Abstract
Objectives
To determine the prevalence of malnutrition using anthropometric measures among hospitalized pediatric and adult patients admitted at Bach Mai Hospital, Hanoi, Vietnam.
Methods
A one-day cross-sectional survey was used in selected wards (Pediatrics, Surgery, Intensive Care Unit, Renal Diseases, Gastroenterology Diseases, Respiratory Diseases, and Endocrinology). Unavailable patients and those discharged within 24 hours were excluded. Anthropometric data included body weight, height (or length), and mid-upper arm circumference. The type, severity, and prevalence rate of malnutrition were defined based on World Health Organization (WHO) criteria.
Results
The sample was hospitalized children and adults: 108 and 571 were children aged 6 months to 18.9 years old and adult patients, respectively. The overall rate of pediatric wasting (weight-for-height ≤−2 SD or BMI ≤−2 SD, kg/m2) was 19.0% (n=19/100) and that of stunting (height-for-age ≤−2 SD) was 13.9% (n=14/101). Using either the mid-upper arm circumference <11.5 cm or the weight-for-height and weight-for-length ≤−3 SD, the rate of severe wasting among children aged 6-59 months old was 7.0% (n=3/43). None of the children were obese based on weight-for-length, weight-for-height or BMI. In adults, the prevalence of under-nutrition (BMI<18.5 kg/m2) was 33.3% (n=141/423) while that of obesity (BMI≥30 kg/m2) was 0.9% (n=4/423). Adults admitted to the Respiratory Diseases ward had the highest prevalence of under-nutrition, 40.9% (n=38/93).
Conclusions
The prevalence of malnutrition was high in this cohort of hospitalized patients, particularly in adults, but comparable to other published reports. Obesity was nearly nonexistent in both children and adults.
Keywords: BMI, children, hospital malnutrition, nutrition assessment, Vietnam
INTRODUCTION
Malnutrition in hospitalized patients is common regardless of the country's income level. Malnutrition is associated with infectious and non-infectious complications and contributes to prolonged hospital stay, increased readmission rates, and higher morbidity and mortality. Based on anthropometric studies,1 the prevalence of undernutrition among hospitalized patients in various countries is estimated to reach 20%-50%, and may be lower among children (6%-32%).2 When overnutrition is taken into consideration, the rate of malnutrition can be as high as 50% in children and 76% in adults.3,4 However, there is limited data on rates of malnutrition among hospitalized patients in the country of Vietnam.
Although the overall nutritional status of Vietnamese citizens has improved dramatically over the past decade, malnutrition is still prevalent.5,6 At the time of developing our survey at Bach Mai Hospital (BMH), we identified two previously published studies in children ages 5 and under: one at Hue Hospital in Hue and one at Children's Hospital #1 in Ho Chi Minh City.7,8 Rates of wasting in children age five and under were similar in both hospitals, approximating 10%. There is a need for anthropometricin other age groups and hospitals in Vietnam as identifying inpatients nutrition risk is a prerequisite for optimizing nutrition support in hospitals.9
A joint collaboration between investigators at Boston University School of Medicine (BUSM), the Vietnamese National Institute of Nutrition (NIN), Hanoi Medical University (HMU) and staff and faculty of BMH facilitated the creation of a partnership entitled the Abbott Fund Institute of Nutrition Sciences (AFINS; Hanoi, Vietnam) with funding from the Abbott Fund, the foundation of the global health care company Abbott, to increase capacity for hospital-based clinical nutrition support and research.
To further document nutritional status in major Vietnamese hospitals, AFINS conducted a one-day cross-sectional anthropometric survey of all individuals hospitalized for at least 24 hours in select BMH patient wards as a nutritional status demonstration project in an urban general hospital in Vietnam.10
METHODS
Subjects and methods
A one-day cross-sectional anthropometric survey was performed to assess the nutritional status of hospitalized patients at BMH in Hanoi, Vietnam. BMH is a general hospital that serves as a referral hospital for North Vietnam and as a teaching hospital for HMU. The average daily number of patients varies with the seasons but is typicaly greater than 2000 per day.
