Abstract
Purpose
Student-run free clinics (SRFCs) provide service–learning opportunities for medical students and care to underserved patients. Few published studies, however, support that they provide high-quality care. In this study, the authors examined the clinical impact of a medical student health educator program for diabetic patients at an SRFC.
Method
In 2012, the authors retrospectively reviewed the electronic medical records of diabetic patients who established care at Shade Tree Clinic in Nashville, Tennessee, between 2008 and 2011. They compared clinical outcomes at initial presentation to the clinic and 12 months later. They analyzed the relationship between the number of patient–student interactions (touchpoints) and change in hemoglobin A1c values between these two time points and compared the quality of care provided to best-practice benchmarks (process and outcomes measures).
Results
The authors studied data from 45 patients. Mean hemoglobin A1c values improved significantly from 9.6 to 7.9, after a mean of 12.5 ± 1.5 months (P < .0001). A trend emerged between increased number of touchpoints and improvement in A1c values (r2 = 0.06, P = .10). A high percentage of patients were screened during clinic visits, whereas a low to moderate percentage met benchmarks for A1c, LDL, and blood pressure levels.
Conclusions
These findings demonstrate that a medical student health educator program at an SRFC can provide high-quality diabetes care and facilitate clinical improvement one year after enrollment, despite inherent difficulties in caring for underserved patients. Future studies should examine the educational and clinical value of care provided at SRFCs.
Student-run free clinics (SRFCs) provide medical students with a valuable opportunity to enrich their clinical training while simultaneously providing care for medically underserved patients. These service–learning experiences play an increasingly important role in undergraduate medical education. In 2011, 71% of graduating medical students reported that they had participated in a free clinic activity during medical school.1 In addition, many medical schools are affiliated with one or more of the 111 SRFCs across the country.2 The preponderance of the current literature on medical student service–learning programs and SRFCs has focused on student learning. For example, participation in service–learning activities has been shown to enhance students’ clinical knowledge, empathy, professional development, cultural competency, communication skills, and exposure to primary care.3–10
However, although a reasonable assumption could be that otherwise medically underserved patients would gain clinical benefits from receiving care at SRFCs, few published reports support this notion. Although some studies have demonstrated that SRFCs can meet national care guidelines for chronic medical illnesses, surprisingly few have assessed longitudinal improvement in clinical outcomes.6,11–14 Without empirical data suggesting otherwise, a critic of SRFCs could reasonably propose that learning at these clinics is at the expense of service to patients. Ethically, the reciprocal nature of service–learning suggests that just as students benefit, so too should patients.
In the spirit of accountability, SRFCs have a responsibility to rigorously assess the quality of care they provide to patients.15,16 Moreover, in the modern era of data-rich and evidence-based medicine, to be consistent with contemporary best practices, SRFCs should assess their quality of care regularly. In this study, we examined the clinical impact of a medical student health educator program for diabetic patients at Shade Tree Clinic, an SRFC at Vanderbilt University School of Medicine.
To help meet the needs of an increasing number of patients with diabetes mellitus type 2 (DM2), Shade Tree Clinic developed the Patient Health Education (PHE) program in 2008. The goal of the program was to provide continuity of care via first- and second-year medical students who acted as diabetes health coaches. Since the program’s start, diabetic patients have been paired with a PHE student who serves as the patient’s individual case manager and provides individualized disease and nutrition counseling, laboratory follow-up communication, and referral coordination. PHE students interact with patients both inside the clinic (as part of the student care team) and outside it (via phone calls).
First-year medical students apply to participate in the PHE program and are selected on the basis of their demonstrated level of commitment and interest in the program and ability to establish rapport with patients. Prior to participating, students complete a structured training course in DM2 disease management facilitated by faculty and staff at Vanderbilt’s Eskind Diabetes Clinic. The training curriculum uses a mix of small-group interactive discussions as well as formal didactic sessions and focuses on diabetes pathophysiology, medications, complications, as well as health coaching strategies for encouraging patient adherence and empowerment. First-year students shadow second-year students in their interactions with patients for several months and then gradually assume responsibility for managing a panel of their own PHE patients as they become more comfortable interacting with them. Students meet weekly with an endocrinologist (M.J.F.) to review laboratory test results and monthly quality improvement reports, which detail outcome measures relative to established care goals. Students volunteer their time and do not receive school credit for participation.
PHE students function as points of contact for patients whenever they have questions regarding their disease management, explain a patient’s disease and optimal care, and provide continuity of care for patients who would otherwise potentially see a new student team and attending physician each time they visit the clinic. The PHE program aims to ensure regular follow-up every one to two months (or as needed, on a patient-by-patient basis). The program was initially developed to be diabetes-specific but has since evolved into a more generalized chronic disease care management program that also applies to patients with congestive heart failure, hypertension, hyperlipidemia, chronic obstructive pulmonary disease, and asthma.
