Abstract
Background and Objectives:
Although cancer in adolescents and young adults (AYAs) is increasingly an area of focus, there is a paucity of clinical and epidemiological data from developing countries. Our objective was to analyze the geographical distribution, sex ratio, histology, and disease patterns of cancers in AYA.
Materials and Methods:
All patients aged 15-29 years with the diagnosis of cancer who were registered with two hospitals in New Delhi during a 12-month period from January 2014 to December 2014 were included. Basic demographic information on age, sex, location of stay, and nationality was available. Using cancer site and morphology codes, the cancers were grouped by the Birch classification of AYA cancers. Clinical information on disease and treatment status, was retrospectively studied.
Results:
There were 287 patients (57.5% male, 85.4% Indian origin) registered with 54 (18.8%), 97 (33.8%), and 136 (47.4%) patients in the 15-19, 20-24, and 25-29 years age groups, respectively. The three most common cancer groups were carcinomas (40.8%), lymphomas (12.9%), and leukemias (10.4%). The three most common sites in carcinomas were gastrointestinal tract (GIT), genitourinary tract, and breast. The most prevalent cancers in younger AYA (15-19 years) were leukemias, lymphomas, central nervous system neoplasms, and in contrast, older AYA (25-29 years) suffered mainly from GIT Carcinomas, lymphomas. The leading cancers were breast and GIT carcinomas in females and lymphomas and GIT carcinomas in males.
Conclusion:
The occurrence of cancer in AYA in India has been described. The distribution differs from the only previous report from India as well as the US Surveillance Epidemiology and End Results database, which can be attributed to a referral bias along with the factual difference in cancer etiology and genetics.
Keywords: Adolescent and young adults, cancer, epidemiology, India
INTRODUCTION
Cancer is regarded as a disease of older adults with cancer of the colorectum, breast, lung, and prostate constituting the major cancers. Little is known and reported in literature about the incidence and patterns of this disease in adolescents and young adults (AYAs). This population poised between children and adults has been called the “lost tribe.”[1]
While the incidence of cancer in AYA is lesser than that in the older adults, the population pyramid of developing countries is predominantly young. As per the latest Census by the Government of India 2011, there are over 5 million residents of the age-group 15-29 years in National Capital Territory of Delhi, which accounts for 30% of its total population recorded.[2] Hence, the annual number of AYA cancers, although small, would still constitute a significant burden. This diagnosis disrupts the normal trajectories of development (physical, psychological, and social) and life goals related to family and careers. For these reasons, cancer in AYA merits attention.
One challenge has been the variable definitions for the age range of AYA. The World Health Organization defines adolescents as those aged 10-19, whereas youth as those aged 15-24 years.[3] The US Surveillance Epidemiology and End Results (SEER) program and few other international societies define the AYA cancer population as those aged between 15 and 29.[4,5] For the purpose of this study, we set the age range of 15-29 years as AYA. Our objective was to study the descriptive epidemiology of cancer in AYAs at our cancer center and to compare this with the available data in Indian and Western literature.
MATERIALS AND METHODS
All patients aged 15-29 years with a diagnosis of cancer who visited the outpatient or inpatient department at Max Cancer Centre, Saket (South Delhi), and Max Cancer Centre, Patparganj (East Delhi) during the time period January 1, 2014-December 31, 2014, were included. Information related to demography, diagnosis, and outcome was extracted from the hospital information system, pathology services, and patient's records. Data on diagnosis were originally coded by site and morphology based on the International Classification of Diseases for Oncology (ICD-O).[6] Using this information, the diagnoses were categorized according to the Birch classification[7] which has now become the accepted vehicle for classifying tumors in AYA.
RESULTS
Of 7511 total cases registered during the 1-year period, 287 (3.82%) were in the 15-29 years age-group. Male to female ratio was 1.35:1 (165/122) [Table 1]. Majority of the patients were in age group 25-29 (n = 136; 47.3%) followed by 20-24 (n = 97; 33.8%) age group with 54 (18.9%) in the 15-19 age group. 15.0% of the patients were from outside India (Asia: Mainly Iraq, Afghanistan, and Uzbekistan; the Gulf countries and Africa) [Figure 1].
Table 1.
Age and sex distribution of the study cohort
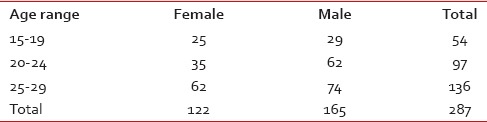
Figure 1.