This survey was part of a quality improvement project carried out in the Pediatrics, Surgery, ICU, Renal Diseases, Gastroenterology Diseases, Respiratory Diseases, and Endocrinology wards at BMH. At BMH patients are assigned to the pediatric ward if they are less than 16 years of age. Patients ages 16 years and older are assigned to the adult wards. The study was conducted in 3 wards on May 12 2010 and the 4 remaining wards, as well as repeating Pediatrics, on June 16 2010. All eligible patients in these wards were included in the study. The inclusion criteria were as follows: elective or urgent admission to the hospital for more than 24 hours, age one month (>30 days old) and older including both children and adult in-patients. Exclusion criteria included patients who were either discharged, unavailable (eg in surgery), died prior to obtaining the measurements, or those patients with physical impairment precluding anthropometric measurements. All participants signed an informed consent. Of the 718 patients admitted on the two days the study was conducted, 26 were excluded based on the study criteria, leaving 692 data for the analysis. Ten records were misplaced between data collection and data entry and have not been accounted for. From the 682 remaining study participants, 3 adult patients did not have either measured or recalled height, weight and mid-upper arm circumference and were removed from the final analysis. The final sample size was 679, including 571 adult patients at least 19 years of age and 108 children between the ages of 6 months and 18.9 years.
Approval to conduct this survey was obtained by the Ethical Committee of National Institute of Nutrition, Vietnam and the Institutional Review Board at the Boston University School of Medicine, Massachusetts, United States of America.
Data collection procedures
The survey was carried over a single defined day in adults but was repeated a second time one month later in pediatrics because the average number of patients admitted in the pediatric ward at BMH is typically around 60 compared with about 100 adults in each of the other wards surveyed. The data collectors included medical doctors and individuals with Bachelors in Science degrees from both NIN and the Clinical Nutrition Center at BMH, as well as medical students. All data collectors were trained prior to the survey to measure weight, height, and mid-upper arm circumference accurately. A list of admitted patients was obtained from each of the department administrative staff. A nurse introduced the investigators to the patients. After receiving a signed informed consent form, demographic data was collected and anthropometric measurements obtained.
General data
Demographic data was abstracted from the medical record to include age (for all inpatients, birth date for children under 5 years old), sex, and ward location. The age of patient was computed as months of age or years of age according to WHO definition for age.6
Anthropometric measurements
Body weight: For children under 16 kg, body weight was measured using a calibrated weighing scale (Laica, LAICA SPA, Italy) with a precision of 10 g. For children at or over 16 kg, body weight was measured using an eletronic weighing scale (Laica, LAICA SPA, Italy) with a precision of 100 g. For adults in the ICU, body weight was also measured with a bed scale (Tronix Bed scale 2002, New York, USA).
Body length: Children under 2 years of age or children had their body length measured using a United Nations Children's Fund (UNICEF) wooden board with a precision of 0.1 cm.
Body height: Body height measurement among children aged more than 2 years old was performed using locally made wooden boards (stadiometer) with a precision of one milimeter. Following WHO recommendations, for children aged more than 2 years old whose measurements were obtained in a supine rather than standing position, we subtracted 0.7 cm from their body length to provide an estimate of their body height (stature).
Mid-upper arm circumference: Measurement tapes provided by UNICEF were used to measure the left mid-upper arm circumference (MUAC) in cm with a precision of one millimeter.11
Body mass index: The body mass index (BMI) was calculated based on weight in kilogram divided by height in meters squared (kg/m2).
Definitions: Pediatric malnutrition can be defined as acute (wasting) or chronic (stunting) with different degrees of severity (mild, moderate, or severe). Malnutrition was defined according to WHO criteria for anthropometric parameters using z-scores or standard deviations (SD).6
Acute malnutrition was defined as wasting (or under-weight based on age with severity as degree of thinness) while chronic malnutrition was defined as stunting (shortness) or obesity (over-nutrition). For children aged 1 to 23 months old, we assessed wasting using weight-for-length z-scores (WLZ), for children aged 24 to 59 months old weight-for-height z-scores (WHZ), and MUAC while length-for-age z-scores (LAZ) or height-for-age z-scores (HAZ) was used for stunting and WLZ or WHZ for obesity. For children ages 2 years old (24 m) to 18 years old (18.9 y), we used the BMI-for-age z-scores (BMIZ) to assess for thinness and we used HAZ and BMIZ to assess for stunting and obesity, respectively. Finally, for adults, we used absolute BMI in kg/m2 to assess for underweight, overweight, and obesity. We also used MUAC with a cutoff point of 22 cm for females and 23 cm for males to report malnutrition rates especially in the Surgery and ICU wards where actual measurements for BMI were missing for more than half of the patients.12
Children were further classified according to their WLZ or WHZ to define severity of malnutrition: moderate wasting (or thinness) for those with WLZ or WHZ between −3 SD and <−2 SD and severe wasting for those with WLZ or WHZ <−3 SD. Children with MUAC measurements ranging between 11.5 to <12.5 cm were considered to have moderate wasting and those with measurements <11.5 cm to have severe wasting. Children were also classified according to their SD in LAZ or HAZ (length for those < 2 y and stature or adjusted length for those >2 y): moderate stunting was defined based on LAZ or HAZ ranging between −3 SD to <−2 SD and severe stunting was based on a HAZ or LAZ <−3 SD. Of note, children aged less than 2 years old were considered obese when their WLZ was at or >3 SD.
