Abstract
Purpose
The aim of this study is to examine predictors of cancer-related financial difficulties and work modifications in a national sample of cancer survivors.
Methods
Using the 2011 Medical Expenditure Panel Survey and Experiences with Cancer Survivorship Supplement, the prevalence of financial difficulties and work modifications was examined. Logistic regression and survey weights were used to model these outcomes as functions of sociodemographic and health covariates separately among survivors in active treatment and survivors under age 65 years.
Results
Among all survivors, 33.2 % reported any financial concern, with 17.9 % reporting financial difficulties such as debt or bankruptcy. Among working survivors, 44.0 % made any work modification and 15.3 % made long-term work modifications (e.g., delayed or early retirement). Among those in active treatment, predictors of financial difficulty included: race/ethnicity other than white, non-Hispanic [OR=8.0; 95 % CI 2.2–28.4]; income <200 % of federal poverty level (FPL) [OR=15.7; 95 % CI 2.6–95.2] or between 200 and 400 % of FPL [OR=8.2; 95 % CI 1.3–51.4]; residence in a non-metropolitan service area [OR=6.4; 95 % CI 1.6–25.0]; and good/fair/poor self-rated health [OR=3.8; 95 % CI 1.0–14.2]. Among survivors under age 65 years, predictors of long-term work modifications included good/fair/poor self-rated health [OR=4.1; 95 % CI 1.6–10.2], being married [OR=2.2; 95 % CI 1.0–4.7], uninsured [OR=3.5; 95 % CI 1.3–9.3], or publicly insured [OR=9.0; 95 % CI 3.3–24.4].
Conclusions
A substantial proportion of cancer survivors experience cancer-related financial difficulties and work modifications, particularly those who report race/ethnicity other than white, non-Hispanic, residence in non-metropolitan areas, worse health status, lower income, and public or no health insurance.
Implications for cancer survivors
Attention to the economic impact of cancer treatment is warranted across the survivorship trajectory, with particular attention to subgroups at higher risk.
Keywords: Survivorship, Medical Expenditure Panel Survey, Financial burden, Employment issues
Background
The number of cancer survivors (defined as anyone with a history of cancer, from the time of diagnosis onward) [1] in the USA is projected to reach 18.1 million by 2020, with an associated 39 % increase in cancer-related treatment costs [2]. Escalating treatment costs, however, represent only one aspect of cancer survivors’ economic burden, which also frequently includes reduced income due to work limitations, and other “hidden” treatment-related costs such as transportation and childcare expenses [3–5].
Together, medical expenses, reduced income due to work limitations, and other hidden costs can lead to financial distress [6]. Indeed, cancer survivors are at increased risk of financial hardship and medically related bankruptcy even when insured [6–10]. A recent study in Washington State found that cancer survivors were 2.65 times more likely to file for bankruptcy compared to those without cancer [10]. In a nationally representative sample, recently diagnosed and previously diagnosed cancer survivors had annual excess economic burdens of over $16,000 and $4000, respectively per survivor, over and above the annual burden of individuals without cancer [11]. Importantly, those experiencing financial distress are more likely to delay or forgo needed medical care—including needed cancer treatments [6, 12]—and are more likely to experience adverse health outcomes, such as anxiety, depression, and poor health-related quality of life [6, 13–16]. Accordingly, national policy recommendations include monitoring and support for financial distress in the growing population of cancer survivors [17].
Despite recent research and policy attention to the issue of financial distress, little is known about the full scope of financial and work-related burden among cancer survivors. Many previous studies of financial and work-related burden in cancer survivors have limited generalizability given small, focused samples in single institutions or among those with a specific type of cancer [3, 6, 9, 14]. Previous population-based studies have generally analyzed expenditures and are limited in their ability to account for indirect costs and other factors that impact the overall financial burden on cancer survivors or use very broad measures of perceived financial burden rather than specific measures such as debt or bankruptcy [4, 5, 8, 11, 16, 18, 19]. A recent systematic review of studies on cancer-related financial distress identified only four US studies reporting the prevalence of financial distress among adult cancer survivors, most of which were conducted at single institutions and focused on subgroups of cancer survivors [12].
The recently released Experiences with Cancer Survivorship Supplement to the Medical Expenditure Panel Survey offers a unique opportunity to improve our knowledge about the overall burden experienced by cancer survivors in the USA [20]. To address gaps in existing literature, we take advantage of these newly available data to examine work and financial burden as reported by cancer survivors in a large, nationally representative sample that included survivors of all cancer types. We produce current national estimates of financial distress and work modifications among cancer survivors and examine related disparities, providing information that researchers, clinicians, and policymakers can use to develop risk-stratified interventions to address work and financial concerns.
Methods
Data source
Data were derived from the 2011 Medical Expenditure Panel Survey Household Component (MEPS-HC) and Experiences with Cancer Survivorship Supplement (ECSS). MEPS-HC is an annual, national survey conducted by the Agency for Healthcare Research and Quality (AHRQ) in a subsample of individuals from the previous year’s National Health Interview Survey (NHIS). MEPS-HC includes individuals of all ages, with all insurance types, and collects information on sociodemographic and health characteristics, as well as medical expenditures and service use [21]. In 2011, cancer survivors identified in NHIS were oversampled and completed the ECSS—a self-administered questionnaire co-developed by the National Cancer Institute (NCI), American Cancer Society (ACS), Centers for Disease Control and Prevention (CDC), National Institutes of Health (NIH), and LIVESTRONG—to provide national estimates of psychosocial, financial, work-related, and other aspects of cancer burden [20, 22]. Response rates for the 2011 MEPS-HC and ECSS were 59.4 and 91 %, respectively [23, 24].
