Abstract
Objectives
The association between body mass index (BMI) and hot flash risk has not been specifically clarifies yet. This meta-analysis was, therefore, conducted to estimate the association between overweight and obesity and hot flash risk.
Methods
We searched PubMed, Web of Science, and Scopus for observational studies addressing the association between BMI and hot flash until August 2015. Data were independently extracted and analyzed using 95% odds ratio (OR), and confidence intervals (CI) based on the random-effects models.
Results
We identified 2,244 references and conducted seven studies with 4,219 participants. The association between hot flash and overweight was estimated 1.13 (95% CI: 0.97-1.32) and that of obesity was estimated 1.79 (95% CI: 1.52-2.11). No evidence of heterogeneity and publication bias was observed.
Conclusion
This meta-analysis demonstrated that, though not to a great extent, obesity does increase the risk of hot flash. The findings from this meta-analysis indicated that obesity is associated with an increased risk of hot flash. Further large prospective cohort studies are required to provide convincing evidence as to whether or not BMI is associated with an increased risk of hot flashes.
Keywords: Body mass index, Case-control studies, Cohort studies, Hot flashes, Meta-analysis
Introduction
Approximately 40% to 70% of midlife women experience hot flashes in menopausal transition periods.1 Hot flashes in midlife women last for a few months, around five years and, in certain cases, even up to 30 years.1 Hot flashes are characterized by the decrease in and the loss of ovarian activity following the reduction in estrogen, permanent cessation of menstruation and loss of reproductive ability.2 Such disease often causes sleep disturbance, fatigue, irritability, forgetfulness, acute physical discomfort and work problems.1
The symptom of hot flashes was known to be affected by various factor such as current and former smoking, older age, hormone levels, tubal ligation, depressive symptom surgical menopausal and race.1,3,4,5
Some studies, however, reported that body mass index (BMI) is the factor related to hot flashes.1 Several epidemiological studies have revealed the relationship between BMI and hot flash, but the results are not consistent.2,6,7 Some studies have reported a positive association between obesity and hot flash2,6,8,9 while others have not.7,10,11
To our knowledge, no meta-analysis has addressed the association between BMI and hot flash in midlife women, hence the present meta-analysis conducted to estimate the overall effect of overweight and obesity on hot flash based on the current evidence.
Materials and Methods
1. Criteria for including studies
Cohort, case-control, and cross-sectional studies were included so as to address the relationship between BMI and hot flash, irrespective of age, race, publication date and language. The exposure of interest was overweight and obesity. BMI, the body mass (kg) divided by the square of the body height (m) is categorized into underweight (< 18.5 kg/m2), normal weight (18.5-24.9 kg/m2), overweight (25-29.9 kg/m2) and obese (≥ 30 kg/m2).12
2. Search methods
We employed a search strategy along with a set of keywords including (hot flush or hot flash) and (BMI or body size or obese or obesity or overweight). Major electronic databases including PubMed, Web of Science, and Scopus were searched until August 2015. In order to find additional references, the reference lists of the included studies were screened. In addition, we contacted the authors of the studies for more potentially eligible studies. Furthermore, the following conference databases were searched:
·The 8th European Congress on Menopause (EMAS); available from: www.maturitas.org/article/S0378-5122(09)70260-9/abstract
·The North American Menopause Society (NAMS); available from: http://www.menopause.org/annualmeetings
3. Data collection and analysis
Two authors independently made the decision on which studies met the inclusion criteria for the objective of this meta-analysis. Any disagreement was resolved after a discussion by the authors. Two authors extracted the data from the included studies. The variables extracted for analysis contained the first author's name, the year and the country where the study was conducted, study design, age mean/range (year), sample size, the effect measure and its 95% confidence interval (CI).
