Abstract
Background: Previous guidelines for the management of thyroid nodules and cancers were geared toward adults. Compared with thyroid neoplasms in adults, however, those in the pediatric population exhibit differences in pathophysiology, clinical presentation, and long-term outcomes. Furthermore, therapy that may be recommended for an adult may not be appropriate for a child who is at low risk for death but at higher risk for long-term harm from overly aggressive treatment. For these reasons, unique guidelines for children and adolescents with thyroid tumors are needed.
Methods: A task force commissioned by the American Thyroid Association (ATA) developed a series of clinically relevant questions pertaining to the management of children with thyroid nodules and differentiated thyroid cancer (DTC). Using an extensive literature search, primarily focused on studies that included subjects ≤18 years of age, the task force identified and reviewed relevant articles through April 2014. Recommendations were made based upon scientific evidence and expert opinion and were graded using a modified schema from the United States Preventive Services Task Force.
Results: These inaugural guidelines provide recommendations for the evaluation and management of thyroid nodules in children and adolescents, including the role and interpretation of ultrasound, fine-needle aspiration cytology, and the management of benign nodules. Recommendations for the evaluation, treatment, and follow-up of children and adolescents with DTC are outlined and include preoperative staging, surgical management, postoperative staging, the role of radioactive iodine therapy, and goals for thyrotropin suppression. Management algorithms are proposed and separate recommendations for papillary and follicular thyroid cancers are provided.
Conclusions: In response to our charge as an independent task force appointed by the ATA, we developed recommendations based on scientific evidence and expert opinion for the management of thyroid nodules and DTC in children and adolescents. In our opinion, these represent the current optimal care for children and adolescents with these conditions.
Introduction
In order to promote best practice standards for the diagnosis and management of thyroid cancers, The American Thyroid Association (ATA) (1), the American Association of Clinical Endocrinologists (2), the National Comprehensive Cancer Network (NCCN) (3), and the British Thyroid Association/Royal College of Physicians (4), previously published guidelines specifically addressing the evaluation, treatment and follow-up of thyroid nodules and differentiated thyroid cancer (DTC) in adults. In most cases, the evaluation, treatment and follow-up of children with thyroid neoplasia have followed adult guidelines. Heretofore, this approach resulted in a high proportion of cure, but required all children to undergo therapy that included total thyroidectomy followed by radioactive iodine (RAI) ablation with iodine-131 (131I). The goal was to eliminate any evidence of disease, documented by a negative whole-body RAI scan and, most recently, by an undetectable serum thyroglobulin (Tg) level. Unfortunately, recent studies with follow-up spanning several decades reveal an increase in all-cause mortality for survivors of childhood DTC, predominately due to second malignancies in children treated with radiation (5–7). These observations, coupled with a better understanding of the excellent prognosis associated with pediatric DTC (5,8–15), have now prompted the ATA to specifically address treatment of children with benign and malignant thyroid tumors.
This inaugural pediatric task force acknowledges that no randomized double-blind controlled clinical trial exists for the treatment of children with DTC. Published data are from retrospective cohorts and are potentially subject to investigator bias or nonrandom assignment to various treatment groups. Further limiting the development of treatment guidelines is the fact that previous series of DTC in children averaged only 10 years of follow-up. This constraint has made it difficult to determine if any treatment results in decreased risk of recurrence, mortality, or complications of therapy for children. Nevertheless, retrospective analysis of therapeutic options has led to a reconsideration of the former concept that all children with DTC should be similarly treated and has provided the opportunity for this task force to broaden the scope of acceptable therapy in an attempt to provide aggressive therapy when warranted and to limit overtreatment of those children who are unlikely to benefit.
Background
According to the Surveillance, Epidemiology and End Results (SEER) program, new cases of thyroid cancer in people age <20 represent 1.8% of all thyroid malignancies diagnosed in the United States (16). Unfortunately, the incidence appears to be increasing (17). Among 15- to 19-year-old adolescents, thyroid cancer is the eighth most frequently diagnosed cancer and the second most common cancer among girls (8,18). Adolescents have a 10-fold greater incidence than younger children, and there is a female to male preponderance (5:1) during adolescence that is not seen in young children (8,18–21). The most common presentation for DTC in children is that of a thyroid nodule. However, papillary thyroid cancer (PTC) also frequently presents as cervical adenopathy with or without a palpable thyroid lesion, or as an incidental finding after imaging or surgery for an unrelated condition (11). Occasionally, the diagnosis is made only after the discovery of distant metastases (22–24).
The pathological classification of DTCs in children is based on standard definitions set by the World Health Organization (WHO), with histological criteria the same for children and adults (25). PTC accounts for 90% or more of all childhood cases (10,12,20,26–28). Follicular thyroid cancer (FTC) is uncommon, while medullary thyroid cancer (MTC), poorly differentiated tumors, and frankly undifferentiated (anaplastic) thyroid carcinomas are rare in young patients. Pediatric PTC may present with a variety of histological variants all having a distinctive but shared set of nuclear characteristics.
Subtypes of PTC in pediatrics include the following histologic variants: classic, solid, follicular, and diffuse sclerosing (25,29). Children, especially those <10 years of age, may not have the classic papillary morphology seen in adults, and such tumors can be un-encapsulated and widely invasive throughout the gland and have a follicular and solid architecture with unique nuclear features and abundant psammoma bodies (30,31). The major risk factor for developing PTC is radiation exposure to the thyroid (32–34). Children, especially those <5 years of age, are the most sensitive (33,35,36). Radiation-induced PTC does not appear to differ in clinical behavior compared with sporadic PTC (37). Activation of the RAS-RAF-MEK-ERK (mitogen-activated protein kinase) pathway is critical for thyroid malignancies (38–40). An estimated 5% of patients with nonmedullary thyroid cancer (NMTC) have a family history of nonsyndromic NMTC (35,41) with conflicting evidence in regard to whether it behaves more aggressively (42).
PTC and FTC exhibit major clinical differences. PTC is frequently multifocal and bilateral and metastasizes to regional neck lymph nodes in the vast majority of children (10,12,13,15,23,24,31,43–47). Hematogenous metastases to the lungs occur in up to 25% of cases (9,11,14,24,31,43,48–52) and generally occur only with significant regional lymph node metastases (10,53). FTC is typically a unifocal tumor and more prone to initial hematogenous metastases to lungs and bones. Metastases to regional lymph nodes are uncommon in FTC. Histologic variants of FTC include: Hürthle cell (oncocytic), clear cell, and insular (poorly differentiated) carcinoma (25).
Based on the rarity of FTC in children and the major clinical and biological differences between PTC and FTC in children, the current guidelines have been developed specifically for PTC in children, and we have chosen to include a separate section dedicated to the treatment of FTC.
Methodology
The ATA selected a task force using a strategy similar to that of previous ATA Guidelines task forces. Members were approved by the ATA and represent an international community of experts from a variety of disciplines including endocrinology, molecular biology, nuclear medicine, radiology, and surgery. None of the scientific or medical content of the manuscript was dictated by the ATA. The task force met by conference calls and in person and developed a series of clinically relevant questions pertaining to the management of children with thyroid nodules and DTC. Task force members were assigned to subcommittees structured along the lines of these clinical questions and attempted to answer them using an extensive literature search, primarily focused on studies that included subjects ≤18 years of age, in addition to expert opinion. Similar to other ATA guidelines, the strength of the recommendations was categorized using a modified schema proposed by the U.S. Preventive Services Task Force (54) (see Table 1). With contributions from all authors, the document was primarily written by the chair and cochairs (GLF, AJB, and SGW). The Pediatric Endocrine Society (PES) codeveloped and endorsed the guidelines. The final document was approved by the ATA (Board of Directors and membership) and the PES (Drug and Therapeutics Committee and Board of Directors).
Table 1.
Strength of Panelists' Recommendations Based on Available Evidence
| Rating | Definition |
|---|---|
| A: Strongly recommends | The recommendation is based on good evidence that the service or intervention can improve important health outcomes. Evidence includes consistent results from well-designed, well-conducted studies in representative populations that directly assess effects on health outcomes. |
| B: Recommends | The recommendation is based on fair evidence that the service or intervention can improve important health outcomes. The evidence is sufficient to determine effects on health outcomes, but the strength of the evidence is limited by the number, quality, or consistency of the individual studies; generalizability to routine practice; or indirect nature of the evidence on health outcomes. |
| C: Recommends | The recommendation is based on expert opinion. |
| D: Recommends against | The recommendation is based on expert opinion. |
| E: Recommends against | The recommendation is based on fair evidence that the service or intervention does not improve important health outcomes or that harms outweigh benefits. |
| F: Strongly recommends against | The recommendation is based on good evidence that the service or intervention does not improve important health outcomes or that harms outweigh benefits. |
| I: Recommends neither for nor against | The panel concludes that the evidence is insufficient to recommend for or against providing the service or intervention because evidence is lacking that the service or intervention improves important health outcomes, the evidence is of poor quality, or the evidence is conflicting. As a result, the balance of benefits and harms cannot be determined. |
Table 2 presents the organization of the task force's results and recommendations. Readers of the print version are referred to the page number for information about specific topics and recommendations. The location key can be used if viewing the guidelines in a file or web page. Each location key is unique and can be copied into the Find or Search functions to rapidly navigate to the section of interest. Specific recommendations are presented as bulleted points in the main body. Table 3 includes definitions to the abbreviations used in the guidelines.
Table 2.
Organization of the Pediatric Thyroid Nodule and Differentiated Thyroid Cancer Guidelines and Recommendations
| Location keya | Page | Section | Recommendation no. | Rating |
|---|---|---|---|---|
| [A1] | 720 | Why do we need specific guidelines for children with thyroid nodules and thyroid cancer? | ||
| [A2] | 720 | To what age group should these guidelines apply? | 1 | C |
| [A3] | 720–721 | Should treatment of children with DTC be stratified into more than one age group? | 2 | B |
| [A4] | 721–722 | What are the goals of therapy for DTC in children? | 3 | C |
| [B1] | 722 | Thyroid nodule guidelines | ||
| [B2] | 722 | How common are thyroid nodules in children and what is the risk for malignancy? | ||
| [B3] | 722–723 | Are there high-risk groups who might benefit from prospective screening for thyroid nodules and thyroid cancer? | 4(A) | B |
| 4(B) | I | |||
| 4(C) | C | |||
| 4(D) | B | |||
| [B4] | 723–725 | What is the optimal evaluation of children with thyroid nodules? | 5 | B |
| [B5] | 725 | Are there molecular signatures that complement FNA and improve the diagnostic tility of FNA in children? | 6 | E |
| [B6] | 725 | How should thyroid nodules be treated in children? | ||
| [B7] | 725 | What is the recommended approach for children with benign thyroid cytopathology? | ||
| [B8] | 725–726 | Is there a role for levothyroxine suppression therapy? | 7 | I |
| [B9] | 726 | Is there a role for surgery in children with benign nodules? | 8 | B |
| [B10] | 726 | What is the optimal management of the child with an autonomous thyroid nodule? | 9 | A |
| [C1] | 726 | Papillary thyroid cancer—initial management guidelines | ||
| [C2] | 726–727 | What is the optimal preoperative evaluation for the child with newly diagnosed PTC? | 10 | A |
| [C3] | 727 | What is the recommended surgical approach for the patient with a diagnosis of PTC? | 11 | A |
| [C4] | 727–728 | Should central neck dissection be performed? | 12(A) | B |
| 12(B) | C | |||
| 12(C) | A | |||
| 12(D) | C | |||
| [C5] | 728 | What are the indications for lateral neck dissection? | 13 | B |
| [C6] | 728–729 | What are the possible complications of surgery and what should be done to minimize the risks of surgery? | 14(A) | B |
| 14(B) | B | |||
| [C7] | 729–730 | What tumor classification systems can be used for pediatric PTC? | 15(A) | B |
| 15(B) | B | |||
| [C8] | 730–732 | What postoperative staging is recommended? | 16 | B |
| [C9] | 733 | What are the goals of 131I treatment? | ||
| [C10] | 733 | What is the impact of 131I therapy on recurrence and survival for children with PTC? | ||
| [C11] | 733 | Which children might benefit from therapeutic 131I? | 17 | B |
| [C12] | 733–734 | How should a child be prepared for 131I? | 18 | A |
| [C13] | 734–736 | What should be considered for administration of 131I? | 19(A) | C |
| 19(B) | F | |||
| [C14] | 736 | How is the activity of therapeutic 131I determined? | 20 | I |
| [C15] | 736 | Should a posttreatment whole-body scan be obtained? | 21 | B |
| [C16] | 736–737 | What are the acute and long-term risks of 131I therapy in children? | 22 | C |
| [D1] | 737 | Surveillance and follow-up of PTC In children | ||
| [D2] | 737–739 | What is the role of Tg testing in the follow-up of PTC in children? | 23(A) | A |
| 23(B) | A | |||
| 23(C) | B | |||
| 23(D) | A | |||
| 23(E) | A | |||
| [D3] | 739 | What is the role of ultrasound in the follow-up of PTC in children? | 24 | A |
| [D4] | 739–740 | How are diagnostic RAI scans best used in the follow-up of PTC in children? | 25(A) | C |
| 25(B) | B | |||
| 25(C) | B | |||
| [D5] | 740 | What imaging studies should be considered in the pediatric PTC patient who is Tg positive but who has no evidence of disease on cervical ultrasound or DxWBS? | 26(A) | B |
| 26(B) | D | |||
| 26(C) | D | |||
| [D6] | 740–741 | What are the goals and potential risks of TSH suppression therapy? | 27 | B |
| [D7] | 741 | What is the optimal approach to the patient with persistent / recurrent cervical disease? | 28(A) | C |
| 28(B) | B | |||
| 28(C) | B | |||
| 28(D) | C | |||
| [D8] | 741–742 | How should children with pulmonary metastases be managed? | 29(A) | A |
| 29(B) | B | |||
| 29(C) | B | |||
| 29(D) | B | |||
| 29(E) | E | |||
| 29(F) | C | |||
| [D9] | 742 | How does one approach the child with an incidental PTC identified after surgery for another thyroid condition? | 30 | B |
| [D10] | 742–743 | What are the optimal approaches to the pediatric patient who develops progressive thyroid cancer that no longer concentrates or responds to 131I? | 31 | C |
| [E1] | 743–744 | Follicular thyroid cancer | 32(A) | C |
| 32(B) | C | |||
| 32(C) | C | |||
| [F1] | 744 | What are the unique issues that may affect children diagnosed with DTC? | 33 | C |
| [G1] | 744–745 | How long should a child with PTC be monitored? | 34 | B |
| [G2] | 745 | What are the areas for future research? |
If viewing these guidelines on the Web, or in a File, copy the Location Key to the Find or Search Function to navigate rapidly to the desired section.
DTC, differentiated thyroid cancer; DxWBS, diagnostic whole-body scan; FNA, fine-needle aspiration; PTC, papillary thyroid cancer; Tg, thyroglobulin; TSH, thyrotropin.
Table 3.
Definitions of Abbreviations Used in the Pediatric Thyroid Nodule and Differentiated Thyroid Cancer Guidelines
| AJCC | American Joint Committee on Cancer |
| AMES | Age-metastasis-extent of disease-size of tumor |
| ATA | American Thyroid Association |
| AUS/FLUS | Atypia or follicular lesion of undetermined significance |
| CND | Central neck dissection |
| CT | Computed tomography |
| DFS | Disease-free survival |
| DTC | Differentiated thyroid cancer |
| DxWBS | Diagnostic whole-body scan |
| ETE | Extrathyroidal extension |
| FDA | Food and Drug Administration |
| 18FDG-PET/CT | [18F]-fluoro-deoxyglucose positron emission tomography/computed tomography |
| FNA | Fine-needle aspiration |
| FNMTC | Familial nonmedullary thyroid cancer |
| FTC | Follicular thyroid cancer |
| Gy | Gray unit of measurement: absorbed dose (of ionizing radiation) |
| iPTH | Intact parathyroid hormone |
| LT4 | Levothyroxine |
| MACIS | Metastasis-age-completeness of resection-invasion-size |
| MRI | Magnetic resonance imaging |
| MTC | Medullary thyroid cancer |
| NCCN | National Comprehensive Cancer Network |
| NIS | Sodium-iodide symporter |
| NMTC | Nonmedullary thyroid cancer |
| PTC | Papillary thyroid cancer |
| PTEN | Gene: phosphatase and tensin homolog |
| PTMC | Papillary thyroid microcarcinoma |
| RAI | Radioactive iodine |
| rhTSH | Recombinant human TSH |
| RLN | Recurrent laryngeal nerve |
| RxWBS | Post-treatment whole-body scan |
| SPECT/CT | Single photon emission computed tomography with integrated conventional CT |
| Tg | Thyroglobulin |
| TgAb | Thyroglobulin antibody |
| TNM | Tumor-Node-Metastasis |
| TSH | Thyrotropin |
| TT | Total or near-total thyroidectomy |
| US | Ultrasound |
| WBS | Whole-body scan |
| WHO | World Health Organization |
[A1] Why do we need Specific Guidelines for Children with Thyroid Nodules and Thyroid Cancer?
There are important clinical, molecular, and pathological differences in DTC among children compared to adults that prompt the development of unique pediatric guidelines. From a clinical perspective, thyroid nodules are uncommon in children. However, nodules diagnosed in children carry a greater risk of malignancy compared to those in adults (22%–26% versus 5%–10% in most series) (27,55,56). Second, when histology and tumor size are controlled for, children with PTC are more likely to have regional lymph node involvement, extrathyroidal extension, and pulmonary metastasis (9–15,23,24,31,43–53). Third, despite extensive disease at clinical presentation, children are much less likely to die from disease (2% or less long-term cause-specific mortality) than are adults (5,8–15), and many children with pulmonary metastases (30%–45%) develop persistent albeit stable disease following 131I therapy (24,57). This is associated with a more favorable progression-free survival in children compared to adults with persistent DTC (9,10,13,14,47,48,51,52). Finally, there may be a continued clinical response demonstrated by a decline in Tg levels after cessation of RAI therapy in children with pulmonary metastases (58).
Compared with adult PTC, childhood PTC is characterized by a higher prevalence of gene rearrangements and a lower frequency of point mutations in the proto-oncogenes implicated in PTC. Recent molecular studies have shown that BRAF mutations are the most common abnormality in adult PTC (36%–83% of cases) (38), but they are rare in children with PTC (59) and virtually absent from the youngest patients. This may be important because point mutations of RAS and BRAF lead to genomic instability and dedifferentiation manifested by decreased expression of the sodium-iodide symporter (NIS) (60,61). In contrast, RET/PTC rearrangements are more common in PTC from children (20,26,40,62) and do not lead to genomic instability. These molecular differences might be one of the reasons for better response to RAI therapy in children with PTC and could partially explain their low mortality and rare progression to less-differentiated tumors. Consistent with this hypothesis, a small study of PTC from children and adolescents found distant metastases and recurrence only in tumors with undetectable NIS, and the activity of 131I required to achieve remission was greater in those cancers with undetectable NIS (63). Finally, these molecular differences may have an impact on the utility of molecular testing for diagnosis of thyroid malignancies in children with thyroid nodules (see Section B5).
[A2] To what age group should these Guidelines apply?
Studies of pediatric DTC have variously included individuals extending up to 21 years of age (5,8–10,13,14,47,48,51,52). With uncommon exception, the majority of pediatric patients have completed growth and development by ≤18 years of age. To more accurately define the impact of the physiologic changes of growth and development on tumor behavior, the upper limit for pediatrics should be defined as patients ≤18 years of age.
■ RECOMMENDATION 1
The pediatric age should be limited to a patient ≤18 years of age. Establishing a uniform upper limit of age will afford an opportunity to better define the potential impact of growth on tumor behavior. From a pragmatic point of view, individual centers may transition pediatric patients to adult care anywhere between 18 and 21 years of age. Clinicians may manage the “child” under these guidelines until transition has been completed.
Recommendation rating: C
[A3] Should treatment of Children with DTC be stratified into more than one Age Group?
Several studies have compared the clinical presentation and outcomes for children diagnosed with DTC <10–15 years of age with that of patients 10–18 years of age. The data are unclear as to whether younger age portends greater risk for extensive disease or recurrence. All studies are retrospective and most include only small numbers of children <10–15 years of age. In general, studies in which 25%–30% of the cohort are of younger age have shown that young age is associated with persistent disease or recurrence, whereas studies with fewer young children have not confirmed this (10,14,50,53,64–66). In addition, treatment regimens varied, which may impact outcomes. For example, surgeons may be less aggressive in lymph node dissection in younger children, and this factor, rather than age, may impact recurrence rates.
In some series, extrathyroidal extension (ETE) (50,66), regional node involvement (50,67), distant metastases (64,67), and lymph node recurrence (10,65,66) have an increased prevalence in younger children, but this is not seen in all series (14,44,50,53). The largest study included 740 children from Belarus (10), 92% of whom had exposure to radionuclides at the time of the Chernobyl disaster. By multivariate regression analysis, younger age was associated with an increased risk of recurrent nodal disease and lung metastases after adjustment for other risk factors. Unfortunately, several features of that study preclude generalization of the data. The Belarus cohort was exposed to radiation, and the relationship between age and outcome might be explained by the heightened sensitivity to radiation in younger children rather than age per se (68).
■ RECOMMENDATION 2
It remains unclear if younger children (<10–15 years of age) are at greater risk for more extensive disease or higher rates of recurrence. Other factors aside from age (treatment approaches, genetic susceptibility, and/or radiation exposure) may interact to modify this risk. However, those studies with a larger proportion of young children show an increased risk of persistent disease/recurrence. In an effort to increase the descriptive nature of these discussions, the committee recommends that “prepubertal” and “pubertal/postpubertal” should be incorporated into future studies to increase uniformity and more accurately represent the potential influence of pubertal development on the incidence and behavior of DTC within the pediatric population.
Recommendation rating: B
[A4] What are the Goals of Therapy for DTC in Children?
Given the fact that disease-specific mortality for children with DTC is very low, it is unlikely that modification of current treatment protocols will further reduce the disease-specific mortality. However, the apparent increased risk of second malignancies and overall mortality among childhood DTC survivors who were treated with radiation (see Section C16) underscores the need to better risk-stratify children with DTC so that more aggressive therapy is reserved for those at highest risk for morbidity and mortality and avoided in those children who are unlikely to derive long-term benefit. The goals for improved treatment are to
1. Maintain the low disease-specific mortality currently experienced by children with DTC.
2. Reduce potential complications from therapy.
A major task in this process is to prospectively identify the minority of children who will benefit from aggressive therapy and to better understand the clinical characteristics that predict a response to such therapies. It is possible that in this search to develop “lower-intensity” therapy, we might increase the risk for residual/recurrent disease and the numbers of patients surviving with low-volume, persistent but progression-free disease. Two major differences in these guidelines compared with previous treatment guidelines are recommendations directed toward:
1. Pre- and postoperative staging
2. Selective use of 131I in children with DTC
The 2009 ATA thyroid cancer guidelines for adult patients recommend that staging should be performed for all patients with DTC using the Tumor-Node-Metastasis (TNM) classification of the American Joint Committee on Cancer (AJCC) (69). In this system, children are classified as either stage I (no distant metastases) or stage II disease (with distant metastases). However, stage I includes a widely diverse group of children: those with a solitary lesion confined to the thyroid, those with extensive locoregional disease and neck nodal metastases, and those with microscopic PTC. Treatment and prognosis for these varied lesions should ideally be stratified to represent the risks of persistent/recurrent disease, and that will require an additional risk-stratification scheme beyond TNM classification.
Studies have confirmed the notion that children with DTC have lower rates of complications when surgery is performed by experienced thyroid surgeons (70–72). For this reason, the current task force recommends that children with DTC should be operated upon by experienced thyroid surgeons. Furthermore, it is our opinion that children with DTC should be cared for by teams of physicians experienced in the management of DTC in children to include, not only high-volume thyroid surgeons, but also experts in nuclear medicine and endocrinology who have experience in managing children with DTC. Evaluation and care should be provided in centers with a full range of pediatric and oncologic resources, which should be organized into a multidisciplinary team that regularly conducts patient review and/or tumor board conferences. This will facilitate interdisciplinary decisions regarding optimal therapy and will help to reduce the possibility that treatment and long-term follow-up will be either overly aggressive or inadequate.
■ RECOMMENDATION 3
Children with DTC should be cared for by teams of physicians experienced in the management of DTC in children. This will facilitate interdisciplinary decisions regarding optimal therapy and will help to reduce the possibility that treatment and long-term follow-up will be either overly aggressive or inadequate.
Recommendation rating: C
[B1] Thyroid Nodule Guidelines
[B2] How Common are Thyroid Nodules in Children and What is the Risk for Malignancy?
Thyroid nodules are less common among children than adults but are more likely to be malignant in children referred for evaluation of nodular thyroid disease (22%–26% versus approximately 5%) (27,55,56). Estimates from ultrasound (US) and postmortem examination suggest that 1%–1.5% of children and up to 13% of older adolescents or young adults have thyroid nodules (73,74), although it is unclear how many of these would have become clinically apparent. Recent data from a large Japanese series using high-resolution US confirm the incidence of solid nodules at 1.65% but also identified cystic lesions in 57% of children and adolescents (75). Such high-resolution US data have not yet been replicated in other pediatric populations, and it remains unclear if thyroid nodules are this prevalent in other regions. Nevertheless, it appears from multiple studies that the prevalence of thyroid nodules is much greater in children than is generally appreciated. It also remains unclear how many of these nodules would reach a clinical threshold during childhood.
[B3] Are there High-Risk Groups Who Might Benefit from Prospective Screening for Thyroid Nodules and Thyroid Cancer?
Several risk factors are associated with the development of thyroid nodules in children, including iodine deficiency, prior radiation exposure, a history of antecedent thyroid disease, and several genetic syndromes (Table 4). One high-risk population is that of childhood cancer survivors who were treated for their primary malignancy with radiation therapy, especially survivors of Hodgkin lymphoma, leukemia, and central nervous system tumors (76,77). Thyroid nodules, many of which can only be detected by US, develop in cancer survivors at a rate of about 2% annually and reach a peak incidence 15–25 years after exposure (78–80). In general the risk is greatest among those who received radiation therapy at a younger age and with doses up to 20–29 Gy (77,81,82). High resolution US may identify small subclinical thyroid tumors (83,84). However, insufficient data exist to determine if early detection of nonpalpable tumors will significantly improve the quality and or longevity of life in patients screened by a standardized protocol using US and fine-needle aspiration (FNA). Furthermore, routine US screening may also identify incidental findings, such as ectopic thymus, that may confuse the clinical picture and potentially lead to unnecessary testing (75).
Table 4.
Hereditary Tumor Syndromes Associated with Thyroid Nodules/Differentiated Thyroid Cancer
| Hereditary syndromea | Gene (chromosomal location) | Type of thyroid neoplasia |
|---|---|---|
| APC-associated polyposis (familial adenomatous polyposis [FAP], attenuated FAP, Gardner syndrome, and Turcot syndrome) | • APC (5q21-q22) | • PTC (cribriform-morular variant) |
| Carney complex | • PRKAR1A (17q24.2) • “CNC2” (2p16) |
• Multinodular goiter • Follicular adenomas • DTC (PTC and FTC) |
| DICER1 Syndrome | • DICER1 (14q32.13) | • Multinodular goiter • DTC (due to second somatic mutation in DICER1, possibly related to treatment of pleuropulmonary blastoma) |
| PTEN hamartoma tumor syndrome (Cowden syndrome, Bannayan-Riley-Ruvalcaba syndrome, PTEN-related Proteus syndrome, and Proteus-like syndrome) | • PTEN (10q23) | • Multinodular goiter • Follicular adenomas • DTC (FTC overrepresented) |
| Werner syndrome | • WRN (8p12) | • DTC (PTC and FTC) |
Although DTC has also been reported to occur in patients with Beckwith–Wiedemann syndrome, the familial paraganglioma syndromes, Li–Fraumeni Syndrome, McCune–Albright syndrome, and Peutz–Jeghers syndrome, it remains unclear if these tumors are a direct result of the underlying genetic defect.
A variety of genetic disorders predispose to thyroid neoplasia (85,86) (Table 4). Benign and malignant thyroid tumors can occur in patients with APC-associated polyposis (87), the Carney complex (88), the DICER1 syndrome (89,90), the PTEN hamartoma tumor syndrome (91–93), and Werner syndrome (94). Cases of DTC have also been reported in Beckwith–Wiedemann syndrome (95), the familial paraganglioma syndromes (96), Li–Fraumeni Syndrome (97), McCune–Albright syndrome (98), and Peutz–Jeghers syndrome (99).
Furthermore, children from kindreds with familial nonmedullary thyroid cancer (FNMTC) may have a predisposition to tumor development (100–105). No clear recommendations exist for prospective screening (outside of routine physical examination) in most cases. However, updated recommendations for US screening have been put forth for both the PTEN hamartoma tumor syndrome and APC-associated polyposis (91,92,106). In addition, in nonsyndromic FNMTC, US surveillance of family members has been shown to detect earlier stages of disease as reflected by smaller tumor size (0.8 vs. 2.85 cm; p<0.001), a lower incidence of lymph node metastasis (23.2% vs. 65.6%; p<0.001) as well as a lower incidence of ETE (20.9% vs. 56.2%; p=0.002) compared to the proband (107).
Limited data exist on children with autoimmune thyroiditis. However, one report shows an increased prevalence of thyroid nodules perhaps as high as 30% with 7 of 11 PTC only detected by US examination (108). It is unclear how many of these would have achieved clinical importance, however. The presence of a palpable thyroid nodule or asymmetry with or without palpable cervical lymphadenopathy warrants referral to an experienced thyroid ultrasonographer and consideration of FNA as indicated based on suspicious sonographic features (see Section B4) or growth over time. There are increasing data to suggest that patients with a nodule and thyrotropin (TSH) levels in the upper tertiles of the reference range may be at increased risk for malignancy (109).
From these data we conclude that thyroid nodules are common in childhood cancer survivors who received radiation therapy, and they are associated with a modest risk of malignancy. Other groups of children with tumor syndromes, as well as those born into a kindred with FNMTC, have an increased risk for thyroid nodules and/or cancers. Some of these cancers are small and not likely to be detected without US. Although this task force could not recommend thyroid US as a routine screening tool in all of these patients, we do encounter children who have incidental nodules identified via screening thyroid US. Similar to palpable nodules, nodules detected in this setting should be interrogated by US performed by an experienced ultrasonographer, and FNA should be performed if the nodule has concerning sonographic features or growth over time.
■ RECOMMENDATION 4(A)
An annual physical examination is recommended in children at high risk for thyroid neoplasia. Additional imaging should be pursued if palpable nodules, thyroid asymmetry, and/or abnormal cervical lymphadenopathy are found on examination.
Recommendation rating: B
■ RECOMMENDATION 4(B)
In children with a history of radiation exposure to the thyroid, the data show that US can detect small thyroid nodules, but the panel is not yet convinced that detection of subclinical disease by US prior to a palpable abnormality on physical examination impacts long-term outcomes. Therefore, routine screening US in high-risk children can neither be recommended for nor against until more data become available.
Recommendation rating: I
■ RECOMMENDATION 4(C)
Patients at increased risk of developing familial DTC should be referred to centers of excellence so that appropriate evaluation, follow-up, genetic counseling, and/or treatment can be undertaken without subjecting patients and families to unwarranted and aggressive therapy.
Recommendation rating: C
■ RECOMMENDATION 4(D)
For patients with autoimmune thyroiditis, evaluation by an experienced thyroid ultrasonographer should be pursued in any patient with a suspicious thyroid examination (suspected nodule or significant gland asymmetry), especially if associated with palpable cervical lymphadenopathy.
Recommendation rating: B
[B4] What is the Optimal Evaluation of Children with Thyroid Nodules?
