ABSTRACT
Background:
This study investigated the effect of a high ratio of fresh frozen plasma (FFP) to red blood cells (RBCs) within the first 6 and 24 h after admission on mortality in patients with severe, blunt trauma.
Methods:
This retrospective observational study included 189 blunt trauma patients with an Injury Severity Score (ISS) ≥16 requiring RBC transfusions within the first 24 h. Receiver operating characteristic (ROC) curve analysis was performed to calculate cut-off values of the FFP/RBC ratio for outcome. The patients were then divided into two groups according to the cut-off value. Patient survival was compared between groups using propensity score matching (PSM).
Results:
The area under the ROC curve was 0.57, and the FFP/RBC ratio was 1.0 at maximum sensitivity (0.57) and specificity (0.67). All patients were then divided into two groups (FFP/RBC ratio ≥1 or <1) and analyzed using PSM and inverse probability of treatment weighting (IPTW). The unadjusted hazard ratio (HR) was 0.44, and the adjusted HR was 0.29. The HR was 0.38 by PSM and 0.41 by IPTW. The survival rate was significantly higher in patients with an FFP/RBC ratio ≥1 within the first 6 h.
Conclusions:
Severe blunt trauma patients transfused with an FFP/RBC ratio ≥1 within the first 6 h had an HR of about 0.4. The transfusion of an FFP/RBC ratio ≥1 within the first 6 h was associated with the outcomes of blunt trauma patients with ISS ≥16 who need a transfusion within 24 h.
Keywords: Blood transfusion, blunt trauma, FFP, fresh frozen plasma, propensity score
INTRODUCTION
Damage control resuscitation (DCR) was proposed in the latter half of the 2000s as a treatment strategy for severe trauma patients with major bleeding (1, 2). This involves planned treatment bundles to reduce mortality rates, including aggressive transfusion of fresh frozen plasma (FFP) and platelets early during treatment (3). Various FFP-packed red blood cell (RBC) ratios were reported, with many recommending a 1:1 ratio (4–6).
Although it has been suggested that a higher FFP/RBC ratio reduces mortality in patients requiring massive transfusions, the time window to accomplish the proposed ratio of FFP/RBC is unclear. Snyder et al. (7), using a Cox proportional hazards analysis with time-dependent variables, found no significant correlation between the FFP/RBC ratio and the mortality rate. However, Holcomb et al. (8) recently performed a prospective, multicenter, observational study and reported that higher plasma and platelet ratios early in resuscitation were associated with decreased mortality in patients who received transfusions of at least 3 units of blood products within 24 h after admission. Cox hazards regression analysis showed that higher FFP/RBC ratios (≥1) were independently associated with decreased 6-h mortality.
The reported studies for the transfusion strategy, including a higher plasma/RBC ratio, were constructed with a study population that consisted of penetrating trauma rates of 40% to 60% (4–9). However, there are many areas or countries with different study populations in which blunt trauma patients are predominant. The Trauma Register of the German Trauma Society (DGU) (10) and the Japan Trauma Data Bank (11) have reported that the rates of blunt trauma were 94.9% and 94.1%, respectively. Patients with blunt trauma and penetrating trauma have a different mechanism of coagulopathy. Blunt trauma stimulates the production of tissue factor and factor VII, which can activate excessive coagulation (12, 13). Therefore, the effective FFP/RBC ratio for patients with blunt trauma can differ from that for penetrating trauma.
This study investigated the effect of a high FFP/RBC ratio within the first 6 h and 24 h after admission on mortality in patients with severe blunt trauma (injury severity score (ISS) ≥16) requiring blood transfusion for resuscitation.
PATIENTS AND METHODS
The Japanese Observational Study for Coagulation and Thrombolysis in Early Trauma (J-OCTET), a multicenter, retrospective study, was planned by the Committee for Future Planning of the Japanese Association for the Surgery of Trauma, and a database was created.
In this retrospective study, data were collected from trauma patients, age ≥18 years and with ISS ≥16, who were admitted to committee member hospitals between January and December 2012. Before creation of the database, 117 patient parameters considered suitable for the purposes of this study by the committee members were selected from the clinical perspective.
Fifteen medical institutions participated, and 796 patients were registered. The present study targeted blunt trauma patients who were transfused early after admission, to investigate the effect of a high FFP/RBC ratio on mortality in patients requiring blood transfusion for resuscitation. Therefore, 201 blunt trauma patients who received RBC transfusions within the first 24 h were included.
The parameters investigated in the present study were selected from this database. When several parameters were judged clinically to have strong correlations, one of them that was clinically relevant was selected as a parameter representative of all of them. The background characteristics of patients included age, sex, mechanism of injury, and use of anticoagulant/antiplatelet drugs. The prehospital data included fluid therapy before admission. The hospital admission data included the ISS (14), heart rate (HR), systolic blood pressure (SBP), and respiratory rate (RR). The interventions after admission included use of tranexamic acid within the first 3 h. Transfusion volumes (units), including RBCs, FFP, and platelets, within the first 6 and 24 h were reviewed. The FFP/RBC ratios at 6 and 24 h were also calculated. The follow-up observation period was until hospital discharge.