BMI was also used to categorize children and adults nutrition status. Children were classified according to their SD in BMIZ: severe wasting (<−3 SD), moderate wasting (−3 SD to < −2 SD), overweight (+1 SD to <+2 SD), and obesity (≥+2 SD). BMI was used to define overweight and obesity for children ≥2 years old. Absolute values of BMI were used to classify adult nutrition status in the following categories: underweight for BMI <18.5 kg/m2, overweight for BMI ranging between 25 to <30 kg/m2, and obesity for BMI was ≥30 kg/m2. Finally, acute malnutrition (underweight) was defined based on BMI <18.5 with severity of thinness as 18.5 to 17.0 (mild), <17 to 16.0 (moderate), and <16.0 (severe).6
Data analysis
A total of 679 patient records were analyzed for the study: 108 were pediatric patients under 19 years of age, and 571 were adults 19 years and older. A total of 100/108 (92.6%) children had both actual weight and height (stature or recumbent) measurements available, while 423/571 (74.1%) had both actual weight and height measurements available. As a result, the study sample considered for classification of malnutrition included 523 patients, of whom 100 were children and 423 were adults with actual height and weight measurements.
Children with at least 1 recalled or missing height or weight compared to children with actual measures of weight and height data were older (12.8±4.8 y vs. 7.3±5.6 y, p=0.01) but they did not differ significantly by mean MUAC measurements (193.3±34.9 mm vs. 171.1±31.8 mm, p=0.08). Compared to those adults with actual weight and height data, adults with at least 1 recalled or missing height or weight were more likely to be older (56.7±17.7 y vs. 51.4±16.4 y, p<0.01), and had a lower mean MUAC measurements (236.0±30.6 mm vs. 245.2±30.5 mm, p<0.01). However, adults with and without actual weight and height measures did not vary significantly by their underweight status based on BMI<18.5 kg/m2 (p=0.99).
All anthropometric parameters z-scores were calculated using the WHO reference data (2006) and WHO anthro software.6 Continuous data was described using means and standard deviation. We used the Student t-test for comparison of continuous data. Categorical data was expressed using absolute numbers and frequencies. We used Fisher's exact test and the Chi square test for categorical variables. A two-sided p value at <0.05 was used to define statistical significance. Analysis was performed using SPSS, version 13.0 (SPSS Inc, Chicago, IL, USA).
RESULTS
Demographic data
General and anthropometric characteristics of the 679 patients with and without actual weight and height measurements is described in Table 1. The adult patients were classified by ward location as follows: 111 (16.4%) from endocrinology, 90 (13.3%) from gastroenterology, 122 (18.0%) from renal/urology, 117 patients (17.2%) from respiratory, 117 (17.2%) from surgery and 29 (4.3%) from ICU and 93 patients (13.7%) from pediatric ward (Table 1). Patient ages ranged from 6 months to 87 years of age. The mean±SD age of children and adolescence was 7.6±5.7 y and that of adults and seniors was 52.8±16.9 y. The average length of stay from admission to the survey day was 10.2±11.2 days (Table 1). Further analysis to classify patients by their nutritional status are presented for those with complete weight and height measurements n=100 for pediatrics, n=423 for adults.
Table 1.
