Abstract
Context:
Despite the fact that breast cancer (BC) is a major health issue, very few studies describe its characteristics in the Middle East.
Aim:
The aim of this study was to evaluate the use and value of Ki-67 as a prognostic marker in BC and associations between Ki-67, clinical, and histopathological parameters were evaluated.
Subjects and Methods:
In a retrospective study, 260 BC women and invasive ductal carcinoma were included to our study in Kermanshah city, Iran. Age, tumor size, lymph node involvement, histological grade, nuclear grade, and vascular invasion were other factors that determined in a lot of patients.
Results:
The mean age at diagnosis was 47.6 years (range, 24-84 years) with 100% female. Of 243 patients that tumor size was determined for them, 207 patients (85.2%) had tumor size ≥2 cm, and 36 patients (14.8%) had size <2 cm and also of 237 patients, 47 patients (19.8%), 140 (59.1%), and 50 (21.1%) had histological grades I, II, and III, respectively. There is significant correlation between Ki-67 with nuclear grade, human epidermal growth factor receptor 2 (HER2), and p53 (P < 0.05). Based on this result, more patients with Ki-67 ≥20% have higher nuclear grade, p53-positive, and HER2-positive. There was correlation between Ki-67 with type of tumor (P = 0.009).
Conclusions:
The higher Ki-67 has a direct significant correlation with higher nuclear grade, p53-positive, and HER2-positive. Furthermore, triple negative patients have higher Ki-67 compared to other subtypes.
Keywords: Breast cancer, histological grade, Ki-67, P53
INTRODUCTION
Breast cancers (BCs) are the most frequent malignancy among women that can be a leading cause of death through middle-aged women. Despite the fact that BC is a major health issue, very few studies describe its characteristics in the Middle East.[1] BCs can be divided based on their gene expression profiles, into at least four groups: Luminal-type, the human epidermal growth factor receptor 2 (HER2)-type, normal-like-type, and basal-type. Luminal-type cancers are characterized by an activated estrogen receptor (ER) signaling pathway and are divided into two subtypes, luminal subtypes “A” and “B”. In general, luminal-subtype-A tumors express higher levels of ER and carry a better prognosis than do luminal-subtype-B tumors.[2] ER positivity predicts response to endocrine therapy such as antiestrogen (tamoxifen) and trastuzumab therapy (herceptin) for tumor with HER2 overexpression.[3] Ki-67 is a nuclear antigen, which exists in proliferative cells. A number of studies have shown that the immune response of Ki-67 is closely associated with the cell cycle. Furthermore, Ki-67 may predict the pathological remission rate in BC patients following neoadjuvant chemotherapy, as an increased Ki-67 level following neoadjuvant chemotherapy indicates a poor prognosis.[4] A meta-analysis involving 12, 155 patients demonstrated that the Ki-67 positivity confers a higher risk of recurrence and a worse survival rate in patients with early BC. Even though this meta-analysis could not scrutinize if Ki-67 had independent prognostic value beyond the standard clinicopathological variables, it confirmed that the high levels of Ki-67 are associated with worse prognoses.[5] The other important biological markers in early BC are tumor size, nuclear grade, axillary lymph node involvement, ER, progesterone receptor (PR), and HER2 status. Uncontrolled proliferation (such as Ki-67) is a key characteristic of malignant tumors and, therefore, tumor proliferation is one of the major factors associated with prognosis.[6,7]
The aim of this study was to evaluate the use and value of Ki-67 as a prognostic marker in BC and associations between Ki-67, clinical, and histopathological parameters were evaluated.