The present study was approved by the ethics committee of each hospital and the Japanese Association for the Surgery of Trauma.
Statistical analysis
For the explanatory variables, normality of continuous variables was assessed by the Shapiro–Wilk test. For two-group comparisons, data with a normal distribution were examined with the t test, and data with a non-normal distribution were examined by the Mann–Whitney U test. Before multivariate analysis, the variance inflation factor (VIF) for each explanatory variable was calculated. A VIF ≥5 was regarded as showing multicollinearity, and variables with a VIF ≥5 were excluded. The VIF for each explanatory variable was recalculated and repeated until all explanatory variables had a VIF <5. Cox proportional hazards analysis (Cox analysis) was performed with these explanatory variables.
Receiver-operating characteristic (ROC) curve analysis was performed to calculate cut-off values for the FFP/RBC ratio as the explanatory variable for survival or death at discharge as the response variable. The FFP and the RBC refer to the units of FFP and RBCs transfused within the first 6 h. Thereafter, the patients were divided into two groups according to the FFP/RBC ratio cut-off value. Differences in the Kaplan–Meier curves between the two groups were compared by the log-rank test.
Caliper propensity score matching (PSM) was used to match these two groups. The caliper scale was 0.003. The standardized difference test was used to measure covariate balance, whereby an absolute standardized difference above 0.1 represents a meaningful imbalance (15). In addition, the two groups were compared using inverse probability of treatment weighting (IPTW), with inverse weighting of the propensity score (16). P < 0.05 was considered significant.
All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan) (17), which is a graphical user interface for R v3.1.1 (The R Foundation for Statistical Computing, Vienna, Austria). More precisely, it is a modified version of R commander designed to add statistical functions frequently used in biostatistics.
RESULTS
Patients’ characteristics and outcomes
Table 1 shows the patients’ characteristics. A total of 139 blunt trauma patients survived and were discharged alive, and 62 blunt trauma patients died. Age and the ISS were significantly higher in the non-survivors.
Table 1.
Patients’ background characteristics and outcomes at hospital discharge
| Survivors | Non-survivors | P value | ||
| n | 139 | 62 | ||
| Sex (%) | Male | 93 (66.9) | 43 (69.4) | 0.87 |
| Age | 48.0 [32.5, 69.5] | 62.0 [45.5, 71.8] | 0.017* | |
| Prehospital fluid (%) | Yes | 19 (13.7) | 11 (17.7) | 0.52 |
| Anticoagulant and/or antiplatelet (%) | Yes | 8 (5.6) | 2 (3.2) | 0.727 |
| Tranexamic acid ≤3 h (%)* | No | 76 (54.7) | 35 (56.5) | 0.88 |
| Yes | 63 (45.3) | 27 (43.5) | ||
| ISS | 26.0 [22.0, 35.0] | 36.50[26.0, 41.0] | <0.001* | |
| Head or neck | AIS code ≤ 3 | 40 (31.2) | 19 (31.1) | 0.02 |
| 4 | 23 (18.0) | 11 (18.0) | ||
| 5 | 17 (13.3) | 24 (39.3) | ||
| Face | ≤3 | 22 (17.2) | 4 (6.6) | |
| Chest | ≤3 | 38 (29.7) | 16 (26.2) | 0.497 |
| 4 | 31 (24.2) | 20 (32.8) | ||
| 5 | 12 (9.4) | 4 (6.6) | ||
| Abdomen or pelvic contents | ≤3 | 108 (84.3) | 53 (86.9) | 0.261 |
| 4 | 19 (14.8) | 6 (9.8) | ||
| 5 | 1 (0.8) | 2 (3.3) | ||
| Extremities or pelvic girdle | ≤3 | 47 (36.7) | 18 (29.5) | 0.364 |
| 4 | 19 (14.8) | 11 (18.0) | ||
| 5 | 10 (7.8) | 8 (13.1) | ||
| External | ≤3 | 125 (97.7) | 61 (100) | 1.000 |
| 4 | 1 (0.8) | 0 (0.0) | ||
| RBC within 6 h (U) | 6.0 [4.0, 10.0] | 16.0 [8.0, 23.5] | <0.001* | |
| FFP within 6 h (U) | 6.0 [2.0, 10.0] | 10.0 [5.3, 20.0] | 0.001* | |
| FFP/RBC ratio at 6 h | 1.0 [0.5, 1.3] | 0.8 [0.6, 1.0] | 0.066 | |
| Platelet trans. ≤6 h (%)** | 0 U | 111 (79.9) | 38 (61.3) | 0.001* |
| 5 U | 1 (0.7) | 0 (0.0) | ||
| 10 U | 13 (9.4) | 5 (8.1) | ||
| 15 U | 1 (0.7) | 2 (3.2) | ||
| 20 U | 9 (6.5) | 15 (24.2) | ||
| 25 U | 0 (0.0) | 1 (1.6) | ||
| 30 U | 0 (0.0) | 1 (1.6) | ||
| 35 U | 1 (0.7) | 0 (0.0) | ||
| 40 U | 3 (2.2) | 0 (0.0) | ||
| RBC within 24 h (U) | 10.0 [6.0, 17.0] | 18.0 [10.0, 28.0] | <0.001* | |
| FFP within 24 h (U) | 10.0 [4.0, 17.0] | 16.0 [8.0, 20.0] | 0.018* | |
