Abstract
Background:
Blunt chest trauma (BCT) poses significant morbidity and mortality worldwide.
Objectives:
We investigated the clinical presentation and outcome of BCT related to road traffic accidents (RTA).
Patients and Methods:
A retrospective observational analysis for patients who sustained BCT secondary to RTA in terms of motor vehicle crash (MVC) and pedestrian-motor vehicle accidents (PMVA) who were admitted to the trauma center at Hamad general hospital, Doha, Qatar, between 2008 and 2011.
Results:
Of 5118 traumatic injury cases, 1004 (20%) were found to have BCT secondary to RTA (77% MVC and 23% PMVA). The majority were males (92%), and expatriates (72%). Among MVCs, 84% reported they did not use protective devices. There was a correlation between chest abbreviated injury score (AIS) and injury severity scoring (ISS) (r = 0.35, r2 = 0.12, P < 0.001). Regardless of mechanism of injury (MOI), multivariate analysis showed that the head injury associated with chest AIS and ISS was a predictor of mortality in BCT. Overall mortality was 15%, and the highest rate was observed within the first 24 hours post-trauma.
Conclusions:
Blunt chest trauma from RTA represents one-fifth of the total trauma admissions in Qatar, with a high overall mortality. Pedestrians are likely to have more severe injuries and higher fatality rates than MVC victims. Specific injury prevention programs focusing on road safety should be implemented to minimize the incidence of such preventable injuries.
Keywords: Chest Trauma, Road Traffic Accidents, Injury, Pedestrians, Motor Vehicle Crashes
1. Background
Blunt chest trauma (BCT) represents 10 - 15% of all traumatic injuries and around 25% of all trauma-related deaths worldwide (1, 2). The etiology and pattern of BCT vary according to the mechanism of injury and socio-economic factors (3, 4). Motor vehicle crashes (MVCs) account for 60 - 70% of all thoracic traumas (5, 6). The mortality rate in BCT patients depends mainly upon the severity of injury and the presence of associated injuries to the other organ systems (3, 6). Unfortunately, developing countries have a greater proportion of road traffic-related deaths (6, 7). Notably, the rapidly developing Middle Eastern countries have a higher incidence of RTA-related fatalities, which is mainly attributed to the high motorization rate (7). Moreover, pedestrians are the most vulnerable road users and sustain significant injuries during RTAs (8, 9). In Qatar, RTAs constitute a higher proportion of BCTs; however, there is a lack of information on the pattern, severity, and outcome of BCT secondary to RTA in terms of MVC vs. pedestrian-motor vehicle accidents.
2. Objectives
This study aimed to evaluate the clinical presentation, severity, and time-based mortality of BCT according to types of RTA (MVC vs. pedestrian motor vehicle accident [PMVA]) in Qatar, a rapidly developing Middle Eastern country.
3. Patients and Methods
This is an observational retrospective analysis of all BCT patients secondary to RTA who required admission to the section of trauma surgery at Hamad general hospital (HGH) between January 2008 and June 2011. Hamad general hospital is the only tertiary hospital with a Level I trauma centre in the state of Qatar. Patients who died at the scene or were declared dead in the trauma resuscitation unit (TRU) were excluded because of incomplete data. The diagnosis of chest injury was made after obtaining the clinical history, a physical examination, and radiologic imaging. Thoracic injuries are defined as injury to the chest wall and/or the contents of the thorax, for example, the pleura, lungs, lower respiratory tract, heart, and great vessels. On arrival, all patients underwent thorough clinical assessment and resuscitation according to advanced TRAUMA life support (ATLS) guidelines. Collected data included age, sex, nationality, mechanism of injury, protective measures, radiological imaging, injury severity score (ISS) calculation using the abbreviated injury scale (AIS), chest AIS value, thoracic trauma (i.e. rib fractures, diaphragmatic injury, pneumothorax, hemothorax, pulmonary contusion, cardiac and major vessels injury), and associated non-thoracic injuries (head and solid organ injuries). Acute interventions (intubation, chest tubes, thoracotomy, tracheostomy, and non-thoracic interventions), hospital length of stay, development of pneumonia, and acute respiratory distress syndrome (ARDS) during hospitalization were also reported. The primary outcome was in-hospital mortality after the initial traumatic event. Data were analyzed according to the type of accident (MVC vs. PMVA), ISS (≤ 15 vs. > 15), and time of death after hospital admission (< 24 hours, 2nd - 7th day, and > 1 week).