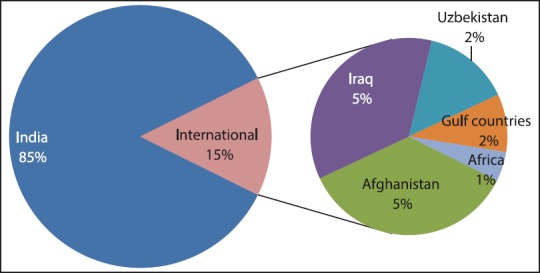
Demographic distribution as per the country of origin
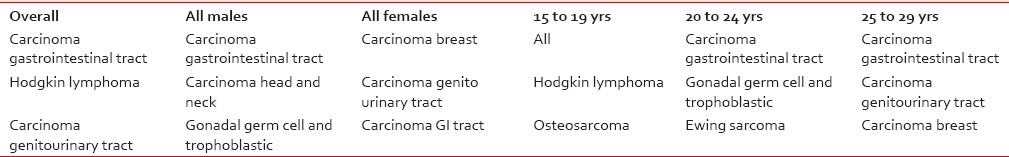
Carcinomas were the most common group of cancer (40.7%), followed by lymphomas (12.9%), leukemias (10.45%), and bone tumors (9.8%) [Table 2]. Among the 42 patients outside India, the most common group were carcinomas (n = 16), bone tumors (n = 8), and lymphomas (n = 6). There were considerable differences in the types of cancers diagnosed in the younger and older AYA. The most prevalent cancers in younger AYA (15-19 years) were acute lymphoblastic leukemia, Hodgkin's lymphomas, and osteogenic sarcoma. In contrast, older AYA (25-29 years) were diagnosed mainly from gastrointestinal carcinomas, genitourinary carcinomas, and breast carcinomas [Table 3].
Table 2.
Age and gender specific distribution of tumors in AYA as per Birch classification
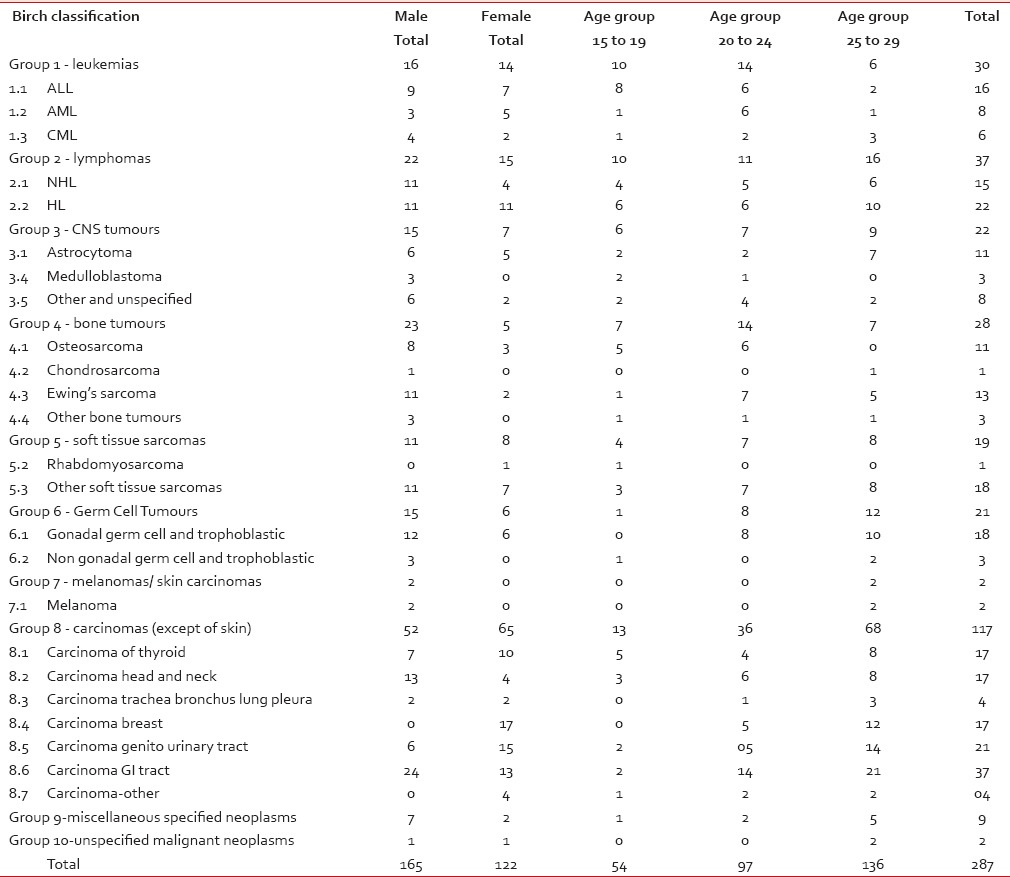
Table 3.