We assessed the risk of bias among the included studies using Grades of Recommendation, Assessment, Development, and Evaluation (GRADE) considering the following key elements: limitation, consistency, directness, precision, reporting bias, strength, gradient, and confounding.13
4. Heterogeneity and publication bias
The statistical heterogeneity was explored using the Q-test. The I2 statistic was used for assessing inconsistency in the results.14 The publication bias was explored employing the Egger's15 and Begg's16 tests and was visualized using a funnel plot.
The odds ratio (OR) and its associated 95% CI were mentioned as a measure of the connection between hot flash and overweight and obesity. Wherever reported, we used the full adjusted forms of OR controlled for at least one or more of the potential confounding factors such as age, smoking, Hormone therapy, race, herbal supplement, tubal ligation, parity, and menopause. Data were analyzed and the results were reported making use of a random-effects model.17 Since the results and the number of the included studies were respectively homogenous and limited, no subgroup analysis was performed. All statistical analyses were performed at a significance level of 0.05 employing Stata software, version 11 (StataCorp, College Station, TX, USA) and Review Manager 5.
Results
1. Results of the search
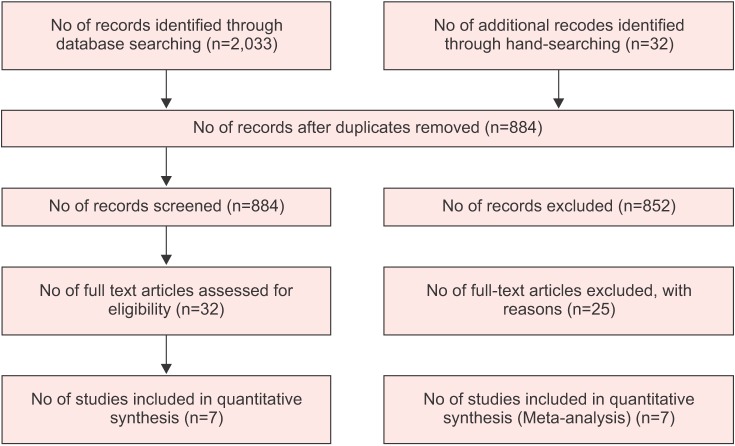
We identified 2,244 references, 2,033 references through searching electronic database and 211 references after checking reference lists. No reference was found through searching conference databases. One thousand two hundred two duplicates and 1,004 irrelevant references were excluded after reading titles and abstracts, while 31 were excluded after reviewing full texts (Fig. 1). Seven studies remained for the final meta-analysis which included 4,219 participants: two cohort,4,9 two cross-sectional,1,2 and three case-control.6,8,18
Fig. 1. Flow of information through the different phases of the meta-analysis.
2. Effects of exposure
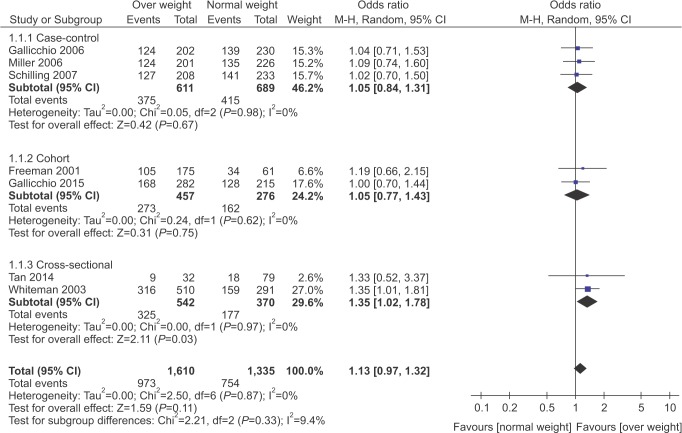
The relationship between overweight and hot flash is shown in Fig. 2. Based on OR estimates obtained from case-control and cohort studies, there was no significant association between hot flash and overweight (1.13; 95% CI: 0.97-1.32).
Fig. 2. Forest plot of the association between hot flash and overweight. CI: confidence interval.