3.1. Statistical Analysis
Data were presented as proportions, medians (range), or mean ± standard deviation, as appropriate. Differences in categorical and continuous variables were analyzed using χ2, student’s t-test, and one-way analysis of variance (ANOVA), as appropriate. For the correlation between chest AIS and ISS, a linear regression analysis was performed. Predictors of mortality among BCTs were assessed using multivariate logistic regression analysis including all relevant and significant univariate variables. Two tailed P values of < 0.05 were considered to be significant. All data were analyzed using the statistical package for the social sciences version 18 (SPSS, Inc. Chicago, Illinois, USA).
4. Results
Out of the 5118 trauma patients admitted to HGH, 1004 (19.6 %) were found to have BCT. The mean age of BCT patients was 33 ± 15 years. Males and expatriates represented 92% and 72%, respectively. Demographics, clinical presentation, and outcome of BCT are presented in Table 1. The MOI of BCT comprised of MVC (77%) and PMVA (23%). Among MVC occupants, chest injuries were predominantly observed in drivers (62%), followed by front-seat (13.4%) and back-seat (12.4%) passengers. Most of the MVC victims (84%) did not use protective devices during crashes.
Table 1. Patients Demographics, Clinical Presentations and Outcomes Based on the Mechanism of Injurya.
| Overall | MVC | PMVA | P Value | |
|---|---|---|---|---|
| Patients, No. (%) | 1004 (100) | 771 (77) | 233 (23) | |
| Mean age, y | 32.7 ± 15 | 32.5 ± 14.3 | 33 ± 16.2 | 0.60 |
| Male | 92 | 92 | 93 | 0.55 |
| Prior lung diseases b | 2 | 2.7 | 0.4 | 0.04 |
| Hospital stay (median) | 7 (1 - 262) | 7 (1 - 262) | 9 (1 - 249) | 0.12 |
| Overall mortality | 15 | 12.3 | 23.2 | 0.001 |
| Thoracic injuries | ||||
| Lung contusion | 74 | 73 | 76 | 0.63 |
| Rib fracture | 57.4 | 59 | 53 | 0.14 |
| Pneumothorax | 29 | 28 | 34 | 0.10 |
| Hemothorax | 23 | 22.9 | 23.3 | 0.88 |
| Cardiac injury | 2 | 2.1 | 1.3 | 0.43 |
| Diaphragmatic injury | 1.4 | 3.9 | 0.02 | |
| Associated injuries | ||||
| Spleen injury | 12.4 | 11 | 16 | 0.10 |
| Liver injury | 15 | 14 | 19 | 0.06 |
| Kidney injury | 6 | 5 | 8 | 0.12 |
| Head injury | 44 | 41 | 54 | 0.001 |
| Interventions | ||||
| Exploratory laparotomy | 7.7 | 7 | 11 | 0.02 |
| Tracheostomy | 4.4 | 4.7 | 3.4 | 0.42 |
| Thoracic tube | 19.4 | 19 | 20 | 0.83 |
| Craniotomy | 3.4 | 2.9 | 5.2 | 0.08 |
| ORIF | 16 | 16 | 15.5 | 0.82 |
| Intubation | 32 | 30 | 39 | 0.009 |
| Thoracotomy | 4.4 | 1.8 | 1.7 | 0.92 |
| Chest AIS | 3(1 - 9) | 2.8 ± 0.9 | 2.8 ± 0.8 | 0.74 |
| ISS | 19 ± 10.7 | 18.6 ± 10.3 | 20.6 ± 11.9 | 0.02 |
| Pneumonia | 4.8 | 4.7 | 5.0 | 0.76 |
Abbreviations: AIS, abbreviated injury scale; ARDS, acute respiratory distress syndrome; CT, computed tomography; MVC, motor vehicle crash; ORIF, open reduction internal fixation; PMVA, pedestrian-motor vehicle accidents; SD, standard deviation.
aValues are presented as mean ± SD or %.
bPrior lung diseases, history of asthma or chronic obstructive pulmonary disease.
The pattern of BCT was predominated by lung contusions (74%), followed by rib fracture (57%), pneumothorax (29%), and hemothorax (23%). Head injuries were reported in 44% of cases. The overall mean ISS was 19 ± 11. Complications such as pneumonia and ARDS were observed in 4.8% and 0.4% cases, respectively.