Sample
Eligible subjects included adult (≥18 years) cancer survivors (defined as having a history of cancer from time of diagnosis onward) who completed the 2011 ECSS (n=1419). We excluded individuals who reported only a history of non-melanoma skin cancer for consistency with prior work, and because these cancers rarely are fatal or require treatment comparable with that of other cancers [11]. After excluding individuals who were missing data on the dependent variables or who reported only non-melanoma skin cancers, the analysis sample included 1209 cancer survivors. Analysis of work modifications was limited to the subpopulation who reported working at any point during their cancer treatment (n=616).
Financial and work concerns
Outcomes included self-reported financial and work concerns. MEPS questions about financial concerns included asking if, due to cancer, the respondent or a family member (1) incurred debt or borrowed money, (2) filed for bankruptcy, (3) was unable to cover the costs of medical care visits, (4) their families made other financial sacrifices, or (5) worried about paying large medical bills. Participants were coded as having a financial difficulty if they answered “yes” to experiencing debt, bankruptcy, or an inability to cover medical costs. They were coded as having a financial worry if they answered “yes” to making other financial sacrifices or worrying about medical bills. Work concern questions included asking if, due to cancer, the respondent (1) changed to a less demanding job, (2) retired earlier than planned, (3) delayed retirement, (4) took unpaid time off of work, or (5) took extended leave from work. Participants were coded as having made a long-term work modification if they answered “yes” to changing to a less demanding job, delaying, or taking early retirement. They were coded as having made a short-term work modification if they took extended or unpaid leave from work. Work concern variables were examined in the subpopulation of cancer survivors who reported working at any point since cancer diagnosis.
Predictors
Sociodemographic and health variables relevant to identifying disparities in work and financial outcomes were included as predictors in our models, including sex, race/ethnicity, marital status, insurance status, health status, residence of survivor (i.e., non-metropolitan service area [non-msa] versus metropolitan service area [msa]), income as a percentage of the federal poverty level, and years of education. In general, groups that tend to have better health outcomes were assigned as the reference groups for predictor variables in order to highlight disparities. The models also controlled for potentially confounding variables, including age at interview, age at cancer diagnosis, treatment status (currently in active treatment versus not in active treatment), and region (West, Midwest, and Northeast, versus South).
Because age at interview and age at cancer diagnosis both have a potentially non-linear relationship with financial and work concerns, quadratic and cubic terms for these variables were tested in the logistic regression models and retained if significant.
Statistical analysis
All analyses were conducted using Stata 12 (College Station, TX). Frequencies and proportions of all variables were calculated. Population proportions and 95 % confidence intervals were estimated for all financial and work-related outcomes. However, predictive models examined only financial difficulty and long-term work modifications. These outcomes were selected to provide more informative results because financial difficulties are more concrete than financial worries, and long-term work modifications are a less ambiguous measure of work impact than short-term work modifications (i.e., short-term work modifications could arguably be negative or positive outcomes based on personal preference). Logistic regression was used to model binary measures of financial difficulties and long-term work modifications (i.e., having any financial difficulty or work modification) as functions of the predictors.
Odds ratios (OR) were calculated with corresponding 95 % confidence intervals (95 % CI) with statistical significance set at p<0.05. Survey weights were applied, and Stata survey commands were used in all analyses to account for the complex survey design and produce national estimates generalizable to the US civilian, non-institutionalized population self-reporting as having been diagnosed with or treated for cancer as an adult.
The work and financial concern questions were not assessed within any specific time frame (e.g., within the last year). Therefore, we stratified all regression models by either age at interview or treatment status to account for potential differences in the measured effects by these variables. Models of work modifications were limited only to survivors who reported working at any point from cancer diagnosis to the survey interview date. In cancer care, economic impact varies substantially by phase of treatment, following a U-shaped curve that reflects greater costs of care during initial treatment and again towards end-of-life care [25]. In addition, cancer-related work limitations may have different effects on employment of younger survivors than among older survivors who are eligible for Medicare or Social Security benefits [10, 26]. Accordingly, we focused on identifying predictors within these high-risk groups and present models of financial distress and long-term work modifications only among those who were less than age 65 years at interview or who were currently in active treatment.
Results
Sample characteristics
Our sample of cancer survivors included a higher proportion of women (58.1 %) compared to men. Over half were age 65 years and older at interview (54.4 %) versus less than age 65 years. The majority of cancer survivors were white, non-Hispanic (84.4 %). 59.4 % reported having good/fair/poor health versus excellent/very good health. 56.7 % reported being married. One third reported having ≥16 years of education (33.5 %). Less than half of survivors reported an adjusted family income ≥400 % of FPL (43.0 %). About two thirds reported having private insurance (68.2 %). Regarding treatment status, survivors in active treatment comprised the smallest proportion of the sample (18.1 %), followed by those <5 years posttreatment (30.9 %), with the largest proportion ≥5 years posttreatment (51.0 %). The most commonly reported cancer sites were breast (20.3 %) and prostate (16.5 %). Just over half of the survivors in our sample were diagnosed with cancer between the ages of 40 and 65 years (53.0 %) and almost a third at age 65 years or older (29.9 %) (Table 1).
Table 1.