SUBJECTS AND METHODS
Patients
In a retrospective study, 260 BC women and invasive ductal carcinoma were included to our study in Kermanshah City, Iran. They received chemotherapy, radiotherapy, or hormone therapy. A lot of patients underwent primary surgery. A sufficient sample size was selected from any patient, and the slides were stained by hematoxylin and eosin (H and E) method. Then 4 µ sections were prepared for staining with H and E and also for immunohistochemical (IHC) (Ki-67, ER, PR, p53, and HER2) staining. ER and PR positivity was defined as ≥10% positive tumor cells with nuclear staining. The HER2 positive was defined as either HER2 gene amplification by fluorescent in situ hybridization (FISH) or scored as 3+ by IHC. In case of HER2 (2+), FISH was performed to determine HER2 positivity. The age, tumor size, lymph node involvement, histological grade, nuclear grade, and vascular invasion were other factors that determined in a lot of patients.
In this study, hormone receptor (HR)-positive and HER2-negative tumors were classified as luminal A type; HR-positive and HER2-positive tumors (HER2 IHC: 3+ or 2+ that amplifiedbyFISH) as luminal B type; HR-negative and HER2-positive tumors as HER2 disease; and HR-negative and HER2-negative tumors as triple negative (TN) type.[8]
Statistical analysis
Statistical analyses were performed using the IBM SPSS version 19 (SPSS Inc., Chicago, IL, USA). Chi-square test was used to analyze the significance of correlation between the expression of Ki-67 and other parameters. The value P < 0.05 was considered significant.
RESULTS
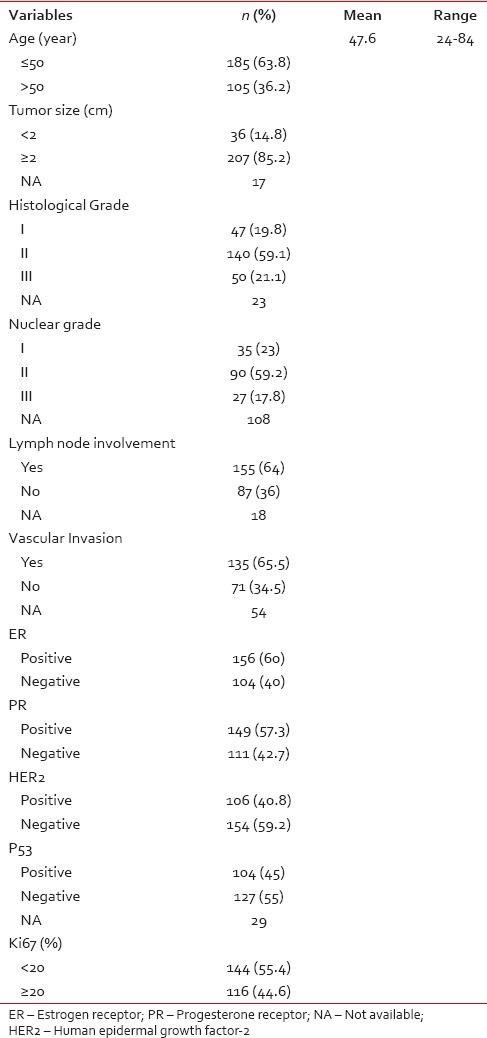
The mean age at diagnosis was 47.6 years (range, 24-84 years) with 100% female. Of 243 patients that tumor size was determined for them, 207 patients (85.2%) had tumor size ≥2 cm, and 36 patients (14.8%) had size <2 cm and also of 237 patients, 47 patients (19.8%), 140 (59.1%), and 50 (21.1%) had histological Grades I, II, and III, respectively [Table 1]. We had nuclear grade for 152 patients that 35 patients (23%), 90 (59.2%), and 27 (17.8%) were Grades I, II, and III, respectively. Of 242 patients, 155 patients (64%) had lymph node involvement and of 206 patients, 135 patients (65.5%) had vascular invasion. Of all patients, 156 (60%), 149 (57.3%), and 106 (40.8%) were ER−, PR−, and HER2− positive, respectively. Of 231 patients, P53-positve was in 104 patients (45%). We divided Ki-67 to two groups: 144 patients (55.4%) had low Ki-67 (Ki-67 <20%) and 116 patients (44.6%) with high Ki-67 (Ki-67 ≥20%).