Age and sex distribution of the most common tumors
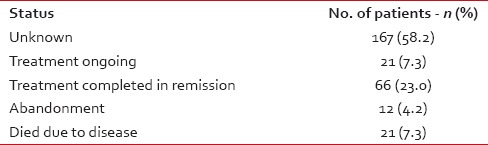
Of 287 patients registered, 220 were newly diagnosed with cancer while 67 cases (23.3%) presented with relapse. Two-third of the patients received treatment at our center while 97 (33.7%) cases were treated outside our center [Table 4].
Table 4.
Status at last follow up
DISCUSSION
This report presents a comprehensive overview of patterns of cancers, age, sex distribution, and histomorphology type of 287 patients of AYA from two cancer centers in Delhi. We have compared our results, wherever possible, with the available literature from India[8,9] and also from international reported series,[4] UK data set,[10] Korean Hospital-based cancer registry (HBCR),[11] and the Netherlands HBCR.[12]
Our observation is that 3.8% of our patients are AYAs. This contrasts with 5.8% seen in urban population-based cancer registry (PBCRs) India and 1.2% England PBCRs — Arora et al.,[10] PBC. Other series report 2.3% in Korea,[11] 2% SEER monograph,[4] 5.2% Kalyani et al.[9] Reasons would include population pyramid of India, effect of being in urban private Delhi where more affluent (and hence older) population is likely to seek healthcare. Hence, our data is poised in between Western data and published India data. The cancer incidence increase with age in AYAs — this observation correlates with other series as well.[4,10,11] The M:F ratio of 1.35 is higher than that reported from India and UK (Arora, et al. 2010) as well as from the Netherlands, Korea, and Australia (Kalyani et al.). It is closer to the Delhi PBCR data from Arora et al. 2010, which was 1.27:1 (unpublished data). This may reflect gender bias or predilection of some morphological types such as Hodgkin lymphoma which have a male preponderance in Delhi or a combination of both the above-stated factors.
Kalyani et al.[9] retrospectively analyzed the pathology records of all nonhematological malignancies at medical college Kolar, Karnataka from 1997 to 2006 of AYA, defined as age-group 15-44 years. Of the 730 cases, 142 (19.45%) were from the age-group 15-29 years. Of these, 50% of the cases were older AYA and M:F ratio was 1:1.32. Padhye et al.[8] analyzed cancer patients diagnosed from 1985 to 2000 at Tata Memorial Hospital (TMH), Mumbai, where 10,717 cases from age-group 15-24 (defined as AYA) were diagnosed. Majority of them were from older age group and M:F ratio was 2.1:1. Akin to the above report by Padhye et al., 47.3% of our cancers were among older AYA with a male preponderance with a caution that this study includes subject's up to 29 years in the study cohort. The female preponderance in Kalyani et al. study is due to the inclusion of older age-group, i.e., 15-44, and thus having more breast, thyroid, and female genital tract malignancies.
There is some variation in the data reported within our country such as higher incidence of leukemia and germ cell tumor in Mumbai study, which is plausible, as more patients with this diagnosis are treated at educational institutes/tertiary referral dedicated cancer centers such as TMH, Mumbai.
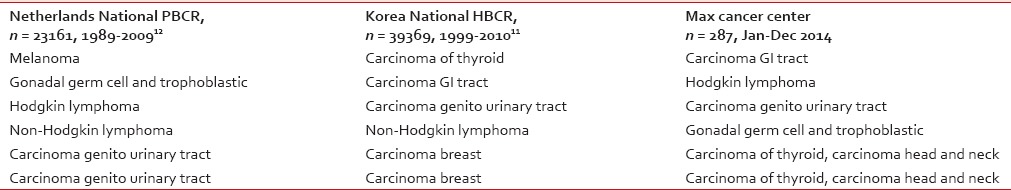
As compared to US SEER database,[4] the tumors considerably more common in the US, as compared to our cohort were lymphomas, germ cell tumors of the female genital tract, and melanomas. In contrast, tumors such as leukemias, carcinomas of the gastrointestinal tract, bone tumors, and central nervous system malignancies were relatively less common. As compared to SEER, Australian database[13] and the Netherlands[12] PBCR decrease in the incidence of melanomas is well-known in our population. Chronic, continuous sun exposure seen in tropical countries such as India is inversely associated with risk of melanoma and increased melanin in dark-skinned individuals acts as a natural sun-protection factor. A larger proportion of cervical cancers among AYA in the UK and Australia as compared to India is paradoxical. This paradox probably reflects differences in sexual behavior and screening practices in the two countries. As cervical screening in England starts at 25 years of age, there may be an artifactual higher incidence of cervical cancers in those aged 25-29 years of age compared with India, where cancers are only diagnosed when symptomatic. Table 5 compares our data set with international cancer registries reporting the AYA cancer incidence with their tumors classified as per the Birch classification.
Table 5.
Five most common AYA cancers (in descending order) based on the Birch classification in our study and published data from other international cancer registries
We have several limitations in this study such as retrospective data collection, lack of incidence and survival analysis, and small sample size with a study duration of a year.