Inpatients characteristics at Bach Mai Hospital
| Characteristics | n | % | Mean±SD |
|---|---|---|---|
| Number of subjects by ward† | 679 | ||
| Endocrinology | 111 | 16.4 | |
| Gastroenterology | 90 | 13.3 | |
| Renal/Urology | 122 | 18.0 | |
| Respiratory | 117 | 17.3 | |
| Surgery | 117 | 17.3 | |
| ICU | 29 | 4.3 | |
| Pediatrics | 93 | 13.7 | |
| Gender (male) | 385 | 56.8 | |
| Subjects' age, y | |||
| Children and adolescents | 108 | 7.6±5.7 | |
| Adults | 571 | 52.8±16.9 | |
| Number of days in hospital, d | 679 | 10.2±11.2 | |
| Anthropometrics | |||
| Sample with actual weight and height | 523 | ||
| Pediatric | 100 | ||
| WLZ (6-23 m), z-score | 27 | −0.61±1.52 | |
| BMI (2-18.9 y), kg/m2 | 73 | 15.2±2.2 | |
| BMIZ (2-18.9 y), z-score | 73 | −1.27±1.53 | |
| Adult | 423 | ||
| BMI (≥19 y), kg/m2 | 423 | 20.0±3.2 | |
| Sample with recalled or missing measures | 156 | ||
| Pediatric | 8 | ||
| WLZ (6-23 m), z-score | 1 | −0.57 | |
| BMI (2-18.9 y), kg/m2 | 4 | 19.1±2.2 | |
| BMIZ (2-18.9 y), z-score | 4 | −0.54±1.32 | |
| Adult | 148 | ||
| BMI (≥19 y), kg/m2 | 139 | 19.6±2.9 | |
| Sample with MUAC, mm | 674 | ||
| MUAC (<5 y) | 42 | 152±22.4 | |
| MUAC ( 5-18.9 y) | 64 | 186±30.8 | |
| MUAC (>19 y) | 568 | 243±30.7 |
pediatric patients (<19 y) comprised the patient population in the following adult wards: Endocrinology <1% (1/111), Gastroenterology =1.1% (1/90), Renal/Urology 6% (6/112), Respiratory 2% (2/117), Surgery 5% (5/116).
ICU: intensive care unit; WLZ: weight-for-length z-score; BMI: body mass index; BMIZ: body mass index z-score; MUAC: mid-upper arm circumference.
The nutritional status of children aged 6 months to 18.9 years
The overall rate of acute malnutrition in the pediatric wards was 19% (19/100) (p<0.002). The mean WLZ for children between ages of 6 months and 23.9 months with actual height and weight measurements was −0.61±1.52 SD (Table 1). The mean BMI for children aged 2-18.9 years old was 15.2±2.2 kg/m2 and the mean BMIZ was −1.27±1.53 (Table 1). Based on WHZ <−2 SD, the prevalence of wasting was 19.0% (19/100) for children aged 6 months to 18.9 years, 14.8% (4/27) for children under 2 years of age, and 6.3% (1/16) for children aged 2 to 4.9 years. The prevalence of wasting according to BMIZ <−2 SD was 24.6% (14/57) for children aged 5 to 18.9 years (Table 2).
Table 2.
Nutrition status of children according to their age, Bach Mai Hospital, Hanoi, using actual measurements (n=100)
| Nutrition status | 6 to 23 m (n=27, %) | 2 to 4.9 y (n=16, %) | 5 to 18.9 y (n=57, %) | 6 m to 18.9 y (n=100, %) |
|---|---|---|---|---|
| Weight relative to height† | ||||
| Wasting or underweight | 4 (14.8) | 1 (6.3) | 14 (24.6) | 19 (19.0) |
| Severe thinness | 2 (7.4) | 0 (0.0) | 7 (12.3) | 9 (9.0) |
| Moderate thinness | 2 (7.4) | 1 (6.3) | 7 (12.3) | 10 (9.0) |
| Well nourished | 21 (77.8) | 15 (93.8) | 42 (73.7) | 78 (78.0) |
| Overweight‡ | 2 (7.4) | 0 (0.0) | 1 (18) | 3 (3.0) |
| Obese‡ | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Height relative to age | ||||
| Stunting | 3 (11.1) | 1 (6.3) | 10 (17.3) | 14 (13.9) |
| Severe | 2 (7.4) | 0 (0.0) | 3 (5.2) | 5 (5.0) |
| Moderate | 1 (3.7) | 1 (6.3) | 7 (12.1) | 9 (8.9) |
| No stunting | 24 (88.9) | 15 (93.7) | 48 (82.7) | 87 (86.1) |
Z-score of Weight-for-Length is used for children <24 months old and Z-score of Body Mass Index is used for children ≥24 months old (2y).
Overweight is defined as BMI from +1 SD to <+2 SD and obesity at >+2 SD, regardless of their age.