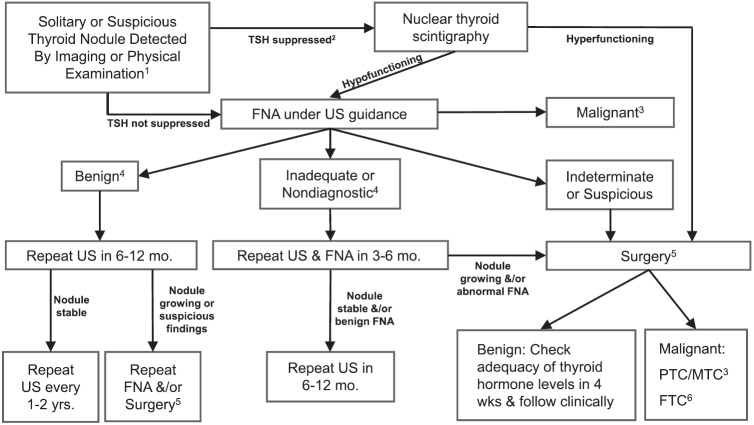
The 2009 ATA adult guidelines indicate that the evaluation and treatment of thyroid nodules in children should be the same as in adults (Recommendation 18). In general, this task force agrees with that sentiment, but there are specific areas in which we feel the approach should differ (Fig. 1).
FIG. 1.
Initial evaluation, treatment, and follow-up of the pediatric thyroid nodule. 1Assumes a solid or partially cystic nodule ≥1 cm or a nodule with concerning ultrasonographic features in a patient without personal risk factors for thyroid malignancy (see Sections B3 and B4). 2A suppressed TSH indicates a value below the lower limits of normal. 3Refer to PTC management guidelines (Section C1) or MTC management guidelines. 4Surgery can always be considered based upon suspicious ultrasound findings, concerning clinical presentation, nodule size >4 cm, compressive symptoms, and/or patient/family preference. 5Surgery implies lobectomy plus isthmusectomy in most cases. Surgery may be deferred in patients with an autonomous nodule and subclinical hyperthyroidism, but FNA should be considered if the nodule has features suspicious for PTC. (See Section B10.) Consider intraoperative frozen section for indeterminate and suspicious lesions. Can consider total thyroidectomy for nodules suspicious for malignancy on FNA. 6Consider completion thyroidectomy ± RAI versus observation ± TSH suppression based upon final pathology (see Section E1).
The 2009 adult guidelines indicate that FNA is not warranted for the evaluation of a nodule <1 cm in size unless the patient is considered high-risk, most commonly with a history of exposure to ionizing radiation, or the nodule is associated with pathologic regional lymph nodes. A size criterion is more problematic in children because thyroid volume changes with age and the size of the nodule alone does not predict malignant histology (110–112). Therefore, US characteristics and clinical context should be used more preferentially to identify nodules that warrant FNA. US features such as hypoechogenicity, irregular margins, and increased intranodular blood flow are more common in malignant lesions (110,113). In addition, the presence of microcalcifications and abnormal cervical lymph nodes increase the likelihood of malignancy (110,113). In all children with a suspicious nodule, US evaluation of the cervical lymph nodes should be performed.
The 2009 adult guidelines indicate that FNA is not warranted for the evaluation of a hyperfunctioning nodule in the adult. Although we concur that preoperative FNA of a hyperfunctioning nodule in a child is similarly not warranted, this is based on the understanding that all hyperfunctioning nodules in children will be surgically removed (see Section B10).
The 2009 adult guidelines indicate that calcitonin screening for MTC in adults with thyroid nodules may be cost effective, but it was neither recommended for nor against. In children and adolescents, the prevalence of sporadic MTC is extremely low. In addition, calcitonin reference ranges in children have not yet been widely validated, especially in children who have background thyroid disease such as thyroiditis. Further studies are needed to determine the cost-effectiveness of adding calcitonin to the evaluation of thyroid nodules in children.
The 2009 adult guidelines indicate that US-guided FNA is preferred for lesions with a higher likelihood of nondiagnostic cytology or sampling error. The sensitivity, specificity, and overall accuracy of FNA in children are similar to that of adults (114–119). However, based on the higher proportion of malignant nodules in children and the potential difficulty in obtaining repeat samples from children, this task force recommends that all FNA in children should be performed with US guidance. This is particularly relevant for complex cystic lesions, which require FNA of the solid portion, and it may also reduce the need for repeat FNA. The latter is important since FNA may alter the ultrasonographic features of thyroid nodules (120), thus making short-term follow-up more difficult.
A unique but very important difference in children is that PTC may present as diffusely infiltrating disease that results in diffuse enlargement of a lobe or the entire gland. For this reason, diffuse thyroid enlargement, especially if associated with palpable cervical lymph nodes, should prompt imaging. With rare exception, the diffuse infiltrating form of PTC is associated with microcalcifications that warrant FNA.
Finally, for both children and adults, cytopathology findings on FNA are categorized according to The Bethesda System for Reporting Thyroid Cytopathology (121). In this six-tier system, FNA results are reported as (a) nondiagnostic or unsatisfactory, (b) benign, (c) atypia or follicular lesion of undetermined significance (AUS/FLUS), (d) follicular/Hürthle neoplasm or suspicious for follicular/Hürthle neoplasm, (e) suggestive of malignancy, or (f) malignant. Insufficient or nondiagnostic cytopathology refers to a specimen with limited cellularity (fewer than six follicular cell groups each containing 10–15 cells per group from at least two separate aspirates), absence of follicular cells or poor fixation and preservation (122). There is a 1%–4% risk of malignancy in insufficient samples from adults (121), but very few data in children. Repeat FNA is an option in children but should be delayed for a minimum of 3 months in order to decrease the potential for atypical cellular features that may arise during the reparative process (123). In adults, the risk of malignancy in indeterminate nodules ranges from ∼5% to 15% in the AUS/FLUS category to 15%–30% in the follicular neoplasm or suggestive of neoplasm group (122). The limited data available suggest these indeterminate FNA categories account for ∼35% of pediatric FNA and that, in children, 28% of AUS/FLUS lesions and 58% of suggestive of follicular or Hürthle cell neoplasm are malignant (26,124). The 2009 adult guidelines suggested that repeat FNA was an option for adults with indeterminate cytopathology. However, due to the apparent increased probability of malignancy among these indeterminate categories in children, the task force recommends definitive surgery (lobectomy plus isthmusectomy) for indeterminate FNA findings in children (see Fig. 1).
■ RECOMMENDATION 5
The evaluation and treatment of thyroid nodules in children (Fig. 1) should be the same as in adults with the exceptions that (a) US characteristics and clinical context should be used rather than size alone to identify nodules that warrant FNA, (b) all FNA in children should be performed under US guidance, (c) preoperative FNA of a hyperfunctioning nodule in a child is not warranted as long as the lesion is removed, (d) a diffusely infiltrative form of PTC may occur in children and should be considered in a clinically suspicious gland, and (e) surgery (lobectomy plus isthmusectomy) is favored over repeat FNA for most nodules with indeterminate cytology.
Recommendation rating: B
[B5] Are There Molecular Signatures That Complement FNA and Improve the Diagnostic Utility of FNA in Children?
Studies in adults have shown that molecular testing aids in the management of thyroid nodules with indeterminate cytopathology (125–130). However, these diagnostic approaches have not yet been validated in pediatric patients. Mutational analysis has been used to examine thyroid nodules in children in limited single institution studies (26,131). Approximately 17% of pediatric FNAs may be positive for a mutation or rearrangement, the presence of which correlated with malignancy in 100% (26). However, the cytopathologic classification for these malignant tumors were AUS/FLUS, suggestive of follicular or Hürthle neoplasm, suggestive of malignancy, or malignant, all of which would have led to surgical removal regardless of the mutational analysis. Although a proprietary multigene expression classifier has been validated to corroborate a benign diagnosis in adults with indeterminate nodules (126), there are no studies determining its usefulness in the evaluation of the indeterminate pediatric thyroid nodule. Therefore, although current molecular diagnostics might improve the diagnostic acumen for indeterminate cytopathology in children, additional studies are required before a formal recommendation can be proffered.
■ RECOMMENDATION 6
A positive mutational test appears highly likely to be associated with malignancy. Conversely, insufficient data exist in children to rely on negative genetic studies to reliably exclude malignancy. Although molecular studies hold promise for complementing the results of FNA, particularly for nodules that yield indeterminate cytology, they have not yet been sufficiently validated in children and cannot be routinely recommended in routine clinical practice until further studies are conducted.
Recommendation rating: E
[B6] How Should Thyroid Nodules Be Treated in Children?
The surgical approach to the child with a thyroid nodule is dictated by the FNA results (see Fig. 1). Every effort should be made to ensure the FNA is performed in a controlled setting designed to accommodate age-appropriate anesthesia and pediatric advanced life support monitoring and intervention. In an effort to provide clarity, the proposed classification scheme from the National Cancer Institute Thyroid FNA State of Science conference is used as a guide to stratify surgical intervention (122).
[B7] What Is the Recommended Approach for Children with Benign Thyroid Cytopathology?
A key element in this question is whether or not “benign” lesions in children as defined by absence of suspicious US findings and benign FNA are ever subsequently found to be malignant. There are insufficient data to answer this question in children, but there are studies that have included both children and adults (132–134). The false-negative rate appears to be quite low, in the range of 3%–5% (114); however, the false negative rate may be higher in larger lesions secondary to an increased risk of sampling error (27,135–137).
[B8] Is There a Role for Levothyroxine Suppression Therapy?
The literature in this area is conflicting. Not all studies have used the same methodology nor have they always separated spontaneous thyroid nodules from radiation-induced thyroid nodules. Furthermore, some but not all benign thyroid nodules regress spontaneously, and this might be more common in small cystic lesions (138,139). Levothyroxine (LT4) suppression therapy has been evaluated for its efficacy to reduce nodule size or to reduce the risk of subsequent nodule formation. However, there are only minimal data regarding long-term safety and potential side-effects of LT4 therapy (140,141).
LT4 therapy has been prescribed to reduce the size of benign thyroid nodules, but the clinical benefit of a small to modest reduction in size is not clear (142–147). About a third (30.6%) of euthyroid children had a ≥50% reduction in nodule size, which was directly correlated with TSH levels (r=0.640, p<0.001) and inversely with LT4 dose (r=−0.389, p=0.009) (140).
Thyroid hormone has also been used in pediatric patients with radiation-induced thyroid nodules in which the formation of subsequent nodules has been shown to be reduced (148,149). It is not clear if this data can be extrapolated to pediatric patients with spontaneous nodules, and LT4 therapy had no effect on the incidence of thyroid cancer (148).
Whether LT4 therapy is used or not, an increase in nodule size is more commonly associated with malignant disease and should prompt re-evaluation and/or surgical resection (see Section B9). Alternatives to surgery have been evaluated in adults, but they have not yet been evaluated in children and their use cannot be recommended.
■ RECOMMENDATION 7
We are unable to recommend for or against the routine use of LT4 therapy for children with benign thyroid nodules. In general, the data support the efficacy of LT4 therapy to reduce the size and risk of subsequent nodule formation, but there are no data to weigh this potential benefit against the potential risks of long-term suppression therapy. In patients with compressive symptoms or a history of radiation exposure the benefits of LT4 therapy may be more apparent.
Recommendation rating: I
[B9] Is There a Role for Surgery in Children with Benign Nodules?
For the subset of children who have benign cytopathology, surgery may be considered due to increasing size, compressive symptoms, cosmetic reasons, or patient/parent choice. For growing nodules (defined in adults as a ≥50% increase in volume or ≥20% increase in at least two dimensions) or nodules that have developed suspicious US characteristics, repeat FNA should be performed prior to surgery to assist with surgical planning and preoperative staging. FNA of nodules >4 cm appears to have decreased sensitivity for the diagnosis of malignancy (27,135–137). Given the high false-negative rate of FNA in large lesions, and also to simplify long-term follow-up, surgery should be considered for FNA-documented benign nodules >4 cm, especially if they are solid. If surgery is undertaken, lobectomy is preferred to minimize the risk for complications.
■ RECOMMENDATION 8
Benign lesions should be followed by serial US (see Fig. 1) and undergo repeat FNA if suspicious features develop or the lesion continues to grow. Lobectomy may be performed in patients with compressive symptoms and cosmetic concerns or according to patient/parent preference and should be considered in all apparently benign solid thyroid nodules >4 cm, those lesions demonstrating significant growth, or in the presence of other clinical concerns for malignancy.
Recommendation rating: B
[B10] What Is the Optimal Management of the Child with an Autonomous Thyroid Nodule?
Pediatric patients are occasionally found to have an autonomously functioning nodule (toxic adenoma) diagnosed by a suppressed TSH and increased, nodule-specific uptake on nuclear medicine radioisotope scan (99mTc pertechnetate or iodine-123 [123I]) (150,151). These lesions are most frequently associated with somatic activating mutations within the genes encoding the TSH receptor or the Gs-alpha subunit (151). On examination, children are either euthyroid or may have mild signs or symptoms of hyperthyroidism.
In adults, the treatment options for autonomous nodules include 131I ablation, surgical resection, or ethanol injection. Because of concerns of the mutagenic effect of low-activity radioiodine on the normal thyroid tissue, and reports that up to one third of patients may be found to have an incidentally discovered DTC associated with autonomous nodules (150), surgical resection is the usual recommendation for most pediatric patients because the safety of observation or alternative treatments is unstudied in children. However, in asymptomatic patients with an autonomous nodule and subclinical hyperthyroidism, surgery may be deferred, but FNA should be considered if the nodule has features suggestive of PTC.
■ RECOMMENDATION 9
For pediatric patients with a suppressed TSH associated with a thyroid nodule, thyroid scintigraphy should be pursued. Increased uptake within the nodule is consistent with autonomous nodular function. Surgical resection, most commonly lobectomy, is the recommended approach for most autonomous nodules in children and adolescents.
Recommendation rating: A
[C1] Papillary Thyroid Cancer—Initial Management Guidelines
[C2] What Is the Optimal Preoperative Evaluation for the Child with Newly Diagnosed PTC?
The preoperative evaluation of the newly diagnosed pediatric PTC patient is critical for optimizing surgical outcome and medical therapy. In all cases, a comprehensive neck US using a high-resolution probe (7.5 MHz or higher) and Doppler technique should be obtained by an experienced ultrasonographer. All regions of the neck should be interrogated, recognizing that US has decreased sensitivity to identify malignant lymphadenopathy in the central neck (level VI) (152,153). A complete US examination should be performed prior to surgery if it was not performed with the FNA. The goal is to identify locoregional metastatic disease otherwise not appreciated on physical examination (154–157).
Given the very high rate of cervical lymph node metastases in children with PTC, the preoperative identification of suspicious lymph nodes affords the surgeon an opportunity to more thoughtfully plan comprehensive, compartment-oriented, lymph node dissection during the initial surgery with the intent to decrease recurrence rates and the need for additional surgery (154,157). In patients with large or fixed thyroid masses or bulky metastatic lymphadenopathy, US may be less sensitive at detecting metastatic disease to deep tissue regions, such as the superior mediastinum (level VII), the retropharyngeal, parapharyngeal, and subclavicular spaces (152,153). The addition of cross-sectional imaging using contrast-enhanced computed tomography (CT) or magnetic resonance imaging (MRI), depending on local expertise and preference, should be considered, especially if there is any concern for invasion of the aero-digestive tract (158–161). If iodinated contrast agents are used, further evaluation and treatment with RAI may need to be delayed for 2–3 months until total body iodine burden decreases. The advantage of CT over MRI is that CT has shorter image acquisition times, making scheduling more accessible and reducing the need for conscious sedation in younger patients.
A chest x-ray and/or chest CT may be considered in those with substantial cervical lymph node disease, in whom the prevalence of lung metastases is increased (9,10,24,65,162,163). Pediatric-specific protocols should be used to minimize ionizing radiation exposure. Routine chest CT is not recommended for patients with minimal neck disease because pulmonary metastases are likely to be identified when the child is subsequently staged with a stimulated Tg and diagnostic whole-body scan (DxWBS) (see Section C8) (24,49,164–166).
Thyroid nuclear scintigraphy for the evaluation of newly diagnosed PTC should only be pursued if the patient presents with a suppressed TSH. Decreased uptake on thyroid scintigraphy is nonspecific for thyroid malignancy (119). Additionally, the task force does not recommend the routine use of additional imaging (e.g., bone scan or [18F]-fluoro-deoxyglucose positron emission tomography/computed tomography [18FDG-PET/CT]) in the evaluation of children for PTC. These studies are not validated in this setting and the likelihood of finding disease in an otherwise asymptomatic patient is low and nonspecific (see Section D5).
■ RECOMMENDATION 10
A comprehensive neck US to interrogate all regions of the neck is required in order to optimize the preoperative surgical plan. FNA of suspicious lateral neck lymph nodes is recommended (see Recommendation 13). Anatomic imaging by MRI or CT with contrast should be considered in patients with large or fixed thyroid masses, vocal cord paralysis, or bulky metastatic lymphadenopathy in order to optimize surgical planning.
Recommendation rating: A
[C3] What Is the Recommended Surgical Approach for the Patient with a Diagnosis of PTC?
For the majority of patients with PTC, total thyroidectomy (TT) is the recommended initial surgical approach. In this procedure, the left and right thyroid lobes, the pyramidal lobe (when present), and the isthmus are resected. Alternatively, in patients with a small unilateral tumor confined to the thyroid gland, a near-TT, whereby a small amount of thyroid tissue (<1%–2%) is left in place at the entry point of the recurrent laryngeal nerve (RLN) and/or superior parathyroid glands, might be considered in an effort to decrease the risk of permanent damage to these structures. This recommendation for more comprehensive thyroid surgery in pediatric patients is based on data showing an increased incidence of bilateral and multifocal disease (30% and 65%, respectively) (11,14,47,52,167), as well as an increased risk for recurrence and subsequent second surgical procedures when less than a near-TT or TT is performed (5,14,15,44,47,51,168). In long-term analysis of 215 pediatric patients with PTC, bilateral lobar resection compared with lobectomy was shown to decrease the incidence of local recurrence from 35% to 6% over 40 years of follow-up (5). Bilateral thyroid surgery also optimizes the use of RAI for imaging and/or treatment and Tg as a marker to detect persistent/recurrent disease (8,169–171). Using an intracapsular approach, the superior parathyroid glands may be most easily preserved by maintaining arterial inflow and venous drainage (172–174).
■ RECOMMENDATION 11
For the majority of children, TT is recommended. The rationale for this approach is based on multiple studies showing an increased incidence of bilateral and multifocal disease. In long-term analysis, bilateral lobar resection compared with lobectomy has been shown to decrease the risk for persistent/recurrent disease.
Recommendation rating: A
[C4] Should Central Neck Dissection Be Performed?
In patients with preoperative evidence of central and/or lateral neck metastasis, a therapeutic central neck dissection (CND) should be performed. For this subgroup of patients, who are also at increased risk of pulmonary metastases (10,14,65), CND is associated with a decreased risk of persistent/ recurrent locoregional disease as well as the potential to increase the efficacy of 131I treatment for distant metastases (14,15,22,47,48).
The increased incidence of cervical metastasis in children suggests that prophylactic CND, as defined in the 2009 ATA consensus statement on the terminology and classification of CND for thyroid cancer (175), should be considered at the time of initial surgery for pediatric patients with PTC. This is particularly relevant given that decreased disease-free survival (DFS) is most strongly correlated with the presence of persistent or recurrent locoregional disease (5,13–15,22,47,52).
Unfortunately, there are no data that reliably predict which subgroup of patients is at increased risk for locoregional metastasis. Larger tumor size (>4 cm) has been shown to correlate with an increased risk of lymph node metastases (10,11,176). However, up to 36% of tumors ≤4 cm have cervical lymph node metastasis (10). In addition, several of the panel experts have cared for children with regional metastasis found in children with primary tumors ≤1 cm in size. In adults, these tumors are labeled papillary thyroid microcarcinoma (PTMC) and scoring systems have been described to predict the likelihood of metastasis (177). However, the thyroid volume is smaller in young children so that the size criteria used for tumor staging (see Section B4), as well as the diagnosis of PTMC, may not apply to children (178).
While data suggest that pediatric patients with thyroid cancer typically have 100% 10-year disease-specific survival (5,8,162,179), the extent of initial surgery appears to have the greatest impact on improving long-term DFS (5,47). However, without long-term, prospective data and a reliable set of criteria to stratify which patients would benefit from more aggressive surgical resection, one must weigh the risks of more aggressive surgery with the potential benefit of decreasing the incidence of persistent/recurrent disease.
The limited data suggest that, in children, TT with prophylactic CND is associated with increased DFS, as high as 95% at 5 and 10 years (46,163). However, the data are mixed and possibly related to the use of adjunctive RAI remnant ablation. In a retrospective study examining 75 children with PTC, 80% of whom underwent TT with 131I remnant ablation, the type and extent of neck dissection did not impact the risk for locoregional or distant metastasis (15). Conversely, another study suggested that TT with prophylactic CND may reduce the risk for reoperation that was as high as 77% in those without CND (44). Some groups suggest routinely considering a prophylactic CND, particularly for larger tumors (1,180,181), whereas others suggest making this decision based upon intraoperative findings (182).
If and when performed, CND should only be performed by a surgeon highly experienced in the procedure. To reduce the risk of recurrence, a comprehensive and compartment-based lymph node dissection should be pursued rather than “berry picking” (183). In patients with unifocal disease, data from adult patients suggest that ipsilateral, prophylactic CND may provide the same potential benefit while decreasing the higher complication rate associated with bilateral CND (184). During ipsilateral CND, the incorporation of frozen section to stratify which patients should undergo contralateral (complete) prophylactic CND may achieve a balance between the potential risks and benefits of this procedure (185).
With these considerations in mind, the following recommendations are made in an attempt to balance the goal of achieving surgical remission with the potential increased risk of complications that may be unnecessary for patients with minimal or no locoregional metastasis.
■ RECOMMENDATION 12(A)
CND is recommended for children with malignant cytology and clinical evidence of gross extrathyroidal invasion and/or locoregional metastasis on preoperative staging or intraoperative findings. This approach may be associated with a decreased need for second surgical procedures and increased DFS.
Recommendation rating: B
■ RECOMMENDATION 12(B)
For patients with PTC and no clinical evidence of gross extrathyroidal invasion and/or locoregional metastasis, prophylactic CND may be selectively considered based upon tumor focality and size and the experience of the surgeon. For patients with unifocal disease, ipsilateral CND, with pursuit of contralateral CND based on intraoperative findings, may help balance the risks and benefits.
Recommendation rating: C
■ RECOMMENDATION 12(C)
Compartment-oriented resection is the recommended approach for lymph node dissection. Berry picking and attempting to use palpation to determine if metastatic disease is present in a lymph node are not recommended.
Recommendation rating: A
■ RECOMMENDATION 12(D)
Future studies to assess if TT with prophylactic CND dissection will lead to reduced reliance on 131I treatment, re-operative procedures, and improved DFS are recommended.
Recommendation rating: C
[C5] What Are the Indications for Lateral Neck Dissection?
Pediatric patients occasionally present with bulky disease to the lateral neck and may have suspicious lymph nodes in the lateral neck on preoperative US imaging. US findings suggestive of metastasis to a lymph node include increased size, rounded shape, loss of central hilum, cystic appearance, peripheral vascularity on Doppler imaging, and microcalcifications (186), with the latter two features having the highest specificity for malignancy (113). The US appearance of the lymph nodes may be considered sufficient evidence to pursue lateral lymph node dissection; however, in patients undergoing surgery, FNA to confirm metastasis to the lateral neck lymph nodes should be performed prior to lateral neck dissection. The addition of a Tg measurement in the FNA washout fluid may be used to confirm equivocal cytological evidence of metastatic disease, even in the presence of serum anti-Tg antibodies (TgAb) (187–191) (see Section D2). When indicated, compartment-oriented lateral neck dissection (levels III, IV, anterior V, and II) is associated with a reduction in persistent/recurrent disease and improved DFS (10,14,47).
■ RECOMMENDATION 13
Cytological confirmation of metastatic disease to lymph nodes in the lateral neck is recommended prior to surgery. Routine prophylactic lateral neck dissection (levels III, IV, anterior V, and II) is not recommended. However, lateral neck dissection should be performed on patients with cytologic evidence of metastases to the lateral neck. Measurement of Tg in the FNA washout can be considered if the cytological diagnosis is equivocal.
Recommendation rating: B
[C6] What Are the Possible Complications of Surgery and What Should Be Done to Minimize the Risks of Surgery?
The lower incidence of thyroid disease requiring surgical intervention in children combined with a higher incidence of locoregional lymph node metastasis has been associated with an increased risk of complications for pediatric patients undergoing TT. Utilizing high-volume thyroid surgeons, defined as a surgeon who performs 30 or more cervical endocrine procedures annually, can reduce the rate of complications (70,71). In a cross-sectional analysis of over 600 pediatric patients undergoing thyroid surgery, there were fewer general complications (8.7% vs. 13.4%) and endocrine complications (5.6% vs. 11%) when the procedures were performed by high-volume surgeons (71). In addition, the duration of stay and cost were significantly lower when the procedure was performed by a high-volume surgeon (71).
The most common complications after thyroidectomy are endocrine related and include transient or permanent hypoparathyroidism, with an average rate of approximately 5%–15%. In a high-volume tertiary endocrine surgical practice, the risk of permanent hypoparathyroidism is <2.5% (72). Surgery specific, non–endocrine-related complications include RLN damage, spinal accessory nerve injury, and Horner syndrome, with an average rate of 1%–6% (10,13,46,47,70,72). In patients younger than 10 years of age, there is an increased risk of complications associated with the presence of ETE, lymph node dissection, and repeat surgery (10,70,168).
The risk of hypoparathyroidism correlates with the extent of surgery. Even in patients in whom the parathyroid glands are identified and viability of gland function is likely, manipulation of the parathyroid glands may lead to transient or permanent hypoparathyroidism. Autotransplantation of parathyroid tissue after frozen-section confirmation is utilized if there is any concern of devitalization, and it is associated with a decreased risk of permanent hypoparathyroidism (192,193). Postoperatively, several approaches can predict which patients are at an increased risk of developing hypocalcemia, including serial measurements of serum calcium (194) as well as measurement of a peri-operative intact parathyroid hormone (iPTH) level. The utility of postoperative iPTH is fairly well established with a level of <10–15 pg/mL correlating with an increased risk to develop clinically significant hypocalcemia (195,196). An elevated postoperative serum phosphorous may also be predictive (197). The use of peri-operative iPTH and/or phosphorus monitoring may decrease morbidity and allow for stratification of patients who would benefit from more intensive monitoring and treatment with calcium and calcitriol. An alternative to this approach is to place all patients who have undergone TT, especially those who undergo concomitant CND, on empiric calcium with or without calcitriol replacement therapy.
No monitoring devices have been shown to decrease the rate of non-endocrine surgical complications. The use of intraoperative RLN monitoring may be considered as an adjunct monitoring device and may be considered for younger patients (<10 years of age), in patients undergoing CND, and in patients undergoing repeat surgical procedures. However, the use of RLN monitoring has not been clearly shown to lower the incidence of RLN damage (198).
■ RECOMMENDATION 14(A)
Pediatric thyroid surgery should be performed in a hospital with the full spectrum of pediatric specialty care, to include, but not be limited to endocrinology, radiology (US and anatomic imaging), nuclear medicine, anesthesia, a high-volume thyroid surgeon, and intensive care. Pediatric thyroid surgery, especially if compartment-focused lymph node resection is indicated, should ideally be performed by a surgeon who performs at least 30 or more cervical endocrine procedures annually. Thyroid surgery performed under these guidelines is associated with lower complications rates, decreased hospital stay, and lower cost.
Recommendation rating: B
■ RECOMMENDATION 14(B)
The early incorporation of calcium and calcitriol in patients at high risk for hypocalcemia may decrease the risks of symptomatic hypocalcemia. Postoperative iPTH measurement may be used to help predict which patients would benefit from more intensive monitoring and treatment.
Recommendation rating: B
[C7] What Tumor Classification Systems Can Be Used for Pediatric PTC?
No single postoperative staging system has been validated in children with PTC, and the utility of extrapolating adult staging systems into the pediatric setting is limited by the observed clinical disparity between the two age groups. Specifically, the age-metastasis-extent of disease-size of tumor (AMES) and metastasis-age-completeness of resection-invasion-size (MACIS) have been examined, but the data are limited and the utility of these staging systems in pediatric patients with PTC remains unclear (176, 199). The AJCC TNM classification system (Table 5) is the most widely used system for describing the extent of disease and prognosis in the adult population (69). However, due to the extremely low disease-specific mortality in children with PTC and the fact that all patients aged<45 years have either stage I (no distant metastases) or stage II disease (with distant metastases), the TNM classification system remains limited in terms of determining prognosis in children. Despite this, the TNM classification is an excellent system with which to describe the extent of disease as well as to stratify an approach to evaluation and management. Especially useful to risk-stratify the pediatric PTC patient is knowledge regarding lymph node status. Children with PTC who have gross cervical lymph node disease at diagnosis are more likely to have multifocal disease (89% vs. 16%), an increased incidence of pulmonary metastasis (20% versus none), and increased persistent (30% versus none) and/or recurrent (53% versus none) disease compared with children without palpable nodal disease (53,65).
Table 5.
American Joint Committee on Cancer TNM Classification System for Differentiated Thyroid Carcinomaa
| Primary tumor (T) | ||
| TX | Size not assessed, limited to the thyroid | |
| T1 | T1a | ≤ 1 cm, limited to the thyroid |
| T1b | > 1 cm but ≤ 2 cm, limited to the thyroid | |
| T2 | > 2 cm but ≤ 4 cm, limited to the thyroid | |
| T3 | > 4 cm, limited to the thyroid, or any tumor with minimal extrathyroid extension | |
| T4 | T4a | Tumor extends beyond the thyroid capsule to invade subcutaneous soft tissues, larynx, trachea, esophagus, or recurrent laryngeal nerve |
| T4b | Tumor invades prevertebral fascia or encases carotid artery or mediastinal vessels | |
| Lymph nodes (N) | ||
| NX | Regional lymph nodes not assessed | |
| N0 | No regional lymph node metastasis | |
| N1 | N1a | Metastasis to level VI (pretracheal, paratracheal, and prelaryngeal/ Delphian lymph nodes) |
| N1b | Metastasis to unilateral, bilateral, or contralateral cervical levels I, II, III, IV, or V) or retropharyngeal or superior mediastinal lymph nodes (level VII) | |
| Distant metastasis (M) | ||
| MX | Distant metastasis not assessed | |
| M0 | No distant metastasis | |
| M1 | Distant metastasis | |
Pediatric patients are considered to have stage II disease if distant metastases are identified (M1); otherwise, all pediatric patients are considered to have stage I disease.
Used with the permission of the American Joint Committee on Cancer (AJCC), Chicago, Illinois. The original source for this material is the AJCC Cancer Staging Manual, 7th edition (2010) published by Springer Science and Business Media LLC, www.springer.com (69).
Therefore, using the TNM classification system, specifically regional lymph node and distant metastasis staging, one can categorize pediatric patients into one of three risk groups. This categorization strategy does not define the risk of mortality (which is low for both stage I and II patients) but identifies patients at risk of persistent cervical disease and helps to determine which patients should undergo postoperative staging to screen for the presence of distant metastasis (Table 6 and Section C8). These three groups are
Table 6.
American Thyroid Association Pediatric Thyroid Cancer Risk Levels and Postoperative Management in Children with Papillary Thyroid Carcinoma
| ATA pediatric risk levela | Definition | Initial postoperative stagingb | TSH goalc | Surveillance of patients with no evidence of diseased |
|---|---|---|---|---|
| Low | Disease grossly confined to the thyroid with N0/Nx disease or patients with incidental N1a disease (microscopic metastasis to a small number of central neck lymph nodes) | Tge | 0.5–1.0 mIU/L | US at 6 months postoperatively and then annually × 5 years Tge on LT4 every 3–6 months for 2 years and then annually |
| Intermediate | Extensive N1a or minimal N1b disease | TSH-stimulated Tge and diagnostic 123I scan in most patients (see Fig. 2) | 0.1–0.5 mIU/L | US at 6 months postoperatively, every 6–12 months for 5 years, and then less frequently Tge on LT4 every 3–6 months for 3 years and then annually Consider TSH-stimulated Tge ± diagnostic 123I scan in 1–2 years in patients treated with 131I |
| High | Regionally extensive disease (extensive N1b) or locally invasive disease (T4 tumors), with or without distant metastasis | TSH-stimulated Tge and diagnostic 123I scan in all patients (see Fig. 2) | <0.1 mIU/L | US at 6 months postoperatively, every 6–12 months for 5 years, and then less frequently Tge on LT4 every 3–6 months for 3 years and then annually TSH-stimulated Tge ± diagnostic 123I scan in 1–2 years in patients treated with 131I |
Please refer to Table 5 for AJCC TNM classification system.