Though the observed differences in literature, as stated above, may be real, it is worthwhile to consider some factors, which may bias these findings. Various factors such as inconsistent defining criteria of AYA population (15-44 years Kalyani et al.[9] vs. 15-24 years TMH study,[8]), different data recording methods (retrospective analysis/population-based registries/prospective data collection, such as SEER database) and various classification schemes (Birch et al./ICD-O) may lead to a reporting bias in the literature. Various etiological factors for nonepithelial cancers such as viruses, chronic infections, radiation, genetic and environmental factors, and for epithelial malignancies such as, tobacco use, alcohol consumption, dietary factors along with racial and ethnic differences are, in reality, responsible for the observed variation among different reports.[14]
CONCLUSION
The patterns of malignancies, their (sub) types and demographic distribution in the AYA cancer patient population not only varies among different countries across the world but also among different cancer centers within India. Knowing the prevalence of cancer and its subtypes among AYA can help us reascertain its importance and provide the interventions and proficiencies that address them. AYA oncology is in its infancy in our country. More research in this field will help us understand the needs of this unique reproductive, young population of India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Michelagnoli MP, Pritchard J, Phillips MB. Adolescent oncology — A homeland for the “lost tribe”. Eur J Cancer. 2003;39:2571–2. doi: 10.1016/j.ejca.2003.09.012. [DOI] [PubMed] [Google Scholar]
- 2.Census of India. Population Enumeration Data; Five-Year Age Group Data C-14 Tables. [Last accessed on 2014 Nov 20]. Available from: http://www.censusindia.gov.in/2011census/C-series/C-14.html .
- 3.Adolescent Health: WHO Health Topic Page on Adolescent Health. [Last accessed on 2014 Nov 20]. Available from: http://www.who.int/topics/adolescent_health/en .
- 4.Bleyer A, Leary MO, Barr R, Ries LA. Bethesda, MD: National Cancer Institute, NIH Pub. No 06-5767; 2006. Cancer Epidemiology in Older Adolescents and Young Adults 15-29 Years of Age, Including SEER Incidence and Survival: 1975-2000. [Google Scholar]
- 5.Ballantine K, Sullivan M. Auckland: National Child Cancer Network; 2013. Adolescent and young adult cancer incidence and survival in New Zealand 2000-2009. [Google Scholar]
- 6.Percy C, Van Holten V, Muir C. International Classification of Diseases for Oncology. 2nd ed. Geneva: World Health Organization; 1990. [Google Scholar]
- 7.Birch JM, Alston RD, Kelsey AM, Quinn MJ, Babb P, McNally RJ. Classification and incidence of cancers in adolescents and young adults in England 1979-1997. Br J Cancer. 2002;87:1267–74. doi: 10.1038/sj.bjc.6600647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Padhye B, Kurkure PA, Arora B, Banavali SD, Vora T, Naryanan P, et al. Patterns of malignancies in adolescents and young adults in tertiary care center from developing country. Implication for outcome optimization and health service SIOP Abstract book 2006. :479–80. [Google Scholar]
- 9.Kalyani R, Das S, Kumar ML. Pattern of cancer in adolescent and young adults — A ten year study in India. Asian Pac J Cancer Prev. 2010;11:655–9. [PubMed] [Google Scholar]
- 10.Arora RS, Alston RD, Eden TO, Moran A, Geraci M, O'Hara C, et al. Cancer at ages 15-29 years: The contrasting incidence in India and England. Pediatr Blood Cancer. 2012;58:55–60. doi: 10.1002/pbc.22738. [DOI] [PubMed] [Google Scholar]
- 11.Moon EK, Park HJ, Oh CM, Jung KW, Shin HY, Park BK, et al. Cancer incidence and survival among adolescents and young adults in Korea. PLoS One. 2014;9:e96088. doi: 10.1371/journal.pone.0096088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aben KK, van Gaal C, van Gils NA, van der Graaf WT, Zielhuis GA. Cancer in adolescents and young adults (15-29 years): A population-based study in the Netherlands 1989-2009. Acta Oncol. 2012;51:922–33. doi: 10.3109/0284186X.2012.705891. [DOI] [PubMed] [Google Scholar]
- 13.Haggar FA, Preen DB, Pereira G, Holman CD, Einarsdottir K. Cancer incidence and mortality trends in Australian adolescents and young adults, 1982-2007. BMC Cancer. 2012;12:151. doi: 10.1186/1471-2407-12-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu X, Groves FD, McLaughlin CC, Jemal A, Martin J, Chen VW. Cancer incidence patterns among adolescents and young adults in the United States. Cancer Causes Control. 2005;16:309–20. doi: 10.1007/s10552-004-4026-0. [DOI] [PubMed] [Google Scholar]