Sociodemographic and health characteristics of adult cancer survivors, Medical Expenditure Panel Survey and Experiences with Cancer Survivorship Supplement 2011 (n=1209)
| na | % (95 % CI) | |
|---|---|---|
| Sex | ||
| Female | 741 | 58.1 (54.6–61.5) |
| Male | 468 | 41.9 (38.5–45.4) |
| Age at interview (years) | ||
| <65 years | 587 | 45.6 (41.6–49.6) |
| ≥65 years | 622 | 54.4 (50.4–58.4) |
| Race/ethnicity | ||
| Minority | 343 | 15.6 (13.2–18.0) |
| White, non-Hispanic | 866 | 84.4 (82.0–86.8) |
| Health status | ||
| Good/fair/poor health | 770 | 59.4 (55.9–63.0) |
| Excellent/very good health | 439 | 40.6 (37.0–44.1) |
| Marital status | ||
| Married | 625 | 56.7 (52.8–60.6) |
| Not married | 584 | 43.3 (39.4–47.2) |
| Years of education | ||
| <12 years | 227 | 12.9 (10.5–15.3) |
| 12 years | 392 | 29.7 (26.6–32.8) |
| ≥12–<16 years | 270 | 23.9 (21.0–26.7) |
| ≥16 years | 312 | 33.5 (29.7–37.2) |
| Income (% FPL)b | ||
| <200 % of FPL | 465 | 26.8 (24.1–29.6) |
| 200–<400 % of FPL | 369 | 30.2 (26.4–33.9) |
| 400 % or higher of FPL | 375 | 43.0 (38.8–47.1) |
| Insurance | ||
| Uninsured | 72 | 4.4 (2.9–5.9) |
| Public insurance | 419 | 27.4 (24.4–30.4) |
| Private insurance | 718 | 68.2 (65.2–71.3) |
| Survivor residence | ||
| Non-metropolitan service area | 231 | 18.0 (13.8–22.2) |
| Metropolitan service area | 978 | 82.0 (77.8–86.2) |
| Treatment status | ||
| Active treatment | 166 | 18.1 (15.0–21.3) |
| <5 years posttreatment | 300 | 30.9 (27.0–34.7) |
| ≥5 years posttreatment | 487 | 51.0 (47.4–54.6) |
| Cancer site | ||
| Breast | 261 | 20.3 (17.7–22.8) |
| Prostate | 184 | 16.5 (13.6–19.5) |
| Lung | 38 | 3.1 (2.0–4.2) |
| Colorectal | 76 | 6.0 (4.4–7.5) |
| Hematologic | 73 | 6.4 (4.8–8.1) |
| Gynecologic | 201 | 13.2 (11–15.5) |
| Other | 376 | 34.5 (31.0–37.9) |
| Age at cancer diagnosis | ||
| <40 years | 251 | 17.1 (14.5–19.7) |
| 40–<65 years | 599 | 53.0 (49.4–56.5) |
| ≥65 years | 342 | 29.9 (26.3–33.6) |
95 % CI 95% confidence interval
Not all ns total 1209 due to missing data
Adjusted family income as a percentage of the federal poverty level
Financial concerns
Among all cancer survivors, 33.2 % reported having at least one financial concern (not shown in tables), 17.9 % reported a financial difficulty, and 28.3 % reported a financial worry (Table 2). A consistently higher proportion of survivors in active treatment had financial concerns compared to those not in active treatment, with significant differences for any financial worry (46.5 versus 24.8 %), worry about paying medical bills (41.6 versus 21.8 %), and financial sacrifice (18.2 versus 9.0 %) (Table 2). Significantly higher proportions of survivors less than age 65 years at interview reported all measures of financial concerns except bankruptcy compared to those age 65 years or older at interview (Table 2), including overall measures of financial difficulty (27.3 versus 10.0 %), and financial worry (39.3 versus 19.1 %) (Table 2). While differences in the proportion reporting bankruptcy were not statistically significant, the proportion of survivors less than age 65 years at interview reporting this outcome was higher than in any other subgroup (2.3 versus 1.4 % [age ≥65 years at interview]; 1.8 % [all survivors]) (Table 2).
Table 2.
