Abstract
Background:
Sickle cell disease (SCD) is a major public health problem in Nigeria. Carrier prevalence is about 25% and it affects about 2 - 3% of the Nigerian population. The disease runs a chronic course, characterized by recurrent ill-health, progressive organ damage and shortened life-span. There is a need for SCD control through public education and other preventive measures.
Objective:
This study aimed at assessing the level of knowledge regarding SCD among a cross-section of new tertiary graduates in Nigeria, as well as factors influencing their knowledge. It also describes their attitudes and patterns of control practices engaged by the respondents regarding SCD.
Method:
This was an analytic, cross-sectional study among 370 new tertiary graduates (youth corps members) in Benin City, Nigeria. Bio-data, data on knowledge, their attitude and control practices of sickle cell disease were obtained using a structured questionnaire. Association between the mean level of knowledge and other variables such as age, gender, course of study, etc were tested using one way analysis of variance.
Results:
Most of the study participants were aged 22 - 29 years. A large proportion (63.5%) of the respondents was females. Only 17.8% of the respondents had a good knowledge of SCD despite high level of awareness (98.4%). Those who studied courses related to medical sciences had significantly higher mean knowledge score. About 94.6% of the respondents knew their SCD carrier status and 80.8% were willing to avoid carrier marriages. Only 38.1% will accept prenatal diagnosis/selective abortion if locally available.
Conclusion:
Most participants demonstrated moderate level of public health knowledge regarding SCD in Nigeria. Considering the relative lack of prenatal diagnostic services, low acceptability of selective abortion among the respondents, sub-optimal care of affected persons and poor access to haemopoeitic stem cell transplantation (HSCT) in our environment, stronger efforts should be directed and sustained at primary prevention through public education and screening regarding SCD.
Keywords: Knowledge, Attitude and practice, Sickle cell disease, New tertiary graduates, Youth corps members.
INTRODUCTION
Sickle cell disease (SCD) is one of the commonest monogenetic diseases worldwide.1,2 Its greatest burden lies mainly in Sub-Saharan Africa, Mediterranean regions, Middle East and South-East Asia.3,4 In Nigeria, about 20 to 30% of the population are carriers of the sickle cell trait.3,5,6 Sickle cell disease affects about 2 to 3% of the Nigerian population.6,7
Sickle cell disease is an inherited haemolytic anaemia that results from homozygous or compound heterozygous inheritance of the sickle haemoglobingene.8 It is characterized by the tendency of sickle haemoglobin to polymerise and deform the red cell to a sickle or crescent shape, thereby resulting in a characteristic vaso-occlusive phenomenon, chronic haemolysis and progressive organ damage.8 Sickle haemoglobinopathies have different genotypes. The archetypal sickle cell disease is the Haemoglobin SS disease, otherwise called sickle cell anaemia. Other sickle cell disease phenotypes include the compound heterozygous states such as haemoglobin SC disease and Haemoglobin S-Thalassemia syndromes.8,9 In sickle cell disease, there is a marked inter- and intra-individual variability in terms of disease manifestations. Disease manifestation may begin as early as 6 months of life, which coincides with the switch of fetal haemoglobin to adult Haemoglobins.9
Regarding treatment of SCD, a few disease modifying interventions are currently in use. Routine general prophylactic and other corrective measures has led to a marked improvement in life expectancy and quality of life among sickle cell disease patients in developed nations. However, in Nigeria, available evidence suggest that care of affected persons is largely sub-optimal.10 Haemopoietic stem cell transplantation (HSCT) is the only potentially curative therapy for sickle cell disease. This form of therapy is often limited to selected patients with severe disease who have a matched sibling donor and are aged less than 17 years.11,12 However, this form of treatment is either locally unavailable or unaffordable by eligible patients in Nigeria. Other local challenges with HSCT include lack of sufficient local expertise, inadequate health infrastructure, lack of political will and low socio-economic status of the patients.13 Other recognized practices in the treatment of sickle cell disease such as hydroxyurea therapy and chronic blood transfusions are also faced with challenges such as inefficient blood banking services and high cost of treatment.14,15 Without any reasonable intervention, life expectancy is significantly reduced as a result of the numerous life-threatening acute complications as well as chronic morbidities associated with the disease8,9 SCD therefore places a major psychological, financial and social burden on patients, their care-givers and society at large. Furthermore, there are very few centres with facilities for prenatal diagnosis in Nigeria.24 Suffice to say that current control measures of sickle cell disease in Nigeria are palpably meager in the face of the enormous burden of this disease.
