Abstract
The incidence of male reproductive failure leading to infertility, whether due to delayed parenthood, environmental issues, genetic factors, drugs, etc., is increasing throughout the world. The diagnosis and prognosis of male subfertility have become a challenge. While the basic semen assessment has been performed for many years, a number of studies question the value of the traditional semen characteristics. This is partly due to inadequate methods and standardization, limited knowledge of technical requirements for quality assurance, and an incomplete understanding of what clinical information a semen assessment can provide. Laboratories currently performing semen and endocrine assessment show great variability. The World Health Organization (WHO) manual for the evaluation of semen has been the core of andrology and fertility evaluation that has helped in further development of this field over many years. These include the physical appearance of the ejaculate, assessments of sperm count, motility, vitality, morphology, and functional aspects of the sperm and semen sample. These tests also include male endocrine profile, biochemical evaluation of the semen, detection of antisperm antibodies in serum, the use of computer-aided sperm analysis (CASA), sperm DNA integrity, and its damage due to oxidative stress. Assisted reproductive techniques (e.g., IVF, ICSI) have shown great success but are too expensive. Further development in this field with newer techniques and extensive training/instructions can improve accuracy and reduce variability, thus maintaining the quality and standards of such an evaluation. There is an urgent need to have standardized training centers and increased awareness in this area of men's health for reproductive success.
Keywords: male infertility, quality control management, reproductive failure, semen evaluation, World Health Organization manual
INTRODUCTION
Male reproductive failure leading to infertility is a significant problem affecting more than 80 million couples worldwide.1 As couples are increasingly delaying parenthood, their advancing age, combined with environmental issues, daily stress, drugs, and genetics, independently affect the entire spectrum of male fertility as assessed by reduced sperm quality and fertilization capacity (both assisted and unassisted). Moreover, epidemiological data suggest that these issues can also lead to higher rates of adverse birth outcomes and congenital anomalies and repeated assisted reproductive failures, especially when the semen parameters are normal. With the latest scares related to Ebola and Zika viruses, and their possible spread through semen, this is a grave concern to all. Standard semen analysis (S/A) fails to detect any abnormality, especially in cases of idiopathic infertility.2 In spite of this, semen analysis has an important role in the routine diagnosis of male infertility and reproductive failure.3
Since 1980, the World Health Organization (WHO) manual for the evaluation of semen and cervical mucus has helped in the development of this field over many years. The latest edition of the WHO manual addresses many of the criticisms leveled at previous versions. It now includes step-by-step methods of S/A, detailed descriptions of sperm morphology and assessment, biologically based references ranges, and constructive discussion of quality control (Q/C) and quality assurance (Q/A).4 However, external Q/C programs have shown that many laboratories have great errors in their analyses5 and many challenges remain to be addressed. This review updates current laboratory evaluation of male infertility and reproductive failure with more emphasis on some newly developed methods, S/A training, and Q/C management, so as to improve such patient care.
EVALUATION OF MALE REPRODUCTIVE FAILURE
Clinical assessment of male reproductive failure represents a great challenge. Several factors (environmental, therapeutic, genetic, occupational, etc.) are responsible for male reproductive failure.6 These factors primarily affect the hypothalamic-pituitary-gonadal (HPG) axis, which results in hormonal imbalance and testicular damage causing reproductive failure and infertility.
Endocrine evaluation
An endocrine evaluation of an infertile male should be performed to check: (1) an abnormal testicular size and/or pathology; (2) abnormal semen parameters; (3) impaired sexual function; (4) other clinical findings suggestive of a specific endocrinopathy. Initial evaluation should include levels of serum testosterone (T), luteinizing hormone (LH), follicular stimulating hormone (FSH), inhibin and also prolactin (if erectile dysfunction is suspected). Table 1 gives the reference values of these male reproductive hormones, although some variations within performing laboratories are observed. Since serum gonadotropins and T are secreted in a pulsatile manner, time of collection is important to determine a patient's endocrine status. If the T level is low, a repeat measurement of total and free/bioavailable T and serum LH is important. A normal serum FSH level does not guarantee the presence of intact spermatogenesis. Abnormal serum FSH and inhibin are indicative of impaired spermatogenesis. The endocrine-related clinical conditions in the male are summarized in Table 2 and briefly mentioned below.
Table 1.
Reference values of male reproductive hormones
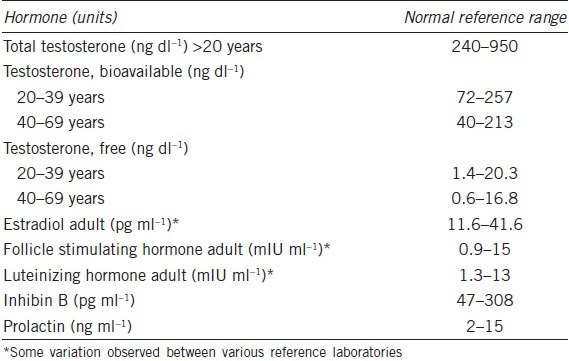
Table 2.
Male reproductive hormone evaluation profile as related to clinical condition
Hypogonadotropic hypogonadism (HH) is characterized by a decreased output of GnRH and low circulating levels of FSH and LH, resulting in androgen deficiency.
Kallmann syndrome results from a failure of the GnRH-releasing neurons to migrate to the olfactory lobe during development and represents the most common X-linked hypogonadotropic hypogonadism. The lack of GnRH in these patients leads to low serum gonadotropins, nonfunctioning testes, delayed puberty, short penis, and infertility.
Kartagener syndrome is due to absent or shortened dynein arms in the sperm tail resulting from axonemal ultrastructural defects that leads to ciliary dyskinesia. All sperm are immotile (asthenospermia).
Hyperprolactinemia results in erectile dysfunction and, ultimately, reproductive failure.
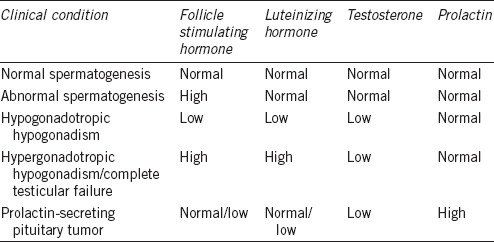
A full evaluation should be done if the initial screening of reproductive history and two properly performed semen analyses demonstrate abnormality (Figure 1). When identification of the etiology of an abnormal semen analysis is not possible, the condition is termed idiopathic.
Figure 1.
Flow chart for the evaluation of male infertility and reproductive. Failure flowchart demonstrating various methods available to measure seminal oxidative stress. GSH: reduced glutathione; GSSG: oxidized glutathione; ROS: reactive oxygen species; TAC: total antioxidant capacity.
SEMEN ANALYSIS – BASIC MODEL
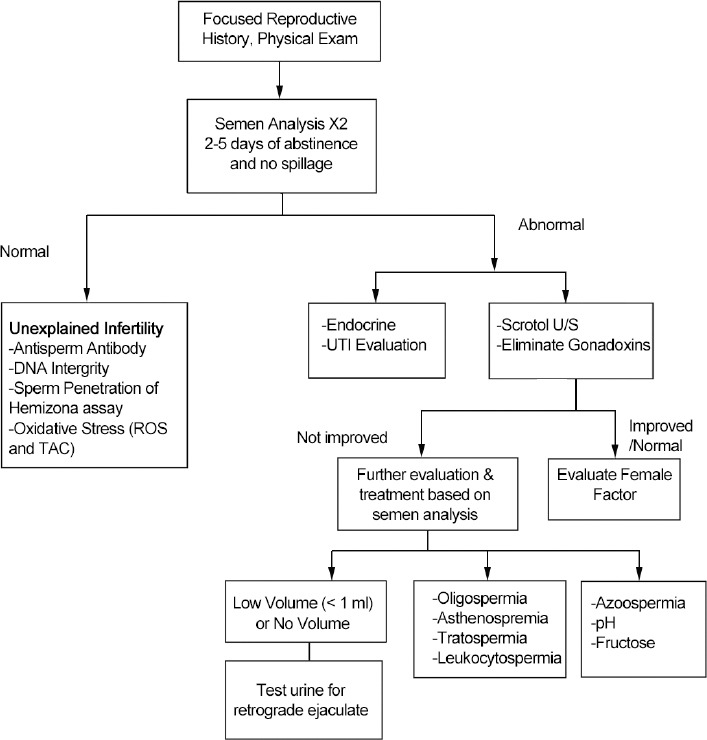
Routine semen analysis is the initial step in evaluation of the infertile male and is not a test of fertility. It provides no insights into the functional potential of the spermatozoon to fertilize an ovum. WHO laboratory manuals have been the primary reference handbooks for semen analysis for many years.7 Table 3 summarizes the reference values of key semen parameters in these WHO manuals.8 The latest WHO (fifth edition, 2010) laboratory manual lists statistically derived fifth centile lower reference limits from several prospective semen analysis studies around the world. These are not cut-off values for diagnosis of sub-fertility, but reflect probabilities based on results from a fertile population. Abnormal semen values suggest possible male factor infertility requiring further clinical and/or laboratory evaluation of the patient. These reference values for semen parameters are not the minimum values to define infertility, as men with semen variables outside these reference ranges are possibly fertile. To ensure accurate results, the laboratory should have a Q/C program for S/A, which adapts to the USA standards outlined in the Clinical Laboratory Improvement Amendments (CLIA). Information on these standards, which include Q/C and proficiency testing, can be found at the CLIA website.9
Table 3.
