Abstract
AIM
To analyze the effect of steep meridian small incision phacoemulsification cataract surgery on anterior, posterior and total corneal wavefront aberration.
METHODS
Steep meridian small incision phacoemulsification cataract surgery was performed in age-related cataract patients which were divided into three groups according to the incision site: 12 o'clock, 9 o'clock and between 9 and 12 o'clock (BENT) incision groups. The preoperative and 3-month postoperative root mean square (RMS) values of anterior, posterior and total corneal wavefront aberration including coma, spherical aberration, and total higher-order aberrations (HOAs), were measured by Pentacam scheimpflug imaging. The mean preoperative and postoperative corneal wavefront aberrations were documented.
RESULTS
Total corneal aberration and total lower-order aberrations decreased significantly in three groups after operation. RMS value of total HOAs decreased significantly postoperatively in the 12 o'clock incision group (P<0.001). Corneal spherical aberration was statistically significantly lower after steep meridian small incision phacoemulsification cataract surgery in BENT incision group (P<0.05) and Pearson correlation analysis indicated that spherical aberration changes had no significant relationship with total astigmatism changes in all three corneal incision location.
CONCLUSION
Corneal incision of phacoemulsification cataract surgery can affect corneal wavefront aberration. The 12 o'clock corneal incision eliminated more HOAs and the spherical aberrations decreased in BENT incision group obviously when we selected steep meridian small incision. Cataract lens replacement using wavefront-corrected intraocular lens combined with optimized corneal incision site would improve ocular aberration results.
Keywords: cataract surgery, corneal aberration, corneal incision
INTRODUCTION
Ocular wavefront and topographic wavefront measure the error in the optical system of the entire eye and the cornea[1]. Higher order wavefront aberrations blur the retinal image, reducing contrast sensitivity and visual acuity in a way that cannot be corrected by simple spherical and cylindrical correction[2]. Spherical aberration (SA) and coma are the higher-order aberrations (HOAs) that contribute mostly to visual disturbances and dissatisfaction in patients after refractive surgery[3]–[4]. With the advent of the clinical aberrometer, measurement of various corneal and total ocular aberrations has become possible. The ability to correct HOAs is expected to improve the visual function of patients[5].
Due to the advances in phacoemulsification technology, modern cataract surgery provides an opportunity to achieve the level of visual outcomes previously only possible through ocular refractive procedures. The size of corneal incision has also become smaller, to minimize the alteration of corneal architecture associated with cataract surgery. However, it was found that small incision phacoemulsification cataract surgery also induced significant trefoil, a third-order Zernike aberration[6]–[7]. In addition, a later study found that phacoemulsification cataract surgery caused significant changes in vertical tetrafoil, a 4th-order Zernike aberration[8]. Although the exact clinical relevance of these HOAs is yet fully understood, studies have used wavefront analysis to compare the influence of incision size (i.e. micro versus small incision size) on corneal optical quality and the results were mixed[9]–[10]. Furthermore, all of studies only measured the corneal aberration of the anterior surface, and failed to consider the effect of incision site. The posterior corneal surface compensates approximately 3.5% of the coma of the anterior surface[11].
We hence conducted this prospective study to investigate the relationships between total and high-order corneal wavefront aberrations (coma, SA, and other HOAs) and three different corneal incision sites in steep meridian small incision phacoemulsification cataract surgery, in an attempt to optimize incision site and reduce corneal aberrations clinically.
SUBJECTS AND METHODS
This prospective clinical study was conducted at the Eye Hospital of China Medical University, Shenyang, China. Informed consent was obtained from all patients enrolled and the tenets of the Declaration of Helsinki were followed for all study procedures. Patients with a history of ocular diseases and intraocular or corneal surgery, or with systemic diseases such as diabetes, were excluded. All patients enrolled had a corneal astigmatism of less than 1.5 diopters and nuclear hardness of grade III according to Emery grading system. Patients who had complications during or after surgery were later excluded. A total of 144 eyes completed the study. All eyes received steep meridian small incision phacoemulsification cataract surgery through a 2.8 mm clear corneal incision placed at exactly 12 o'clock, 9 o'clock and between 9 and 12 o'clock (BENT) positions. Incision location was chosen based in pre-existing corneal cylinder, the 12 o'clock incision group included patients with steep corneal curvature between 70 and 110 degree meridians; the 9 o'clock group between 160 and 200 meridians of right eye; BENT group between 115 and 155 meridians. All tests were performed within 2d before surgery, and 3mo after surgery by an ophthalmologist other than the surgeon who performed all the surgeries.