Table 1.
The baseline characteristics of patients with breast cancer (n = 260)
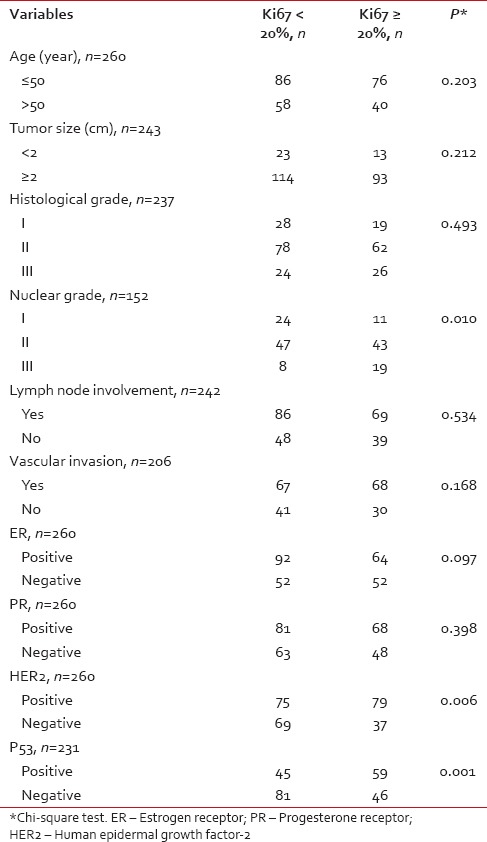
The correlation between Ki-67 with other factors in BC patients has been shown in Table 2. There is a significant correlation between Ki-67 with nuclear grade, HER2, and p53 (P < 0.05). Based on this result, more patients with Ki-67 ≥20% have a higher nuclear grade, p53-positive, and HER2-positive.
Table 2.
The correlation between Ki67 with other factors in breast cancer patients
The Figure 1 shows the number of patients based on Ki-67 for types of tumor. There was correlation between Ki-67 with type of tumor (P = 0.009). Therefore, more TN patients have high Ki-67 and more patients with other subtypes have low Ki-67.
Figure 1.
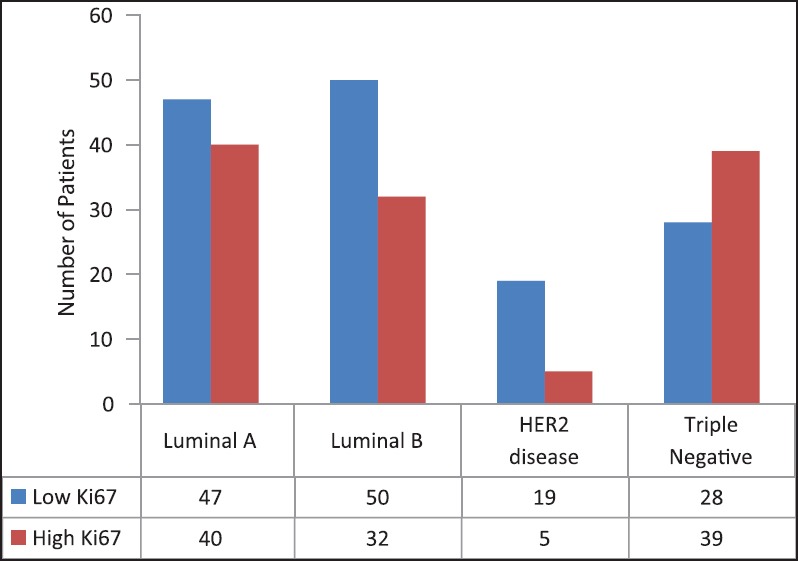
Number of patients based on Ki67 and types of tumor
DISCUSSION
Invasive breast carcinoma is the most common malignant tumor in women worldwide and is a heterogeneous disease with distinct pathological and histological features and can be classified into several subtypes based on the expression of 3 receptors: ER, PR, and HER2.[3] Ki-67 is an immunohistochemical proliferation marker in many types of cancer and has been widely studied among BC patients mostly through retrospective studies.[9]
In our study, higher Ki-67 expression was more frequently associated with HER2-positive. A number of other studies also showed that a higher Ki-67 index significantly correlated with HER2-positive,[6,8,10,11] but in other study, HER2-negative had significantly higher Ki-67 values.[12]
A higher nuclear grade[8,12,13,14] had a direct significantly correlation with higher Ki-67 and also the overexpression of p53 bears a direct statistically significant relationship to Ki-67.[8,15,16] In TN patients has been shown that there is a direct correlation between Ki-67 and p53 that more patients with p53-positive had high Ki-67.[15] In our study, higher Ki-67 expression was more frequently associated with higher nuclear grade and p53-positive.