Table 1 also demonstrates the injury pattern and outcome according to the type of RTA.
There was no significant difference in the pattern of chest injuries between the two groups regarding lung contusions or rib fractures. Patients in the PMVA group had a higher rate of head injury (P = 0.001). Intubation (P = 0.009), injury severity score (P = 0.02) and mortality (P = 0.001) were higher in the PMVA than the MVC group. Tables 2 and 3 show the characteristics of the MVC and PMVA groups according to ISS. Moreover, there was a correlation between chest AIS and ISS (r = 0.35, R2 = 0.125, and adjusted R2 = 0.124; P < 0.001).
Table 2. Patients Demographics, Clinical Presentations and Outcomes in the MVC Group According to Injury Severity Scorea.
| ISS ≤ 15 | ISS > 15 | P Value | |
|---|---|---|---|
| Patients, No. (%) | 341 (44.8) | 421 (55.2) | |
| Mean age, y | 33.4 ± 14.7 | 31.6 ± 14 | 0.09 |
| Male | 87.7 | 95.5 | 0.001 |
| Overall mortality | 2.1 | 19.5 | 0.001 |
| Lung injury | 63 | 83 | 0.001 |
| Rib fracture | 67 | 53 | 0.001 |
| Pneumothorax | 26 | 30 | 0.28 |
| Hemothorax | 16 | 29 | 0.001 |
| Cardiac injury | 1.5 | 2.6 | 0.27 |
| Protective measures used | 0.001 | ||
| Seatbelt only | 24.1 | 10.4 | |
| Airbag + Seatbelt | 3.2 | 1.2 | |
| Airbag Only | 2.1 | 1.2 | |
| Position in vehicle | 0.03 | ||
| Driver | 64.6 | 60.5 | |
| Front passenger | 12.9 | 13.8 | |
| Back passenger | 14.8 | 10.7 | |
| Unknown | 7.7 | 15 | |
| Associated injuries | |||
| Head injury | 17.3 | 60.5 | 0.001 |
| Spleen injury | 5.3 | 16.6 | 0.001 |
| Liver injury | 6 | 20 | 0.001 |
| Kidney injury | 2.1 | 7.6 | 0.001 |
| Interventions | |||
| Exploratory Laparotomy | 1.5 | 10.9 | 0.001 |
| Tracheostomy | 0.6 | 8 | 0.001 |
| Thoracic tube | 8.5 | 28.6 | 0.001 |
| Craniotomy | 0 | 5.2 | 0.001 |
| ORIF | 9 | 22 | 0.001 |
| Intubation | 9.4 | 46.6 | 0.001 |
| Thoracotomy | 0.6 | 2.9 | 0.02 |
| Hospital stay (median) | 4 (1 - 64) | 13 (1 - 186) | 0.001 |
| Chest AIS | 2.5 ± 0.9 | 3 ± 0.8 | 0.001 |
| Pneumonia | 0.9 | 7.8 | 0.001 |
Abbreviations: ARDS, acute respiratory distress syndrome; AIS, abbreviated injury scale; CT, computed tomography; ISS, injury severity score; ORIF, open reduction internal fixation; SD, standard deviation.
aValues are expressed as mean ± SD or %.
Table 3. Patients Demographics, Clinical Presentations and Outcomes in the PMVA Group According to Injury Severity Scorea.
| ISS ≤ 15 | ISS > 15 | P Value | |
|---|---|---|---|
| Patients | 86 (38.2) | 139 (61.8) | |
| Mean age | 30.5 ± 17.6 | 34.7 ± 15 | .06 |
| Male | 92 | 94 | .63 |
| Hospital stay | 6 (1 - 61) | 12 (1 - 168) | .004 |
| Chest AIS | 2.4 ± 1 | 3 ± 0.6 | .001 |
| Pneumonia | 1.2 | 7.9 | .02 |
| Overall mortality | 9.3 | 29.5 | .001 |
| Associated injuries | |||
| Head injury | 32.6 | 68.3 | .001 |
| Lung injury | 71 | 81 | .07 |
| Rib fracture | 49 | 55 | .33 |
| Hemothorax | 20 | 27 | .21 |
| Pneumothorax | 33 | 35 | .75 |
| Cardiac injury | 1.2 | 1.4 | .86 |
| Spleen injury | 6 | 22 | .001 |
| Liver injury | 14 | 22 | .12 |
| Kidney injury | 5.8 | 9.4 | .34 |
| Interventions | |||
| Exploratory laparotomy | 9.3 | 12.2 | .49 |
| Tracheostomy | 0 | 6 | .02 |
| Thoracic tube | 11 | 26 | .007 |
| Craniotomy | 3.5 | 6.5 | .33 |
| ORIF | 11.6 | 18 | .20 |
| Intubation | 16.3 | 51.8 | .001 |
| Thoracotomy | 1.2 | 2.2 | .58 |
Abbreviations: AIS, abbreviated injury scale; CT, computed tomography; ISS, injury severity score; ORIF, open reduction internal fixation; SD, standard deviation.