| FFP/RBC ratio at 24 h | 1.0 [0.6, 1.3] | 0.83 [0.6, 1.1] | 0.177 | |
| Platelet trans. ≤24 h (%) | 0 U | 90 (64.7) | 30 (48.4) | 0.182 |
| 10 U | 16 (11.5) | 6 (9.7) | ||
| 15 U | 3 (2.2) | 3 (4.8) | ||
| 20 U | 20 (14.4) | 18 (29.0) | ||
| 30 U | 3 (2.2) | 3 (4.8) | ||
| 40 U | 3 (2.2) | 1 (1.6) | ||
| 50 U | 2 (1.4) | 1 (1.6) | ||
| 55 U | 1 (0.7) | 0 (0.0) | ||
| 100 U | 1 (0.7) | 0 (0.0) | ||
| Heart rate on admission | 100.0 [79.0, 120.0] | 103.0 [83.0, 120.0] | 0.753 | |
| SBP on admission (mmHg) | 110.0 [89.0, 140.0] | 118.0 [80.0, 142.5] | 0.623 | |
| Respiratory rate on admission | 23.5 [20.0, 30.0] | 22.0 [18.0, 29.5] | 0.53 | |
| WBC on admission (×103/μL) | 11.9 [9.0, 17.0] | 11.8 [8.7, 15.6] | 0.718 | |
| Hb on admission (g/dL) | 11.9 [10.2, 13.5] | 11.9 [10.1, 14.0] | 0.999 | |
| PLT on admission (×104/μL) | 20.0 [15.5, 25.2] | 18.50 [14.25, 22.53] | 0.046 | |
| CPK on admission (IU/L) n = 204 | 373.0 [217.0, 645.0] | 320.0 [218.0, 522.0] | 0.916 | |
| Base excess on admission n = 198 | −3.4 [−6.4, −1.1] | −5.5 [−10.5, −3.7] | <0.001* |
*Shows a significant difference (P < 0.05) median [25th percentile, 75th percentile].
Prehospital fluid: whether the patients received intravenous infusion before admission or not.
Anticoagulant and/or antiplatelet: whether the patients had been receiving these drugs based on their history.
Tranexamic acid ≤3 h: whether the patients received tranexamic acid intravenously within 3 h after admission.
RBC within 6 h (U): the total number of units of packed red blood cells that the patients received within 6 h after admission.
FFP within 6 h (U): the total number of units of fresh frozen plasma that the patients received within 6 h after admission.
FFP/RBC ratio at 6 h: the total number of units of fresh frozen plasma that the patients received within 6 h after admission divided by the total number units of packed red blood cells.
Platelet trans. ≤6 h: the total number of units of platelet transfusion within the first 6 h after admission.
AIS indicates abbreviated injury scale; CPK, creatine phosphokinase; Hb, hemoglobin; ISS, injury severity score; PLT, platelet count; SBP, systolic blood pressure; WBC, white blood cell count.
The mean volume of RBCs or FFP transfused within the first 6 h was significantly higher in the non-survivor group than in the survivor group. The mean volume of RBCs or FFP transfused within the first 24 h was significantly higher in the non-survivor group. Platelet transfusion volume within the first 6 h was also significantly greater in the non-survivor group. The blood test results on admission showed that the base excess (BE) was significantly lower in the non-survivor group. The VIF was calculated for each parameter in Table 1. The VIF was ≥5 for volume of RBCs and FFP within the first 6 and 24 h. These parameters were excluded from the Cox analysis.
Cox analysis and the FFP/RBC ratio cut-off value
Since 12 patients had missing values, Cox analysis included 189 blunt trauma patients. Significant factors were age, ISS, platelet transfusion volume within the first 6 h, the FFP/RBC ratio at 6 h, SBP on admission, hemoglobin (Hb) on admission, and BE on admission (see Supplement Table 1, Supplemental Digital Content 1).
Using the FFP/RBC ratio at 6 h, which was the significant independent variable on Cox analysis, ROC curve analysis was performed for survival at discharge as the response variable. The area under the curve (AUC) was 0.57 (0.50–0.66), and the FFP/RBC ratio was 1.0 at maximum sensitivity (0.57) and specificity (0.67). This ratio of 1.0 was set as the cut-off value. This cut-off value was then used to divide the patients into two groups (based on an FFP/RBC ratio ≥1 and an FFP/RBC ratio <1.0), and Cox analysis was again performed (Table 2). The significant factors were age, ISS, platelet transfusion volume within the first 6 h, FFP/RBC ratio ≥1 within 6 h, SBP on admission, Hb on admission, and BE on admission. These significant factors were equal to the factors presented in Supplement Table 1, Supplemental Digital Content 1. It was found that transfusion of an FFP/RBC ratio ≥1 or <1 within the first 6 h was the significant independent variable for patients’ outcomes.
