Abstract
AIM
To investigate the prevalence of and risk factors for lens opacities in populations living at two different altitudes in China.
METHODS
A total of 813 subjects aged ≥40y in Lhasa (Tibet Autonomous Region, China. Altitude: 3658 m) and Shaoxing (Zhejiang Province, China. Altitude: 15 m) were underwent eye examinations and interviewed in this cross-sectional study. Participants' lens opacities were graded according to the Lens Opacities Classification System II (LOCS II) and the types of opacities with LOCS II scores ≥2 were determined. Univariate and stepwise logistic regression were used to evaluate the associations of independent risk factors with lens opacities.
RESULTS
Lens opacities were significantly more prevalent in the high-altitude than in the low-altitude area (χ2=10.54, P<0.001). Lens opacities appear to develop earlier in people living at high than at low altitude. The main types of lens opacity in Lhasa and Shaoxing were mixed (23.81%) and cortical (17.87%), respectively. Independent risk factors associated with all lens opacities were age, ultraviolet (UV) radiation exposure, and educational level. Compared with participants aged 40-49y, the risk of lens opacities increased gradually from 2 to 85 times per 10y [odds ratio (OR)=2.168-84.731, P<0.05). The risk of lens opacities was about two times greater in participants with the highest UV exposure than in those with the lowest exposure (OR=2.606, P=0.001). Educational level was inversely associated with lens opacities; literacy deceased the risk by about 25% compared with illiteracy (OR=0.758, P=0.041).
CONCLUSION
Old age, higher UV exposure and lower educational level are important risk factors for the development of lens opacities. Lens opacities are more prevalent among high-altitude than low-altitude inhabitants.
Keywords: lens opacities, risk factor, altitude, ultraviolet exposure, cataract
INTRODUCTION
Age-related lens opacity (cataract) is the leading cause of blindness worldwide[1]–[2]. Of an estimated 39 million blind people worldwide in 2010, 51% of cases were attributed to cataract[3]. As populations age, the number of blind people is expected to double by 2025[4]. Age-related cataracts account for 80% of all cataracts[5]. More than 60 million patients in China had cataracts in 2007, and more than 7 million had disabilities caused by cataracts[6]. The burden of cataract is expected to pose increasing challenges for healthcare systems in future years.
Ultraviolet (UV) radiation, an important ambient factor associated with age-related lens opacity, was taken as a continual focus of research for several decades[7]. Many epidemiological studies of sunlight and cataract with diverse designs and approaches were conducted. Generally, sunlight or UV exposure was quantified using annual or daily hours of sunshine[8]–[10], average daily erythemal UVB exposure[11], indoor/outdoor occupation and residential history[12]–[13], or a UVB or UVA exposure index combined with ambient solar or UV radiation and personal behavior[14]–[15]. Assessment endpoints of the effects of sunlight or UV radiation on cataract were typically the prevalence of cataract under a given UV exposure condition[8]–[9] or associations between different types of lens opacity and sunlight or UV exposure, expressed as odds ratios (ORs)[16]–[17]. Due to differences in examination methods and diagnostic or evaluative criteria, the results of these studies were usually not compared and some were controversial.
Latitude and altitude are two basic geographical factors that influence the intensity of UV radiation. UV exposure and the prevalence of age-related cataract increase with decreasing latitude and increasing altitude[10]. Lhasa (Tibet Autonomous Region, China. Altitude: 3658 m; latitude: 29.7° N) is one of the high altitude areas of human being to exposure high intensity UV radiation, it is the highly valuable area of human survival with extreme UV exposure in the world. The herdsmen live here with extreme higher UV exposure is rare in the traditional style of life. Moreover, because modern life style will make herders less to outdoor activities, it is very difficult to search such effects of higher UV exposure on cataract in the future, our present research provided important exposure upper limit information on dose response relationship between UV exposure and cataract, and Shaoxing (Zhejiang Province, China. Altitude: 15 m; latitude: 30.2° N) was taken as control. Thus, the current study was conducted to explore the prevalence of lens opacities in populations living at two different altitudes but similar latitudes, and to examine the risk factors for all lens opacities.
SUBJECTS AND METHODS
Ethics Statement
The ethics committee of China Medical University approved the study protocol and all subjects provided written informed consent before participating.
Subjects
Subjects were from rural areas at high (Lhasa, Tibet Autonomous Region, China. Altitude: 3658 m; latitude: 29.7° N) and low (Shaoxing, Zhejiang Province, China. Altitude: 15 m; latitude: 30.2° N) altitudes in China. In both areas, we notified local residents of the research aim with the help of village committees and invited them to participate in the study. Only native-born local residents aged ≥40y who had not migrated were enrolled. All subjects were farmers with stable, regular lifestyles and simple daily routines. Subjects with glaucoma, pseudophakia, and bilateral aphakia were excluded.