To date, our anecdotal sense has been that the comprehensive care model of the PHE program enables our patients to achieve significant improvement in clinical outcomes. However, without a rigorous assessment, we lack the empirical data to support this notion. In this formal examination of the program’s clinical utility, we assessed the health outcomes of patients with DM2 who participated in our PHE program, the relationship between those outcomes and the amount of patient–student interaction, and our program’s process measures, comparing the quality of clinical care delivered to best-practice benchmarks.
Method
Study procedure
We used Shade Tree Clinic’s electronic patient registry, which includes all past and current patients, to identify those patients meeting the eligibility criteria described below. In 2012, two authors (A.P. and P.G.) abstracted data from the electronic medical records (EMRs) for all eligible patients. We stored these abstracted, deidentified data in a secure study database.
To start, we identified the first glycosylated hemoglobin A1c (A1c) lab value drawn in connection with each patient’s initial presentation to the clinic. We then recorded the month and year of this visit as Time-0 (T-0) and the A1c value as the T-0 A1c. To determine Time-1 (T-1), we looked in the EMR for visits 12 months after T-0 when another A1c test was done. Because we retrospectively examined clinical encounters, patients did not always visit the clinic exactly 12 months after T-0. Thus, we considered visits that were 12 ± 3 months after T-0 to be eligible as a T-1 visit.
To assess the patient–student relationship, we defined a touchpoint as a documented interaction in the patient’s EMR that focused on clinical care. Documented touchpoints included visits or phone calls regarding clinical care, health counseling or social work, visits for drawing labs or refilling medications, and phone calls regarding lab test results. Next, we assessed the EMR for defined process measures (the presence or absence of the measures within 12 months after T-0, independent of the number of months between T-0 and T-1) and outcome measures (the values of the measures at T-1).
The Vanderbilt University institutional review board approved the study’s protocol as an exempt research project. Because this study was a retrospective review of EMRs, neither the patients nor the students were aware of our study at the time of their participation in the PHE program, and informed consent was not required for participation.
Patient population
We reviewed EMRs for all patients who established care at Shade Tree Clinic after 2008 to assess their eligibility for inclusion in our study. Inclusion criteria were age 18 years or older; DM2 diagnosis (defined by either [1] an initial A1c ≥ 6.5 or [2] a patient-reported diagnosis of DM2 and concurrent prescription for insulin or a DM2-specific medication); first visit to Shade Tree Clinic to establish care between 2008 and 2011; enrolling in the PHE program after the first visit; and at least one subsequent visit to the clinic within 15 months, at which time an A1c lab was drawn. Exclusion criteria were gestational diabetes, diabetes mellitus type 1, and age less than 18 years.
Study setting
Operating within an urban community health clinic in Nashville, Tennessee, Shade Tree Clinic provides free medical care, medications, laboratory services, immunizations, social services, and disease management to nearly 400 uninsured and underserved patients annually. Grounded in the service–learning model, the clinic strives both to educate medical students and provide comprehensive primary and specialty care to patients.
In the 2011–2012 academic year, 286 preclinical and clinical students (65% of the Vanderbilt student body) volunteered at the clinic. At twice-weekly clinic sessions, teams of preclinical and clinical medical students work under the supervision of faculty providers. Bedside teaching during the clinical encounter is common, and structured educational activities include student-led preclinic “chalk talks” (small-group discussions of clinical topics relevant to patients scheduled in the clinic), faculty-led postclinic “wrap-up” discussions that afford students an opportunity to share interesting or particularly educational cases they saw in the clinic that day, weekly laboratory review sessions, quarterly case presentation series, and annual clinical skills workshops.
Data analysis
We managed our study data using REDCap, a secure, research-oriented, Web-based application.17 We computed all statistical analyses and data plots using SPSS version 19.0.1 (IBM, Somers, New York) and Prism version 5.0d (GraphPad, La Jolla, California).
We described participant characteristics using means and standard deviations (SDs) for continuous measures (age and months between T-0 and T-1) and percentages for nonparametric measures (sex, ethnicity, and race). Using a related-samples Wilcoxon signed rank test, we compared paired A1c values at T-0 and T-1. To examine the relationship between the number of touchpoints and change in A1c values between T-0 and T-1, we used linear regression, and we plotted data with best-fit lines and 95% confidence intervals (CIs). Finally, we described process and outcome measures by percentage of total cohort.
