Abstract
Couples with a spinal cord injured male partner require assisted ejaculation techniques to collect semen that can then be further used in various assisted reproductive technology methods to achieve a pregnancy. The majority of men sustaining a spinal cord injury regardless of the cause or the level of injury cannot ejaculate during sexual intercourse. Only a small minority can ejaculate by masturbation. Penile vibratory stimulation and electroejaculation are the two most common methods used to retrieve sperm. Other techniques such as prostatic massage and the adjunct application of other medications can be used, but the results are inconsistent. Surgical sperm retrieval should be considered as a last resort if all other methods fail. Special attention must be paid to patients with T6 and rostral levels of injury due to the risk of autonomic dysreflexia resulting from stimulation below the level of injury. Bladder preparation should be performed before stimulation if retrograde ejaculation is anticipated. Erectile dysfunction is ubiquitous in the spinal cord injured population but is usually easily managed and does not pose a barrier to semen retrieval in these men. Semen analysis parameters of men with spinal cord injury are unique for this population regardless of the method of retrieval, generally presenting as normal sperm concentration but abnormally low sperm motility and viability. When sperm retrieval is desired in this population, emphasis should be placed on initially trying the simple methods of penile vibratory stimulation or electroejaculation before resorting to more advanced and invasive surgical procedures.
Keywords: assisted reproductive technology, ejaculation, electroejaculation, male infertility, paraplegia, penile vibratory stimulation, semen, sperm, spinal cord injury, surgical sperm retrieval
INTRODUCTION
Each year in the United States approximately 12 500 new spinal cord injuries occur. Nearly 80% of these injuries occur in males with an average age of 42 years.1 Similar statistics are observed in other parts of the world.2,3,4,5,6 Females with spinal cord injury (SCI) typically are capable of conceiving and delivering children without any complications but are considered high-risk pregnancies.7,8,9 Three common sequelae of SCI prevent men from fathering their own children via sexual intercourse: erectile dysfunction, ejaculatory dysfunction, and abnormal semen analysis parameters.10 This review will discuss the effect of these complications on male fertility after SCI and the available management options to treat couples with a male partner with SCI. These discussions will also include the most recent research efforts to increase ejaculation success rates and improve semen quality in this population.
SEQUELAE OF SCI THAT AFFECT MALE FERTILITY
The reproductive process from erection through ejaculation is complex. It requires a basic hormonal milieu and the integrity of both the sympathetic and parasympathetic branches of the autonomic nervous system (ANS). Control of the ANS is exerted via excitatory and inhibitory pathways originating in the brain and traveling through the spinal cord (Figure 1a). This control is most often affected by SCI, leaving the processes of erection and ejaculation as unmodulated reflexes. Sympathetic outflow from the T11-L2 spinal segments is generally considered responsible for the production of psychogenic erections, seminal emission, and closure of the bladder neck during ejaculation. The parasympathetic output from the S2-S4 spinal segments is responsible for the initiation of reflexogenic erections and the pulsatile expulsion of the semen during ejaculation, as well as the integrity of the pudendal nerve and the dorsal nerve of the penis. In the absence of any other injuries or co-morbidities, the vascular component of the erectile process, (nitric oxide → cGMP → cavernous smooth muscle relaxation → increased arterial vascular engorgement of the cavernous sinuses) is intact (Figure 1b). Likewise, spermatogenesis seems to be little affected by SCI, judging by the normal numbers of sperm seen in most ejaculates. In contrast, sperm motility and sperm viability are abnormally low in most men with SCI. To what extent the abnormal semen analysis parameters are directly related to the SCI is a subject of active research.
Figure 1.
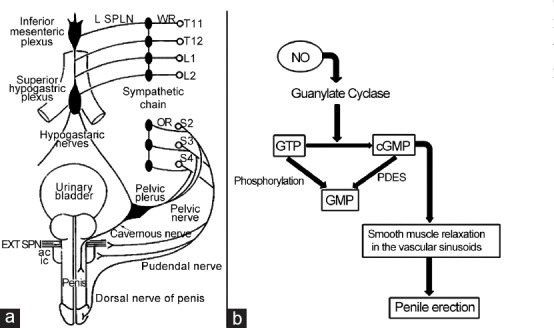
Innervation of the penis and mechanism for erection. (a) Sympathetic penile innervation from segments T10-L2 pass via the sympathetic chain, inferior mesenteric and superior hypogastric plexuses to the pelvic plexus via the hypogastric nerve. Parasympathetic penile innervation arises from segments S2-S4 to the pelvic plexus via the pelvic nerve. The pudendal nerve innervates the external sphincter, bulbospongiosus and ischiocavernosus muscles and also provides sensory fibers to the dorsal nerve of the penis. (b) Cyclic GMP (cGMP) is responsible for the vascular changes which occur in the corpora cavernosa that result in erection. Cyclic GMP is hydrolyzed by PDE-5 to GMP resulting in loss of penile tumescence. The process is initiated by endogenous nitric oxide (NO) activation of guanylate cyclase which results in increased conversion of GTP to cGMP. The inhibition of PDE-5 results in the maintenance of high levels of cGMP.
Erectile dysfunction (ED)
Most spinal cord injuries leave intact the S2-S4 segments of the spinal cord, thus making it possible for reflex erections to occur. Reflex erection is preserved in 95% of males with upper motor neuron lesions and 25% of those with lower motor neuron lesions.11 When reflex erections occur, they are often inconvenient and not long-lasting. Because the basic vascular mechanisms are usually intact, most patients can respond to the administration of the same PDE-5 inhibitors that are available for treating ED in the general population, i.e., sildenafil citrate (Viagra®, Pfizer Inc., Mission, KS, USA),12 vardenafil hydrochloride (Levitra®, Bayer HealthCare, Whippany, NJ, USA)13 and tadalafil (Cialis®, Lilly USA, LLC, Indianapolis, IN, USA).14 When an erection has been achieved through stimulation, these medications help to maintain the erection during sexual activity. Newer PDE-5 inhibitors such as avanafil (Stendra®, Auxilium Pharmaceuticals, Inc., Chesterbrook, PA, USA) have not been tested in men with SCI.
If a patient is unable to obtain a reflexogenic erection, or if PDE-5 inhibitors fail to induce a sustained erection, more invasive methods are used. These methods include intracavernous injection of prostaglandin E1 (alprostadil); a combination of phentolamine and papaverine (Bimix); or combination of prostaglandin 1, phentolamine and papaverine (Trimix).15,16 The patient should be counseled with regard to side effects, such as hematoma and priapism that may occur with the use of intracavernous injections. Variable success rates and variable patient satisfaction rates have been reported for two other methods of ED management in men with SCI, which include intraurethral application of alprostadil (MUSE),17 and vacuum constriction devices.18,19,20 The last resort in the treatment of ED in men with SCI is the surgically implanted penile prosthesis. Satisfactory results are reported using both the inflatable three-piece device,21 as well as the semi-rigid penile prosthesis.22 Lack of penile sensation can result in penile erosion if early signs are not observed by the patient and for this reason, the inflatable devices are favored in the SCI population.
Ejaculatory dysfunction
Anejaculation in men with SCI
As outlined earlier, normal ejaculation requires an intact ejaculatory reflex. This reflex is controlled by both sympathetic and somatic neural inputs as well as sensory inputs. The dorsal nerve of the penis relays sensory input to the S2-S4 spinal segments while the sympathetic fibers (arising from T10-L2 through the sympathetic chain and the hypogastric plexus) control bladder neck closure and seminal emission. Somatic fibers from S2-S4 cause rhythmic contraction of the periurethral muscles followed by projectile ejaculation. The majority of men with SCI cannot ejaculate with sexual intercourse and will require medical assistance to induce an ejaculation.23,24,25 Only 10%–15% of them can achieve ejaculation with masturbation.26 Patients with a level of injury at or rostral to T10 are more likely to respond to penile vibratory stimulation (PVS) than patients with a level of injury T11 or caudal. The former group generally will have enough integrity of sympathetic and parasympathetic components of the ejaculatory reflex, as well as the integrity of the dorsal nerve of the penis, to be able to respond to PVS.
Management of anejaculation in men with SCI
Methods of sperm retrieval in men with SCI
In the general population, sperm may be obtained from the ejaculate or from reproductive tissues, such as the testis or epididymis. In the noninjured population, the ejaculate is typically the first source of sperm examined in the male partner of an infertile couple. Similarly, it is recommended that the ejaculate be the first source of sperm examined in the male partner with SCI. Owing to the condition of anejaculation in most men with SCI, medical assistance is typically required to induce ejaculation. The method of PVS is recommended as the first line of treatment for obtaining the ejaculate in anejaculatory men with SCI.