aValues are presented as mean ± SD or No. (%).
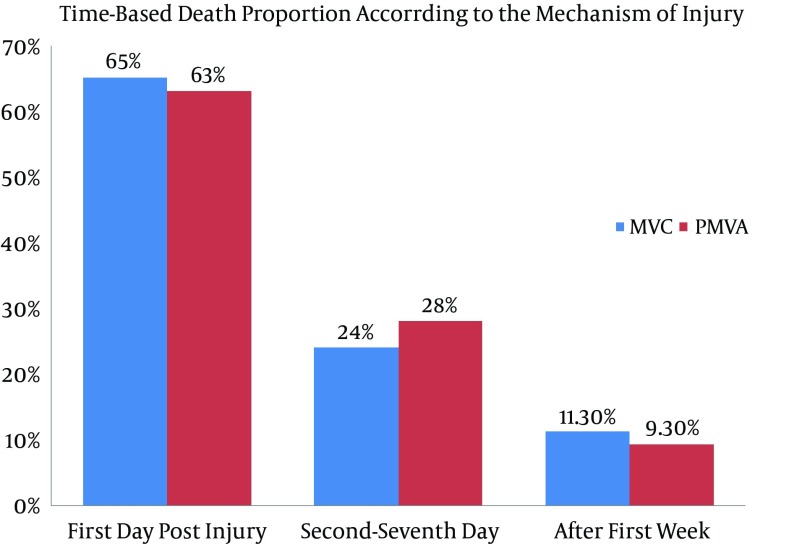
Table 4 and Figure 1 demonstrate BCT in vehicle occupants and pedestrians according to the time of death. The overall mortality was 15% (n = 149), and the highest proportion of mortalities (64%) was observed within the first day post-trauma. A significantly higher proportion of vehicle occupants who died after 7 days had complications such as pneumonia and ARDS (P = 0.001). On the other hand, pedestrians who died between 2 and 7 days post-injury had higher rates of lung contusion and pneumonia.
Table 4. Clinical Presentations and Complications in the MVC and PMVA Group, Stratified by Time of Deatha.
| MVC | PMVA | |||||||
|---|---|---|---|---|---|---|---|---|
| 1st Day | 2nd - 7th Day | > 1 Week | P Value | 1st Day | 2nd - 7th Day | > 1 Week | P Value | |
| Age, y | 31.8 ± 11 | 30.2 ± 13 | 37.6 ± 17.5 | 0.38 | 39.8 ± 21.5 | 34.1 ± 13.3 | 40.4 ± 19.5 | 0.65 |
| Males | 92.3 | 94.7 | 100 | 0.66 | 94 | 100 | 100 | 0.54 |
| Head injury | 71 | 84 | 89 | 0.33 | 71 | 87 | 60 | 0.37 |
| Lung contusion | 69 | 84 | 78 | 0.42 | 47 | 93 | 100 | 0.002 |
| Rib fractures | 46 | 37 | 78 | 0.12 | 41 | 27 | 80 | 0.10 |
| Spleen injury | 5.8 | 15.8 | 22.2 | 0.19 | 18 | 27 | 20 | 0.77 |
| Liver injury | 9.6 | 10.5 | 22.2 | 0.53 | 11.8 | 13.3 | 40 | 0.24 |
| Kidney injury | 5.8 | 0 | 0 | 0.43 | 2.9 | 6.7 | 0 | 0.73 |
| Cardiac injury | 3.8 | 0 | 0 | 0.57 | NA | NA | NA | NA |
| Hemothorax | 25 | 31.6 | 33.3 | 0.78 | 15 | 20 | 40 | 0.39 |
| Pneumothorax | 19 | 37 | 22 | 0.30 | 12 | 40 | 80 | 0.002 |
| ISS | 30.6 ± 13.5 | 31.9 ± 8 | 32.8 ± 11.5 | 0.84 | 25.9 ± 16.6 | 36.5 ± 14.8 | 34.4 ± 9.6 | 0.09 |
| Chest AIS | 4.1 ± 2.2 | 3.3 ± 1.6 | 2.9 ± 0.6 | 0.14 | 3.1 ± 1.4 | 2.9 ± 0.7 | 3.2 ± 0.4 | 0.87 |
| Pneumonia | 0 | 0 | 22.2 | 0.001 | 2.9 | 20 | 0 | 0.08 |
Abbreviations: ARDS, acute respiratory distress syndrome; AIS, abbreviated injury scale; ISS, injury severity score; NA, not available; SD, standard deviation.