“Risk” is defined as the likelihood of having persistent cervical disease and/or distant metastases after initial total thyroidectomy ± lymph node dissection by a high volume thyroid surgeon and is not the risk for mortality, which is extremely low in the pediatric population. See Section C7 for further discussion.
Initial postoperative staging that is done within 12 weeks after surgery.
These are initial targets for TSH suppression and should be adapted to the patient's known or suspected disease status; in ATA Pediatric Intermediate- and High-risk patients who have no evidence of disease after 3–5 years of follow-up, the TSH can be allowed to rise to the low normal range.
Postoperative surveillance implies studies done at 6 months after the initial surgery and beyond in patients who are believed to be disease free; the intensity of follow-up and extent of diagnostic studies are determined by initial postoperative staging, current disease status, and whether or not 131I was given; may not necessarily apply to patients with known or suspected residual disease (see Fig. 3) or FTC.
Assumes a negative TgAb (see Section D2); in TgAb-positive patients, consideration can be given (except in patients with T4 or M1 disease) to deferred postoperative staging to allow time for TgAb clearance.
ATA, American Thyroid Association; LT4, levothyroxine; TgAb, thyroglobulin antibody; US, ultrasound.
-
1. ATA Pediatric Low-Risk
Disease grossly confined to the thyroid with N0 or NX disease or patients with incidental N1a metastasis in which “incidental” is defined as the presence of microscopic metastasis to a small number of central neck lymph nodes. These patients appear to be at lowest risk for distant metastasis but may still be at risk for residual cervical disease, especially if the initial surgery did not include a CND.
-
2. ATA Pediatric Intermediate-Risk
Extensive N1a or minimal N1b disease. These patients appear to be at low risk for distant metastasis but are at an increased risk for incomplete lymph node resection and persistent cervical disease.
The impact of the pathologic identification of microscopic (ETE) (T3 disease) on management and outcomes has not been well studied in children with PTC, but patients with minimal ETE are probably either ATA Pediatric Low- or Intermediate-Risk, depending on other clinical factors.
-
3. ATA Pediatric High-Risk
Regionally extensive disease (extensive N1b) or locally invasive disease (T4 tumors), with or without distant metastasis. Patients in this group are at the highest risk for incomplete resection, persistent disease, and distant metastasis.
■ RECOMMENDATION 15(A)
The AJCC TNM classification system should be used to describe the extent of disease in pediatric patients with PTC (Table 5). Children with PTC should be stratified into risk levels (ATA Pediatric Low-, Intermediate-, or High-Risk) based on clinical presentation, tumor size, and evidence of regional invasion and metastasis (Table 6). The extent of disease in the neck at diagnosis appears to correlate best with the risk for distant metastasis and/or persistent disease that may require additional treatment.
Recommendation rating: B
■ RECOMMENDATION 15(B)
Patients found to have disease confined to the thyroid gland, as well as incidental evidence of minimal, microscopic disease to lymph nodes in the central neck (level VI), fall into the ATA Pediatric Low-Risk level (Table 6).
The presence of extensive, extrathyroidal invasion or metastasis defines patients at greater risk for persistent regional or distant metastasis. Patients with these features are categorized within the ATA Pediatric Intermediate- or High-Risk levels (Table 6). Within these categories, additional postoperative staging is warranted to better define which patients may or may not benefit from additional therapy.
Recommendation rating: B
[C8] What Postoperative Staging Is Recommended?
For most patients, initial staging (Fig. 2) is typically performed within 12 weeks postoperatively. This affords the patient and family time to recover from surgery, while at the same time avoiding delay in additional therapy, if needed. The purpose of postoperative staging is to assess for evidence of persistent locoregional disease and to identify patients who are likely to benefit from additional therapy with 131I, such as those suspected or known to have distant metastases. The individual patient's risk level (Table 6) helps to determine the extent of postoperative testing. While the committee recognizes that no prospective studies have been performed to validate a stratified risk-based approach in children with PTC, an individualized approach incorporating pathologic findings and postoperative clinical data is founded on well-accepted approaches to therapy in adults (1,3) as well as personal experience in certain pediatric practices (200). The foundation of this stratification system for pediatric patients, however, assumes complete and accurate preoperative staging for regional disease (see Section C2) and appropriate surgery that is performed by a high-volume thyroid cancer surgeon.
FIG. 2.
Initial postoperative staging for American Thyroid Association pediatric intermediate- and high-risk pediatric thyroid carcinoma. 1Assumes a negative TgAb (see Section D2) and a TSH >30 mIU/L; in TgAb-positive patients, consideration can be given (except in patients with T4 tumors or clinical M1 disease) to deferred evaluation to allow time for TgAb clearance (“delayed” staging). 2Imaging includes neck ultrasonography ± SPECT/CT at the time of the diagnostic thyroid scan. 3Consider 131I in patients with thyroid bed uptake and T4 tumors or known residual microscopic cervical disease. 4While there are no prospective studies in patients ≤18 years of age, the use of 131I remnant ablation may not decrease the risk for persistent or recurrent disease. Consider surveillance rather than 131I with further therapy determined by surveillance data. 5Repeat postoperative staging 3–6 months after surgery. 6See Table 6 and Figures 3 and 4.
For ATA Pediatric Low-risk patients, initial postoperative staging includes a TSH-suppressed Tg. The interpretation of serum Tg and most importantly, interpretation of the trend in serum Tg over time are summarized in Section D2.
In contrast, for ATA Pediatric Intermediate- and High-Risk patients, a TSH-stimulated Tg and DxWBS are generally recommended for further risk stratification and determination of treatment with 131I (Fig. 2). Children who fall into the ATA Pediatric Intermediate- and High-Risk categories are prepared following standard guidelines for 131I therapy (see Section C12), and the TSH-stimulated Tg and DxWBS data are used to assess for evidence of residual disease (Fig. 2). In patients without evidence of TgAb, the TSH-stimulated Tg is a reliable marker for evaluating for the presence or absence of residual disease (see Section D2). In a recent study examining 218 consecutive adult DTC patients across all ATA risk stratification levels, a TSH-stimulated Tg <2 ng/mL had a 94.9% predictive value for the absence of disease (201).
Whether a DxWBS might image disease that is not identified through neck US is a matter of debate and few data in children address this. In one pediatric study, US and DxWBS equally identified lymph node metastases in the majority of patients (35/45); however, in six patients, lymph node metastases were found only with a posttreatment RAI WBS (202). Two of the patients were TgAb positive, reinforcing the potential benefit of DxWBS in patients who are TgAb positive (202,203). DxWBS may also visualize disease in the lungs or mediastinum that would not otherwise be shown by neck US or other cross-sectional imaging (49).
For patients with cervical iodine uptake, the addition of hybrid imaging using single photon emission computed tomography with integrated conventional CT (SPECT/CT) offers improved anatomic imaging to determine whether cervical uptake is secondary to remnant thyroid tissue or metastasis to regional lymph nodes (204–206).
A potential drawback of DxWBS imaging is that if 131I is used, the small diagnostic activity may theoretically “stun” the iodine-avid tissue and reduce subsequent 131I uptake if high-activity 131I treatment is then used (207,208). This issue can be reduced by selecting the lowest possible activity of 131I (2.7–4.0 mCi=100–148 MBq) (209) or by using 123I (207,210). Due to its lower cost, 131I is more commonly used, but 123I provides superior imaging quality and generates lower absorbed doses of radiation to the tissues (207,211), which favors its use in children.
Taken together, postoperative staging is used to further stratify which children may or may not benefit from additional treatment with surgery and/or RAI therapy. Irrespective of initial risk stratification, all patients will enter surveillance, ensuring that appropriate therapy will be given if evidence of disease is ultimately identified. As long as the patient is maintained on tailored LT4 suppression and a proper surveillance plan is followed (Table 6, Fig. 2), delayed treatment is not expected to alter the already low disease-specific mortality due to the indolent nature of PTC in children. Furthermore, a more individualized and conservative approach to postoperative staging and treatment will decrease unnecessary exposure to 131I in children without evidence of disease, in whom the risks of routine 131I therapy likely outweigh any benefit. Because of the lack of high-level evidence to help guide these difficult medical decisions, families should be fully informed about the options and their risks/benefits as the surveillance and treatment plans are being formulated.
■ RECOMMENDATION 16
Postoperative staging is usually performed within 12 weeks after surgery (Fig. 2) and allows for stratification of patients who may or may not benefit from further therapy, to include additional surgery or 131I therapy. ATA Pediatric Low-Risk patients may be initially assessed and followed with a TSH-suppressed Tg alone. In contrast, a TSH-stimulated Tg and a DxWBS is typically recommended to assess for evidence of persistent disease in ATA Pediatric Intermediate- and High-Risk patients. Additional imaging, to include neck US and/or hybrid imaging using SPECT/CT, may be used conjunctively to more accurately define the anatomic location of RAI uptake noted on a DxWBS. Whenever possible, 123I should be used for the DxWBS.
Recommendation rating: B
[C9] What Are the Goals of 131I Treatment?
The traditional approach to managing pediatric patients with DTC included reflexive postsurgical 131I therapy, which was prescribed in an effort to eliminate residual thyroid tissue in order to increase the sensitivity for using serum Tg as a biomarker for recurrent disease. In addition, 131I was prescribed in an effort to decrease the risk of recurrent disease (see Section C10).
The goal of 131I therapy is to decrease the risks of thyroid cancer recurrence and theoretically to improve mortality by eliminating iodine-avid disease. RAI was proposed as a specific treatment for DTC in 1946 after an adult with functional thyroid cancer metastases responded to multiple RAI treatments (212), and 131I therapy has since been broadly incorporated into treatment protocols for both adults and children (1,213). A recent survey indicates that use of therapeutic 131I for all thyroid cancers, regardless of tumor size, has increased from 1990 to 2008 (214).
With increased awareness of the potential long-term side effects of 131I treatment (see Section C16), there are increased efforts to identify patients who have a high likelihood of benefit from therapy. Unfortunately, the majority of available data are based on a nonstratified approach in which all children underwent TT and variable extent of lymph node dissection, and the majority received therapeutic 131I. The challenge is to reduce or eliminate unnecessary 131I exposure for children who may not benefit without increasing disease-specific morbidity and mortality. The following sections address various aspects of this question.
[C10] What Is the Impact of 131I Therapy on Recurrence and Survival for Children with PTC?
Adjunctive 131I therapy may improve DFS in young adults (including some adolescents) but this has not been universally shown for those with small, stage I lesions (215). Reflective of this, the 2009 ATA guidelines and the current NCCN guidelines support the selective rather than universal administration of 131I, especially for young patients (<45 years of age) with intrathyroidal PTC and either no or limited lymph node disease (1,3).
Studies specifically examining the potential benefits of 131I therapy in children have been difficult to perform because the number of patients is small and the prognosis is favorable, regardless of adjunctive therapy (11,169,216,217). Arguments in favor of universal therapeutic 131I for children have been based on the observation that retention of the normal thyroid remnant may decrease the sensitivity for detecting metastases or recurrent disease by serum Tg and/or DxWBS (218,219). Arguments against the universal prescription of therapeutic 131I are based on the known short- and long-term toxicities (220), lack of data showing conclusive benefit from routine 131I therapy (5,13), a possible increase in the risk of secondary malignancies (5–7,221,222), and studies showing that Tg can remain useful and become undetectable in patients post TT despite not having received 131I (223–225).
Most of the data regarding 131I use in children have examined treatment of known residual disease rather than ablation of the normal thyroid remnant only (9). In patients with known residual disease, 131I therapy appears to decrease recurrence (9,43,51,162,226). However, large retrospective series in children show conflicting results regarding the potential for benefit from adjunctive 131I. In one study, 131I remnant ablation did not clearly decrease the risk for locoregional recurrence, distant metastases, or all-sites recurrence compared with surgery alone, but there was a trend toward reduction in the risk of distant metastases (p=0.06) (5). Unfortunately, overall survival was reduced in patients who had received external beam therapy, radium implants, or 131I, primarily secondary to an increase in nonthyroid, second malignancies. Another study also found no improvement in DFS following remnant ablation (13), but additional studies revealed a significant improvement in DFS for children with PTC treated with 131I and no clear increase in the risk of second primary malignancies (169).
[C11] Which Children Might Benefit from Therapeutic 131I?
131I is indicated for treatment of nodal or other locoregional disease that is not amenable to surgery as well as distant metastases that are known or presumed to be iodine-avid (169). In addition, some experts also advocate routine 131I therapy for children with T3 tumors or extensive regional nodal involvement (extensive N1a or N1b disease) (9,169).
Published studies show that children with iodine-avid pulmonary metastases benefit from 131I treatment, and complete remission is achievable for many patients, particularly those with microscopic and small-volume lung disease (9,57,58,162,227). Thus, for patients with pulmonary metastases, 131I is considered therapeutic, with the understanding that increasing burden of disease may ultimately require administration of multiple activities (57) (see Section D8).
■ RECOMMENDATION 17
131I is indicated for treatment of iodine-avid persistent locoregional or nodal disease that cannot be resected as well as known or presumed iodine-avid distant metastases. For patients with persistent disease following 131I administration, the decision to pursue additional 131I therapy should be individualized according to clinical data and previous response (see Fig. 3 and 4). The potential risks and benefits must be weighed on an individual basis.
Recommendation rating: B
FIG. 3.
Management of the pediatric patient with known or suspected residual/recurrent disease (no known distant metastases). This algorithm is intended to be used in children who are known or suspected to have residual or recurrent disease based upon the suppressed Tg level and knowledge of previous disease extent 6–12 months after all primary therapies have been completed. 1Assumes a negative TgAb (see Section D2); in TgAb-positive patients, the presence of TgAb alone cannot be interpreted as a sign of disease unless the titer is clearly rising. 2Imaging includes SPECT/CT at the time of the diagnostic thyroid scan and/or contrast-enhanced CT/MRI neck. 3Repeat 131I therapy in patients previously treated with high-dose 131I should generally be undertaken only if iodine-avid disease is suspected and a response to previous 131I therapy was observed (see Sections D7 and D8).
FIG. 4.
Management of the pediatric patient with known distant metastases. 1Assumes a negative TgAb (see Section D2); in TgAb-positive patients, the presence of TgAb alone cannot be interpreted as a sign of disease unless the titer is clearly rising; a declining TgAb titer would suggest continued response to treatment. 2Tg can transiently rise after 131I therapy and should not be misinterpreted as evidence for progression. 3Repeat 131I therapy in patients previously treated with high-dose 131I should be undertaken only if iodine-avid disease is suspected and if there was a previous response to therapy (see Section D7 and D8).
[C12] How Should a Child Be Prepared for 131I?
If 131I is prescribed, the TSH should be above 30 mIU/L to facilitate uptake (21,228,229). The majority of children will achieve this level of TSH by ≥14 days of LT4 withdrawal (230). For that reason, triiodothyronine supplementation during LT4 withdrawal is not usually required but can be considered for children who are especially sensitive to hypothyroid symptoms or if the withdrawal period extends beyond 3 weeks.
Recombinant human TSH (rhTSH) has been used for remnant ablation as well as for treatment of intermediate- and high-risk DTC in adults (231–233) and may result in a lower absorbed radiation activity to the blood (as much as one third lower) (234). However, data regarding the use of rhTSH in children are limited (235,236). Experience in children would suggest that the typical adult dose of rhTSH (two doses of 0.9 mg given 24 hours apart) appears to be safe and generates sufficient TSH levels (169,236,237). In particular, rhTSH might have a role in situations in which endogenous hypothyroidism should be avoided (e.g., significant medical comorbidities) or is impossible (e.g., TSH deficiency) (169,236).
To facilitate RAI uptake, a low-iodine diet is generally prescribed for 2 weeks prior to therapy, but the efficacy of this practice in children has not been specifically demonstrated. Nevertheless, a low-iodine diet has been shown to increase the effective radiation dose to the thyroid by 50%–150% in adults (238). For that reason, a low-iodine diet is commonly recommended. In children who received intravenous contrast during preoperative staging, it is advisable to wait approximately 2–3 months or to confirm normal (median normal 24-hour urine iodine excretion=143 μg/24 hour, 5%–95% range=75–297 μg/24 hour) (239) or low 24-hour urine iodine values before performing either a DxWBS or administering therapeutic 131I.
■ RECOMMENDATION 18
In order to facilitate 131I uptake by residual iodine-avid cancer, the TSH level should be above 30 mIU/L. This can be achieved in almost all children by withdrawing LT4 for ≥14 days. In selected patients who cannot mount an adequate TSH response or cannot tolerate profound hypothyroidism, rhTSH may be considered. Low-iodine diets have not been specifically evaluated in children but may enhance the effective radiation activity of 131I and are recommended.
Recommendation rating: A
[C13] What Should Be Considered for Administration of 131I?
General guidelines for safety in the administration of 131I were reviewed by the ATA Task Force on Radiation Safety in 2011 (240). There are few specific references to children, but the overall document pertains to children as well as adults. Once the decision to administer 131I is made, the safety of family members and classmates will help guide the decision for inpatient or outpatient therapy. This will be largely based on patient age and ability to comprehend the tasks required for outpatient therapy. Other factors to consider are the amount of radiation retained by the patient and the potential exposure time and distance between patient and others (240). In general, children and adolescents with PTC are primarily a radiation risk to others during the first 1–2 days after 131I therapy. For young children, this may be especially problematic, if they are not yet toilet trained or are frightened to sleep alone. Detailed instructions for the daily care of children who have received 131I are provided in the ATA guidelines on radiation safety and abbreviated in appendix 1 of that document (240).
Adjunctive therapies to minimize the risk of 131I to the treated child have not been well studied. Adequate hydration is essential to enhance 131I clearance and should be encouraged. Regular bowel evacuation is also important, so stool softeners or laxatives may be considered. Nausea and/or vomiting are common following 131I therapy, particularly in young children and those receiving higher 131I activities. In such cases, anti-emetics like the serotonin 5-HT3 receptor antagonists can be considered. Accelerating 131I clearance from the salivary glands may reduce the risk of sialadenitis, but the use of sialagogues such as sour candy or lemon juice is poorly studied in children. Some studies in adults found benefit by starting lemon drops 24 hours after 131I dosing (241), but some experts do not recommend this practice. Similarly, the use of the radioprotectant amifostine has not been validated in children, and a recent review of randomized control trials in adults found no benefit from amifostine therapy (242).
Adjunctive treatments to increase the efficacy of 131I therapy have also not been well studied in children. In adults with PTC, co-treatment with lithium has been suggested to increase 131I retention and improve the efficacy of treatment of metastatic tumors (243). To our knowledge, no study of children with PTC has evaluated the safety and efficacy of lithium co-treatment. Because the expression of NIS is more common and more robust in pediatric PTC, the effect of lithium on 131I retention might be less than that found in adults (169).
■ RECOMMENDATION 19(A)
Adequate hydration should be ensured in all children receiving therapeutic 131I to facilitate clearance of the radioisotope, and additional supportive care with anti-emetic medications and stool softeners/laxatives should be considered. Sour candy or lemon drops can be given after 131I treatment, but not all experts ascribe to this practice.
Recommendation rating: C
■ RECOMMENDATION 19(B)
The routine use of lithium and amifostine cannot be recommended.
Recommendation rating: F
[C14] How Is the Activity of Therapeutic 131I Determined?
Therapeutic 131I administration is commonly based on either empiric dosing or whole body dosimetry. There are no standardized activities of 131I for children and, to our knowledge, there are no data that compare the efficacy, safety, or long-term outcomes from 131I administration in children using these different approaches.
Empiric dosing offers the advantage of simplicity. Some adjust 131I activity according to weight or body surface area and give a fraction (e.g., child's weight in kilograms/70 kg) based on the typical adult activity used to treat similar disease extent (1,3,21,219,229). Others suggest that 131I activities to treat residual disease should be based on body weight alone (1.0–1.5 mCi/kg; 37–56 MBq/kg), while still others feel this may not be as reliable as dosing based on body surface area. In general terms, a 15-year-old may require five sixths of the adult activity, a 10-year-old may require one half of the adult activity, and a 5-year-old may only require one third of the adult activity for similar extent of disease (169).
For children with diffuse lung uptake or significant distant metastases, those undergoing multiple 131I treatments, or children who may have limited bone marrow reserve due to prior chemotherapy or radiation therapy, whole-body dosimetry can be used to calculate the largest activity of 131I that could theoretically be administered so that the absorbed activity to the blood does not exceed 200 rads (cGy) and that the whole-body retention 48 hours after administration does not exceed 4.44 GBq (120 mCi) in the absence, or 2.96 GBq (80 mCi) in the presence, of iodine-avid diffuse lung metastases, respectively (244–246). Lesional dosimetry can also be performed to select effective activities of 131I for children with substantial lung involvement or large tumor burden at distant sites such as bone (209,210,245,247,248). One must keep in mind that these toxicity constraints have not been validated in pediatrics and may be associated with significant toxicity in young children (249,250). Furthermore, these protocols are time consuming and not routinely available at all referral centers.
■ RECOMMENDATION 20
Based on the lack of data comparing empiric treatment and treatment informed by dosimetry, we are unable to recommend for or against either approach in most patients. Many experts provide the first activity of 131I based on an empiric estimate and reserve dosimetry for patients with diffuse pulmonary metastases or subsequent activities of 131I in patients with iodine-avid distant metastases who require additional therapy. However, dosimetry can be considered prior to the first 131I treatment in small children and in patients with limited bone marrow reserve. Due to the differences in body size and iodine clearance in children compared with adults, it is recommended that all activities of 131I should be calculated by experts with experience in dosing children.
Recommendation rating: I
[C15] Should a Posttreatment Whole-Body Scan Be Obtained?
Approximately 4–7 days after 131I therapy, a posttreatment whole-body scan should be performed to take advantage of the increased sensitivity associated with administration of the larger activity of 131I used for therapy (208). Newer gamma-camera systems allow scanning as early as 72 hours after 131I therapy (251). On occasion, the posttreatment WBS (RxWBS) may reveal metastatic disease (regional or pulmonary) that was not apparent on the DxWBS (218), but it remains uncertain if this knowledge informs future treatment or outcomes. If new lesions are identified on the RxWBS, the addition of SPECT/CT to the RxWBS may afford greater definition of residual disease during postoperative restaging (252).
In addition, the clearance of RAI from thyroid cancers has been shown to vary substantially with biological half-life ranging from 3 to 12 days (253). Rapid turnover of iodine might clear 131I by the time standard imaging protocols are performed, while other lesions might be better revealed with delayed imaging (254). For the rare child with elevated serum Tg and negative RxWBS, serial acquisition times may be beneficial in documenting disease and iodine avidity.
■ RECOMMENDATION 21
A posttreatment WBS is recommended for all children 4–7 days after 131I therapy. The addition of SPECT/CT may help to distinguish the anatomic location of focal uptake.
Recommendation rating: B
[C16] What Are the Acute and Long-Term Risks of 131I Therapy in Children?
There are both acute and long-term side effects and complications associated with exposure to therapeutic 131I. The side effects can be organized by organ system, and the majority are explained by mechanistic exposure based on the method of delivery, absorption, distribution, and clearance.
The short-term side effects of 131I are well known and include damage to tissues that incorporate iodine, resulting in sialadenitis, xerostomia, dental caries, stomatitis, ocular dryness, and nasolacrimal duct obstruction (255,256). Strategies exist to help treat or prevent 131I-related side effects (257,258); however, even a single activity of 131I may lead to permanent salivary gland dysfunction with life-long xerostomia, an increased incidence of dental caries, and an increase in the risk for salivary gland malignancy (258,259). The use of sour candy or lemon juice, starting 24 hours after 131I dosing, with vigorous hydration for 3–5 days may protect salivary gland function (241). The use of rhTSH has not been shown to decrease salivary gland toxicity compared to thyroid hormone withdrawal (260); however, lacrimal dysfunction (watery eyes) was more frequent in patients undergoing thyroid hormone withdrawal (261). None of these prophylactic measures or other sialogogues have been formally studied in the pediatric population.
Gonadal damage has been reported in both women and men (262,263). In postpubertal males, transient rise in follicle-stimulating hormone is common and may persist for up to 18 months after 131I exposure (263,264). Increasing cumulative activities of 131I may lead to decreased spermatogenesis generally without an effect on testosterone production (263,265,266). Current guidelines recommend that males avoid attempts at conception for at least 4 months post 131I therapy. Postpubertal testes appear to be more vulnerable than prepubertal testes to the toxic effects of ionizing radiation (267). Therefore, postpubertal males should be counseled and sperm banking should be considered for those receiving cumulative activities ≥400 mCi (14.8 GBq) (268).
Transient amenorrhea and menstrual irregularities are reported in up to 17% of females under the age of 40 years. This is true despite the fact that 65% of young women received a single low activity of 131I (average=81 mCi; 3 GBq) (269). Other studies have not shown an increase in infertility, miscarriage, or birth defects following 131I (262,270,271). Collectively, these data have led to the recommendation that conception should be avoided during the year immediately following 131I administration (272).
Acute suppression of bone marrow may occur but hematologic parameters usually normalize within 60 days after 131I exposure. Commonly a decline in leukocyte (∼57%) and platelet counts (∼44%) occurs within the first month after treatment. This is followed by a less pronounced decline in erythrocyte count (∼10%) by the second month after treatment, but usually all parameters normalize ∼3 months post therapy (273). Long-term bone marrow suppression is rare; however, there are reported cases of leukemia after multiple high activities of 131I administered over a short span of time (274). Therefore, it is important to allow for recovery of bone marrow between 131I treatments.
In support of these clinical observations, 131I has been shown in peripheral lymphocytes to induce a significant increase in the number of dicentric chromosomes (275–277), and the aberrations of chromosomes 1, 4, and 10 are not only more prevalent but are still apparent after 4 years (276). A recent report comparing thyroid hormone withdrawal to rhTSH suggests a lower frequency of lymphocyte chromosomal rearrangements after 131I dosing using rhTSH preparation (278).
A few studies combining patients of all ages have shown that 131I therapy is associated with an increased risk for second malignancies and an increase in overall mortality for patients with DTC (7). A large study by Brown et al. (6) reviewed data from over 30,000 subjects and found a significant increase in second malignancies among patients treated with 131I (relative risk 1.16, p<0.05). They also noted that the risk was greater for younger patients. In a study that exclusively evaluated children, Hay et al. (5) found that children who were treated with radiation (external beam radiation, radium implants, or 131I) developed a variety of second cancers (leukemia, stomach, bladder, colon, salivary gland, and breast) and had increased mortality compared with the general population. However, only 4 of the 15 patients that died from nonthyroid second primary malignancies were associated with the sole administration of 131I (one acute myelogenous leukemia, one lung, one adenocarcinoma, and one breast cancer) (5). Whether this resulted from aggressive treatment, an underlying predisposition to cancer, or from a direct effect of 131I is unknown, but the increase in overall mortality following 131I treatment of a disease with low disease-specific mortality is of growing concern.
It is difficult to determine from these data if there is a “safe” cumulative exposure to 131I or if the increase in second malignancies occurs following any amount of 131I. Further complicating this question is the fact that the effects of RAI may be amplified in children because a given activity of 131I is distributed over shorter distances, taken up by smaller organs, and accumulated by cells with increased growth and proliferation potential. Despite these limitations, Rubino et al. (7) proposed an activity–response relationship in which the relative risk for second malignancy appears to increase above a cumulative activity of 200 mCi (7.4 GBq) 131I, and Rivkees et al. (220) suggested an increased risk above a cumulative exposure to 300 mCi (11.1 GBq) 131I. However, there are anecdotal reports of acute myelogenous leukemia after 85 mCi (3.1 GBq) 131I, lung cancer after 150 mCi (5.6 GBq) 131I, and adenocarcinoma after 200 mCi (7.4 GBq) 131I (5). Unfortunately, there is a lack of long-term data to define a “safe” activity of 131I, and additional study is clearly warranted.
Lastly, for pediatric patients with lung metastases, a significant risk exists for 131I-induced pulmonary fibrosis when the retained 131I activity exceeds 80 mCi (3 GBq) (228,279). For that reason, patients with significant uptake on DxWBS are candidates for dosimetry or reduced 131I dosing.
In summary, there are clear benefits and risks, both acute and chronic, following administration of 131I. The challenge is to define the subgroup of patients who will not experience an increase in morbidity or disease-specific mortality if 131I is deferred or withheld.
■ RECOMMENDATION 22
There are clear benefits and risks, both acute and chronic, following administration of 131I during childhood. The challenge is to identify the patients for whom the benefits of 131I therapy outweigh the risks. Families should be provided full disclosure of the risks and benefits of 131I, and their opinion must be considered in the final decision.
Recommendation rating: C
[D1] Surveillance and Follow-Up of PTC in Children
[D2] What Is the Role of Tg Testing in the Follow-Up of PTC in Children?
Tg is a thyroid-specific glycoprotein that is synthesized and secreted by the normal thyroid and by differentiated thyroid carcinomas. Following surgery and 131I therapy, serum Tg levels serve as a sensitive marker of residual or recurrent disease (280–283); the magnitude of serum Tg elevation appears to correlate with the site(s) of metastatic disease and with the tumor subtype (280).
Highly sensitive and specific immunometric analyses for serum Tg have been shown to be more sensitive for detecting residual thyroid cancer in adults compared with the DxWBS (281,284–286). Currently, most laboratories use immunometric methods for Tg measurement, and these should be calibrated against the CRM-457 international standard (1). However, even with standardization, there can be significant differences in Tg results between various assays (171). For that reason, serial Tg measurements should ideally be performed in the same laboratory using the same assay.
In the absence of TgAb (see following section), serum Tg has a high degree of sensitivity and specificity to detect residual/recurrent DTC, with the highest sensitivity noted following TSH stimulation (TSH-stimulated Tg) (282). Serum Tg levels rise with TSH stimulation, and the duration of stimulation is generally longer in the hypothyroid state, resulting in higher serum Tg levels than occur after rhTSH in the euthyroid state (281). In adults, a TSH-stimulated serum Tg level >2 ng/mL has a high predictive value for disease (287).
Previous studies of children with DTC have focused on DxWBS as the “gold standard” for disease status (11,219,288), and there are few data regarding the interpretation of Tg levels in children with DTC. Because data suggest that serum Tg levels might be higher in children compared with adults with a similar extent of disease (58,289), application of data from adult studies to children is difficult. Therefore, it is not yet clear if elevated Tg levels have the same prognostic value for children, who may have a different Tg threshold for what would be considered clinically relevant or “actionable” disease.
Incorporating Tg levels into clinical care
In conjunction with neck US and other imaging procedures (see Sections D3–D5), the measurement of serum Tg is a critical component in the management of the pediatric DTC patient, both at the time of initial postoperative staging (see Table 6, Fig. 2) as well as during long-term surveillance and subsequent restaging (see Table 6, Fig. 3 and 4). At the same degree of TSH suppression, the Tg level on LT4 is thought to be the best predictor of changes in tumor mass (281,290). Therefore, monitoring of the nonstimulated Tg (in addition to neck US; see Section D3) is the ideal approach to assess for recurrence or disease progression, noting that a negative Tg on LT4 therapy may not reliably predict a negative TSH-stimulated Tg response (291–293). The use of highly sensitive Tg assays may ultimately obviate the need to perform a stimulated Tg measurement (292-297), although data in children are lacking.