There is a pressing need to focus on primary prevention of SCD through public health education and other control measures. Good knowledge regarding SCD is required for individuals especially carriers to make informed decisions about their reproductive life and other health related choices. As well, the burden of social stigma regarding SCD is reduced. This study therefore seeks to evaluate the extent of health knowledge of sickle cell disease among a cross-section of recent tertiary graduates in Nigeria, as well as their attitude to sickle cell disease. It also seeks to explore current practices engaged in the control of SCD in the study population. The association between their level of knowledge and different socio-economic groups, their sources of information and haemoglobin phenotype status were also investigated.
METHODOLOGY
Study Design
This was a cross-sectional, analytic study carried out among a cohort of recent tertiary graduates during their National Youth Service Corps (NYSC) in Benin City, Edo state, Nigeria. The study was conducted over a three month period between April and June, 2014.
Study Area and Study Population
Benin City is a cosmopolitan city in Edo State, South-South Nigeria, comprising three local government areas (LGAs), namely Oredo, Egor and Ikpoba-Okha LGAs. NYSC is a national scheme established by the Federal Government in May, 1973 with a view to properly encourage and develop common ties among the youths of Nigeria and the promotion of national unity.16 Each year, eligible Nigerian graduates from universities and polytechnics all over the world are enrolled into this compulsory scheme for a period of one year. Annually, thousands of Nigerian graduates from various citadels of higher learning are mobilized out of their geopolitical zones in three batches, batch A, B and C. The main segments of the service year include the orientation program, primary assignment, community development service (CDS) and winding-up/passing out. For the purpose of this study, the subjects included a section of new tertiary graduates that were deployed by NYSC to Benin City, Edo state to undertake this one year service to the nation.
Sample Size
Sample size for this study was estimated using this formula for cross-sectional surveys: N = (z2pq)/d2 Where N = minimum sample size, z = standard normal deviate (1.96), p = 0.253 (Olatona et al 2012 found that 25.3% had good knowledge of SCD among youth corps members in Lagos).17
q = 1 - p, 0.747
d = degree of precision to be used (0.05)
The minimum sample size (n) for this study was estimated to be 290.41 ~ 290. A larger sample size was accommodated. Four hundred and five (405) questionnaires were distributed, expecting a minimum response rate of 90%.
Data Collection and Analysis
Data was collected in each of the three local government areas (LGAs) in Benin City using a structured interviewer-administered questionnaire. Only graduates who voluntarily gave consent were allowed to participate in the study. Questionnaires were administered to a convenient sample of 135 corps members in each of the three LGAs in Benin City during their joint monthly CDS Programme. A total of 405 questionnaires were distributed. Effort was made to collect the filled questionnaires at the same time in order to ensure optimal compliance. Three hundred and ninety two (392) questionnaires were retrieved and 22 were invalidated due to wrong/incomplete entries. Three hundred and seventy (370) valid questionnaires were subjected to statistical analysis. The questionnaire elicited data on their socio-demographic parameters, knowledge, attitude and practices related to control of sickle cell disease in different sections. Respondents' age, gender, course of study, marital status, religion were captured in the socio-demographic section. Section on knowledge elicited responses on aetiology, disease manifestations, control measures and treatment of sickle cell disease. Structured closed ended questions offering trichotomous choices of 'yes', 'no' and 'I don't know' were used in the knowledge section. Respondents' attitude were assessed on a three point scale including responses such as 'agree', 'disagree' and 'not decided'. The questionnaire was pretested among 20 randomly selected undergraduates of the University of Benin Main Campus, Benin City.
In order to facilitate data analysis, each of the 24 questions in the knowledge section were scored as 1 for 'yes' response, and 0 for 'no/I don't know' response, giving an aggregate score of 24. A score of 0 - 8 was considered poor knowledge, 9 - 16 was considered fair knowledge, while 17 - 24 was considered good knowledge. Data were inputed and analyzed using Statistical Package for Social Sciences (SPSS) version 16. Descriptive and inferential analysis were performed and presented as frequency counts and percentages in tables. The mean SCD knowledge scores were compared between groups using one way analysis of variance (ANOVA). Probability value less than 0.05 was considered statistically significant.
