Abstract
Objectives
Menopause can have psychological, physical, and vasomotor symptoms along with sexual dysfunction and these symptoms can affect the quality of life (QOL). The purpose of this research was to determine and association the effective factors on QOL among postmenopausal Iranian women.
Methods
This cross-sectional study was conducted in 2015 on 300 postmenopausal women in Hamadan, Iran. We used the Menopause-Specific QOL questionnaire (MENQOL) for measuring QOL in postmenopausal women. SPSS version 16 was used for data analysis.
Results
The mean scores of QOL for vasomotor, psychosocial, physical, and sexual domains were 11.65 ± 5.93, 19.36 ± 1.20, 39.12 ± 1.95 and 11.02 ± 5.66, respectively. Higher scores had worse QOL. Using MENQOL scores, our study showed significant differences in QOL based on age, education level, financial status, number of children, employment, and body mass index (BMI).
Conclusion
Menopause causes a decrease in QOL, which is dependent to age, work, BMI, financial status and number of children variables. Therefore, it is necessary to develop effective intervention programs to improve QOL in postmenopausal women.
Keywords: Cross-sectional studies, Iran, Menopause, Quality of life
Introduction
Natural menopause is the permanent cessation of menstruation which is determined 12 months after the last menstrual period.1 The number of postmenopausal women has been increasing in recent years due to the increase of life expectancy.2,3 Nowadays, most women spend more than one-third of their life beyond their menopause.4 The etiology of menopause is not well-known. However, it seems that it is related to ovarian dysfunction and hormonal changes.5
Nearly, 50% to 80% of women complain of menopausal symptoms such as hot flashing, sweating, sleep disturbance, tiredness, and depression.6
Menopause can have psychological, physical, and vasomotor symptoms along with sexual dysfunction.5,7,8 These symptoms can affect the quality of life (QOL). According to the World Health Organization (WHO), QOL is defined as "an individual's perception of their position in the context of the culture and value systems in which they live and in relation to their goals".9,10
A review study in 2015 reported that different sociodemographic factors such as body mass index (BMI), marital dimension, economic dimension, educational level, working status, duration of menopause, parity, and race affected the QOL in menopausal women.11
Iranian culture give special value and importance on the elderly and older women have a significant place in the culture because of their extensive experience as mothers and wives. In addition, some of the values women hold in Iran might be at risk due to mood fluctuations and other challenges might occur related to QOL.12 Only a few studies showed the association between socio-demographic factors and QOL among postmenopausal women.13
Therefore, the purpose of this cross-sectional research was to determinate the effective factors on QOL among postmenopausal Iranian women.
Materials and Methods
This cross sectional study was conducted in 2015. We enrolled eligible postmenopausal women in Hamadan city located in the west of Iran from June 2015 to October 2015. This research was approved in the Ethics Committee of Hamadan University of Medical Sciences.
According to the results of a cross-sectional study conducted by Makvandi et al.14 in Iran, the mean (standard deviation [SD]) QOL in postmenopausal women was 9.72 (3.27). Based on these results, we arrived at a total sample size of 280 at 95% significance level. Anticipating an 8% rejection due to failure in completing the questionnaire, we increased the sample size to a maximum of 300 women. For this purpose, we prepared a list of all the 20 health centers in Hamadan city and categorized them into four different areas based on socio-demographic status. Eligible women were selected randomly based on quotas set for each health center and their names and numbers were listed. If a woman was absent for the interview, she was given a second chance. In case a woman was not present, we selected another woman from the center.
Inclusion criteria consisted of women (a) from whose last menstrual period at least 1 year had passed (b) had intact uterus and ovaries (c) had no history of physical and mental disorders (d) and had not used hormone replacement therapy. Exclusion criteria consisted of women who participated in classes of promoting QOL.
We used the Menopause-Specific QOL (MENQOL) questionnaire for measuring the QOL in postmenopausal women. This questionnaire consists of 29 items in vasomotor (3 items), psychosocial (7 items), physical (16 items) and sexual (3 items) domains.15 The validity and reliability tests for this questionnaire were conducted in Iran.16 In this study, test-retest (intraclass correlation coefficients) was used for the MENQOL questionnaire reliability. The scores of MENQOL questionnaire were 0.93, 0.88, 0.87, and 0.92 for the physical, psychological, sexual and vasomotor domains, respectively.
This questionnaire has seven-point Likert scale and ranges from 0 to 7. A "zero" is equivalent to a woman responding "no", showing she has not experienced this symptom in the past month. Score "one" shows that the woman experienced the symptom, but it was not bothersome at all. Scores "two" through "seven" show increasing levels of bother experienced from the symptom and correspond to "1" through "6" check boxes on the MENQOL. Each item was manually calculated into a 0-7 score. Hence, the average for each domain was calculated between 0 and 7. The high scores in MENQOL subscales indicate low QOL.