Based on adult studies, a negative TSH-stimulated Tg after surgery and 131I identifies patients with a high probability of being disease-free (286,287,298–300). Therefore, an undetectable TSH-stimulated Tg in children is similarly considered to be an indicator of disease remission, although a mildly positive stimulated Tg (<10 ng/mL) in such patients should not be considered an actionable finding in the absence of other evidence for active disease. This is due to multiple factors, including our understanding that some adult patients with a TSH-stimulated Tg level >2 ng/mL but <10 ng/mL will remain free of clinical disease and will have stable or decreasing TSH-stimulated Tg levels over time (281,287,301) and the fact that patients with DTC can demonstrate a continued decline in Tg levels over many years despite receiving no additional therapy (281,301,302).
If the Tg on LT4 is detectable, there is no added value from performing a TSH-stimulated Tg because the likelihood of persistent or recurrent disease is high. In these patients, a rising Tg level indicates disease that is likely to become clinically apparent (281,283,301,303–305). In this setting, routine surveillance is recommended with imaging and treatment determined by the degree of Tg elevation and its trend over time (see Fig. 3 and Sections D3–5). However, when imaging fails to confirm or localize disease, the clinical importance of a low-level disease burden identified only by Tg testing in children is not yet clear, and there is no absolute serum Tg value above which empiric treatment is indicated (281,301). The Tg level above which additional studies and or an empiric activity of RAI therapy (see Section D5) should be considered has not been delineated in children and adolescents. A mildly positive TSH-stimulated Tg (<10 ng/mL) in such patients should not be considered an automatic, actionable finding in the absence of evidence for progressive disease.
Although repeating a TSH-stimulated Tg in patients whose Tg is undetectable on suppressive therapy but previously detectable after TSH stimulation may help to confirm the absence of disease, there is no need to repeat a TSH-stimulated Tg level in patients with an undetectable Tg on LT4 and a previously negative TSH-stimulated Tg, since these patients are likely in remission (287,298–300).
Finally, in the patient who has not been treated with 131I, the Tg level while on LT4 can still be reliable (223–225) assuming the initial surgery was done by an experienced thyroid surgeon. A TSH-stimulated Tg is of no value in this situation outside of its use in initial postoperative staging (Fig. 2).
Children with Tg autoantibodies
TgAb are detected in up to 20%–25% of patients with DTC, primarily PTC, and they interfere with Tg measurements in a qualitative, quantitative, and method-dependent manner, rendering the Tg level uninterpretable (304,306–310). Antibody interference with the most commonly used Tg immunometric assays always results in underestimation of Tg (i.e., a potentially false negative test), whereas interference with radioimmunoassay has the potential to cause either under- or overestimation of Tg, depending on the characteristics of the patient-specific TgAb and the radioimmunoassay reagents (307,310). All specimens sent for Tg measurement require concomitant TgAb testing because TgAb status can change over time and even very low TgAb concentrations can interfere (310). Similar to measuring Tg levels, the measurement of TgAb levels should be performed in the same laboratory using the same assay every time (307). Newer technologies using liquid chromatography–tandem mass spectrometry to measure Tg in TgAb-positive samples are now available (311). However, further studies are required before these methods can be broadly incorporated into clinical practice.
Because TgAb concentrations respond to changes in the levels of circulating Tg antigen, and thereby indirectly represent changes in thyroid tissue mass, the TgAb level can serve as a surrogate tumor marker for DTC (306,307). Most studies have reported that the de novo appearance, persistence, or a rising trend in TgAb concentrations in the postoperative period are significant risk factors for persistent or recurrent disease (312–316). However, it is unknown if a positive TgAb correlates with extent or invasiveness of disease or the prognosis. A decline in TgAb titers indicates a declining disease burden, but it may take a median of 3 years to clear TgAb after cure of DTC (317). A significant rise in Tg antibodies suggests disease progression that warrants further evaluation. Patients may have persistent TgAb during the first year after diagnosis and may even exhibit a rise in (or de novo appearance of) TgAb during the 6 months following 131I treatment, when there is release of Tg antigen secondary to 131I-induced damage to thyroid tissue (310,314,318). Likewise, persistence of a low TgAb concentration years after the initial surgery does not necessarily indicate the presence of disease, especially if the TgAb titers display a declining trend (315). Similar to the Tg, the trend in TgAb concentrations is more relevant for disease detection than any single TgAb concentration. Once the child becomes Tg antibody negative, the Tg level on LT4 or after TSH stimulation is considered interpretable.
■ RECOMMENDATION 23(A)
Tg serves as a sensitive tumor marker in the evaluation, treatment, and long-term follow-up of DTC in children, even in children not previously treated with 131I. TgAb levels should be simultaneously measured in all samples because the presence of TgAb will render the Tg result uninterpretable. Tg and TgAb levels should be measured using the same laboratory and assay technique. The trend in serial Tg and/or TgAb levels is much more informative in regard to determining disease status than any single measurement.
Recommendation rating: A
■ RECOMMENDATION 23(B)
An undetectable TSH-stimulated Tg (with negative TgAb) identifies patients in remission with a very high probability to remain completely free of disease during follow-up and in whom the intensity of disease surveillance and the magnitude of TSH suppression should be relaxed. Monitoring the TSH-suppressed Tg level on LT4 treatment is the recommended approach to long-term follow-up, with the trend of this value being the most reliable indicator of disease activity. Repeat TSH-stimulated Tg levels are not necessary if the TSH-suppressed Tg is detectable or if a previous TSH-stimulated Tg was undetectable.
Recommendation rating: A
■ RECOMMENDATION 23(C)
Detection of a low-level TSH-stimulated Tg (<10 ng/mL) in a patient who has undergone surgery and therapeutic 131I may indicate persistent disease. However, this value may decline over time without additional therapy. Continued follow-up with serial TSH-suppressed Tg and TgAb levels as well as radiologic imaging (neck US) are indicated in this situation.
Recommendation rating: B
■ RECOMMENDATION 23(D)
Increasing or frankly elevated levels of TSH-stimulated Tg (>10 ng/mL) warrant further evaluation to localize disease and inform the decision as to whether additional surgery and/or 131I therapy would be beneficial or whether one should pursue continued observation.
Recommendation rating: A
■ RECOMMENDATION 23(E)
The Tg level cannot be interpreted in children with positive TgAb. In this setting, the TgAb trend should be followed using the same assay. If the TgAb trend is clearly rising, then further evaluation is warranted.
Recommendation rating: A
[D3] What Is the Role of Ultrasound in the Follow-Up of PTC in Children?
Children with PTC who have residual/recurrent disease are most likely to have cervical lymph node disease (5,9,11,14,163,217,319). US, in conjunction with Tg levels, has proven highly effective in identifying and localizing regional nodal metastases in both adults and children with PTC (113,190,191,202,283,286) and appears even more sensitive than a TSH-stimulated Tg to identify disease (190,202,297). US has also proven useful for directing FNA of suspicious lesions/lymph nodes in the thyroid bed or lateral neck that can then be evaluated by routine cytology and Tg immunoassay of the needle washout, especially if cytopathology is equivocal or uninformative (187–191). Therefore, US is the most important clinical tool for identifying cervical disease and is recommended at routine intervals based upon the patient's ATA Pediatric Risk level and clinical concern for persistent or recurrent disease (see Table 6, Fig. 2 and 3).
■ RECOMMENDATION 24
Neck US is recommended in the follow-up of children with PTC (Table 6 and Fig. 3). Neck US should be performed at least 6 months after initial surgery and then at 6- to 12-month intervals for ATA Pediatric Intermediate- and High-Risk patients and at annual intervals for ATA Pediatric Low-Risk patients. Follow-up beyond 5 years should be individualized based on recurrence risk.
Recommendation rating: A
[D4] How Are Diagnostic RAI Scans Best Used in the Follow-Up of PTC in Children?
A DxWBS is usually performed as part of the postoperative staging following initial surgery in ATA Pediatric Intermediate- and High-Risk patients and can be considered in ATA Pediatric Low-Risk patients who have evidence of residual disease after short-term follow-up (see Table 6, Fig. 2 and 3, and Sections C8/C12).
Routine surveillance for persistent or recurrent disease in children with DTC has historically relied on sequential DxWBS (11,219,288). However, serial neck US and measures of serum Tg appear to be sensitive indicators of disease status in the vast majority of pediatric patients. For that reason, there is no role for serial thyroid scintigraphy in a child who has not previously been treated with 131I, unless evidence exists for persistent or recurrent disease (see Fig. 3).
For the child who has received therapeutic 131I, there may be a role for a follow-up DxWBS, typically 1–2 years following the initial treatment with 131I (Table 6). Children with known iodine-avid metastases based upon a prior posttreatment scan are the most likely to benefit from subsequent staging with a DxWBS. Ideally, the DxWBS should be performed only after a significant period of time has elapsed to assess the response from the last dose of therapeutic 131I, recognizing that clinical response can continue for years (58) (see Fig. 4 and Section D8). Finally, once a DxWBS is negative, repeating the procedure has no utility unless disease is clinically suspected.
■ RECOMMENDATION 25(A)
During the follow-up of children with PTC who are suspected to have residual disease, a DxWBS can be used to inform the decision of whether or not to use 131I and the activity of 131I to be administered (Fig. 3). A final DxWBS can be considered to confirm the absence of iodine-avid disease in children who were previously treated with 131I and who have no evidence of disease 1–2 years after initial therapy.
Recommendation rating: C
■ RECOMMENDATION 25(B)
A DxWBS should be performed in children with ATA Pediatric High-Risk disease who were previously treated with 131I or known to have iodine-avid metastatic disease based upon a previous posttreatment scan. The DxWBS should be obtained after at least 12 months of clinical follow-up, and deferred even longer in children who continue to demonstrate a clinical response to previous treatment.
Recommendation rating: B
■ RECOMMENDATION 25(C)
Once a negative DxWBS is obtained, there is no benefit from serial DxWBS to survey for disease recurrence as long as the patient otherwise remains without clinical evidence of disease.
Recommendation rating: B
[D5] What Imaging Studies Should Be Considered in the Pediatric PTC Patient Who Is Tg Positive but Who Has No Evidence of Disease on Cervical Ultrasound or DxWBS?
The child previously treated with surgery and 131I who has a serum Tg suggestive of residual/recurrent disease but no other evidence of disease presents a particularly challenging clinical situation. In this setting, one should first ensure that cervical US has been performed by an experienced radiologist and also confirm that iodinated contrast agents were not given to the patient within the 3 months prior to an RAI scan. Treatment algorithms have been proposed for adults who are “Tg-positive, scan-negative” and generally focus on anatomic imaging of the neck and chest, 18FDG-PET/CT, and additional therapeutic 131I with a posttreatment scan (1,3,320).
In children, the neck and chest are the most likely sites of persistent disease, and contrast-enhanced imaging of these areas with CT or MRI is favored when US cannot identify disease. 18FDG-PET/CT has become a commonly used tool in the evaluation of adults with persistent non–iodine-avid thyroid cancer (3,321–326) and appears to offer prognostic information that might change clinical management (327–330). However, there are extremely limited data regarding the use of 18FDG-PET/CT in children except for a case report (331), isolated pediatric subjects embedded within adult studies, and unpublished data that suggest low sensitivity of 18FDG-PET/CT to identify residual disease in children that otherwise cannot be identified via cervical US and cross-sectional imaging of the neck and chest (personal communication, SGW). Whether or not the use of 18F-FDG PET has similar prognostic value or will change disease management in children with thyroid cancer remains to be determined. Finally, empiric treatment with 131I does not appear to be effective in adults who have a negative DxWBS (332,333). Although children are more likely to have RAI-responsive disease compared with adults, empiric treatment with high-activity 131I is not generally advocated to identify disease unless there is evidence for clinical progression (e.g., a rising Tg level) and a documented clinical response to previous 131I therapy (see Fig. 3).
■ RECOMMENDATION 26(A)
For the child with a detectable TSH-suppressed Tg but a negative cervical US and DxWBS, contrast-enhanced cross-sectional imaging of the neck and chest should be considered once iodine excess has been eliminated as a cause of a false-negative DxWBS.
Recommendation rating: B
■ RECOMMENDATION 26(B)
The utility of 18FDG-PET/CT is poorly studied in pediatric DTC, and 18FDG-PET/CT cannot be routinely recommended in the care of children who have persistent evidence of DTC on follow-up.
Recommendation rating: D
■ RECOMMENDATION 26(C)
Empiric 131I therapy and a posttreatment scan are not recommended to localize disease in the child with DTC and a negative DxWBS unless there is evidence for clinical progression (e.g., a rising Tg level) and a documented clinical response to previous 131I therapy.
Recommendation rating: D
[D6] What Are the Goals and Potential Risks of TSH Suppression Therapy?
DTCs in children are well-differentiated tumors that may respond to TSH stimulation with increased growth and Tg production. For that reason, TSH suppression has been an important cornerstone of treatment, especially for high-risk groups (217,334–336). However, there are no data in children with which to compare the outcomes, risks, and benefits of various TSH suppression strategies. Some experts recommend initial TSH suppression to <0.1 mIU/L followed by relaxation to 0.5 mIU/L following remission of DTC (337). The ATA guidelines for adults stratify target TSH levels based on the risk of recurrence (1). Recognizing the paucity of data regarding TSH suppression in children with DTC, the panel has concluded that the initial TSH goal should be tied to ATA Pediatric Risk level and current disease status (Table 6). In children without evidence of disease, the TSH can be normalized to the low-normal range after an appropriate period of surveillance.
The actual risks of TSH suppression in children with DTC have been poorly studied. Extrapolating from patients with Graves' disease, the potential risks of TSH suppression include growth acceleration, advanced bone age, early onset puberty, reduced bone mineral content, poor academic performance, tachyarrhythmia, and others (338,339). It should be emphasized, however, that patients with Graves' disease generally have much greater elevations in thyroxine levels than do patients on TSH-suppressive therapy for DTC. Thus, the applicability of these data to long-term DTC management is currently unknown.
■ RECOMMENDATION 27
TSH suppression in children with DTC should be determined by ATA Pediatric Risk level and current disease status (Table 6). In children with known or suspected persistent disease, TSH suppression should be maintained. In children with no evidence of disease, the TSH can be normalized to the low-normal range after an appropriate period of surveillance.
Recommendation rating: B
[D7] What Is the Optimal Approach to the Patient with Persistent/Recurrent Cervical Disease?
The majority of residual/recurrent PTC in children will be identified in cervical lymph nodes (5,9,11,14,163,217,319), and the optimal management depends on several factors, including the location and size of disease, the previous surgical and 131I treatment history, the presence of distant metastases, and whether or not the disease is iodine-avid (see Fig. 3). Patients with cervical RAI uptake due to disease that is small (i.e., <1 cm) or that cannot be visualized via cross-sectional imaging can be considered for treatment with therapeutic 131I, which may reduce future recurrence risk but is unlikely to improve mortality (9,14,169). Although repeat surgery may also be an option, finding a small recurrence in the neck intraoperatively may be difficult. In most cases, children with small volume residual disease <1 cm can be safely observed while continuing TSH suppression. Given the overall excellent prognosis, and the low risk for clinically significant progression, the risk to benefit ratio for the treatment of small-volume disease in a child who has already undergone surgery and 131I is unfavorable.
On the other hand, in patients with structural disease >1 cm in size that is visualized by US and/or anatomic imaging (CT or MRI) and confirmed via FNA, surgical resection is preferable to 131I and can result in safe and effective long-term control of disease, especially when surgery is performed by a high-volume surgeon (340,341).
■ RECOMMENDATION 28(A)
The decision to treat or to observe structurally identifiable cervical disease should be individualized and include considerations of age, initial ATA Pediatric Risk classification, the presence of distant metastases, and prior treatment history (including complications from previous therapy), in addition to the size, extent, anatomic location, and iodine avidity of the disease (see Fig. 3).
Recommendation rating: C
■ RECOMMENDATION 28(B)
Children with macroscopic cervical disease (>1 cm in size) should be assessed by a high-volume thyroid surgeon to determine the feasibility of additional surgery.
Recommendation rating: B
■ RECOMMENDATION 28(C)
Iodine-avid cervical disease (visualized with DxWBS) could be treated with surgery or 131I depending on individual patient risks and the presence or absence of distant metastases. Surgery would be favored for disease localized to the neck, especially if located in a lymph node compartment not previously operated upon.
Recommendation rating: B
■ RECOMMENDATION 28(D)
If repeat surgery is performed, postoperative restaging can be utilized to determine whether additional 131I treatment is warranted, especially in the patient who has not received previous therapeutic 131I.
Recommendation rating: C
[D8] How Should Children with Pulmonary Metastases Be Managed?
The majority of children with pulmonary metastases have micronodular disease that typically demonstrates excellent RAI uptake. Because of this, distant metastases in children are more amenable and responsive to 131I therapy compared with adults. Serial 131I treatments can result in remission in many, but not all, children with pulmonary metastases from PTC, the vast majority of whom will demonstrate stable metastatic disease and low disease-specific mortality (10,57,58,162,176,179,227,289,319,342–344). The optimal frequency of 131I treatment has not been determined. The maximal clinical and biochemical response from an administered activity of 131I may not be reached for up to 15–18 months (302), and recent studies have also demonstrated a continuous improvement in serum Tg levels for years following discontinuation of 131I therapy in children with pulmonary metastases (58), all of which suggests that the effects of therapy can be seen well beyond the first years after treatment. Because children with pulmonary metastases have historically been treated aggressively with repeated activities of 131I, it remains unknown how these pediatric patients would respond to the less-aggressive use of 131I. Given that a majority of children with pulmonary metastases will not have a complete response to therapy and because it may take years to see the full response of 131I, an undetectable Tg level should no longer be the sole goal of treatment of children with pulmonary metastases. Furthermore, longer intervals between 131I therapy would seem prudent in the child who does not demonstrate progressive disease.
For patients with persistent pulmonary metastases who have already received treatment with high-activity 131I, the decision to re-treat should be individualized (see Fig. 4). Because of our improved understanding regarding prognosis and duration of response in children with pulmonary metastases, and to minimize the long-term risks associated with high cumulative activities of 131I (see Section C16), it is logical to monitor the TSH-suppressed Tg and imaging studies in these children, deferring repeat evaluation and treatment with RAI until the full response to previous 131I is demonstrated. In the rare event of disease progression, further evaluation and treatment would be warranted, as long as it has been >12 months from the previous activity of 131I (see Fig. 4). For serologic progression, waiting at least 12 months would better establish a trend to ensure that the rise in the Tg or TgAb levels is not spurious or due to previous 131I-induced tumor destruction. Furthermore, a longer interval between treatments may minimize the risk of late effects of 131I (see Section C16). In all cases, therapeutic 131I should be considered only if the patient is known or presumed to have RAI-responsive disease and has not already received high cumulative activities of 131I. If the child did not have previous RAI uptake on a posttreatment scan or if their disease continued to progress despite high-activity 131I, further 131I therapy is unlikely to be helpful and should not be given. In these cases, continued observation and TSH suppression are indicated, with alternative therapies considered if progression of iodine-refractory disease becomes clinically significant (Section D10).
As children with pulmonary metastases may have diffuse RAI uptake in the lungs, there is a real concern about treatment-induced pulmonary fibrosis (57,258,345–348). In these cases, administering lower 131I activities and employing dosimetry should be considered to limit radiation exposure to the nontarget normal lung parenchyma (244–246,347,349) (Section C14). The utility and optimal intervals at which to perform pulmonary function testing in children with lung metastases have not been studied, but many experts recommend that pulmonary function testing be done intermittently in children with pulmonary metastases, especially if multiple 131I treatments are planned.
■ RECOMMENDATION 29(A)
Children with RAI-avid pulmonary metastases visualized with a DxWBS are good candidates for 131I therapy.
Recommendation rating: A
■ RECOMMENDATION 29(B)
After a therapeutic activity of 131I, the TSH-suppressed Tg level and imaging studies should be monitored until the full clinical and biochemical (Tg) response is reached.
Recommendation rating: B
■ RECOMMENDATION 29(C)
If the full clinical and biochemical (Tg) response suggests persistent disease or if there is documented disease progression >12 months after 131I therapy, further evaluation with a DxWBS and a TSH-stimulated Tg is indicated.
Recommendation rating: B
■ RECOMMENDATION 29(D)
Re-treatment of RAI-avid pulmonary metastases should be considered in children who have demonstrated progression of disease and a previous response to 131I, with each treatment carefully individualized based on the child's unique clinical course, side-effect profile, risk tolerance, and cumulative administered 131I activity. Treatment with 131I should be performed by experts with experience in managing children with pulmonary metastases.
Recommendation rating: B
■ RECOMMENDATION 29(E)
Re-treatment of pulmonary metastases with 131I is not recommended in children who do not have uptake on a DxWBS and who have not demonstrated a previous response to 131I.
Recommendation rating: E
■ RECOMMENDATION 29(F)
Pulmonary function testing should be considered in all children with diffuse pulmonary metastases, especially if multiple 131I treatments are planned.
Recommendation rating: C
[D9] How Does One Approach the Child with an Incidental PTC Identified After Surgery for Another Thyroid Condition?
Small foci of PTC may be incidentally discovered on histological examination of thyroid tissue resected for other benign diseases such as Graves' disease, autonomous nodule(s), or multinodular goiter. No consensus exists regarding the benefit of completion thyroidectomy (assuming lobectomy was initially performed) or 131I therapy for children with incidental PTC. However, these children should undergo neck US, if not already performed, and be managed similar to other children with ATA Pediatric Low-Risk PTC (Table 6).
■ RECOMMENDATION 30
Children with incidental PTC should be managed similarly to other children with ATA Pediatric Low-Risk disease. Neck US is recommended to detect contralateral disease or disease in the regional lymph nodes. Completion thyroidectomy is not required in those children who had less than a TT unless there is US evidence and cytologic confirmation of contralateral thyroid disease or malignant lymphadenopathy.
Recommendation rating: B
[D10] What Are the Optimal Approaches to the Pediatric Patient Who Develops Progressive Thyroid Cancer That No Longer Concentrates or Responds to 131I?
Very rarely, children with thyroid cancer may develop progressive symptomatic and/or life-threatening disease that is not amenable to further surgery or 131I. In such cases, systemic therapy should be considered. Clinical trials would be preferred, but there has not yet been a clinical trial developed for children with 131I-refractory DTC. Some drugs with potential efficacy may be available through phase 1 pediatric studies. Doxorubicin remains the only United States Food and Drug Administration (FDA)-approved cytotoxic chemotherapy for this indication and has been used either as a single agent or in combination with cisplatin or interferon-α (39,350,351), but it is generally ineffective in treating advanced DTC.
Molecularly targeted therapies using oral small molecule kinase inhibitors have brought newer options to the management of 131I-refractory thyroid cancer in adults (39,352). The pediatric experience has been limited to published case reports and anecdotal clinical experience, primarily with sorafenib (353,354), which is FDA-approved for the treatment of advanced iodine-refractory DTC in adults based upon the results of a phase III trial (355). [Subsequent to the completion of these guidelines, lenvatinib was also approved by the FDA based upon a pivotal phase III clinical trial in adults (356).] Although more study is required regarding the use of these agents in children, particularly with respect to dosing and toxicity, the use of molecularly targeted therapies may be contemplated in the rare situation in which a child warrants systemic treatment. However, it is difficult to define iodine-refractory disease in pediatric DTC, and iodine-refractory DTC can remain stable over years of follow-up. For that reason, all children being considered for anti-neoplastic therapy should be referred to centers familiar with the use of these novel therapeutic agents in thyroid cancer. In all cases, a systematic approach to care and toxicity evaluation should be undertaken (357).
■ RECOMMENDATION 31
Most children with asymptomatic and nonprogressive 131I-refractory disease can be safely monitored while continuing TSH suppression. Systemic treatment for advanced thyroid cancer in children remains unstudied and at this time should be considered the purview of specialized centers for the treatment of children with thyroid cancer. Consultation with experts in this area should be invited prior to initiation of treatment. In exceptional cases in which systemic treatment is contemplated, clinical trials are preferred. If unavailable, the use of oral kinase inhibitors may be considered.
Recommendation rating: C
[E1] Follicular Thyroid Cancer
Pediatric FTC is a rare and poorly studied malignancy with an age-adjusted annual incidence of 0.5 cases per million population (8). FTC currently represents 10% or less of thyroid cancer cases diagnosed in children or young adults (8,50,358–360), and the prevalence of true FTC appears to be decreasing over time (361). FTC is most commonly diagnosed in adolescents, and there is less of a female to male preponderance compared with PTC (9,11,50,51,226). Iodine deficiency is the one clear risk factor for the development of FTC, and iodine-deficient countries have a higher prevalence of FTC compared with PTC (226,358,362,363). Unlike for PTC, the role of ionizing radiation in the pathogenesis of FTC is much less clear (20,364).
The major histopathologic variants of FTC are the oncocytic (Hürthle cell) and clear cell variants. Poorly differentiated thyroid carcinomas (e.g., insular carcinomas) can arise from a pre-existing FTC and are defined by the WHO as follicular cell malignancies with limited evidence of follicular cell differentiation (25). Such tumors are exceedingly rare in the pediatric population (365,366).
Although mutations in RAS and the PAX8/PPARγ rearrangement have been implicated in adult FTC (130,367), the somatic genetic events that contribute to the pathogenesis of pediatric FTC remain largely unstudied. FTC can be a component of the PTEN hamartoma tumor syndrome (including Cowden syndrome) that results from germline mutations in PTEN (see Table 4) (91,92,197,368–370). Therefore, there should be a high index of suspicion for an underlying PTEN mutation in children with FTC, particularly in those with macrocephaly, penile freckling, or a suggestive family history (92,324,369,371). FTC may also develop as part of other genetic syndromes (see Section B3 and Table 4).
FTC is typically an encapsulated lesion and the diagnosis is based on the pathologic identification of capsular and/or vascular invasion in the resected tumor (358,372,373). The diagnosis can only be secured after surgical resection and a thorough examination of the tumor capsule as it interfaces with the thyroid. FNA is not sufficient for making the diagnosis of FTC, which usually has an indeterminate result, such as “atypia of undetermined significance,” “follicular lesion of undetermined significance,” “follicular neoplasm,” or “suspicious for follicular neoplasm” (see Section B4) (121,374,375).
The clinical behavior of FTC in children is distinct from PTC. Pediatric FTC may be less aggressive than PTC and is generally associated with less advanced disease, fewer distant metastases, and a lower rate of recurrence (9,11,50,167,376). Except for the aggressive variants, FTC is typically a unifocal tumor that rarely spreads to regional lymph nodes (11,25,50,51,358,372,376–379) and may have autonomous function (380–382). However, unlike PTC, FTC is prone to early hematogenous metastases, which occurs even in the absence of cervical node involvement (383,384). Despite that, conventional FTC has an excellent prognosis when diagnosed during childhood, and long-term survival is the norm (8,385,386).
Depending on the extent of invasion, FTC is currently subdivided into two major groups: minimally invasive and widely invasive FTC (367,373). Tumors with microscopic capsular invasion alone and/or very limited vascular invasion are typically classified as minimally invasive carcinomas, whereas grossly invasive neoplasms that show widespread infiltration into blood vessels and/or adjacent thyroid tissue and often lack complete tumor encapsulation are deemed widely invasive FTC.
Minimally invasive FTC has the lowest risk for recurrence and/or metastases, whereas widely invasive FTC is associated with significant morbidity and mortality in adults (358,367,372,373,378,383,387–392). Vascular invasion appears to be the most important clinical prognostic indicator, and any degree of vascular invasion, especially if more than three blood vessels are involved, may portend more advanced disease and a worse prognosis (372,373,387–390,393). However, not all studies support the negative impact of vascular invasion (383,394). Furthermore, size of the primary tumor appears to be an important factor, with metastases less likely to occur in smaller cancers (377,383,384,391,393).
In clinical practice, the initial evaluation and treatment of FTC in children is generally the same as for PTC (200,395). Surgery by a high-volume thyroid surgeon is the definitive therapy, and at a minimum the child with an FNA that demonstrates an indeterminate lesion should undergo an ipsilateral thyroid lobectomy and isthmusectomy (see Section B4 and Fig. 1). Intraoperative frozen section can be considered, primarily to assess for PTC, but frozen section cannot reliably distinguish FTC from benign disease and is not routinely recommended (396). With a minimally invasive FTC, lobectomy alone may be sufficient treatment (378,392). However, if more than three vascular invasions are identified or if the tumor is >4 cm, completion thyroidectomy is recommended because of the higher risk of distant metastasis (373). In children who have had a TT, postoperative staging (Fig. 2) can help to identify the children with FTC who may benefit from 131I treatment (200). Further studies are required to understand the benefit of routine 131I treatment in children with no evidence for iodine-avid metastases and a stimulated Tg ≤10 ng/mL.
The follow-up of children with FTC is similar to PTC and will include serial monitoring of serum Tg levels and TSH suppression (see Table 6). One notable difference is that routine neck US is typically of lesser importance for the pediatric patient with conventional FTC who has had a TT, especially when there is no evidence of disease based upon the Tg data. However, intermittent ultrasonography in children who have had only lobectomy may be valuable.
Pediatric FTC is a rare malignancy. Because of the paucity of data regarding FTC in children, strong recommendations regarding therapy cannot be made and further studies are required to better understand the long-term outcomes and to risk-stratify children who would benefit from more extensive thyroid surgery and 131I therapy.
■ RECOMMENDATION 32(A)
Patients with clear evidence of vascular invasion (more than three involved blood vessels), known distant metastasis, and/or tumor size >4 cm should be treated with TT and staged postoperatively with RAI.
Recommendation rating: C
■ RECOMMENDATION 32(B)
Minimally invasive FTC <4 cm in size and with no or minimal vascular invasion (three or fewer involved blood vessels) should be treated on a case-by-case basis, but lobectomy alone rather than TT with 131I therapy may be sufficient.
Recommendation rating: C
■ RECOMMENDATION 32(C)
In all children diagnosed with FTC, consideration should be given to genetic counseling and genetic testing for germline PTEN mutations particularly in the child with macrocephaly or with a family history suggestive of the PTEN hamartoma tumor syndrome.
Recommendation rating: C
[F1] What are the Unique Issues that may Affect Children Diagnosed with DTC?
Long-term psychosocial issues have been reported in survivors of other childhood cancers and appear to be more pronounced in the unemployed, the poorly educated, and those with poor financial resources (397). Parents perceive children with cancer to be more vulnerable than their peers, and this may lead to overprotection and a reduction in the child's quality of life (398), a measure that may not be directly related to the severity of the cancer prognosis (399). Furthermore, this perception of vulnerability has been shown to persist for at least 5–10 years after completion of therapy (400). One small study in children and adolescents treated for thyroid cancer demonstrated no difference in quality of life or anxiety levels compared to children treated for hypothyroidism or normative controls (401); however, this was a cross-sectional study and 11 of 16 patients were in remission at the time of completing the survey. Further exploration of the psychosocial impact of thyroid cancer on the patient and his or her parents and siblings is required (402). Based on the data from other forms of childhood cancer, similar parental perceptions of vulnerability and other psychosocial issues may occur in children with DTC as they age. Providers should be aware of this possibility and remain alert to signs of psychosocial distress.
As with any chronic illness, adherence to life-long LT4 therapy is an issue, and it is not uncommon for children to have elevated levels of TSH when not required for evaluation or treatment with RAI (403). Therefore, medication adherence can be a challenge and frequent assessments of thyroid hormone levels along with education about the benefit of TSH suppression in the long-term management of DTC are important. Motivational interviewing may be a nonjudgmental means by which to improve compliance (404,405). For patients who received 131I therapy, health care providers should also continue to be aware of the potential for second malignancies and chronic adverse effects from 131I treatment (see Section C16).
■ RECOMMENDATION 33
Children with DTC may experience adverse psychosocial effects and be nonadherent with LT4 therapy. Attention to these possibilities and supportive counseling as required are important adjuncts in the long-term follow-up of children with DTC. Future studies on the impact of a DTC diagnosis and treatment on quality of life in children are required.
Recommendation rating: C
[G1] How Long Should a Child with PTC be Monitored?
Overall recurrence rates for children with PTC are approximately 30%. In some studies, more than half of recurrences were seen in the first 7 years after treatment (11), while others found equal recurrence rates in the first and second decades after surgery (169). Delayed recurrence as long as 20–40 years after diagnosis has also been reported (5,217). From these data, it would appear that children with PTC should be followed for several decades to detect all late recurrences. However, Tg levels were not reported for patients in these earlier studies, and it remains unclear if these recurrence data apply to children with an undetectable stimulated Tg. Until additional long-term data are available, we suggest that all children with PTC should be followed prospectively but with reduced intensity over time, especially for those with undetectable TSH-stimulated Tg (see Table 6).