Surgical Procedure
One experienced surgeon (Zhang JS) performed all cataract surgeries using topical anesthesia. In all cases, the phacoemulsification was performed using right hand through a 2.8 mm clear corneal incision, with a 1.0 mm paracentesis site 3 o'clock hours away at the left hand. A 5.5-6.0 mm capsulorhexis was created after the anterior chamber was filled with an ophthalmic viscosurgical device (OVD). Infiniti system (Alcon, USA) was used and foldable one piece intraocular lens (IOL) (Alcon, USA) implanted using an IOL injector in all cases. All the incisions were closed by stromal hydration without sutures. After surgery, a standard topical antibiotic and steroid regimen was prescribed.
Pentacam Scheimpflug Imaging
Corneal tomography was performed preoperatively and postoperatively using a Pentacam HR anterior segment tomography system (Oculus GmbH, Wetzlar, Germany). Lower and HOAs were extracted and compared among the 3 incision sites. In particular, the following parameters of the cornea were assessed, refraction error, vertical and horizontal coma (Z3−1 and Z31), trefoil (Z3−3 and Z33), SA (Z40), second astigmatism (Z4−4 and Z44) and root mean square (RMS) error of the total aberration, and the total lower-order aberration (tLOA) and total higher-order aberration (tHOA). The same measurement procedure was used in all cases. For each eye, the mean of 3 measurements at a 6.0 mm diameter central area with respect to the pupil center was calculated and used as the final estimate of the aberration measurements.
Statistical Analysis
An t-test was used to compare the preoperative and postoperative mean corneal Zernike aberrations and RMS of the corneal wavefront aberrations in the 3 groups. Pearson correlation analysis was conduct and all these analyses were performed using SPSS software (version 12.0, SPSS, Inc.). A P value of less than 0.05 was considered statistically significant for individual Zernike aberrations.
RESULTS
Steep meridian small incision phacoemulsification cataract surgery was performed in 144 eyes. Table 1 shows the patients' baseline data. There was no significant difference between the 3 groups in preoperative age, corneal astigmatism, or cornea power. No eyes had surgical complications.
Table 1. Demographics of all studied groups according to age, gender, and corneal power.
| Incision site group | 12 o'clock incision group | 9 o'clock clear corneal incisions | BENT incision group |
| Gender | |||
| Female | 25 (52.1) | 22 (47.8) | 25 (50.0) |
| Male | 23 (47.9) | 24 (52.2) | 25 (50.0) |
| Age (a) | 63.3±5.6 | 65.8±6.0 | 64.9±5.2 |
| Eye | |||
| Right | 26 (54.2) | 46 (100.0) | 25 (50.0) |
| Left | 22 (45.8) | 25 (50.0) | |
| Corneal astigmatism (D) | 1.11±0.45 | 1.19±0.31 | 1.08±0.47 |
| Corneal power (D) | 44.61±3.09 | 43.62±2.42 | 44.29±3.46 |
n (%)
Total Preoperative and Postoperative Corneal Aberrations
Table 2 shows the mean preoperative and postoperative corneal aberrations over a 6.0 mm area centered on the pupil center for Zernike terms from the 2nd to 4th order. The Zernike terms of 5th and 6th order are not shown because they were small in magnitude. Table 2 also contains the RMS values for total corneal wavefront aberrations from the 2nd to 6th order and tHOA RMS values from the 3rd to 6th order. Total corneal aberration and tLOA decreased significantly in three groups after operation. tHOA increased after operation in BENT and 9 o'clock groups without statistical significance, but significantly decreased in the 12 o'clock incision group (P<0.001). Trefoil and coma were stable in all three groups before and after the operation (P>0.05). Secondary astigmatisms were stable after operation in BENT and 9 o'clock incision groups but not in the 12 o'clock incision group. Tetrafoil aberrations increased significantly after operation in the 12 o'clock and 9 o'clock incision groups (P<0.001), but kept stable in the BENT incision group (Table 2). Pearson correlation analysis results indicated that trefoil, tetrafoil, secondary astigmatisms and coma changes between pre and post-operation had no relationship with total astigmatism in all three groups.
Table 2. Mean preoperative and postoperative RMS values and Zernike aberrations (µm) in the total cornea over a 6.0 mm diameter central area in 3 groups.