Lens Examination and Lens Opacity Classification
Following dilation with 1% tropicamide and 2.5% phenylephrine, participants' lenses were examined using a slit lamp. The Lens Opacities Classification System II (LOCS II)[17] was used to classify opacities into seven cortical (C0, Ctr, CI-CV), five nuclear (N0-NIV), and five posterior subcapsular (PSC; P0-PIV) grades of increasing severity, according to photographic standards. Individuals with a single type of opacity (LOCS II grade ≥2) in one or both eyes were assigned to the cortical, nuclear, or PSC opacity category, as appropriate. For participants with unilateral lens extraction, LOCS II grades from contralateral phakic eyes were used to define lens opacity type. Those with various combinations of nuclear, cortical, and PSC opacities (LOCS II grade ≥2) in one or both eyes were classified as having mixed-type lens opacities.
Data Collection and Risk Factor Assessment
Trained investigators interviewed participants and used a questionnaire to collect data on demographic and lifestyle characteristics, including age, gender, nationality, smoking status, alcohol consumption, educational level, fruit and vegetable intake, and amount of outdoor activity. Smoking status was classified as yes (had smoked for at least 6mo during his/her life) or no (did not smoke at all or had ever smoked less than 6mo during his/her life). Alcohol consumption status was classified as yes (at least once per week) or no (no consumption or less than once per week). Educational level was classified as literacy (more than primary school) or illiteracy (less than primary school). Fruit intake over participants' lifetimes was classified as yes (≥2d every week) or no (<2d every week). Vegetable intake over participants' lifetimes was classified as yes (≥2 diet every day) or no (<2 diet every day).
The amounts of outdoor activity in four stages of participants' lives (pre-school, school, work, and special periods such as recuperation after a serious illness) were used to evaluate UV exposure. Interviewers asked participants to recall the typical numbers of hours spent outdoors between 06:00 and 19:00 on work/school and non-work/school days during each stage.
Ultraviolet Exposure Calculation and Evaluation
Using average annual erythemal UV exposure data from the National Aeronautics and Space Administration (NASA)[18] and National Oceanic and Atmospheric Administration (NOAA)[19] procedures for calculating local times of sunrise, solar noon, sunset, dawn, and dusk, we calculated daily erythemal UV exposure and hours of sunshine for Lhasa and Shaoxing. We then determined hourly erythemal UV exposure. Participants' UV exposure was determined by multiplying hourly erythemal UV exposure by reported daily average hours of outdoor activity, and classified into four grades according to quartiles (<1000, 1000-1199, 1200-2700, and >2700 J/m2).
Statistical Analysis
The Chi-squared test was used to assess differences in categorical sociodemographic variables between the low- and high-altitude groups overall and between and within regions by age group and gender. Variables with P-values ≤0.2 were considered to be candidate risk factors for lens opacities and included in a multivariate logistic regression model. Stepwise logistic regression including data from the entire study sample was performed to evaluate independent associations between these risk factors and lens opacities, with estimated ORs and 95% confidence intervals (CI). All statistical analyses were performed using SPSS software (ver. 16.0 for Windows; SPSS Inc., Chicago, IL, USA).
RESULTS
Characteristics of the Study Population
After the exclusion of subjects with glaucoma (n=6), pseudophakia (n=7), and bilateral aphakia (n=7), 813 eligible volunteers (231 in Lhasa, 582 in Shaoxing) were included in this study. Participants' characteristics are summarized by altitude in Table 1. The average age was 58.14 (range, 40-91)y. The mean UV exposure was 1750.19±1111.77 (range, 366.47-5301.42) J/m2 and the mean (±standard deviation) daily outdoor time was 5.33±1.56 (range, 1.57-10.81)h. UV exposure levels and outdoor times were significantly higher in subjects from Lhasa than in those from Shaoxing (3404.46±573.78 vs 1093.60±277.95 J/m2 and 6.98±1.17 vs 4.69±1.19h/d, respectively; both P<0.001). Compared with literate participants, illiterate participants had longer outdoor times (5.87±1.59 vs 4.94±1.42h/d, P<0.001) and significantly greater UV exposure (2191.19±1262.52 vs 1441.12±869.31 J/m2, P<0.001).