Financial and work concerns reported by adult cancer survivors in the USA, Medical Expenditure Panel Survey and Experiences with Cancer Survivorship Supplement 2011 (n=1209)
| Treatment status | Age at interview | ||||
|---|---|---|---|---|---|
| All survivors (n=1209) |
Active treatment (n=166) |
Not in active treatment (n=1043) |
<65 years (n=587) |
≥65 years (n=622) |
|
| % (95 % CI) | % (95 % CI) | % (95 % CI) | % (95 % CI) | % (95 % CI) | |
| Any financial difficulty | 17.9 (15.1–20.8) | 21.3 (15.8–28.1) | 17.2 (14.2–20.7) | 27.3 (22.9–31.6)* | 10.0 (0.7–13.6) |
| Debt | 8.0 (6.2–9.7) | 9.5 (5.7–15.1) | 7.7 (5.9–9.9) | 14.3 (11.2–18.0)* | 2.7 (1.5–4.8) |
| Bankruptcy | 1.8 (0.8–2.7) | 1.9 (0.5–7.0) | 1.7 (1.0–3.1) | 2.3 (0.8–3.7) | 1.4 (0.5–3.4) |
| Unable to pay medical bills | 13.0 (10.5–15.5) | 17.6 (12.5–24.3) | 12.1 (9.6–15.2) | 18.2 (14.6–21.9)* | 8.6 (6.2–11.8) |
| Any financial worry | 28.3 (24.8–31.8) | 46.5 (37.2–56.0)* | 24.8 (21.4–28.4) | 39.3 (34.1–44.5)* | 19.1 (15.0–23.2) |
| Worry about medical bills | 25.0 (21.7–28.4) | 41.6 (32.3–51.6)* | 21.8 (18.7–25.2) | 35.0 (30.2–40.1)* | 16.7 (13.2–20.9) |
| Financial sacrifice | 10.5 (8.4–12.6) | 18.2 (11.1–25.2)* | 9.0 (7.0–11.6) | 13.8 (10.4–17.2)* | 7.8 (5.6–10.7) |
| Working survivorsa (n=616) |
Active treatment (n=97) |
Not in active treatment (n=519) |
<65 years (n=382) |
≥65 years (n=234) |
|
| % (95 % CI) | % (95 % CI) | % (95 % CI) | % (95 % CI) | % (95 % CI) | |
| Long-term work modifications | 15.3 (11.7–19.0) | 20.7 (12.8–31.8) | 14.3 (10.7–18.9) | 13.9 (10.1–18.8) | 17.5 (12.3–24.2) |
| Change to a less demanding job | 3.4 (1.4–5.3) | 0.3 (0.0–2.0)* | 3.9 (2.2–7.0) | 3.2 (1.8–5.6) | 3.7 (1.5–8.5) |
| Delayed retirement | 2.3 (0.8–3.8) | 4.2 (1.3–13.1) | 2.0 (0.9–4.2) | 2.7 (1.4–5.3) | 1.7 (0.4–7.1) |
| Early retirement | 11.1 (8.2–14.1) | 11.1 (8.5–14.4) | 10.2 (7.3–13.9) | 8.8 (5.8–13.3) | 14.6 (10.2–20.4) |
| Short-term work modifications | 39.3 (34.8–43.7) | 48.0 (36.6–59.6) | 37.6 (32.9–42.5) | 45.7 (39.7–51.7)* | 29.7 (23.5–36.7) |
| Unpaid leave of absence | 19.8 (16.1–23.3) | 26.2 (17.0–38.0) | 18.5 (15.0–22.7) | 24.0 (19.3–29.4)* | 13.4 (9.2–19.1) |
| Extended leave of absence | 30.7 (26.4–34.9) | 34.2 (24.1–46.0) | 30.0 (25.5–34.9) | 30.7 (26.6–35.1)* | 24.0 (18.3–30.9) |
95 % CI 95% confidence interval
Significant (p<0.05) χ2 for those in active treatment versus those not in active treatment or age <65 years versus age ≥65 years at interview
Long- and short-term work modifications examined in a subgroup of survivors who reported working at some point since cancer diagnosis
Work modifications
Among cancer survivors who reported working, 44.0 % made at least one work modification due to cancer (not shown in tables), including long-term work modifications (15.3 %) and short-term work modifications (39.3 %) (Table 2). The only statistically significant difference between those in active treatment versus those not in active treatment was a lower proportion of survivors who changed to a less demanding job (0.3 versus 3.9 %) (Table 2). A significantly greater proportion of survivors less than age 65 years at interview reported making short-term work modifications, including extended leave of absence (30.7 versus 24.0 %) or unpaid leave of absence (24.0 versus 13.4 %) (Table 2).
Fully adjusted regression models
Survivors in active treatment
In fully adjusted logistic regression models among survivors currently in active treatment, significant predictors of having any financial difficulty (i.e., debt, bankruptcy, or inability to pay bills) included race/ethnicity other than white, non-Hispanic [OR=8.0; 95 % CI 2.2–28.4]); good/fair/poor health status [OR=3.8; 95 % CI 1.0–14.2]; income <200 % of FPL [OR=15.7; 95 % CI 2.6, 95.2] or between 200 and 400 % of FPL [OR=8.2; 95 % CI 1.3–52.4]; and residing in a non-metropolitan service area [OR=6.4; 95 % CI 1.6–25.0] (Table 3). Among survivors currently in active treatment, the only significant predictor of making a long-term work modification (i.e., changing to a less demanding job, taking delayed or early retirement) was good/fair/poor health status [OR=10.4; 95 % CI 2.0–54.8] (Table 3).
Table 3.
Logistic regression models for adult cancer survivors currently in active treatment (n= 166), Medical Expenditures Panel Survey and Experiences with Cancer Survivorship Supplement 2011
| Financial difficulties OR (95 % CI) | Long-term work modifications OR (95 % CI) | |
|---|---|---|
| Sex | ||
| Female | 1.4 (0.5–4.4) | 1.3 (0.2–8.4) |
| Male | … | … |
| Race/ethnicity | ||
| Minority | 8.0 (2.2–28.4)* | 0.8 (0.1–4.8) |
| White, non-Hispanic | … | … |
| Health status | ||
| Good/fair/poor health | 3.8 (1.0–14.2)* | 10.4 (2.0–54.8)* |
| Excellent/very good health | … | … |
| Marital status | ||
| Married | 1.9 (0.3–10.6) | 2.3 (0.5–11.3) |
| Not married | … | … |
| Years of education | ||
| <12 years | 1.8 (0.3–11.8) | 0.4 (0.0–6.6) |
| 12 years | 1.2 (0.3–4.2) | 0.2 (0.0–1.6) |
| ≥12–<16 years | 3.4 (0.9–13.8) | 0.3 (0.0–2.0) |
| ≥16 years | … | … |
| Income (% FPL)a | ||
| <200 % of FPL | 15.7 (2.6–95.2)* | 6.1 (0.5–71.1) |
| 200–<400 % of FPL | 8.2 (1.3–52.4)* | 3.6 (0.5–25.7) |
| 400 % or higher of FPL | … | … |
| Insurance | ||
| Uninsured | 0.4 (0.0–6.4) | 0.3 (0.0–11.5) |
| Public insurance | 0.7 (0.2–2.7) | 3.7 (0.5–27.4) |
| Private insurance | … | … |
| Survivor residence | ||
| Non-metropolitan service area | 6.4 (1.6–25.0)* | 3.0 (0.5–17.7) |
| Metropolitan service area | … | … |
Models also controlled for age at interview, age at cancer diagnosis, and region of residence; polynomial terms for age at interview were significant only for the model of financial difficulties among survivors in active treatment (see Fig. 1); (…) denotes reference group
OR odds ratio, 95 % CI 95% confidence interval
Statistically significant, p<0.05
Adjusted family income as a percentage of the federal poverty level
Survivors less than age 65 years at interview
Among survivors less than age 65 years at interview, significant predictors of having a financial difficulty included good/fair/poor health status [OR=2.4; 95 % CI 1.4–4.1] and between 12 and 16 years of education [OR=1.9; 95 % CI 1.1–3.6] (Table 4).