Table 2.
Cox proportional hazards analysis of time to death of enrolled patients (n = 189)
| Hazard ratio (95% CI) | P value | |
| Age | 1.02 (1.00–1.03) | 0.045* |
| Sex | 1.40 (0.73–2.67) | 0.310 |
| Prehospital fluid | 1.13 (0.53–2.40) | 0.760 |
| Anticoagulant and/or antiplatelet | 0.47 (0.10–2.21) | 0.340 |
| ISS | 1.05 (1.03–1.08) | <0.001* |
| Tranexamic acid ≤3 h | 0.75 (0.42–1.31) | 0.310 |
| Platelet trans. ≤6 h | 1.32 (1.04–1.68) | 0.023* |
| FFP/RBC ratio ≥ 1 within 6 h† | 0.29 (0.14–0.62) | 0.001* |
| Platelet trans. ≤ 24 h | 0.92 (0.78–1.10) | 0.370 |
| FFP/RBC ratio ≥ 1 within 24 h† | 1.27 (0.59–2.74) | 0.540 |
| HR on admission | 0.99 (0.98–1.01) | 0.330 |
| SBP on admission | 1.01 (1.00–1.02) | 0.045* |
| RR on admission | 0.98 (0.95–1.01) | 0.250 |
| WBC on admission | 1.00 (0.94–1.06) | 0.980 |
| Hb on admission | 1.16 (1.01–1.34) | 0.032* |
| PLT on admission | 0.95 (0.90–1.00) | 0.041* |
| CPK on admission | 1.00 (1.00–1.00) | 0.260 |
| Base excess on admission | 0.90 (0.85–0.96) | 0.001* |
*Shows a significant difference (P < 0.05).
†This factor was composed of two categorical variables: FFP/RBC ratio ≥1 or FFP/RBC <1.
Prehospital fluid: whether the patients received intravenous infusion before admission or not.
Anticoagulant and/or antiplatelet: whether the patients had been receiving these drugs based on their history.
Tranexamic acid ≤3 h: whether the patients received tranexamic acid intravenously within 3 h after admission.
FFP/RBC ratio within 6 h: the ratio of the total number units of fresh frozen plasma that the patients received within the first 6 h after admission to the total number units of packed red blood cells.
Platelet trans. ≤6 h: the total number of units of platelet transfusion within the first 6 h after admission.
CPK indicates creatine phosphokinase; Hb, haemoglobin; ISS, injury severity score; PLT, platelet count; SBP, systolic blood pressure; WBC, white blood cell count.
Comparison of outcomes between groups by propensity score matching (PSM)
PSM was performed to compare the two groups (FFP/RBC ratio ≥1 within the first 6 h and FFP/RBC ratio <1 within the first 6 h). The propensity score was created from the following 13 covariates: age, fluid therapy before admission, use of anticoagulant/antiplatelet drugs, ISS, use of tranexamic acid, HR, SBP, RR, WBC, Hb, PLT, CPK, and BE.
Before the matching, there were 96 patients with an FFP/RBC ratio <1 within the first 6 h, and 93 patients with an FFP/RBC ratio ≥1 within the first 6 h (see Supplement Table 2, Supplemental Digital Content 1). Although there were no significant differences in all covariates, 7 of 13 covariates had absolute standardized differences ≥1.0, which represented meaningful imbalance.
Table 3 shows the PSM results. There were 53 patients with an FFP/RBC ratio <1 within the first 6 h, and 53 patients with an FFP/RBC ratio ≥1 within the first 6 h. All covariates had absolute standardized differences <1.0. Figure 1 shows Kaplan–Meier curves for the patients after PSM. Patients with an FFP/RBC ratio ≥1 within the first 6 h had significantly better survival (log-rank test; P = 0.022).
Table 3.