For all statistical tests, we considered a P value of less than .05 significant. Using G*Power version 3.1.7, we completed a power analysis to determine the sample size required to detect a meaningful change in A1c values between T-0 and T-1.18 With 80% power, an α of 5%, and a moderate effect size of 0.5, the minimum required sample size was 35 patients.19
Results
Patient characteristics
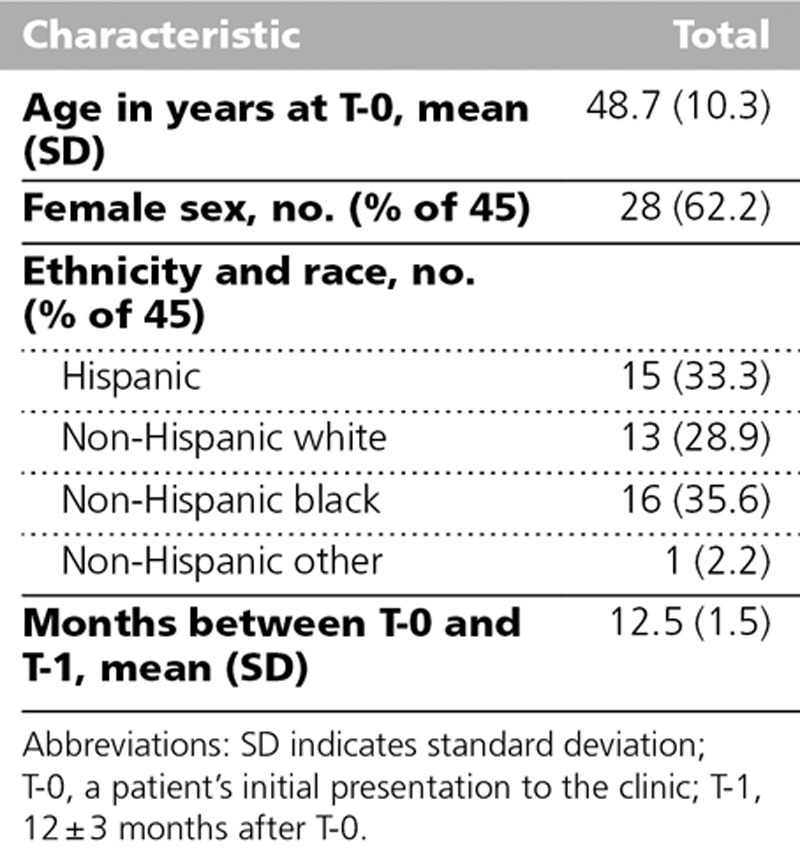
We abstracted data from the EMRs of 45 eligible patients (see Table 1). Patients had a mean age at T-0 of 48.7 ± 10.3 years. The cohort was 62.2% (28/45) female and primarily of three racial and ethnic backgrounds (33.3% [15/45] Hispanic, 28.9% [13/45] non-Hispanic white, and 35.6% [16/45] non-Hispanic black). The mean number of months between T-0 and T-1 was 12.5 ± 1.5.
Table 1.
Characteristics of 45 Diabetes Mellitus Type 2 Patients at the Shade Tree Clinic Whose Data Were Used in a Study of Clinical Outcomes at a Student-Run Free Clinic, 2008–2011
Change in A1c values between T-0 and T-1
To assess for improvement in glycemic control, we compared A1c values at T-0 and T-1 (see Figure 1). In a pairwise, nonparametric analysis, we found a significant difference in median A1c values between T-0 and T-1 (P < .0001). The mean change was 1.7 (95% CI 1.1–2.5), improving from a mean of 9.6 at T-0 to a mean of 7.9 at T-1.
Figure 1.
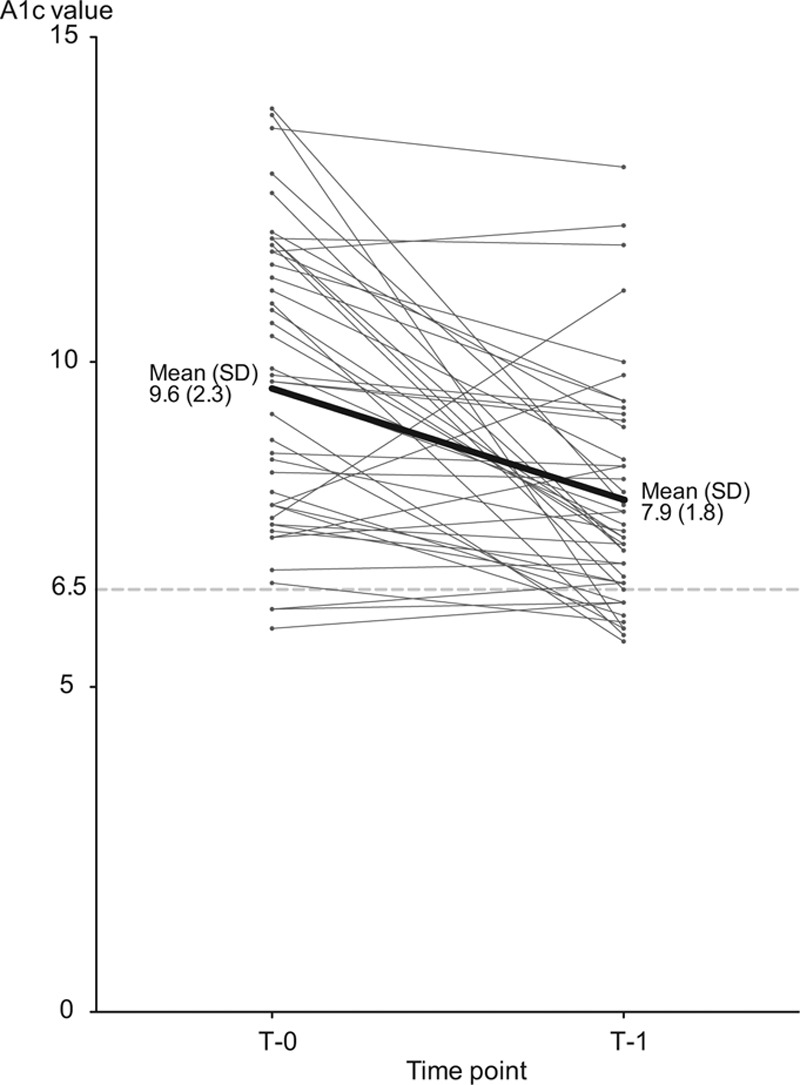
Change in hemoglobin A1c values from initial presentation to the Shade Tree Clinic (T-0) to 12 ± 3 months later (T-1). At T-0, the mean (standard deviation) A1c value was 9.6 (2.3); at T-1, it was 7.9 (1.8). A related-samples Wilcoxon signed rank test showed a significant difference in median A1c values at T-0 and T-1 (P < .0001). The mean change was 1.7 (95% confidence interval 1.1–2.5). The thin lines indicate individual patient’s A1c values, and the thick line indicates the mean value. The dotted line indicates the reference value of 6.5, which is the American Diabetes Association goal value.
Relationship of touchpoints and change in A1c values between T-0 and T-1
To determine whether a beneficial relationship existed between the number of patient–student clinical interactions and patients’ clinical outcomes, we performed linear regression analyses (see Figure 2). We used the average number of touchpoints per month (mean 1.3, SD 0.6) as an independent variable and change in A1c values between T-0 and T-1 as a dependent variable. Although we did not find a significant relationship between the number of touchpoints and change in A1c values (r2 = 0.06, P = .10), the data suggest a trend that more touchpoints correlate with more improvement in A1c values (see Figure 2).