Table 4.
Logistic regression models for adult cancer survivors less than 65 years of age (n=587), Medical Expenditures Panel Survey and Experiences with Cancer Survivorship Supplement 2011
| Financial difficulties | Long-term work modifications | |
|---|---|---|
| OR (95 % CI) | OR (95 % CI) | |
| Treatment status | ||
| In active treatment | 1.1 (0.6–1.9) | 1.2 (0.5–3.0) |
| Not in active treatment | … | … |
| Sex | ||
| Female | 1.8 (0.9–3.2) | 1.2 (0.6–2.7) |
| Male | … | … |
| Race/ethnicity | ||
| Minority | 1.7 (1.0–2.8) | 1.1 (0.5–2.4) |
| White, non-Hispanic | … | … |
| Health status | ||
| Good/fair/poor health | 2.4 (1.4–4.1)* | 4.1 (1.6–10.2)* |
| Excellent/very good health | … | … |
| Marital status | ||
| Married | 0.9 (0.5–1.6) | 2.2 (1.0–4.7)* |
| Not married | … | … |
| Years of education | ||
| <12 years | 1.1 (0.4–2.6) | 0.6 (0.1–4.7) |
| 12 years | 0.7 (0.4–1.5) | 0.7 (0.3–1.7) |
| ≥12–<16 years | 1.9 (1.1–3.6)* | 0.5 (0.2–1.4) |
| ≥16 years | … | … |
| Income (% FPL)a | ||
| <200 % of FPL | 1.5 (0.7–3.4) | 1.6 (0.5–4.9) |
| 200–<400 % of FPL | 1.3 (0.6–2.8) | 2.0 (0.9–4.5) |
| 400 % or higher of FPL | … | … |
| Insurance | ||
| Uninsured | 1.8 (0.8–4.3) | 3.5 (1.3–9.3)* |
| Public insurance | 1.6 (0.7–3.6) | 9.0 (3.3–24.4)* |
| Private insurance | … | … |
| Survivor residence | ||
| Non-metropolitan service area | 1.5 (0.7–2.9) | 0.9 (0.4–2.4) |
| Metropolitan service area | … | … |
Models also controlled for age at interview, age at cancer diagnosis, and region of residence; polynomial terms for age at interview were significant only for the model of financial difficulties among survivors less than age 65 years at interview (see Fig. 2); (…) denotes reference group
Statistically significant, p<0.05
OR odds ratio, 95 % CI 95% confidence interval
Adjusted family income as a percentage of the federal poverty level
Among survivors less than age 65 years at interview, significant predictors of making a long-term work modification included good/fair/poor health status [OR=4.1; 95 % CI 1.6–10.2], being married [OR=2.2; 95 % CI 1.0–4.7], and being uninsured [OR=3.5; 95 % CI 1.3–9.3] or publicly insured [OR=9.0; 95 % CI 3.3–24.4] (Table 4).
The effect of age
Predicted marginal effects for age at interview were calculated post-estimation for models in which age at interview was a significant predictor. Age at interview was not a significant predictor of long-term work modifications for either subpopulation but had a significant curvilinear relationship with the odds of financial difficulty for survivors less than age 65 years and survivors currently in active treatment.
For survivors currently in active treatment, the odds of financial difficulty were minimal for younger patients, but began increasing in the mid-40s, peaking at approximately 60 years of age (Fig. 1). For survivors less than age 65 years at interview, the odds of financial difficulty were highest among the youngest survivors, leveling off at approximately age 30 and decreasing at approximately age 62 (Fig. 2).
Fig. 1.
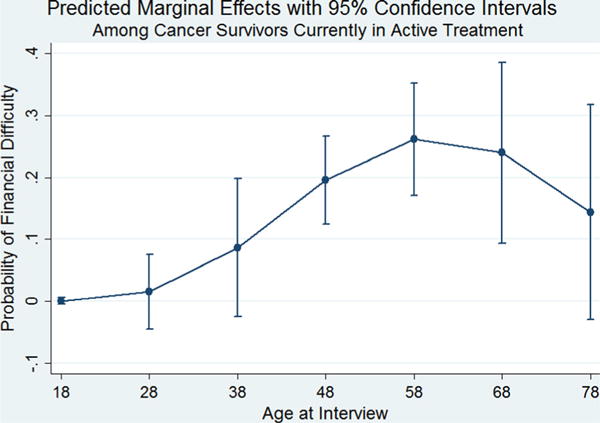
Predicted marginal effects with 95 % confidence intervals among cancer survivors currently in active treatment
Fig. 2.