Penile vibratory stimulation (PVS)
History and evolution of PVS: The first electromechanical vibrator was patented in 1880 by an English physician and was used for the treatment of female sexual dysfunction.27 Successful ejaculation in men with SCI by PVS was later reported.28,29,30 Various over-the-counter (OTC) devices have been used for PVS of men with SCI (Figure 2a). The first FDA-approved device designed specifically for inducing ejaculation in men with SCI was introduced in 1995. An amplitude of 2.5 mm was shown to optimize success with this method31 (Figure 2b). This PVS device has adjustable frequency and amplitude, and is sold commercially as the FertiCare® personal (Multicept A/S, DK, Frederiksberg C, Denmark). Another FDA-approved device, Viberect X3® (Reflexonic, Frederick, MD, USA), was recently developed for assisted ejaculation in men with SCI. This device uses two vibrating pads to stimulate the penis (Figure 2c).32
Figure 2.
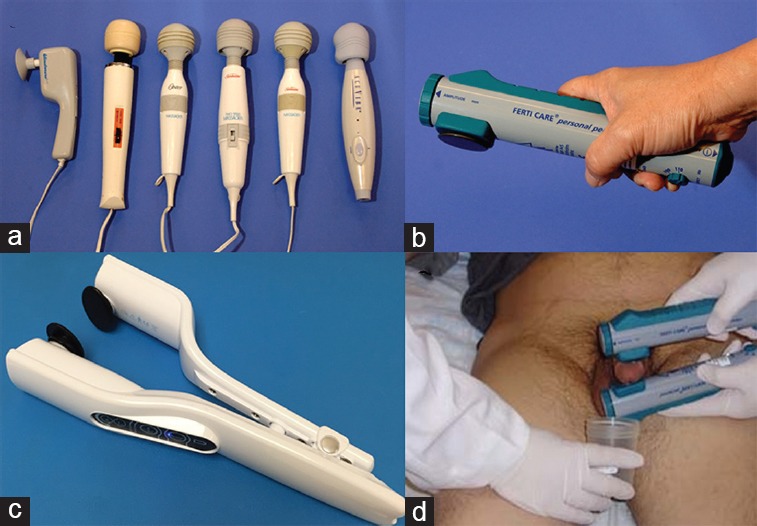
Penile vibratory stimulation (PVS) (a) various over-the-counter devices, often called wand massagers, have been used for PVS in men with SCI. The Personal FertiCare® (b) and the Viberect X3® (c), are devices that have been specifically engineered for the purpose of PVS in men with SCI. (d) The correct placement of two FertiCare devices, which is a recommended method when one device fails to induce ejaculation.
Patient preparation for PVS: The presence of a bulbocavernosus response and a hip flexor response have been shown to be a good predictors of ejaculation by PVS in men with SCI.33 Testing for these reflexes is recommended before stimulation. Patients whose level of injury is T6 or rostral should be pretreated with nifedipine as described below in the section on autonomic dysreflexia (AD). We recommend that an automatic vital signs monitor be used throughout the procedure to record heart rate and blood pressure every minute. Alarms for systolic BP are set at 140 mm Hg and diastolic BP at 100 mm Hg.
If retrograde ejaculation is expected, the bladder should be prepared as described below in the section on retrograde ejaculation.
PVS technique: PVS can be performed with the patient in a supine, reclining or sitting position either on the exam table or in the wheelchair if the transfer is an issue. The patient may suggest a preferred position. To perform PVS, two persons are typically necessary with one to apply the vibrator, and one to hold a sterile specimen cup to collect any antegrade ejaculate. The vibrator is placed on the dorsum, frenulum or both sides of the penis, depending on the device used, or based on previously successful placements for that patient. Vibratory stimulation is applied for 2–3 min, and then stopped if there is no ejaculation. The penile skin is then examined for early detection of skin abrasions or edema, which if found, should warrant termination of that stimulation session. Stimulation can be repeated (stopping every 2–3 min to inspect the penile skin) until an ejaculate is produced or for a total of 15 min. The typical response time is 3 min or less.
Some extra-genital somatic responses may be seen in reaction to PVS. Increased spasticity below the level of injury is commonly observed in patients who have some spasticity of their extremities. Due to the strong nature of these spasms, extremities should be gently guarded to avoid injury. Patients with cervical or upper thoracic levels of injury may experience some tightening of the abdominal and/or intercostal muscles, giving the patient a feeling of difficulty in breathing. As the stimulation progresses, the abdominal contractions become more rhythmic, more frequent, and more forceful.34 This pattern usually indicates that ejaculation is imminent. A firm erection may precede ejaculation. However, ejaculation can occur with no erection. After ejaculation, patients may experience periods of muscular flaccidity that can last from few minutes to hours.35
If ejaculation does not occur with one FertiCare device, two FertiCare devices can be tried (Figure 2d). The use of two devices has been shown to salvage up to 22% of men who failed to respond to one device.36 Although the Viberect X3 allows for simultaneous stimulation of the dorsum and frenulum of the penis, patient satisfaction scores are lower for the Viberect X3 than for the FertiCare.32 The procedure of PVS may be enhanced by adjunct therapies. The following therapies, administered simultaneously with PVS, have each been shown to rescue failures to PVS alone: abdominal electrical stimulation;37 PDE-5 inhibitors;38,39 and midodrine.40,41,42
Success rate of PVS: An 18-year single center experience of 500 men with SCI reported an 86% success rate for PVS when the patient's level of injury was T10 or rostral, and a 15% success rate when the patient's level of injury was T11 or caudal.23 Success can most likely be attributed to an intact dorsal penile nerve (indicating an intact ejaculatory reflex) when the injury is rostral to T10.43 Similar success rates have been reported in other studies.44 Men with SCI who are unable to respond to PVS are often referred for EEJ as an alternative method of obtaining semen.
Electroejaculation (EEJ)
History and evolution of EEJ: Induction of ejaculation using the method of EEJ was initially developed in the 1930s for use in animal husbandry.45 In 1948, Horne et al. reported the first series of EEJ cases.46 His patients were 18 men in a Veterans Administration Hospital. Of these men, 15 ejaculated with EEJ. No complications were reported. In the 1980's, Dr. Seager developed the only FDA approved device for EEJ in humans. This device allowed for the first time, a safe, reliable, and nearly 100% successful method for obtaining an ejaculate in men with SCI (Figure 3).47,48 This device is currently in use worldwide (Dalzell USA Medical Systems, The Plains, VA, USA).
Figure 3.

Electroejaculation machine with an attached rectal probe.
Patient preparation for EEJ: To perform EEJ, the patient is transferred from his wheelchair to an exam table or hospital bed. Patients whose level of injury is T6 or rostral should be premedicated as described in the section on AD. The chance of retrograde ejaculation is higher with EEJ than with PVS. Therefore, bladder preparation is performed immediately before all EEJ procedures, as described below in the section on retrograde ejaculation. The patient is then placed in the lateral decubitus position with knees drawn up, giving the physician performing the procedure access to the rectum for probe introduction. An assistant on the other side of the patient collects the ejaculate.
EEJ procedure: A digital rectal exam is followed by a proctoscopic examination to ensure the integrity of the anus and lower rectum where the EEJ probe is to be placed. Next, a rectal probe is inserted with one electrode facing the prostate anteriorly and two electrodes facing both seminal vesicles. The probes are supplied in different sizes ranging from 1 inch to 1 5/16 inches (2.5–3.30 cm) depending on the size of the rectum. Rectal temperature is monitored throughout the procedure via the built-in sensor (Figure 3).
Practitioners typically use one of two methods for delivering current during the EEJ procedure. The first method is the original method developed by Dr. Seager whereby electric current is gradually increased in a continuous manner until antegrade ejaculation is produced or until the procedure aborted by the physician.48,49 The other method involves delivering electric current in an interrupted fashion, whereby current is delivered for 5 s then turned off. After a rest period of 5 s, current is turned back on, and increased by 2 V above the previous voltage. This step-wise increase in stimulation continues until antegrade ejaculation occurs or until the procedure is stopped by the physician. A study comparing both methods concluded that the interrupted method resulted in a higher proportion of sperm in the antegrade fraction than the continuous method.50 This outcome is most likely due to sphincteric (internal and external) events during EEJ which favor the antegrade flow of semen during the rest periods.51 Regardless of the current delivery method, the patient's urine should be examined for evidence of retrograde ejaculation. A bladder wash/lavage using sperm wash medium (SWM) may also be performed, especially if the initial bladder drainage yielded few sperm.
Most patients tolerate EEJ with little or no discomfort, and the procedure may be performed without anesthesia in the majority of patients. A minority of men with SCI retain pelvic sensation after SCI.48 In these men, EEJ can cause significant discomfort or pain, and hence, conscious sedation or general anesthesia may be necessary.52
EEJ success rates: EEJ is successful in obtaining semen in nearly 100% of men with SCI in whom it is performed.23 In the largest study of its kind to date, EEJ was performed 953 times in 210 patients. Of the 210 patients, 193 (91.9%) responded to EEJ. Responders were consistent over consecutive trials, for example, 897 of the 953 EEJ trials (94.1%) resulted in ejaculation. The remaining 17 patients who did not ejaculate with EEJ felt pain during the procedure and did not elect further trials under anesthesia.23 We have observed that patients in the acute phase of SCI, i.e., patients still in the period of spinal shock, and others <1 year postinjury may not respond to EEJ (unpublished data).
