the aforementioned categories. Participants who tested positive for HBsAg were given appointment times and scheduled to attend a screening event to receive additional tests, including hepatic function panel (i.e., total bilirubin, bilirubin direct, alkaline phosphatase, aspartate aminotransferase, alanine transaminase, albuminand total protein), hepatitis B e-antigen, and hepatitis B viral load. After additional tests were processed, participants were scheduled for a counseling session with our medical director, who explained the test results with the participant and counseled them on next steps.
RESULTS
We screened 1,004 Asian Americans (i.e., 283 Koreans, 242 Chinese, 233 Vietnamese, 223 Hmong, and 23 people from other Asian communities), meeting the screening goal of 1,000 tests. Nearly all (98%) of the participants were foreign born and 87% had a language preference other than English. Of the 1,004 people screened, 76 (7.6%) tested HBsAg positive (Table 1). Of the 76 participants who tested HBsAg positive, 51 (67.1%) were counseled (46 by the medical director and five by their primary care physician). The 25 participants not counseled on their results were lost to follow-up because of a wrong telephone number, a phone disconnection, not picking up after three attempts, no show, and/or declined counseling. All 46 participants who were counseled by the medical director received follow-up testing during their counseling session (Table 2).
Table 1.
Number of participants susceptible to, immune to, and confirmed with HBV infection, by Asian American ethnicity and sex, in the Hepatitis Testing and Linkage to Care (HepTLC) initiative, Sacramento County, California, September 2012–September 2013a
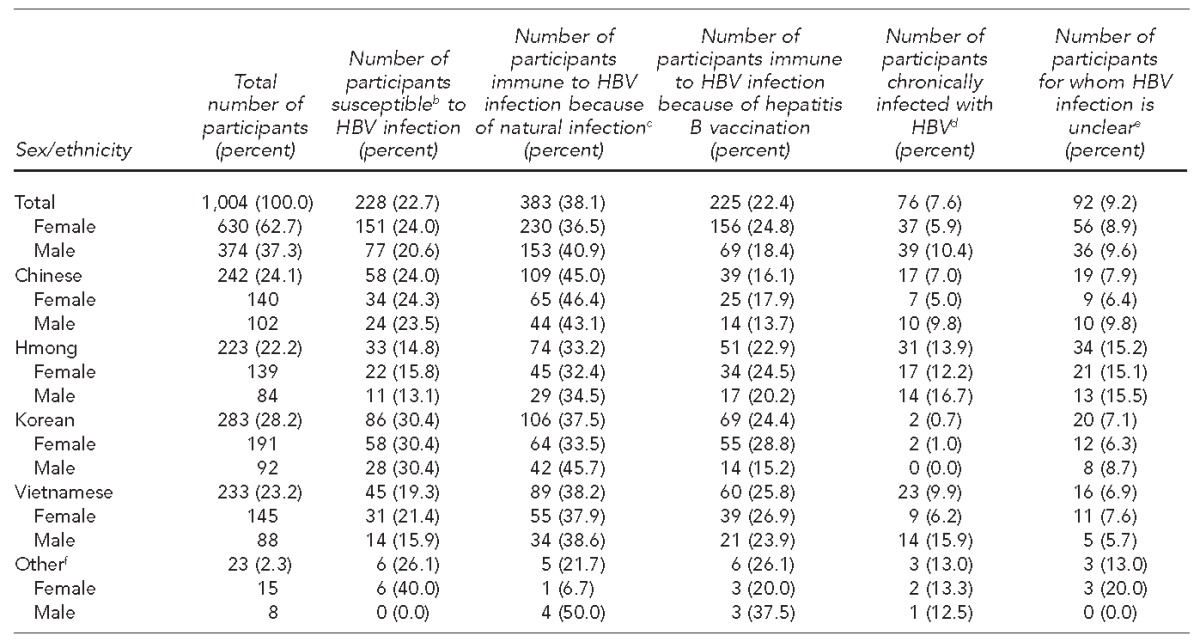
The HepTLC initiative promoted viral hepatitis B and hepatitis C screening, posttest counseling, and linkage to care at 34 U.S. sites, including nine programs that provided hepatitis B virus testing.
bIndividuals who are susceptible have the following test results: HBsAg negative, anti-HBc negative, and anti-HBs negative.
cIndividuals who are immune because of natural infection have the following test results: HBsAg negative, anti-HBc positive, and anti-HBs positive.
dIncludes participants who were HBsAg positive and did not have results available for the other markers.
eIndividuals for whom HBV infection is unclear having the following test results: HBsAg negative, anti-HBc positive, and anti-HBs negative (Note: This serological pattern may occur in the presence of resolved infection, false-positive anti-HBc, low-level chronic infection, and resolving acute infection).
fOther defined as Cambodian, Mien, Mongolian, and Chinese/Vietnamese
HBV = hepatitis B virus
HBsAg = hepatitis B surface antigen
anti-HBc = hepatitis B core antibody
anti-HBs = hepatitis B surface antibody
Table 2.