Table 1. Demographic characteristics of the study population.
| Parameters | Lhasa (high altitude; n=231) | Shaoxing (low altitude; n=582) |
| Age (a; x±s) | 56.64±12.19 | 58.74±11.18 |
| 40-49 | 77 (33.3) | 145 (24.9) |
| 50-59 | 75 (32.5) | 161 (27.7) |
| 60-69 | 36 (15.6) | 174 (29.9) |
| 70-79 | 28 (12.1) | 81 (13.9) |
| ≥80 | 15 (6.5) | 21 (3.6) |
| Gender | ||
| F | 156 (67.5) | 355 (61.0) |
| M | 75 (32.5) | 227 (39.0) |
| Smoking | ||
| No | 186 (80.5) | 419 (72.0) |
| Occasional | 12 (5.2) | 12 (2.1) |
| Former | 7 (3.0) | 45 (7.7) |
| Current | 26 (11.3) | 106 (18.2) |
| Drinking | ||
| No | 133 (57.6) | 333 (57.2) |
| Occasional | 79 (34.2) | 69 (11.9) |
| Former | 6 (2.6) | 35 (6.0) |
| Current | 13 (5.6) | 145 (24.9) |
| Level of education | ||
| Illiteracy | 148 (64.0) | 187 (32.1) |
| Primary school | 60 (26.0) | 240 (41.2) |
| Middle school | 15 (6.5) | 122 (21.0) |
| College | 8 (3.5) | 33 (5.7) |
| Fruit | ||
| No | 111 (48.1) | 244 (41.9) |
| Yes | 120 (51.9) | 338 (58.1) |
| Vegetable | ||
| ≤1diet/d | 63 (27.3) | 28 (4.8) |
| 2 diet/d | 153 (66.2) | 185 (31.8) |
| 3 diet/d | 15 (6.5) | 369 (63.4) |
| Outdoors time (h/d; x±s) | 6.98±1.17 | 4.69±1.19 |
| UV exposure level (J/m2; x±s) | 3404.46±573.78 | 1093.60±277.95 |
| <1000 | - | 209 (35.9) |
| 1000-1199 | - | 206 (35.4) |
| 1200-2700 | 29 (12.6) | 167 (28.7) |
| >2700 | 202 (87.4) | - |
n (%)
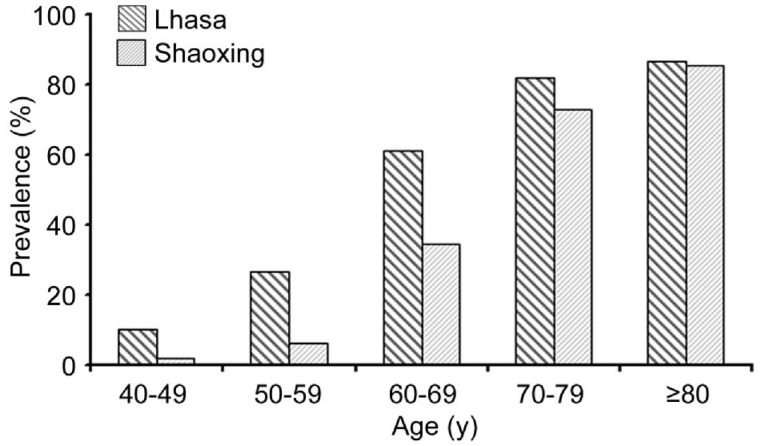
Figure 1 depicts the overall prevalence of lens opacities by age group in Lhasa and Shaoxing. The overall prevalence of lens opacities was significantly higher in the high-altitude than in the low-altitude group (37.23% vs 25.77%; χ2=10.54, P<0.001). This pattern was evident in participants aged 40-49 (χ2=7.39, P=0.007), 50-59 (χ2=19.29, P<0.001), and 60-69 (χ2=8.89, P<0.001)y (high altitude: 10.39%, 26.67%, and 61.11%, respectively; low altitude: 2.07%, 6.21%, and 34.48%, respectively), but not in the 70-79 and ≥80 year age groups.
Figure 1. The prevalence of lens opacities in Lhasa and Shaoxing by age group.