Autonomic dysreflexia (AD)
Before administration of any assisted ejaculation procedure, patients should be assessed for risk of AD, which is a sympathetic reflex response of the nervous system that lacks supra-spinal inhibition to an irritating stimulus below the level of injury. The major manifestation is hypertension, which occasionally may reach dangerous levels. It is often accompanied by bradycardia (which results from an aortic arch baroreceptor response to the elevated blood pressure) but tachycardia may also be seen. In addition, headache, sweating, and chills are commonly seen symptoms.
Spinal cord injuries at or rostral to T6 may disrupt the supra-spinal inhibition of the sympathetic outflow, and men with such injuries are susceptible to AD during any assisted ejaculation procedure. Pretreatment with 10–20 mg nifedipine sublingually or orally will mitigate the elevated blood pressure in most patients. The sublingual dose can be given 10–15 min before initiating the procedure; while the oral dose should be 30–45 min. An occasional patient may have to be titrated up to higher levels. Each dosage increase should be done on separate visits (i.e., not on the same day). Vital signs must be continuously monitored throughout the procedure.53
Retrograde ejaculation
Lack of antegrade ejaculation after assisted ejaculation trials in men with SCI does not necessarily mean anejaculation. Owing to the condition of neurogenic bladder dysfunction present in many men with SCI, retrograde ejaculation is possible during assisted ejaculation procedures.54 Therefore, it is important to prepare the bladder for retrograde ejaculation before administering assisted ejaculation procedures. Retrograde ejaculation is more common during EEJ than with PVS.
The management of retrograde ejaculation aims at increasing the number of motile and viable sperm in the ejaculate by attempting to improve the bladder environment to which the sperm are exposed, i.e., by decreasing urinary acidity. Our protocol is to empty the bladder by urinary catheterization, and to instill the bladder with 25–50 ml of sperm washing medium (SWM, such as Modified Human Tubal Fluid [HTF] with Human Serum Albumin [HSA]) immediately before the ejaculation attempt.55 We have tried other regimens such as administration of oral calcium carbonate in an attempt to alkalinize the urine, sometimes accompanied with oral antibiotics to treat active bacteria in the urine, however, we have not found these measures to be as effective as SWM in maintaining sperm motility in retrograde ejaculates.56
We recommend that bladder preparation for retrograde ejaculation be performed before the first two PVS or EEJ procedures for any patient unless the patient cannot be or refuses to be catheterized. If no retrograde ejaculation occurs during the PVS or EEJ procedures, bladder preparation may be suspended in subsequent procedures.
Patients with a suprapubic catheter in whom a retrograde ejaculate is expected require extra preparation steps including replacing the catheter with a new one, lavaging the bladder with normal saline 2–3 times before instilling SWM and clamping the catheter during the procedure. Following the procedure, the bladder is emptied by unclamping the suprapubic catheter. The collected urine is centrifuged, and the pellet examined for the presence of sperm. A postprocedure lavage with sperm buffer may be performed, if needed, through the suprapubic tube.
Prostate massage
Prostate massage has been used as an alternative method of semen retrieval in men with SCI. Indications include patients with no access to centers performing PVS/EEJ, or patients failing PVS, who do not wish to undergo EEJ. Prostate massage is a simple procedure that may be done in an office setting. Semen is expressed by digital pressure on the prostate gland and seminal vesicles to push sperm out of their storage locations.57,58 Sperm retrieved using prostate massage can be utilized in various assisted conception procedures. Pregnancy success rates vary owing to the typically low yield of sperm obtained by this method.59,60,61
Surgical sperm retrieval (SSR)
If the procedures of PVS or EEJ yield no sperm in the antegrade or retrograde ejaculate, sperm may be sought by surgically removing tissue from reproductive structures, such as the testis or epididymis, and examining the removed tissue for the presence of sperm. Various techniques are used to extract sperm surgically including:
Open testis biopsy – Performed through a small incision in the skin then the tunica vaginalis, posterior testicular pressure allows the expulsion of some seminiferous tubules that are collected with fine scissors. Collected testicular tissue is placed on a slide and examined under the microscope for the presence of sperm62
Percutaneous testicular biopsy – Through a very small scrotal skin incision, an automatic biopsy gun is used to collect the core of tissue that is further examined for sperm identification and/or cryopreservation63
Testicular sperm aspiration (TESA) – Also known as percutaneous testicular fine-needle aspiration. In this procedure, a 23-gauge needle is attached to a 10 ml syringe, inserted into the testis and suction is then applied to aspirate tissues for a total of 20–30 times64
Percutaneous epididymal sperm aspiration (PESA) – Using a smaller 21- or 22-gauge needle, tissues are aspirated from the epididymis and examined using a bench microscope65
Microdissection TESE – Originally described by Schlegel and Li in 1998,66 this technique employs the use of a surgical microscope to identify visually seminiferous tubules that contain active spermatogenesis.67
To date, there are no reports comparing the success rates of various SSR procedures in men with SCI. Such studies have been performed in the general male infertility population. However, extrapolation of these studies to the SCI population is not entirely appropriate, because most men with SCI are neither azoospermic nor severely oligozoospermic, i.e., the conditions that typically indicate SSR in the general population. We recommend that SSR be used in men with SCI only after the semen has been examined and ruled out as a source of sperm for assisted conception procedures.
Semen retrieval algorithm for men with SCI
Our group at the Miami Project to Cure Paralysis has developed an algorithm for semen retrieval in men with SCI based on our long experience in treating this population. Patients unable to ejaculate by masturbation should be administered a trial of PVS with one FertiCare device. If this vibrator fails, a trial should be administered with two FertiCare devices. Patients in whom two vibrators fail may undergo optional adjunct therapies (described in the section on PVS technique), or may undergo optional prostatic massage, before proceeding to EEJ. A review of our database of 500 men with SCI, and 3152 semen retrieval procedures performed in an IRB approved study, showed that sperm were obtained nonsurgically from 422 of 435 men with SCI (97%) who completed this algorithm (Figure 4).23 These patients had a mean age of 34.1 ± 0.4 years (range, 17–63), and a mean time after injury of 10.0 ± 0.3 years. Their level of injury was cervical in 203 men, T1–T6 in 123, T7–T12 in 150, L1 and lower in 20, and unknown in 4. The most common cause of injury was motor vehicle accident followed by gunshot wounds, sports related injuries and falls. Of the 500 patients in the study, 43 (9%) could ejaculate by masturbation. These 43 patients performed a total of 134 masturbation trials. Of the 134 trials, 130 (97%) resulted in ejaculation. PVS was done 2065 times in 461 patients. Success rates depended on the level of injury, as described above in the section on PVS success rates. EEJ was performed 953 times in 210 patients. Anesthesia was not administered during the majority of procedures, and patients experienced little or no discomfort. Only men with retained pelvic sensation (<5% of patients) experienced pain during EEJ. Cases of failed EEJ were referred to surgical sperm retrieval.
Figure 4.
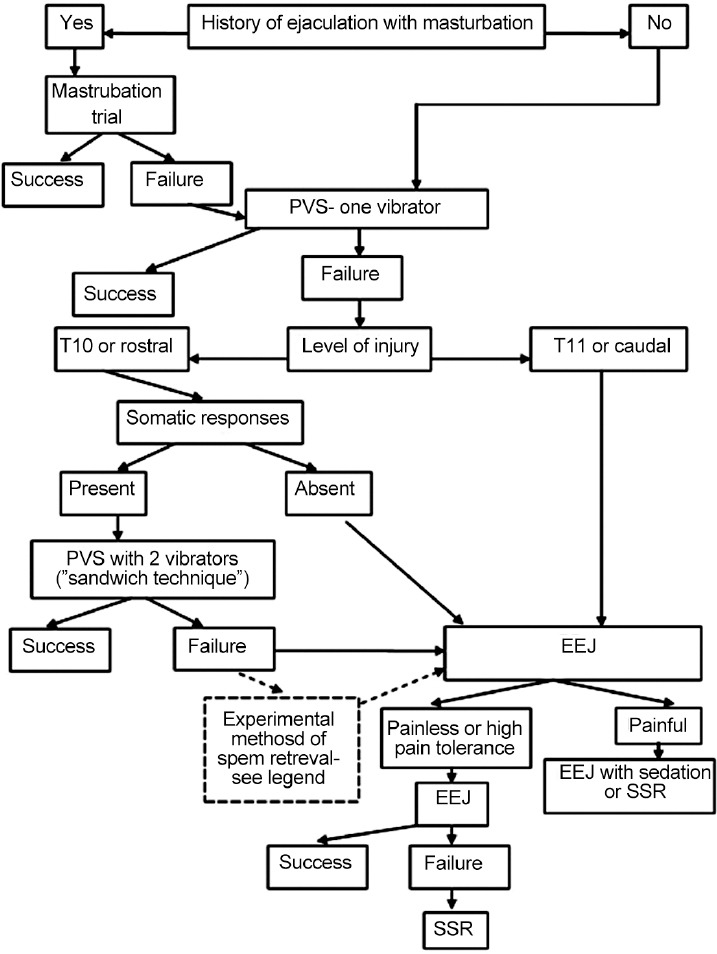
Recommended algorithm for sperm retrieval from men with spinal cord injury. Adapted from Brackett et al.23
SEMEN ABNORMALITIES IN MEN WITH SCI
Abnormal semen analysis parameters constitute the third obstacle in achieving the goal of biological fatherhood in men with SCI. Most have a unique semen profile characterized by normal sperm concentration, but abnormally low sperm motility and viability.24,25,68,69,70 Numerous factors have been hypothesized to be associated with these abnormalities, such as lifestyle changes, physiological changes, method of sperm retrieval, accessory gland dysfunction, seminal plasma biochemical alterations, inflammatory, and immunological changes.