Approval
Permission to conduct the study was duly obtained from the office of Zonal NYSC Inspector in Benin City. Written consent was also obtained from each respondent after detailed explanation of the intended study and assurance of confidentiality.
RESULTS
Socio-Demographic Data:
A total of 370 duly completed questionnaires were used to represent the study population. The modal age of the respondents was 26 - 29 years (Table 1) . Female gender was more frequent, accounting for 63.5% of the respondents. About a quarter (24.9%) of the respondents were married while most other respondents (74.9%) were single. Of the studied population, 23.2% studied courses related to management sciences and 15.7% studied physical sciences (Table 1). Most (86.5%) of the respondents were Christians (Table 1).
Table 1:
Socio-Demographic Characteristics of the Respondents
| Age(years) | Frequency (n) | Percentage (%) |
|---|---|---|
|
| ||
| 18 – 21 | 19 | 5.1 |
| 22 – 25 | 150 | 40.5 |
| 26 – 29 | 168 | 45.4 |
| 30 – 32 | 24 | 6.5 |
| >32 | 9 | 2.4 |
| Marital status | ||
| Single | 277 | 74.9 |
| Married | 92 | 24.9 |
| Other | 1 | 0.3 |
| Sex | ||
| Male | 135 | 36.5 |
| Female | 235 | 63.5 |
| Religion | ||
| Christianity | 320 | 86.5 |
| Islam | 44 | 11.9 |
| Others | 6 | 1.6 |
| Faculty | ||
| Life sciences | 37 | 10.0 |
| Physical sciences | 58 | 15.7 |
| Arts | 35 | 9.5 |
| Engineering | 27 | 7.3 |
| Management | 86 | 23.2 |
| Social sciences/law | 38 | 10.3 |
| Medical sciences | 35 | 9.5 |
| Education | 22 | 5.9 |
| Enviro/agricultural | 32 | 8.6 |
Total (n) = 370 (100%)
Awareness of Sickle Cell Disease (SCD) and Haemopoietic Stem Cell Transplantation (HSCT).
Most (98.4%) of the respondents had heard about sickle cell disease (Table 2). The main channel of information (45.9%) was health talks/mass media (Table 3). About a quarter (23.2%) of the respondents claimed to have affected relations or friends. Only 14.1% of the respondents had some form of formal learning about SCD. About a quarter (22.4%) of the respondents are aware of the availability of HSCT in Benin City, Nigeria (Table 2).
Table 2:
Awareness of SCD and HSCT
| Awareness | Frequency(n) | Percentage (%) |
|---|---|---|
|
| ||
| Level of awareness on sickle cell disease | ||
| Yes | 364 | 98.4 |
| No | 6 | 1.6 |
| Level of awareness about HSCT in Benin City | ||
| Yes | 83 | 22.4 |
| No | 287 | 77.6 |
Total (n) = 370 (100%)
Table 3:
Respondent's level of knowledge and source of knowledge about SCD
| Variable | Frequency(n) | Percentage (%) |
|---|---|---|
|
| ||
| Level of Knowledge | ||
| 0 – 8 (poor) | 69 | 18.6 |
| 9 – 16 (fair) | 235 | 63.5 |
| 17 – 24 (good) | 66 | 17.8 |
| Mean knowledge score = 12.49 ± 4.75 | ||
| Source of Knowledge | ||
| Literature | 51 | 13.8 |
| Health talks | 170 | 45.9 |
| Affected persons | 86 | 23.2 |
| Formal learning | 52 | 14.1 |
| Others | 5 | 1.4 |
| Unaware | 6 | 1.6 |
N =370 (100%)
Knowledge of Sickle Cell Disease
Most of the respondents (63.5%) had a fair knowledge of sickle cell disease (Table 3). Only 49(17.8%) of the respondents had good knowledge of SCD. The mean knowledge score among the respondents is 12.49 ± 4.75.