Comparison between patients with/without FFP/RBC ratio ≥1 within 6 h with propensity score matching
| FFP/RBC ≥1 within 6 h | |||||
| No | Yes | P value | Standardized difference test | ||
| n | 53 | 53 | |||
| Age | 53.0 [18.0, 87.0] | 50.0 [22.0, 90.0] | 0.914 | 0.08 | |
| Prehospital fluid (%) | Yes | 7 (13.2) | 9 (17.0) | 0.787 | 0.05 |
| Anticoagulant and/or antiplatelet (%) | Yes | 3 (5.7) | 3 (5.7) | 1 | 0.00 |
| ISS | 29.0 [16.0, 66.0] | 29.0 [16.0, 57.0] | 0.766 | 0.04 | |
| Tranexamic acid ≤3 h (%) | Yes | 26 (49.1) | 22 (41.5) | 0.559 | 0.08 |
| Heart rate on admission | 101.0 [42.0, 161.0] | 94.0 [52.0, 164.0] | 0.417 | 0.03 | |
| SBP on admission (mmHg) | 116.0 [18.0, 175.0] | 110.0 [40.0, 190.0] | 0.542 | 0.01 | |
| Respiratory rate on admission | 23.0 [12.0, 50.0] | 22.0 [10.0, 49.0] | 0.257 | 0.06 | |
| WBC on admission (×103/μL) | 12.8 [3.4, 32.5] | 11.2 [4.3, 36.9] | 0.17 | 0.07 | |
| Hb on admission (g/dL) | 11.6 [6.5, 16.2] | 11.9 [2.8, 16.0] | 0.618 | 0.06 | |
| PLT on admission (×104/μL) | 20.0 [9.4, 37.6] | 19.4 [4.6, 37.8] | 0.431 | 0.05 | |
| CPK on admission (IU/L) | 397.0 [64.0, 2835.0] | 378.0 [64.0, 1401.0] | 0.485 | 0.05 | |
| Base excess on admission | −4.6 [−17.9, 3.8] | −4.7 [−20.9, 1.7] | 0.892 | 0.04 | |
The propensity score was created from all variables in Table 4. Caliper Matching (scale = 0.003) was performed.
Prehospital fluid: whether the patients received intravenous infusion before admission or not.
Anticoagulant and/or antiplatelet: whether the patients had been receiving these drugs based on their history.
Tranexamic acid ≤3 h: whether the patients received tranexamic acid intravenously within 3 h after admission.
CPK indicates creatine phosphokinase; Hb, haemoglobin; ISS, injury severity score; PLT, platelet count; SBP, systolic blood pressure; WBC, white blood cell count.
Fig. 1.
Kaplan–Meier curves of patients transfused with an FFP/RBC ratio ≥1 within the first 6 h (red line) and patients transfused with an FFP/RBC ratio <1 within the first 6 h (black line).
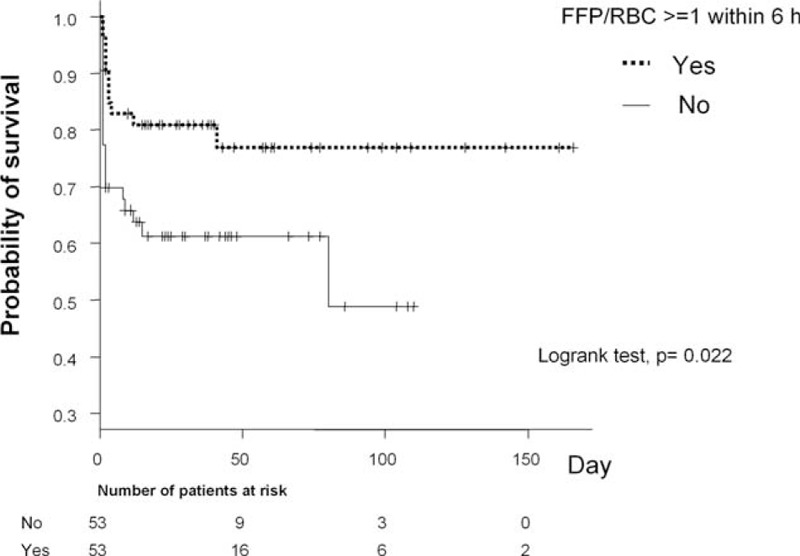
Propensity score matching was done between the two groups. The FFP/RBC ratio ≥1 group has a significantly higher survival rate at discharge (log-rank test; P = 0.022).
Comparison of outcomes between groups by hazard ratios (Cox analysis, PMS, and IPTW)
Table 4 shows the hazard ratio results. Patients with an FFP/RBC ratio ≥1 within the first 6 h had significantly better survival, with an unadjusted hazard ratio of 0.44 and an adjusted hazard ratio of 0.29 (adjusted by all variables in Table 2). However, between the groups with an FFP/RBC ratio ≥1 within 24 h and <1 within 24 h, survival rates were not significantly different (unadjusted and adjusted hazard ratios). The results with PSM when patients were divided into two groups (FFP/RBC ratio ≥1 within the first 6 h and FFP/RBC ratio <1 within the first 6 h) showed significantly better survival with an FFP/RBC ratio ≥1, with a hazard ratio of 0.38. The between-group comparison using IPTW also showed significantly better survival with an FFP/RBC ratio ≥1, with a hazard ratio of 0.41.
Table 4.