■ RECOMMENDATION 34
Recurrence of DTC in children has been reported as long as 40 years after initial therapy. For that reason, children with DTC should be followed for life, albeit with decreasing intensity for those with no evidence for disease.
Recommendations rating: B
[G2] What are the Areas for Future Research?
The treatment of children with DTC is evolving. We have moved from an era of intensive therapy in which all children received TT and 131I to an era of personalized therapy in which treatment is individualized based on pre- and postoperative staging and continuous risk stratification. Although the current recommendations have been made based on the best available data and clinical experience, such evolution in care generates uncertainty in providers, parents, and patients. The greatest uncertainty surrounds the proper use of 131I, the interpretation of Tg and TgAb levels, the role of prospective US monitoring in presymptomatic children at risk for thyroid neoplasia, the use of novel targeted therapies for advanced disease that is unresponsive to 131I, and the long-term psychosocial impacts of this disease on children and their families. These areas require well-designed long-term, multicenter studies that will be difficult to perform because of the rarity of pediatric DTC and the prolonged follow-up required to reach meaningful end-points. Further research should be facilitated by ensuring that children with DTC are treated when possible at centers with multidisciplinary interest and expertise in this disease.
Acknowledgments
The task force would like to thank Ms. Shirlyn Barger, ATA assistant to the task force, for her diligence, ever-pleasant nature, and incredible support during the guidelines development process. We acknowledge Martha Zeigler, MD (ATA board liaison) for her helpful contributions to our discussions and all of our colleagues who have indirectly contributed to these guidelines via informal discussions and patient care. Finally, we acknowledge and thank our patients and families who have impassioned us to develop these guidelines and who continue to inspire and teach us.
Endorsements
The final document was officially endorsed by the British Nuclear Medicine Society; Canadian Society of Otolaryngology-Head and Neck Surgery; European Association for Cranio-Maxillo-Facial Surgery; European Association of Nuclear Medicine; International Association of Endocrine Surgeons; International Federation of Head and Neck Oncologic Societies; Latin American Thyroid Society; The Endocrine Society; The Endocrine Society of Australia.
Disclaimer
It is our goal in formulating these inaugural guidelines, and the ATA's goal in providing support for the development of these guidelines, that they assist in the clinical care of patients and improve the standard of care of children with thyroid neoplasia. These guidelines include what we believe to be contemporary, rational, and optimal medical practice, but they are not intended to be inclusive of all proper approaches to care nor exclusive of other treatments that are reasonably directed at the same outcomes. We developed these guidelines based on the evidence available in the recent literature and the expert opinion of the task force. It is not the intent of these guidelines to replace individual decision making, the wishes of the patient or family, or clinical judgment.
Author Disclosure Statement
These guidelines were funded by the ATA without support from any commercial sources. The patient organization, ThyCa: Thyroid Cancer Survivors' Association, Inc., also contributed an unrestricted educational grant toward the development of the pediatric thyroid cancer guidelines.
AJB was a consultant for Akrimax; SB received research support from IBSA Institute Biochimique; GLF received research support from Grifols, Novo Nordisk, and Juvenile Diabetes Research Foundation; MR was a speaker for Pfizer and Novo Nordisk and served as a consultant and received research support from Eli Lilly; SGW was a consultant for Novo Nordisk. M.L. was a consultant for AstraZeneca, Bayer Healthcare, Genzyme, and Sobi and has received speaker honoraria and research support from Genzyme, Henning, and Merck. AJB, GLF, and SGW also served as advisors to ThyCa. PA, JMC, CAD, JH, IDH, ML, MTP, GBT, and SY reported no financial interests, arrangements, or affiliations with the manufacturer of any products or devices.
References
- 1.Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM. 2009. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19:1167–1214 [DOI] [PubMed] [Google Scholar]
- 2.Cobin RH, Gharib H, Bergman DA, Clark OH, Cooper DS, Daniels GH, Dickey RA, Duick DS, Garber JR, Hay ID, Kukora JS, Lando HM, Schorr AB, Zeiger MA; Thyroid Carcinoma Task Force 2001. AACE/AAES medical/surgical guidelines for clinical practice: management of thyroid carcinoma. American Association of Clinical Endocrinologists. American College of Endocrinology. Endocr Pract 7:202–220 [PubMed] [Google Scholar]
- 3.The NCCN Clinical Practice Guidelines in Oncology, Thyroid Carcinoma (Version 2.2013). Available at www.nccn.org/professionals/physician_gls/f_guidelines.asp#site (accessed October3, 2013)
- 4.British Thyroid Association, Royal College of Physicians 2007. Guidelines for the Management of Thyroid Cancer. Second edition. Royal College of Physicians, London [Google Scholar]
- 5.Hay ID, Gonzalez-Losada T, Reinalda MS, Honetschlager JA, Richards ML, Thompson GB. 2010. Long-term outcome in 215 children and adolescents with papillary thyroid cancer treated during 1940 through 2008. World J Surg 34:1192–1202 [DOI] [PubMed] [Google Scholar]
- 6.Brown AP, Chen J, Hitchcock YJ, Szabo A, Shrieve DC, Tward JD. 2008. The risk of second primary malignancies up to three decades after the treatment of differentiated thyroid cancer. J Clin Endocrinol Metab 93:504–515 [DOI] [PubMed] [Google Scholar]
- 7.Rubino C, de Vathaire F, Dottorini ME, Hall P, Schvartz C, Couette JE, Dondon MG, Abbas MT, Langlois C, Schlumberger M. 2003. Second primary malignancies in thyroid cancer patients. Br J Cancer 89:1638–1644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hogan AR, Zhuge Y, Perez EA, Koniaris LG, Lew JI, Sola JE. 2009. Pediatric thyroid carcinoma: incidence and outcomes in 1753 patients. J Surg Res 156:167–172 [DOI] [PubMed] [Google Scholar]
- 9.Chow SM, Law SC, Mendenhall WM, Au SK, Yau S, Mang O, Lau WH. 2004. Differentiated thyroid carcinoma in childhood and adolescence-clinical course and role of radioiodine. Pediatr Blood Cancer 42:176–183 [DOI] [PubMed] [Google Scholar]
- 10.Demidchik YE, Demidchik EP, Reiners C, Biko J, Mine M, Saenko VA, Yamashita S. 2006. Comprehensive clinical assessment of 740 cases of surgically treated thyroid cancer in children of Belarus. Ann Surg 243:525–532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Welch Dinauer CA, Tuttle RM, Robie DK, McClellan DR, Svec RL, Adair C, Francis GL. 1998. Clinical features associated with metastasis and recurrence of differentiated thyroid cancer in children, adolescents and young adults. Clin Endocrinol 49:619–628 [DOI] [PubMed] [Google Scholar]
- 12.Harness JK, Thompson NW, McLeod MK, Pasieka JL, Fukuuchi A. 1992. Differentiated thyroid carcinoma in children and adolescents. World J Surg 16:547–553; discussion 553–544. [DOI] [PubMed] [Google Scholar]
- 13.Newman KD, Black T, Heller G, Azizkhan RG, Holcomb GW, 3rd, Sklar C, Vlamis V, Haase GM, La Quaglia MP. 1998. Differentiated thyroid cancer: determinants of disease progression in patients <21 years of age at diagnosis: a report from the Surgical Discipline Committee of the Children's Cancer Group. Ann Surg 227:533–541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Handkiewicz-Junak D, Wloch J, Roskosz J, Krajewska J, Kropinska A, Pomorski L, Kukulska A, Prokurat A, Wygoda Z, Jarzab B. 2007. Total thyroidectomy and adjuvant radioiodine treatment independently decrease locoregional recurrence risk in childhood and adolescent differentiated thyroid cancer. J Nucl Med 48:879–888 [DOI] [PubMed] [Google Scholar]
- 15.Popovtzer A, Shpitzer T, Bahar G, Feinmesser R, Segal K. 2006. Thyroid cancer in children: management and outcome experience of a referral center. Otolaryngol Head Neck Surg 135:581–584 [DOI] [PubMed] [Google Scholar]
- 16.Howlader N, Noone AM, Krapcho M, Garshell J, Neyman N, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Cho H, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA. (eds) SEER Cancer Statistics Review, 1975–2010. Available at http://seer.cancer.gov/csr/1975_2010/ (updated June 14, 2013; accessed November18, 2013)
- 17.Vergamini LB, Frazier AL, Abrantes FL, Ribeiro KB, Rodriguez-Galindo C. 2014. Increase in the incidence of differentiated thyroid carcinoma in children, adolescents, and young adults: a population-based study. J Pediatr 164:1481–1485 [DOI] [PubMed] [Google Scholar]
- 18.Wu XC, Chen VW, Steele B, Roffers S, Klotz JB, Correa CN, Carozza SE. 2003. Cancer incidence in adolescents and young adults in the United States, 1992–1997. J Adolesc Health 32:405–415 [DOI] [PubMed] [Google Scholar]
- 19.Waguespack S, Wells S, Ross J, Bleyer A. 2006. Thyroid cancer. In: Bleyer A, O'Leary M, Barr R, Ries L. (eds) Cancer Epidemiology in Older Adolescents and Young Adults 15 to 29 Years of Age, Including SEER Incidence and Survival 1975–2000. Vol NIH Pub. No. 06-5767. National Cancer Institute, Bethesda, MD, pp 143–154 [Google Scholar]
- 20.Demidchik YE, Saenko VA, Yamashita S. 2007. Childhood thyroid cancer in Belarus, Russia, and Ukraine after Chernobyl and at present. Arq Bras Endocrinol Metabol 51:748–762 [DOI] [PubMed] [Google Scholar]
- 21.Spoudeas HA. 2005. Paediatric Endocrine Tumours: A Multi-Disciplinary Consensus Statement of Best Practice from a Working Group Convened Under the Auspices of the The British Society of Paediatric Endocrinology & Diabetes and the United Kingdom Children's Cancer Study Group. Novo Nordisk Ltd, West Sussex, United Kingdom [Google Scholar]
- 22.Feinmesser R, Lubin E, Segal K, Noyek A. 1997. Carcinoma of the thyroid in children—a review. J Pediatr Endocrinol Metab 10:561–568 [DOI] [PubMed] [Google Scholar]
- 23.Frankenthaler RA, Sellin RV, Cangir A, Goepfert H. 1990. Lymph node metastasis from papillary-follicular thyroid carcinoma in young patients. Am J Surg 160:341–343 [DOI] [PubMed] [Google Scholar]
- 24.Vassilopoulou-Sellin R, Klein MJ, Smith TH, Samaan NA, Frankenthaler RA, Goepfert H, Cangir A, Haynie TP. 1993. Pulmonary metastases in children and young adults with differentiated thyroid cancer. Cancer 71:1348–1352 [DOI] [PubMed] [Google Scholar]
- 25.DeLellis RA, Lloyd RV, Heitz PU, Eng C. 2004. Pathology and Genetics of Tumours of Endocrine Organs World Health Organization Classification of Tumours, Volume 8 IARC Press, Lyon, France [Google Scholar]
- 26.Monaco SE, Pantanowitz L, Khalbuss WE, Benkovich VA, Ozolek J, Nikiforova MN, Simons JP, Nikiforov YE. 2012. Cytomorphological and molecular genetic findings in pediatric thyroid fine-needle aspiration. Cancer Cytopathol 120:342–350 [DOI] [PubMed] [Google Scholar]
- 27.Gupta A, Ly S, Castroneves LA, Frates MC, Benson CB, Feldman HA, Wassner AJ, Smith JR, Marqusee E, Alexander EK, Barletta J, Doubilet PM, Peters HE, Webb S, Modi BP, Paltiel HJ, Kozakewich H, Cibas ES, Moore FD, Jr, Shamberger RC, Larsen PR, Huang SA. 2013. A standardized assessment of thyroid nodules in children confirms higher cancer prevalence than in adults. J Clin Endocrinol Metab 98:3238–3245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Halac I, Zimmerman D. 2005. Thyroid nodules and cancers in children. Endocrinol Metab Clin North Am 34:725–744, x. [DOI] [PubMed] [Google Scholar]
- 29.Koo JS, Hong S, Park CS. 2009. Diffuse sclerosing variant is a major subtype of papillary thyroid carcinoma in the young. Thyroid 19:1225–1231 [DOI] [PubMed] [Google Scholar]
- 30.Harach HR, Williams ED. 1995. Childhood thyroid cancer in England and Wales. Br J Cancer 72:777–783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zimmerman D, Hay ID, Gough IR, Goellner JR, Ryan JJ, Grant CS, McConahey WM. 1988. Papillary thyroid carcinoma in children and adults: long-term follow-up of 1039 patients conservatively treated at one institution during three decades. Surgery 104:1157–1166 [PubMed] [Google Scholar]
- 32.Tucker MA, Jones PH, Boice JD, Jr, Robison LL, Stone BJ, Stovall M, Jenkin RD, Lubin JH, Baum ES, Siegel SE, et al. . 1991. Therapeutic radiation at a young age is linked to secondary thyroid cancer. The Late Effects Study Group. Cancer Res 51:2885–2888 [PubMed] [Google Scholar]
- 33.Sinnott B, Ron E, Schneider AB. 2010. Exposing the thyroid to radiation: a review of its current extent, risks, and implications. Endocr Rev 31:756–773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yamashita S. 2014. Tenth Warren K. Sinclair keynote address-the Fukushima nuclear power plant accident and comprehensive health risk management. Health Physics 106:166–180 [DOI] [PubMed] [Google Scholar]
- 35.Schlumberger M, Pacini F. 2003. Thyroid Tumors. Vol. Nucleon, Paris [Google Scholar]
- 36.Faggiano A, Coulot J, Bellon N, Talbot M, Caillou B, Ricard M, Bidart JM, Schlumberger M. 2004. Age-dependent variation of follicular size and expression of iodine transporters in human thyroid tissue. J Nucl Med 45:232–237 [PubMed] [Google Scholar]
- 37.Naing S, Collins BJ, Schneider AB. 2009. Clinical behavior of radiation-induced thyroid cancer: factors related to recurrence. Thyroid 19:479–485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sobrinho-Simoes M, Maximo V, Rocha AS, Trovisco V, Castro P, Preto A, Lima J, Soares P. 2008. Intragenic mutations in thyroid cancer. Endocrinol Metab Clin North Am 37:333–362, viii. [DOI] [PubMed] [Google Scholar]
- 39.Woyach J, Shah M. 2009. New therapeutic advances in the management of progressive thyroid cancer. Endocr Relat Cancer 16:715–731 [DOI] [PubMed] [Google Scholar]
- 40.Yamashita S, Saenko V. 2007. Mechanisms of disease: molecular genetics of childhood thyroid cancers. Nat Clin Pract Endocrinol Metab 3:422–429 [DOI] [PubMed] [Google Scholar]
- 41.Kebebew E. 2008. Hereditary non-medullary thyroid cancer. World J Surg 32:678–682 [DOI] [PubMed] [Google Scholar]
- 42.Alsanea O, Wada N, Ain K, Wong M, Taylor K, Ituarte PH, Treseler PA, Weier HU, Freimer N, Siperstein AE, Duh QY, Takami H, Clark OH. 2000. Is familial non-medullary thyroid carcinoma more aggressive than sporadic thyroid cancer? A multicenter series. Surgery 128:1043–1051 [DOI] [PubMed] [Google Scholar]
- 43.Samuel AM, Sharma SM. 1991. Differentiated thyroid carcinomas in children and adolescents. Cancer 67:2186–2190 [DOI] [PubMed] [Google Scholar]
- 44.Machens A, Lorenz K, Nguyen Thanh P, Brauckhoff M, Dralle H. 2010. Papillary thyroid cancer in children and adolescents does not differ in growth pattern and metastatic behavior. J Pediatr 157:648–652 [DOI] [PubMed] [Google Scholar]
- 45.Wada N, Sugino K, Mimura T, Nagahama M, Kitagawa W, Shibuya H, Ohkuwa K, Nakayama H, Hirakawa S, Rino Y, Masuda M, Ito K. 2009. Pediatric differentiated thyroid carcinoma in stage I: risk factor analysis for disease free survival. BMC Cancer 9:306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Savio R, Gosnell J, Palazzo FF, Sywak M, Agarwal G, Cowell C, Shun A, Robinson B, Delbridge LW. 2005. The role of a more extensive surgical approach in the initial multimodality management of papillary thyroid cancer in children. J Pediatr Surg 40:1696–1700 [DOI] [PubMed] [Google Scholar]
- 47.Jarzab B, Handkiewicz Junak D, Wloch J, Kalemba B, Roskosz J, Kukulska A, Puch Z. 2000. Multivariate analysis of prognostic factors for differentiated thyroid carcinoma in children. Eur J Nucl Med 27:833–841 [DOI] [PubMed] [Google Scholar]
- 48.Schlumberger M, De Vathaire F, Travagli JP, Vassal G, Lemerle J, Parmentier C, Tubiana M. 1987. Differentiated thyroid carcinoma in childhood: long term follow-up of 72 patients. J Clin Endocrinol Metab 65:1088–1094 [DOI] [PubMed] [Google Scholar]
- 49.Bal CS, Kumar A, Chandra P, Dwivedi SN, Mukhopadhyaya S. 2004. Is chest x-ray or high-resolution computed tomography scan of the chest sufficient investigation to detect pulmonary metastasis in pediatric differentiated thyroid cancer? Thyroid 14:217–225 [DOI] [PubMed] [Google Scholar]
- 50.O'Gorman CS, Hamilton J, Rachmiel M, Gupta A, Ngan BY, Daneman D. 2010. Thyroid cancer in childhood: a retrospective review of childhood course. Thyroid 20:375–380 [DOI] [PubMed] [Google Scholar]
- 51.Giuffrida D, Scollo C, Pellegriti G, Lavenia G, Iurato MP, Pezzin V, Belfiore A. 2002. Differentiated thyroid cancer in children and adolescents. J Endocrinol Invest 25:18–24 [DOI] [PubMed] [Google Scholar]
- 52.Grigsby PW, Gal-or A, Michalski JM, Doherty GM. 2002. Childhood and adolescent thyroid carcinoma. Cancer 95:724–729 [DOI] [PubMed] [Google Scholar]
- 53.Wada N, Sugino K, Mimura T, Nagahama M, Kitagawa W, Shibuya H, Ohkuwa K, Nakayama H, Hirakawa S, Yukawa N, Rino Y, Masuda M, Ito K. 2009. Treatment strategy of papillary thyroid carcinoma in children and adolescents: clinical significance of the initial nodal manifestation. Ann Surg Oncol 16:3442–3449 [DOI] [PubMed] [Google Scholar]
- 54.U.S. Preventive Services Task Force Ratings: Grade Definitions. Available at www.uspreventiveservicestaskforce.org/page/name/us-preventive-services-task-force-ratings (accessed June3, 2015)
- 55.Niedziela M. 2006. Pathogenesis, diagnosis and management of thyroid nodules in children. Endocr Relat Cancer 13:427–453 [DOI] [PubMed] [Google Scholar]
- 56.Gharib H, Papini E, Valcavi R, Baskin HJ, Crescenzi A, Dottorini ME, Duick DS, Guglielmi R, Hamilton CR, Jr, Zeiger MA, Zini M. 2006. American Association of Clinical Endocrinologists and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules. Endocr Pract 12:63–102 [DOI] [PubMed] [Google Scholar]
- 57.Pawelczak M, David R, Franklin B, Kessler M, Lam L, Shah B. 2010. Outcomes of children and adolescents with well-differentiated thyroid carcinoma and pulmonary metastases following 131I treatment: a systematic review. Thyroid 20:1095–1101 [DOI] [PubMed] [Google Scholar]
- 58.Biko J, Reiners C, Kreissl MC, Verburg FA, Demidchik Y, Drozd V. 2011. Favourable course of disease after incomplete remission on (131)I therapy in children with pulmonary metastases of papillary thyroid carcinoma: 10 years follow-up. Eur J Nucl Med Mol Imaging 38:651–655 [DOI] [PubMed] [Google Scholar]
- 59.Penko K, Livezey J, Fenton C, Patel A, Nicholson D, Flora M, Oakley K, Tuttle RM, Francis G. 2005. BRAF mutations are uncommon in papillary thyroid cancer of young patients. Thyroid 15:320–325 [DOI] [PubMed] [Google Scholar]
- 60.Mitsutake N, Knauf JA, Mitsutake S, Mesa C, Jr, Zhang L, Fagin JA. 2005. Conditional BRAFV600E expression induces DNA synthesis, apoptosis, dedifferentiation, and chromosomal instability in thyroid PCCL3 cells. Cancer Res 65:2465–2473 [DOI] [PubMed] [Google Scholar]
- 61.Saavedra HI, Knauf JA, Shirokawa JM, Wang J, Ouyang B, Elisei R, Stambrook PJ, Fagin JA. 2000. The RAS oncogene induces genomic instability in thyroid PCCL3 cells via the MAPK pathway. Oncogene 19:3948–3954 [DOI] [PubMed] [Google Scholar]
- 62.Fenton CL, Lukes Y, Nicholson D, Dinauer CA, Francis GL, Tuttle RM. 2000. The ret/PTC mutations are common in sporadic papillary thyroid carcinoma of children and young adults. J Clin Endocrinol Metab 85:1170–1175 [DOI] [PubMed] [Google Scholar]
- 63.Patel A, Jhiang S, Dogra S, Terrell R, Powers PA, Fenton C, Dinauer CA, Tuttle RM, Francis GL. 2002. Differentiated thyroid carcinoma that express sodium-iodide symporter have a lower risk of recurrence for children and adolescents. Pediatr Res 52:737–744 [DOI] [PubMed] [Google Scholar]
- 64.Bal CS, Padhy AK, Kumar A. 2001. Clinical features of differentiated thyroid carcinoma in children and adolescents from a sub-Himalayan iodine-deficient endemic zone. Nucl Med Commun 22:881–887 [DOI] [PubMed] [Google Scholar]
- 65.Borson-Chazot F, Causeret S, Lifante JC, Augros M, Berger N, Peix JL. 2004. Predictive factors for recurrence from a series of 74 children and adolescents with differentiated thyroid cancer. World J Surg 28:1088–1092 [DOI] [PubMed] [Google Scholar]
- 66.Alessandri AJ, Goddard KJ, Blair GK, Fryer CJ, Schultz KR. 2000. Age is the major determinant of recurrence in pediatric differentiated thyroid carcinoma. Med Pediatr Oncol 35:41–46 [DOI] [PubMed] [Google Scholar]
- 67.Lazar L, Lebenthal Y, Steinmetz A, Yackobovitch-Gavan M, Phillip M. 2009. Differentiated thyroid carcinoma in pediatric patients: comparison of presentation and course between pre-pubertal children and adolescents. J Pediatr 154:708–714 [DOI] [PubMed] [Google Scholar]
- 68.Zablotska LB, Ron E, Rozhko AV, Hatch M, Polyanskaya ON, Brenner AV, Lubin J, Romanov GN, McConnell RJ, O'Kane P, Evseenko VV, Drozdovitch VV, Luckyanov N, Minenko VF, Bouville A, Masyakin VB. 2011. Thyroid cancer risk in Belarus among children and adolescents exposed to radioiodine after the Chornobyl accident. Br J Cancer 104:181–187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.2010. Thyroid. In: Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. (eds) AJCC Cancer Staging Manual. Seventh edition. Springer, New York, NY, pp 87–96 [Google Scholar]
- 70.Sosa JA, Tuggle CT, Wang TS, Thomas DC, Boudourakis L, Rivkees S, Roman SA. 2008. Clinical and economic outcomes of thyroid and parathyroid surgery in children. J Clin Endocrinol Metab 93:3058–3065 [DOI] [PubMed] [Google Scholar]
- 71.Tuggle CT, Roman SA, Wang TS, Boudourakis L, Thomas DC, Udelsman R, Ann Sosa J. 2008. Pediatric endocrine surgery: who is operating on our children? Surgery 144:869–877; discussion 877. [DOI] [PubMed] [Google Scholar]
- 72.Kundel A, Thompson GB, Richards ML, Qiu LX, Cai Y, Schwenk FW, Lteif AN, Pittock ST, Kumar S, Tebben PJ, Hay ID, Grant CS. 2014. Pediatric endocrine surgery: a 20-year experience at the Mayo Clinic. J Clin Endocrinol Metab 99:399–406 [DOI] [PubMed] [Google Scholar]
- 73.Niedziela M, Korman E, Breborowicz D, Trejster E, Harasymczuk J, Warzywoda M, Rolski M, Breborowicz J. 2004. A prospective study of thyroid nodular disease in children and adolescents in western Poland from 1996 to 2000 and the incidence of thyroid carcinoma relative to iodine deficiency and the Chernobyl disaster. Pediatr Blood Cancer 42:84–92 [DOI] [PubMed] [Google Scholar]
- 74.Oertel JE, Klinck GH. 1965. Structural changes in the thyroid glands of healthy young men. Med Ann Dist Columbia 34:75–77 [PubMed] [Google Scholar]
- 75.Hayashida N, Imaizumi M, Shimura H, Okubo N, Asari Y, Nigawara T, Midorikawa S, Kotani K, Nakaji S, Otsuru A, Akamizu T, Kitaoka M, Suzuki S, Taniguchi N, Yamashita S, Takamura N; Investigation Committee for the Proportion of Thyroid Ultrasound Findings 2013. Thyroid ultrasound findings in children from three Japanese prefectures: Aomori, Yamanashi and Nagasaki. PLoS One 8:e83220. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 76.Sklar C, Whitton J, Mertens A, Stovall M, Green D, Marina N, Greffe B, Wolden S, Robison L. 2000. Abnormalities of the thyroid in survivors of Hodgkin's disease: data from the Childhood Cancer Survivor Study. J Clin Endocrinol Metab 85:3227–3232 [DOI] [PubMed] [Google Scholar]
- 77.Meadows AT, Friedman DL, Neglia JP, Mertens AC, Donaldson SS, Stovall M, Hammond S, Yasui Y, Inskip PD. 2009. Second neoplasms in survivors of childhood cancer: findings from the Childhood Cancer Survivor Study cohort. J Clin Oncol 27:2356–2362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mazzaferri EL. 1993. Management of a solitary thyroid nodule. N Engl J Med 328:553–559 [DOI] [PubMed] [Google Scholar]
- 79.Schneider AB, Bekerman C, Leland J, Rosengarten J, Hyun H, Collins B, Shore-Freedman E, Gierlowski TC. 1997. Thyroid nodules in the follow-up of irradiated individuals: comparison of thyroid ultrasound with scanning and palpation. J Clin Endocrinol Metab 82:4020–4027 [DOI] [PubMed] [Google Scholar]
- 80.Ito M, Yamashita S, Ashizawa K, Namba H, Hoshi M, Shibata Y, Sekine I, Nagataki S, Shigematsu I. 1995. Childhood thyroid diseases around Chernobyl evaluated by ultrasound examination and fine needle aspiration cytology. Thyroid 5:365–368 [DOI] [PubMed] [Google Scholar]
- 81.Ron E, Lubin JH, Shore RE, Mabuchi K, Modan B, Pottern LM, Schneider AB, Tucker MA, Boice JD., Jr 1995. Thyroid cancer after exposure to external radiation: a pooled analysis of seven studies. Radiat Res 141:259–277 [PubMed] [Google Scholar]
- 82.Ronckers CM, Sigurdson AJ, Stovall M, Smith SA, Mertens AC, Liu Y, Hammond S, Land CE, Neglia JP, Donaldson SS, Meadows AT, Sklar CA, Robison LL, Inskip PD. 2006. Thyroid cancer in childhood cancer survivors: a detailed evaluation of radiation dose response and its modifiers. Radiat Res 166:618–628 [DOI] [PubMed] [Google Scholar]
- 83.Brignardello E, Corrias A, Isolato G, Palestini N, Cordero di Montezemolo L, Fagioli F, Boccuzzi G. 2008. Ultrasound screening for thyroid carcinoma in childhood cancer survivors: a case series. J Clin Endocrinol Metab 93:4840–4843 [DOI] [PubMed] [Google Scholar]
- 84.Metzger ML, Howard SC, Hudson MM, Gow KW, Li CS, Krasin MJ, Merchant T, Kun L, Shelso J, Pui CH, Shochat SJ, McCarville MB. 2006. Natural history of thyroid nodules in survivors of pediatric Hodgkin lymphoma. Pediatr Blood Cancer 46:314–319 [DOI] [PubMed] [Google Scholar]
- 85.Son EJ, Nose V. 2012. Familial follicular cell-derived thyroid carcinoma. Front Endocrinol (Lausanne) 3:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kalkan E, Waguespack SG. 2013. Endocrine tumors associated with neurofibromatosis type 1, Peutz-Jeghers syndrome and other familial neoplasia syndromes. Front Horm Res 41:166–181 [DOI] [PubMed] [Google Scholar]
- 87.Septer S, Slowik V, Morgan R, Dai H, Attard T. 2013. Thyroid cancer complicating familial adenomatous polyposis: mutation spectrum of at-risk individuals. Hered Cancer Clin Pract 11:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bertherat J, Horvath A, Groussin L, Grabar S, Boikos S, Cazabat L, Libe R, Rene-Corail F, Stergiopoulos S, Bourdeau I, Bei T, Clauser E, Calender A, Kirschner LS, Bertagna X, Carney JA, Stratakis CA. 2009. Mutations in regulatory subunit type 1A of cyclic adenosine 5′-monophosphate-dependent protein kinase (PRKAR1A): phenotype analysis in 353 patients and 80 different genotypes. J Clin Endocrinol Metab 94:2085–2091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.de Kock L, Sabbaghian N, Soglio DB, Guillerman RP, Park BK, Chami R, Deal CL, Priest JR, Foulkes WD. 2014. Exploring the association between DICER1 mutations and differentiated thyroid carcinoma. J Clin Endocrinol Metab 99:E1072–E1077 [DOI] [PubMed] [Google Scholar]
- 90.Doros L, Schultz KA, Stewart DR, Bauer AJ, Williams G, Rossi CT, Carr A, Yang J, Dehner LP, Messinger Y, Hill DA. 1993. DICER1-related disorders. In: Pagon RA, Adam MP, Ardinger HH, Bird TD, Dolan CR, Fong CT, Smith RJH, Stephens K. (eds) GeneReviews, Seattle, WA [Google Scholar]