Reference values of major semen parameters as published in consecutive WHO manuals11
What is semen analysis (S/A)?
S/A is actually a panel of tests that measure the functions of many male reproductive organs and glands. Ejaculation is the sequential emptying of epididymis and vas deferens contents (sperm) and secretions from the prostate and seminal vesicles. Normally, sperm are expelled first together with prostatic fluid, whereas the later 2/3rd of the ejaculate consists of seminal vesicular fluid.10,11,12,13
Sample collection and delivery
Semen sample should be collected by masturbation after 2–5 days of abstinence in a wide-mouth sterile plastic container. The specimen may be collected at home but preferably at the laboratory conducting S/A. The specimen should be kept at room or body temperature during transportation and examined within 1 h of collection.
(A) Macroscopic examination of semen
This involves visual observation of color, opalescence, volume, pH, consistency, odor, etc.
Interpretation guidelines:
Very clear or translucent sample is azoospermic or has very low sperm concentration (severely oligozoospermia)
Red or brownish appearance may indicate blood or infection (hematospermia)
Yellowish color indicates increased concentration of flavoproteins, often related to long abstinence time. May also suggest acute infection and inflammatory cells in semen.
Volume (normal 1.5–6.0 ml)
The bulk of semen volume is from seminal vesicles. It is usually measured by graduated pipette. Alternately, weighing the sample has been recommended.14,15 Given the variability of ejaculation during semen collection, this practice seems overly stringent, time consuming, and not very practical in a physician's office laboratory setting. Low semen volume suggests (a) incomplete sample collection; (b) secretory dysfunction of accessory sex glands; (c) stress during sample collection.
Consistency/viscosity
Highly viscous semen sample is difficult to process for evaluating accurate volume, sperm motility, concentration, morphology, and preparing for assisted reproductive techniques (ARTs). The presence of coagulum is also not normal. Gently passing the sample (avoiding air bubbles) through 21-gauge needle or treatment of sample with chymotrypsin before evaluation helps. Increased consistency may be related to chronic inflammation of the prostate.
pH (normal 6.4–8)
The pH is determined by acidic secretions of the prostate and alkaline secretions of the seminal vesicles. Low pH (<7.0) along with low volume (usually <1.0 ml in absence of any spillage) and no spermatozoa often indicates obstructive azoospermia.
Odor
Strong and pungent smell may indicate bacterial infection.
(B) Microscopic examination of semen
This involves evaluation of well mixed aliquot (5–10 μl) of semen for following parameters using a calibrated microscope that has ×20 phase objective and ocular grid.
Liquefaction
Normal semen should fully liquefy within 15–20 min at 37°C due to the activity of proteases. Results are reported as “normal,” “delayed” (liquefied at >30 min), “incomplete” (liquefied at 60 min), or “not liquefied” (that requires further clinical evaluation) of the patient.
Sperm agglutination and aggregation
Agglutination is the clumps of spermatozoa adhering to each other (not to other cells and debris), which is observed as head to head, head to tail, tail to tail, or mixed. This should be recorded. High agglutination suggests further evaluation of antisperm antibodies, if clinically indicated.
Presence of round cells, and other cellular debris
During motility assessment, if round cells are observed, these should be counted in the same fields. If >1 × 106 round cells per ml are found, a differential staining method for distinguishing leukocytes and immature germ cells (IGCs) should be performed to assess the concentration of WBC in semen (>1 × 106 WBC per ml is termed leukocytospermia). Large amounts of debris should be regarded as abnormal. Increased presence of epithelial cells has not been linked to any specific pathology.
Manual assessment of sperm motility
Sperm motility (%) is evaluated in duplicate within 1 h of semen collection, by counting moving and nonmoving sperm in several microscopic fields. At least 200 spermatozoa are counted and classified as (i) “rapidly progressive” (Class a) that move forward with speed of at least 25 μm s−1 (half a tail or 5 head lengths); (ii) “slowly progressive” (Class b) that move forward with more than 5 μm s−1 (one head lengths) but <25 μm s−1; (iii) “nonprogressive” (Class c) that are slow and only move <5 μm s−1; and (iv) “immotile” (Class d) that do not move and appear dead.15,16 Only complete spermatozoa (head with tail) are included in such counts. Slow moving sperm (Class b + c) can be easily and accurately counted compared to rapidly moving (Class a) sperm. A multi-button tally is used to differentially count such motility.
If the sperm are moving very slowly and the sample has very few sperm, counting progressive and nonprogressive sperm can be performed without many problems. If many sperm are moving with rapid forward progression, evaluation of such subjective motility with any accuracy/precision is difficult and requires much skill and experience. An alternate approach especially for expressing total motility has been suggested by placing an aliquot of semen vial in a heated water bath to make them immotile and then counting all immotile sperm. Counting nonmoving sperm is easy and reproducible, thus minimizing variation. However, this approach misses the evaluation of progressive motility, is time consuming, and needs extra equipment (e.g., heated water bath) and additional regulatory issues, especially when performed in a physician's office laboratory.
Since sperm function requires progressive motility, simple assessment of total motility has less biological and clinical relevance. Another parameter is to express total motile sperm count (TMSC), which is obtained by multiplying total sperm count with total % motility divided by 100.17,18
Interpretation guidelines:
Poor progression with reduced overall motility can be due to infection/inflammation in the prostate and seminal vesicles
Complete absence of sperm motility can be seen in men with cytotoxic antisperm antibodies, and with ciliary dyskinesia (immotile cilia syndrome or Kartagener's syndrome).
Sperm concentration
This is the most important parameter of testicular toxicity/dysfunction. Many counting chambers are available for manual sperm counting. Hemocytometer, although the oldest chamber and used historically in hematology practice, has been widely used for sperm counting. However, it requires a great deal of labor, time,19,20 and is associated with large variation in proficiency testing.21 Many IVF labs are currently using Makler chambers. The hemocytometer and Makler chambers are nondisposable and, along with coverslips must be thoroughly cleaned and dried before reusing. Repeated cleaning will gradually wear down the surface, increasing the depth of these chambers and potentially leading to incorrect sperm count. Therefore, these chambers should be replaced every 1–2 years or when scratched.
Disposable sperm counting chambers currently popular in andrology labs have been shown to be better with many advantages: (1) these have depth appropriate for human sperm with 20 μm that allows viewing of the motile and immotile sperm in the same focal plane;22,23 (2) eliminates chamber cleaning, saving labor and inconvenience; (3) increases counting precision. However, the fluid dynamics of particle flow in such capillary-loaded chambers can lead to differential migration of sperm into the chamber, termed the “Segre–Silberberg effect.” This creates some problems for a highly viscous semen sample. It is advised to count in the center of the chamber viewing area avoiding the margins. Thorough mixing of the semen before dilution and before loading the counting chamber is essential. Correct dilution is preferably done by using calibrated positive-displacement pipettes. It is important to perform duplicate assessments.