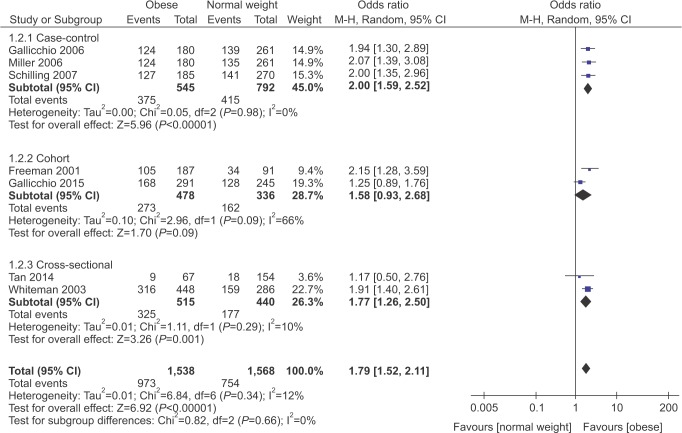
The connection between obesity and hot flash is illustrated in Fig. 3. As can be seen, unlike overweight, a significant association exists between hot flash and obesity (1.79; 95% CI: 1.52-2.11).
Fig. 3. Forest plot of the association between hot flash and obesity. CI: confidence interval.
3. Heterogeneity and publication bias
The I2 statistics and Cochran homogeneity test revealed no evidence of heterogeneity among the included studies addressing the association between hot flash and overweight (0%, P = 0.87) and obesity (10%, P = 0.29).
Publication bias was explored using Begg's and Egger's tests and was visualized employing a funnel plot. The Egger regression test and Begg's test revealed no evidence of publication bias among the included studies that addressed addressing the association between hot flash and overweight (P = 0.911 and P = 0.138) and obesity (P = 0.877 and P = 0.621), respectively. No evidence of publication bias was observed in the funnel plots (Fig. S1, S2 in supplement files) either.
The quality of the studies assessed using GRADE. The five studies were moderate in quality while the two other studies had low qualities (Table S1 in supplement files).
Discussion
The results of this meta-analysis indicated that overweight and obesity may increase the risk of hot flashes. One finding in this review was an apparent dose-response relationship between BMI and a hot flash where the risk of a hot flash was higher among obese women than overweight women; the higher the BMI, the higher the risk of hot flash is. it should be noted that a dose-response relationship is strong evidence for a causal relationship.19 Although no heterogeneity was observed in the included studies, owing to the limited number of studies there was little evidence as to the association between BMI and hot flash.
The results of this meta-analysis indicated that obesity is associated with an increased risk of hot flash which is inconsistent with the long-standing hypothesis that heavier women have higher endogenous estrogen levels and thus run a lower risk of hot flashes.20 The studies reported that obese women had a significantly lower mean estradiol level than women of normal weight from the age of 45 to 52 years. In analyses of BMI and estrogen levels, BMI was negatively associated with estradiol levels and, to a lesser extent, estrone levels in midlife women.18
In addition to the hypotheses suggesting that obese women may experience earlier ovarian insufficiency, other studies support to the findings of the present research. Forming estrogens from circulating androgen precursors, adipose tissue also produces hormones such as leptin and causes tumor necrosis that may inhibit ovarian steroid production, thus increasing the risk of hot flashes.21,22 Thurston et al.23 reported that associations between adipokines, adiposity, and hot flashes changed by menopausal stage in midlife, with hot flashes being associated with an adverse adipokine profile early, but not late, in the menopausal transition.
Additionally, in a study by Avis et al.24 in 2015, women with greater BMI had longer durations of total vasomotor symptoms and were more liable to develop hot flashes with higher adiposity.