Figure 2.

Relationship of the number of patient–student interactions (touchpoints) and change in hemoglobin A1c values between initial presentation to the Shade Tree Clinic (T-0) and 12 ± 3 months later (T-1). The data suggest a trend that more touchpoints correlate with more improvement in A1c values. Linear regression found a nonsignificant best-fit line relating the two variables (slope 0.97; 95% confidence interval −0.19 to 2.13; P = .10, r2 = 0.06). The Y axis shows the change in A1c values from T-0 to T-1, with positive values indicating improvement (mean 1.7, standard deviation 2.3). The X axis shows the average number of touchpoints per month (mean 1.3, standard deviation 0.6). The dotted reference line indicates no change in A1c values; the solid black line, the best-fit line; and the gray areas, the 95% confidence interval.
Process and outcome measures
To evaluate our PHE program for consistency with evidence-based best practices in caring for diabetic patients, we determined whether patients met a selected subset of American Diabetes Association (ADA) process and outcome measure benchmarks.20 We assessed our process measures at 12 months after T-0 to determine objectively how well we were able to meet standards of care within one year of a patient establishing care at our clinic (see Table 2).
Table 2.
Process Measures Assessing the Quality of Clinical Care Delivered to 45 Diabetes Mellitus Type 2 Patients at the Shade Tree Clinic Relative to Best-Practice Benchmarks, 2008–2011
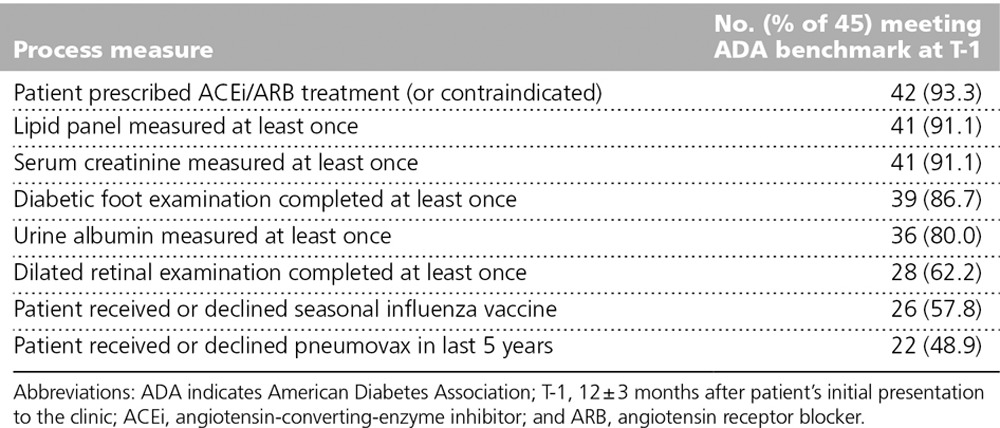
We found that a consistently high percentage of the total cohort was screened using laboratory tests during their clinic visits (from the lowest screening rate of 80.0% [36/45] for urine albumin to the highest screening rate of 91.1% [41/45] for serum creatinine and lipid levels). Our vaccination rates ranged from 48.9% (22/45) to 57.8% (26/45), and retinal (62.2%, 28/45) and foot (86.7%, 39/45) screening rates were modest and high, respectively. Finally, 93.3% (42/45) of patients were, when not clinically contraindicated, prescribed angiotensin-converting-enzyme inhibitor or angiotensin receptor blocker therapy.