| Parameters | 12 o'clock incision group |
9 o'clock clear corneal incisions |
BENT incision group |
||||||
| Preop. | Postop. | P | Preop. | Postop. | P | Preop. | Postop. | P | |
| Total RMS | 2.212±0.877 | 1.956±0.939 | 0.219 | 2.640±0.918 | 2.424±1.065 | 0.284 | 2.123±0.844 | 1.945±0.690 | 0.165 |
| tLOA | 2.152±0.868 | 1.868±0.955 | 0.267 | 2.540±0.900 | 2.263±1.052 | 0.167 | 2.023±0.823 | 1.825±0.688 | 0.100 |
| tHOA | 0.723±0.371 | 0.483±0.177 | 0.000 | 0.697±0.258 | 0.758±0.315 | 0.175 | 0.612±0.283 | 0.642±0.210 | 0.639 |
| Z (3, -3) | -0.019±0.101 | 0.026±0.150 | 0.214 | -0.025±0.109 | -0.077±0.242 | 0.142 | -0.009±0.256 | -0.055±0.164 | 0.398 |
| Z (3, -1) | -0. 000±0.254 | -0.086±0.236 | 0.214 | 0.168±0.230 | 0.190±0.327 | 0.637 | 0.186±0.242 | 0.092±0.247 | 0.010 |
| Z (3,1) | 0.029±0.192 | 0.025±0.174 | 0.936 | 0.103±0.239 | 0.129±0.218 | 0.445 | 0.084±0.156 | 0.138±0.177 | 0.057 |
| Z (3,3) | -0.008±0.067 | -0.030±0.100 | 0.084 | 0.010±0.121 | 0.044±0.164 | 0.249 | -0.013±0.089 | 0.005±0.165 | 0.550 |
| Z(4, -4) | 0.001±0.083 | -0.079±0.269 | 0.159 | 0.010±0.151 | -0.070±0.253 | 0.116 | 0.063±0.216 | -0.027±0.211 | 0.129 |
| Z (4, -2) | -0.020±0.080 | 0.027±0.082 | 0.056 | 0.009±0.090 | 0.028±0.097 | 0.315 | 0.000±0.083 | 0.048±0.111 | 0.062 |
| Z (4, 0) | 0.251±0.139 | 0.239±0.143 | 0.730 | 0.371±0.149 | 0.328±0.154 | 0.111 | 0.334±0.127 | 0.243±0.092 | 0.000 |
| Z (4, 2) | -0.018±0.087 | 0.023±0.112 | 0.035 | -0.039±0.150 | -0.078±0.123 | 0.229 | -0.045±0.104 | -0.058±0.113 | 0.466 |
| Z (4,4) | -0.056±0.105 | -0.277±0.247 | 0.000 | -0.006±0.242 | -0.209±0.256 | 0.000 | -0.048±0.121 | 0.051±0.168 | 0.024 |
| Coma | 0.047±0.307 | -0.031±0.260 | 0.019 | 0.187±0.587 | 0.199±0.777 | 0.841 | 0.270±0.287 | 0.230±0.290 | 0.316 |
| Trefoil | -0.006±0.131 | -0.083±0.489 | 0.321 | 0.005±0.200 | -0.017±0.279 | 0.638 | -0.022±0.239 | -0.050±0.272 | 0.661 |
| Tetrafoil | -0.057±0.125 | -0.358±0.302 | 0.000 | 0.016±0.285 | -0.267±0.373 | 0.000 | 0.018±0.282 | 0.024±0.287 | 0.939 |
| Secondary astigmatism | -0.035±0.117 | 0.048±0.128 | 0.004 | -0.032±0.175 | -0.052±0.166 | 0.579 | -0.042±0.133 | -0.010±0.147 | 0.264 |
RMS: Root mean square; tLOA: Total low order aberration; tHOA: Total high order aberration; Z: Zernik; Coma: Z3−1 and Z31; Trefoil: Z3−3 and Z33; Tetrafoil: Z4−4 and Z44; Secondary astigmatism: Z4−2 and Z42. The terms of coma, trefoil, tetrafoli and secondary astigmatism indicate the RMS values of the 2 Zernike aberration, P<0.05; P<0.01; P<0.001.
Changes of Anterior Surface Corneal Aberrations in Three Groups
Table 3 shows the mean preoperative and postoperative aberrations of anterior cornea over a 6.0 mm area centered on the pupil center for Zernike terms from the 2nd to 4th order, the total RMS values from the 2nd to 6th order, and tHOA RMS values from the 3rd to 6th order. Comparing pre- and post-operative total anterior corneal aberrations and tLOA aberrations, no statistical significance was found in all three groups. High-order aberrations increased after operation in BENT and 9 o'clock incision groups, but decreased in 12 o'clock group with statistical significance (P<0.01). Coma, trefoil and secondary oblique astigmatism were stable after operation in all three groups. But in the 12 o'clock incision group, tetrafoil aberration increased after operation with statistical significance (P<0.01) (Table 3). Pearson correlation analysis showed same results that trefoil, tetrafoil, secondary astigmatisms and coma changes of anterior corneal surface between pre and post-operation had no relationship with total astigmatism in all three groups.