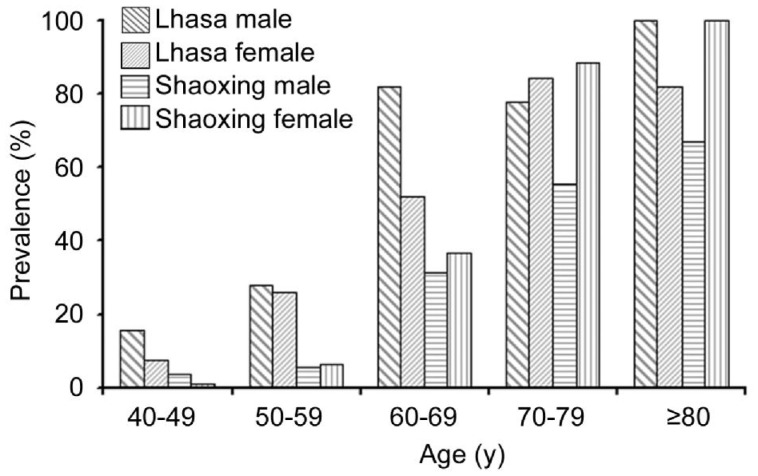
Figure 2 presents gender differences in the prevalence of lens opacities by age group in Lhasa and Shaoxing. This prevalence did not differ between men and women in Lhasa overall or in any age group. In Shaoxing, the prevalence of lens opacities did not differ between men and women overall, but it was significantly higher in women than in men in the 70-79y (88.37% vs 56.26%; χ2=11.18, P<0.001) and ≥80y (100% vs 66.67%; χ2=4.67, P=0.031) age groups. The prevalence of lens opacities was significantly higher among men aged 50-59 and 60-69y in Lhasa than among men of the same ages in Shaoxing (28% vs 5.56%, χ2=7.59, P=0.006 and 81.82% vs 31.51%, χ2=10.26, P<0.001, respectively). Opacities were more prevalent among women aged 40-49 and 50-59y in Lhasa than in corresponding participants in Shaoxing (7.84% vs 1.10%, χ2 =4.38, P=0.036 and 26.00% vs 6.48%, χ2=11.78, P<0.001, respectively).
Figure 2. Gender differences in the prevalence of lens opacities in Lhasa and Shaoxing.
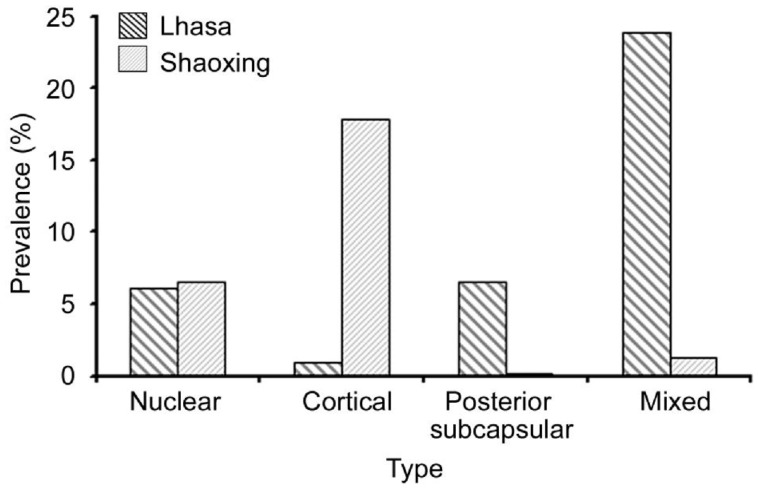
Figure 3 shows differences in the prevalence of lens opacities by type in Lhasa and Shaoxing. The main type of lens opacity in Lhasa was mixed (23.81%), followed by PSC (6.49%), nuclear (6.06%), and cortical (0.87%). In Shaoxing, cortical lens opacities were most common (17.87%), followed by nuclear (6.53%), mixed (1.20%), and PSC (0.17%) opacities.
Figure 3. The prevalence of lens opacities in Lhasa and Shaoxing by type.
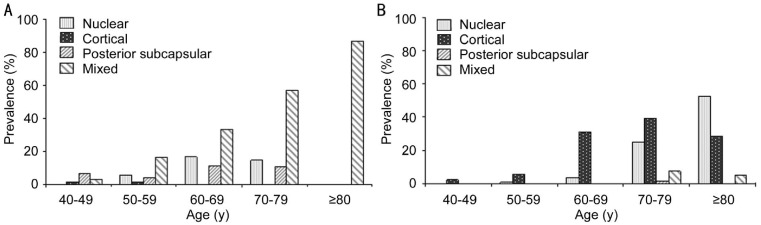
In Lhasa, the most common type of opacity in subjects aged 50-79y was mixed, followed by nuclear and PSC; the prevalence of these three types of lens opacity increased with age in these participants (Figure 4A). Cortical lens opacities were detected only in participants aged 40-59y, and all opacities in participants aged ≥80y were mixed. In contrast, the prevalence of cortical lens opacities increased gradually with age from 40 to ≥80y and nuclear opacities were distributed mainly in subjects aged >60y in Shaoxing (Figure 4B). Mixed lens opacities were detected in subjects aged >70y and a few PSC opacities were found in those aged 70-79y in Shaoxing.