Attitude and Control Practices of Sickle Cell Disease
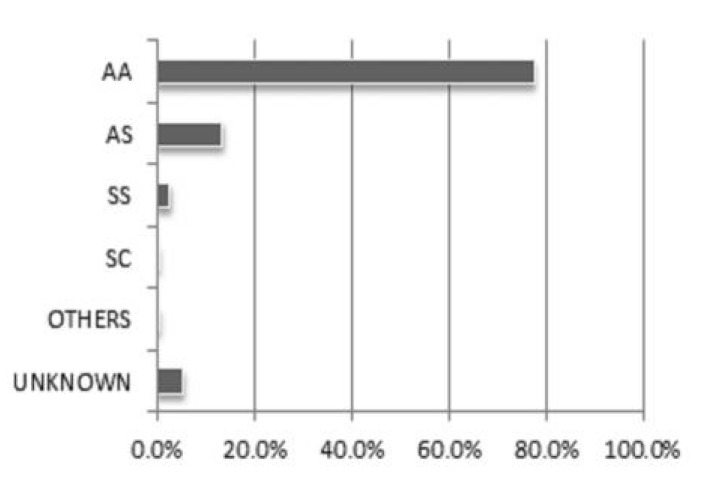
Majority (94.6%) of the respondents knew their haemoglobin genotype status (SCD carrier status). The commonest reason/indication for checking their carrier status was school entry (32.7%) (Table 4). Other indications for carrier status check included personal curiosity (18.1%), medical doctor's request (17.8%) and pre-marital screening (13.2%). Seven percent (7%) of the respondents claimed to have been screened for SCD at infancy. The most reported haemoglobin variant among the study participants was AA (77.6%), followed by AS (13.5%) (Figure 1) and 3% had sickle cell disease. Two respondents (0.5%) indicated other phenotypes while 5.4% of the respondents did not know their carrier status (Figure 1).
Table 4:
Reasons for checking haemoglobin phenotypes
| Distribution | Frequency (n) | Percentage (%) |
|---|---|---|
|
| ||
| Distribution of Haemoglobin Phenotypes | ||
| AA | 287 | 77.6 |
| AS | 50 | 13.5 |
| SS | 10 | 2.7 |
| SC | 1 | 0.3 |
| Others | 2 | 0.5 |
| Unknown | 20 | 5.4 |
| Reasons/Modalities for Carrier Status Check | ||
| Infancy | 26 | 7.0 |
| School entry | 121 | 32.7 |
| Pre-employment | 12 | 3.2 |
| Doctors request | 66 | 17.8 |
| Curiosity | 67 | 18.1 |
| Pre-marital testing | 49 | 13.2 |
| Others | 9 | 2.4 |
| Unknown | 20 | 5.4 |
Total (n) = 370 (100%)
Figure 1:
Distribution of Haemoglobin Phenotypes
A few (8.6%) of the respondents expressed willingness to marry another sickle cell trait carrier despite the risk of raising children with sickle cell disease (Table 5). Most of the respondents (80.8%) were unwilling to take such actions, while remaining 10.5% were undecided. Only 38.1% of the respondents will opt for termination of pregnancy compared to 49.5% who will allow the pregnancy to continue if they discovered their unborn child had sickle cell disease, remaining 12.4% indicated other responses such as to seek spiritual help/healing, opt for HSCT and others were undecided as at the time of the study. About fifty five percent of the respondents agreed to the use of legislation against marital union between trait carriers to prevent further births of SCD babies (Table 5). About 34% of the respondents thought that selective abortion of babies prenatally diagnosed with sickle cell disease should be encouraged by law.
Table 5:
Respondents' attitude to sickle cell disease
| Questions on Attitude | Frequency (n) | Percentage (%) |
|---|---|---|
|
| ||
| Knowledge of own haemoglobin genotype status | ||
| Yes | 350 | 94.6 |
| No | 20 | 5.4 |
| Willingness to marry another carrier partner despite knowing risk of SCD Births | ||
| Yes | 32 | 8.6 |
| No | 299 | 80.8 |
| I don’t know | 39 | 10.5 |
| Response to your unborn baby following prenatal diagnosis of SCD | ||
| Abortion | 141 | 38.1 |
| Allow pregnancy | 183 | 49.5 |
| Undecided | 46 | 12.4 |
| Legislation against marriage union between two SCD trait carriers | ||
| Agree | 202 | 54.6 |
| Disagree | 102 | 27.6 |
| Undecided | 66 | 17.8 |
| Abortion of an unborn SCD Baby should be encouraged by law | ||
| Agree | 124 | 33.5 |
| Disagree | 174 | 47.0 |
| Undecided | 72 | 19.5 |
Total (n) = 370 (100%)
Studying a medically related course and being exposed to formal learning/teaching about sickle cell disease was significantly associated with good knowledge of sickle cell disease (p value < 0.001) (Table 6). Interestingly, the mean knowledge score among the respondents increased with age but was not found to be statistically significant (p = 0.179). Being married was associated with higher knowledge (p = 0.017).