Interpretation guidelines: only valid when the entire ejaculate has been collected for analysis (the first fraction contains most of the spermatozoa). Besides incomplete sample collection and less abstinence duration, there are many external factors that can influence the total number of spermatozoa in the ejaculate, for example, fever, some drugs, and occupational exposure, etc.
Total sperm count
This is a more relevant measure of spermatogenesis and depends on testicular size and semen volume. Total sperm count (×106/ejaculate) has more meaning than concentration, and is obtained by multiplying the sperm concentration by the semen volume. The total sperm count is also useful when recommending ART treatment, since it indicates the total number of potentially functional spermatozoa that might be available.
Sperm morphology
Sperm morphology is an important parameter of semen evaluation to identify male factor infertility and toxic exposure from environmental and occupational sources.24,25 It is probably the most complex and difficult component to perform and to interpret.26 Proper thin smear is first prepared by pulling the semen slowly across the clean labeled (using #2 pencil) slide. The angle can be increased or decreased depending on the concentration of sperm in the sample. It should be fixed using a spray cytology fixative (to reduce air-drying artifacts), dried thoroughly, and then stored in a dry place until stained.
A proper thin smear is essential so that each spermatozoa is in the same focal plane, and can be visualized clearly and separately, so its true form can be observed. For evaluating sperm morphology a microscope with better quality optics equipped with bright-field illumination and an oil immersion or dry nonphase contrast objective of at least ×100 magnification should be used. If the sperm concentration is very low (<2 × 106 ml−1), an aliquot of the semen sample can be centrifuged (preferably 300 ×g) and the pellet resuspended in a small amount of clean seminal plasma (i.e., the supernatant) to make the morphology smear. With highly viscous samples it may be difficult to prepare good, thin smear unless treated with alpha-amylase or chymotrypsin,27 or alternatively, a part of the semen specimen can be diluted with 170 mmol l−1 sodium chloride or sperm immobilizing solution and used to make smears.28
For routine evaluation, rapid staining methods, such as the Diff-Quik® can be used after standardization in each laboratory.15,27 Over-staining of the spermatozoa and intense background staining of the seminal plasma are negative aspects of this method. Another method. Spermac®29 also has the advantage of providing detailed differential staining of the acrosome, postacrosomal region, and tail. Such staining differentiates head defects, neck/midpiece defects, tail defects, and cytoplasmic residues. Each morphologically abnormal spermatozoa will have at least one of these abnormalities. The term teratozoospermia index (TZI) has been introduced as an indication of the mean number of abnormalities per abnormal spermatozoon15,27,30 but is not widely used. Since smearing, fixation, air-drying, and staining can induce artifacts that must be identified, it is essential that each analyst is properly trained, and that the laboratory performs regular QC. It is advisable to use services of recognized central laboratories that are well-equipped and have trained personnel to stain and read these morphology slides, especially for multicenter trials, to minimize variation and provide accurate results.
Why is sperm morphology so difficult to standardize and quantify?
Over the last 50 years, five major classification systems for evaluating sperm morphology have been introduced, adding confusion to already complex evaluation.7,13,15,31,32,33 WHO 2010 manual recommends strict morphology criteria (4% normal forms). This is important, especially for IVF centers where success of fertilization is critical. However, many andrology facilities and clinicians dealing with male infertility and toxicology believe that this strict WHO 2010 manual recommendation is not appropriate, is time-consuming, and requires extensive training to evaluate such basic morphology.31,34 The WHO 1999 (third-edition) system classifies borderline sperm into normal morphology with 30% sperm as normal forms. Unfortunately, there are many variations of the two schemes that learning both and comparing the results is time-consuming and difficult, and until a universal standard is available, ambiguity will exist.35 Such confusion about sperm morphology classification can be reduced by education, practice, and discussion.36,37,38
Sperm vitality
Sperm vitality/viability is measured with staining methods as per WHO methods. It is clinically important when very few (<35%) spermatozoa are motile. The proportion of live spermatozoa should be higher than the proportion of motile spermatozoa in the sample.
Leukocytes in semen
There is considerable controversy about the role and evaluation of seminal leukocytes (WBC) in male infertility. A direct count of round cells in wet preparation, at the time of motility evaluation, is first performed. Numerous techniques can then detect seminal WBCs and immature germ cells (IGCs) by specific differential staining as well as by the observing nuclear size and shape. The more accurate way to evaluate leukocytes is to use specifics assays, such as the detection of peroxidase-positive cells (Endtz test), enzyme-linked immunosorbent assay (ELISA), monoclonal antibodies against leukocyte specific antigens (CD45), flow cytometry and immunocytochemistry. However, the peroxidase test is currently the method of choice for immediate clinical assessment of leukocytospermia in a patient. The WHO reference range is set at 1 × 106 ml−1 leukocytes as threshold for leukocytospermia.
Evaluation of antisperm antibodies
Antisperm antibodies (AsAb) are present in 3%–12% of men seeking evaluation of infertility. Prevalence and clinical significance of AsAb in the diagnosis of subfertility and its treatment is controversial since men with high levels of AsAbs can be fertile. AsAb interfere with normal fertilization via several mechanisms including excessive sperm agglutination, issues with cervical mucus penetration, and interfering with sperm-oocyte interaction. AsAb may be generated from the breakdown of the blood-testis barrier, inoculation of the host with sperm antigens, failure of immunosuppression and acute and chronic prostatitis.39 The evaluation is performed preferably by immunobead binding in patient's sperm for “direct assay” or by “indirect assay” using male or female serum or seminal plasma.
Interpretation guidelines:
Head bound AsAb, especially in men after vasovasostomy surgery, have greater clinical significance and is considered to be pathological40
The detection of IgM type AsAb may indicate recent trauma to the male reproductive tract or testicular cancer and needs further investigations
When these tests are positive (50% or more AsAb binding), additional sperm-cervical mucus penetration test should be performed after pretreatment of cervical mucus with bromelain.
Evaluation of retrograde ejaculation
Very low semen volume <1 ml or the absence of antegrade ejaculate, associated with orgasmic response, suggests retrograde ejaculation, lack of emission, ejaculatory duct obstruction, hypogonadism, or congenital absence of vas deferens (CAVD). Retrograde ejaculation is evaluated by observing sperm in resuspended pellet of postejaculatory urine.
Postvasectomy semen evaluation
Semen investigation is usually performed 3–4 months after vasectomy surgery. Azoospermia should not be interpreted until the specimen is centrifuged, and the pellet is examined. Although the AUA guidelines recommend such a centrifugation at maximum speed (preferably 3000 ×g) for 15 min, it is better to first centrifuge at lower speed (300 ×g) and observe the pellet for the presence of motile or immotile spermatozoa.
Microbiological examination of the semen
Bacterial infections
Bacterial infection of the male reproductive tract can affect spermatogenesis and the secretory function of the accessory glands, thus contributing to subfertility.41 The main infectious agents could be Neisseria gonorrhoeae, Chlamydia trachomatis, Ureaplasma urealyticum and Escherichia coli.
Viral infections
Sexually transmitted viruses such as human immunodeficiency virus (HIV), cytomegalovirus (CMV); human papillomavirus (HPV), herpes simplex (HSV), human herpes virus (HHV), Epstein–Barr virus (EBV), hepatitis B virus (HBV), and recently the Ebola and Zika viruses have been detected in human semen by polymerase chain reaction (PCR) or ligase (LCR) technologies. While there are no widespread rapid tests for EBV or HBV, efforts are currently underway to develop them soon. Also the clinical implications and the fertility status of these affected men are not clear.