Participation in the care cascade, by Asian American ethnicity, for participants screened for HBV during the Hepatitis Testing and Linkage to Care (HepTLC) initiative, Sacramento County, California, September 2012–September 2013a
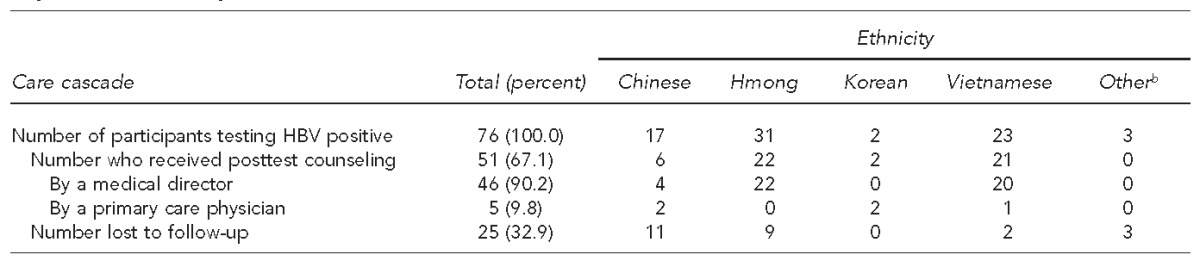
The HepTLC initiative promoted viral hepatitis B and hepatitis C screening, posttest counseling, and linkage to care at 34 U.S. sites, including nine program for hepatitis B virus testing.
bOther defined as Cambodian, Mien, Mongolian, and Chinese/Vietnamese
HBV = hepatitis B virus
When the findings were disaggregated by ethnicity, the Hmong population experienced the highest rate of infection (11.2%); when disaggregated by sex, men from the Hmong (14.3%) and Vietnamese (13.6%) communities experienced the highest rates of chronic hepatitis B infection. Participants whose test results indicated a susceptibility to HBV infection were counseled to receive an HBV vaccination and were either referred to their primary care provider or to UC Davis free of charge. Twenty-nine participants qualified for the free vaccine; of those, 21 completed the three-shot series.
DISCUSSION
This screening effort was the largest to date in Sacramento, a city with the 10th-largest Asian population in the United States.7 The screening program identified many previously undetected HBsAg-positive people who were referred for further evaluation and care. The overall prevalence of HBsAg-positive participants was 7.6%, which was similar to prevalences reported by three other programs funded through the HepTLC initiative.13 People with a primary care provider were referred to their own providers, while those without a primary care provider were referred to the Paul Hom Asian Clinic, which offers indigent care staffed by interpreters who are fluent in Asian languages.
We counseled 67.1% of those who were chronically infected, which, although short of our goal (90%), was respectable considering that this population moves around frequently. We were unable to document appropriate medical management of those determined to be HBsAg positive because the project period was only for one year and because resources were limited. However, most of the HBsAg-positive participants were patients of our student-run medical clinics; as such, a copy of their test results has been included in their medical records.
Limitations and strengths
This study was subject to several limitations. The program was cross-sectional in design and based on a convenience sample of participants who consented to testing through outreach efforts. More women than men were screened, as is the tendency for most HBV screening interventions involving Asian Americans, because Asian women are generally more interested in their health than Asian men.14 As such, our findings were not representative of the Asian American population of Sacramento County.
This study also had several strengths. Familiar locations where screening occurred, available transportation, translating materials into relevant Asian languages (e.g., Cantonese, Mandarin, Hmong, Korean, and Vietnamese), and offering translation services to explain test results were indispensable to participation and satisfaction. By collaborating with community partners, we also minimized cultural barriers.
CONCLUSION
This program exemplified how community partners can work together to address linguistic, cultural, and transportation barriers among an Asian population to implement a successful HBV screening initiative. The findings support the need for disaggregated data by Asian American ethnic populations vs. by aggregated Asian American health data. Disaggregation of chronic HBV infection rates by Asian ethnicity and sex are important to provide a more precise picture of the need for targeted and tailored screening programs. Because of the higher number of Hmong and Vietnamese men identified with chronic HBV infection compared with other Asian groups, we are targeting them for future screening efforts.