aValues are expressed as mean ± SD or No (%).
Figure 1. Time-Based Mortality Among Blunt Chest Traumas Based on the Mechanism of Injury; Motor Vehicle Crash vs. Pedestrian Injury.
Multivariate logistic regression analysis (Table 5) revealed that associated head injury (odds ratio [OR] 2.7; 95% confidence interval (CI) 1.516 - 4.684) and chest AIS (OR 2.0; 95% CI 1.506 - 2.570) and ISS (OR 1.1; 95% CI 1.084 - 1.137) were independent predictors of in-hospital mortality.
Table 5. Predictors of Mortality in Patients with Blunt Chest Injury.
| Variable | P Value | Odds Ratio | 95% Confidence Interval |
|---|---|---|---|
| Age, y | 0.105 | 1.013 | 0.997 - 1.029 |
| Head injury | 0.001 | 2.665 | 1.516 - 4.684 |
| Diaphragmatic injury | 0.092 | 0.217 | 0.037 - 1.280 |
| Injury severity scoring | 0.001 | 1.110 | 1.084 - 1.137 |
| Chest AIS | 0.001 | 1.967 | 1.506 - 2.570 |
| Pneumonia | 0.275 | 0.614 | 0.256 - 1.473 |
| MVC vs. pedestrian injury | 0.082 | 1.577 | 0.943 - 2.636 |
| Thoracotomy | 0.185 | 2.398 | 0.658 - 8.748 |
5. Discussion
This is a unique study from a single center in the Arab Middle East that assesses the clinical presentation and time-based mortality of BCT based on the mode of injury. The majority of RTA victims were young males. In this analysis, lung contusion was the most common type of BCT, followed by rib fracture, which is consistent with other studies (10-12). Earlier studies have reported hemothorax and pneumothorax as the most frequent lesions in BCT (13). Similarly, around one-third of our chest injury cases presented with pneumothorax and one-fourth had hemothorax.
Although seatbelt compliance is the most appropriate mode of minimizing RTA traumatic injuries (11), we have observed a low rate of seatbelt use in our cohort. Studies from Saudi Arabia and UAE have reported consistently lower seatbelt compliance rates among drivers and front-seat passengers (14, 15). Similar to earlier reports (4, 6, 16), the present study observed a higher proportion of extra-thoracic injuries among BCT patients, which possibly increased the risk of complications. The presence of associated head injury is considered a significant predictor of mortality in BCT patients (4, 6). Moreover, injuries of the liver and spleen also increase the risk of mortality by three times (17). In our study, hepatic and splenic injuries accounted for 15% and 12%, respectively.
In our cohort, pedestrians had higher ISS, associated head injury, intubation, and mortality rates than occupants of motor vehicles. Demetriades et al. (18) also observed a significant association of PMVA with higher injury severity and higher incidence of head injury and mortality when compared to other road users. In the present study, the severity of injury was stratified according to the ISS to correlate its impact on the overall outcome. There are few studies that have attempted to correlate the BCT injury severity and outcomes (19, 20). Veysi et al. (21) reviewed 1164 BCT patients and observed that high chest AIS was associated with high overall ISS and mortality. Consistently, in our cohort, both vehicle occupants and pedestrians with severe injuries (ISS > 15) required more acute interventions and prolonged hospital stays, and had higher rates of extra-thoracic injuries, complications, and mortality. Moreover, the present analysis showed a correlation between ISS and chest AIS.