Cox proportional hazards analysis of time to death in patients with FFP/RBC use (n = 189)
| Model | Hazard ratio | P value | |
| FFP/RBC ≥1 within 6 h | Unadjusted | 0.44 (0.25–0.74) | 0.002* |
| Within 6 h | Multivariable adjusted** | 0.29 (0.14–0.62) | 0.001* |
| Within 24 h | Unadjusted | 0.62 (0.36–1.00) | 0.051 |
| Within 24 h | Multivariable adjusted** | 1.27 (0.59–2.74) | 0.540 |
| **All variables in Table 2 were selected. | |||
| Cox proportional hazards analysis of FFP/RBC ratio ≥1 within 6 h and mortality among patients matched by propensity score and among patients adjusted by inverse probability of treatment weighting with propensity scores | |||
| Model | Hazard ratio | P value | |
| FFP/RBC ratio ≥1 within 6 h (n = 106)* | Adjusted by propensity Score matching | 0.38 (0.17–0.86) | 0.020 |
| within 6 h (n = 189)† | Adjusted by IPTW | 0.41 (0.24–0.70) | 0.001 |
*106 is the number of patients matched by propensity score; the number of patients with FFP/RBC ratio ≥1 within 6 h included 53 patients, and those with an FFP/RBC ratio <1 included 53 patients.
†195 is the number of study patients without missing values.
IPTW indicates inverse probability of treatment weighting.
Histogram of transfused RBC volume
Figure 2 is a histogram of the number of units of RBCs transfused within the first 6 h. The highest proportion in both groups received between 2 and 6 units of RBCs. The difference in the RBC units between patients transfused with FFP/RBC ≥1 and FFP/RBC <1 decreased after matching.
Fig. 2.
Histograms of RBC units received within the first 6 h in patients transfused with an FFP/RBC ratio ≥1 (red) and patients transfused with an FFP/RBC ratio <1 (black).
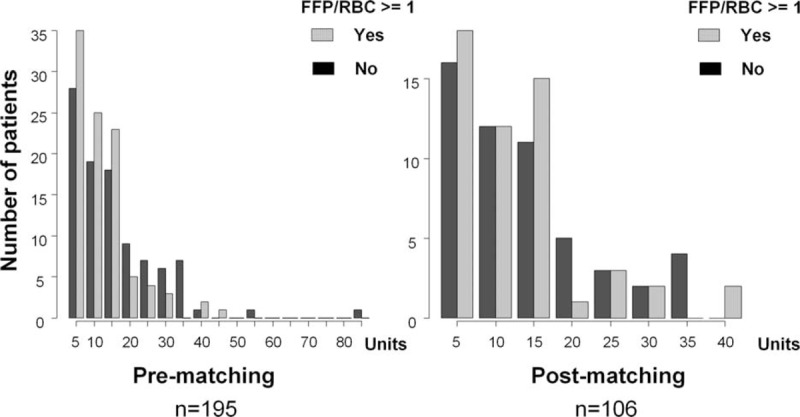
The left side of the figure shows the histogram of the prematching patients’ group, and the right side shows the histogram of the post-matching patients’ group. The highest proportion of patients in both groups received between two and six units of RBCs. However, the difference in the RBC units between patients transfused with FFP/RBC ≥1 and FFP/RBC <1 decreased after matching.
DISCUSSION
In 2005, Ho et al. (18) reported that, when hemorrhage is difficult to control because of severe clotting factor deficiency associated with major bleeding in trauma, 1 to 1.5 units of FFP must be given for every unit of RBCs to control the bleeding. They also stated that, when clotting factors decrease by about 50%, a 1:1 ratio of FFP to RBCs should be given to prevent further clotting factor deficiency. Although their study was based on a simulation, several clinical studies were later conducted to confirm these results (4, 5, 7, 19, 20).
However, none of the above studies examined the time window for achievement of a high FFP/RBC ratio transfusion. Recently, Kutcher et al. (21) and Holcomb et al. (8) used Cox regression analysis to prospectively examine the relationship between the FFP/RBC ratio and the mortality rate, considering the time factor. Kutcher et al. (21) reported that the hazard ratio was 0.58 for a high FFP /RBC ratio within 24 h in patients who received a massive transfusion (≥10 units of RBCs). Holcomb et al. (8) reported that the hazard ratio was 0.31 for a high FFP/RBC ratio within the first 6 h after admission in patients who received ≥3 units of RBCs. Thus, the mortality rate was significantly lower in the high FFP ratio group, even considering the time window for the accomplishment of this high ratio.
The present study focused on FFP and RBC volumes transfused within the first 6 h and within the first 24 h after admission to examine the FFP/RBC ratio within the first 6 h and the first 24 h. Univariate analysis and Cox analysis did not show the FFP/RBC ratio within the first 24 h to be a significant factor, but the FFP/RBC ratio within the first 6 h was a significant factor in both analyses. ROC analysis for survival at discharge was performed using the FFP/RBC ratio within the first 6 h as a significant independent variable. The FFP/RBC ratio was 1.0 for maximum sensitivity and specificity, which agrees with the results of Ho et al. (18). The present results showed a hazard ratio ranging from 0.29 to 0.44 for patients transfused with an FFP/RBC ratio ≥1 within the first 6 h based on univariate analysis, Cox analysis, PSM, and IPTW, and their survival rates were significantly higher. These hazard ratios were similar to the results of Kutcher et al. (21) and Holcomb (8), even in a study population composed of blunt trauma patients.