- 91.Smith JR, Marqusee E, Webb S, Nose V, Fishman SJ, Shamberger RC, Frates MC, Huang SA. 2011. Thyroid nodules and cancer in children with PTEN hamartoma tumor syndrome. J Clin Endocrinol Metab 96:34–37 [DOI] [PubMed] [Google Scholar]
- 92.Ngeow J, Mester J, Rybicki LA, Ni Y, Milas M, Eng C. 2011. Incidence and clinical characteristics of thyroid cancer in prospective series of individuals with Cowden and Cowden-like syndrome characterized by germline PTEN, SDH, or KLLN alterations. J Clin Endocrinol Metab 96:E2063–E2071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pilarski R, Burt R, Kohlman W, Pho L, Shannon KM, Swisher E. 2013. Cowden syndrome and the PTEN hamartoma tumor syndrome: systematic review and revised diagnostic criteria. J Natl Cancer Inst 105:1607–1616 [DOI] [PubMed] [Google Scholar]
- 94.Lauper JM, Krause A, Vaughan TL, Monnat RJ., Jr 2013. Spectrum and risk of neoplasia in Werner syndrome: a systematic review. PLoS One 8:e59709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lapunzina P. 2005. Risk of tumorigenesis in overgrowth syndromes: a comprehensive review. Am J Med Genet C Semin Med Genet 137C:53–71 [DOI] [PubMed] [Google Scholar]
- 96.Papathomas TG, Gaal J, Corssmit EP, Oudijk L, Korpershoek E, Heimdal K, Bayley JP, Morreau H, van Dooren M, Papaspyrou K, Schreiner T, Hansen T, Andresen PA, Restuccia DF, van Kessel I, van Leenders GJ, Kros JM, Looijenga LH, Hofland LJ, Mann W, van Nederveen FH, Mete O, Asa SL, de Krijger RR, Dinjens WN. 2014. Non-pheochromocytoma (PCC)/paraganglioma (PGL) tumors in patients with succinate dehydrogenase-related PCC-PGL syndromes: a clinicopathological and molecular analysis. Eur J Endocrinol 170:1–12 [DOI] [PubMed] [Google Scholar]
- 97.Masciari S, Van den Abbeele AD, Diller LR, Rastarhuyeva I, Yap J, Schneider K, Digianni L, Li FP, Fraumeni JF, Jr, Syngal S, Garber JE. 2008. F18-fluorodeoxyglucose-positron emission tomography/computed tomography screening in Li-Fraumeni syndrome. JAMA 299:1315–1319 [DOI] [PubMed] [Google Scholar]
- 98.Collins MT, Sarlis NJ, Merino MJ, Monroe J, Crawford SE, Krakoff JA, Guthrie LC, Bonat S, Robey PG, Shenker A. 2003. Thyroid carcinoma in the McCune-Albright syndrome: contributory role of activating Gs alpha mutations. J Clin Endocrinol Metab 88:4413–4417 [DOI] [PubMed] [Google Scholar]
- 99.Triggiani V, Guastamacchia E, Renzulli G, Giagulli VA, Tafaro E, Licchelli B, Resta F, Sabba C, Bagnulo R, Lastella P, Stella A, Resta N. 2011. Papillary thyroid carcinoma in Peutz-Jeghers syndrome. Thyroid 21:1273–1277 [DOI] [PubMed] [Google Scholar]
- 100.Capezzone M, Marchisotta S, Cantara S, Busonero G, Brilli L, Pazaitou-Panayiotou K, Carli A, Caruso G, Toti P, Capitani S, Pammolli A, Pacini F. 2008. Familial non-medullary thyroid carcinoma displays the features of clinical anticipation suggestive of a distinct biological entity. Endocr Relat Cancer 15:1075–1081 [DOI] [PubMed] [Google Scholar]
- 101.Charkes ND. 2006. On the prevalence of familial nonmedullary thyroid cancer in multiply affected kindreds. Thyroid 16:181–186 [DOI] [PubMed] [Google Scholar]
- 102.Mazeh H, Benavidez J, Poehls JL, Youngwirth L, Chen H, Sippel RS. 2012. In patients with thyroid cancer of follicular cell origin, a family history of nonmedullary thyroid cancer in one first-degree relative is associated with more aggressive disease. Thyroid 22:3–8 [DOI] [PubMed] [Google Scholar]
- 103.Moses W, Weng J, Kebebew E. 2011. Prevalence, clinicopathologic features, and somatic genetic mutation profile in familial versus sporadic nonmedullary thyroid cancer. Thyroid 21:367–371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Robenshtok E, Tzvetov G, Grozinsky-Glasberg S, Shraga-Slutzky I, Weinstein R, Lazar L, Serov S, Singer J, Hirsch D, Shimon I, Benbassat C. 2011. Clinical characteristics and outcome of familial nonmedullary thyroid cancer: a retrospective controlled study. Thyroid 21:43–48 [DOI] [PubMed] [Google Scholar]
- 105.Sippel RS, Caron NR, Clark OH. 2007. An evidence-based approach to familial nonmedullary thyroid cancer: screening, clinical management, and follow-up. World J Surg 31:924–933 [DOI] [PubMed] [Google Scholar]
- 106.Steinhagen E, Guillem JG, Chang G, Salo-Mullen EE, Shia J, Fish S, Stadler ZK, Markowitz AJ. 2012. The prevalence of thyroid cancer and benign thyroid disease in patients with familial adenomatous polyposis may be higher than previously recognized. Clin Colorectal Cancer 11:304–308 [DOI] [PubMed] [Google Scholar]
- 107.Rosario PW, Mineiro Filho AF, Prates BS, Silva LC, Lacerda RX, Calsolari MR. 2012. Ultrasonographic screening for thyroid cancer in siblings of patients with apparently sporadic papillary carcinoma. Thyroid 22:805–808 [DOI] [PubMed] [Google Scholar]
- 108.Corrias A, Cassio A, Weber G, Mussa A, Wasniewska M, Rapa A, Gastaldi R, Einaudi S, Baronio F, Vigone MC, Messina MF, Bal M, Bona G, de Sanctis C. 2008. Thyroid nodules and cancer in children and adolescents affected by autoimmune thyroiditis. Arch Pediatr Adolesc Med 162:526–531 [DOI] [PubMed] [Google Scholar]
- 109.McLeod DS, Watters KF, Carpenter AD, Ladenson PW, Cooper DS, Ding EL. 2012. Thyrotropin and thyroid cancer diagnosis: a systematic review and dose-response meta-analysis. J Clin Endocrinol Metab 97:2682–2692 [DOI] [PubMed] [Google Scholar]
- 110.Lyshchik A, Drozd V, Demidchik Y, Reiners C. 2005. Diagnosis of thyroid cancer in children: value of gray-scale and power doppler US. Radiology 235:604–613 [DOI] [PubMed] [Google Scholar]
- 111.McHenry CR, Huh ES, Machekano RN. 2008. Is nodule size an independent predictor of thyroid malignancy? Surgery 144:1062–1068; discussion 1068–1069. [DOI] [PubMed] [Google Scholar]
- 112.Drozd VM, Lushchik ML, Polyanskaya ON, Fridman MV, Demidchik YE, Lyshchik AP, Biko J, Reiners C, Shibata Y, Saenko VA, Yamashita S. 2009. The usual ultrasonographic features of thyroid cancer are less frequent in small tumors that develop after a long latent period after the Chernobyl radiation release accident. Thyroid 19:725–734 [DOI] [PubMed] [Google Scholar]
- 113.Leboulleux S, Girard E, Rose M, Travagli JP, Sabbah N, Caillou B, Hartl DM, Lassau N, Baudin E, Schlumberger M. 2007. Ultrasound criteria of malignancy for cervical lymph nodes in patients followed up for differentiated thyroid cancer. J Clin Endocrinol Metab 92:3590–3594 [DOI] [PubMed] [Google Scholar]
- 114.Stevens C, Lee JK, Sadatsafavi M, Blair GK. 2009. Pediatric thyroid fine-needle aspiration cytology: a meta-analysis. J Pediatr Surg 44:2184–2191 [DOI] [PubMed] [Google Scholar]
- 115.Amrikachi M, Ponder TB, Wheeler TM, Smith D, Ramzy I. 2005. Thyroid fine-needle aspiration biopsy in children and adolescents: experience with 218 aspirates. Diagn Cytopathol 32:189–192 [DOI] [PubMed] [Google Scholar]
- 116.Liel Y, Ariad S, Barchana M. 2001. Long-term follow-up of patients with initially benign thyroid fine-needle aspirations. Thyroid 11:775–778 [DOI] [PubMed] [Google Scholar]
- 117.Yokozawa T, Fukata S, Kuma K, Matsuzuka F, Kobayashi A, Hirai K, Miyauchi A, Sugawara M. 1996. Thyroid cancer detected by ultrasound-guided fine-needle aspiration biopsy. World J Surg 20:848–853; discussion 853. [DOI] [PubMed] [Google Scholar]
- 118.Izquierdo R, Shankar R, Kort K, Khurana K. 2009. Ultrasound-guided fine-needle aspiration in the management of thyroid nodules in children and adolescents. Thyroid 19:703–705 [DOI] [PubMed] [Google Scholar]
- 119.Corrias A, Einaudi S, Chiorboli E, Weber G, Crino A, Andreo M, Cesaretti G, de Sanctis L, Messina MF, Segni M, Cicchetti M, Vigone M, Pasquino AM, Spera S, de Luca F, Mussa GC, Bona G. 2001. Accuracy of fine needle aspiration biopsy of thyroid nodules in detecting malignancy in childhood: comparison with conventional clinical, laboratory, and imaging approaches. J Clin Endocrinol Metab 86:4644–4648 [DOI] [PubMed] [Google Scholar]
- 120.Sohn YM, Kim EK, Moon HJ, Kim SJ, Kwak JY. 2011. Suspiciously malignant findings on ultrasound after fine needle aspiration biopsy in a thyroid nodule with initially benign ultrasound and cytologic result: to repeat or to follow-up. Clin Imaging 35:470–475 [DOI] [PubMed] [Google Scholar]
- 121.Cibas ES, Ali SZ. 2009. The Bethesda System for Reporting Thyroid Cytopathology. Thyroid 19:1159–1165 [DOI] [PubMed] [Google Scholar]
- 122.Baloch ZW, LiVolsi VA, Asa SL, Rosai J, Merino MJ, Randolph G, Vielh P, DeMay RM, Sidawy MK, Frable WJ. 2008. Diagnostic terminology and morphologic criteria for cytologic diagnosis of thyroid lesions: a synopsis of the National Cancer Institute Thyroid Fine-Needle Aspiration State of the Science Conference. Diagn Cytopathol 36:425–437 [DOI] [PubMed] [Google Scholar]
- 123.Baloch ZW, LiVolsi VA. 1999. Post fine-needle aspiration histologic alterations of thyroid revisited. Am J Clin Pathol 112:311–316 [DOI] [PubMed] [Google Scholar]
- 124.Smith M, Pantanowitz L, Khalbuss WE, Benkovich VA, Monaco SE. 2013. Indeterminate pediatric thyroid fine needle aspirations: a study of 68 cases. Acta Cytol 57:341–348 [DOI] [PubMed] [Google Scholar]
- 125.Nikiforov YE, Ohori NP, Hodak SP, Carty SE, LeBeau SO, Ferris RL, Yip L, Seethala RR, Tublin ME, Stang MT, Coyne C, Johnson JT, Stewart AF, Nikiforova MN. 2011. Impact of mutational testing on the diagnosis and management of patients with cytologically indeterminate thyroid nodules: a prospective analysis of 1056 FNA samples. J Clin Endocrinol Metab 96:3390–3397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Alexander EK, Kennedy GC, Baloch ZW, Cibas ES, Chudova D, Diggans J, Friedman L, Kloos RT, Livolsi VA, Mandel SJ, Raab SS, Rosai J, Steward DL, Walsh PS, Wilde JI, Zeiger MA, Lanman RB, Haugen BR. 2012. Preoperative diagnosis of benign thyroid nodules with indeterminate cytology. N Engl J Med 367:705–715 [DOI] [PubMed] [Google Scholar]
- 127.Cerutti JM. 2011. Employing genetic markers to improve diagnosis of thyroid tumor fine needle biopsy. Curr Genomics 12:589–596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Duick DS. 2012. Overview of molecular biomarkers for enhancing the management of cytologically indeterminate thyroid nodules and thyroid cancer. Endocr Pract 18:611–615 [DOI] [PubMed] [Google Scholar]
- 129.Ferraz C, Eszlinger M, Paschke R. 2011. Current state and future perspective of molecular diagnosis of fine-needle aspiration biopsy of thyroid nodules. J Clin Endocrinol Metab 96:2016–2026 [DOI] [PubMed] [Google Scholar]
- 130.Nikiforov YE, Nikiforova MN. 2011. Molecular genetics and diagnosis of thyroid cancer. Nat Rev Endocrinol 7:569–580 [DOI] [PubMed] [Google Scholar]
- 131.Buryk MA, Monaco SE, Witchel SF, Mehta DK, Gurtunca N, Nikiforov YE, Simons JP. 2013. Preoperative cytology with molecular analysis to help guide surgery for pediatric thyroid nodules. Int J Pediatr Otorhinolaryngol 77:1697–1700 [DOI] [PubMed] [Google Scholar]
- 132.Elisei R, Romei C, Vorontsova T, Cosci B, Veremeychik V, Kuchinskaya E, Basolo F, Demidchik EP, Miccoli P, Pinchera A, Pacini F. 2001. RET/PTC rearrangements in thyroid nodules: studies in irradiated and not irradiated, malignant and benign thyroid lesions in children and adults. J Clin Endocrinol Metab 86:3211–3216 [DOI] [PubMed] [Google Scholar]
- 133.Millman B, Pellitteri PK. 1997. Nodular thyroid disease in children and adolescents. Otolaryngol Head Neck Surg 116:604–609 [DOI] [PubMed] [Google Scholar]
- 134.Orlandi A, Puscar A, Capriata E, Fideleff H. 2005. Repeated fine-needle aspiration of the thyroid in benign nodular thyroid disease: critical evaluation of long-term follow-up. Thyroid 15:274–278 [DOI] [PubMed] [Google Scholar]
- 135.Pinchot SN, Al-Wagih H, Schaefer S, Sippel R, Chen H. 2009. Accuracy of fine-needle aspiration biopsy for predicting neoplasm or carcinoma in thyroid nodules 4 cm or larger. Arch Surg 144:649–655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.McCoy KL, Jabbour N, Ogilvie JB, Ohori NP, Carty SE, Yim JH. 2007. The incidence of cancer and rate of false-negative cytology in thyroid nodules greater than or equal to 4 cm in size. Surgery 142:837–844; discussion 844 e831–833. [DOI] [PubMed] [Google Scholar]
- 137.Wharry LI, McCoy KL, Stang MT, Armstrong MJ, Lebeau SO, Tublin ME, Sholosh B, Silbermann A, Ohori NP, Nikiforov YE, Hodak SP, Carty SE, Yip L. 2014. Thyroid nodules (>/=4 cm): can ultrasound and cytology reliably exclude cancer? World J Surg 38:614–621 [DOI] [PubMed] [Google Scholar]
- 138.Burch HB. 1995. Evaluation and management of the solid thyroid nodule. Endocrinol Metab Clin North Am 24:663–710 [PubMed] [Google Scholar]
- 139.Lawrence W, Jr, Kaplan BJ. 2002. Diagnosis and management of patients with thyroid nodules. J Surg Oncol 80:157–170 [DOI] [PubMed] [Google Scholar]
- 140.Corrias A, Mussa A, Wasniewska M, Segni M, Cassio A, Salerno M, Gastaldi R, Vigone MC, Bal M, Matarazzo P, Weber G, De Luca F. 2011. Levothyroxine treatment in pediatric benign thyroid nodules. Horm Res Paediatr 75:246–251 [DOI] [PubMed] [Google Scholar]
- 141.Faber J, Galloe AM. 1994. Changes in bone mass during prolonged subclinical hyperthyroidism due to L-thyroxine treatment: a meta-analysis. Eur J Endocrinol 130:350–356 [DOI] [PubMed] [Google Scholar]
- 142.Celani MF, Mariani M, Mariani G. 1990. On the usefulness of levothyroxine suppressive therapy in the medical treatment of benign solitary, solid or predominantly solid, thyroid nodules. Acta Endocrinol (Copenh) 123:603–608 [DOI] [PubMed] [Google Scholar]
- 143.Gharib H, Mazzaferri EL. 1998. Thyroxine suppressive therapy in patients with nodular thyroid disease. Ann Intern Med 128:386–394 [DOI] [PubMed] [Google Scholar]
- 144.Papini E, Petrucci L, Guglielmi R, Panunzi C, Rinaldi R, Bacci V, Crescenzi A, Nardi F, Fabbrini R, Pacella CM. 1998. Long-term changes in nodular goiter: a 5-year prospective randomized trial of levothyroxine suppressive therapy for benign cold thyroid nodules. J Clin Endocrinol Metab 83:780–783 [DOI] [PubMed] [Google Scholar]
- 145.Shimaoka K, Sokal JE. 1974. Suppressive therapy of nontoxic goiter. Am J Med 57:576–583 [DOI] [PubMed] [Google Scholar]
- 146.Wemeau JL, Caron P, Schvartz C, Schlienger JL, Orgiazzi J, Cousty C, Vlaeminck-Guillem V. 2002. Effects of thyroid-stimulating hormone suppression with levothyroxine in reducing the volume of solitary thyroid nodules and improving extranodular nonpalpable changes: a randomized, double-blind, placebo-controlled trial by the French Thyroid Research Group. J Clin Endocrinol Metab 87:4928–4934 [DOI] [PubMed] [Google Scholar]
- 147.Sdano MT, Falciglia M, Welge JA, Steward DL. 2005. Efficacy of thyroid hormone suppression for benign thyroid nodules: meta-analysis of randomized trials. Otolaryngol Head Neck Surg 133:391–396 [DOI] [PubMed] [Google Scholar]
- 148.Fogelfeld L, Wiviott MB, Shore-Freedman E, Blend M, Bekerman C, Pinsky S, Schneider AB. 1989. Recurrence of thyroid nodules after surgical removal in patients irradiated in childhood for benign conditions. N Engl J Med 320:835–840 [DOI] [PubMed] [Google Scholar]
- 149.Subbiah S, Collins BJ, Schneider AB. 2007. Factors related to the recurrence of thyroid nodules after surgery for benign radiation-related nodules. Thyroid 17:41–47 [DOI] [PubMed] [Google Scholar]
- 150.Niedziela M, Breborowicz D, Trejster E, Korman E. 2002. Hot nodules in children and adolescents in western Poland from 1996 to 2000: clinical analysis of 31 patients. J Pediatr Endocrinol Metab 15:823–830 [DOI] [PubMed] [Google Scholar]
- 151.Schwab KO, Pfarr N, van der Werf-Grohmann N, Pohl M, Radecke J, Musholt T, Pohlenz J. 2009. Autonomous thyroid adenoma: only an adulthood disease? J Pediatr 154:931–933 e932. [DOI] [PubMed] [Google Scholar]
- 152.Hwang HS, Orloff LA. 2011. Efficacy of preoperative neck ultrasound in the detection of cervical lymph node metastasis from thyroid cancer. Laryngoscope 121:487–491 [DOI] [PubMed] [Google Scholar]
- 153.Park JS, Son KR, Na DG, Kim E, Kim S. 2009. Performance of preoperative sonographic staging of papillary thyroid carcinoma based on the sixth edition of the AJCC/UICC TNM classification system. AJR Am J Roentgenol 192:66–72 [DOI] [PubMed] [Google Scholar]
- 154.Kouvaraki MA, Shapiro SE, Fornage BD, Edeiken-Monro BS, Sherman SI, Vassilopoulou-Sellin R, Lee JE, Evans DB. 2003. Role of preoperative ultrasonography in the surgical management of patients with thyroid cancer. Surgery 134:946-954; discussion 954–945. [DOI] [PubMed] [Google Scholar]
- 155.Solorzano CC, Carneiro DM, Ramirez M, Lee TM, Irvin GL., 3rd 2004. Surgeon-performed ultrasound in the management of thyroid malignancy. Am Surg 70:576–580; discussion 580–572. [PubMed] [Google Scholar]
- 156.Gonzalez HE, Cruz F, O'Brien A, Goni I, Leon A, Claure R, Camus M, Dominguez F, Mosso L, Arteaga E, Gonzalez G, Lopez JM, Rodriguez JA, Carrasco C, Fardella C. 2007. Impact of preoperative ultrasonographic staging of the neck in papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg 133:1258–1262 [DOI] [PubMed] [Google Scholar]
- 157.Stulak JM, Grant CS, Farley DR, Thompson GB, van Heerden JA, Hay ID, Reading CC, Charboneau JW. 2006. Value of preoperative ultrasonography in the surgical management of initial and reoperative papillary thyroid cancer. Arch Surg 141:489–494; discussion 494–486. [DOI] [PubMed] [Google Scholar]
- 158.Shimamoto K, Satake H, Sawaki A, Ishigaki T, Funahashi H, Imai T. 1998. Preoperative staging of thyroid papillary carcinoma with ultrasonography. Eur J Radiol 29:4–10 [DOI] [PubMed] [Google Scholar]
- 159.Choi JS, Kim J, Kwak JY, Kim MJ, Chang HS, Kim EK. 2009. Preoperative staging of papillary thyroid carcinoma: comparison of ultrasound imaging and CT. AJR Am J Roentgenol 193:871–878 [DOI] [PubMed] [Google Scholar]
- 160.Mihailovic J, Prvulovic M, Ivkovic M, Markoski B, Martinov D. 2010. MRI versus 131I whole-body scintigraphy for the detection of lymph node recurrences in differentiated thyroid carcinoma. AJR Am J Roentgenol 195:1197–1203 [DOI] [PubMed] [Google Scholar]
- 161.Miyakoshi A, Dalley RW, Anzai Y. 2007. Magnetic resonance imaging of thyroid cancer. Top Magn Reson Imaging 18:293–302 [DOI] [PubMed] [Google Scholar]
- 162.Brink JS, van Heerden JA, McIver B, Salomao DR, Farley DR, Grant CS, Thompson GB, Zimmerman D, Hay ID. 2000. Papillary thyroid cancer with pulmonary metastases in children: long-term prognosis. Surgery 128:881–886; discussion 886–887. [DOI] [PubMed] [Google Scholar]
- 163.Jarzab B, Handkiewicz-Junak D. 2007. Differentiated thyroid cancer in children and adults: same or distinct disease? Hormones (Athens) 6:200–209 [PubMed] [Google Scholar]
- 164.Schlumberger M, Arcangioli O, Piekarski JD, Tubiana M, Parmentier C. 1988. Detection and treatment of lung metastases of differentiated thyroid carcinoma in patients with normal chest X-rays. J Nucl Med 29:1790–1794 [PubMed] [Google Scholar]
- 165.Kuo SF, Chen ST, Kao PF, Chang YC, Chou SC, Lin JD. 2004. Papillary thyroid cancer with chest metastases only detected using radioactive iodine. Chang Gung Med J 27:663–672 [PubMed] [Google Scholar]
- 166.Ilgan S, Karacalioglu AO, Pabuscu Y, Atac GK, Arslan N, Ozturk E, Gunalp B, Ozguven MA. 2004. Iodine-131 treatment and high-resolution CT: results in patients with lung metastases from differentiated thyroid carcinoma. Eur J Nucl Med Mol Imaging 31:825–830 [DOI] [PubMed] [Google Scholar]
- 167.La Quaglia MP, Corbally MT, Heller G, Exelby PR, Brennan MF. 1988. Recurrence and morbidity in differentiated thyroid carcinoma in children. Surgery 104:1149–1156 [PubMed] [Google Scholar]
- 168.Bargren AE, Meyer-Rochow GY, Delbridge LW, Sidhu SB, Chen H. 2009. Outcomes of surgically managed pediatric thyroid cancer. J Surg Res 156:70–73 [DOI] [PubMed] [Google Scholar]
- 169.Jarzab B, Handkiewicz-Junak D, Wloch J. 2005. Juvenile differentiated thyroid carcinoma and the role of radioiodine in its treatment: a qualitative review. Endocr Relat Cancer 12:773–803 [DOI] [PubMed] [Google Scholar]
- 170.Pacini F, Capezzone M, Elisei R, Ceccarelli C, Taddei D, Pinchera A. 2002. Diagnostic 131-iodine whole-body scan may be avoided in thyroid cancer patients who have undetectable stimulated serum Tg levels after initial treatment. J Clin Endocrinol Metab 87:1499–1501 [DOI] [PubMed] [Google Scholar]
- 171.Spencer CA, Lopresti JS. 2008. Measuring thyroglobulin and thyroglobulin autoantibody in patients with differentiated thyroid cancer. Nat Clin Pract Endocrinol Metab 4:223–233 [DOI] [PubMed] [Google Scholar]
- 172.Toni R, Casa CD, Castorina S, Roti E, Ceda G, Valenti G. 2005. A meta-analysis of inferior thyroid artery variations in different human ethnic groups and their clinical implications. Ann Anat 187:371–385 [DOI] [PubMed] [Google Scholar]
- 173.Toni R, Della Casa C, Castorina S, Malaguti A, Mosca S, Roti E, Valenti G. 2004. A meta-analysis of superior thyroid artery variations in different human groups and their clinical implications. Ann Anat 186:255–262 [DOI] [PubMed] [Google Scholar]
- 174.Nobori M, Saiki S, Tanaka N, Harihara Y, Shindo S, Fujimoto Y. 1994. Blood supply of the parathyroid gland from the superior thyroid artery. Surgery 115:417–423 [PubMed] [Google Scholar]
- 175.Carty SE, Cooper DS, Doherty GM, Duh QY, Kloos RT, Mandel SJ, Randolph GW, Stack BC, Jr, Steward DL, Terris DJ, Thompson GB, Tufano RP, Tuttle RM, Udelsman R. 2009. Consensus statement on the terminology and classification of central neck dissection for thyroid cancer. Thyroid 19:1153–1158 [DOI] [PubMed] [Google Scholar]
- 176.Powers PA, Dinauer CA, Tuttle RM, Robie DK, McClellan DR, Francis GL. 2003. Tumor size and extent of disease at diagnosis predict the response to initial therapy for papillary thyroid carcinoma in children and adolescents. J Pediatr Endocrinol Metab 16:693–702 [DOI] [PubMed] [Google Scholar]
- 177.Buffet C, Golmard JL, Hoang C, Tresallet C, Du Pasquier Fediaevsky L, Fierrard H, Aurengo A, Menegaux F, Leenhardt L. 2012. Scoring system for predicting recurrences in patients with papillary thyroid microcarcinoma. Eur J Endocrinol 167:267–275 [DOI] [PubMed] [Google Scholar]
- 178.Farahati J, Reiners C, Demidchik EP. 1999. Is the UICC/AJCC classification of primary tumor in childhood thyroid carcinoma valid? J Nucl Med 40:2125. [PubMed] [Google Scholar]
- 179.Vassilopoulou-Sellin R, Goepfert H, Raney B, Schultz PN. 1998. Differentiated thyroid cancer in children and adolescents: clinical outcome and mortality after long-term follow-up. Head Neck 20:549–555 [DOI] [PubMed] [Google Scholar]
- 180.Sywak M, Cornford L, Roach P, Stalberg P, Sidhu S, Delbridge L. 2006. Routine ipsilateral level VI lymphadenectomy reduces postoperative thyroglobulin levels in papillary thyroid cancer. Surgery 140:1000–1005; discussion 1005–1007. [DOI] [PubMed] [Google Scholar]
- 181.Grubbs EG, Rich TA, Li G, Sturgis EM, Younes MN, Myers JN, Edeiken-Monroe B, Fornage BD, Monroe DP, Staerkel GA, Williams MD, Waguespack SG, Hu MI, Cote G, Gagel RF, Cohen J, Weber RS, Anaya DA, Holsinger FC, Perrier ND, Clayman GL, Evans DB. 2008. Recent advances in thyroid cancer. Curr Probl Surg 45:156–250 [DOI] [PubMed] [Google Scholar]
- 182.Shen WT, Ogawa L, Ruan D, Suh I, Duh QY, Clark OH. 2010. Central neck lymph node dissection for papillary thyroid cancer: the reliability of surgeon judgment in predicting which patients will benefit. Surgery 148:398–403 [DOI] [PubMed] [Google Scholar]
- 183.Musacchio MJ, Kim AW, Vijungco JD, Prinz RA. 2003. Greater local recurrence occurs with “berry picking” than neck dissection in thyroid cancer. Am Surg 69:191–196; discussion 196–197. [PubMed] [Google Scholar]
- 184.Moo TA, Umunna B, Kato M, Butriago D, Kundel A, Lee JA, Zarnegar R, Fahey TJ., 3rd 2009. Ipsilateral versus bilateral central neck lymph node dissection in papillary thyroid carcinoma. Ann Surg 250:403–408 [DOI] [PubMed] [Google Scholar]
- 185.Giordano D, Valcavi R, Thompson GB, Pedroni C, Renna L, Gradoni P, Barbieri V. 2012. Complications of central neck dissection in patients with papillary thyroid carcinoma: results of a study on 1087 patients and review of the literature. Thyroid 22:911–917 [DOI] [PubMed] [Google Scholar]
- 186.Fish SA, Langer JE, Mandel SJ. 2008. Sonographic imaging of thyroid nodules and cervical lymph nodes. Endocrinol Metab Clin North Am 37:401–417, ix. [DOI] [PubMed] [Google Scholar]
- 187.Baskin HJ. 2004. Detection of recurrent papillary thyroid carcinoma by thyroglobulin assessment in the needle washout after fine-needle aspiration of suspicious lymph nodes. Thyroid 14:959–963 [DOI] [PubMed] [Google Scholar]
- 188.Boi F, Baghino G, Atzeni F, Lai ML, Faa G, Mariotti S. 2006. The diagnostic value for differentiated thyroid carcinoma metastases of thyroglobulin (Tg) measurement in washout fluid from fine-needle aspiration biopsy of neck lymph nodes is maintained in the presence of circulating anti-Tg antibodies. J Clin Endocrinol Metab 91:1364–1369 [DOI] [PubMed] [Google Scholar]
- 189.Cunha N, Rodrigues F, Curado F, Ilheu O, Cruz C, Naidenov P, Rascao MJ, Ganho J, Gomes I, Pereira H, Real O, Figueiredo P, Campos B, Valido F. 2007. Thyroglobulin detection in fine-needle aspirates of cervical lymph nodes: a technique for the diagnosis of metastatic differentiated thyroid cancer. Eur J Endocrinol 157:101–107 [DOI] [PubMed] [Google Scholar]
- 190.Frasoldati A, Pesenti M, Gallo M, Caroggio A, Salvo D, Valcavi R. 2003. Diagnosis of neck recurrences in patients with differentiated thyroid carcinoma. Cancer 97:90–96 [DOI] [PubMed] [Google Scholar]
- 191.Giovanella L, Bongiovanni M, Trimboli P. 2013. Diagnostic value of thyroglobulin assay in cervical lymph node fine-needle aspirations for metastatic differentiated thyroid cancer. Curr Opin Oncol 25:6–13 [DOI] [PubMed] [Google Scholar]
- 192.Skinner MA, Norton JA, Moley JF, DeBenedetti MK, Wells SA., Jr 1997. Heterotopic autotransplantation of parathyroid tissue in children undergoing total thyroidectomy. J Pediatr Surg 32:510–513 [DOI] [PubMed] [Google Scholar]
- 193.Barczynski M, Cichon S, Konturek A, Cichon W. 2008. Applicability of intraoperative parathyroid hormone assay during total thyroidectomy as a guide for the surgeon to selective parathyroid tissue autotransplantation. World J Surg 32:822–828 [DOI] [PubMed] [Google Scholar]
- 194.Walsh SR, Kumar B, Coveney EC. 2007. Serum calcium slope predicts hypocalcaemia following thyroid surgery. Int J Surg 5:41–44 [DOI] [PubMed] [Google Scholar]
- 195.Grodski S, Lundgren CI, Sidhu S, Sywak M, Delbridge L. 2009. Postoperative PTH measurement facilitates day 1 discharge after total thyroidectomy. Clin Endocrinol 70:322–325 [DOI] [PubMed] [Google Scholar]
- 196.Grodski S, Serpell J. 2008. Evidence for the role of perioperative PTH measurement after total thyroidectomy as a predictor of hypocalcemia. World J Surg 32:1367–1373 [DOI] [PubMed] [Google Scholar]
- 197.Sam AH, Dhillo WS, Donaldson M, Moolla A, Meeran K, Tolley NS, Palazzo FF. 2011. Serum phosphate predicts temporary hypocalcaemia following thyroidectomy. Clin Endocrinol 74:388–393 [DOI] [PubMed] [Google Scholar]