Despite a sharp decline in the rate of pneumonia and ARDS mortality in recent years, these complications still account for a mortality rate of 20% - 43% (22). In our study, pneumonia and ARDS were significantly more common among motor vehicle occupants, particularly among those who died late in the hospital. It is also important to note that the most frequent intrathoracic injury associated with mortality in both MVC and PMVA patients was pulmonary contusion, while head injury constituted the most frequent extrathoracic injury that was closely associated with mortality in both groups of patients. In the multivariate analysis, associated head injury and chest injury AIS in addition to ISS were independent predictors of mortality in MVCs and PMVAs. Also, our findings showed that regardless of the mechanism of RTA, peak mortality was seen within the first day post-trauma, which reflects the severity of injury and prehospital care.
One of the limitations of our study is the retrospective observational design. Alcohol use and the use of seatbelts in motor vehicles were not reported for the entire cohort. Also, we do not have data on the circumstances of the PMVAs, road conditions such as lighting, distance from pedestrian crosswalks, pedestrian overpasses, type of vehicle, or information on the drivers. The rate of seatbelt use could be underestimated, as its documentation was not validated with police data and other sources. The number of deaths may be underestimated, as those who died at the scene were not included in the study. The exact cause of death is also lacking, as no routine post-mortem analysis was feasible. To improve the prediction of outcomes in BCT patients, a validated severity score such as thoracic trauma severity score (TTSS) is required; our data were not complete enough to comply with that. However, TTSS is not the final word in BCT evaluation (23).
In conclusion, chest injuries secondary to RTAs represent one-fifth of the total trauma admissions in Qatar, with a high overall mortality. However, pedestrians are likely to have more severe injuries and higher fatality rates than MVC victims. Specific injury prevention programs focusing on safe driving practices and the safety of road users should be implemented to minimize the incidence of traffic-related chest injuries.
Acknowledgments
This study was conducted with the approval of the medical research center at Hamad Medical Corporation, Qatar (IRB #12010/12).
Footnotes
Authors’ Contribution:All authors contributed to and approved the manuscript.
References
- 1.Demirhan R, Onan B, Oz K, Halezeroglu S. Comprehensive analysis of 4205 patients with chest trauma: a 10-year experience. Interact Cardiovasc Thorac Surg. 2009;9(3):450–3. doi: 10.1510/icvts.2009.206599. [DOI] [PubMed] [Google Scholar]
- 2.O'Connor JV, Adamski J. The diagnosis and treatment of non-cardiac thoracic trauma. J R Army Med Corps. 2010;156(1):5–14. doi: 10.1136/jramc-156-01-02. [DOI] [PubMed] [Google Scholar]
- 3.Liman ST, Kuzucu A, Tastepe AI, Ulasan GN, Topcu S. Chest injury due to blunt trauma. Eur J Cardiothorac Surg. 2003;23(3):374–8. doi: 10.1016/s1010-7940(02)00813-8. [DOI] [PubMed] [Google Scholar]
- 4.Al-Koudmani I, Darwish B, Al-Kateb K, Taifour Y. Chest trauma experience over eleven-year period at al-mouassat university teaching hospital-Damascus: a retrospective review of 888 cases. J Cardiothorac Surg. 2012;7:35. doi: 10.1186/1749-8090-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stitzel JD, Kilgo PD, Weaver AA, Martin RS, Loftis KL, Meredith JW. Age thresholds for increased mortality of predominant crash induced thoracic injuries. Ann Adv Automot Med. 2010;54:41–50. [PMC free article] [PubMed] [Google Scholar]
- 6.El-Menyar A, Latifi R, AbdulRahman H, Zarour A, Tuma M, Parchani A, et al. Age and traumatic chest injury: a 3-year observational study. Eur J Trauma Emerg Surg. 2013;39(4):397–403. doi: 10.1007/s00068-013-0281-7. [DOI] [PubMed] [Google Scholar]