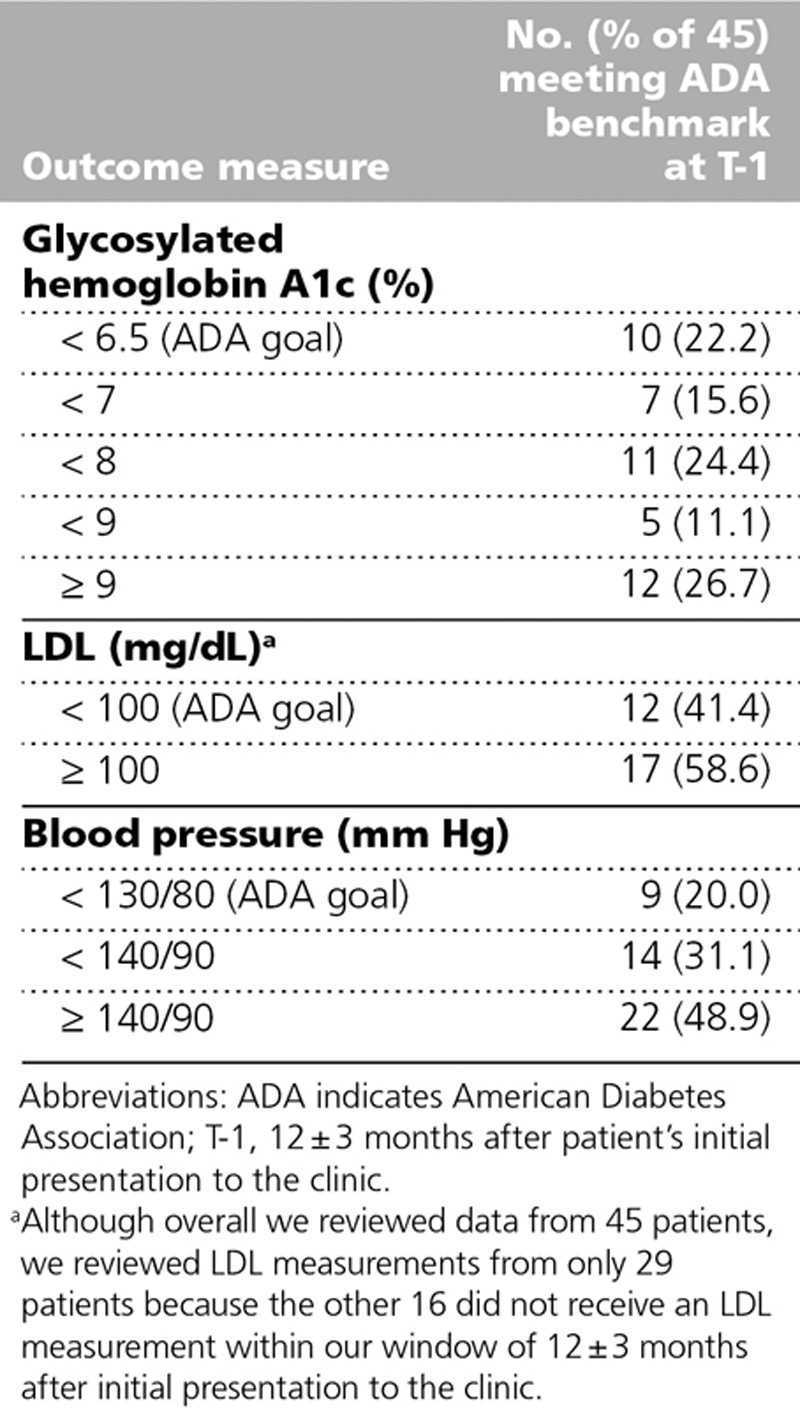
We assessed our ADA outcome measures at T-1 to determine the program’s efficacy in meeting DM2-specific goals after approximately one year of care (see Table 3). The percentage of our study population who met ADA goals for A1c (22.2%, 10/45), LDL (41.4%, 12/29), and blood pressure (20.0%, 9/45) levels were all low to moderate. Although overall we reviewed data from 45 patients, we reviewed LDL measurements from only 29 patients because the other 16 did not receive an LDL measurement within our window of 12 ± 3 months after T-0.