Table 6:
Comparison of level of knowledge within different groups
| Variables | Frequency(n) | Mean Scores | SD |
|---|---|---|---|
|
| |||
| Age(in years) | |||
| 18 – 21 | 19 | 10.53 | 4.02 |
| 22 – 25 | 150 | 12.11 | 4.55 |
| 26 – 29 | 168 | 12.96 | 4.89 |
| 30 – 32 | 24 | 12.96 | 5.14 |
| >32 | 9 | 13.22 | 4.82 |
| Df = 4, F = 1.58, p-value = 0.179 | |||
| Marital Status | |||
| Single | 277 | 12.16 | 4.56 |
| Married +Other | 93 | 13.51 | 5.14 |
| Df = 1, F = 5.800, p-value = 0.017 | |||
| Sex | |||
| Male | 135 | 11.96 | 4.65 |
| Female | 235 | 12.81 | 4.78 |
| Df = 1, F = 2.78, p-value = 0.096 | |||
| Religion | |||
| Christianity | 320 | 12.68 | 4.83 |
| Islam | 44 | 11.41 | 4.12 |
| Others | 6 | 10.67 | 3.01 |
| Df = 2, F = 1.852, p-value = 0.158 | |||
| Faculty | |||
| LifeScience | 37 | 14.29 | 5.29 |
| Physical Science | 58 | 12.31 | 3.91 |
| Arts | 35 | 13.09 | 4.55 |
| Engineering | 27 | 11.41 | 3.57 |
| Management | 86 | 11.41 | 4.08 |
| SocialScience/Law | 38 | 10.47 | 5.35 |
| MedicalSciences | 35 | 18.31 | 4.09 |
| Education | 22 | 11.45 | 3.47 |
| Environmental/Agric | 32 | 10.72 | 3.47 |
| Df = 8, F = 11.893, p-value = 0.000 | |||
| Haemoglobin Phenotypes | |||
| AA | 287 | 12.75 | 4.59 |
| AS | 50 | 11.48 | 5.24 |
| SS + SC | 11 | 14.91 | 4.50 |
| Others | 2 | 9.50 | 6.36 |
| Unknown | 20 | - | - |
| Df = 3, F = 2.221, p-value = 0.085 | |||
| Source of Knowledge | |||
| Literature | 51 | 12.55 | 4.08 |
| Health talks | 170 | 11.61 | 4.37 |
| Affected persons | 86 | 12.06 | 3.86 |
| Formal learning | 52 | 17.21 | 4.75 |
| Others | 5 | 9.20 | 3.49 |
| Unaware | 6 | - | - |
| Df = 4, F = 18.670, p-value = 0.000 | |||
Mean knowledge score of the respondents = 12.49 ± 4.75, Total (N) = 370 (100%)
DISCUSSION
About 95% of the study participants had heard about SCD, suggesting a good level of awareness. Their sources of information about SCD had significant impact on their extent of knowledge. Participants who were exposed to formal education about SCD through medical sciences had higher knowledge scores. Establishment of designated training and genetic counseling centers on SCD with adequate resource staff will prove effective in improving public health knowledge about SCD especially among the trait carriers. When compared, the knowledge of SCD among normal (haemoglobin AA) individuals, trait carriers (haemoglobin AS), affected persons (haemoglobin SS + SC) and others (such as Haemoglobin AC) were not significantly different.