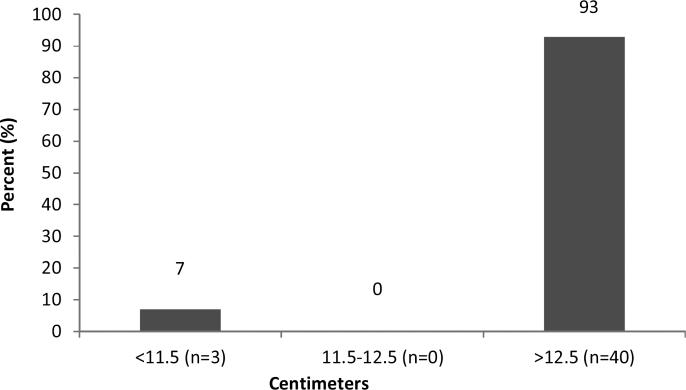
The overall prevalence of pediatric stunting (LAZ or HAZ <−2 SD) was 13.9 % (14/100) with 11.1% (n=3/27) for the under 2 years-old, 6.3% (n=1/16) for the 2-4.9 y and 17.3% (n=10/57) for the 5-18.9 y. There was no significant difference in wasting (p=0.17) and stunting (p=0.33) between under 5 years old and those 5-18.9 y. None of the children aged 6 months to 18.9 years old were considered obese and only 7.4% (2/27) were over-weight based on a WHZ >2 SD for those under 2 years of age and 1.8% (1/57) were overweight based on BMIZ >1 SD for those 5-18.9 y (Table 2). Using a cut off point for MUAC of 11.5 cm among children aged 6-59 months old, 7.0% (3/43) were considered severely wasted (Figure 1). None of the children had a MUAC ranging from 11.5-12.5 cm.
Figure 1.
Classification of wasting in children ages 6-59 months according to their mid-upper arm circumference (n=43)
The nutritional status among adult hospitalized patients (≥19 years old)
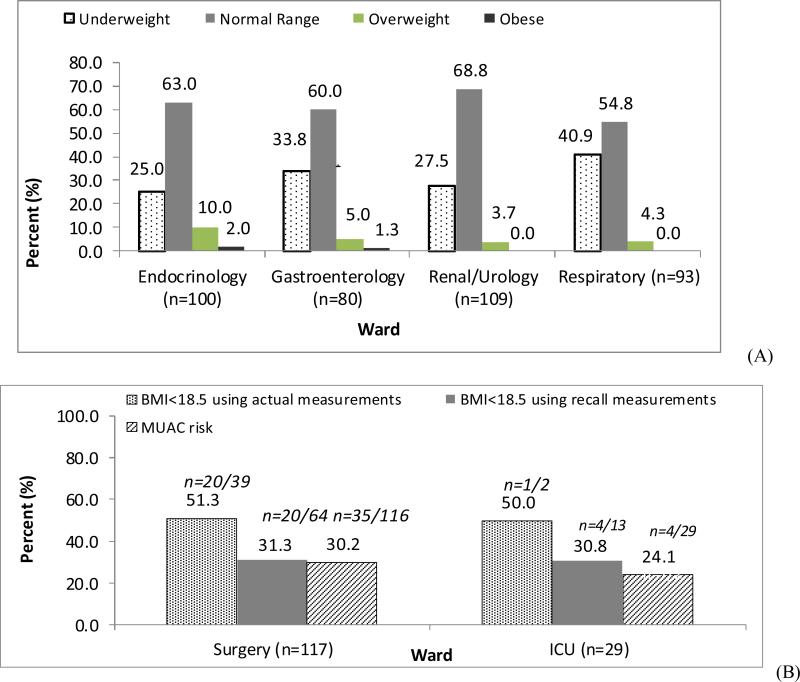
Like the children, adults (age ≥19 years) were classified based on WHO criteria. Using BMI, the prevalence rate of acute malnutrition (underweight) in adults was 33.3% (141/423), overweight 5.7% (24/423), and obesity 0.9% (4/423). Severity of acute malnutrition was also based on BMI categories: 8.0% (34/423) were severely underweight, 13.9% (59/423) were moderately underweight, and 11.3% (48/423) were mildly underweight.
The prevalence of acute malnutrition varied significantly according to the ward location (Figure 2A; p<0.001). The prevalence of acute malnutrition was 27.5% (30/109) in the renal/urology ward, 25.0% (25/100) in the endocrinology ward, 40.9% (38/93) in the respiratory ward, and 33.8% (27/80) in the gastroenterology ward (Figure 2 A). Using actual (rather than actual plus recall) measurements for BMI, the prevalence of acute malnutrition was 51.3% (20/39) in the surgery ward, and 50.0% (1/2) in the ICU ward. As opposed to BMI, most patient had a MUAC measured (571/574). Using MUAC <22 cm for females and <23 cm for males, the prevalence of malnutrition in all adult patients was 25.7% (n=147/571). In the surgery ward, 29.5% of patients were at malnutrition risk as determined by MUAC (n=33/112), and in ICU 24.1% of patients (n=7/29) (Figure 2B).
Figure 2.