Figure 4. Age-related differences in the prevalence of lens opacity types in Lhasa (A) and Shaoxing (B).
Risk Factors for All Lens Opacities
Table 2 presents the results of final logistic regression models that evaluated the associations of various risk factors with lens opacities. Age, educational level, fruit intake, and UV exposure were identified as candidate risk factors at the univariate level (P<0.2) and included in the multivariate model; gender, smoking status, and alcohol consumption were not included in this model. The results of stepwise logistic regression showed that independent risk factors associated with lens opacities were older age, educational level, and UV exposure. Compared with participants aged 40-49y, the prevalence of lens opacities was about two times higher in those aged 50-59y (OR=2.168, P=0.035), 11 times higher in those aged 60-69y (OR=11.95, P<0.001), 52 times higher in subjects aged 70-79y (OR=52.045, P<0.001), and more than about 85-fold higher in those aged ≥80y (OR=84.731, P<0.001). The risk of lens opacities was higher in subjects with high (>2700 J/m2) UV exposure levels than in those with low (<1000 J/m2) UV exposure (OR=2.606, P=0.001). Educational level was inversely associated with lens opacities, the risk among literate participants was about 75% that among illiterate subjects (OR=0.758, P=0.041).
Table 2. Risk factors for lens opacities in populations in Lhasa and Shaoxing.
| Variables | No (n=813) | Univariate OR (95% CI) | 1P | Multivariate OR (95% CI) | 2P |
| Age (a) | |||||
| 40-49 | 222 | 1 | 1 | - | |
| 50-59 | 236 | 2.549 (1.270-5.114) | 0.008 | 2.168 (1.056-4.451) | 0.035 |
| 60-69 | 210 | 11.211 (5.885-21.355) | <0.001 | 11.950 (6.000-23.799) | <0.001 |
| 70-79 | 109 | 53.148 (25.707-109.881) | <0.001 | 52.045 (23.849-113.580) | < 0.001 |
| ≥80 | 36 | 108.500 (35.781-329.009) | 0.001 | 84.731 (26.658-269.314) | <0.001 |
| Gender | |||||
| M | 302 | 1 | |||
| F | 511 | 1.053 (0.770-1.442) | 0.745 | - | - |
| Education | |||||
| Illiteracy | 335 | 1 | 1 | ||
| Literacy | 478 | 0.429 (0.344-0.534) | <0.001 | 0.758 (0.581-0.989) | 0.041 |
| Fruit | |||||
| No | 355 | 1 | |||
| Yes | 458 | 0.746 (0.637-0.874) | <0.001 | - | - |
| UV exposure (J/m2) | |||||
| <1000 | 209 | 1 | 1 | ||
| 1000-1199 | 206 | 1.959 (1.254-3.060) | 0.003 | 1.220 (0.705-2.110) | 0.477 |
| 1200-2700 | 196 | 1.365 (0.854-2.171) | 0.195 | 0.882 (0.501-1.551) | 0.662 |
| >2700 | 202 | 2.449 (1.575-3.810) | <0.001 | 2.606 (1.454-4.671) | 0.001 |
OR: Odds ratio; CI: Confidence interval. 1P value of univariate OR; 2P value of multivariate OR.
DISCUSSION
From west to east, China encompasses a nearly 4000 m difference in altitude, making it an ideal setting for research on the effects of altitude on lens opacities. To eliminate the effects of latitude and focus solely on those of altitude, participants in the present study were from low- (Shaoxing) and high- (Lhasa) altitude regions at almost the same latitude. Furthermore, we chose to study native-born rural farmers with stable lifestyles and simple daily routines to eliminate the complex effects of urban inhabitants' diverse occupations, lifestyles, and outdoor activity patterns. Time spent outdoors was almost entirely consistent with farming activities among our participants, which aided the comparative evaluation of ambient UV exposure.
The results of the present study showed that the prevalence of lens opacities increased with age in both regions and was significantly higher in Lhasa than in Shaoxing, especially among those aged <70y. Thus, lens opacities appear to develop earlier in people living at high than at low altitude. Cortical lens opacities were most common in Shaoxing, consistent with the findings of several studies that strongly support UVB as a risk factor for cortical cataract[15],[20]. In contrast, the main type of lens opacity in Lhasa was mixed. This finding contrasts with that of EI Chehab et al[21] who reported that UV exposure at an altitude >3000 m was a risk factor for anterior cortical cataract in a maintain guide group (OR=1.16, P<0.01). The reason for this difference is not clear.