SPINAL CORD INJURY (SCI) AND INFERTILITY
SCI results in male infertility due to erectile dysfunction, ejaculatory issues, scrotal hyperthermia, urinary tract infection UTls, testicular atrophy, SCI-related hypothalamic-pituitary-gonadal axis dysfunction, abnormal semen composition, and leukocytospermia.42 Abnormal concentrations of leukocytes that predominantly activate T-helper lymphocytes in the semen of men with SCI are considered to have a detrimental effect on sperm motility and viability through the production of reactive oxygen species (ROS). The complex relationship between infection, inflammation, and male fertility has been incompletely elucidated to date. However, sperm motility stimulation by certain agents like pentoxifylline has been successfully used in combination with intrauterine insemination resulting in fertility in such SCI men.43
REFERENCE VALUES FOR SEMEN PARAMETERS
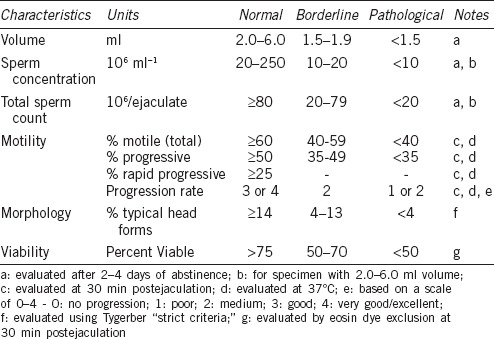
Since there is a considerable overlap between the semen characteristics of fertile and sub-fertile men; no single parameter can be used to provide correct prognostic information about the fertility potential in a couple. Despite many WHO manual updates since 1980 that defined cut-off values to differentiate between normal and abnormal semen, the reference values for semen parameters are still not very clear (Table 3). The new cut-off values in the 2010 manual44 are assessed based on a population of fertile men. Values below the fifth percentile of this group of fertile men are considered as abnormal (Table 3). Based on these cut-off values, the WHO manual uses a descriptive nomenclature to classify the different forms of male factor infertility, (e.g., low count is oligozoospermia [O]; low motility is asthenozoospermia [A], poor morphology is teratozoospermia [T]; and combinations of these is [OAT]). Surprisingly, many men are fertile in spite of lower reference limits; and many men are infertile despite such normal parameters. Thus, Table 445 lists consensus-based reference values in simple terms that are widely accepted in andrology clinics with reference to normal, borderline, or pathological limits.
Table 4.
General (consensus – based) reference values for evaluation of key semen parameters49
BIOCHEMICAL TESTS
Assessment of zinc in seminal fluid
Zinc in semen is considered to be a marker for the prostatic function. It is important for maintaining sperm motility, survival, and chromatin stability. Low zinc content indicates reduced secretory function of the prostate, due to an on-going prostatitis or as inflammatory disease of the prostate.
Assessment of fructose in seminal plasma
Fructose in semen is a marker of seminal vesicles function. A content less than 13.0 μmol indicates low androgen specific contribution of seminal vesicular fluid. Very low content of fructose, low semen volume, and low pH suggests obstructive azoospermia.
COMPUTER-AIDED SEMEN ANALYSIS (CASA)
Despite greatly improved technology since its first introduction in 1985, the CASA is still not widely accepted in routine diagnostic andrology laboratories. This has been attributed to unrealistic expectations of the technology, and early attempts to sell CASA systems as automated semen analyzers.46 CASA technology now mainly assesses sperm movement characteristics (“Kinematics”). Since semen analysis is a set of very different tests; it is difficult to create technology that can accurately evaluate all sperm parameters at the same time. Semen analysis remains predominately a highly complex manual test with CLIA regulated requirements. In addition, automation of semen analysis has not been widely accepted by many clinical laboratories mainly because of complexity of such semen analysis. The major problem with the automatic CASA system is with the true identification and differentiation of spermatozoa from other objects of similar size, such as some round cells, cytoplasmic droplets, or debris. In addition, all equipment requires constant visual supervision and calibration by trained personnel, and is very expensive, difficult to learn, and not sufficiently robust.
SPERM FUNCTION EVALUATION
The term, “sperm function” signifies the ability of spermatozoa to successfully deliver the male genetic material to an ovum. Sperm function testing, once commonly performed for the infertile couple before recommending ART, is now mainly carried out for research purposes. Such testing can provide valuable clinical insights into defects causing reproductive failure and male infertility.
Hyperactivation
This is identified as rapid tail movements with little forward progression. The clinical value of assessing human sperm hyperactivation is still unclear. Hyperactivated spermatozoa quickly undergoes capacitation and acrosome reaction generally in the female reproductive tract.47
Acrosome reaction
During fertilization the spermatozoa undergoes acrosome reaction (AR) on the surface of the zona pellucida (ZP). The zona glycoprotein ZP3 evaluation for the spontaneous AR has little positive predictive value since most of the AR problems can be solved by ICSI. A modified zona-induced acrosome reaction (ZIAR) assesses sperm function potential and correlates well with sperm morphology.48,49
Tests of hemizona and zona-pellucida binding
Sperm binding and penetration of the zona pellucida is important for successful fertilization. Such tests of sperm zona binding, when properly performed, could help select patients for IVF–ICSI. However, the test is difficult to perform in the average andrology or IVF laboratory.
Zona – free hamster egg penetration test
Once popular during the 1980s and early 1990s, the “hamster egg penetration test” (HEPT) or the “sperm penetration assay” (SPA) is currently used in very few laboratories.1 Yanagimachi et al.50 developed the SPA using denuded hamster ova to test sperm capacitation, and their ability to penetrate the egg for successful fertilization. Although several modifications to this test have been developed, its functional predictive value is controversial and no longer ordered even for men with normal semen parameters.
Tests of sperm DNA damage
Routine DNA integrity testing for the functional evaluation of spermatozoa of the infertile male has not been established, although it has potential to become an important test for fertility laboratories. Currently, there are no therapies to correct an abnormal DNA integrity.
SPERM CHROMATIN INTEGRITY TESTS
Sperm DNA integrity is essential in maintaining reproductive potential.51 Since natural selection allows only sperm with intact DNA to fertilize, testing for such DNA integrity has become more relevant due to the increasing use of ARTs, which bypass natural selection.52 Sperm DNA damage affects fertility and pregnancy outcome that cannot be detected by routine semen analysis. Several DNA fragmentation tests have been developed during the last 30 years. There are still many challenges related to standardization of such techniques, and many of these tests are also expensive to perform.
Sperm Chromatin structure assay (SCSA)
Acridine orange is a metachromatic dye that has a different fluorescent property in the presence of single- (red) or double-stranded (green) DNA. The test is easy and fast, but it is limited by inter-observer subjectivity and rapid fading of the fluorescence.53 SCSA is the flow cytometric version of the acridine orange test and measures the susceptibility of sperm DNA to breakage, and allows the analysis of large number of sperm. However, it gives only the percentage of sperm with higher susceptibility to DNA breaks but not much information about the amount of DNA damage in a single sperm.54
Terminal deoxynucleotidyl transferase-mediated nick end labeling (TUNEL)
This test has been found to have a high predictive value for pregnancy, especially for IUI.55 Given its high predictive value and the commercial availability of the test kit, the TUNEL test is currently recommended for measuring sperm DNA fragmentation.
Comet assay
This consists of single-cell gel electrophoresis which performed under neutral or alkaline conditions. With this method, it is possible to analyze many cells and the percentages of single and double DNA breaks are easily detectable, but the technique setup is labor-intensive, needs dedicated software to analyze the results and the DNA damage can be overestimated.56
The sperm chromatin dispersion (halo) test
The halo test can easily detect the number of both single- and double-strand DNA breaks for single spermatozoa in a large number of cells. As with comet assay, the setup is not easy, dedicated software is necessary, and DNA damage can be overestimated.57,58
ASSESSMENT OF REACTIVE OXYGEN SPECIES (ROS)
ROS have been detected in the semen of many infertile men with high WBC.59 ROS in spermatozoa mainly originate from mitochondria as a result of the monovalent reduction of molecular oxygen during oxidative phosphorylation.60,61,62,63,64,65 The ROS test is particularly useful to detect the presence of oxidative stress due to excessive free radicals in the semen as potential cause of infertility in men (e.g., varicoceles, infections or occupational exposure to toxins such as lead or cadmium).66,67,68 However, pathological levels of ROS in infertile semen samples have not been defined accurately. An oxidative stress (OS) test may accurately discriminate between fertile and infertile men and identify those with a clinical diagnosis of male-factor infertility.69
When OS is a significant factor, antioxidant supplementation may benefit. In the absence of a standard protocol to assess seminal oxidants, there is no consensus at this time concerning the inclusion of OS analysis as part of the routine diagnostic workup of an infertile male.