Vasomotor symptoms in menopause women may increase the odds of cardiovascular disease. Szmuilowicz and Manson25 reported in 2011 that women with a history of early vasomotor symptoms did not develop future clinical cardiovascular disease or all-cause mortality. The risks of stroke and total cardiovascular disease events were reduced among women with early vasomotor symptoms, but late vasomotor symptoms were associated with increased risk of major coronary heart disease and all-cause mortality.25
This meta-analysis had a few limitations and potential biases, the most important of which was the limited number of eligible studies. Second, we attempted to use an adjusted form of OR estimates, while some studies did not report adjusted forms of effect measure,2,9 an issue which may result in information bias. Third, hot flash data were obtained by self-reports that could possibly be produced by other diseases, an issue which may lead to selection bias. Finally, we found 'ONE' study that seemed potentially eligible to be included in this meta-analysis, but we could not access the full text of this study. This issue may raise the possibility of selection bias.
This meta-analysis demonstrated that, though not to a great extent, obesity does increase the risk of hot flash. Further large prospective cohort studies are required to provide convincing evidence as to whether or not BMI can heighten the risk of a hot flash.
Acknowledgement
This article is a part of the PhD thesis supported by Hamadan University of Medical Sciences. We would like to thank the Vice-chancellor of education, as well as the Vice-chancellor of research and technology of the University for their Financial Support.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
Supplementary Materials
Quality assessment of studies addressing the association between body mass index and cervical cancer risk
Funnel plot of included studies addressing the association between hot flash and overweight.
OR: odds ratio.
Funnel plot of included studies addressing the association between hot flash and obesity.
OR: odds ratio.
References
- 1.Whiteman MK, Staropoli CA, Benedict JC, Borgeest C, Flaws JA. Risk factors for hot flashes in midlife women. J Womens Health (Larchmt) 2003;12:459–472. doi: 10.1089/154099903766651586. [DOI] [PubMed] [Google Scholar]
- 2.Tan MN, Kartal M, Guldal D. The effect of physical activity and body mass index on menopausal symptoms in Turkish women: a cross-sectional study in primary care. BMC Womens Health. 2014;14:38. doi: 10.1186/1472-6874-14-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freeman EW, Sherif K. Prevalence of hot flushes and night sweats around the world: a systematic review. Climacteric. 2007;10:197–214. doi: 10.1080/13697130601181486. [DOI] [PubMed] [Google Scholar]
- 4.Gallicchio L, Miller SR, Kiefer J, Greene T, Zacur HA, Flaws JA. Risk factors for hot flashes among women undergoing the menopausal transition: baseline results from the Midlife Women\'s Health Study. Menopause. 2015;22:1098–1107. doi: 10.1097/GME.0000000000000434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gold EB, Block G, Crawford S, Lachance L, FitzGerald G, Miracle H, et al. Lifestyle and demographic factors in relation to vasomotor symptoms: baseline results from the Study of Women\'s Health Across the Nation. Am J Epidemiol. 2004;159:1189–1199. doi: 10.1093/aje/kwh168. [DOI] [PubMed] [Google Scholar]
- 6.Schilling C, Gallicchio L, Miller SR, Langenberg P, Zacur H, Flaws JA. Relation of body mass and sex steroid hormone levels to hot flushes in a sample of mid-life women. Climacteric. 2007;10:27–37. doi: 10.1080/13697130601164755. [DOI] [PubMed] [Google Scholar]
- 7.Whiteman MK, Staropoli CA, Langenberg PW, McCarter RJ, Kjerulff KH, Flaws JA. Smoking, body mass, and hot flashes in midlife women. Obstet Gynecol. 2003;101:264–272. doi: 10.1016/s0029-7844(02)02593-0. [DOI] [PubMed] [Google Scholar]