- 198.Angelos P. 2009. Recurrent laryngeal nerve monitoring: state of the art, ethical and legal issues. Surg Clin North Am 89:1157–1169 [DOI] [PubMed] [Google Scholar]
- 199.Powers PA, Dinauer CA, Tuttle RM, Francis GL. 2004. The MACIS score predicts the clinical course of papillary thyroid carcinoma in children and adolescents. J Pediatr Endocrinol Metab 17:339–343 [DOI] [PubMed] [Google Scholar]
- 200.Waguespack SG, Francis G. 2010. Initial management and follow-up of differentiated thyroid cancer in children. J Natl Compr Canc Netw 8:1289–1300 [DOI] [PubMed] [Google Scholar]
- 201.Lee JI, Chung YJ, Cho BY, Chong S, Seok JW, Park SJ. 2013. Postoperative-stimulated serum thyroglobulin measured at the time of 131I ablation is useful for the prediction of disease status in patients with differentiated thyroid carcinoma. Surgery 153:828–835 [DOI] [PubMed] [Google Scholar]
- 202.Antonelli A, Miccoli P, Fallahi P, Grosso M, Nesti C, Spinelli C, Ferrannini E. 2003. Role of neck ultrasonography in the follow-up of children operated on for thyroid papillary cancer. Thyroid 13:479–484 [DOI] [PubMed] [Google Scholar]
- 203.Rosario PW, Mineiro Filho AF, Lacerda RX, dos Santos DA, Calsolari MR. 2012. The value of diagnostic whole-body scanning and serum thyroglobulin in the presence of elevated serum thyrotropin during follow-up of anti-thyroglobulin antibody-positive patients with differentiated thyroid carcinoma who appeared to be free of disease after total thyroidectomy and radioactive iodine ablation. Thyroid 22:113–116 [DOI] [PubMed] [Google Scholar]
- 204.Barwick TD, Dhawan RT, Lewington V. 2012. Role of SPECT/CT in differentiated thyroid cancer. Nucl Med Commun 33:787–798 [DOI] [PubMed] [Google Scholar]
- 205.Kim HY, Gelfand MJ, Sharp SE. 2011. SPECT/CT imaging in children with papillary thyroid carcinoma. Pediatr Radiol 41:1008–1012 [DOI] [PubMed] [Google Scholar]
- 206.Xue YL, Qiu ZL, Song HJ, Luo QY. 2013. Value of 131I SPECT/CT for the evaluation of differentiated thyroid cancer: a systematic review of the literature. Eur J Nucl Med Mol Imaging 40:768–778 [DOI] [PubMed] [Google Scholar]
- 207.Cohen JB, Kalinyak JE, McDougall IR. 2004. Clinical implications of the differences between diagnostic 123I and post-therapy 131I scans. Nucl Med Commun 25:129–134 [DOI] [PubMed] [Google Scholar]
- 208.Hurley JR. 2000. Management of thyroid cancer: radioiodine ablation, “stunning,” and treatment of thyroglobulin-positive, (131)I scan-negative patients. Endocr Pract 6:401–406 [DOI] [PubMed] [Google Scholar]
- 209.Lassmann M, Hanscheid H, Chiesa C, Hindorf C, Flux G, Luster M. 2008. EANM Dosimetry Committee series on standard operational procedures for pre-therapeutic dosimetry I: blood and bone marrow dosimetry in differentiated thyroid cancer therapy. Eur J Nucl Med Mol Imaging 35:1405–1412 [DOI] [PubMed] [Google Scholar]
- 210.Luster M, Lassmann M, Freudenberg LS, Reiners C. 2007. Thyroid cancer in childhood: management strategy, including dosimetry and long-term results. Hormones (Athens) 6:269–278 [DOI] [PubMed] [Google Scholar]
- 211.Urhan M, Dadparvar S, Mavi A, Houseni M, Chamroonrat W, Alavi A, Mandel SJ. 2007. Iodine-123 as a diagnostic imaging agent in differentiated thyroid carcinoma: a comparison with iodine-131 post-treatment scanning and serum thyroglobulin measurement. Eur J Nucl Med and molecular imaging 34:1012–1017 [DOI] [PubMed] [Google Scholar]
- 212.Seidlin SM, Marinelli LD, Oshry E. 1946. Radioactive iodine therapy; effect on functioning metastases of adenocarcinoma of the thyroid. J Am Med Assoc 132:838–847 [DOI] [PubMed] [Google Scholar]
- 213.Singer PA, Cooper DS, Daniels GH, Ladenson PW, Greenspan FS, Levy EG, Braverman LE, Clark OH, McDougall IR, Ain KV, Dorfman SG. 1996. Treatment guidelines for patients with thyroid nodules and well-differentiated thyroid cancer. American Thyroid Association. Arch Intern Med 156:2165–2172 [PubMed] [Google Scholar]
- 214.Haymart MR, Banerjee M, Stewart AK, Koenig RJ, Birkmeyer JD, Griggs JJ. 2011. Use of radioactive iodine for thyroid cancer. JAMA 306:721–728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.DeGroot LJ, Kaplan EL, McCormick M, Straus FH. 1990. Natural history, treatment, and course of papillary thyroid carcinoma. J Clin Endocrinol Metab 71:414–424 [DOI] [PubMed] [Google Scholar]
- 216.La Quaglia MP, Telander RL. 1997. Differentiated and medullary thyroid cancer in childhood and adolescence. Semin Pediatr Surg 6:42–49 [PubMed] [Google Scholar]
- 217.Landau D, Vini L, A'Hern R, Harmer C. 2000. Thyroid cancer in children: the Royal Marsden Hospital experience. Eur J Cancer 36:214–220 [DOI] [PubMed] [Google Scholar]
- 218.Nemec J, Rohling S, Zamrazil V, Pohunkova D. 1979. Comparison of the distribution of diagnostic and thyroablative I-131 in the evaluation of differentiated thyroid cancers. J Nucl Med 20:92–97 [PubMed] [Google Scholar]
- 219.Hung W, Sarlis NJ. 2002. Current controversies in the management of pediatric patients with well-differentiated nonmedullary thyroid cancer: a review. Thyroid 12:683–702 [DOI] [PubMed] [Google Scholar]
- 220.Rivkees SA, Mazzaferri EL, Verburg FA, Reiners C, Luster M, Breuer CK, Dinauer CA, Udelsman R. 2011. The treatment of differentiated thyroid cancer in children: emphasis on surgical approach and radioactive iodine therapy. Endocr Rev 32:798–826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Iyer NG, Morris LG, Tuttle RM, Shaha AR, Ganly I. 2011. Rising incidence of second cancers in patients with low-risk (T1N0) thyroid cancer who receive radioactive iodine therapy. Cancer 117:4439–4446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Sawka AM, Thabane L, Parlea L, Ibrahim-Zada I, Tsang RW, Brierley JD, Straus S, Ezzat S, Goldstein DP. 2009. Second primary malignancy risk after radioactive iodine treatment for thyroid cancer: a systematic review and meta-analysis. Thyroid 19:451–457 [DOI] [PubMed] [Google Scholar]
- 223.Durante C, Montesano T, Attard M, Torlontano M, Monzani F, Costante G, Meringolo D, Ferdeghini M, Tumino S, Lamartina L, Paciaroni A, Massa M, Giacomelli L, Ronga G, Filetti S. 2012. Long-term surveillance of papillary thyroid cancer patients who do not undergo postoperative radioiodine remnant ablation: is there a role for serum thyroglobulin measurement? J Clin Endocrinol Metab 97:2748–2753 [DOI] [PubMed] [Google Scholar]
- 224.Torlontano M, Crocetti U, Augello G, D'Aloiso L, Bonfitto N, Varraso A, Dicembrino F, Modoni S, Frusciante V, Di Giorgio A, Bruno R, Filetti S, Trischitta V. 2006. Comparative evaluation of recombinant human thyrotropin-stimulated thyroglobulin levels, 131I whole-body scintigraphy, and neck ultrasonography in the follow-up of patients with papillary thyroid microcarcinoma who have not undergone radioiodine therapy. J Clin Endocrinol Metab 91:60–63 [DOI] [PubMed] [Google Scholar]
- 225.Nascimento C, Borget I, Troalen F, Al Ghuzlan A, Deandreis D, Hartl D, Lumbroso J, Chougnet CN, Baudin E, Schlumberger M, Leboulleux S. 2013. Ultrasensitive serum thyroglobulin measurement is useful for the follow-up of patients treated with total thyroidectomy without radioactive iodine ablation. Eur J Endocrinol 169:689–693 [DOI] [PubMed] [Google Scholar]
- 226.Kumar A, Bal CS. 2003. Differentiated thyroid cancer. Indian J Pediatr 70:707–713 [DOI] [PubMed] [Google Scholar]
- 227.La Quaglia MP, Black T, Holcomb GW, 3rd, Sklar C, Azizkhan RG, Haase GM, Newman KD. 2000. Differentiated thyroid cancer: clinical characteristics, treatment, and outcome in patients under 21 years of age who present with distant metastases. A report from the Surgical Discipline Committee of the Children's Cancer Group. J Pediatr Surg 35:955–959; discussion 960. [DOI] [PubMed] [Google Scholar]
- 228.Rachmiel M, Charron M, Gupta A, Hamilton J, Wherrett D, Forte V, Daneman D. 2006. Evidence-based review of treatment and follow up of pediatric patients with differentiated thyroid carcinoma. J Pediatr Endocrinol Metab 19:1377–1393 [DOI] [PubMed] [Google Scholar]
- 229.Dinauer C, Francis GL. 2007. Thyroid cancer in children. Endocrinol Metab Clin North Am 36:779–806, vii. [DOI] [PubMed] [Google Scholar]
- 230.Kuijt WJ, Huang SA. 2005. Children with differentiated thyroid cancer achieve adequate hyperthyrotropinemia within 14 days of levothyroxine withdrawal. J Clin Endocrinol Metab 90:6123–6125 [DOI] [PubMed] [Google Scholar]
- 231.Pacini F, Schlumberger M, Dralle H, Elisei R, Smit JW, Wiersinga W. 2006. European consensus for the management of patients with differentiated thyroid carcinoma of the follicular epithelium. Eur J Endocrinol 154:787–803 [DOI] [PubMed] [Google Scholar]
- 232.Tuttle RM, Brokhin M, Omry G, Martorella AJ, Larson SM, Grewal RK, Fleisher M, Robbins RJ. 2008. Recombinant human TSH-assisted radioactive iodine remnant ablation achieves short-term clinical recurrence rates similar to those of traditional thyroid hormone withdrawal. J Nucl Med 49:764–770 [DOI] [PubMed] [Google Scholar]
- 233.Hugo J, Robenshtok E, Grewal R, Larson S, Tuttle RM. 2012. Recombinant human thyroid stimulating hormone-assisted radioactive iodine remnant ablation in thyroid cancer patients at intermediate to high risk of recurrence. Thyroid 22:1007–1015 [DOI] [PubMed] [Google Scholar]
- 234.Hanscheid H, Lassmann M, Luster M, Thomas SR, Pacini F, Ceccarelli C, Ladenson PW, Wahl RL, Schlumberger M, Ricard M, Driedger A, Kloos RT, Sherman SI, Haugen BR, Carriere V, Corone C, Reiners C. 2006. Iodine biokinetics and dosimetry in radioiodine therapy of thyroid cancer: procedures and results of a prospective international controlled study of ablation after rhTSH or hormone withdrawal. J Nucl Med 47:648–654 [PubMed] [Google Scholar]
- 235.Lau WF, Zacharin MR, Waters K, Wheeler G, Johnston V, Hicks RJ. 2006. Management of paediatric thyroid carcinoma: recent experience with recombinant human thyroid stimulating hormone in preparation for radioiodine therapy. Intern Med J 36:564–570 [DOI] [PubMed] [Google Scholar]
- 236.Luster M, Handkiewicz-Junak D, Grossi A, Zacharin M, Taieb D, Cruz O, Hitzel A, Casas JA, Mader U, Dottorini ME. 2009. Recombinant thyrotropin use in children and adolescents with differentiated thyroid cancer: a multicenter retrospective study. J Clin Endocrinol Metab 94:3948–3953 [DOI] [PubMed] [Google Scholar]
- 237.Iorcansky S, Herzovich V, Qualey RR, Tuttle RM. 2005. Serum thyrotropin (TSH) levels after recombinant human TSH injections in children and teenagers with papillary thyroid cancer. J Clin Endocrinol Metab 90:6553–6555 [DOI] [PubMed] [Google Scholar]
- 238.Pluijmen MJ, Eustatia-Rutten C, Goslings BM, Stokkel MP, Arias AM, Diamant M, Romijn JA, Smit JW. 2003. Effects of low-iodide diet on postsurgical radioiodide ablation therapy in patients with differentiated thyroid carcinoma. Clin Endocrinol 58:428–435 [DOI] [PubMed] [Google Scholar]
- 239.Knudsen N, Christiansen E, Brandt-Christensen M, Nygaard B, Perrild H. 2000. Age- and sex-adjusted iodine/creatinine ratio. A new standard in epidemiological surveys? Evaluation of three different estimates of iodine excretion based on casual urine samples and comparison to 24 h values. Eur J Clin Nutr 54:361–363 [DOI] [PubMed] [Google Scholar]
- 240.Sisson JC, Freitas J, McDougall IR, Dauer LT, Hurley JR, Brierley JD, Edinboro CH, Rosenthal D, Thomas MJ, Wexler JA, Asamoah E, Avram AM, Milas M, Greenlee C. 2011. Radiation safety in the treatment of patients with thyroid diseases by radioiodine 131I : practice recommendations of the American Thyroid Association. Thyroid 21:335–346 [DOI] [PubMed] [Google Scholar]
- 241.Nakada K, Ishibashi T, Takei T, Hirata K, Shinohara K, Katoh S, Zhao S, Tamaki N, Noguchi Y, Noguchi S. 2005. Does lemon candy decrease salivary gland damage after radioiodine therapy for thyroid cancer? J Nucl Med 46:261–266 [PubMed] [Google Scholar]
- 242.Ma C, Xie J, Jiang Z, Wang G, Zuo S. 2010. Does amifostine have radioprotective effects on salivary glands in high-dose radioactive iodine-treated differentiated thyroid cancer. Eur J Nucl Med Mol Imaging 37:1778–1785 [DOI] [PubMed] [Google Scholar]
- 243.Koong SS, Reynolds JC, Movius EG, Keenan AM, Ain KB, Lakshmanan MC, Robbins J. 1999. Lithium as a potential adjuvant to 131I therapy of metastatic, well differentiated thyroid carcinoma. J Clin Endocrinol Metab 84:912–916 [DOI] [PubMed] [Google Scholar]
- 244.Tuttle RM, Leboeuf R, Robbins RJ, Qualey R, Pentlow K, Larson SM, Chan CY. 2006. Empiric radioactive iodine dosing regimens frequently exceed maximum tolerated activity levels in elderly patients with thyroid cancer. J Nucl Med 47:1587–1591 [PubMed] [Google Scholar]
- 245.Lassmann M, Hanscheid H, Verburg FA, Luster M. 2011. The use of dosimetry in the treatment of differentiated thyroid cancer. Q J Nucl Med Mol Imaging 55:107–115 [PubMed] [Google Scholar]
- 246.Benua RS, Cicale NR, Sonenberg M, Rawson RW. 1962. The relation of radioiodine dosimetry to results and complications in the treatment of metastatic thyroid cancer. Am J Roentgenol Radium Ther Nucl Med 87:171–182 [PubMed] [Google Scholar]
- 247.Maxon HR, 3rd, Englaro EE, Thomas SR, Hertzberg VS, Hinnefeld JD, Chen LS, Smith H, Cummings D, Aden MD. 1992. Radioiodine-131 therapy for well-differentiated thyroid cancer—a quantitative radiation dosimetric approach: outcome and validation in 85 patients. J Nucl Med 33:1132–1136 [PubMed] [Google Scholar]
- 248.Tuttle RM, Grewal RK, Larson SM. 2007. Radioactive iodine therapy in poorly differentiated thyroid cancer. Nat Clin Pract Oncol 4:665–668 [DOI] [PubMed] [Google Scholar]
- 249.Sgouros G, Song H, Ladenson PW, Wahl RL. 2006. Lung toxicity in radioiodine therapy of thyroid carcinoma: development of a dose-rate method and dosimetric implications of the 80-mCi rule. J Nucl Med 47:1977–1984 [PMC free article] [PubMed] [Google Scholar]
- 250.Hobbs RF, Wahl RL, Lodge MA, Javadi MS, Cho SY, Chien DT, Ewertz ME, Esaias CE, Ladenson PW, Sgouros G. 2009. 124I PET-based 3D-RD dosimetry for a pediatric thyroid cancer patient: real-time treatment planning and methodologic comparison. J Nucl Med 50:1844–1847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Luster M, Clarke SE, Dietlein M, Lassmann M, Lind P, Oyen WJ, Tennvall J, Bombardieri E. 2008. Guidelines for radioiodine therapy of differentiated thyroid cancer. Eur J Nucl Med Mol Imaging 35:1941–1959 [DOI] [PubMed] [Google Scholar]
- 252.Ciappuccini R, Heutte N, Trzepla G, Rame JP, Vaur D, Aide N, Bardet S. 2011. Postablation (131)I scintigraphy with neck and thorax SPECT-CT and stimulated serum thyroglobulin level predict the outcome of patients with differentiated thyroid cancer. Eur J Endocrinol 164:961–969 [DOI] [PubMed] [Google Scholar]
- 253.Stanbury JB, Brownell GL, Riggs DS, Perinetti H, Del Castillo E, Itoiz J, Houssay A, Trucco E, Yaciofano AC. 1952. The iodine-deficient human thyroid gland; a preliminary report. J Clin Endocrinol Metab 12:191–207 [DOI] [PubMed] [Google Scholar]
- 254.Lee JW, Lee SM, Koh GP, Lee DH. 2011. The comparison of (131)I whole-body scans on the third and tenth day after (131)I therapy in patients with well-differentiated thyroid cancer: preliminary report. Ann Nucl Med 25:439–446 [DOI] [PubMed] [Google Scholar]
- 255.Goolden AW, Kam KC, Fitzpatrick ML, Munro AJ. 1986. Oedema of the neck after ablation of the thyroid with radioactive iodine. Br J Radiol 59:583–586 [DOI] [PubMed] [Google Scholar]
- 256.Kloos RT, Duvuuri V, Jhiang SM, Cahill KV, Foster JA, Burns JA. 2002. Nasolacrimal drainage system obstruction from radioactive iodine therapy for thyroid carcinoma. J Clin Endocrinol Metab 87:5817–5820 [DOI] [PubMed] [Google Scholar]
- 257.Kloos RT. 2009. Protecting thyroid cancer patients from untoward effects of radioactive iodine treatment. Thyroid 19:925–928 [DOI] [PubMed] [Google Scholar]
- 258.Lee SL. 2010. Complications of radioactive iodine treatment of thyroid carcinoma. J Natl Compr Canc Netw 8:1277–1286; quiz 1287. [DOI] [PubMed] [Google Scholar]
- 259.Klubo-Gwiezdzinska J, Van Nostrand D, Burman KD, Vasko V, Chia S, Deng T, Kulkarni K, Wartofsky L. 2010. Salivary gland malignancy and radioiodine therapy for thyroid cancer. Thyroid 20:647–651 [DOI] [PubMed] [Google Scholar]
- 260.Grewal RK, Larson SM, Pentlow CE, Pentlow KS, Gonen M, Qualey R, Natbony L, Tuttle RM. 2009. Salivary gland side effects commonly develop several weeks after initial radioactive iodine ablation. J Nucl Med 50:1605–1610 [DOI] [PubMed] [Google Scholar]
- 261.Schlumberger M, Catargi B, Borget I, Deandreis D, Zerdoud S, Bridji B, Bardet S, Leenhardt L, Bastie D, Schvartz C, Vera P, Morel O, Benisvy D, Bournaud C, Bonichon F, Dejax C, Toubert ME, Leboulleux S, Ricard M, Benhamou E. 2012. Strategies of radioiodine ablation in patients with low-risk thyroid cancer. N Engl J Med 366:1663–1673 [DOI] [PubMed] [Google Scholar]
- 262.Sawka AM, Lakra DC, Lea J, Alshehri B, Tsang RW, Brierley JD, Straus S, Thabane L, Gafni A, Ezzat S, George SR, Goldstein DP. 2008. A systematic review examining the effects of therapeutic radioactive iodine on ovarian function and future pregnancy in female thyroid cancer survivors. Clin Endocrinol 69:479–490 [DOI] [PubMed] [Google Scholar]
- 263.Sawka AM, Lea J, Alshehri B, Straus S, Tsang RW, Brierley JD, Thabane L, Rotstein L, Gafni A, Ezzat S, Goldstein DP. 2008. A systematic review of the gonadal effects of therapeutic radioactive iodine in male thyroid cancer survivors. Clin Endocrinol 68:610–617 [DOI] [PubMed] [Google Scholar]
- 264.Rosario PW, Barroso AL, Rezende LL, Padrao EL, Borges MA, Guimaraes VC, Purisch S. 2006. Testicular function after radioiodine therapy in patients with thyroid cancer. Thyroid 16:667–670 [DOI] [PubMed] [Google Scholar]
- 265.Edmonds CJ, Smith T. 1986. The long-term hazards of the treatment of thyroid cancer with radioiodine. Br J Radiol 59:45–51 [DOI] [PubMed] [Google Scholar]
- 266.Hyer S, Vini L, O'Connell M, Pratt B, Harmer C. 2002. Testicular dose and fertility in men following I(131) therapy for thyroid cancer. Clin Endocrinol 56:755–758 [DOI] [PubMed] [Google Scholar]
- 267.Wallace WH. 2011. Oncofertility and preservation of reproductive capacity in children and young adults. Cancer 117:2301–2310 [DOI] [PubMed] [Google Scholar]
- 268.Pacini F, Gasperi M, Fugazzola L, Ceccarelli C, Lippi F, Centoni R, Martino E, Pinchera A. 1994. Testicular function in patients with differentiated thyroid carcinoma treated with radioiodine. J Nucl Med 35:1418–1422 [PubMed] [Google Scholar]
- 269.Vini L, Hyer S, Al-Saadi A, Pratt B, Harmer C. 2002. Prognosis for fertility and ovarian function after treatment with radioiodine for thyroid cancer. Postgrad Med J 78:92–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Smith MB, Xue H, Takahashi H, Cangir A, Andrassy RJ. 1994. Iodine 131 thyroid ablation in female children and adolescents: long-term risk of infertility and birth defects. Ann Surg Oncol 1:128–131 [DOI] [PubMed] [Google Scholar]
- 271.Garsi JP, Schlumberger M, Rubino C, Ricard M, Labbe M, Ceccarelli C, Schvartz C, Henri-Amar M, Bardet S, de Vathaire F. 2008. Therapeutic administration of 131I for differentiated thyroid cancer: radiation dose to ovaries and outcome of pregnancies. J Nucl Med 49:845–852 [DOI] [PubMed] [Google Scholar]
- 272.Casara D, Rubello D, Saladini G, Piotto A, Pelizzo MR, Girelli ME, Busnardo B. 1993. Pregnancy after high therapeutic doses of iodine-131 in differentiated thyroid cancer: potential risks and recommendations. Eur J Nucl Med 20:192–194 [DOI] [PubMed] [Google Scholar]
- 273.Verburg FA, Hanscheid H, Biko J, Hategan MC, Lassmann M, Kreissl MC, Reiners C, Luster M. 2010. Dosimetry-guided high-activity (131)I therapy in patients with advanced differentiated thyroid carcinoma: initial experience. Eur J Nucl Med Mol Imaging 37:896–903 [DOI] [PubMed] [Google Scholar]
- 274.Van Nostrand D, Neutze J, Atkins F. 1986. Side effects of “rational dose” iodine-131 therapy for metastatic well-differentiated thyroid carcinoma. J Nucl Med 27:1519–1527 [PubMed] [Google Scholar]
- 275.Baugnet-Mahieu L, Lemaire M, Leonard ED, Leonard A, Gerber GB. 1994. Chromosome aberrations after treatment with radioactive iodine for thyroid cancer. Radiat Res 140:429–431 [PubMed] [Google Scholar]
- 276.Puerto S, Marcos R, Ramirez MJ, Galofre P, Creus A, Surralles J. 2000. Equal induction and persistence of chromosome aberrations involving chromosomes 1, 4 and 10 in thyroid cancer patients treated with radioactive iodine. Mutat Res 469:147–158 [DOI] [PubMed] [Google Scholar]
- 277.Richter HE, Lohrer HD, Hieber L, Kellerer AM, Lengfelder E, Bauchinger M. 1999. Microsatellite instability and loss of heterozygosity in radiation-associated thyroid carcinomas of Belarussian children and adults. Carcinogenesis 20:2247–2252 [DOI] [PubMed] [Google Scholar]
- 278.Frigo A, Dardano A, Danese E, Davi MV, Moghetti P, Colato C, Francia G, Bernardi F, Traino C, Monzani F, Ferdeghini M. 2009. Chromosome translocation frequency after radioiodine thyroid remnant ablation: a comparison between recombinant human thyrotropin stimulation and prolonged levothyroxine withdrawal. J Clin Endocrinol Metab 94:3472–3476 [DOI] [PubMed] [Google Scholar]
- 279.Thompson GB, Hay ID. 2004. Current strategies for surgical management and adjuvant treatment of childhood papillary thyroid carcinoma. World J Surg 28:1187–1198 [DOI] [PubMed] [Google Scholar]
- 280.Robbins RJ, Srivastava S, Shaha A, Ghossein R, Larson SM, Fleisher M, Tuttle RM. 2004. Factors influencing the basal and recombinant human thyrotropin-stimulated serum thyroglobulin in patients with metastatic thyroid carcinoma. J Clin Endocrinol Metab 89:6010–6016 [DOI] [PubMed] [Google Scholar]
- 281.Mazzaferri EL, Robbins RJ, Spencer CA, Braverman LE, Pacini F, Wartofsky L, Haugen BR, Sherman SI, Cooper DS, Braunstein GD, Lee S, Davies TF, Arafah BM, Ladenson PW, Pinchera A. 2003. A consensus report of the role of serum thyroglobulin as a monitoring method for low-risk patients with papillary thyroid carcinoma. J Clin Endocrinol Metab 88:1433–1441 [DOI] [PubMed] [Google Scholar]
- 282.Eustatia-Rutten CF, Smit JW, Romijn JA, van der Kleij-Corssmit EP, Pereira AM, Stokkel MP, Kievit J. 2004. Diagnostic value of serum thyroglobulin measurements in the follow-up of differentiated thyroid carcinoma, a structured meta-analysis. Clin Endocrinol 61:61–74 [DOI] [PubMed] [Google Scholar]
- 283.Durante C, Costante G, Filetti S. 2013. Differentiated thyroid carcinoma: defining new paradigms for postoperative management. Endocr Relat Cancer 20:R141–154 [DOI] [PubMed] [Google Scholar]
- 284.Mazzaferri EL, Massoll N. 2002. Management of papillary and follicular (differentiated) thyroid cancer: new paradigms using recombinant human thyrotropin. Endocr Relat Cancer 9:227–247 [DOI] [PubMed] [Google Scholar]
- 285.Robbins RJ, Chon JT, Fleisher M, Larson SM, Tuttle RM. 2002. Is the serum thyroglobulin response to recombinant human thyrotropin sufficient, by itself, to monitor for residual thyroid carcinoma? J Clin Endocrinol Metab 87:3242–3247 [DOI] [PubMed] [Google Scholar]
- 286.Pacini F, Molinaro E, Castagna MG, Agate L, Elisei R, Ceccarelli C, Lippi F, Taddei D, Grasso L, Pinchera A. 2003. Recombinant human thyrotropin-stimulated serum thyroglobulin combined with neck ultrasonography has the highest sensitivity in monitoring differentiated thyroid carcinoma. J Clin Endocrinol Metab 88:3668–3673 [DOI] [PubMed] [Google Scholar]
- 287.Kloos RT, Mazzaferri EL. 2005. A single recombinant human thyrotropin-stimulated serum thyroglobulin measurement predicts differentiated thyroid carcinoma metastases three to five years later. J Clin Endocrinol Metab 90:5047–5057 [DOI] [PubMed] [Google Scholar]
- 288.McClellan DR, Francis GL. 1996. Thyroid cancer in children, pregnant women, and patients with Graves' disease. Endocrinol Metab Clin North Am 25:27–48 [DOI] [PubMed] [Google Scholar]
- 289.Hanscheid H, Verburg FA, Biko J, Diessl S, Demidchik YE, Drozd V, Reiners C. 2011. Success of the postoperative 131I therapy in young Belarusian patients with differentiated thyroid cancer after Chernobyl depends on the radiation absorbed dose to the blood and the thyroglobulin level. Eur J Nucl Med Mol Imaging 38:1296–1302 [DOI] [PubMed] [Google Scholar]
- 290.Schlumberger M, Berg G, Cohen O, Duntas L, Jamar F, Jarzab B, Limbert E, Lind P, Pacini F, Reiners C, Sanchez Franco F, Toft A, Wiersinga WM. 2004. Follow-up of low-risk patients with differentiated thyroid carcinoma: a European perspective. Eur J Endocrinol 150:105–112 [DOI] [PubMed] [Google Scholar]
- 291.Kloos RT. 2010. Thyroid cancer recurrence in patients clinically free of disease with undetectable or very low serum thyroglobulin values. J Clin Endocrinol Metab 95:5241–5248 [DOI] [PubMed] [Google Scholar]
- 292.Malandrino P, Latina A, Marescalco S, Spadaro A, Regalbuto C, Fulco RA, Scollo C, Vigneri R, Pellegriti G. 2011. Risk-adapted management of differentiated thyroid cancer assessed by a sensitive measurement of basal serum thyroglobulin. J Clin Endocrinol Metab 96:1703–1709 [DOI] [PubMed] [Google Scholar]
- 293.Spencer C, Fatemi S, Singer P, Nicoloff J, Lopresti J. 2010. Serum basal thyroglobulin measured by a second-generation assay correlates with the recombinant human thyrotropin-stimulated thyroglobulin response in patients treated for differentiated thyroid cancer. Thyroid 20:587–595 [DOI] [PubMed] [Google Scholar]
- 294.Smallridge RC, Meek SE, Morgan MA, Gates GS, Fox TP, Grebe S, Fatourechi V. 2007. Monitoring thyroglobulin in a sensitive immunoassay has comparable sensitivity to recombinant human TSH-stimulated thyroglobulin in follow-up of thyroid cancer patients. J Clin Endocrinol Metab 92:82–87 [DOI] [PubMed] [Google Scholar]
- 295.Iervasi A, Iervasi G, Ferdeghini M, Solimeo C, Bottoni A, Rossi L, Colato C, Zucchelli GC. 2007. Clinical relevance of highly sensitive Tg assay in monitoring patients treated for differentiated thyroid cancer. Clin Endocrinol 67:434–441 [DOI] [PubMed] [Google Scholar]
- 296.Schlumberger M, Hitzel A, Toubert ME, Corone C, Troalen F, Schlageter MH, Claustrat F, Koscielny S, Taieb D, Toubeau M, Bonichon F, Borson-Chazot F, Leenhardt L, Schvartz C, Dejax C, Brenot-Rossi I, Torlontano M, Tenenbaum F, Bardet S, Bussiere F, Girard JJ, Morel O, Schneegans O, Schlienger JL, Prost A, So D, Archambeaud F, Ricard M, Benhamou E. 2007. Comparison of seven serum thyroglobulin assays in the follow-up of papillary and follicular thyroid cancer patients. J Clin Endocrinol Metab 92:2487–2495 [DOI] [PubMed] [Google Scholar]
- 297.Chindris AM, Diehl NN, Crook JE, Fatourechi V, Smallridge RC. 2012. Undetectable sensitive serum thyroglobulin (<0.1 ng/mL) in 163 patients with follicular cell-derived thyroid cancer: results of rhTSH stimulation and neck ultrasonography and long-term biochemical and clinical follow-up. J Clin Endocrinol Metab 97:2714–2723 [DOI] [PubMed] [Google Scholar]
- 298.Castagna MG, Brilli L, Pilli T, Montanaro A, Cipri C, Fioravanti C, Sestini F, Capezzone M, Pacini F. 2008. Limited value of repeat recombinant human thyrotropin (rhTSH)-stimulated thyroglobulin testing in differentiated thyroid carcinoma patients with previous negative rhTSH-stimulated thyroglobulin and undetectable basal serum thyroglobulin levels. J Clin Endocrinol Metab 93:76–81 [DOI] [PubMed] [Google Scholar]