World Health Organization (WHO) recommends that in areas where haemoglobin disorders are common, special dedicated centers are required, in appropriate numbers, appropriately situated, and with a high degree of autonomy.18 Currently in Nigeria, there are very few specialized centers with multi-specialist team dedicated to the care of persons with sickle cell disease. WHO also advocates carrier detection and genetic counseling.18, 19 Carrier detection and genetic counseling are reported to be effective in control of thalassemia in countries such as Cyprus and Iran.20-22 However, none of the respondents indicated genetic counseling centres as their source of knowledge about SCD. This may partly be explained by the relative absence of genetic counseling services in the nation.
In Nigeria, newborn screening programme for SCD is underdeveloped. This may explain why about 7% reported to have had some form of screening for SCD during infancy. Unavailability of neonatal screening is associated with significant delay in diagnosis and prompt institution of treatment in affected persons. A recent report in Lagos revealed mean age at diagnosis among children with sickle cell disease to be 27.3 months, a quarter of the children were diagnosed before infancy and three-quarters before three years of age.23 Those who have a relatively mild disease might not even be diagnosed until later life.
Participants who were older and married had a better knowledge of sickle cell disease. This may be due to the fact that advancing age and marriage confers greater societal responsibility.
School entry, followed by a doctor's request and pre-marital screening were observed to be the commonest indication for carrier status check. Doctors in student environment should endeavor to communicate the results of carrier screening with clients, as well as educate them on its implications. Marriage registries and religious bodies involved in marital rites should also be supported.
Approximately 95% of the respondents knew their SCD carrier status, suggesting a good attitude towards prevention and control of the sickle cell disease. A significant proportion (80.8%) of the respondents was averse to union of trait carriers, also suggesting a positive attitude. SCD carrier prevalence rate in Nigeria is about 20 to 30%. In this study, 13.5% of the respondents were carriers. The difference observed may be related to a possible over-reporting of normal haemoglobin status (AA) due to social desirability or perhaps erroneous reports generated from sub-standard medical laboratories. However, large epidemiologic survey will be needed to continually evaluate carrier prevalence of SCD in Nigeria. Nwogoh et al observed a carrier prevalence rate of about 23% in Benin City in 2013.7
The option of prenatal diagnosis and selective abortion was also explored in this study group. It was observed that about half of the respondents (49.5%) were averse to termination of an affected pregnancy while 38.1% will agree to selective abortion if permitted by law and locally available. However, their reasons for deterrence may be related to observations in other studies including religious beliefs and fear of complications as observed by Durosinmi et al in Ile-Ife.25 Similarly, Adeyemi et al reported a low acceptance of selective abortion among health workers in Ogbomosho. Only 21.4% of the doctors would accept early termination of affected pregnancy, 32.0% of nurses and 32.3% of the other health workers would accept termination of affected pregnancy.26 According to another survey among health professionals and students in North-East Nigeria, Kagu et al observed that 53% would not terminate pregnancy by abortion of PND confirmed SCD baby in the first trimester.27 Currently in Nigeria, abortion is illegal. Apart from relatively low acceptance rate in Nigeria, the cost of pre-natal diagnosis in Nigeria may be unaffordable to the average Nigerian couples who may require such services. In 2009, Oladapo et al estimated the cost of Chorionic villi sampling and amniocentesis in Nigeria to be about 1290 US Dollars.28 The cost of PND, low awareness and poor access may be challenges to its utilization in Nigeria.
Compared to Benin City with awareness level of 22%, awareness of the practice of HSCT might even be lower in other parts of the country where HSCT is not been practiced.29 Previous studies have also suggested the need for continuous medical education for health professionals on the diagnosis, clinical features, management, treatment and control of sickle cell disease. 30
Though 54.6% of the respondents agree that legislation against carrier marriages might be engaged in SCD control in Nigeria, use of punitive measures in control of thalassemia in Greece gave disappointing results, as it lead to increase anxiety, stigmatization, denial and falsification of records.21 Cost benefit analysis of prevention versus treatment of a similar genetic disease such as thalassemia showed that prevention is cheaper and more effective.21 Primary preventive measures such as avoidance of carrier marriages/pregnancies through health education, population screening, carrier detection, genetic counseling and pre-conceptual/pre-implantation diagnosis should be given greater emphasis in control of SCD in Nigeria.
CONCLUSION
Most participants demonstrated a moderate level of knowledge regarding sickle cell disease and its control in Nigeria. Similar studies are needed to evaluate the SCD knowledge and control among the less educated or educationally disadvantaged Nigerians. Stronger efforts should be directed at public health education to improve general knowledge and forge positive attitudes and practices in SCD control. General studies on sickle cell disease and other challenging tropical diseases should be introduced into school curricula and the NYSC programme.