Table 3.
Outcome Measures Assessing the Quality of Clinical Care Delivered to 45 Diabetes Mellitus Type 2 Patients at the Shade Tree Clinic Relative to Best-Practice Benchmarks, 2008–2011
Discussion
Our longitudinal examination of clinical outcomes in diabetes care demonstrates that a medical student health educator program at an SRFC can provide high-quality diabetes care and facilitate clinical improvement one year after enrollment. Our findings contribute to the current literature on SRFCs in three important ways.
First, to our knowledge, this study is the first to demonstrate longitudinal and clinically significant improvement in diabetes care at an SRFC. Only one other published study has reported on the utility of diabetes care in such a setting. The East Harlem Health Outreach Partnership, an SRFC in New York, reported meeting or exceeding standards for a number of diabetes quality-of-care indicators; however, the study design did not allow for longitudinal assessment of clinical outcomes.13 A separate study involving preclinical medical students in a Houston, Texas, preceptorship program in various family medicine practices, not SRFCs, demonstrated that medical students can provide high-quality diabetes foot exam screenings.12 Our results are consistent with and add to the findings of these studies by demonstrating that medical students trained as diabetes health educators can help patients achieve meaningful and lasting clinical improvement.
Second, our results contribute to the growing literature that suggests that medical students at SRFCs can design and implement systems of care that meet national quality-of-care measures. As compliance with process metrics can be viewed as a partial surrogate for a clinic’s system of care, we were encouraged to learn that we had moderate to high rates of compliance with key ADA process measures, such as laboratory screening, immunizations, and foot and retinal examinations. Our results are consistent with those published by the East Harlem Health Outreach Partnership.13 Moreover, the existing literature suggests that SRFCs also can meet quality-of-care standards in other chronic medical conditions, such as hypertension and smoking cessation.6,9,11,14 Taken together, our data and the existing literature support the argument that medical students can design and implement effective systems of care that meet care standards for patients with diabetes and other chronic medical conditions.
Although compliance rates with process measures were high in our study, measures of clinical outcomes were not. For example, the percentages of patients in our study who met ADA outcome metric goals (A1c < 6.5, LDL < 100, and blood pressure < 130/80) were moderate to low. We were initially discouraged by these findings; however, these clinical outcomes are consistent with those reported in the 2009 Healthcare Effectiveness Data and Information Set (HEDIS) report from Tennessee Medicaid.21 Although there are demographic and assessment differences between the patient populations analyzed in the HEDIS report and in our study, these results allow us to view our findings in a broader context. Thus, our outcomes data may reflect both the complex, multifactorial nature of chronic illness and, in part, the inherent difficulties in caring for indigent and medically underserved populations.
Third, we offer our experience as a blueprint and model for the development of comprehensive medical student health educator programs at other SRFCs. As the national prevalence of chronic diseases continues to rise in underserved populations, SRFCs may care for an increasing share of these patients.22 Our experience with the PHE program suggests that medical students, as early as their first year, can be effective care coordinators and health coaches. In addition, the findings that we reported here demonstrate that our PHE program fulfills obligations to the service component of service–learning. Our intuitive sense is that preclinical students benefit from the variety of clinical experiences, such as laboratory explanation and disease counseling, available at the clinic. However, an important next step, through ongoing and future studies, will be to assess those educational benefits.
Likely, the improvement in A1c values that we reported here was affected by some combination of patients’ interactions with PHE students, access to medications, and establishing new care relationships with a clinic. We investigated the contribution of PHE interactions with an analysis correlating A1c values to number of touchpoints and observed a nonsignificant trend towards correlation between these factors. These data suggest that interactions between students and patients are important but that a change in A1c values is not solely attributable to the number of touchpoints. One study reported that 23.6 hours of touchpoint time in a disease management program corresponds to a one-point reduction in A1c values.23 However, the literature as a whole shows mixed results on the strength of this relationship.24 Future studies should clarify the specific contribution of patient–student interaction time to clinical improvement.