Table 3. Mean preoperative and postoperative RMS values and Zernike aberrations (µm) in the anterior corneal surface over a 6.0 mm diameter central area in 3 groups.
| Parameters | 12 o'clock incision group |
9 o'clock clear corneal incisions |
BENT incision group |
||||||
| Preop. | Postop. | P | Preop. | Postop. | P | Preop. | Postop. | P | |
| Total RMS | 2.153±0.840 | 2.074±0.907 | 0.493 | 2.486±1.425 | 2.545±1.717 | 0.625 | 1.999±0.815 | 1.941±0.736 | 0.589 |
| tLOA | 2.007±0.829 | 2.003±0.920 | 0.966 | 2.395±1.389 | 2.398±1.680 | 0.982 | 1.912±0.794 | 1.826±0.739 | 0.406 |
| tHOA | 0.699±0.328 | 0.499±0.179 | 0.001 | 0.610±0.421 | 0.806±0.451 | 0.002 | 0.560±0.247 | 0.635±0.169 | 0.115 |
| Z (3, -3) | -0.020±0.106 | 0.063±0.333 | 0.462 | -0.0001±0.090 | -0.064±0.225 | 0.065 | -0.077±0.207 | -0.056±0.172 | 0.646 |
| Z (3, -1) | -0. 015±0.247 | -0.001±0.256 | 0.617 | 0.093±0.314 | 0.109±0.428 | 0.691 | 0.145±0.220 | 0.138±0.232 | 0.791 |
| Z (3, 1) | 0.097±0.193 | 0.078±0.177 | 0.300 | -0.003±0.305 | 0.005±0.331 | 0.736 | 0.070±0.128 | 0.093±0.152 | 0.305 |
| Z (3,3) | -0.012±0.063 | -0.037±0.177 | 0.130 | 0.020±0.104 | 0.045±0.159 | 0.318 | 0.006±0.068 | 0.016±0.146 | 0.730 |
| Z (4, -4) | 0.007±0.116 | -0.101±0.216 | 0.026 | -0.005±0.113 | -0.026±0.248 | 0.638 | 0.273±0.179 | 0.048±0.182 | 0.139 |
| Z (4, -2) | -0.010±0.067 | 0.016±0.069 | 0.025 | 0.007±0.070 | 0.017±0.106 | 0.552 | 0.016±0.078 | 0.029±0.080 | 0.514 |
| Z (4, 0) | 0.277±0.142 | 0.278±0.141 | 0.875 | 0.408±0.249 | 0.374±0.211 | 0.146 | 0.328±0.116 | 0.294±0.094 | 0.024 |
| Z (4, 2) | -0.005±0.089 | -0.007±0.110 | 0.871 | -0.026±0.103 | -0.044±0.113 | 0.505 | -0.050±0.095 | -0.059±0.098 | 0.558 |
| Z (4,4) | -0.011±0.069 | -0.170±0.255 | 0.003 | -0.007±0.133 | -0.194±0.197 | 0.000 | 0.011±0.149 | 0.037±0.223 | 0.553 |
| Coma | 0.111±0.303 | 0.079±0.315 | 0.291 | 0.090±0.511 | 0.030±0.082 | 0.493 | 0.216±0.252 | 0.231±0.251 | 0.638 |
| Trefoil | -0.008±0.131 | -0.100±0.479 | 0.254 | 0.019±0.127 | 0.019±0.046 | 0.992 | -0.072±0.226 | -0.040±0.240 | 0.585 |
| Tetrafoil | -0.018±0.136 | -0.271±0.329 | 0.001 | -0.011±0.148 | -0.037±0.055 | 0.391 | 0.038±0.266 | -0.011±0.321 | 0.502 |
| Secondary astigmatism | -0.014±0.103 | 0.009±0.116 | 0.226 | -0.019±0.109 | -0.031±0.028 | 0.572 | -0.034±0.111 | -0.030±0.143 | 0.855 |
RMS: Root mean square; tLOA: Total low order aberration; tHOA: Total high order aberration; Z: Zernik; Coma: Z3−1 and Z31; Trefoil: Z3−3 and Z33; Tetrafoil: Z4−4 and Z44; Secondary astigmatism: Z4−2 and Z42. The terms of coma, trefoil, tetrafoli and secondary astigmatism indicate the RMS values of the 2 Zernike aberration, P<0.05; P<0.01; P<0.001.