A number of studies reported that a higher Ki-67 index significantly correlated with larger tumors,[8,10,17] positive lymph nodes.[8,18] Therefore, Ki-67 expression in axillary lymph nodes is significantly higher in lymph nodes than that in primary cancer in some cases.[19,20] A total of 194 cases of diagnosed BC were included in a study that significant association was found between Ki-67 and tumor grade, PR, and lymph node status, but no link was apparent with ER positivity and tumor size.[11] A number of studies reported that among classical histopathological parameters, grading was strongly correlated to Ki-67-labeling indices.[10,21,22] Other studies showed that ER status has been largely identified as being inversely correlated with Ki-67, with the higher rates of ER positivity shown in the lowest proliferating tumors.[8,9,12,21] In our study, there is a significant correlation between tumor size, lymph node involvement, histological grade, ER, and PR status with Ki-67.
A study reported that in univariate analyses, high Ki-67-labeling index was associated with vascular invasion.[10] Furthermore, in other studies had been shown that vascular and lymphatic invasion associated with higher Ki-67 values.[10,23]
A higher Ki-67 index significantly correlated with younger age.[8] In a study reported that in BC, there is a strong correlation has been found between the percentage of cells positive for Ki-67 and age.[13,14] In our study, there was no significant correlation between Ki-67 with age and vascular invasion. Possible cause of the difference in the results of various studies returns to type of division for Ki-67. In a number of studies, Ki-67 has been divided based on ≥10% and <10% and other studies based on ≥20% and <20% such as our study, and even a few studies based on other numbers. For a good result about correlation between Ki-67 with other factors in BC, it needs that the researchers do the studies based on a constant and accurate number.
The results in a study with 960 patients with BC showed that in luminal A patients, only one had a Ki-67 level higher than 20%. In luminal B, the Ki-67 was higher than 20% in 51.16% of the patients. In the HER2 subtype, the Ki-67 level was more than 20% in 48.63%. In TN patients, Ki-67 was more than 20% in 63.86%. The data indicated that the level of Ki-67 may be considered one of the valuable biomarkers in BC patients.[24] In our study, the Ki-67 ≥20% was 45.9%, 39%, 20.8%, and 58.2% in luminal A, luminal B, HER2 disease, and TN patients, respectively. Therefore, TN patients have more Ki-67 ≥20% (high Ki-67) compared to other subtypes.