Limitations
Important limitations must be considered when interpreting our data. First, this is a retrospective study, which lacks the benefits of prospective cohort ascertainment. Indeed, not all patients were seen in the clinic with the same frequency, depending on patient factors and clinical indications. Next, interpretation of our data is limited by the lack of a control cohort for comparison. Third, touchpoint data relied on students to document interactions, a process that is susceptible to information bias. However, we suggest that this process would lead to an underestimation of the number of touchpoints, diluting any potential relationship between touchpoints and improvement in A1c values. In addition, this single-site study is based on a relatively small sample size, and thus it may not generalize to other health care settings and delivery modalities at other SRFCs. Fifth, our findings are limited to one year of follow-up, requiring future studies to determine the long-term stability of the improvements we have reported here. Moreover, this study does not capture the other benefits to patients of SRFCs, such as health literacy, awareness of community resources, and insurance eligibility screening.9,25,26 Furthermore, this study does not quantify the benefit that early preclinical medical students may receive from the early clinical education and mentorship that they receive from the clinical medical students, residents, and faculty whom they encounter while volunteering at clinic.27,28 Finally, this study does not address the costs associated with providing care to our patient population, limiting the discussion of value by dissociating quality of care from cost. As modern medicine is increasingly aware of the cost of care, future studies should assess the value of our service–learning program.
Going forward
Building on our experiences caring for diabetic patients with the PHE program, we have expanded the model to incorporate the effective management of other chronic illnesses through student-led case management. In the winter of 2011, the first group of cardiovascular disease and respiratory student health educators were trained and started following patients with congestive heart failure, hypertension, hyperlipidemia, chronic obstructive pulmonary disease, and asthma. Currently at Shade Tree Clinic, nearly half of all patients are paired with a PHE student. With this expansion, we intend to collect outcome measures to determine whether our findings apply beyond diabetes care.
Conclusions
This retrospective study is the first, supported by validated longitudinal outcome measures, to describe a comprehensive model of care using medical student health educators at an SRFC. Through this rigorous assessment of the quality of care provided, we found that a medical student health educator program can provide high-quality care for DM2 patients at an SRFC. We offer our program as a model for how SRFCs can rigorously assess the quality of care they provide. We suggest that SRFCs have a twofold obligation to pursue such assessments. First, the ethics of parity dictate that both patients and students benefit from service–learning experiences, rather than one benefiting at the expense of the other. Second, a central tenet of modern medical care is objective evidence to support best practices. To determine whether they fulfill both these obligations, SRFCs must rigorously study the care they provide their patients. Looking to the broad community of SRFCs, we eagerly anticipate future quantitative investigations into the educational and clinical value of the care they provide.
Acknowledgments: The authors thank Drs. Meredith Albin and Arytom Sedykh for their involvement in the original planning of this project and Ms. Paula Marincola for her critical reading of the manuscript.
Footnotes
Funding/Support: This project was supported in part by award T32GM07347 from the National Institute of General Medical Sciences/National Institutes of Health for the Vanderbilt Medical Scientist Training Program (P.G., I.R.) and award UL1TR000445 from the National Center for Advancing Translational Science/National Institutes of Health for the Vanderbilt Institute for Clinical and Translational Research. Funding from the Association of American Medical Colleges Caring for the Community grant, the Boulevard Bolt Foundation, and the Nashville Baptist Healing Trust provided program and patient care support.
Other disclosures: None reported.
Ethical approval: The Vanderbilt University institutional review board approved the study’s protocol as an exempt research project.
Disclaimers: This article reflects the views of the authors and does not reflect the opinions or views of any of the above listed funding sources.
The authors have informed the journal that they agree that both Dr. Gorrindo and Dr. Peltz completed the intellectual and other work typical of the first author.
References
- 1.Association of American Medical Colleges; Association of American Medical Colleges. Medical School Graduation Questionnaire 2011 All Schools Summary Report. Washington, DC: 2011. https://www.aamc.org/download/263712/data/. Accessed December 18, 2013. [Google Scholar]