Lifestyle changes
Many lifestyle changes occur after SCI, one of which is sitting in a wheelchair for long periods of time. It has been hypothesized that this condition leads to scrotal hyperthermia which subsequently leads to abnormal semen analysis parameters. To date, no studies have reported normalizing semen parameters by cooling the scrotum of men with SCI. Furthermore, a study by Brackett et al. reported similar scrotal temperature in men with SCI versus noninjured men.71 In this study, a cohort of ambulatory men with SCI were found to have similar abnormalities in their semen analysis parameters as did men with SCI that sat in wheelchairs.
Another lifestyle change after SCI is neurogenic voiding dysfunction. Various methods of bladder management are necessary for patients who may be in urinary retention and/or incontinent. It has been hypothesized that these methods lead to abnormal semen analysis parameters in men with SCI. Studies have shown that clean intermittent catheterization and other cleaner bladder management methods are associated with somewhat higher sperm motility than management by more invasive methods, such as indwelling catheters, but no method is associated with normal semen analysis parameters, not even spontaneous voiding.72,73 Similarly, methods of semen retrieval have been studied as possible causes of abnormal semen analysis parameters in men with SCI. In a study comparing these methods, ejaculates obtained by masturbation had higher sperm motility than ejaculates obtained by PVS or EEJ. However, semen parameters remained abnormal in all three methods.26
Physiological changes
Cross-sectional studies and longitudinal studies have shown that semen quality generally remains stable during the chronic phase of SCI, with no definitive relationship to the duration of injury.50,74 Studies to date have not demonstrated any relationship between the age at injury and semen quality, except in boys injured before puberty. These boys may have impaired spermatogenesis as adults.75 Many studies have shown hormonal changes after SCI; however, these hormonal changes have not shown clear associations with abnormal semen analysis parameters in men with SCI.10
Accessory gland dysfunction
The accessory glands, i.e., the prostate and seminal vesicles, contribute the majority of volume to seminal fluid. They share much of the same innervation as the bladder and penis. It has been hypothesized that SCI leads to abnormal innervation/function of these glands, and this condition leads to abnormalities in the seminal plasma, which in turn, contributes to low sperm motility. To investigate this hypothesis, a study by Brackett et al. added seminal plasma from men with SCI to healthy sperm from noninjured men. The result was an immediate and profound decrease in sperm motility, indicating a role of the seminal plasma in abnormal sperm motility in men with SCI.76 This role was further indicated in a study which found higher motility in sperm aspirated from the vas deferens of men with SCI compared to sperm in the ejaculates of those same men.77 These studies strongly suggest that the seminal plasma from men with SCI has a deleterious effect on sperm. In addition, a number of studies indicate abnormal function of the prostate and seminal vesicles after SCI.78,79,80,81,82,83
Inflammation and immunological changes
When examining the seminal plasma of men with SCI, a common finding is leukocytospermia.81,84 Most of the leukocytes are activated T-lymphocytes,85 and these cells are known to secrete cytokines. Analysis of semen in men with SCI showed elevated pro-inflammatory cytokines including IL-1β, IL-6, and TNF-α.86 Neutralization of these cytokines led to improved sperm motility.87,88 To investigate the mechanism leading to elevated semen cytokines in men with SCI, components of the inflammasome were examined. Two of these components, caspase-1 and ASC, were found to be elevated in semen of men with SCI89 (Figure 5). In vitro neutralization of ASC significantly improved sperm motility in these men.90 Therapies to prevent the formation of the inflammasome offer promise as a treatment for low sperm motility in men with SCI.
Figure 5.
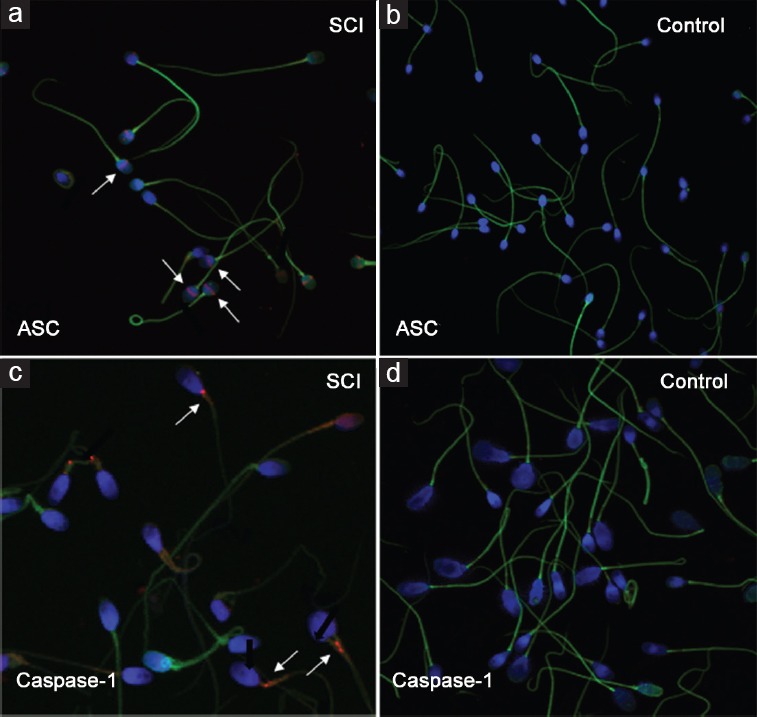
Immunocytochemistry and confocal microscopy images of sperm cells. (a) Sperm cells from men with SCI showing ASC signals in the equatorial segment of sperm cells from men with SCI. (b) No signal in the non-SCI control sperm. (c) Caspase-1 signal in the midpiece of SCI sperm. (d) No signal in non-SCI sperm.
MANAGEMENT OF COUPLES WITH SCI-RELATED MALE FACTOR INFERTILITY
Advances in assisted reproductive technologies (ARTs) have made parenthood a reachable goal for couples with SCI male partners. Although men with SCI almost always present with male factor infertility, there may also be a female factor present as in any couple presenting for infertility. It is important that the female partner be evaluated by an appropriate specialist, such as a reproductive endocrinologist, before attempts at assisted conception. If no female factors dictate otherwise, the choice of ART will be guided primarily by the number of motile sperm available. The lower the total motile sperm count (TMSC) is, the more advanced the technology will be recommended. This guiding principle is used for couples in the general male infertility population, and should also be used when male infertility is due to SCI.
Intravaginal insemination (“in-home insemination”)
Intravaginal insemination is the least expensive and closest to normal conception of the currently available ART techniques. This method involves collecting semen and introducing it into the vagina. If semen collection involves PVS, the couple should be taught how to perform PVS, and should demonstrate their ability to safely perform PVS in the clinic before attempting PVS at home. Before attempting intravaginal insemination, the female partner should have a standard pre-ART evaluation. The insemination procedure is timed to the woman's ovulatory cycle usually with the aid of an OTC ovulation monitoring kit. Ghazeeri et al. reported a 50%–100% LH detection range using five different urinary LH kits compared to values determined by RIA.91 The couple should be cautioned in regards to the limited accuracy of these ovulation detection kits. Semen is collected in a nonspermicidal specimen cup. The semen is drawn up into an appropriately-sized syringe barrel (usually 3 cc or 5 cc), depending on the semen volume. The syringe barrel (with no needle attached) is then introduced into the vagina. The plunger of the syringe is gently pushed to deposit the semen into the vagina.