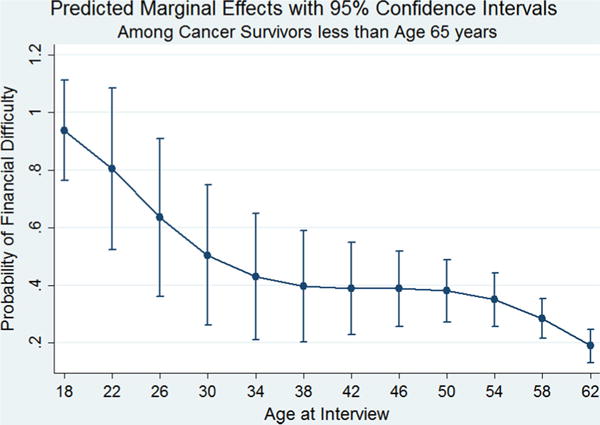
Predicted marginal effects with 95 % confidence intervals among cancer survivors less than age 65 years
Discussion
In a nationally representative sample, we found that one in three cancer survivors experienced financial concerns and nearly half of employed cancer survivors made work modifications. Our results are consistent with prior reports showing that cancer survivors face productivity losses and heavy financial burdens as a result of their disease and related treatment [3, 4, 6, 8–13, 18, 19]. Previous estimates of the proportion of cancer survivors with financial distress have ranged from 14–78 % [12]. The proportion of cancer survivors filing for bankruptcy—just one of several measures of financial distress we examined—has been previously been estimated at 2.2 % and is similar to findings in our study [10]. While few studies have used comparable measures of work modifications, a recent national study estimated that about 30 % of cancer survivors experience limitations in work or usual activities due to physical health [8]. We provide estimates that both support and extend current literature by highlighting cancer survivors’ experiences of work and financial burden, such as borrowing money or delaying retirement. Prior studies have, in contrast, predominantly used broad measures (e.g., perception of financial distress) or purely quantitative measures (e.g., out of pocket expenditures and missed work days) that, while important, do not adequately characterize the impact of disease and treatment-related costs on survivors’ lives.
We identified substantial disparities in financial difficulties, with survivors who were of race/ethnicity other than white, non-Hispanic, had incomes <400 % of FPL, who lived in non-metropolitan areas, or who reported good/fair/poor health at increased risk among those in active treatment, as well as survivors with good/fair/poor health status and between 12 and 16 years of education among those less than 65 years of age at interview. The disparities we identified persisted despite controlling for insurance, suggesting that survivors in these subgroups experience financial problems even when insured [3, 9]. The disparities we identified for financial difficulties are congruent with previous studies, which have consistently identified predictors of both financial hardship and productivity losses as younger age, minority race/ethnicity, lower income, and active treatment status/recent diagnosis [6, 7, 9, 10, 12, 13, 16].
Our study contributes several novel findings with respect to financial burden among cancer survivors. Among survivors less than age 65 years at interview, we found significantly higher odds of financial difficulty for those who had between 12 and 16 years of education, roughly equivalent to having some college, but not a college degree. This finding suggests that individuals with this upper-middle level of education may have jobs that place them at particular risk for medically related financial problems in this age group, perhaps a result of underinsurance or other competing financial burdens (e.g., childcare, student loans). Among survivors in active treatment, we found significantly higher odds of financial difficulty associated with residence in non-metropolitan service areas—a finding that points to the need for further research to examine the drivers of financial distress for patients in rural settings.
Our results with respect to work modifications also provide novel contributions. We found, among survivors less than age 65 years at interview, that those who are married, uninsured, or publicly insured have higher odds of making a long-term work modification. Within this age group, private insurance is largely tied to employment, and individuals with public insurance may be eligible for reasons related to work disability. Alternatively, these findings may be a result of the need for younger survivors with private insurance to maintain employment. Individuals who are married (and therefore eligible for insurance through a spouse) or who lack private insurance could potentially make long-term employment changes without affecting insurance coverage. Importantly, these findings come from a survey conducted in 2011 before implementation of the Affordable Care Act (ACA). It will be important to monitor how ACA implementation impacts work and financial problems for cancer survivors in light of potentially improved access to affordable insurance coverage that is not dependent on employment.
Lastly, we provide novel estimates that describe the relationship between age and the probability of experiencing financial difficulties. Our findings point to the complex relationship between age and financial burden and suggest that while older patients may experience greater financial challenges during the initial treatment phase, financial burden for younger patients may increase over time and extend into the posttreatment phase. Possibly, these long-term financial effects occur because younger survivors face not only treatments costs but also longer-term effects on productivity and income. Future studies, ideally using longitudinal designs, are warranted to more fully understand the work and financial experiences of survivors across the life course.
Many patients report a desire to discuss treatment costs, and practice guidelines suggest that financial discussions are important to high-quality care [27, 28]. However, evidence suggests that conversations about costs happen infrequently, and little is known about barriers and facilitators for these conversations [28–30]. Patients might benefit from discussion of financial and work concerns, particularly when alternative treatment options may provide similar benefit at lower cost [27, 31]. However, such conversations are sensitive—doctors and patients frequently believe the other should be responsible for initiating such discussions [32], and even patients who wish to be aware of the costs of care may prefer that providers not consider costs in decision making, fearing that they will receive subpar treatment if they have a limited ability to pay [33, 34]. Survivors experiencing difficulties might benefit from programs that assist with financial and employment issues; however, such programs are relatively few. The high prevalence of financial and work concerns in our study suggests the need for additional support and program development in this area. Further research and policy attention to work and financial concerns might maximize impact by focusing on groups at higher risk of financial and work problems, such as younger survivors, minorities, those with lower incomes or without private insurance, those living in more rural service areas and those with worse overall health.