Prevalence of adult malnutrition (≥ 19 y) in select wards. A. Nutrition status based on actual BMI. Definitions: Underweight BMI<18.5 kg/m2; Overweight BMI 25-30 kg/m2; Obese BMI≥30 kg/m2. B. Underweight based on recall BMI, actual BMI, and actual MUAC. Definition: Underweight: BMI<18.5 kg/m2 from actual measures; BMI<18.5 kg/m2 from recall measures; and, MUAC<23 cm for males and MUAC<22 cm for females. Abbreviations: BMI, body mass index; MUAC: mid-upper arm circumference; ICU: intensive care unit.
DISCUSSION
Our findings indicate that malnutrition is common among hospitalized patients in a major urban Vietnamese teaching hospital and varies significantly by age group and ward location. A total of 19.0% hospitalized pediatric patients aged 6 month to 18.9 years old and 33.3% hospitalized adults age >19 years old were considered to have malnutrition. As opposed to acute malnutrition, very few children and adults were categorized as overweight or obese. Stunting was highly prevalent among the hospitalized children. To our knowledge, this is the first anthropometric survey conducted in a Vietnamese urban general hospital designed to concomitantly assess the nutritional status of both pediatric and adult patients.
The rate of wasting and stunting among children age >6 months old at Bach Mai Hospital was 19.0% and 13.9%, which is similar to that of 19% observed in a recent nationwide survey of hospitals in the Netherlands (n=42).2 However, these authors noted that the rates of wasting were higher in academic (22%) compared with non-academic hospitals (17%), while stunting was significantly higher in non-academic versus academic hospitals (14% vs. 6%). This data is not currently available for comparison in Vietnam.
The prevalence rate of wasting in hospitalized children at Bach Mai hospital is comparable to that in other Vietnamese studies. Using WHZ, the prevalence rate of wasting among children 5 and under was 11.6% at Bach Mai Hospital compared to 16.4% at the National Pediatric Hospital in Hanoi,13 10.3% at Hue Central Hospital in Hue,7 and 9.3% at the Pediatric # 1 hospital, Ho Chi Minh City.8 Using BMIZ <−2 SD, the prevalence rate of wasting for children aged 5 to 18.9 years old was similar to that observed in the National Pediatric Hospital (24.6% vs. 25.4%).13 Although the pediatric rates of acute malnutrition at Bach Mai Hospital are within the 6% to 32% range identified in other countries.1,2
As opposed to other pediatric studies in Vietnam, we also used MUAC measurements to identify wasting among children ages 6-59.9 months old. Our results were comparable using either MUAC or WHZ data. In fact, MUAC was previously identified as a practical screening tool that performed at least as well as WHZ in predicting subsequent inpatient mortality among severely malnourished hospitalized children in Kenya.14 Although MUAC is not typically used in Vietnam in the hospital setting, it is inexpensive, more commonly available and easier to measure than WHZ, does not require growth charts for interpretation, and may thus be highly relevant for hospital-based nutrition interventions in this age group.
The rate of underweight among adults at Bach Mai Hospital was more than 1.5 times that reported in English hospitals but similar to that of a study conducted in Spain (26.7%; age >14 y).4,15 Data from the 1970s to the 1990s showed rates of hospital acute malnutrition ranging from 20% to 50%.1,16 Investigators have shown that rates of wasting varied with severity of diagnosis at admission.15 Our study showed that the highest prevalence rates of underweight admitted patients was in the surgery and the respiratory wards compared to the adult gastroenterology, renal/urology, and endocrinology wards, and the pediatric ward. Finally, there is some concerns that the rate of undernutrition in the endocrinology and gastroenterology ward at Bach Mai Hospital may be increasing compared to 5 years ago (25% vs 21.7% and 33.8% vs 28.9% respectively).17
It has been reported that undernutrition is an independent risk factor for higher morbidity, increased length of hospital stay, higher readmission rates, delayed recovery, lower quality of life as well as higher hospital costs and higher mortality. Many studies to date have demonstrated that appropriate enteral and parenteral nutritional support, as indicated based on gastrointestinal function, improves the nutritional status of the patients and potentially increases the effectiveness of treatment. Although nutrition support is one of the topics needing to be addressed in the formal recommendations issued by the Vietnamese Ministry of Health, specialized feeding options for patients and nutritional therapies not given adequate attention. Our findings showed evidence that may prompt policy makers, hospital leaders and clinicians to improve nutrition assessment and support activity in the hospital setting.18
The nutritional statuses of patients admitted in hospitals are typically different than those in the community. The rate of adult underweight in hospitalized patients (≥19 years of age) was much higher than that observed in the community (33.3% vs 17.2%).19 The prevalence of wasting in hospitalized children under 5 was higher than that observed in the community (11.6% vs 7.1%).19 However, the rate of stunting was less prevalent in hospitalized children than that observed in community (13.9% vs 29.3%) and that of obesity in children was nul at Bach Mai Hospital compared to the community (0% vs 2.8%).19 The high rate of malnutrition in our study may be explained by current referral patterns to a major urban tertiary care hospital, by the lack of nutrition care delivery standards during hospitalization, or both.