Stepwise logistic regression of data from the entire study population revealed that age, UV exposure, and educational level were independent risk factors for lens opacities. The development of lens opacities is often considered a normal part of the aging process; a strong association between age and cataracts has been reported widely, and the Barbados Eye and Age-Related Eye Disease studies found that age was a significant risk factor for incident nuclear, cortical, and PSC lens opacities[22]–[24]. The risk of lens opacities increased gradually from 2- to 85-fold in our study subjects, similar to the findings of previous studies. However, the link between age and lens opacities likely entails increased cumulative exposure to numerous risks, including environmental (e.g. UVB exposure, oxidative damage) and biological (e.g. hormone, metabolism) factors.
Many epidemiological studies conducted worldwide have examined UV exposure as a risk factor for lens opacities, but the effects of altitude and the associations between different altitudes and UV exposure levels remain unclear. In the present study, we calculated participants' UV exposure using daily erythemal exposure values from NASA and found that all subjects with the lowest (<1000 J/m2) exposure levels were from Shaoxing, whereas all of those with the highest (>2700 J/m2) levels were from Lhasa. Our data suggest that the risk of lens opacities is more than two times greater among people living at high altitudes with higher UV exposure levels than among those living at low altitudes with lower exposure levels.
Socioeconomic and lifestyle factors may influence the development of lens opacities. Consistent with previous findings that education level is inversely associated with the risk of nuclear and cortical cataract development[25]–[26], the results of the present study indicated that educational level was a significant and inversely associated risk factor for lens opacities in low- and high-altitude areas. Literacy was associated with a 25% decrease in the risk of lens opacities compared with illiteracy. We also found that illiterate participants spent more hours outdoors and had significantly greater UV exposure than literate participants, suggesting that a high education level is associated with less time spent outdoors. These results further highlight the importance of high UV exposure at high altitude as a risk factor related to lens opacities.
Smoking and alcohol consumption have been related directly to at least one type of lens opacity in many cross-sectional[27]–[28] and longitudinal[29] studies. However, we found no evidence suggesting a relationship between smoking, alcohol consumption, or fruit and vegetable intake and lens opacities.
In addition, the Tibetan Plateau has an average altitude of more than 4000 m, the annual average oxygen content in the air is only 64.3% of that in the plain. In Lhasa, the highest oxygen contents in the autumn and the lowest oxygen contents in the winter is 66.2% and 63.3% of that in the plain, respectively. Some experimental studies were conducted on the effects of hypoxia on the mechanism of cataract formation[30]–[31]. Thus, the role of hypoxia in the formation of cataract is also not negligible in the high altitude area.
The small number of subjects constitutes a limitation of the current study. Although the results showed distinct differences in the prevalence of lens opacities in Lhasa and Shaoxing, insufficient numbers of subjects were classified as having nuclear, cortical, PSC, and mixed lens opacities to examine covariance in the logistic regression model or to explore type-specific risk factors. Thus, we analyzed only the relationships of risk factors with the overall prevalence of lens opacities at the two altitudes. In addition, the Chinese policies of reform and opening have led increasing numbers of rural young men to migrate from rural to urban areas for work in recent years, dramatically changing the rural population structure. Thus, our study population predominantly comprised women and older individuals. Furthermore, almost all participants in Lhasa were of Zang nationality, whereas those in Shaoxing were of Han nationality; genetic differences and dietary customs in high-altitude residents may affect the prevalence of lens opacities, but these factors were not examined in the present study.
Overall, notwithstanding these limitations, the results of this study provide new evidence for the link between altitude and lens opacities. Using the LOCS II, we determined that lens opacities were more prevalent in high-altitude than in low-altitude rural communities located at similar latitudes. Lens opacities also appeared to develop earlier at high than at low altitude. Older age, higher UV exposure, and lower educational level were associated with a higher prevalence of lens opacities. Further studies with larger samples are needed to explore how and why high altitude induces the development of different types of lens opacity.
Acknowledgments
Foundation: Supported by the Natural Science Foundation of Liaoning Province, China (No. 2014021009).
Conflicts of Interest: Yu JM, None; Yang DQ, None; Wang H, None; Xu J, None; Gao Q, None; Hu LW, None; Wang F, None; Wang Y, None; Yan QC, None; Zhang JS, None; Liu Y, None.