Footnotes
The authors thank Tina Fung, MPH; Duong Ton; and the community leaders and partnering organizations, without whom this program could not have been conducted. Community leaders and their respective organizations included Aeyon Lee, Shalom Korean Cancer Support Group; Kendra Thao and Youa Lo, Hmong Women's Heritage Association; Ruth Vinall, PhD, and the California Northstate University Cancer Awareness, Research, and Training student organization; and Sherri Paul and Daniel Brent, University of California, Davis (UC Davis) Health System, Department of Pathology and Laboratory Medicine. Physicians who participated in this program included Ronald Jan, MD, Paul Hom Asian Free Clinic, and MaryPat Pauly, MD, Kaiser Permanente.
The UC Davis Institutional Review Board approved the protocol for participation. Bilingual program staff members obtained written consent from participants during screening events. This program was funded in part through U51PS0039441-01, P30CA093373 (UC Davis Comprehensive Cancer Center), and U54CA153499 (Asian American Network for Cancer Awareness, Research, and Training). The views in this article are those of the authors and do not necessarily reflect the views of the funding agencies.
REFERENCES
- 1.Kuper H, Adami HO, Trichopoulos D. Infections as a major preventable cause of human cancer. J Intern Med. 2000;248:171–83. doi: 10.1046/j.1365-2796.2000.00742.x. [DOI] [PubMed] [Google Scholar]
- 2.Custer B, Sullivan SD, Hazlet T, Iloeje U, Veenstra D, Kowdley K. Global epidemiology of hepatitis B virus. J Clin Gastroenterol. 2004;38(Suppl 3):S158–68. doi: 10.1097/00004836-200411003-00008. [DOI] [PubMed] [Google Scholar]
- 3.Mitchell T, Armstrong GL, Hu DJ, Wasley A, Painter JA. The increasing burden of imported chronic hepatitis B—United States, 1974–2008. PLoS One. 2011;6:e27717. doi: 10.1371/journal.pone.0027717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weinbaum CM, Williams I, Mast EE, Wang SA, Finelli L, Wasley A, et al. Recommendations for identification and public health management of persons with chronic hepatitis B virus infection. MMWR Recomm Rep. 2008;19(RR-8):1–20. [PubMed] [Google Scholar]
- 5.Kowdley KV, Wang CC, Welch S, Roberts H, Brosgart CL. Prevalence of chronic hepatitis B among foreign-born persons living in the United States by country of origin. Hepatology. 2012;56:422–33. doi: 10.1002/hep.24804. [DOI] [PubMed] [Google Scholar]
- 6.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5–29. doi: 10.3322/caac.21254. [DOI] [PubMed] [Google Scholar]
- 7.Census Bureau (US) The Asian population: 2010 [cited 2016 Feb 2] Available from: https://www.census.gov/prod/cen2010/briefs/c2010br-11.pdf.
- 8.Census Bureau (US) American Community Survey 2006–2010 [cited 2016 Feb 3] Available from: www.census.gov/programs-surveys/acs.
- 9.Fang DM, Lee S, Stewart S, Ly MY, Chen MS., Jr Factors associated with pap testing among Hmong women. J Health Care Poor Underserved. 2010;21:839–50. doi: 10.1353/hpu.0.0338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen MS, Jr, Fang DM, Stewart SL, Ly MY, Lee S, Dang JH, et al. Increasing hepatitis B screening for Hmong adults: results from a randomized controlled community-based study. Cancer Epidemiol Biomarkers Prev. 2013;22:782–91. doi: 10.1158/1055-9965.EPI-12-1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bailey MB, Shiau R, Fernyak Se, Fang T, SK, Chang ET. San Francisco Hep B Free: a grassroots community coalition to prevent hepatitis B and liver cancer. J Community Health. 2011;36:538–51. doi: 10.1007/s10900-010-9339-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention (US) Interpretation of hepatitis B serologic test results [cited 2015 Dec 30] Available from: http://www.cdc.gov/hepatitis/hbv/pdfs/serologicchartv8.pdf.
- 13.Beckett GA, Ramirez G, Vanderhoff A, Nichols K, Chute SM, Wyles DL, et al. Early identification and linkage to care of persons with chronic hepatitis B virus infection—three U.S. sites, 2012–2014. MMWR Morb Mortal Wkly Rep. 2014;63(18):399–401. [PMC free article] [PubMed] [Google Scholar]
- 14.Maxwell AE, Bastani R, Glenn BA, Taylor VM, Nguyen TT, Stewart SL, et al. Developing theoretically based and culturally appropriate interventions to promote hepatitis B testing in four Asian American populations, 2006–2011. Prev Chronic Dis. 2014;11:e72. doi: 10.5888/pcd11.130245. [DOI] [PMC free article] [PubMed] [Google Scholar]