In the absence of a fully functional nationwide programme, major health institutions may create local policies and programmes for newborn screening of sickle haemoglobinopathies. Premarital couple screening by religious bodies/marriage registries and antenatal screening of mothers should be strengthened. The option of prenatal diagnosis and selective abortion may also be explored. Medical doctors and other health professionals should at every opportunity request haemoglobin genotype check on patients/clients with unknown haemglobin phenotype status, especially sick children.
Government attention should be diverted to provision of comprehensive sickle cell centers with the capacity to render multi-specialist care at subsided rates for its affected populace. In addition, health care providers involved in the treatment of SCD should continually undergo continuous professional education and development in order to optimize their knowledge and skills.
ACKNOWLEDGEMENT
The authors are grateful to all corps members who participated in this study.
REFERENCES
- 1.Weatherall DJ, Clegg JB. Inherited haemoglobin disorders: An increasing global health problem. Bull World Health Organ. 2001;79(8):704–712. [PMC free article] [PubMed] [Google Scholar]
- 2.Modell B, Darlison M. Global epidemiology of haemoglobin disorders and derived service indicators. Bull World Health Organ. 2008;86(6):480–487. doi: 10.2471/BLT.06.036673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Updated estimates of the frequency of the haemoglobin disorders in each country. www.who.ch/programmes/ncd/hgm/haemogl.htm . [accessed May 2001].
- 4.Serjeant GR. Sickle-cell disease. Lancet . 1997;350(9079):725–730. doi: 10.1016/S0140-6736(97)07330-3. [DOI] [PubMed] [Google Scholar]
- 5.Serjeant GR, Sergent BE. The epidemiology of sickle cell disorder: A challenge for Africa. Arch Ibadan Med . 2001;2(2):4–52. [Google Scholar]
- 6.Fleming AF, Storey J, Molineaux L, et al. Abnormal haemoglobins in the Sudan savanna of Nigeria. I. Prevalence of haemoglobins and relationships between sickle cell trait, malaria and survival. Ann Trop Med Parasitol . 1979;73: 161–172. doi: 10.1080/00034983.1979.11687243. [DOI] [PubMed] [Google Scholar]
- 7.Nwogoh B, Adewoyin AS, Iheanacho OE, Bazuaye GN. Prevalence of haemoglobin variants in Benin City, Nigeria. Ann. Biomed. Sci. June. 2012; 11(2):60–64. [Google Scholar]
- 8.Lal A, Vinchinsky EP. Sickle cell disease. In: Hoffbrand AV, Catovsky D, Tuddenham EGD, Green AR, editors. Postgraduate Haematology. 6 ed. Vol. 7. Blackwell Publishing Ltd; 2011. pp. 109–125. [Google Scholar]
- 9.Beutler E. Disorders of haemoglobin structure: sickle cell anaemia and related abnormalities. In: Marshall A. Lichtman , et al., editors. Williams Haematology. Vol. 47. McGraw-Hill; 2006. pp. 667–700. [Google Scholar]
- 10.Galadanci N, Wudil BJ, Balogun TM, et al. Current sickle cell disease management practices in Nigeria. Int Health (online) 2013. [DOI] [PMC free article] [PubMed]
- 11.Roberts I. Current status of allogeneic transplantation for haemoglobinopathies. Br J Haematol. 1997;98:1–7. doi: 10.1046/j.1365-2141.1997.1332948.x. [DOI] [PubMed] [Google Scholar]
- 12.Abboud MR. Hematopoietic Stem Cell Transplantation for Adults with Sickle Cell Disease. N Engl J Med. 2009;361(24):2380–2381. doi: 10.1056/NEJMe0908574. [DOI] [PubMed] [Google Scholar]
- 13.Oyekunle AA. Haemopoietic Stem Cell Transplantation: prospects and challenges in Nigeria. Annals of Ibadan Postgraduate Medicine. 2006;4(1):17–27. [Google Scholar]
- 14.Davies SC, Gilmore A. The role of hydroxyurea in the management of sickle cell disease. Blood Reviews (online) . 2003;17:99–109. doi: 10.1016/s0268-960x(02)00074-7. [DOI] [PubMed] [Google Scholar]
- 15.Win N. Iheanyi E Okpala. Practical management of Haemoglobinopathies . Blackwell Publishing; 2004. Blood transfusion therapy for Haemoglobinopathies; pp. 99–106. [Google Scholar]
- 16.http://www.nysc.gov.ng/history2.php .