There are no available guidelines regarding the optimal TMSC for this method. A study of 140 couples between 1988 and 2008 reported a 43% pregnancy rate using intravaginal insemination. The male partners’ age ranged from 22 to 44 years and the level of injury from C2 to T9. All semen samples were collected by PVS and the median TMSC in this group was 29 × 106 (range, 1–92 × 106).92 Another study between 1991 and 2010 showed a 37.8% pregnancy rate by intravaginal insemination in 82 couples in which the male partner had SCI. Semen samples were collected by PVS in 64%, EEJ in 29% and masturbation in 7% of the cases. The mean antegrade TMSC for couples achieving pregnancy was 90.1 ± 30.8 × 106 (range, 2.6–544.5 × 106).93 Multiple studies reported pregnancies rates ranging from 25% to 70% using intravaginal insemination in couples with a male partner with SCI.94,95,96,97
Intrauterine insemination (IUI)
IUI should be the next option if multiple intravaginal insemination attempts have failed or if intravaginal insemination is not indicated. IUI can be successful and cost-effective in couples with SCI male partners. Semen is obtained using PVS or EEJ. Semen is processed to remove the seminal plasma and concentrate the sperm pellet to a volume of approximately 0.5 ml.98 Sperm are introduced into the uterine cavity using a fine cannula. IUI procedures can be performed with or without ovarian stimulation.99 Higher pregnancy rates are achieved with ovarian stimulation and a TMSC of ≥10 × 106. In a study by Kathiresan et al. IUI was performed in 57 couples with an SCI male partner. Nineteen pregnancies were achieved in 14 couples with a pregnancy rate of 24.6% and a cycle fecundity rate of 7.9%.93
In vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI)
There is a lack of consensus regarding the lower limit of TMSC for considering IUI. For example, in a study of 107 centers; 63%, 31%, and 3% of centers respectively reported that the lowest TMSC they would consider for IUI was: 1–4 × 106, 5–10 × 106, and 11–20 × 106.100 If TMSC is lower than the treating center's guidelines for IUI, then IVF/ICSI is the method of choice. The hierarchy of methods of sperm retrieval including masturbation, PVS, EEJ, SSR has been discussed in a previous section and Figure 4. SSR should not be considered before an examination of the semen is performed. If it is not possible to obtain semen for examination, then SSR may be considered early on. Multiple studies have shown pregnancy success rates with IVF/ICSI for couples with an SCI male partner to be similar to those reported for couples with other male factor etiologies.101,102,103 For example, a recent study showed a pregnancy rate of 58.1% per SCI couple and 57.9% per non-SCI.104 These rates were not significantly different.
Current issues in managing couples
With the advancement in ART techniques, couples with an SCI male partner are frequently not offered PVS or EEJ. In a survey sent to practitioners managing couples with an SCI male partner, one in four centers used SSR as the only method of sperm retrieval for ART procedures. Lack of training and/or equipment was the main reason given for not offering PVS or EEJ. In the same study, 34% of the surveyed centers did not offer IUI regardless of the semen quality.100 With SSR as the only option for sperm retrieval, IVF/ICSI becomes essentially the only ART method possible. The low yield of motile sperm precludes the use of less invasive and less expensive options. As discussed in this review, ejaculates can be obtained, without surgery, from 97% of men with SCI. In many cases, there is sufficient TMSC to warrant consideration of intravaginal insemination or intrauterine insemination. We advocate treating these couples on a case by case basis, just as is done for any other couple with a male fertility problem.
CONCLUSIONS
SCI impairs erectile function, ejaculatory function, and semen analysis parameters. These combined effects reduce the fertility potential of this patient group, the majority of who are injured at the peak of their reproductive health. Treatments for ED that are effective in the general population are also effective in men with SCI. Methods to induce ejaculation, such as PVS and EEJ, should be used to assess semen quality before counseling the couple on options for assisted conception. Use of SSR should be applied only in cases in which PVS and EEJ have failed or have resulted in insufficient sperm for ART.
Ejaculates retrieved from men with SCI typically are characterized by normal sperm concentration, but abnormally low sperm motility and viability. Despite impaired sperm parameters, pregnancy outcomes from ART using sperm from men with SCI are similar to those using sperm from non-SCI men. Future studies should focus on improving methods of assisted ejaculation, exploring causes of abnormal semen analysis parameters including immunological factors, and exploring methods to improve semen quality in men with SCI.
COMPETING INTERESTS
None of the authors declare competing financial interests.
ACKNOWLEDGMENTS
We would like to thank Teodoro C Aballa, M.S.
REFERENCES
- 1.National SCI Statistical Center. Spinal Cord Injury – Facts and Figures at a Glance. 2015. [Last accessed on 2015 Nov 09]. Available from: https://www.nscisc.uab.edu/Public/Facts%202015%20Aug.pdf .
- 2.Bjornshave Noe B, Mikkelsen EM, Hansen RM, Thygesen M, Hagen EM. Incidence of traumatic spinal cord injury in Denmark, 1990–2012: a hospital-based study. Spinal Cord. 2015;53:436–40. doi: 10.1038/sc.2014.181. [DOI] [PubMed] [Google Scholar]
- 3.Majdan M, Brazinova A, Mauritz W. Epidemiology of traumatic spinal cord injuries in Austria 2002-2012. Eur Spine J. 2016;25:62–73. doi: 10.1007/s00586-015-3985-z. [DOI] [PubMed] [Google Scholar]
- 4.Singh A, Tetreault L, Kalsi-Ryan S, Nouri A, Fehlings MG. Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol. 2014;6:309–31. doi: 10.2147/CLEP.S68889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sothmann J, Stander J, Kruger N, Dunn R. Epidemiology of acute spinal cord injuries in the Groote Schuur Hospital Acute Spinal Cord Injury (GSH ASCI) Unit, Cape Town, South Africa, over the past 11 years. S Afr Med J. 2015;105:835–9. doi: 10.7196/SAMJnew.8072. [DOI] [PubMed] [Google Scholar]
- 6.Zhou Y, Wang XB, Kan SL, Ning GZ, Li YL, et al. Traumatic spinal cord injury in Tianjin, China: a single-center report of 354 cases. Spinal Cord. 2015;13:173. doi: 10.1038/sc.2015.173. [DOI] [PubMed] [Google Scholar]
- 7.Ghidini A, Healey A, Andreani M, Simonson MR. Pregnancy and women with spinal cord injuries. Acta Obstet Gynecol Scand. 2008;87:1006–10. doi: 10.1080/00016340802356909. [DOI] [PubMed] [Google Scholar]
- 8.American College of Obstetrics and Gynecology. ACOG committee opinion. Obstetric management of patients with spinal cord injuries. Number 275, September 2002. Committee on Obstetric Practice. American College of Obstetrics and Gynecology. Int J Gynaecol Obstet. 2002;79:189–91. doi: 10.1016/s0020-7292(02)00329-6. [DOI] [PubMed] [Google Scholar]
- 9.Camune BD. Challenges in the management of the pregnant woman with spinal cord injury. J Perinat Neonatal Nurs. 2013;27:225–31. doi: 10.1097/JPN.0b013e31829ca83f. [DOI] [PubMed] [Google Scholar]
- 10.Ibrahim E, Lynne CM, Brackett NL. Male fertility following spinal cord injury: an update. Andrology. 2016;4:13–26. doi: 10.1111/andr.12119. [DOI] [PubMed] [Google Scholar]