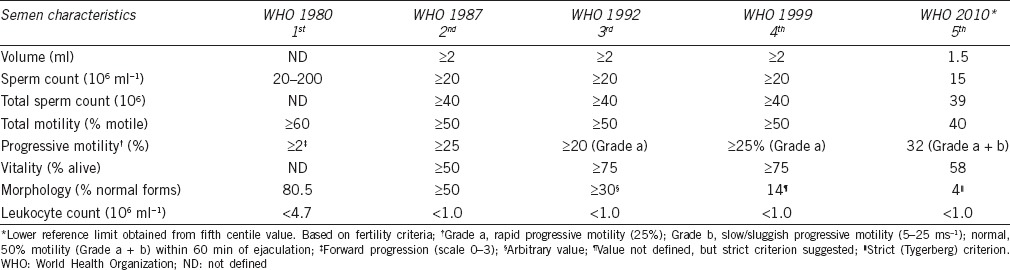
Currently available tests for detecting seminal oxidative stress
Various methods for measuring seminal oxidative stress are as follows (Figure 2).70
Figure 2.
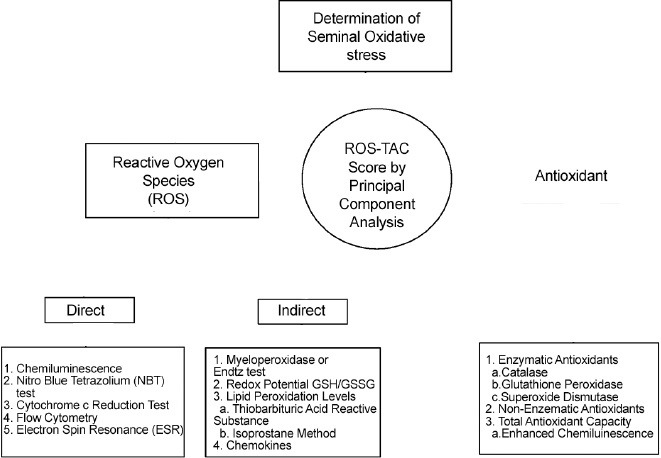
Scheme showing Various Methods for Evaluation of Seminal Oxidative Stress.
Chemiluminescence
Chemiluminescence assay is the most common method to assess ROS concentration in semen.69,71 Luminol is a highly sensitive membrane-permeable probe that reacts with a variety of ROS at neutral pH, and can be used to measure both extracellular and intracellular OS. ROS have a very short lifespan and must be measured quickly after semen collection. The reaction produces photons that are converted to electrical signals which are measured with a luminometer.71 A variety of luminometers are available that can measure the light intensity resulting from the chemiluminescence reaction. The data is expressed as counts per minute (cpm), or as relative light units (RLUs), or as millivolts per second (mV s−1). However, many factors, for example, presence of leukocytes and cellular debris in semen, analysis time, poor liquefaction, repeated centrifugation, changes in the pH etc., can affect the chemiluminescent reaction and the results.72
Nitro blue tetrazolium (NBT) test
NBT is a yellow water-soluble, nitro-substituted aromatic tetrazolium compound that reacts with cellular superoxide ions to form a formazan derivative. This can be measured quantitatively by spectrophotometer.73,74 NBT reduction is a readily available, easily performed, inexpensive, and highly sensitive test.75
Flow cytometry
Flow cytometry distinguishes viable and nonviable sperm using specific dyes such as propidium iodide (PI) and Yopro-1. However, the technique involves the use of expensive flow cytometer instrumentation, skilled personnel, and software for data analysis.
Electron spin resonance (ESR) or electron paramagnetic resonance (EPR)
ESR/EPR spectroscopy, although it is an expensive and cumbersome technique, is the most direct and rapid method for detecting free radicals of interest without artifacts from added chemicals. However, ESR detects only selective oxidants.73,76,77
Determination of seminal antioxidants
Measuring the levels of catalase, glutathione peroxidase, and superoxide dismutase, provides an indirect assessment of the level of seminal OS. These natural antioxidant enzyme are known to protect spermatozoa against oxidative damage.70 Total antioxidant capacity (TAC) reflects the cumulative effect of all antioxidants present in semen. Several methods and commercial kits have been developed to measure TAC in biological fluids, such as the oxygen radical absorbance capacity (ORAC), Cayman chemical antioxidant kit (Cayman Chemical Company, Ann Arbor, MI, USA), Randox total antioxidant status kit (Randox Laboratories, San Francisco, CA, USA).78
ROS-TAC score
Since neither ROS nor TAC alone can adequately quantify seminal OS, a new index called the ROS-TAC score combines both variables. Levels of ROS are measured in the semen sample by the chemiluminescence assay, and the TAC is evaluated by either colorimetric or enhanced chemiluminescence assay. It appears that individuals with ROS-TAC scores below 30 have issues with fertility.78 However, currently there is not enough data available to validate application of this score in clinical practice. Such evaluation of oxidative stress status (OSS) is gaining importance since it plays a major role in the sperm DNA damage and its testing.
GENETIC TESTING AND MALE FACTOR INFERTILITY
Genetic testing is recommended when one or more of the following conditions exist:
Azoospermia or severe Oligospermia
Small testicle size, or absence of vas deferens
Several miscarriages.
Chromosomal aneuploidy in sperm
Aneuploidy is an abnormality in the number of chromosomes, and occurs as a result of a meiotic defect during spermatogenesis. Fluorescence in situ hybridization provides a method to test for sperm chromosomal aneuploidy. These tests detect abnormalities in the chromosomes, (e.g., Y-chromosome microdeletions or translocation or the presence of specific gene mutations such as the cystic fibrosis gene), that are associated with the obstruction or lack of the vas deferens. Testing for genetic conditions is recommended when infertility in men with <5 × 106 total motile sperm could be related to gene deletions, mutations or chromosomal abnormalities.
Chromosome abnormality
Karyotype of some infertile men shows an extra X-chromosome; for example, instead of 47 XXY karyotype they have a 46 XY karyotype. This condition is known as “Klinefelter Syndrome” and results in male infertility. Other chromosome abnormalities, especially in couples who have several miscarriages and/or unexplained infertility may be found during a karyotype test.
Y-chromosome micro-deletions
Some men with azoospermia or severe oligospermia have deletions in their Y-chromosome, known as the DAZ gene. Their karyotype is normal (46 XY) but further evaluation of the Y-chromosome shows some missing sections of this Y-chromosome. The male offspring will also inherit such Y-chromosome deletion.
Single gene mutations/cystic fibrosis (CF) gene test
Although CF is a genetic condition affecting the lungs, a “variant” form of CF affects male fertility, and is associated with either complete or part of absence of the vas deferens. Sperm can be recovered from the testes in these men by surgical retrieval and cryopreserved to be used later for IVF or ICSI. It is important to test female partners for CF mutations to avoid significant risk of having a child with CF.
SEMEN ANALYSIS TRAINING, QUALITY CONTROL, PROFICIENCY, AND COMPETENCY TESTING
Quality control (QC) is a requirement for any good laboratory assay. Many countries and states have now specific regulations for maintaining QC in semen analysis. In the USA, semen analysis is categorized as a high-complexity test requiring CLIA-approved laboratories and two levels of quality controls every 8 h of patient testing. This not only documents the ability to perform the test correctly, but also provides confidence in reporting the results of the test.38,79 WHO 2010 details such Q/C requirement and procedures.7
External quality assurance (EQA)
Participation in an EQA program allows an analytical performance evaluation of a laboratory in comparison with other laboratories. A suspension of washed and preserved intact human sperm suspension is the only valid Q/C sample for validating sperm count. Video recordings, although they lack the direct handling aspects of a semen sample, are easy to prepare and very useful in reproducible training, especially for motility evaluation. Semen smears stained with the appropriate stain can be used for sperm morphology and sperm viability Q/C.