Changes of Posterior Surface Corneal Aberration in Three Groups
Table 4 shows the mean preoperative and postoperative aberrations of posterior cornea over a 6.0 mm area centered on the pupil center for Zernike terms from the 2nd to 4th order, the total RMS values from the 2nd to 6th order, and HOA RMS values from the 3rd to 6th order. Postoperatively, total posterior corneal aberration, total posterior corneal low-order aberration, and total posterior corneal high-order aberration increased significantly in all three groups (Table 4). Trefoil was stable after operation in all three groups. Coma increased significantly in the 12 o'clock incision group (P<0.01) and BENT incision group (P<0.05). Tetrafoil decreased significantly in the 9 o'clock incision group (P<0.01). Secondary astigmatism was stable after operation in 9 o'clock and BENT incision groups, but decreased with statistical significance in the 12 o'clock incision group (P<0.05) (Table 4). Pearson correlation analysis about trefoil, tetrafoil, secondary astigmatisms and coma changes of posterior corneal surface between pre and post-operation versus total astigmatism showed same results as total corneal and anterior corneal surface.
Table 4. Mean preoperative and postoperative RMS values and Zernike aberrations (µm) in the posterior corneal surface over a 6.0 mm diameter central area in 3 groups.
| Parameters | 12 o'clock incision group |
9 o'clock clear corneal incisions |
BENT incision group |
||||||
| Preop. | Postop. | P | Preop. | Postop. | P | Preop. | Postop. | P | |
| Total RMS | 0.757±0.177 | 0.902±0.343 | 0.023 | 0.672±0.200 | 0.770±0.154 | 0.001 | 0.754±0.198 | 0.951±0.291 | 0.002 |
| tLOA | 0.735±0.176 | 0.869±0.328 | 0.025 | 0.645±0.205 | 0.734±0.155 | 0.003 | 0.730±0.196 | 0.917±0.284 | 0.002 |
| tHOA | 0.180±0.037 | 0.238±0.115 | 0.012 | 0.181±0.031 | 0.225±0.062 | 0.000 | 0.183±0.046 | 0.247±0.083 | 0.003 |
| Z (3, -3) | 0.020±0.032 | 0.036±0.061 | 0.240 | -0.013±0.033 | -0.014±0.047 | 0.876 | 0.026±0.041 | 0.023±0.061 | 0.810 |
| Z (3, -1) | 0. 003±0.055 | -0.062±0.095 | 0.001 | 0.029±0.060 | 0.005±0.122 | 0.184 | -0.005±0.048 | -0.059±0.083 | 0.002 |
| Z (3, 1) | 0.003±0.308 | 0.006±0.051 | 0.718 | 0.001±0.043 | 0.045±0.063 | 0.000 | 0.009±0.033 | 0.034±0.058 | 0.016 |
| Z (3,3) | -0.0004±0.024 | 0.000±0.055 | 0.656 | 0.006±0.028 | 0.003±0.048 | 0.733 | -0.003±0.031 | -0.020±0.073 | 0.258 |
| Z (4, -4) | 0.014±0.027 | 0.032±0.062 | 0.081 | 0.000±0.044 | -0.005±0.068 | 0.655 | 0.006±0.031 | 0.011±0.100 | 0.789 |
| Z (4, -2) | 0.002±0.017 | 0.000±0.025 | 0.808 | -0.003±0.018 | 0.010±0.028 | 0.021 | 0.004±0.030 | 0.018±0.034 | 0.070 |
| Z (4, 0) | -0.136±0.038 | -0.147±0.039 | 0.024 | -0.125±0.037 | -0.135±0.033 | 0.033 | -0.131±0.027 | -0.144±0.033 | 0.008 |
| Z (4, 2) | -0.023±0.027 | -0.007±0.034 | 0.029 | -0.056±0.080 | -0.040±0.033 | 0.330 | -0.023±0.030 | -0.015±0.043 | 0.269 |
| Z (4,4) | -0.040±0.033 | -0.024±0.078 | 0.292 | -0.037±0.029 | -0.001±0.051 | 0.000 | -0.033±0.046 | -0.044±0.049 | 0.360 |
| Coma | 0.006±0.062 | -0.056±0.122 | 0.008 | 0.114±0.681 | 0.050±0.150 | 0.604 | 0.004±0.062 | -0.025±0.096 | 0.018 |
| Trefoil | 0.016±0.043 | 0.036±0.084 | 0.243 | -0.019±0.267 | 0.017±0.060 | 0.493 | 0.023±0.058 | 0.003±0.104 | 0.353 |
| Tetrafoil | -0.026±0.046 | 0.007±0.100 | 0.057 | -0.220±0.374 | -0.006±0.091 | 0.005 | -0.028±0.055 | -0.033±0.102 | 0.835 |
| Secondary astigmatism | -0.021±0.029 | -0.007±0.036 | 0.035 | -0.027±0.154 | -0.031±0.048 | 0.895 | -0.019±0.026 | 0.002±0.054 | 0.055 |
RMS: Root mean square; tLOA: Total low order aberration; tHOA: Total high order aberration; Z: Zernik; Coma: Z3−1 and Z31; Trefoil: Z3−3 and Z33; Tetrafoil: Z4−4 and Z44; Secondary astigmatism: Z4−2 and Z42. The terms of coma, trefoil, tetrafoli and secondary astigmatism indicate the RMS values of the 2 Zernike aberration, P<0.05; P<0.01; P<0.001.