- 11.Courtois FJ, Charvier KF, Leriche A, Raymond DP. Sexual function in spinal cord injury men. I. Assessing sexual capability. Paraplegia. 1993;31:771–84. doi: 10.1038/sc.1993.120. [DOI] [PubMed] [Google Scholar]
- 12.Lombardi G, Macchiarella A, Cecconi F, Del Popolo G. Ten-year follow-up of sildenafil use in spinal cord-injured patients with erectile dysfunction. J Sex Med. 2009;6:3449–57. doi: 10.1111/j.1743-6109.2009.01426.x. [DOI] [PubMed] [Google Scholar]
- 13.Giuliano F, Rubio-Aurioles E, Kennelly M, Montorsi F, Kim ED, et al. Efficacy and safety of vardenafil in men with erectile dysfunction caused by spinal cord injury. Neurology. 2006;66:210–6. doi: 10.1212/01.wnl.0000194260.43583.32. [DOI] [PubMed] [Google Scholar]
- 14.Giuliano F, Sanchez-Ramos A, Löchner-Ernst D, Del Popolo G, Cruz N, et al. Efficacy and safety of tadalafil in men with erectile dysfunction following spinal cord injury. Arch Neurol. 2007;64:1584–92. doi: 10.1001/archneur.64.11.nct70001. [DOI] [PubMed] [Google Scholar]
- 15.Conejero SJ, Munoz VA, Sarrias LF, Ramirez GL. Prostaglandin treatment in neurological patients with erectile dysfunction. Arch Esp Urol. 2002;55:63–8. [PubMed] [Google Scholar]
- 16.Lebib BA, Laffont I, Boyer F, Boiteau F, Dizien O. Intracavernous injections in the treatment of erectile dysfunction in spinal cord injured patients: experience with 36 patients. Ann Readapt Med Phys. 2001;44:35–40. doi: 10.1016/s0168-6054(00)00061-1. [DOI] [PubMed] [Google Scholar]
- 17.Bodner DR, Haas CA, Krueger B, Seftel AD. Intraurethral alprostadil for treatment of erectile dysfunction in patients with spinal cord injury. Urology. 1999;53:199–202. doi: 10.1016/s0090-4295(98)00435-x. [DOI] [PubMed] [Google Scholar]
- 18.Denil J, Ohl DA, Smythe C. Vacuum erection device in spinal cord injured men: patient and partner satisfaction. Arch Phys Med Rehabil. 1996;77:750–3. doi: 10.1016/s0003-9993(96)90252-x. [DOI] [PubMed] [Google Scholar]
- 19.Lloyd EE, Toth LL, Perkash I. Vacuum tumescence: an option for spinal cord injured males with erectile dysfunction. Sci Nurs. 1989;6:25–8. [PubMed] [Google Scholar]
- 20.Rivas DA, Chancellor MB. Complications associated with the use of vacuum constriction devices for erectile dysfunction in the spinal cord injured population. J Am Paraplegia Soc. 1994;17:136–9. doi: 10.1080/01952307.1994.11735923. [DOI] [PubMed] [Google Scholar]
- 21.Zermann DH, Kutzenberger J, Sauerwein D, Schubert J, Loeffler U. Penile prosthetic surgery in neurologically impaired patients: long-term followup. J Urol. 2006;175:1041–4. doi: 10.1016/S0022-5347(05)00344-7. [DOI] [PubMed] [Google Scholar]
- 22.Kim YD, Yang SO, Lee JK, Jung TY, Shim HB. Usefulness of a malleable penile prosthesis in patients with a spinal cord injury. Int J Urol. 2008;15:919–23. doi: 10.1111/j.1442-2042.2008.02115.x. [DOI] [PubMed] [Google Scholar]
- 23.Brackett NL, Ibrahim E, Iremashvili V, Aballa TC, Lynne CM. Treatment for ejaculatory dysfunction in men with spinal cord injury: an 18-year single center experience. J Urol. 2010;183:2304–8. doi: 10.1016/j.juro.2010.02.018. [DOI] [PubMed] [Google Scholar]
- 24.Brown DJ, Hill ST, Baker HW. Male fertility and sexual function after spinal cord injury. Prog Brain Res. 2006;152:427–39. doi: 10.1016/S0079-6123(05)52029-6. [DOI] [PubMed] [Google Scholar]
- 25.DeForge D, Blackmer J, Garritty C, Yazdi F, Cronin V, et al. Fertility following spinal cord injury: a systematic review. Spinal Cord. 2005;43:693–703. doi: 10.1038/sj.sc.3101769. [DOI] [PubMed] [Google Scholar]
- 26.Kathiresan AS, Ibrahim E, Modh R, Aballa TC, Lynne CM, et al. Semen quality in ejaculates produced by masturbation in men with spinal cord injury. Spinal Cord. 2012;50:891–4. doi: 10.1038/sc.2012.71. [DOI] [PubMed] [Google Scholar]
- 27.Maines R. 1st ed. Baltimore, Maryland: Johns Hopkins University Press; 1999. The Technology of Orgasm: “Hysteria,” the Vibrator, and Women's Sexual Satisfaction. [Google Scholar]
- 28.Brindley GS. Reflex ejaculation under vibratory stimulation in paraplegic men. Paraplegia. 1981;19:299–302. doi: 10.1038/sc.1981.57. [DOI] [PubMed] [Google Scholar]
- 29.Brindley GS. The fertility of men with spinal injuries. Paraplegia. 1984;22:337–48. doi: 10.1038/sc.1984.56. [DOI] [PubMed] [Google Scholar]
- 30.Comarr AE. Sexual function among patients with spinal cord injury. Urol Int. 1970;25:134–68. doi: 10.1159/000279669. [DOI] [PubMed] [Google Scholar]
- 31.Sonksen J, Biering-Sorensen F, Kristensen JK. Ejaculation induced by penile vibratory stimulation in men with spinal cord injuries. The importance of the vibratory amplitude. Paraplegia. 1994;32:651–60. doi: 10.1038/sc.1994.105. [DOI] [PubMed] [Google Scholar]
- 32.Castle SM, Jenkins LC, Ibrahim E, Aballa TC, Lynne CM, et al. Safety and efficacy of a new device for inducing ejaculation in men with spinal cord injuries. Spinal Cord. 2014;52(Suppl 2):S27–9. doi: 10.1038/sc.2014.110. [DOI] [PubMed] [Google Scholar]
- 33.Bird VG, Brackett NL, Lynne CM, Aballa TC, Ferrell SM. Reflexes and somatic responses as predictors of ejaculation by penile vibratory stimulation in men with spinal cord injury. Spinal Cord. 2001;39:514–9. doi: 10.1038/sj.sc.3101200. [DOI] [PubMed] [Google Scholar]
- 34.Szasz G, Carpenter C. Clinical observations in vibratory stimulation of the penis of men with spinal cord injury. Arch Sex Behav. 1989;18:461–74. doi: 10.1007/BF01541673. [DOI] [PubMed] [Google Scholar]
- 35.Laessoe L, Sonksen J, Bagi P, Biering-Sorensen F, Ohl DA, et al. Effects of ejaculation by penile vibratory stimulation on bladder reflex activity in a spinal cord injured man. J Urol. 2001;166:627. doi: 10.1016/s0022-5347(05)66011-9. [DOI] [PubMed] [Google Scholar]
- 36.Brackett NL, Kafetsoulis A, Ibrahim E, Aballa TC, Lynne CM. Application of 2 vibrators salvages ejaculatory failures to 1 vibrator during penile vibratory stimulation in men with spinal cord injuries. J Urol. 2007;177:660–3. doi: 10.1016/j.juro.2006.09.044. [DOI] [PubMed] [Google Scholar]
- 37.Kafetsoulis A, Ibrahim E, Aballa TC, Goetz LL, Lynne CM, et al. Abdominal electrical stimulation rescues failures to penile vibratory stimulation in men with spinal cord injury: a report of two cases. Urology. 2006;68:204–11. doi: 10.1016/j.urology.2006.01.074. [DOI] [PubMed] [Google Scholar]
- 38.Lombardi G, Macchiarella A, Cecconi F, Del Popolo G. Ten years of phosphodiesterase type 5 inhibitors in spinal cord injured patients. J Sex Med. 2009;6:1248–58. doi: 10.1111/j.1743-6109.2008.01205.x. [DOI] [PubMed] [Google Scholar]
- 39.Giuliano F, Rubio-Aurioles E, Kennelly M, Montorsi F, Kim ED, et al. Vardenafil improves ejaculation success rates and self-confidence in men with erectile dysfunction due to spinal cord injury. Spine. 2008;33:709–15. doi: 10.1097/BRS.0b013e3181695040. [DOI] [PubMed] [Google Scholar]
- 40.Courtois F, Charvier K, Leriche A, Vezina JG, Cote I, et al. Perceived physiological and orgasmic sensations at ejaculation in spinal cord injured men. J Sex Med. 2008;5:2419–30. doi: 10.1111/j.1743-6109.2008.00857.x. [DOI] [PubMed] [Google Scholar]
- 41.Leduc BE, Fournier C, Jacquemin G, Lepage Y, Vinet B, et al. Midodrine in patients with spinal cord injury and anejaculation: a double-blind randomized placebo-controlled pilot study. J Spinal Cord Med. 2015;38:57–62. doi: 10.1179/2045772314Y.0000000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Soler JM, Previnaire JG, Plante P, Denys P, Chartier-Kastler E. Midodrine improves ejaculation in spinal cord injured men. J Urol. 2007;178:2082–6. doi: 10.1016/j.juro.2007.07.047. [DOI] [PubMed] [Google Scholar]