- 2.Simpson SA, Long JA. Medical student-run health clinics: Important contributors to patient care and medical education. J Gen Intern Med. 2007;22:352–356. doi: 10.1007/s11606-006-0073-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shrader S, Kavanagh K, Thompson A. A diabetes self-management education class taught by pharmacy students. Am J Pharm Educ. 2012;76:13. doi: 10.5688/ajpe76113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sheu LC, Zheng P, Coelho AD, et al. Learning through service: Student perceptions on volunteering at interprofessional hepatitis B student-run clinics. J Cancer Educ. 2011;26:228–233. doi: 10.1007/s13187-010-0142-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meah YS, Smith EL, Thomas DC. Student-run health clinic: Novel arena to educate medical students on systems-based practice. Mt Sinai J Med. 2009;76:344–356. doi: 10.1002/msj.20128. [DOI] [PubMed] [Google Scholar]
- 6.Liang En W, Koh GC, Lim VK. Caring for underserved patients through neighborhood health screening: Outcomes of a longitudinal, interprofessional, student-run home visit program in Singapore. Acad Med. 2011;86:829–839. doi: 10.1097/ACM.0b013e31821d841d. [DOI] [PubMed] [Google Scholar]
- 7.Clark DL, Melillo A, Wallace D, Pierrel S, Buck DS. A multidisciplinary, learner-centered, student-run clinic for the homeless. Fam Med. 2003;35:394–397. [PubMed] [Google Scholar]
- 8.Brazeau CM, Schroeder R, Rovi S, Boyd L. Relationship between medical student service and empathy. Acad Med. 2011;86:S42–S45. doi: 10.1097/ACM.0b013e31822a6ae0. [DOI] [PubMed] [Google Scholar]
- 9.Berman R, Powe C, Carnevale J, et al. The Crimson Care Collaborative: A student–faculty initiative to increase medical students’ early exposure to primary care. Acad Med. 2012;87:651–655. doi: 10.1097/ACM.0b013e31824d5269. [DOI] [PubMed] [Google Scholar]
- 10.Bennard B, Wilson JL, Ferguson KP, Sliger C. A student-run outreach clinic for rural communities in Appalachia. Acad Med. 2004;79:666–671. doi: 10.1097/00001888-200407000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Zucker J, Gillen J, Ackrivo J, Schroeder R, Keller S. Hypertension management in a student-run free clinic: Meeting national standards? Acad Med. 2011;86:239–245. doi: 10.1097/ACM.0b013e31820465e0. [DOI] [PubMed] [Google Scholar]
- 12.Sifuentes F, Chang L, Nieman LZ, Foxhall LE. Evaluating a diabetes foot care program in a preceptorship for medical students. Diabetes Educ. 2002;28:930–932, 935. doi: 10.1177/014572170202800608. [DOI] [PubMed] [Google Scholar]
- 13.Ryskina KL, Meah YS, Thomas DC. Quality of diabetes care at a student-run free clinic. J Health Care Poor Underserved. 2009;20:969–981. doi: 10.1353/hpu.0.0231. [DOI] [PubMed] [Google Scholar]
- 14.Lough LE, Ebbert JO, McLeod TG. Evaluation of a student-run smoking cessation clinic for a medically underserved population. BMC Res Notes. 2011;4:55. doi: 10.1186/1756-0500-4-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hunt JB, Bonham C, Jones L. Understanding the goals of service learning and community-based medical education: A systematic review. Acad Med. 2011;86:246–251. doi: 10.1097/ACM.0b013e3182046481. [DOI] [PubMed] [Google Scholar]
- 16.Buchanan D, Witlen R. Balancing service and education: Ethical management of student-run clinics. J Health Care Poor Underserved. 2006;17:477–485. doi: 10.1353/hpu.2006.0101. [DOI] [PubMed] [Google Scholar]
- 17.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 19.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: L. Erlbaum Associates; 1988. [Google Scholar]
- 20.American Diabetes Association. Standards of medical care in diabetes—2012. Diabetes Care. 2012;35(suppl 1):S11–S63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bureau of TennCare. 2010 HEDIS/CAHPS Report: A Comparative Analysis of Audited Results from TennCare Managed Care Organizations. Nashville, Tenn: Department of Finance and Administration, State of Tennessee; 2010. http://www.tn.gov/tenncare/forms/hedis10.pdf. Accessed December 18, 2013. [Google Scholar]
- 22.Wilper AP, Woolhandler S, Lasser KE, McCormick D, Bor DH, Himmelstein DU. A national study of chronic disease prevalence and access to care in uninsured U.S. adults. Ann Intern Med. 2008;149:170–176. doi: 10.7326/0003-4819-149-3-200808050-00006. [DOI] [PubMed] [Google Scholar]
- 23.Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: A meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25:1159–1171. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]
- 24.Glazier RH, Bajcar J, Kennie NR, Willson K. A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Diabetes Care. 2006;29:1675–1688. doi: 10.2337/dc05-1942. [DOI] [PubMed] [Google Scholar]
- 25.Cadzow RB, Servoss TJ, Fox CH. The health status of patients of a student-run free medical clinic in inner-city Buffalo, NY. J Am Board Fam Med. 2007;20:572–580. doi: 10.3122/jabfm.2007.06.070036. [DOI] [PubMed] [Google Scholar]
- 26.Niescierenko ML, Cadzow RB, Fox CH. Insuring the uninsured: A student-run initiative to improve access to care in an urban community. J Natl Med Assoc. 2006;98:906–911. [PMC free article] [PubMed] [Google Scholar]
- 27.Sternszus R, Cruess S, Cruess R, Young M, Steinert Y. Residents as role models: Impact on undergraduate trainees. Acad Med. 2012;87:1282–1287. doi: 10.1097/ACM.0b013e3182624c53. [DOI] [PubMed] [Google Scholar]
- 28.Turner SR, White J, Poth C, Rogers WT. Preparing students for clerkship: A resident shadowing program. Acad Med. 2012;87:1288–1291. doi: 10.1097/ACM.0b013e3182623143. [DOI] [PubMed] [Google Scholar]