- 299.Han JM, Kim WB, Yim JH, Kim WG, Kim TY, Ryu JS, Gong G, Sung TY, Yoon JH, Hong SJ, Kim EY, Shong YK. 2012. Long-term clinical outcome of differentiated thyroid cancer patients with undetectable stimulated thyroglobulin level one year after initial treatment. Thyroid 22:784–790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Klubo-Gwiezdzinska J, Burman KD, Van Nostrand D, Wartofsky L. 2011. Does an undetectable rhTSH-stimulated Tg level 12 months after initial treatment of thyroid cancer indicate remission? Clin Endocrinol 74:111–117 [DOI] [PubMed] [Google Scholar]
- 301.Baudin E, Do Cao C, Cailleux AF, Leboulleux S, Travagli JP, Schlumberger M. 2003. Positive predictive value of serum thyroglobulin levels, measured during the first year of follow-up after thyroid hormone withdrawal, in thyroid cancer patients. J Clin Endocrinol Metab 88:1107–1111 [DOI] [PubMed] [Google Scholar]
- 302.Padovani RP, Robenshtok E, Brokhin M, Tuttle RM. 2012. Even without additional therapy, serum thyroglobulin concentrations often decline for years after total thyroidectomy and radioactive remnant ablation in patients with differentiated thyroid cancer. Thyroid 22:778–783 [DOI] [PubMed] [Google Scholar]
- 303.Schaap J, Eustatia-Rutten CF, Stokkel M, Links TP, Diamant M, van der Velde EA, Romijn JA, Smit JW. 2002. Does radioiodine therapy have disadvantageous effects in non-iodine accumulating differentiated thyroid carcinoma? Clin Endocrinol 57:117–124 [DOI] [PubMed] [Google Scholar]
- 304.Schaadt B, Feldt-Rasmussen U, Rasmusson B, Torring H, Foder B, Jorgensen K, Hansen HS. 1995. Assessment of the influence of thyroglobulin (Tg) autoantibodies and other interfering factors on the use of serum Tg as tumor marker in differentiated thyroid carcinoma. Thyroid 5:165–170 [DOI] [PubMed] [Google Scholar]
- 305.Miyauchi A, Kudo T, Miya A, Kobayashi K, Ito Y, Takamura Y, Higashiyama T, Fukushima M, Kihara M, Inoue H, Tomoda C, Yabuta T, Masuoka H. 2011. Prognostic impact of serum thyroglobulin doubling-time under thyrotropin suppression in patients with papillary thyroid carcinoma who underwent total thyroidectomy. Thyroid 21:707–716 [DOI] [PubMed] [Google Scholar]
- 306.Spencer CA. 2013. Commentary on: Implications of thyroglobulin antibody positivity in patients with differentiated thyroid cancer: a clinical position paper. Thyroid 23:1190–1192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Verburg FA, Luster M, Cupini C, Chiovato L, Duntas L, Elisei R, Feldt-Rasmussen U, Rimmele H, Seregni E, Smit JW, Theimer C, Giovanella L. 2013. Implications of thyroglobulin antibody positivity in patients with differentiated thyroid cancer: a clinical position statement. Thyroid 23:1211–1225 [DOI] [PubMed] [Google Scholar]
- 308.Schneider AB, Pervos R. 1978. Radioimmunoassay of human thyroglobulin: effect of antithyroglobulin autoantibodies. J Clin Endocrinol Metab 47:126–137 [DOI] [PubMed] [Google Scholar]
- 309.Feldt-Rasmussen U, Rasmussen AK. 1985. Serum thyroglobulin (Tg) in presence of thyroglobulin autoantibodies (TgAb). Clinical and methodological relevance of the interaction between Tg and TgAb in vitro and in vivo. J Endocrinol Invest 8:571–576 [DOI] [PubMed] [Google Scholar]
- 310.Spencer CA. 2011. Clinical utility of thyroglobulin antibody (TgAb) measurements for patients with differentiated thyroid cancers (DTC). J Clin Endocrinol Metab 96:3615–3627 [DOI] [PubMed] [Google Scholar]
- 311.Hoofnagle AN, Roth MY. 2013. Clinical review: improving the measurement of serum thyroglobulin with mass spectrometry. J Clin Endocrinol Metab 98:1343–1352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Spencer CA, Takeuchi M, Kazarosyan M, Wang CC, Guttler RB, Singer PA, Fatemi S, LoPresti JS, Nicoloff JT. 1998. Serum thyroglobulin autoantibodies: prevalence, influence on serum thyroglobulin measurement, and prognostic significance in patients with differentiated thyroid carcinoma. J Clin Endocrinol Metab 83:1121–1127 [DOI] [PubMed] [Google Scholar]
- 313.Chung JK, Park YJ, Kim TY, So Y, Kim SK, Park DJ, Lee DS, Lee MC, Cho BY. 2002. Clinical significance of elevated level of serum antithyroglobulin antibody in patients with differentiated thyroid cancer after thyroid ablation. Clin Endocrinol 57:215–221 [DOI] [PubMed] [Google Scholar]
- 314.Gorges R, Maniecki M, Jentzen W, Sheu SN, Mann K, Bockisch A, Janssen OE. 2005. Development and clinical impact of thyroglobulin antibodies in patients with differentiated thyroid carcinoma during the first 3 years after thyroidectomy. Eur J Endocrinol 153:49–55 [DOI] [PubMed] [Google Scholar]
- 315.Kim WG, Yoon JH, Kim WB, Kim TY, Kim EY, Kim JM, Ryu JS, Gong G, Hong SJ, Shong YK. 2008. Change of serum antithyroglobulin antibody levels is useful for prediction of clinical recurrence in thyroglobulin-negative patients with differentiated thyroid carcinoma. J Clin Endocrinol Metab 93:4683–4689 [DOI] [PubMed] [Google Scholar]
- 316.Seo JH, Lee SW, Ahn BC, Lee J. 2010. Recurrence detection in differentiated thyroid cancer patients with elevated serum level of antithyroglobulin antibody: special emphasis on using (18)F-FDG PET/CT. Clin Endocrinol 72:558–563 [DOI] [PubMed] [Google Scholar]
- 317.Chiovato L, Latrofa F, Braverman LE, Pacini F, Capezzone M, Masserini L, Grasso L, Pinchera A. 2003. Disappearance of humoral thyroid autoimmunity after complete removal of thyroid antigens. Ann Intern Med 139:346–351 [DOI] [PubMed] [Google Scholar]
- 318.Kumar A, Shah DH, Shrihari U, Dandekar SR, Vijayan U, Sharma SM. 1994. Significance of antithyroglobulin autoantibodies in differentiated thyroid carcinoma. Thyroid 4:199–202 [DOI] [PubMed] [Google Scholar]
- 319.Powers PA, Dinauer CA, Tuttle RM, Francis GL. 2003. Treatment of recurrent papillary thyroid carcinoma in children and adolescents. J Pediatr Endocrinol Metab 16:1033–1040 [DOI] [PubMed] [Google Scholar]
- 320.Kloos RT. 2008. Approach to the patient with a positive serum thyroglobulin and a negative radioiodine scan after initial therapy for differentiated thyroid cancer. J Clin Endocrinol Metab 93:1519–1525 [DOI] [PubMed] [Google Scholar]
- 321.Podoloff DA, Ball DW, Ben-Josef E, Benson AB, 3rd, Cohen SJ, Coleman RE, Delbeke D, Ho M, Ilson DH, Kalemkerian GP, Lee RJ, Loeffler JS, Macapinlac HA, Morgan RJ, Jr, Siegel BA, Singhal S, Tyler DS, Wong RJ. 2009. NCCN task force: clinical utility of PET in a variety of tumor types. J Natl Compr Canc Netw 7 Suppl 2:S1–26 [DOI] [PubMed] [Google Scholar]
- 322.Dong MJ, Liu ZF, Zhao K, Ruan LX, Wang GL, Yang SY, Sun F, Luo XG. 2009. Value of 18F-FDG-PET/PET-CT in differentiated thyroid carcinoma with radioiodine-negative whole-body scan: a meta-analysis. Nucl Med Commun 30:639–650 [DOI] [PubMed] [Google Scholar]
- 323.Miller ME, Chen Q, Elashoff D, Abemayor E, St John M. 2011. Positron emission tomography and positron emission tomography-CT evaluation for recurrent papillary thyroid carcinoma: meta-analysis and literature review. Head Neck 33:562–565 [DOI] [PubMed] [Google Scholar]
- 324.Bannas P, Derlin T, Groth M, Apostolova I, Adam G, Mester J, Klutmann S. 2012. Can (18)F-FDG-PET/CT be generally recommended in patients with differentiated thyroid carcinoma and elevated thyroglobulin levels but negative I-131 whole body scan? Ann Nucl Med 26:77–85 [DOI] [PubMed] [Google Scholar]
- 325.Esteva D, Muros MA, Llamas-Elvira JM, Jimenez Alonso J, Villar JM, Lopez de la Torre M, Muros T. 2009. Clinical and pathological factors related to 18F-FDG-PET positivity in the diagnosis of recurrence and/or metastasis in patients with differentiated thyroid cancer. Ann Surg Oncol 16:2006–2013 [DOI] [PubMed] [Google Scholar]
- 326.Treglia G, Muoio B, Giovanella L, Salvatori M. 2013. The role of positron emission tomography and positron emission tomography/computed tomography in thyroid tumours: an overview. Eur Arch Otorhinolaryngol 270:1783–1787 [DOI] [PubMed] [Google Scholar]
- 327.Robbins RJ, Wan Q, Grewal RK, Reibke R, Gonen M, Strauss HW, Tuttle RM, Drucker W, Larson SM. 2006. Real-time prognosis for metastatic thyroid carcinoma based on 2-[18F]fluoro-2-deoxy-D-glucose-positron emission tomography scanning. J Clin Endocrinol Metab 91:498–505 [DOI] [PubMed] [Google Scholar]
- 328.Mirallie E, Guillan T, Bridji B, Resche I, Rousseau C, Ansquer C, Bodet-Milin C, Curtet C, Carnaille B, Murat A, Charbonnel B, Kraeber-Bodere F. 2007. Therapeutic impact of 18FDG-PET/CT in the management of iodine-negative recurrence of differentiated thyroid carcinoma. Surgery 142:952–958; discussion 952–958. [DOI] [PubMed] [Google Scholar]
- 329.Shammas A, Degirmenci B, Mountz JM, McCook BM, Branstetter B, Bencherif B, Joyce JM, Carty SE, Kuffner HA, Avril N. 2007. 18F-FDG PET/CT in patients with suspected recurrent or metastatic well-differentiated thyroid cancer. J Nucl Med 48:221–226 [PubMed] [Google Scholar]
- 330.Wang W, Larson SM, Tuttle RM, Kalaigian H, Kolbert K, Sonenberg M, Robbins RJ. 2001. Resistance of [18F]-fluorodeoxyglucose-avid metastatic thyroid cancer lesions to treatment with high-dose radioactive iodine. Thyroid 11:1169–1175 [DOI] [PubMed] [Google Scholar]
- 331.Armstrong S, Worsley D, Blair GK. 2002. Pediatric surgical images: PET evaluation of papillary thyroid carcinoma recurrence. J Pediatr Surg 37:1648–1649 [DOI] [PubMed] [Google Scholar]
- 332.Kim WG, Ryu JS, Kim EY, Lee JH, Baek JH, Yoon JH, Hong SJ, Kim ES, Kim TY, Kim WB, Shong YK. 2010. Empiric high-dose 131-iodine therapy lacks efficacy for treated papillary thyroid cancer patients with detectable serum thyroglobulin, but negative cervical sonography and 18F-fluorodeoxyglucose positron emission tomography scan. J Clin Endocrinol Metab 95:1169–1173 [DOI] [PubMed] [Google Scholar]
- 333.Rosario PW, Mourao GF, Dos Santos JB, Calsolari MR. 2014. Is empirical radioactive iodine therapy still a valid approach to patients with thyroid cancer and elevated thyroglobulin? Thyroid 24:533–536 [DOI] [PubMed] [Google Scholar]
- 334.Hurley JR. 2011. Historical note: TSH suppression for thyroid cancer. Thyroid 21:1175–1176 [DOI] [PubMed] [Google Scholar]
- 335.Biondi B, Filetti S, Schlumberger M. 2005. Thyroid-hormone therapy and thyroid cancer: a reassessment. Nat Clin Pract Endocrinol Metab 1:32–40 [DOI] [PubMed] [Google Scholar]
- 336.Cooper DS, Specker B, Ho M, Sperling M, Ladenson PW, Ross DS, Ain KB, Bigos ST, Brierley JD, Haugen BR, Klein I, Robbins J, Sherman SI, Taylor T, Maxon HR., 3rd 1998. Thyrotropin suppression and disease progression in patients with differentiated thyroid cancer: results from the National Thyroid Cancer Treatment Cooperative Registry. Thyroid 8:737–744 [DOI] [PubMed] [Google Scholar]
- 337.Leboulleux S, Baudin E, Hartl DW, Travagli JP, Schlumberger M. 2005. Follicular cell-derived thyroid cancer in children. Horm Res 63:145–151 [DOI] [PubMed] [Google Scholar]
- 338.Rivkees SA. 2010. Pediatric Graves' disease: controversies in management. Horm Res Paediatr 74:305–311 [DOI] [PubMed] [Google Scholar]
- 339.Bauer AJ. 2011. Approach to the pediatric patient with Graves' disease: when is definitive therapy warranted? J Clin Endocrinol Metab 96:580–588 [DOI] [PubMed] [Google Scholar]
- 340.Clayman GL, Agarwal G, Edeiken BS, Waguespack SG, Roberts DB, Sherman SI. 2011. Long-term outcome of comprehensive central compartment dissection in patients with recurrent/persistent papillary thyroid carcinoma. Thyroid 21:1309–1316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Clayman GL, Shellenberger TD, Ginsberg LE, Edeiken BS, El-Naggar AK, Sellin RV, Waguespack SG, Roberts DB, Mishra A, Sherman SI. 2009. Approach and safety of comprehensive central compartment dissection in patients with recurrent papillary thyroid carcinoma. Head Neck 31:1152–1163 [DOI] [PubMed] [Google Scholar]
- 342.Hindie E, Melliere D, Lange F, Hallaj I, de Labriolle-Vaylet C, Jeanguillaume C, Lange J, Perlemuter L, Askienazy S. 2003. Functioning pulmonary metastases of thyroid cancer: does radioiodine influence the prognosis? Eur J Nucl Med Mol Imaging 30:974–981 [DOI] [PubMed] [Google Scholar]
- 343.Dottorini ME, Vignati A, Mazzucchelli L, Lomuscio G, Colombo L. 1997. Differentiated thyroid carcinoma in children and adolescents: a 37-year experience in 85 patients. J Nucl Med 38:669–675 [PubMed] [Google Scholar]
- 344.Samuel AM, Rajashekharrao B, Shah DH. 1998. Pulmonary metastases in children and adolescents with well-differentiated thyroid cancer. J Nucl Med 39:1531–1536 [PubMed] [Google Scholar]
- 345.Hebestreit H, Biko J, Drozd V, Demidchik Y, Burkhardt A, Trusen A, Beer M, Reiners C. 2011. Pulmonary fibrosis in youth treated with radioiodine for juvenile thyroid cancer and lung metastases after Chernobyl. Eur J Nucl Med Mol Imaging 38:1683–1690 [DOI] [PubMed] [Google Scholar]
- 346.Reiners C, Biko J, Haenscheid H, Hebestreit H, Kirinjuk S, Baranowski O, Marlowe RJ, Demidchik E, Drozd V, Demidchik Y. 2013. Twenty-five years after Chernobyl: outcome of radioiodine treatment in children and adolescents with very high-risk radiation-induced differentiated thyroid carcinoma. J Clin Endocrinol Metab 98:3039–3048 [DOI] [PubMed] [Google Scholar]
- 347.Chen L, Shen Y, Luo Q, Yu Y, Lu H, Zhu R. 2010. Pulmonary fibrosis following radioiodine therapy of pulmonary metastases from differentiated thyroid carcinoma. Thyroid 20:337–340 [DOI] [PubMed] [Google Scholar]
- 348.Lee J, Sogutlu G, Leard L, Zarnegar R, Bailey J, Golden J, Hays S, Kebebew E, Duh QY, Clark O. 2007. Lung transplantation for pulmonary metastases and radiation-induced pulmonary fibrosis after radioactive iodine ablation of extensive lung metastases from papillary thyroid carcinoma. Thyroid 17:367–369 [DOI] [PubMed] [Google Scholar]
- 349.Verburg FA, Reiners C, Hanscheid H. 2013. Approach to the patient: role of dosimetric RAI Rx in children with DTC. J Clin Endocrinol Metab 98:3912–3919 [DOI] [PubMed] [Google Scholar]
- 350.Argiris A, Agarwala SS, Karamouzis MV, Burmeister LA, Carty SE. 2008. A phase II trial of doxorubicin and interferon alpha 2b in advanced, non-medullary thyroid cancer. Invest New Drugs 26:183–188 [DOI] [PubMed] [Google Scholar]
- 351.Sherman SI. 2010. Cytotoxic chemotherapy for differentiated thyroid carcinoma. Clin Oncol (R Coll Radiol) 22:464–468 [DOI] [PubMed] [Google Scholar]
- 352.Haugen BR, Sherman SI. 2013. Evolving approaches to patients with advanced differentiated thyroid cancer. Endocr Rev 34:439–455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Waguespack SG, Sherman SI, Williams MD, Clayman GL, Herzog CE. 2009. The successful use of sorafenib to treat pediatric papillary thyroid carcinoma. Thyroid 19:407–412 [DOI] [PubMed] [Google Scholar]
- 354.Iyer P, Mayer JL, Ewig JM. 2014. Response to sorafenib in a pediatric patient with papillary thyroid carcinoma with diffuse nodular pulmonary disease requiring mechanical ventilation. Thyroid 24:169–174 [DOI] [PubMed] [Google Scholar]
- 355.Brose MS, Nutting CM, Jarzab B, Elisei R, Siena S, Bastholt L, de la Fouchardiere C, Pacini F, Paschke R, Shong YK, Sherman SI, Smit JW, Chung J, Kappeler C, Pena C, Molnar I, Schlumberger MJ, investigators D. 2014. Sorafenib in radioactive iodine-refractory, locally advanced or metastatic differentiated thyroid cancer: a randomised, double-blind, phase 3 trial. Lancet 384:319–328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Schlumberger M, Tahara M, Wirth LJ, Robinson B, Brose MS, Elisei R, Habra MA, Newbold K, Shah MH, Hoff AO, Gianoukakis AG, Kiyota N, Taylor MH, Kim SB, Krzyzanowska MK, Dutcus CE, de las Heras B, Zhu J, Sherman SI. 2015. Lenvatinib versus placebo in radioiodine-refractory thyroid cancer. N Engl J Med 372:621–630 [DOI] [PubMed] [Google Scholar]
- 357.Carhill AA, Cabanillas ME, Jimenez C, Waguespack SG, Habra MA, Hu M, Ying A, Vassilopoulou-Sellin R, Gagel RF, Sherman SI, Busaidy NL. 2013. The noninvestigational use of tyrosine kinase inhibitors in thyroid cancer: establishing a standard for patient safety and monitoring. J Clin Endocrinol Metab 98:31–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.McHenry CR, Phitayakorn R. 2011. Follicular adenoma and carcinoma of the thyroid gland. Oncologist 16:585–593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Raval MV, Bentrem DJ, Stewart AK, Ko CY, Reynolds M. 2010. Utilization of total thyroidectomy for differentiated thyroid cancer in children. Ann Surg Oncol 17:2545–2553 [DOI] [PubMed] [Google Scholar]
- 360.Roy R, Kouniavsky G, Schneider E, Allendorf JD, Chabot JA, Logerfo P, Dackiw AP, Colombani P, Zeiger MA, Lee JA. 2011. Predictive factors of malignancy in pediatric thyroid nodules. Surgery 150:1228–1233 [DOI] [PubMed] [Google Scholar]
- 361.Otto KJ, Lam JS, MacMillan C, Freeman JL. 2010. Diminishing diagnosis of follicular thyroid carcinoma. Head Neck 32:1629–1634 [DOI] [PubMed] [Google Scholar]
- 362.Woodruff SL, Arowolo OA, Akute OO, Afolabi AO, Nwariaku F. 2010. Global variation in the pattern of differentiated thyroid cancer. Am J Surg 200:462–466 [DOI] [PubMed] [Google Scholar]
- 363.Mishra A, Mishra SK, Agarwal A, Das BK, Agarwal G, Gambhir S. 2002. Metastatic differentiated thyroid carcinoma: clinicopathological profile and outcome in an iodine deficient area. World J Surg 26:153–157 [DOI] [PubMed] [Google Scholar]
- 364.LiVolsi VA, Abrosimov AA, Bogdanova T, Fadda G, Hunt JL, Ito M, Rosai J, Thomas GA, Williams ED. 2011. The Chernobyl thyroid cancer experience: pathology. Clin Oncol (R Coll Radiol) 23:261–267 [DOI] [PubMed] [Google Scholar]
- 365.Lo CY, Lam KY, Wan KY. 2000. Insular thyroid carcinoma in adolescents. Eur J Surg 166:585–588 [DOI] [PubMed] [Google Scholar]
- 366.Yusuf K, Reyes-Mugica M, Carpenter TO. 2003. Insular carcinoma of the thyroid in an adolescent: a case report and review of the literature. Curr Opin Pediatr 15:512–515 [DOI] [PubMed] [Google Scholar]
- 367.DeLellis RA. 2006. Pathology and genetics of thyroid carcinoma. J Surg Oncol 94:662–669 [DOI] [PubMed] [Google Scholar]
- 368.Liaw D, Marsh DJ, Li J, Dahia PL, Wang SI, Zheng Z, Bose S, Call KM, Tsou HC, Peacocke M, Eng C, Parsons R. 1997. Germline mutations of the PTEN gene in Cowden disease, an inherited breast and thyroid cancer syndrome. Nat Genet 16:64–67 [DOI] [PubMed] [Google Scholar]
- 369.Nagy R, Ganapathi S, Comeras I, Peterson C, Orloff M, Porter K, Eng C, Ringel MD, Kloos RT. 2011. Frequency of germline PTEN mutations in differentiated thyroid cancer. Thyroid 21:505–510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Scholz S, Smith JR, Chaignaud B, Shamberger RC, Huang SA. 2011. Thyroid surgery at Children's Hospital Boston: a 35-year single-institution experience. J Pediatr Surg 46:437–442 [DOI] [PubMed] [Google Scholar]
- 371.Mester JL, Tilot AK, Rybicki LA, Frazier TW, 2nd, Eng C. 2011. Analysis of prevalence and degree of macrocephaly in patients with germline PTEN mutations and of brain weight in Pten knock-in murine model. Eur J Hum Genet 19:763–768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Sobrinho-Simoes M, Eloy C, Magalhaes J, Lobo C, Amaro T. 2011. Follicular thyroid carcinoma. Mod Pathol 24(Suppl 2):S10–S18 [DOI] [PubMed] [Google Scholar]
- 373.Dionigi G, Kraimps JL, Schmid KW, Hermann M, Sheu-Grabellus SY, De Wailly P, Beaulieu A, Tanda ML, Sessa F. 2014. Minimally invasive follicular thyroid cancer (MIFTC)-a consensus report of the European Society of Endocrine Surgeons (ESES). Langenbecks Arch Surg 399:165–184 [DOI] [PubMed] [Google Scholar]
- 374.Bongiovanni M, De Saussure B, Kumar N, Pache JC, Cibas ES. 2009. A quality control study on cytotechnologist-cytopathologist concordance and its relationship to the number of dots on the slide. Acta Cytol 53:653–658 [DOI] [PubMed] [Google Scholar]
- 375.Layfield LJ, Cibas ES, Gharib H, Mandel SJ. 2009. Thyroid aspiration cytology: current status. CA Cancer J Clin 59:99–110 [DOI] [PubMed] [Google Scholar]
- 376.Farahati J, Bucsky P, Parlowsky T, Mader U, Reiners C. 1997. Characteristics of differentiated thyroid carcinoma in children and adolescents with respect to age, gender, and histology. Cancer 80:2156–2162 [DOI] [PubMed] [Google Scholar]
- 377.Machens A, Holzhausen HJ, Dralle H. 2005. The prognostic value of primary tumor size in papillary and follicular thyroid carcinoma. Cancer 103:2269–2273 [DOI] [PubMed] [Google Scholar]
- 378.Thompson LD, Wieneke JA, Paal E, Frommelt RA, Adair CF, Heffess CS. 2001. A clinicopathologic study of minimally invasive follicular carcinoma of the thyroid gland with a review of the English literature. Cancer 91:505–524 [DOI] [PubMed] [Google Scholar]
- 379.Alfalah H, Cranshaw I, Jany T, Arnalsteen L, Leteurtre E, Cardot C, Pattou F, Carnaille B. 2008. Risk factors for lateral cervical lymph node involvement in follicular thyroid carcinoma. World J Surg 32:2623–2626 [DOI] [PubMed] [Google Scholar]
- 380.Tan C, Sidhu S, Sywak M, Delbridge L. 2009. Management of hyperfunctioning single thyroid nodules in the era of minimally invasive thyroid surgery. ANZ J Surg 79:386–389 [DOI] [PubMed] [Google Scholar]
- 381.Yalla NM, Reynolds LR. 2011. Hürthle cell thyroid carcinoma presenting as a “hot” nodule. Endocr Pract 17:e68–72 [DOI] [PubMed] [Google Scholar]
- 382.Croom RD, 3rd, Thomas CG, Jr, Reddick RL, Tawil MT. 1987. Autonomously functioning thyroid nodules in childhood and adolescence. Surgery 102:1101–1108 [PubMed] [Google Scholar]
- 383.Sugino K, Ito K, Nagahama M, Kitagawa W, Shibuya H, Ohkuwa K, Yano Y, Uruno T, Akaishi J, Kameyama K, Ito K. 2011. Prognosis and prognostic factors for distant metastases and tumor mortality in follicular thyroid carcinoma. Thyroid 21:751–757 [DOI] [PubMed] [Google Scholar]
- 384.Lin JD, Chao TC, Chen ST, Huang YY, Liou MJ, Hsueh C. 2007. Operative strategy for follicular thyroid cancer in risk groups stratified by pTNM staging. Surg Oncol 16:107–113 [DOI] [PubMed] [Google Scholar]
- 385.Kowalski LP, Goncalves Filho J, Pinto CA, Carvalho AL, de Camargo B. 2003. Long-term survival rates in young patients with thyroid carcinoma. Arch Otolaryngol Head Neck Surg 129:746–749 [DOI] [PubMed] [Google Scholar]
- 386.Lee YM, Lo CY, Lam KY, Wan KY, Tam PK. 2002. Well-differentiated thyroid carcinoma in Hong Kong Chinese patients under 21 years of age: a 35-year experience. J Am Coll Surg 194:711–716 [DOI] [PubMed] [Google Scholar]
- 387.Lang W, Choritz H, Hundeshagen H. 1986. Risk factors in follicular thyroid carcinomas. A retrospective follow-up study covering a 14-year period with emphasis on morphological findings. Am J Surg Pathol 10:246–255 [PubMed] [Google Scholar]
- 388.van Heerden JA, Hay ID, Goellner JR, Salomao D, Ebersold JR, Bergstralh EJ, Grant CS. 1992. Follicular thyroid carcinoma with capsular invasion alone: a nonthreatening malignancy. Surgery 112:1130–1136; discussion 1136–1138. [PubMed] [Google Scholar]
- 389.Lo CY, Chan WF, Lam KY, Wan KY. 2005. Follicular thyroid carcinoma: the role of histology and staging systems in predicting survival. Ann Surg 242:708–715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 390.D'Avanzo A, Treseler P, Ituarte PH, Wong M, Streja L, Greenspan FS, Siperstein AE, Duh QY, Clark OH. 2004. Follicular thyroid carcinoma: histology and prognosis. Cancer 100:1123–1129 [DOI] [PubMed] [Google Scholar]
- 391.Asari R, Koperek O, Scheuba C, Riss P, Kaserer K, Hoffmann M, Niederle B. 2009. Follicular thyroid carcinoma in an iodine-replete endemic goiter region: a prospectively collected, retrospectively analyzed clinical trial. Ann Surg 249:1023–1031 [DOI] [PubMed] [Google Scholar]
- 392.Sugino K, Kameyama K, Ito K, Nagahama M, Kitagawa W, Shibuya H, Ohkuwa K, Yano Y, Uruno T, Akaishi J, Suzuki A, Masaki C. 2012. Outcomes and prognostic factors of 251 patients with minimally invasive follicular thyroid carcinoma. Thyroid 22:798–804 [DOI] [PubMed] [Google Scholar]
- 393.Mai KT, Khanna P, Yazdi HM, Perkins DG, Veinot JP, Thomas J, Lamba M, Nair BD. 2002. Differentiated thyroid carcinomas with vascular invasion: a comparative study of follicular, Hürthle cell and papillary thyroid carcinoma. Pathology 34:239–244 [DOI] [PubMed] [Google Scholar]
- 394.Furlan JC, Bedard YC, Rosen IB. 2004. Clinicopathologic significance of histologic vascular invasion in papillary and follicular thyroid carcinomas. J Am Coll Surg 198:341–348 [DOI] [PubMed] [Google Scholar]
- 395.Tuttle RM, Ball DW, Byrd D, Dilawari RA, Doherty GM, Duh QY, Ehya H, Farrar WB, Haddad RI, Kandeel F, Kloos RT, Kopp P, Lamonica DM, Loree TR, Lydiatt WM, McCaffrey JC, Olson JA, Jr, Parks L, Ridge JA, Shah JP, Sherman SI, Sturgeon C, Waguespack SG, Wang TN, Wirth LJ. 2010. Thyroid carcinoma. J Natl Compr Canc Netw 8:1228–1274 [DOI] [PubMed] [Google Scholar]
- 396.Udelsman R, Westra WH, Donovan PI, Sohn TA, Cameron JL. 2001. Randomized prospective evaluation of frozen-section analysis for follicular neoplasms of the thyroid. Ann Surg 233:716–722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Massimo L, Zarri D, Caprino D. 2005. Psychosocial aspects of survivors of childhood cancer or leukemia. Minerva Pediatr 57:389–397 [PubMed] [Google Scholar]
- 398.Hullmann SE, Wolfe-Christensen C, Meyer WH, McNall-Knapp RY, Mullins LL. 2010. The relationship between parental overprotection and health-related quality of life in pediatric cancer: the mediating role of perceived child vulnerability. Qual Life Res 19:1373–1380 [DOI] [PubMed] [Google Scholar]
- 399.Singer S, Lincke T, Gamper E, Bhaskaran K, Schreiber S, Hinz A, Schulte T. 2012. Quality of life in patients with thyroid cancer compared with the general population. Thyroid 22:117–124 [DOI] [PubMed] [Google Scholar]
- 400.Vrijmoet-Wiersma CM, Egeler RM, Koopman HM, Bresters D, Norberg AL, Grootenhuis MA. 2010. Parental stress and perceived vulnerability at 5 and 10 years after pediatric SCT. Bone Marrow Transplant 45:1102–1108 [DOI] [PubMed] [Google Scholar]
- 401.Oren A, Benoit MA, Murphy A, Schulte F, Hamilton J. 2012. Quality of life and anxiety in adolescents with differentiated thyroid cancer. J Clin Endocrinol Metab 97:E1933–1937 [DOI] [PubMed] [Google Scholar]
- 402.Mostoufi-Moab S, Barakat LP, Bauer AJ. 2012. Quality of life in adolescent patients with differentiated thyroid cancer: moving beyond survival. J Clin Endocrinol Metab 97:3453–3456 [DOI] [PubMed] [Google Scholar]
- 403.Morris LF, Waguespack SG, Warneke CL, Ryu H, Ying AK, Anderson BJ, Sturgis EM, Clayman GL, Lee JE, Evans DB, Grubbs EG, Perrier ND. 2012. Long-term follow-up data may help manage patient and parent expectations for pediatric patients undergoing thyroidectomy. Surgery 152:1165–1171 [DOI] [PubMed] [Google Scholar]
- 404.Pinto BM, Floyd A. 2008. Theories underlying health promotion interventions among cancer survivors. Semin Oncol Nurs 24:153–163 [DOI] [PubMed] [Google Scholar]
- 405.Martins RK, McNeil DW. 2009. Review of Motivational Interviewing in promoting health behaviors. Clin Psychol Rev 29:283–293 [DOI] [PubMed] [Google Scholar]