- 8.Miller SR, Gallicchio LM, Lewis LM, Babus JK, Langenberg P, Zacur HA, et al. Association between race and hot flashes in midlife women. Maturitas. 2006;54:260–269. doi: 10.1016/j.maturitas.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Freeman EW, Sammel MD, Grisso JA, Battistini M, Garcia-Espagna B, Hollander L. Hot flashes in the late reproductive years: risk factors for Africa American and Caucasian women. J Womens Health Gend Based Med. 2001;10:67–76. doi: 10.1089/152460901750067133. [DOI] [PubMed] [Google Scholar]
- 10.Gallicchio L, Miller SR, Kiefer J, Greene T, Zacur HA, Flaws JA. Change in body mass index, weight, and hot flashes: a longitudinal analysis from the midlife women's health study. J Womens Health (Larchmt) 2014;23:231–237. doi: 10.1089/jwh.2013.4526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gallicchio L, Visvanathan K, Miller SR, Babus J, Lewis LM, Zacur H, et al. Body mass, estrogen levels, and hot flashes in midlife women. Am J Obstet Gynecol. 2005;193:1353–1360. doi: 10.1016/j.ajog.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 12.Bauman WA, Korsten MA, Radulovic M, Schilero GJ, Wecht JM, Spungen AM. 31st g. Heiner sell lectureship: secondary medical consequences of spinal cord injury. Top Spinal Cord Inj Rehabil. 2012;18:354–378. doi: 10.1310/sci1804-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schünemann HJ, Brożek J, Guyatt G, Oxman AD. GRADE handbook for grading quality of evidence and strength of recommendations. Orlando, FL: The GRADE Working Group; 2013. [cited by 2013 Oct 30]. Available from: www.guidelinedevelopment.org/handbook. [Google Scholar]
- 14.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- 17.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 18.Gallicchio L, Miller SR, Visvanathan K, Lewis LM, Babus J, Zacur H, et al. Cigarette smoking, estrogen levels, and hot flashes in midlife women. Maturitas. 2006;53:133–143. doi: 10.1016/j.maturitas.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 19.Gordis L. Epidemiology: with STUDENT CONSULT online access. 5th ed. Philadelphia, PA: Saunders; 2014. [Google Scholar]
- 20.Klinga K, von Holst T, Runnebaum B. Influence of severe obesity on peripheral hormone concentrations in pre- and postmenopausal women. Eur J Obstet Gynecol Reprod Biol. 1983;15:103–112. doi: 10.1016/0028-2243(83)90178-8. [DOI] [PubMed] [Google Scholar]
- 21.Rice VM, Williams VR, Limback SD, Terranova PF. Tumour necrosis factor-alpha inhibits follicle-stimulating hormoneinduced granulosa cell oestradiol secretion in the human: dependence on size of follicle. Hum Reprod. 1996;11:1256–1261. doi: 10.1093/oxfordjournals.humrep.a019368. [DOI] [PubMed] [Google Scholar]
- 22.Zachow RJ, Magoffin DA. Direct intraovarian effects of leptin: impairment of the synergistic action of insulin-like growth factor-I on follicle-stimulating hormone-dependent estradiol-17 beta production by rat ovarian granulosa cells. Endocrinology. 1997;138:847–850. doi: 10.1210/endo.138.2.5035. [DOI] [PubMed] [Google Scholar]
- 23.Thurston RC, Sowers MR, Sutton-Tyrrell K, Everson-Rose SA, Lewis TT, Edmundowicz D, et al. Abdominal adiposity and hot flashes among midlife women. Menopause. 2008;15:429–434. doi: 10.1097/gme.0b013e31815879cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Avis NE, Crawford SL, Greendale G, Bromberger JT, Everson-Rose SA, Gold EB, et al. Duration of menopausal vasomotor symptoms over the menopause transition. JAMA Intern Med. 2015;175:531–539. doi: 10.1001/jamainternmed.2014.8063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Szmuilowicz ED, Manson JE. Menopausal vasomotor symptoms and cardiovascular disease. Menopause. 2011;18:345–347. doi: 10.1097/gme.0b013e318209239a. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Quality assessment of studies addressing the association between body mass index and cervical cancer risk
Funnel plot of included studies addressing the association between hot flash and overweight.
OR: odds ratio.
Funnel plot of included studies addressing the association between hot flash and obesity.
OR: odds ratio.