Limitations
Our study has several important limitations. First, our findings must be interpreted cautiously in light of the imprecise time frame around the work and financial burden questions in the ECSS. Cancer survivors reported whether or not they ever experienced these burdens due to cancer, but not within a specific time period (e.g., during the past 12 months). Therefore, differences in outcomes are potentially confounded by age, poor recall of past events, or differences in healthcare policies affecting costs and employment benefits for long-term versus recent survivors. We minimized this confounding by controlling for both current age and age of cancer diagnosis in all models and by stratifying the models by treatment status and age. Second, because the financial and work-related questions were included in a survey supplement administered only to cancer survivors, it is not possible to compare these outcomes between individuals with and without a history of cancer. Third, the MEPS sample includes only civilian, non-institutionalized individuals and excludes those in nursing homes, long-term care, or other institutions. This may have caused us to underestimate work and financial burden, since those who are institutionalized are likely to be in worse health and have greater treatment-related expenses. Underestimates may also have resulted due to the self-reported nature of survey responses and the stigma related to reporting certain aspects of work or financial distress [26]. Fourth, the 59.4 % response rate may reflect some level of sampling bias in the MEPS if there are unmeasured characteristics associated with choosing to respond to the survey versus choosing not to respond. Finally, the relatively small sample size of the MEPS ECSS may have contributed to wide confidence intervals for some of our estimates, overlapping confidence intervals in the analysis of the effect of age on financial difficulties, and may have limited our power to detect important disparities in some subgroups.
Conclusions
Our study yields important new insights about the scope of work and financial burden among cancer survivors in the USA by providing current national estimates of work modifications and financial distress in this growing population. Our findings point to the urgent need for attention to the work and financial impact of treatment on cancer survivors from active treatment through long-term survivorship.
Acknowledgments
Funding No funding was received for this research.
Footnotes
Conflicts of interest The authors declare they have no conflicts of interest.
References
- 1.NCI. Dictionary of cancer terms. http://www.cancer.gov/dictionary?cdrid=450125 Accessed November 12 2014.
- 2.Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst. 2011;103(2):117–28. doi: 10.1093/jnci/djq495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arozullah AM, Calhoun EA, Wolf M, Finley DK, Fitzner KA, Heckinger EA, et al. The financial burden of cancer: estimates from a study of insured women with breast cancer. J Support Oncol. 2004;2(3):271–8. [PubMed] [Google Scholar]
- 4.Banegas MP, Yabroff KR. Out of pocket, out of sight? An unmeasured component of the burden of cancer. J Natl Cancer Inst. 2013;105(4):252–3. doi: 10.1093/jnci/djs641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tang DH, Alberts DS, Nevins R, Sullivan S, Skrepnek GH. Health care expenditures, hospitalizations, and productivity associated with cancer in US employer settings. J Occup Environ Med Am Coll Occup Environ Med. 2012;54(12):1453–60. doi: 10.1097/JOM.0b013e31827943e0. [DOI] [PubMed] [Google Scholar]
- 6.Zafar SY, Peppercorn JM, Schrag D, Taylor DH, Goetzinger AM, Zhong X, et al. The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist. 2013;18(4):381–90. doi: 10.1634/theoncologist.2012-0279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Finkelstein EA, Tangka FK, Trogdon JG, Sabatino SA, Richardson LC. The personal financial burden of cancer for the working-aged population. Am J Manag Care. 2009;15(11):801–6. [PubMed] [Google Scholar]
- 8.Dowling EC, Chawla N, Forsythe LP, de Moor J, McNeel T, Rozjabek HM, et al. Lost productivity and burden of illness in cancer survivors with and without other chronic conditions. Cancer. 2013;119(18):3393–401. doi: 10.1002/cncr.28214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shankaran V, Jolly S, Blough D, Ramsey SD. Risk factors for financial hardship in patients receiving adjuvant chemotherapy for colon cancer: a population-based exploratory analysis. J Clin Oncol. 2012;30(14):1608–14. doi: 10.1200/JCO.2011.37.9511. [DOI] [PubMed] [Google Scholar]
- 10.Ramsey S, Blough D, Kirchhoff A, Kreizenbeck K, Fedorenko C, Snell K, et al. Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff (Project Hope) 2013;32(6):1143–52. doi: 10.1377/hlthaff.2012.1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guy GP, Jr, Ekwueme DU, Yabroff KR, Dowling EC, Li C, Rodriguez JL, et al. Economic burden of cancer survivorship among adults in the United States. J Clin Oncol Off J Am Soc Clin Oncol. 2013;31(30):3749–57. doi: 10.1200/jco.2013.49.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Azzani M, Roslani AC, Su TT. The perceived cancer-related financial hardship among patients and their families: a systematic review. Support Care Cancer Off J Multinational Assoc Support Care Cancer. 2014 doi: 10.1007/s00520-014-2474-y. [DOI] [PubMed] [Google Scholar]