Spherical Aberration Changes in Three Groups
Total cornea SA and anterior cornea SA decreased 3mo after operation in all three groups. In 9 o'clock and 12 o'clock incision groups, total SA decreased after operation without statistical significance (P=0.73, 0.111), but in BENT incision group, total cornea SA decreased from 0.334±0.127 µm to 0.243±0.092 µm after operation (P=0.000) (Figure 1A). For anterior cornea aberration, the results were same. In 9 o'clock and 12 o'clock incision groups, SA decreased without statistical significance (P=0.875, 0.146), but in BENT incision group, anterior cornea SA decreased from 0.328±0.116 µm to 0.294±0.094 µm after operation (P=0.024) (Figure 1B). For posterior cornea surface, SA increased in all three groups after operation with statistical significance (P=0.024, 0.033 and 0.008, respectively) (Figure 1C). Pearson correlation analysis results indicated that SA changes of total cornea between pre and post-operation had no significant relationship with total astigmatism in all three groups.
Figure 1. SA RMS changes in three groups.
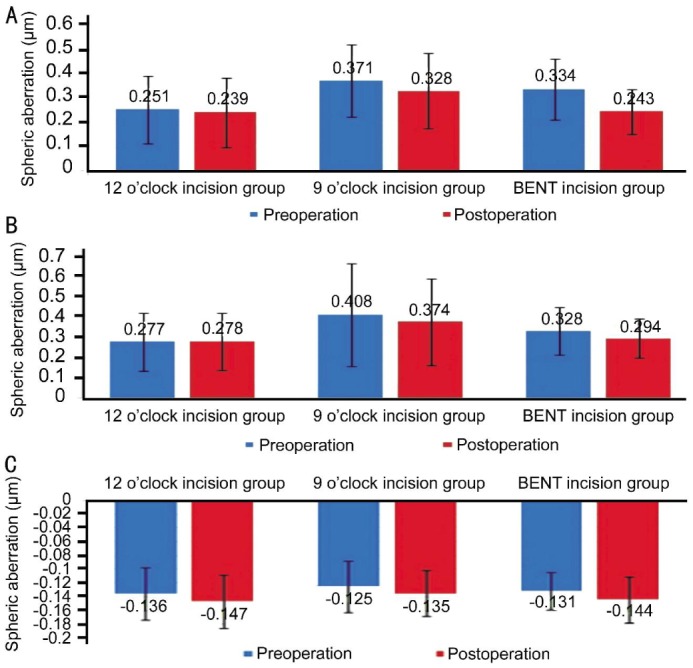
Total cornea SA (A) and anterior cornea SA (B) decreased after operation in all three groups. And in BENT incision group, SA of total cornea and anterior corneal surface decreased with statistic significance (P<0.01). C: SA of posterior cornea surface increased in all three groups after operation with statistical significance (P=0.024, 0.033 and 0.008, respectively).
DISCUSSION
The optical quality degradation is caused in part by the aberration of the optical system especially SA and other HOAs[12]. For cataract patients, both corneal and IOL induced wavefront aberrations can affect the visual quality after cataract surgery. In this prospective study, we measured wavefront aberrations of the anterior, posterior corneal surface and total cornea preoperatively and postoperatively in age-related cataract eyes and evaluated the influence of incision location on corneal aberrations postoperatively.
It is well known that the radius of curvature flattens from the center to the limbus and does so at different rates in different semi-meridians[11],[13]. As a result, different incision location can induce different levels of astigmatism and corneal aberration. Steep meridian incision was selected in cataract surgery for better correction of corneal astigmatism. Our study revealed that total corneal aberration and tLOA decreased significantly when we select steep meridian small incision in cataract surgery. It appears that the increase of the HOAs resulted from both anterior and posterior corneal surfaces after surgery. In addition, tHOA also increased 3mo after surgery, especially if we select 12 o'clock corneal incision. Although steep meridian small incision indicated that this study wasn't a random study, but Pearson relationship analysis results showed that all the aberration changes had no relationship with surgical induced astigmatism.