- 43.Wieder J, Brackett N, Lynne C, Green J, Aballa T. Anesthetic block of the dorsal penile nerve inhibits vibratory-induced ejaculation in men with spinal cord injuries. Urology. 2000;55:915–7. doi: 10.1016/s0090-4295(99)00608-1. [DOI] [PubMed] [Google Scholar]
- 44.Fode M, Ohl DA, Sonksen J. A step-wise approach to sperm retrieval in men with neurogenic anejaculation. Nat Rev Urol. 2015;12:607–16. doi: 10.1038/nrurol.2015.241. [DOI] [PubMed] [Google Scholar]
- 45.Gunn RM. Fertility in sheep: artificial production of seminal ejaculation and the characteristics of the spermatozoa contained therein. Aust Commonw Counc Sci Ind Res. 1936;94:1–5. [Google Scholar]
- 46.Horne HW, Paull DP, Munro D. Fertility studies in the human male with traumatic injuries of the spinal cord and cauda equina. N Engl J Med. 1948;239:959–61. doi: 10.1056/NEJM194812162392504. [DOI] [PubMed] [Google Scholar]
- 47.Brindley GS. Electroejaculation and the fertility of paraplegic men. Sex Disabil. 1980;3:223–9. [Google Scholar]
- 48.Halstead LS, VerVoort S, Seager SW. Rectal probe electrostimulation in the treatment of anejaculatory spinal cord injured men. Paraplegia. 1987;25:120–9. doi: 10.1038/sc.1987.21. [DOI] [PubMed] [Google Scholar]
- 49.Shaban SF, Seager SW, Lipshultz LI. Clinical electroejaculation. Med Instrum. 1988;22:77–81. [PubMed] [Google Scholar]
- 50.Brackett NL, Ead DN, Aballa TC, Ferrell SM, Lynne CM. Semen retrieval in men with spinal cord injury is improved by interrupting current delivery during electroejaculation. J Urol. 2002;167:201–3. [PubMed] [Google Scholar]
- 51.Sønksen J, Ohl DA, Wedemeyer G. Sphincteric events during penile vibratory ejaculation and electroejaculation in men with spinal cord injuries. J Urol. 2001;165:426–9. doi: 10.1097/00005392-200102000-00018. [DOI] [PubMed] [Google Scholar]
- 52.Heruti RJ, Katz H, Menashe Y, Weissenberg R, Raviv G, et al. Treatment of male infertility due to spinal cord injury using rectal probe electroejaculation: the Israeli experience. Spinal Cord. 2001;39:168–75. doi: 10.1038/sj.sc.3101120. [DOI] [PubMed] [Google Scholar]
- 53.Krassioukov A, Warburton DE, Teasell R, Eng JJ. A systematic review of the management of autonomic dysreflexia after spinal cord injury. Arch Phys Med Rehabil. 2009;90:682–95. doi: 10.1016/j.apmr.2008.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Soler JM, Previnaire JG. Ejaculatory dysfunction in spinal cord injury men is suggestive of dyssynergic ejaculation. Eur J Phys Rehabil Med. 2011;47:677–81. [PubMed] [Google Scholar]
- 55.Suominen JJ, Kilkku PP, Taina EJ, Puntala PV. Successful treatment of infertility due to retrograde ejaculation by instillation of serum-containing medium into the bladder. A case report. Int J Androl. 1991;14:87–90. doi: 10.1111/j.1365-2605.1991.tb01069.x. [DOI] [PubMed] [Google Scholar]
- 56.Mehta A, Sigman M. Management of the dry ejaculate: a systematic review of aspermia and retrograde ejaculation. Fertil Steril. 2015;104:1074–81. doi: 10.1016/j.fertnstert.2015.09.024. [DOI] [PubMed] [Google Scholar]
- 57.Arafa MM, Zohdy WA, Shamloul R. Prostatic massage: a simple method of semen retrieval in men with spinal cord injury. Int J Androl. 2007;30:170–3. doi: 10.1111/j.1365-2605.2006.00733.x. [DOI] [PubMed] [Google Scholar]
- 58.Fahmy I, Kamal A, Metwally M, Rhodes C, Mansour K, et al. Vigorous prostate massage: a simple method to retrieve spermatazoa for ICSI in psychogenic anejaculation. Hum Reprod. 1999;14:2050–3. doi: 10.1093/humrep/14.8.2050. [DOI] [PubMed] [Google Scholar]
- 59.Engin-Uml SY, Korkmaz C, Duru NK, Baser I. Comparison of three sperm retrieval techniques in spinal cord-injured men: pregnancy outcome. Gynecol Endocrinol. 2006;22:252–5. doi: 10.1080/09513590600647326. [DOI] [PubMed] [Google Scholar]
- 60.Marina S, Marina F, Alcolea R, Nadal J, Pons MC, et al. Triplet pregnancy achieved through intracytoplasmic sperm injection with spermatozoa obtained by prostatic massage of a paraplegic patient: case report. Hum Reprod. 1999;14:1546–8. doi: 10.1093/humrep/14.6.1546. [DOI] [PubMed] [Google Scholar]
- 61.Momen MN, Fahmy I, Amer M, Arafa M, Zohdy W, et al. Semen parameters in men with spinal cord injury: changes and aetiology. Asian J Androl. 2007;9:684–9. doi: 10.1111/j.1745-7262.2007.00277.x. [DOI] [PubMed] [Google Scholar]
- 62.Hirsch IH, Choi H. Quantitative testicular biopsy in congenital and acquired genital obstruction. J Urol. 1990;143:311–2. doi: 10.1016/s0022-5347(17)39942-1. [DOI] [PubMed] [Google Scholar]
- 63.Morey AF, MacDonald MF, Rozanski TA, Natarajan S, Thompson IM. Yield and efficacy of biopty gun testis needle biopsy. Urology. 1999;53:604–7. doi: 10.1016/s0090-4295(98)00551-2. [DOI] [PubMed] [Google Scholar]
- 64.Craft I, Tsirigotis M, Courtauld E, Farrer-Brown G. Testicular needle aspiration as an alternative to biopsy for the assessment of spermatogenesis. Hum Reprod. 1997;12:1483–7. doi: 10.1093/humrep/12.7.1483. [DOI] [PubMed] [Google Scholar]
- 65.Tsirigotis M, Pelekanos M, Beski S, Gregorakis S, Foster C, et al. Cumulative experience of percutaneous epididymal sperm aspiration (PESA) with intracytoplasmic sperm injection. J Assist Reprod Genet. 1996;13:315–9. doi: 10.1007/BF02070145. [DOI] [PubMed] [Google Scholar]
- 66.Schlegel PN, Li PS. Microdissection TESE: sperm retrieval in non-obstructive azoospermia. Hum Reprod Update. 1998;4:439. doi: 10.1093/humupd/4.4.439. [DOI] [PubMed] [Google Scholar]
- 67.Schlegel PN. Nonobstructive azoospermia: a revolutionary surgical approach and results. Semin Reprod Med. 2009;27:165–70. doi: 10.1055/s-0029-1202305. [DOI] [PubMed] [Google Scholar]
- 68.Restelli AE, Bertolla RP, Spaine DM, Miotto A, Jr, Borrelli M, Jr, et al. Quality and functional aspects of sperm retrieved through assisted ejaculation in men with spinal cord injury. Fertil Steril. 2009;91:819–25. doi: 10.1016/j.fertnstert.2007.12.060. [DOI] [PubMed] [Google Scholar]
- 69.Patki P, Woodhouse J, Hamid R, Craggs M, Shah J. Effects of spinal cord injury on semen parameters. J Spinal Cord Med. 2008;31:27–32. doi: 10.1080/10790268.2008.11753977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Utida C, Truzzi JC, Bruschini H, Simonetti R, Cedenho AP, et al. Male infertility in spinal cord trauma. Int Braz J Urol. 2005;31:375–83. doi: 10.1590/s1677-55382005000400013. [DOI] [PubMed] [Google Scholar]
- 71.Brackett NL, Lynne CM, Weizman MS, Bloch WE, Padron OF. Scrotal and oral temperatures are not related to semen quality or serum gonadotropin levels in spinal cord-injured men. J Androl. 1994;15:614–9. [PubMed] [Google Scholar]
- 72.Ohl DA, Denil J, Fitzgerald-Shelton K, McCabe M, McGuire EJ, et al. Fertility of spinal cord injured males: effect of genitourinary infection and bladder management on results of electroejaculation. J Am Paraplegic Soc. 1992;15:53–9. doi: 10.1080/01952307.1992.11735862. [DOI] [PubMed] [Google Scholar]
- 73.Rutkowski SB, Middleton JW, Truman G, Hagen DL, Ryan JP. The influence of bladder management on fertility in spinal cord injured males. Paraplegia. 1995;33:263–6. doi: 10.1038/sc.1995.59. [DOI] [PubMed] [Google Scholar]
- 74.Iremashvili V, Brackett NL, Ibrahim E, Aballa TC, Lynne CM. Semen quality remains stable during the chronic phase of spinal cord injury: a longitudinal study. J Urol. 2010;184:2073–7. doi: 10.1016/j.juro.2010.06.112. [DOI] [PubMed] [Google Scholar]