REFERENCES
- 1.Gollogly HE, Hodge DO, St Sauver JL, Erie JC. Increasing incidence of cataract surgery: population-based study. J Cataract Refract Surg. 2013;39(9):1383–1389. doi: 10.1016/j.jcrs.2013.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Watkinson S, Seewoodhary R. Cataract management: effect on patients' quality of life. Nurs Stand. 2015;29(21):42–48. doi: 10.7748/ns.29.21.42.e9222. [DOI] [PubMed] [Google Scholar]
- 3.Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96(5):614–618. doi: 10.1136/bjophthalmol-2011-300539. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization . Prevention of blindness and visual impairment: WHO releases the new global estimates on visual impairment. Geneva: World Health Organization; Available at: http://www.who.int/blindness/en/index.html. Accessed November 25, 2013. [Google Scholar]
- 5.Stevens GA, White RA, Flaxman SR, Price H, Jonas JB, Keeffe J, Leasher J, Naidoo K, Pesudovs K, Resnikoff S, Taylor H, Bourne RR. Global prevalence of vision impairment and blindness: magnitude and temporal trends, 1990-2010. Ophthalmology. 2013;120(12):2377–2384. doi: 10.1016/j.ophtha.2013.05.025. [DOI] [PubMed] [Google Scholar]
- 6.Office of the Second China National Sample Survey on Disability . Documentation of the Second China National Sample Survey on Disability. Beijing: China Statistics Press; 2007. p. 1380. [Google Scholar]
- 7.West SK, Longstreth JD, Munoz BE, Pitcher HM, Duncan DD. Model of risk of cortical cataract in the US population with exposure to increased ultraviolet radiation due to stratospheric ozone depletion. Am J Epidemiol. 2005;162(11):1080–1088. doi: 10.1093/aje/kwi329. [DOI] [PubMed] [Google Scholar]
- 8.Wang Y, Yu J, Gao Q, Hu L, Gao N, Gong H, Liu Y. The relationship between the disability prevalence of cataracts and ambient erythemal ultraviolet radiation in China. PLoS One. 2012;7(11):e51137. doi: 10.1371/journal.pone.0051137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yam JC, Kwok AK. Ultraviolet light and ocular diseases. Int Ophthalmol. 2014;34(2):383–400. doi: 10.1007/s10792-013-9791-x. [DOI] [PubMed] [Google Scholar]
- 10.Díez-Ajenjo MA, García-Domene MC, Artigas JM, Felipe A, Peris-Martínez C, Menezo JL. Lens opacities in Valencia, Spain. Eur J Ophthalmol. 2011;21(6):715–722. doi: 10.5301/EJO.2011.6507. [DOI] [PubMed] [Google Scholar]
- 11.Roberts JE. Ultraviolet radiation as a risk factor for cataract and macular degeneration. Eye Contact Lens. 2011;37(4):246–249. doi: 10.1097/ICL.0b013e31821cbcc9. [DOI] [PubMed] [Google Scholar]
- 12.Mrena S, Kivelä T, Kurttio P, Auvinen A. Lens opacities among physicians occupationally exposed to ionizing radiation-a pilot study in Finland. Scand J Work Environ Health. 2011;37(3):237–243. doi: 10.5271/sjweh.3152. [DOI] [PubMed] [Google Scholar]
- 13.Finger RP, Sivasubramaniam S, Morjaria P, Bansal A, Muhit M, Kinra S, Gilbert CE. Migration study of lens opacities in Bangladeshi adults in London and Bangladesh: a pilot study. Br J Ophthalmol. 2015;99(6):762–767. doi: 10.1136/bjophthalmol-2014-305971. [DOI] [PubMed] [Google Scholar]
- 14.Allinson S, Asmuss M, Baldermann C, Bentzen J, Buller D, Gerber N, Green AC, Greinert R, Kimlin M, Kunrath J, Matthes R, Pölzl-Viol C, Rehfuess E, Rossmann C, Schüz N, Sinclair C, Deventer Ev, Webb A, Weiss W, Ziegelberger G. Validity and use of the UV index: report from the UVI working group, Schloss Hohenkammer, Germany, 5-7 December 2011. Health Phys. 2012;103(3):301–306. doi: 10.1097/HP0b013e31825b581e. [DOI] [PubMed] [Google Scholar]
- 15.Zhu M, Yu J, Gao Q, Wang Y, Hu L, Zheng Y, Wang F, Liu Y. The relationship between disability-adjusted life years of cataracts and ambient erythemal ultraviolet radiation in China. J Epidemiol. 2015;25(1):57–65. doi: 10.2188/jea.JE20140017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Delcourt C, Cougnard-Grégoire A, Boniol M, Carrière I, Doré JF, Delyfer MN, Rougier MB, Le Goff M, Dartigues JF, Barberger-Gateau P, Korobelnik JF. Lifetime exposure to ambient ultraviolet radiation and the risk for cataract extraction and age-related macular degeneration: the Alienor Study. Invest Ophthalmol Vis Sci. 2014;55(11):7619–7627. doi: 10.1167/iovs.14-14471. [DOI] [PubMed] [Google Scholar]
- 17.Pastor-Valero M, Fletcher AE, de Stavola BL, Chaqués-Alepúz V. Years of sunlight exposure and cataract: a case-control study in a Mediterranean population. BMC Ophthalmol. 2007;7:18. doi: 10.1186/1471-2415-7-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nimbus 7 data NASA Goddard Space Flight Center Data Archive Center database. Available at: ftp://toms.gsfc.nasa.gov/pub/nimbus7/data/uv_ery_4_wave lengths/ery_dose/ Accessed 27 April 2006.