The blunt trauma rates have been low in studies of Western countries reporting the effectiveness of early FFP transfusion (4, 5, 7, 8, 18–22). We believed that coagulopathy in patients with blunt trauma would be more severe than that in patients with penetrating trauma, and, consequently, the volume of FFP transfusion in blunt trauma would be greater than in penetrating trauma. However, the present results showed that severe blunt trauma patients who were transfused with FFP with an FFP/RBC ratio ≥1 had a similar hazard ratio to previous studies where the study populations were predominantly penetrating trauma patients (8, 9, 21). We believe that the similarity of these hazard ratios may demonstrate clinical robustness.
Many studies have examined patients who received RBC transfusions ≥ 10 U within the first 24 h to prove the efficacy of a massive transfusion protocol (4, 5, 7, 20, 21). However, patients with severe blunt trauma may already have developed trauma-induced coagulopathy before fluid resuscitation. We recommend that early aggressive administration of FFP should be performed even for patients requiring a small number of RBC units, because it would attenuate trauma-induced coagulopathy.
Since the present study was a retrospective analysis, a survival bias may be present. Many patients with severe trauma die early after admission, and because it takes time to thaw and administer FFP, some patients die before receiving sufficient FFP. As a result, they may have received a smaller amount of FFP. Conversely, patients with relatively less severe trauma have more time to receive FFP together with other treatments, so their FFP ratios may be higher (7).
The present patients may also have included patients who received non-massive transfusions of 2 to 6 units of RBCs within the first 6 h only to raise their hemoglobin levels, or patients who died while receiving RBCs before the FFP was transfused sufficiently. Patients who died before sufficient FFP transfusion had shorter survival times, and as a result, they presumably also received lower amounts of RBC transfusions. Nevertheless, if these biases were strong, we would expect differences in the distribution in the RBC transfusion histogram between the groups who received an FFP/RBC ratio ≥1 and an FFP/RBC ratio <1. Examining the histogram of RBCs received within the first 6 h in the unmatched and matched patient groups (Fig. 2), the highest proportion of patients in both groups received 2 to 6 units of RBCs. However, the difference in the RBC units between patients transfused with FFP/RBC ≥1 and FFP/RBC <1 decreased after matching. Thus, the survival bias may have been reduced after PSM.
Study limitations
Observational studies always have some cause and effect relation biases, including a survival bias; this study undoubtedly also had such biases. For example, some patients with severe blunt trauma may have died before FFP was thawed and transfused. However, we believe that the statistical analysis using propensity score matching may minimize such bias as much as possible.
To perform early aggressive administration of FFP, preservation of thawed FFP is needed. Radwan et al. (22) reported that keeping thawed plasma in an emergency department expedites transfusion of plasma to severely injured patients. Unfortunately, the Ministry of Health, Labour and Welfare of Japan prohibits transfusion of stored thawed plasma. After FFP is thawed, it must be transfused within 3 h. However, we believe that these concerns will be resolved in the future by activity of the Japanese Association for the Surgery of Trauma.
A prospective, randomized, controlled study is needed to prove the efficacy of the transfusion of an FFP/RBC ratio ≥1 within the first 6 h.
CONCLUSION
Blunt trauma patients transfused with an FFP/RBC ratio ≥1 within the first 6 h after admission had a hazard ratio of about 0.4. In other words, their risk of death was reduced by about 60%. Transfusion of an FFP/RBC ratio ≥1 within the first 6 h was associated with the outcome of severe blunt trauma patients with ISS ≥16 and needed a transfusion within 24 h. The present results suggest that early aggressive administration of FFP may be crucial for resuscitation in patients with severe blunt trauma requiring blood transfusion.
Supplementary Material
Footnotes
AH designed the study and collected and analyzed the data, and AH, SK, DS, and MH wrote the manuscript. SK, HK, JS, HO, TM, TU, NM, HI, MH, and MT collected the data. DS and AS presented the statistical methods. YO, HY, TS, and HT supported this study as directors of the Japanese Association for the Surgery of Trauma. All authors approved the final version of the manuscript.
A publication fee was paid by the general insurance association of Japan.
The authors report no conflicts of interest.