CONCLUSIONS
The higher Ki-67 has a direct significant correlation with higher nuclear grade; p53-positive and HER2-positive. Furthermore, TN patients have higher Ki-67 compared to other subtypes. For a good result about correlation between Ki-67 with other factors in BC, it needs that Ki-67 indexing divided based on a constant and accurate percent in the future studies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ahmadi AS, Mahdipour L, Payandeh M, Sadeghi M. Epidemiology, pathology and histochemistry features in women with breast cancer. Am J Cancer Prev. 2015;3:54–7. [Google Scholar]
- 2.Kobayashi T, Iwaya K, Moriya T, Yamasaki T, Tsuda H, Yamamoto J, et al. A simple immunohistochemical panel comprising 2 conventional markers, Ki67 and p53, is a powerful tool for predicting patient outcome in luminal-type breast cancer. BMC Clin Pathol. 2013;13:5. doi: 10.1186/1472-6890-13-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Payandeh M, Sadeghi M, Sadeghi E, Aeinfar M. Clinicopathology figures and long-term effects of tamoxifen plus radiation on survival of women with invasive ductal carcinoma and triple negative breast cancer. Asian Pac J Cancer Prev. 2015;16:4863–7. doi: 10.7314/apjcp.2015.16.12.4863. [DOI] [PubMed] [Google Scholar]
- 4.Masuda H, Masuda N, Kodama Y, Ogawa M, Karita M, Yamamura J, et al. Predictive factors for the effectiveness of neoadjuvant chemotherapy and prognosis in triple-negative breast cancer patients. Cancer Chemother Pharmacol. 2011;67:911–7. doi: 10.1007/s00280-010-1371-4. [DOI] [PubMed] [Google Scholar]
- 5.de Azambuja E, Cardoso F, de Castro G, Jr, Colozza M, Mano MS, Durbecq V, et al. Ki-67 as prognostic marker in early breast cancer: A meta-analysis of published studies involving 12,155 patients. Br J Cancer. 2007;96:1504–13. doi: 10.1038/sj.bjc.6603756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colozza M, Azambuja E, Cardoso F, Sotiriou C, Larsimont D, Piccart MJ. Proliferative markers as prognostic and predictive tools in early breast cancer: Where are we now? Ann Oncol. 2005;16:1723–39. doi: 10.1093/annonc/mdi352. [DOI] [PubMed] [Google Scholar]
- 7.Stuart-Harris R, Caldas C, Pinder SE, Pharoah P. Proliferation markers and survival in early breast cancer: A systematic review and meta-analysis of 85 studies in 32,825 patients. Breast. 2008;17:323–34. doi: 10.1016/j.breast.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 8.Nishimura R, Osako T, Okumura Y, Hayashi M, Toyozumi Y, Arima N. Ki-67 as a prognostic marker according to breast cancer subtype and a predictor of recurrence time in primary breast cancer. Exp Ther Med. 2010;1:747–54. doi: 10.3892/etm.2010.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kontzoglou K, Palla V, Karaolanis G, Karaiskos I, Alexiou I, Pateras I, et al. Correlation between Ki67 and breast cancer prognosis. Oncology. 2013;84:219–25. doi: 10.1159/000346475. [DOI] [PubMed] [Google Scholar]
- 10.Inwald EC, Klinkhammer-Schalke M, Hofstädter F, Zeman F, Koller M, Gerstenhauer M, et al. Ki-67 is a prognostic parameter in breast cancer patients: Results of a large population-based cohort of a cancer registry. Breast Cancer Res Treat. 2013;139:539–52. doi: 10.1007/s10549-013-2560-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haroon S, Hashmi AA, Khurshid A, Kanpurwala MA, Mujtuba S, Malik B, et al. Ki67 index in breast cancer: Correlation with other prognostic markers and potential in pakistani patients. Asian Pac J Cancer Prev. 2013;14:4353–8. doi: 10.7314/apjcp.2013.14.7.4353. [DOI] [PubMed] [Google Scholar]