The main limitation of this study was related to the one-day cross-sectional design which precludes the identification of malnutrition resulting from hospitalization. Although weight measurements were performed only once on each patient using a variety of scales, all surveyors were trained prior to the survey and had a refresher course before the survey to minimize error of measurement. Although children with actual weight and height measurements were older, there was no significant difference in their nutrition status based on MUAC, which suggests that under- or over-estimate of malnutrition rates is unlikely. Hospitalized adults with both weight and height measurements were significantly more likely to have lower MUAC measurements than patients with at least 1 recall or missing height or weight. However, adult malnutrition rates based on MUAC <22 cm for females and <23 cm for males or BMI <18.5 kg/m2 did not differ between those with recall or actual measurements.12 Therefore, the rates of malnutrition observed in this study should be a good approximation of hospital malnutrition at Bach Mai Hospital. However, further evaluation in surgery and ICU wards need is warranted.
In summary, we found that the prevalence of malnutrition at Bach Mai Hospital, Hanoi, Vietnam was comparable to other published studies of hospitalized patients but the prevalence of malnutrition in adults was higher than that of children. As opposed to many other countries, the rates of obesity were nearly non-existent in both children and adults. Finally, we were able to reproduce the findings of a recent Kenyan study14 comparing WLZ and MUAC in children under 5 years old and to show that acute malnutrition defined based on BMI or MUAC in the ICU was comparable. These findings are highly relevant to the development and evaluation of hospital nutrition screening tools and nutrition support interventions.
ACKNOWLEDGEMENTS
We are grateful to all staff in Clinical Nutrition Department in National Institute of Nutrition and all staff in Clinical Nutrition Center, and related clinical wards in Bach Mai Hospital and all patients who participated in this survey.
AUTHOR DISCLOSURES
Funding support for the AFINS project in Viet Nam comes from the Abbott Fund (http://www.abbottfund.org). Dr Lenders is supported by National Institutes of Health grants P30 DK46200 and K23 DK082732 and the New Balance Foundation. Dr Ziegler is supported by National Institutes of Health grant K24 DK096574. Dr Apovian has participated on advisory boards for Amylin, Merck, Johnson and Johnson, Arena, Nutrisystem, Zafgen and Sanofi-Aventis, Orexigen, EnteroMedics and has received research funding from Lilly, Amylin, Aspire Bariatrics, GI Dynamics, Pfizer, Sanofi-Aventis, Orexigen, MetaProteomics, and the Dr. Robert C. and Veronica Atkins Foundation.
REFERENCES
- 1.Fuchs V, Mostkoff D, Salmeán GG, Amancio O. Nutritional status in hospitalized patients in a public hospital in Mexico City. Nutr Hosp. 2008;23:294–303. doi:10.1017/S1368980008004527. [PubMed] [Google Scholar]
- 2.Joosten KF, Hulst JM. Prevalence of malnutrition in pediatric hospital patients. Curr Opin Pediatr. 2008;20:590–6. doi: 10.1097/MOP.0b013e32830c6ede. doi: 10.1097/MOP.0b013e32830c6ed. [DOI] [PubMed] [Google Scholar]
- 3.Hendricks KM, Duggan C, Gallagher L, Carlin AC, Richardson DS, Collier SB, et al. Malnutrition in hospitalized pediatric patients. Arch Pediatr Adolesc Med. 1995;149:1118–22. doi: 10.1001/archpedi.1995.02170230072010. doi:10.1001/archpedi.1995.02170230072010. [DOI] [PubMed] [Google Scholar]