External Q/C or proficiency testing (PT) is important for comparing the results between various laboratories, especially for multicenter trials, and help trouble shoot the issues and improve the quality of such procedures.80 Additional competency testing must include direct observation of test performance by a technical director/supervisor and review of intermediate test results, Q/C records, and proficiency testing. This should also provide preventive maintenance records, and assessment of problem-solving skills.
TRAINING
A standardized training system is essential to avoid variability and ensure accuracy of results, especially for multicenter trials, as well as in centers with fast personnel turnover in order to attain the experience necessary to perform procedures independently. Training progress has to be closely followed, documented and approved by the laboratory director. Studies have revealed large variation between laboratories, even when the same standardized protocols are used.81,82 Thus, inter- and intra-technician coefficients of variation should be calculated for each sperm parameter. Furthermore, the mean percent difference from the chosen standard value should be calculated and expressed.
Standardization of semen analysis requires clear, detailed and robust methods followed up by on-going Q/C and PT. A detailed manual or handbook cannot replace proper, basic hands on technical training. Although, many studies have documented improved performance after a standardized training course,79,81 there are very few formal training centers. Many laboratories do not have budgets to afford such training, especially when travel is involved.
REGULATORY ASPECTS
The requirement for accreditation or licensing of the laboratories varies widely between countries. Good laboratory practice (GLP) refers to a systems of management controls for laboratories to ensure the consistency and reliability of results. Various regulatory and nongovernment bodies have GLP guidelines, rules or regulations. There are clear regulatory guidelines now available for semen analysis, sperm preparation for assisted conception treatment, and for sperm cryobanking. It is essential that the laboratory personnel are aware of these regulations. Each country has (or is likely to have) its own particular system, e.g., CLIA in the USA, NATA in Australia, CPA and HFEA in the UK.
CONCLUSIONS
Correct performance of S/A is complex, time consuming, labor intensive, and tedious. There is a need for better Q/C, more reproducibility, and better functional as well as biochemical tests to assess the fertilizing potential of spermatozoa. Using standardized techniques, conventional semen analysis will give reproducible results. Internal Q/C is mandatory and strict standards for technical accuracy must be applied to minimize inter- and intra-observer variability. Introduction of newer tools and more advanced biochemical, cytological, and functional tests have increased the performance of complete semen analysis. Semen analysis can distinguish the fertile, sub fertile, and infertile men, and it can also help define particular causes of infertility, contribute to the selection of most appropriate treatment, predict outcome, and help to improve the diagnosis and treatment of an infertile male.
EXPERT COMMENTARY/KEY ISSUES/FUTURE DEVELOPMENTS
This is an exciting time in Andrology. Following the discovery of mRNA in mature human sperm, there have been a number of studies suggesting that these mRNAs could be used as a diagnostic tool – equivalent to a transcriptome. While the data to support this is in its infancy, this is likely to be an area of rapid development which holds great promise. The power of proteomics is now increasingly being applied to mature spermatozoa. Certainly, in the coming years, existing methods will be refined, and many new techniques will be developed.
AUTHOR CONTRIBUTIONS
SCS is the main author of this contribution. WJGH contributed to the concept and review.
COMPETING INTERESTS
None.
ACKNOWLEDGMENTS
Lucy Daniels helped in compiling, Dr. Jaideep helped in review and references, and Jessica Daigle helped in editorial corrections.
REFERENCES
- 1.Boivin J, Bunting L, Collins JA, Nygren KG. International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care. Hum Reprod. 2007;22:1506–12. doi: 10.1093/humrep/dem046. [DOI] [PubMed] [Google Scholar]
- 2.Nallella KP, Sharma RK, Aziz N, Agarwal A. Significance of sperm characteristics in the evaluation of male infertility. Fertil Steril. 2006;85:629–34. doi: 10.1016/j.fertnstert.2005.08.024. [DOI] [PubMed] [Google Scholar]
- 3.Omu AE. Sperm parameters: paradigmatic index of good health and longevity. Med Princ Pract. 2013;22(Suppl 1):30–42. doi: 10.1159/000354208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Jonge CJ, Barratt CL. WHO manual... who should care? Hum Reprod. 1999;14:2431–3. doi: 10.1093/humrep/14.10.2431. [DOI] [PubMed] [Google Scholar]
- 5.Pacey AA. Is quality assurance in semen analysis still really necessary? A view from the andrology laboratory. Hum Reprod. 2006;21:1105–9. doi: 10.1093/humrep/dei460. [DOI] [PubMed] [Google Scholar]
- 6.Phillips KP, Tanphaichitr N. Human exposure to endocrine disrupters and semen quality. J Toxicol Environ Health B Crit Rev. 2008;11:188–220. doi: 10.1080/10937400701873472. [DOI] [PubMed] [Google Scholar]
- 7.5th ed. Geneva: WHO; 2010. WHO. WHO Laboratory Manual for the Examination and Processing of Human Semen. [Google Scholar]
- 8.Esteves SC, Zini A, Aziz N, Alvarez JG, Sabanegh ES, Jr, et al. Critical appraisal of World Health Organization's new reference values for human semen characteristics and effect on diagnosis and treatment of subfertile men. Urology. 2012;79:7. doi: 10.1016/j.urology.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 9.Carrell DT, Cartmill D. A brief review of current and proposed federal government regulation of assisted reproduction laboratories in the United States. J Androl. 2006;23:611–7. [PubMed] [Google Scholar]
- 10.Bjorndahl L, Kjellberg S, Kvist U. Ejaculatory sequence in men with low sperm chromatin-zinc. Int J Androl. 1991;14:174–8. doi: 10.1111/j.1365-2605.1991.tb01079.x. [DOI] [PubMed] [Google Scholar]
- 11.Bjorndahl L, Kvist U. Influence of seminal vesicular fluid on the zinc content of human sperm chromatin. Int J Androl. 1990;13:232–7. doi: 10.1111/j.1365-2605.1990.tb00981.x. [DOI] [PubMed] [Google Scholar]
- 12.Lindholmer C. Survival of human spermatozoa in different fractions of split ejaculate. Fertil Steril. 1973;24:521–6. [PubMed] [Google Scholar]
- 13.Macleod J, Gold RZ. The male factor in fertility and infertility. III. An analysis of motile activity in the spermatozoa of 1000 fertile men and 1000 men in infertile marriage. Fertil Steril. 1951;2:187–204. [PubMed] [Google Scholar]
- 14.Cooper TG, Brazil C, Swan SH, Overstreet JW. Ejaculate volume is seriously underestimated when semen is pipetted or decanted into cylinders from the collection vessel. J Androl. 2007;28:1–4. doi: 10.2164/jandrol.106.001297. [DOI] [PubMed] [Google Scholar]