- 19. The web ( http://www.srrb.noaa.gov/highlights/sunrise/sunrise.html) Calculation of local times of sunrise, solar noon, sunset, dawn, and dusk based on the calculation procedure by NOAA.
- 20.Galichanin K, Löfgren S, Söderberg P. Cataract after repeated daily in vivo exposure to ultraviolet radiation. Health Phys. 2014;107(6):523–529. doi: 10.1097/HP.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 21.EI Chehab H, Blein JP, Herry JP, Chave N, Ract-Madoux G, Agard E, Guarracino G, Swalduz B, Mourgues G, Dot C. Ocular phototoxicity and altitude among mountain guides. J Fr Ophtalmol. 2012;35(10):809–815. doi: 10.1016/j.jfo.2012.06.012. [DOI] [PubMed] [Google Scholar]
- 22.Athanasiov PA, Casson RJ, Sullivan T, Newland HS, Shein WK, Muecke JS, Selva D, Aung T. Cataract in rural Myanmar: prevalence and risk factors from the Meiktila Eye Study. Br J Ophthalmol. 2008;92(9):1169–1174. doi: 10.1136/bjo.2008.139725. [DOI] [PubMed] [Google Scholar]
- 23.Hennis A, Wu SY, Nemesure B, Leske MC. Risk factors for incident cortical and posterior subcapsular lens opacities in the Barbados Eye Studies. Arch Ophthalmol. 2004;122(4):525–530. doi: 10.1001/archopht.122.4.525. [DOI] [PubMed] [Google Scholar]
- 24.Chang JR, Koo E, Agron E, Hallak J, Clemons T, Azar D, Sperduto RD, Ferris FL, 3rd, Chew EY, Age-Related Eye Disease Study Group Risk factors associated with incident cataracts and cataract surgery in the Age-Related Eye Disease Study (AREDS): AREDS report number 32. Ophthalmology. 2011;118(11):2113–2119. doi: 10.1016/j.ophtha.2011.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nam GE, Han K, Ha SG, Han BD, Kim DH, Kim YH, Cho KH, Park YG, Ko BJ. Relationship between socioeconomic and lifestyle factors and cataracts in Koreans: The Korea National Health and Nutrition Examination Survey 2008-2011. Eye (Lond) 2015;29(7):913–920. doi: 10.1038/eye.2015.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Park S, Kim T, Cho SI, Lee EH. Association between cataract and the degree of obesity. Optom Vis Sci. 2013;90(9):1019–1027. doi: 10.1097/OPX.0b013e31829cae62. [DOI] [PubMed] [Google Scholar]
- 27.Lu ZQ, Sun WH, Yan J, Jiang TX, Zhai SN, Li Y. Cigarette smoking, body mass index associated with the risks of age-related cataract in male patients in northeast China. Int J Ophthalmol. 2012;5(3):317–322. doi: 10.3980/j.issn.2222-3959.2012.03.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fan AZ, Li Y, Zhang X, Klein R, Mokdad AH, Saaddine JB, Balluz L. Alcohol consumption, drinking pattern, and self-reported visual impairment. Ophthalmic Epidemiol. 2012;19(1):8–15. doi: 10.3109/09286586.2011.591037. [DOI] [PubMed] [Google Scholar]
- 29.Steel N, Hardcastle AC, Clark A, Mounce LT, Bachmann MO, Richards SH, Henley WE, Campbell JL, Melzer D. Self-reported quality of care for older adults from 2004 to 2011: a cohort study. Age Ageing. 2014;43(5):716–720. doi: 10.1093/ageing/afu091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goralska M, Fleisher LN, McGahan MC. Hypoxia induced changes in expression of proteins involved in iron uptake and storage in cultured lens epithelial cells. Exp Eye Res. 2014;125:135–141. doi: 10.1016/j.exer.2014.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Akoyev V, Das S, Jena S, Grauer L, Takemoto DJ. Hypoxia-regulated activity of PKCepsilon in the lens. Invest Ophthalmol Vis Sci. 2009;50(3):1271–1282. doi: 10.1167/iovs.08-2599. [DOI] [PMC free article] [PubMed] [Google Scholar]