- 75.Celigoj FA, Ibrahim E, Aballa TC, Lynne CM, Brackett NL. Semen quality in men who sustained a spinal cord injury during the prepubertal period. J Urol. 2012;188:521–5. doi: 10.1016/j.juro.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 76.Brackett NL, Davi RC, Padron OF, Lynne CM. Seminal plasma of spinal cord injured men inhibits sperm motility of normal men. J Urol. 1996;155:1632–5. [PubMed] [Google Scholar]
- 77.Brackett NL, Lynne CM, Aballa TC, Ferrell SM. Sperm motility from the vas deferens of spinal cord injured men is higher than from the ejaculate. J Urol. 2000;164:712–5. doi: 10.1097/00005392-200009010-00022. [DOI] [PubMed] [Google Scholar]
- 78.Wieder JA, Lynne CM, Ferrell SM, Aballa TC, Brackett NL. Brown-colored semen in men with spinal cord injury. J Androl. 1999;20:594–600. [PubMed] [Google Scholar]
- 79.Alexandrino AP, Rodrigues MA, Matsuo T. Evaluation of serum and seminal levels of prostate specific antigen in men with spinal cord injury. J Urol. 2004;171:2230–2. doi: 10.1097/01.ju.0000125241.77517.10. [DOI] [PubMed] [Google Scholar]
- 80.Lynne CM, Aballa TC, Wang TJ, Rittenhouse HG, Ferrell SM, et al. Serum and seminal plasma prostate specific antigen (PSA) levels are different in young spinal cord injured men compared to normal controls. J Urol. 1999;162:89–91. doi: 10.1097/00005392-199907000-00022. [DOI] [PubMed] [Google Scholar]
- 81.Randall JM, Evans DH, Bird VG, Aballa TC, Lynne CM, et al. Leukocytospermia in spinal cord injured patients is not related to histological inflammatory changes in the prostate. J Urol. 2003;170:897–900. doi: 10.1097/01.ju.0000080569.51319.40. [DOI] [PubMed] [Google Scholar]
- 82.Dashtdar H, Valojerdi MR. Ultrastructure of rat seminal vesicle epithelium in the acute phase of spinal cord transection. Neurol Res. 2008;30:487–92. doi: 10.1179/016164108X268287. [DOI] [PubMed] [Google Scholar]
- 83.Ohl DA, Menge A, Jarow J. Seminal vesicle aspiration in spinal cord injured men: insight into poor semen quality. J Urol. 1999;162:2048–51. doi: 10.1016/S0022-5347(05)68097-4. [DOI] [PubMed] [Google Scholar]
- 84.Trabulsi EJ, Shupp-Byrne D, Sedor J, Hirsh IH. Leukocyte subtypes in electroejaculates of spinal cord injured men. Arch Phys Med Rehabil. 2002;83:31–3. doi: 10.1053/apmr.2002.26250. [DOI] [PubMed] [Google Scholar]
- 85.Basu S, Lynne CM, Ruiz P, Aballa TC, Ferrell SM, et al. Cytofluorographic identification of activated T-cell subpopulations in the semen of men with spinal cord injuries. J Androl. 2002;23:551–6. [PubMed] [Google Scholar]
- 86.Basu S, Aballa TC, Ferrell SM, Lynne CM, Brackett NL. Inflammatory cytokine concentrations are elevated in seminal plasma of men with spinal cord injuries. J Androl. 2004;25:250–4. doi: 10.1002/j.1939-4640.2004.tb02785.x. [DOI] [PubMed] [Google Scholar]
- 87.Brackett NL, Cohen DR, Ibrahim E, Aballa TC, Lynne CM. Neutralization of cytokine activity at the receptor level improves sperm motility in men with spinal cord injuries. J Androl. 2007;28:717–21. doi: 10.2164/jandrol.106.002022. [DOI] [PubMed] [Google Scholar]
- 88.Cohen DR, Basu S, Randall JM, Aballa TC, Lynne CM, et al. Sperm motility in men with spinal cord injuries is enhanced by inactivating cytokines in the seminal plasma. J Androl. 2004;25:922–5. doi: 10.1002/j.1939-4640.2004.tb03162.x. [DOI] [PubMed] [Google Scholar]
- 89.Zhang X, Ibrahim E, Rivero Vaccari JP, Lotocki G, Aballa TC, et al. Involvement of the inflammasome in abnormal semen quality of men with spinal cord injury. Fertil Steril. 2013;99:118–24. doi: 10.1016/j.fertnstert.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 90.Ibrahim E, Castle SM, Aballa TC, Keane RW, de Rivero Vaccari JP, et al. Neutralization of ASC improves sperm motility in men with spinal cord injury. Hum Reprod. 2014;29:2368–73. doi: 10.1093/humrep/deu230. [DOI] [PubMed] [Google Scholar]
- 91.Ghazeeri GS, Vongprachanh P, Kutteh WH. The predictive value of five different urinary LH kits in detecting the LH surge in regularly menstruating women. Int J Fertil Womens Med. 2000;45:321–6. [PubMed] [Google Scholar]
- 92.Sonksen J, Fode M, Lochner-Ernst D, Ohl DA. Vibratory ejaculation in 140 spinal cord injured men and home insemination of their partners. Spinal Cord. 2012;50:63–6. doi: 10.1038/sc.2011.101. [DOI] [PubMed] [Google Scholar]
- 93.Kathiresan AS, Ibrahim E, Aballa TC, Attia GR, Lynne CM, et al. Pregnancy outcomes by intravaginal and intrauterine insemination in 82 couples with male factor infertility due to spinal cord injuries. Fertil Steril. 2011;96:328–31. doi: 10.1016/j.fertnstert.2011.05.019. [DOI] [PubMed] [Google Scholar]
- 94.Dahlberg A, Ruutu M, Hovatta O. Pregnancy results from a vibrator application, electroejaculation, and a vas aspiration programme in spinal-cord injured men. Hum Reprod. 1995;10:2305–7. doi: 10.1093/oxfordjournals.humrep.a136290. [DOI] [PubMed] [Google Scholar]
- 95.Elliott S. Sexual dysfunction and infertility in men with spinal cord disorders. In: Lin V, editor. Spinal Cord Medicine: Principles and Practice. New York: Demos Medical Publishing; 2003. pp. 349–65. [Google Scholar]
- 96.Lochner-Ernst D, Mandalka B, Kramer G, Stohrer M. Conservative and surgical semen retrieval in patients with spinal cord injury. Spinal Cord. 1997;35:463–8. doi: 10.1038/sj.sc.3100412. [DOI] [PubMed] [Google Scholar]
- 97.Nehra A, Werner M, Bastuba M, Title C, Oates R. Vibratory stimulation and rectal probe electroejaculation as therapy for patients with spinal cord injury: semen parameters and pregnancy rates. J Urol. 1996;155:554–9. [PubMed] [Google Scholar]
- 98.Zhao Y, Vlahos N, Wyncott D, Petrella C, Garcia J, et al. Impact of semen characteristics on the success of intrauterine insemination. J Assist Reprod Genet. 2004;21:143–8. doi: 10.1023/B:JARG.0000031246.76666.f6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Guzick DS, Carson SA, Coutifaris C, Overstreet JW, Factor-Litvak P, et al. Efficacy of superovulation and intrauterine insemination in the treatment of infertility. National Cooperative Reproductive Medicine Network. N Engl J Med. 1999;340:177–83. doi: 10.1056/NEJM199901213400302. [DOI] [PubMed] [Google Scholar]
- 100.Kafetsoulis A, Brackett NL, Ibrahim E, Attia GR, Lynne CM. Current trends in the treatment of infertility in men with spinal cord injury. Fertil Steril. 2006;86:781–9. doi: 10.1016/j.fertnstert.2006.01.060. [DOI] [PubMed] [Google Scholar]
- 101.Kanto S, Uto H, Toya M, Ohnuma T, Arai Y, et al. Fresh testicular sperm retrieved from men with spinal cord injury retains equal fecundity to that from men with obstructive azoospermia via intracytoplasmic sperm injection. Fertil Steril. 2009;92:1333–6. doi: 10.1016/j.fertnstert.2008.07.1776. [DOI] [PubMed] [Google Scholar]
- 102.Shieh JY, Chen SU, Wang YH, Chang HC, Ho HN, et al. A protocol of electroejaculation and systematic assisted reproductive technology achieved high efficiency and efficacy for pregnancy for anejaculatory men with spinal cord injury. Arch Phys Med Rehabil. 2003;84:535–40. doi: 10.1053/apmr.2003.50126. [DOI] [PubMed] [Google Scholar]
- 103.Gat I, Maman E, Yerushalmi G, Baum M, Dor J, et al. Electroejaculation combined with intracytoplasmic sperm injection in patients with psychogenic anejaculation yields comparable results to patients with spinal cord injuries. Fertil Steril. 2012;97:1056–60. doi: 10.1016/j.fertnstert.2012.01.129. [DOI] [PubMed] [Google Scholar]
- 104.Kathiresan AS, Ibrahim E, Aballa TC, Attia GR, Ory SJ, et al. Comparison of in vitro fertilization/intracytoplasmic sperm injection outcomes in male factor infertility patients with and without spinal cord injuries. Fertil Steril. 2011;96:562–6. doi: 10.1016/j.fertnstert.2011.06.078. [DOI] [PubMed] [Google Scholar]