REFERENCES
- 1.Holcomb JB, Jenkins D, Rhee P, Johannigman J, Mahoney P, Mehta S, Cox ED, Gehrke MJ, Beilman GJ, Schreiber M, et al. Damage control resuscitation: directly addressing the early coagulopathy of trauma. J Trauma 2007; 62:307–310. [DOI] [PubMed] [Google Scholar]
- 2.Ball CG. Damage control resuscitation: history, theory and technique. Can J Surg 2014; 57:55–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hess JR, Holcomb JB, Hoyt DB. Damage control resuscitation: the need for specific blood products to treat the coagulopathy of trauma. Transfusion 2006; 46:685–686. [DOI] [PubMed] [Google Scholar]
- 4.Borgman MA, Spinella PC, Perkins JG, Grathwohl KW, Repine T, Beekley AC, Sebesta J, Jenkins D, Wade CE, Holcomb JB. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma 2007; 63:805–813. [DOI] [PubMed] [Google Scholar]
- 5.Holcomb JB, Wade CE, Michalek JE, Chisholm GB, Zarzabal LA, Schreiber MA, Gonzalez EA, Pomper GJ, Perkins JG, Spinella PC, et al. Increased plasma and platelet to red blood cell ratios improves outcome in 466 massively transfused civilian trauma patients. Ann Surg 2008; 248:447–458. [DOI] [PubMed] [Google Scholar]
- 6.Schuster KM, Davis KA, Lui FY, Maerz LL, Kaplan LJ. The status of massive transfusion protocols in United States trauma centers: massive transfusion or massive confusion? Transfusion 2010; 50:1545–1551. [DOI] [PubMed] [Google Scholar]
- 7.Snyder CW, Weinberg JA, McGwin G, Jr, Melton SM, George RL, Reiff DA, Cross JM, Hubbard-Brown J, Rue LW, 3rd, Kerby JD. The relationship of blood product ratio to mortality: survival benefit or survival bias? J Trauma 2009; 66:358–362.discussion 362–354. [DOI] [PubMed] [Google Scholar]
- 8.Holcomb JB, del Junco DJ, Fox EE, Wade CE, Cohen MJ, Schreiber MA, Alarcon LH, Bai Y, Brasel KJ, Bulger EM, et al. The prospective, observational, multicenter, major trauma transfusion (PROMMTT) study: comparative effectiveness of a time-varying treatment with competing risks. JAMA Surg 2013; 148:127–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holcomb JB, Tilley BC, Baraniuk S, Fox EE, Wade CE, Podbielski JM, del Junco DJ, Brasel KJ, Bulger EM, Callcut RA, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA 2015; 313:471–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trauma Register DGU. Available at: http://www.dgu-online.de/fileadmin/published_content/5.Qualitaet_und_Sicherheit/PDF/2013_TR_DGU_annual_report.pdf Accessed date December 7, 2015. [Google Scholar]
- 11.Japan Trauma Data Bank Report 2013 (2008–2012). Available at: http://www.jtcr-jatec.org/traumabank/dataroom/data/JTDB2013.pdf Accessed date December 7, 2015. [Google Scholar]
- 12.Maegele M, Spinella PC, Schochl H. The acute coagulopathy of trauma: mechanisms and tools for risk stratification. Shock 2012; 38:450–458. [DOI] [PubMed] [Google Scholar]
- 13.Dobson GP, Letson HL, Sharma R, Sheppard FR, Cap AP. Mechanisms of early trauma-induced coagulopathy: the clot thickens or not? J Trauma Acute Care Surg 2015; 79:301–309. [DOI] [PubMed] [Google Scholar]
- 14.Baker SP, O’Neill B, Haddon W, Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 1974; 14:187–196. [PubMed] [Google Scholar]
- 15.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- 16.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 2011; 46:399–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kanda Y. Investigation of the freely available easy-to-use software ’EZR’ for medical statistics. Bone Marrow Transplant 2013; 48:452–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ho AM, Dion PW, Cheng CA, Karmakar MK, Cheng G, Peng Z, Ng YW. A mathematical model for fresh frozen plasma transfusion strategies during major trauma resuscitation with ongoing hemorrhage. Can J Surg 2005; 48:470–478. [PMC free article] [PubMed] [Google Scholar]
- 19.Duchesne JC, Hunt JP, Wahl G, Marr AB, Wang YZ, Weintraub SE, Wright MJ, McSwain NE., Jr Review of current blood transfusions strategies in a mature level I trauma center: were we wrong for the last 60 years? J Trauma 2008; 65:272–276.discussion 276–278. [DOI] [PubMed] [Google Scholar]
- 20.Sperry JL, Ochoa JB, Gunn SR, Alarcon LH, Minei JP, Cuschieri J, Rosengart MR, Maier RV, Billiar TR, Peitzman AB, et al. An FFP: PRBC transfusion ratio >/=1:1.5 is associated with a lower risk of mortality after massive transfusion. J Trauma 2008; 65:986–993. [DOI] [PubMed] [Google Scholar]
- 21.Kutcher ME, Kornblith LZ, Narayan R, Curd V, Daley AT, Redick BJ, Nelson MF, Fiebig EW, Cohen MJ. A paradigm shift in trauma resuscitation: evaluation of evolving massive transfusion practices. JAMA Surg 2013; 148:834–840. [DOI] [PubMed] [Google Scholar]
- 22.Radwan ZA, Bai Y, Matijevic N, del Junco DJ, McCarthy JJ, Wade CE, Holcomb JB, Cotton BA. An emergency department thawed plasma protocol for severely injured patients. JAMA Surg 2013; 148:170–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