- 7.Mamtani R, Al-Thani MH, Al-Thani AA, Sheikh JI, Lowenfels AB. Motor vehicle injuries in Qatar: time trends in a rapidly developing Middle Eastern nation. Inj Prev. 2012;18(2):130–2. doi: 10.1136/injuryprev-2011-040147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Asim M, El-Menyar A, Al-Thani H, Abdelrahman H, Zarour A, Latifi R. Blunt traumatic injury in the Arab Middle Eastern populations. J Emerg Trauma Shock. 2014;7(2):88–96. doi: 10.4103/0974-2700.130878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abdulrazzaq H, Zarour A, El-Menyar A, Majid M, Al Thani H, Asim M, et al. Pedestrians: the daily underestimated victims on the road. Int J Inj Contr Saf Promot. 2013;20(4):374–9. doi: 10.1080/17457300.2012.748811. [DOI] [PubMed] [Google Scholar]
- 10.Al-Hassani A, Afifi I, Abdelrahman H, El-Menyar A, Almadani A, Recicar J, et al. Concurrent rib and pelvic fractures as an indicator of solid abdominal organ injury. Int J Surg. 2013;11(6):483–6. doi: 10.1016/j.ijsu.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 11.Abdulrahman H, Afifi I, El-Menyar A, Al-Hassani A, Almadani A, Al-Thani H, et al. Clinical outcomes of multiple rib fractures: does age matter? Eur J Trauma Emerg Surg. 2013;39(6):605–11. doi: 10.1007/s00068-013-0291-5. [DOI] [PubMed] [Google Scholar]
- 12.Murkey P, Nagrale N, Tirpude B, Wankhade P, Patond S. Pattern Of Chest Injuries In Fatal Vehicular Accidents In Central India. J Forensic Med Sci Law. 2012;21. [Google Scholar]
- 13.Hanafi M, Al-Sarraf N, Sharaf H, Abdelaziz A. Pattern and presentation of blunt chest trauma among different age groups. Asian Cardiovasc Thorac Ann. 2011;19(1):48–51. doi: 10.1177/0218492310395954. [DOI] [PubMed] [Google Scholar]
- 14.Bendak S. Seat belt utilization in Saudi Arabia and its impact on road accident injuries. Accid Anal Prev. 2005;37(2):367–71. doi: 10.1016/j.aap.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 15.Abu-Zidan FM, Abbas AK, Hefny AF, Eid HO, Grivna M. Effects of seat belt usage on injury pattern and outcome of vehicle occupants after road traffic collisions: prospective study. World j surg. 2012;36(2):255–9. doi: 10.1007/s00268-011-1386-y. [DOI] [PubMed] [Google Scholar]
- 16.Emircan S, Ozguc H, Akkose Aydin S, Ozdemir F, Koksal O, Bulut M. Factors affecting mortality in patients with thorax trauma. Ulus Travma Acil Cerrahi Derg. 2011;17(4):329–33. [PubMed] [Google Scholar]
- 17.Kulshrestha P, Munshi I, Wait R. Profile of chest trauma in a level I trauma center. J Trauma Acute Care Surg. 2004;57(3):576–81. doi: 10.1097/01.TA.0000091107.00699.C7. [DOI] [PubMed] [Google Scholar]
- 18.Demetriades D, Murray J, Martin M, Velmahos G, Salim A, Alo K, et al. Pedestrians injured by automobiles: relationship of age to injury type and severity. J Am Coll Surg. 2004;199(3):382–7. doi: 10.1016/j.jamcollsurg.2004.03.027. [DOI] [PubMed] [Google Scholar]
- 19.Pape HC, Remmers D, Rice J, Ebisch M, Krettek C, Tscherne H. Appraisal of early evaluation of blunt chest trauma: development of a standardized scoring system for initial clinical decision making. J Trauma. 2000;49(3):496–504. doi: 10.1097/00005373-200009000-00018. [DOI] [PubMed] [Google Scholar]
- 20.Richter M, Krettek C, Otte D, Wiese B, Stalp M, Ernst S, et al. Correlation between crash severity, injury severity, and clinical course in car occupants with thoracic trauma: a technical and medical study. J Trauma. 2001;51(1):10–6. doi: 10.1097/00005373-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Veysi VT, Nikolaou VS, Paliobeis C, Efstathopoulos N, Giannoudis PV. Prevalence of chest trauma, associated injuries and mortality: a level I trauma centre experience. Int Orthop. 2009;33(5):1425–33. doi: 10.1007/s00264-009-0746-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leenen L, Beenen L, Aukema T, Hietbrink F. Validation of the Thorax Trauma Severity Score for mortality and its value for the development of acute respiratory distress syndrome. Open Access Emerg Med. 2011;3:49–53. doi: 10.2147/OAEM.S22802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barlow M, Prince JM. Predicting outcomes in the setting of blunt thoracic trauma. J Surg Res. 2013;183(1):100–1. doi: 10.1016/j.jss.2012.04.025. [DOI] [PubMed] [Google Scholar]