- 15.4th ed. Cambridge, UK: Cambridge University Press; 1999. WHO. WHO Laboratory Manual for the Examination of Human Semen and Sperm-cervical Mucus Interaction. [Google Scholar]
- 16.Mortimer D. The essential partnership between diagnostic andrology and modern assisted reproductive technologies. Hum Reprod. 1994;9:1209–13. doi: 10.1093/oxfordjournals.humrep.a138680. [DOI] [PubMed] [Google Scholar]
- 17.Ayala C, Steinberger E, Smith DP. The influence of semen analysis parameters on the fertility potential of infertile couples. J Androl. 1996;17:718–25. [PubMed] [Google Scholar]
- 18.Smith KD, Rodriguez-Rigau LJ, Steinberger E. Relation between indices of semen analysis and pregnancy rate in infertile couples. Fertil Steril. 1977;28:1314–9. doi: 10.1016/s0015-0282(16)42976-6. [DOI] [PubMed] [Google Scholar]
- 19.Cooper TG, Neuwinger J, Bahrs S, Nieschlag E. Internal quality control of semen analysis. Fertil Steril. 1992;58:172–8. [PubMed] [Google Scholar]
- 20.Freund M, Carol B. Factors affecting haemocytometer counts of sperm concentration in human semen. J Reprod Fertil. 1964;8:149–55. doi: 10.1530/jrf.0.0080149. [DOI] [PubMed] [Google Scholar]
- 21.Keel BA. How reliable are results from the semen analysis? Fertil Steril. 2004;82:41–4. doi: 10.1016/j.fertnstert.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 22.Ginsburg KA, Armant DR. The influence of chamber characteristics on the reliability of sperm concentration and movement measurements obtained by manual and videomicrographic analysis. Fertil Steril. 1990;53:882–7. doi: 10.1016/s0015-0282(16)53526-2. [DOI] [PubMed] [Google Scholar]
- 23.Johnson JE, Boone WR, Blackhurst DW. Manual versus computer-automated semen analyses. Part I. Comparison of counting chambers. Fertil Steril. 1996;65:150–5. doi: 10.1016/s0015-0282(16)58043-1. [DOI] [PubMed] [Google Scholar]
- 24.Schrader SM, Chapin RE, Clegg ED, Davis RO, Fourcroy JL, et al. Laboratory methods for assessing human semen in epidemiologic studies: a consensus report. Reprod Toxicol. 1992;6:275–9. doi: 10.1016/0890-6238(92)90184-u. [DOI] [PubMed] [Google Scholar]
- 25.Schrader SM, Ratcliffe JM, Turner TW, Hornung RW. The use of new field methods of semen analysis in the study of occupational hazards to reproduction: the example of ethylene dibromide. J Occup Med. 1987;29:963–6. [PubMed] [Google Scholar]
- 26.Souchier C, Czyba JC, Grantham R. Difficulties in morphologic classification of human spermatozoa. J Reprod Med. 1978;21:244–8. [PubMed] [Google Scholar]
- 27.Menkveld R. The basic semen analysis. In: Oehringer S, Kruger TF, editors. Male Infertility. Ch. 9. Oxford: Informa Healthcare, UK; 2007. pp. 141–70. [Google Scholar]
- 28.Kvist U, Björndahl L. Manual on Basic Semen Analysis. Oxford: Oxford University Press; 2002. [DOI] [PubMed] [Google Scholar]
- 29.Oettlé EE. Using a new acrosome stain to evaluate sperm morphology. Vet Med. 1986;81:263–6. [Google Scholar]
- 30.3rd ed. Cambridge, UK: Cambridge University Press; 1992. WHO. WHO Laboratory Manual for the Examination of Human Semen and Sperm-cervical Mucus. [Google Scholar]
- 31.Kruger TF, Acosta AA, Simmons KF, Swanson RJ, Matta JF, et al. Predictive value of abnormal sperm morphology in in vitro fertilization. Fertil Steril. 1988;49:112–7. doi: 10.1016/s0015-0282(16)59660-5. [DOI] [PubMed] [Google Scholar]
- 32.Macleod J. A possible factor in the etiology of human male infertility: preliminary report. Fertil Steril. 1962;13:29–33. doi: 10.1016/s0015-0282(16)34383-7. [DOI] [PubMed] [Google Scholar]
- 33.2nd ed. Cambridge, UK: Cambridge University Press; 1987. WHO. Laboratory Manual for the Examination of Human Semen and Sperm-cervical Mucus Interaction. [Google Scholar]
- 34.Chow V, Cheung AP. Male infertility. J Reprod Med. 2006;51:149–56. [PubMed] [Google Scholar]
- 35.Freund M. Standards for the rating of human sperm morphology. A cooperative study. Int J Fertil. 1966;11:97–180. [PubMed] [Google Scholar]
- 36.Davis RO, Gravance CG. Consistency of sperm morphology classification methods. J Androl. 1994;15:83–91. [PubMed] [Google Scholar]
- 37.Davis RO, Gravance CG, Overstreet JW. A standardized test for visual analysis of human sperm morphology. Fertil Steril. 1995;63:1058–63. doi: 10.1016/s0015-0282(16)57548-7. [DOI] [PubMed] [Google Scholar]
- 38.Franken DR, Barendsen R, Kruger TF. A continuous quality control program for strict sperm morphology. Fertil Steril. 2000;74:721–4. doi: 10.1016/s0015-0282(00)01498-9. [DOI] [PubMed] [Google Scholar]
- 39.Turek PJ. Immunopathology and infertility. Philadelphia, PA: Mosby Year Book; 1997. [Google Scholar]
- 40.Sikka SC, Hellstrom WJG. infertility in the Male. 4th edition. Chapter 37. Cambridge UK: ed Larry Lipshultz, Stuart Howards and Craig Niederberger, Cambridge Univ. Press; 2009. Tests for Antisperm Antibodies; pp. 603–12. [Google Scholar]
- 41.Ochsendorf FR. Sexually transmitted infections: impact on male fertility. Andrologia. 2008;40:72–5. doi: 10.1111/j.1439-0272.2007.00825.x. [DOI] [PubMed] [Google Scholar]
- 42.Linsenmeyer TA, Perkash I. Infertility in men with spinal cord injury. Arch Phys Med Rehabil. 1991;72:747–54. [PubMed] [Google Scholar]
- 43.Armstrong JS, Rajasekaran M, Hellstrom WJ, Sikka SC. Antioxidant potential of human serum albumin: role in the recovery of high quality human spermatozoa for assisted reproductive technology. J Androl. 1998;19:412–9. [PubMed] [Google Scholar]
- 44.Cooper TG, Noonan E, von Eckardstein S, Auger J, Baker HW, et al. World Health Organization reference values for human semen characteristics. Hum Reprod Update. 2010;16:231–45. doi: 10.1093/humupd/dmp048. [DOI] [PubMed] [Google Scholar]
- 45.Bjorndahl L, Mortimer D, Barratt CLR, Castilla JA, Menkveld R, et al. A Practical Guide to Basic Laboratory Andrology. Cambridge, UK: Cambridge University Press; 2010. p. 264. [Google Scholar]
- 46.Davis RO, Katz DF. Computer-aided sperm analysis: technology at a crossroads. Fertil Steril. 1993;59:953–5. doi: 10.1016/s0015-0282(16)55909-3. [DOI] [PubMed] [Google Scholar]
- 47.Mortimer ST, Swan MA. Variable kinematics of capacitating human spermatozoa. Hum Reprod. 1995;10:3178–82. doi: 10.1093/oxfordjournals.humrep.a135882. [DOI] [PubMed] [Google Scholar]
- 48.Bastiaan HS, Menkveld R, Oehninger S, Franken DR. Zona pellucida induced acrosome reaction, sperm morphology, and sperm-zona binding assessments among subfertile men. J Assist Reprod Genet. 2002;19:329–34. doi: 10.1023/A:1016058625874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu DY, Stewart T, Baker HW. Normal range and variation of the zona pellucida-induced acrosome reaction in fertile men. Fertil Steril. 2003;80:384–9. doi: 10.1016/s0015-0282(03)00603-4. [DOI] [PubMed] [Google Scholar]
- 50.Yanagimachi R, Yanagimachi H, Rogers BJ. The use of zona-free animal ova as a test-system for the assessment of the fertilizing capacity of human spermatozoa. Biol Reprod. 1976;15:471–6. doi: 10.1095/biolreprod15.4.471. [DOI] [PubMed] [Google Scholar]
- 51.Agarwal A, Allamaneni SS. The effect of sperm DNA damage on assisted reproduction outcomes. A review. Minerva Ginecol. 2004;56:235–45. [PubMed] [Google Scholar]