The quality of vision can be affected by HOAs such as coma and SA. Some pseudophakic patients continue to experience glare, halos, and starburst in their vision that could be attributed to SA. Taking into the account of both ocular and corneal SA, various aspheric IOLs have been manufactured[13]–[15]. Such aspheric design has improved the contrast sensitivity and reduced the occurrence of glare and halos in patients' vision after cataract surgery[15]–[17]. Corneal aberration was the other important factor affected the visual quality. In our study, the total cornea SA decreased after surgery in all of three groups, but only decreased significantly in BENT corneal incision group. Therefore, operating on BENT axis can enhance the reduction effects of SA and the BENT corneal incision is preferable for correcting SA in cataract surgery.
Masket et al[18] found that corneal aberrations increased after IOL implantation, particularly in astigmatism and trefoil terms. Carricondo et al[19] suggested that small incision surgeries introduce changes in corneal aberrations, such as coma, trefoil, and astigmatism, especially in nasal incisions. In our study, we found a significant increase in tetrafoil, secondary astigmatism and coma, especially in 12 o'clock incision group at 3mo postoperatively. Such increase may be attributable to incision healing, however, in the BENT and 9 o'clock incision groups, similar increase was not seen. The coma variation came from posterior surface of cornea, but tetrafoil came from anterior corneal surface, suggesting that the posterior corneal surface recovery was important in reducing coma formation. Previously, the topography of the anterior corneal surface has mostly been measured to evaluate surgically induced aberrations and accurate data on the shape of the posterior surface of the cornea have been rather insufficient, despite the considerable contribution of the posterior surface to total corneal power. Perceivably, intraocular operations will tend to alter the shape of the posterior corneal surface considering the dynamics of fluid flow, surgical manipulation and inflammation after surgery[20]–[21]. Longer follow-up with more patients is needed in the future to elucidate long-term changes of posterior surface aberration.
Studies have demonstrated a nearly linear decline in image quality with age, suggesting a significant increase in the optical aberrations in the eye over time. Both ocular and corneal wavefront aberrations will change with age. Our study was based on a group of aged cataract patients, whereas the corneal aberration induced after surgery could be different in younger patients.
In conclusion, our study suggests that the 12 o'clock clear corneal incision eliminated more HOAs after steep meridian small incision phacoemulsification cataract surgery and its use should be encouraged. The BENT incision helps to reduce total corneal SA and could correct more SA when operating on this axis. The adoption of ocular wavefront technology in clinical ophthalmology makes it possible to quantify total ocular aberrations and better understand the potential benefits of a customized IOL to correct the aberrations of the eye. The corneal incision sites indeed contribute significantly to the postoperative corneal aberrations. Cataract lens replacement using wavefront-corrected IOL combined with optimized corneal incision site would improve visual quality.
Acknowledgments
Conflicts of Interest: Chu L, None; Zhao JY, None; Zhang JS, None; Meng J, None; Wang MW, None; Yang YJ, None; Yu JM, None.
REFERENCES
- 1.Liu F, Huang YJ, Xu M, Wang XH, Feng W, Lian JC. High-order aberration and visual quality. Guoji Yanke Zazhi (Int Eye Sci) 2007;7(4):1113–1115. [Google Scholar]
- 2.Li YJ, Choi JA, Kim H, Yu SY, Joo CK. Changes in ocular wavefront aberrations and retinal image quality with objective accommodation. J Cataract Refract Surg. 2011;37(5):835–841. doi: 10.1016/j.jcrs.2010.11.031. [DOI] [PubMed] [Google Scholar]
- 3.Beiko GH. Personalized correction of spherical aberration in cataract surgery. J Cataract Refract Surg. 2007;33(8):1455–1460. doi: 10.1016/j.jcrs.2007.04.019. [DOI] [PubMed] [Google Scholar]
- 4.Villegas EA, Alcón E, Artal P. Optical quality of the eye in subjects with normal and excellent visual acuity. Invest Ophthalmol Vis Sci. 2008;49(10):4688–4696. doi: 10.1167/iovs.08-2316. [DOI] [PubMed] [Google Scholar]