- 4.Planas M, Audivert S, Pérez-Portabella C, Burgos R, Puiggrós C, Casanelles JM, et al. Nutritional status among adult patients admitted to a university-affiliated hospital in Spain at the time of genoma. Clin Nutr. 2004;23:1016–24. doi: 10.1016/j.clnu.2004.01.003. doi:10.1016/j.clnu.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Khan NC, Khoi HH. Double burden of malnutrition: the Vietnamese perspective. Asia Pac J Clin Nutr. 2008;17:116–8. doi:10.1046/j.1440-6047.11.s1.2. [PubMed] [Google Scholar]
- 6.WHO . Child growth standards, methods and development. World Health organization; Geneva: 2006. [2014/3/30]; Available from: http://www.who.int/childgrowth/standards/technical_report/en/index.htm, http://www.who.int/childgrowth/standards/ac_for_age/en/index.html. doi:10.2471/BLT.11.040411. [Google Scholar]
- 7.Ha VTB. Malnutrition status of under five children, who come for health examine and treatment in Hue hospital 2005. J Food Nutr Sci. 2006;2:189–99. doi:10.3961/jpmph.2008.41.4.232. [Google Scholar]
- 8.Hoa NT, Tin HT, Khan NC. The nutritional status and risk factor of hospitalized patients with acute illness in the pediatric hospital Number 1. Ho Chi Minh City 2007. J Food Nutr Sci. 2008;4:202–12. doi:10.1080/07315724.2001.10719066. [Google Scholar]
- 9.Kondrup J, Allison SP, Elia M, Vellas B, Plauth M. ESPEN Guidelines for nutrition screening 2002. Clin Nutr. 2003;22:415–21. doi: 10.1016/s0261-5614(03)00098-0. doi:10.1016/S0261-5614(03)00098. [DOI] [PubMed] [Google Scholar]
- 10.Lenders CM, Henry E, the AFINS Group . Experimental Biology. Poster presentation; San Diego, CA: 2012. A global partnership to improve nutrition medicine in Vietnam. Boston Univ. Sch. of Med. and AFINS Ctr, Hanoi. p. 1028. [Google Scholar]
- 11.Gibson RS. Principles of nutritional assessment. Oxford University Press; New York: 1990. doi:10.1093/med/9780199558278.003.002. [Google Scholar]
- 12.Ferro-Luzzi A, James WPT. Adult malnutrition: simple assessment techniques for use in emergencies. Brit J Nutr. 1996;75:3–10. doi: 10.1079/bjn19960105. doi:10.1079/BJN199601. [DOI] [PubMed] [Google Scholar]
- 13.Huong PTT, Thu NN, Quyen TC, Huy ND, Lien DTK, Thuc LM, et al. Nutrition status of hospitalized children in Viet Nam. Abstract 537.. The 7 Asia Pacific Conference on Clinical Nutrition.; Bangkok, Thailand. 2011. http://www2.kenes.com/apccn/scientific/Pages/ListofAbstracts.aspx. [Google Scholar]
- 14.Berkley J, Mwangi I, Griffiths K, Ahmed I, Mithwani S, English M, et al. Assessment of severe malnutrition among hospitalized children in rural Kenya: comparison of weight for height and mid upper arm circumference. JAMA. 2005;294:591–7. doi: 10.1001/jama.294.5.591. doi:10.1001/jama.294.5.591. [DOI] [PubMed] [Google Scholar]
- 15.Edington J, Boorman J, Durrant ER, Perkins A, Giffin CV, James R, et al. Prevalence of malnutrition on admission to four hospitals in England. The Malnutrition Prevalence Group. Clin Nutr. 2000;19:191–5. doi: 10.1054/clnu.1999.0121. doi:10.1054/clnu.1999.0121. [DOI] [PubMed] [Google Scholar]
- 16.Barker LA, Gout BS, Crowe TC. Hospital malnutrition: prevalence, identification and impact on patients and the healthcare system. Int J Environ Res Public Health. 2011;8:514–27. doi: 10.3390/ijerph8020514. doi:10.3390/ijerph8020514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huong PT, Lam NT, Lien DTK, Ngoc NB, Quyen TC, Thu NN, et al. Nutritional status of inpatients in gastroenterology and endocrinology wards in Bach Mai Hospital. J Food Nutr Sci. 2006;2:85–90. [Google Scholar]
- 18.Stratton RJ, Green CJ, Elia M. Disease-related malnutrition. An evidence-based approach to treatment. CABI Publishing; Oxon: Wallingford, UK: 2003. doi:10.1079/BJN20031059. [Google Scholar]
- 19.National Institute of Nutrition, United Nations Children's Fund . A review of the nutritionsituation in Vietnam 2009-2010. Medical Publishing House; Hanoi: 2011. Available from: http://viendinhduong.vn/news/vi/134/89/a/so-lieu-thong-ke-ve-tinh-trang-dinh-duong-tre-em-qua-cac-nam.aspx. [Google Scholar]