- 12.Nishimura R, Osako T, Nishiyama Y, Tashima R, Nakano M, Fujisue M, et al. Prognostic significance of Ki-67 index value at the primary breast tumor in recurrent breast cancer. Mol Clin Oncol. 2014;2:1062–8. doi: 10.3892/mco.2014.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sahin AA, Ro J, Ro JY, Blick MB, el-Naggar AK, Ordonez NG, et al. Ki-67 immunostaining in node-negative stage I/II breast carcinoma. Significant correlation with prognosis. Cancer. 1991;68:549–57. doi: 10.1002/1097-0142(19910801)68:3<549::aid-cncr2820680318>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 14.Keshgegian AA, Cnaan A. Proliferation markers in breast carcinoma. Mitotic figure count, S-phase fraction, proliferating cell nuclear antigen, Ki-67 and MIB-1. Am J Clin Pathol. 1995;104:42–9. doi: 10.1093/ajcp/104.1.42. [DOI] [PubMed] [Google Scholar]
- 15.Payandeh M, Malayeri R, Sadeghi M, Sadeghi E, Gholami F. Expression of p53 and Ki67 in the patients with triple negative breast cancer and invasive ductal carcinoma. Am J Cancer Prev. 2015;3:58–61. [Google Scholar]
- 16.Sirvent JJ, Salvadó MT, Santafé M, Martínez S, Brunet J, Alvaro T, et al. p53 in breast cancer. Its relation to histological grade, lymph-node status, hormone receptors, cell-proliferation fraction (ki-67) and c-erbB-2. Immunohistochemical study of 153 cases. Histol Histopathol. 1995;10:531–9. [PubMed] [Google Scholar]
- 17.González-Sistal A, Sánchez AB, Del Rio MC, Arias JI, Herranz M, Ruibal A. Association between tumor size and immunohistochemical expression of Ki-67, p53 and BCL2 in a node-negative breast cancer population selected from a breast cancer screening program. Anticancer Res. 2014;34:269–73. [PubMed] [Google Scholar]
- 18.Li FY, Wu SG, Zhou J, Sun JY, Lin Q, Lin HX, et al. Prognostic value of Ki-67 in breast cancer patients with positive axillary lymph nodes: A retrospective cohort study. PLoS One. 2014;9:e87264. doi: 10.1371/journal.pone.0087264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park D, Kåresen R, Noren T, Sauer T. Ki-67 expression in primary breast carcinomas and their axillary lymph node metastases: Clinical implications. Virchows Arch. 2007;451:11–8. doi: 10.1007/s00428-007-0435-2. [DOI] [PubMed] [Google Scholar]
- 20.Dikicioglu E, Barutca S, Meydan N, Meteoglu I. Biological characteristics of breast cancer at the primary tumour and the involved lymph nodes. Int J Clin Pract. 2005;59:1039–44. doi: 10.1111/j.1742-1241.2005.00546.x. [DOI] [PubMed] [Google Scholar]
- 21.Spyratos F, Ferrero-Poüs M, Trassard M, Hacène K, Phillips E, Tubiana-Hulin M, et al. Correlation between MIB-1 and other proliferation markers: Clinical implications of the MIB-1 cutoff value. Cancer. 2002;94:2151–9. doi: 10.1002/cncr.10458. [DOI] [PubMed] [Google Scholar]
- 22.Trihia H, Murray S, Price K, Gelber RD, Golouh R, Goldhirsch A, et al. Ki-67 expression in breast carcinoma: Its association with grading systems, clinical parameters, and other prognostic factors — A surrogate marker? Cancer. 2003;97:1321–31. doi: 10.1002/cncr.11188. [DOI] [PubMed] [Google Scholar]
- 23.Jacquemier J, Charafe-Jauffret E, Monville F, Esterni B, Extra JM, Houvenaeghel G, et al. Association of GATA3, P53, Ki67 status and vascular peritumoral invasion are strongly prognostic in luminal breast cancer. Breast Cancer Res. 2009;11:R23. doi: 10.1186/bcr2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stathopoulos GP, Malamos NA, Markopoulos C, Polychronis A, Armakolas A, Rigatos S, et al. The role of Ki-67 in the proliferation and prognosis of breast cancer molecular classification subtypes. Anticancer Drugs. 2014;25:950–7. doi: 10.1097/CAD.0000000000000123. [DOI] [PMC free article] [PubMed] [Google Scholar]