- 17.Olatona FA, Odeyemi KA, Onajole AT, Asuzu MC. Effects of Health Education on Knowledge and Attitude of Youth Corps Members to Sickle Cell Disease and its Screening in Lagos State. J Community Med Health Educ (online) . 2012;2(163) [Google Scholar]
- 18.World Health Organisation Guidelines for the control of haemoglobin disorders. Sardinia. WHO . 1994.
- 19.Sickle Cell Anaemia. Agenda item 11.4. In: 59th World Health Assembly, 27 May 2006. WHA 59.20. Available from: http://www.who.int/gb/e b w h a/p d f _ f i l e s/W H A 5 9 - R E C 1/e/WHA59_2006_REC1-en.pdf . [Last accessed on 6th February, 2008]. p. [p. 26].
- 20.Angastiniotis MA, Hadjiminas MG. Prevention of Thalassaemia in Cyprus. Lancet. 1981;1: 369 –370. doi: 10.1016/s0140-6736(81)91682-2. [DOI] [PubMed] [Google Scholar]
- 21.Angastiniotis M, Kyrikidou S, Hadjiminas M. How Thalassaemia was controlled in Cyprus. World Health Forum . 1986;7: 291–297. [Google Scholar]
- 22.Miri M, Tabrizi Namini M, Hadipour Dehshal M, et al. Thalassemia in Iran in Last Twenty Years: the Carrier Rates and the Births Trend. Iranian Journal of Blood and Cancer. 2013;6(1):11–18. [Google Scholar]
- 23.Akodu F, Diaku-Akinwumi IN, Njokanma OF. Age at diagnosis of sickle cell anaemia in Lagos, Nigeria. Mediterr J Hematol Infect Dis. 2013;5(1) doi: 10.4084/MJHID.2013.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Adewole TA, Olukosi YA, Disu F, et al. Application of polymerase chain reaction to the prenatal diagnosis of sickle cell anaemia in Nigeria. West Afr J Med. 1999;18:160–164. [PubMed] [Google Scholar]
- 25.Durosinmi MA, Odebiyi AI, Adediran IA, Akinola NO, et al. Acceptability of prenatal diagnosis of sickle cell anaemia (SCA) by female patients and parents of SCA patients in Nigeria. Soc Sci Med. 1995;41(3):433–436. doi: 10.1016/0277-9536(94)00361-v. [DOI] [PubMed] [Google Scholar]
- 26.Adeyemi AS, Adekanle DA. Knowledge and attitude of female health workers towards prenatal diagnosis of sickle cell disease. Nigerian Journal of Medicine. 2007;16(3):268–270. [PubMed] [Google Scholar]
- 27.Kagu MB, Abjah UA, Ahmed SG. Awareness and acceptability of prenatal diagnosis of sickle cell anaemia among health professionals and students in North Eastern Nigeria. Niger J Med. 2004;13(1):48–51. [PubMed] [Google Scholar]
- 28.Oladapo OT. The WHO Reproductive health library. Geneva: World Health Organization; Amniocentesis and chorionic villus sampling for prenatal diagnosis: RHL commentary. (last revised: 1 April 2009) [Google Scholar]
- 29.Bazuaye GN, Nwogoh B, Ikponwen D, et al. First successful allogenic haemopoietic stem cell transplantation for a sickle cell disease patient in a low resource country (Nigeria): A case report. Ann Transplant . 2014;19:210–213. doi: 10.12659/AOT.890248. [DOI] [PubMed] [Google Scholar]
- 30.Animasahun BA, Akitoye CO, Njokanma OF. Sickle cell: awareness among health professionals and medical students at the Lagos University Teaching Hospital, Lagos. Nig Q J Hosp Med. 2009;19(4):195–199. doi: 10.4314/nqjhm.v19i4.54524. [DOI] [PubMed] [Google Scholar]