- 13.Kent EE, Forsythe LP, Yabroff KR, Weaver KE, de Moor JS, Rodriguez JL, et al. Are survivors who report cancer-related financial problems more likely to forgo or delay medical care? Cancer. 2013;119(20):3710–7. doi: 10.1002/cncr.28262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meneses K, Azuero A, Hassey L, McNees P, Pisu M. Does economic burden influence quality of life in breast cancer survivors? Gynecol Oncol. 2012;124(3):437–43. doi: 10.1016/j.ygyno.2011.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharp L, Carsin AE, Timmons A. Associations between cancer-related financial stress and strain and psychological well-being among individuals living with cancer. Psycho-Oncology. 2013;22(4):745–55. doi: 10.1002/pon.3055. [DOI] [PubMed] [Google Scholar]
- 16.Weaver KE, Rowland JH, Bellizzi KM, Aziz NM. Forgoing medical care because of cost: assessing disparities in healthcare access among cancer survivors living in the United States. Cancer. 2010;116(14):3493–504. doi: 10.1002/cncr.25209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shih YC, Ganz PA, Aberle D, Abernethy A, Bekelman J, Brawley O, et al. Delivering high-quality and affordable care throughout the cancer care continuum. J Clin Oncol Off J Am Soc Clin Oncol. 2013;31(32):4151–7. doi: 10.1200/JCO.2013.51.0651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ekwueme DU, Yabroff KR, Guy GP, Jr, Banegas MP, de Moor JS, Li C, et al. Medical costs and productivity losses of cancer survivors—United States, 2008–2011. MMWR Morb Mortal Wkly Rep. 2014;63(23):505–10. [PMC free article] [PubMed] [Google Scholar]
- 19.Guy GP, Jr, Yabroff KR, Ekwueme DU, Smith AW, Dowling EC, Rechis R, et al. Estimating the health and economic burden of cancer among those diagnosed as adolescents and young adults. Health Aff (Project Hope) 2014;33(6):1024–31. doi: 10.1377/hlthaff.2013.1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yabroff KR, Dowling E, Rodriguez J, Ekwueme DU, Meissner H, Soni A, et al. The medical expenditure panel survey (MEPS) experiences with cancer survivorship supplement. J Cancer Surviv Res Pract. 2012;6(4):407–19. doi: 10.1007/s11764-012-0221-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.AHRQ. Medical Expenditures Panel Survey background. http://meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp. Accessed November 5 2014.
- 22.CDC. MEPS experiences with cancer survivorship supplement. doi: 10.1007/s11764-012-0221-2. http://www.cdc.gov/cancer/survivorship/what_cdc_is_doing/meps.htm. Accessed November 5 2014. [DOI] [PMC free article] [PubMed]
- 23.AHRQ. http://meps.ahrq.gov/survey_comp/hc_response_rate.jsp. Accessed November 5 2014.
- 24.National Cancer Institute. http://appliedresearch.cancer.gov/meps/meps_fact_sheet.pdf. Accessed November 5 2014.
- 25.Yabroff KR, Lund J, Kepka D, Mariotto A. Economic burden of cancer in the United States: estimates, projections, and future research. Cancer Epidemiol Biomark Prev. 2011;20(10):2006–14. doi: 10.1158/1055-9965.EPI-11-0650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bhandari A, Wagner T. Self-reported utilization of health care services: improving measurement and accuracy. Med Care Res Rev. 2006;63(2):217–35. doi: 10.1177/1077558705285298. [DOI] [PubMed] [Google Scholar]
- 27.Meropol NJ, Schrag D, Smith TJ, Mulvey TM, Langdon RM, Jr, Blum D, et al. American Society of Clinical Oncology guidance statement: the cost of cancer care. J Clin Oncol Off J Am Soc Clin Oncol. 2009;27(23):3868–74. doi: 10.1200/jco.2009.23.1183. [DOI] [PubMed] [Google Scholar]
- 28.Irwin B, Kimmick G, Altomare I, Marcom PK, Houck K, Zafar Y, et al. Patient experience and attitudes toward addressing the cost of breast cancer care. Oncologist. 2014 doi: 10.1634/theoncologist.2014-0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Souza JA, Wong YN. Financial distress in cancer patients. J Med Person. 2013;11(2) doi: 10.1007/s12682-013-0152-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bestvina CM, Zullig LL, Rushing C, Chino F, Samsa GP, Altomare I, et al. Patient-oncologist cost communication, financial distress, and medication adherence. J Oncol Pract Am Soc Clin Oncol. 2014;10(3):162–7. doi: 10.1200/jop.2014.001406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moriates C, Shah NT, Arora VM. First, do no (financial) harm. JAMA J Am Med Assoc. 2013;310(6):577–8. doi: 10.1001/jama.2013.7516. [DOI] [PubMed] [Google Scholar]
- 32.Henrikson NB, Tuzzio L, Loggers ET, Miyoshi J, Buist DS. Patient and oncologist discussions about cancer care costs. Support Care Cancer. 2014;22(4):961–7. doi: 10.1007/s00520-013-2050-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bullock AJ, Hofstatter EW, Yushak ML, Buss MK. Understanding patients’ attitudes toward communication about the cost of cancer care. J Oncol Pract. 2012;8(4):e50–8. doi: 10.1200/JOP.2011.000418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sommers R, Goold SD, McGlynn EA, Pearson SD, Danis M. Focus groups highlight that many patients object to clinicians’ focusing on costs. Health Aff. 2013;32(2):338–46. doi: 10.1377/hlthaff.2012.0686. [DOI] [PMC free article] [PubMed] [Google Scholar]