- 5.Ueda T, Nawa Y, Masuda K, Ishibashi H, Hara Y, Uozato H. Relationship between corneal aberrations and contrast sensitivity after hyperopic laser in situ keratomileusis. Jpn J Ophthalmol. 2006;50(2):147–152. doi: 10.1007/s10384-005-0285-x. [DOI] [PubMed] [Google Scholar]
- 6.Guirao A, Tejedor J, Artal P. Corneal aberrations before and after small-incision cataract surgery. Invest Ophthalmol Vis Sci. 2004;45(12):4312–4319. doi: 10.1167/iovs.04-0693. [DOI] [PubMed] [Google Scholar]
- 7.Alió JL, Plaza-Puche AB, Piñero DP, Amparo F, Rodríguez-Prats JL, Ayala MJ. Quality of life evaluation after implantation of 2 multifocal intraocular lens models and a monofocal model. J Cataract Refract Surg. 2011;37(4):638–648. doi: 10.1016/j.jcrs.2010.10.056. [DOI] [PubMed] [Google Scholar]
- 8.Marcos S, Rosales P, Llorente L, Jiménez-Alfaro I. Change in corneal aberrations after cataract surgery with 2 types of aspherical intraocular lenses. J Cataract Refract Surg. 2007;33(2):217–226. doi: 10.1016/j.jcrs.2006.10.021. [DOI] [PubMed] [Google Scholar]
- 9.Yao K, Tang X, Ye P. Corneal astigmatism, high order aberrations, and optical quality after cataract surgery: microincision versus small incision. J Refract Surg. 2006;22:S1079–1082. doi: 10.3928/1081-597X-20061102-13. [DOI] [PubMed] [Google Scholar]
- 10.Tong N, He JC, Lu F, Wang Q, Qu J, Zhao YE. Changes in corneal wavefront aberrations in microincision and small-incision cataract surgery. J Cataract Refract Surg. 2008;34(12):2085–2090. doi: 10.1016/j.jcrs.2008.08.020. [DOI] [PubMed] [Google Scholar]
- 11.Zhang L, Wang Y. The shape of posterior corneal surface in normal, post-LASIK, and post-epi-LASIK eyes. Invest Ophthalmol Vis Sci. 2010;51(7):3468–3475. doi: 10.1167/iovs.09-4811. [DOI] [PubMed] [Google Scholar]
- 12.Carney LG, Mainstone JC, Henderson BA. Corneal topography and myopia A cross-sectional study. Invest Ophthalmol Vis Sci. 2007;38(2):311–320. [PubMed] [Google Scholar]
- 13.McKelvie J, McArdle B, McGhee C. Relationship between aspheric IOL power and spherical aberration. J Cataract Refract Surg. 2011;37(10):1915. doi: 10.1016/j.jcrs.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 14.Sandoval HP, Fernández de Castro LE, Vroman DT, Solomon KD. Comparison of visual outcomes, photopic contrast sensitivity, wavefront analysis, and patient satisfaction following cataract extraction and IOL implantation: aspheric vs spherical acrylic lenses. Eye (Lond) 2008;22(12):1469–1475. doi: 10.1038/sj.eye.6702925. [DOI] [PubMed] [Google Scholar]
- 15.Pepose JS, Qazi MA, Edwards KH, Sanderson JP, Sarver EJ. Comparison of contrast sensitivity, depth of field and ocular wavefront aberrations in eyes with an IOL with zero versus positive spherical aberration. Graefes Arch Clin Exp Ophthalmol. 2009;247(7):965–973. doi: 10.1007/s00417-009-1038-1. [DOI] [PubMed] [Google Scholar]
- 16.Cheng AC, Lam DS. High-order aberrations in pseudophakia with different IOLs. J Cataract Refract Surg. 2005;31(5) doi: 10.1016/j.jcrs.2005.03.042. [DOI] [PubMed] [Google Scholar]
- 17.Pieh S, Fiala W, Malz A, Stork W. In vitro Strehl ratioswith spherical, aberration-free, average, and customized spherical aberra-tion-correcting intraocular lenses. Invest Ophthalmol Vis Sci. 2009;50(3):1264–1270. doi: 10.1167/iovs.08-2187. [DOI] [PubMed] [Google Scholar]
- 18.Masket S, Wang L, Belani S. Induced astigmatism with 2.2-and 3.0-mm coaxial phacoemulsification incisions. J Refract Surg. 2009;25(1):21–24. doi: 10.3928/1081597X-20090101-04. [DOI] [PubMed] [Google Scholar]
- 19.Carricondo PC, Fortes AC, Mourao Pde C, Hajnal M, Jose NK. Senior resident phacoemulsification learning curve ( corrected from cure) Arq Bras Oftalmol. 2010;73(1):66–69. doi: 10.1590/s0004-27492010000100012. [DOI] [PubMed] [Google Scholar]
- 20.Prakash G, Jhanji V, Sharma N, Gupta K, Titiyal JS, Vajpayee RB. Assessment of perceived difficulties by residents in performing routine steps in phacoemulsification surgery and in managing complications. Can J Ophthalmol. 2009;44(3):284–287. doi: 10.3129/i09-051. [DOI] [PubMed] [Google Scholar]
- 21.Morales EL, Rocha KM, Chalita MR, Nosé W, Avila MP. Comparison of optical aberrations and contrast sensitivity between aspheric and spherical intraocular lenses. J Refract Surg. 2011;27(10):723–728. doi: 10.3928/1081597X-20110708-02. [DOI] [PubMed] [Google Scholar]