- 52.Tandara M, Bajic A, Tandara L, Bilic-Zulle L, Sunj M, et al. Sperm DNA integrity testing: big halo is a good predictor of embryo quality and pregnancy after conventional IVF. Andrology. 2014;2:678–86. doi: 10.1111/j.2047-2927.2014.00234.x. [DOI] [PubMed] [Google Scholar]
- 53.McMaster GK, Carmichael GG. Analysis of single- and double-stranded nucleic acids on polyacrylamide and agarose gels by using glyoxal and acridine orange. Proc Natl Acad Sci U S A. 1977;74:4835–8. doi: 10.1073/pnas.74.11.4835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Evenson DP. Sperm chromatin structure assay (SCSA (R)) Methods Mol Biol. 2013;927:147–64. doi: 10.1007/978-1-62703-038-0_14. [DOI] [PubMed] [Google Scholar]
- 55.Duran EH, Morshedi M, Taylor S, Oehninger S. Sperm DNA quality predicts intrauterine insemination outcome: a prospective cohort study. Hum Reprod. 2002;17:3122–8. doi: 10.1093/humrep/17.12.3122. [DOI] [PubMed] [Google Scholar]
- 56.Olive PL, Durand RE, Banath JP, Johnston PJ. Analysis of DNA damage in individual cells. Methods Cell Biol. 2001;64:235–49. doi: 10.1016/s0091-679x(01)64016-0. [DOI] [PubMed] [Google Scholar]
- 57.Fernandez JL, Muriel L, Goyanes V, Segrelles E, Gosalvez J, et al. Simple determination of human sperm DNA fragmentation with an improved sperm chromatin dispersion test. Fertil Steril. 2005;84:833–42. doi: 10.1016/j.fertnstert.2004.11.089. [DOI] [PubMed] [Google Scholar]
- 58.Henkel R, Hoogendijk CF, Bouic PJ, Kruger TF. TUNEL assay and SCSA determine different aspects of sperm DNA damage. Andrologia. 2010;42:305–13. doi: 10.1111/j.1439-0272.2009.01002.x. [DOI] [PubMed] [Google Scholar]
- 59.Tremellen K. Oxidative stress and male infertility – A clinical perspective. Hum Reprod Update. 2008;14:243–58. doi: 10.1093/humupd/dmn004. [DOI] [PubMed] [Google Scholar]
- 60.Holland MK, Alvarez JG, Storey BT. Production of superoxide and activity of superoxide dismutase in rabbit epididymal spermatozoa. Biol Reprod. 1982;27:1109–18. doi: 10.1095/biolreprod27.5.1109. [DOI] [PubMed] [Google Scholar]
- 61.Fraga CG, Motchnik PA, Shigenaga MK, Helbock HJ, Jacob RA, et al. Ascorbic acid protects against endogenous oxidative DNA damage in human sperm. Proc Natl Acad Sci U S A. 1991;88:11003–6. doi: 10.1073/pnas.88.24.11003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sikka SC, Rajasekaran M, Hellstrom WJG. role of oxidative stress and antioxidants in male infertility. J Androl. 1995;16:464–71. [PubMed] [Google Scholar]
- 63.Alvarez JG, Storey BT. Differential incorporation of fatty acids into and peroxidative loss of fatty acids from phospholipids of human spermatozoa. Mol Reprod Dev. 1995;42:334–46. doi: 10.1002/mrd.1080420311. [DOI] [PubMed] [Google Scholar]
- 64.Aitken RJ, Baker HW. Seminal leukocytes: passengers, terrorists or good samaritans? Hum Reprod. 1995;10:1736–9. doi: 10.1093/oxfordjournals.humrep.a136165. [DOI] [PubMed] [Google Scholar]
- 65.Aitken RJ, West K, Buckingham D. Leukocytic infiltration into the human ejaculate and its association with semen quality, oxidative stress, and sperm function. J Androl. 1994;15:343–52. [PubMed] [Google Scholar]
- 66.Aitken RJ. A free radical theory of male infertility. Reprod Fertil Dev. 1994;6:19–23. doi: 10.1071/rd9940019. [DOI] [PubMed] [Google Scholar]
- 67.Agarwal A, Ikemoto I, Loughlin KR. Relationship of sperm parameters with levels of reactive oxygen species in semen specimens. J Urol. 1994;152:107–10. doi: 10.1016/s0022-5347(17)32829-x. [DOI] [PubMed] [Google Scholar]
- 68.Aitken RJ, Clarkson JS, Fishel S. Generation of reactive oxygen species, lipid peroxidation, and human sperm function. Biol Reprod. 1989;41:183–97. doi: 10.1095/biolreprod41.1.183. [DOI] [PubMed] [Google Scholar]
- 69.Sharma RK, Agarwal A. Role of reactive oxygen species in male infertility. Urology. 1996;48:835–50. doi: 10.1016/s0090-4295(96)00313-5. [DOI] [PubMed] [Google Scholar]
- 70.Kashou AH, Sharma R, Agarwal A. Assessment of oxidative stress in sperm and semen. Methods Mol Biol. 2013;927:351–61. doi: 10.1007/978-1-62703-038-0_30. [DOI] [PubMed] [Google Scholar]
- 71.Kobayashi H, Gil-Guzman E, Mahran AM, Rakesh, Nelson DR, et al. Quality control of reactive oxygen species measurement by luminol-dependent chemiluminescence assay. J Androl. 2001;22:568–74. [PubMed] [Google Scholar]
- 72.Aitken RJ, Baker MA, O’Bryan M. Shedding light on chemiluminescence: the application of chemiluminescence in diagnostic andrology. J Androl. 2004;25:455–65. doi: 10.1002/j.1939-4640.2004.tb02815.x. [DOI] [PubMed] [Google Scholar]
- 73.Armstrong JS, Bivalacqua TJ, Chamulitrat W, Sikka S, Hellstrom WJ. A comparison of the NADPH oxidase in human sperm and white blood cells. Int J Androl. 2002;25:223–9. doi: 10.1046/j.1365-2605.2002.00351.x. [DOI] [PubMed] [Google Scholar]
- 74.Baehner RL, Boxer LA, Davis J. The biochemical basis of nitroblue tetrazolium reduction in normal human and chronic granulomatous disease polymorphonuclear leukocytes. Blood. 1976;48:309–13. [PubMed] [Google Scholar]
- 75.Esfandiari N, Sharma RK, Saleh RA, Thomas AJ, Jr, Agarwal A. Utility of the nitroblue tetrazolium reduction test for assessment of reactive oxygen species production by seminal leukocytes and spermatozoa. J Androl. 2003;24:862–70. doi: 10.1002/j.1939-4640.2003.tb03137.x. [DOI] [PubMed] [Google Scholar]
- 76.Jones R, Mann T, Sherins R. Peroxidative breakdown of phospholipids in human spermatozoa, spermicidal properties of fatty acid peroxides, and protective action of seminal plasma. Fertil Steril. 1979;31:531–7. doi: 10.1016/s0015-0282(16)43999-3. [DOI] [PubMed] [Google Scholar]
- 77.de Lamirande E, Gagnon C. Impact of reactive oxygen species on spermatozoa: a balancing act between beneficial and detrimental effects. Hum Reprod. 1995;10(Suppl 1):15–21. doi: 10.1093/humrep/10.suppl_1.15. [DOI] [PubMed] [Google Scholar]
- 78.Sharma RK, Pasqualotto FF, Nelson DR, Thomas AJ, Jr, Agarwal A. The reactive oxygen species-total antioxidant capacity score is a new measure of oxidative stress to predict male infertility. Hum Reprod. 1999;14:2801–7. doi: 10.1093/humrep/14.11.2801. [DOI] [PubMed] [Google Scholar]
- 79.Toft G, Rignell-Hydbom A, Tyrkiel E, Shvets M, Giwercman A. Quality control workshops in standardization of sperm concentration and motility assessment in multicentre studies. Int J Androl. 2005;28:144–9. doi: 10.1111/j.1365-2605.2005.00518.x. [DOI] [PubMed] [Google Scholar]
- 80.Hassemer DJ. Interlaboratory surveys to assess performance: more than proficiency testing. MLO Med Lab Obs. 2006;38:20. [PubMed] [Google Scholar]
- 81.Auger J, Eustache F, Ducot B, Blandin T, Daudin M, et al. Intra- and inter-individual variability in human sperm concentration, motility and vitality assessment during a workshop involving ten laboratories. Hum Reprod. 2000;15:2360–8. doi: 10.1093/humrep/15.11.2360. [DOI] [PubMed] [Google Scholar]
- 82.Jorgensen N, Auger J, Giwercman A, Irvine DS, Jensen TK, et al. Semen analysis performed by different laboratory teams: an intervariation study. Int J Androl. 1997;20:201–8. doi: 10.1046/j.1365-2605.1997.00052.x. [DOI] [PubMed] [Google Scholar]