Moreover, some socio-demographic variables were asked from these women including age, menopause duration, marital status, education, employment status, number of children, income level, weight, and height. BMI is weight in kilograms divided by the square of the height in meters. BMI is divided into underweight (<18.5 kg/m2), normal weight (18.5-24.9 kg/m2), overweight (25-29.9 k/m2) and obese (≥30 kg/m2).17
The postmenopausal women were interviewed by female interviewer and on average, each interview lasted 19 minutes.
SPSS version 16 (SPSS Inc., Chicago, IL, USA) was used for data analysis. The relation of demographic variables with QOL was investigated using analysis of variance (ANOVA), t-test and logistic regression analysis. P values less than 0.05 were considered significant.
Results
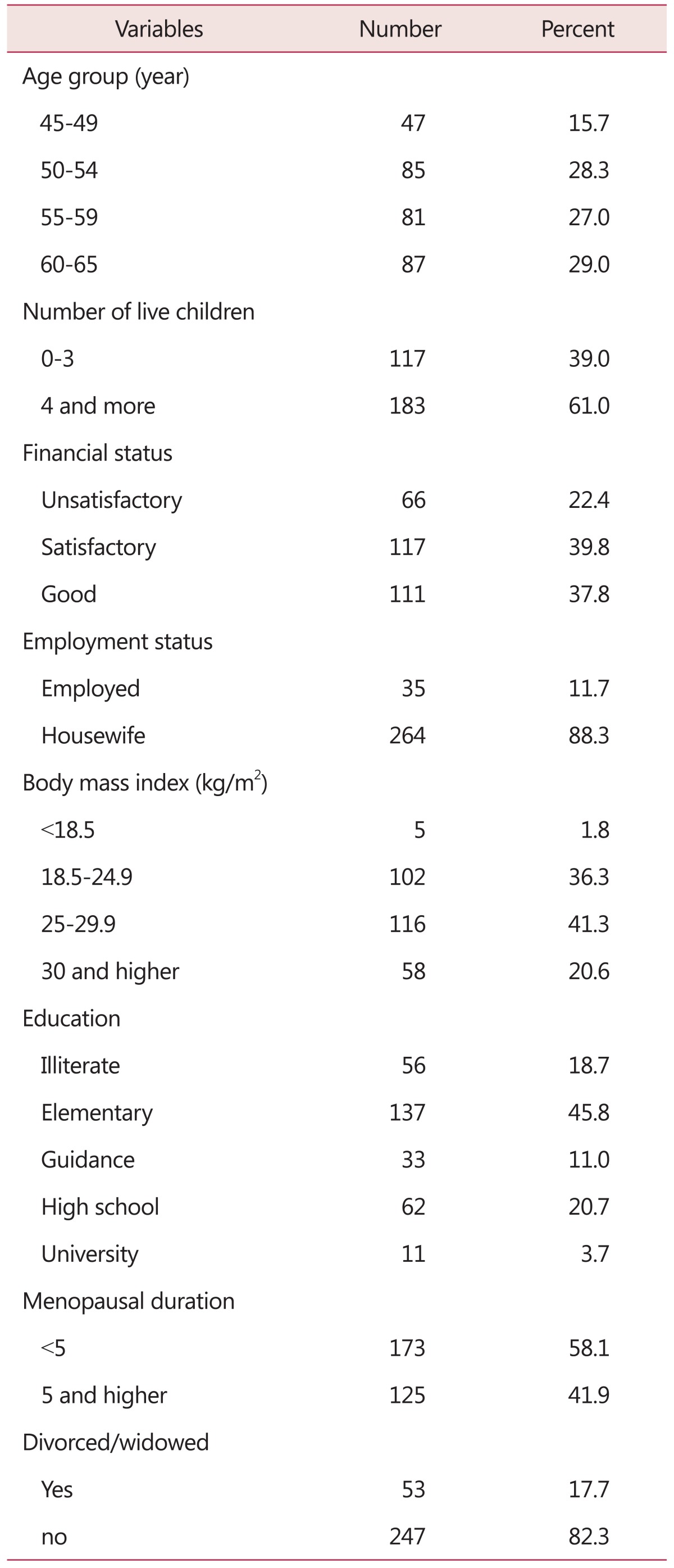
Overall, 11 women refused to participate in this study and were replaced by other eligible women. The age range of women was 45 to 65 years and the mean age was 55.46 (SD = 5.49).
Most of the women (48%) had between 4 to 6 lvie children. 41.3% of the menopausal women had overweight. The mean BMI in postmenopausal women was 26.48 (SD = 4.48). Table 1 shows the characteristics of the eligible women. The mean (median) scores of QOL for vasomotor, psychosocial, physical and sexual domains were 11.65 ± 5.93 (median: 12), 19.36 ± 1.20 (median: 18), 39.12 ± 1.95 (median: 39) and 11.02 ± 5.66 (median: 12), respectively.
Table 1. Characteristics of the participating women.
According to the MENQOL questionnaire most mean scores in vasomotor, psychosocial, physical and sexual domains belong to the items of "night sweats" (4.17 ± 2.08), "feeling anxious or nervous" (3.34 ± 2.14), "ache in muscles and joints" (3.41 ± 2.04) and "change in your sexual desire" (3.77 ± 2.11), respectively.
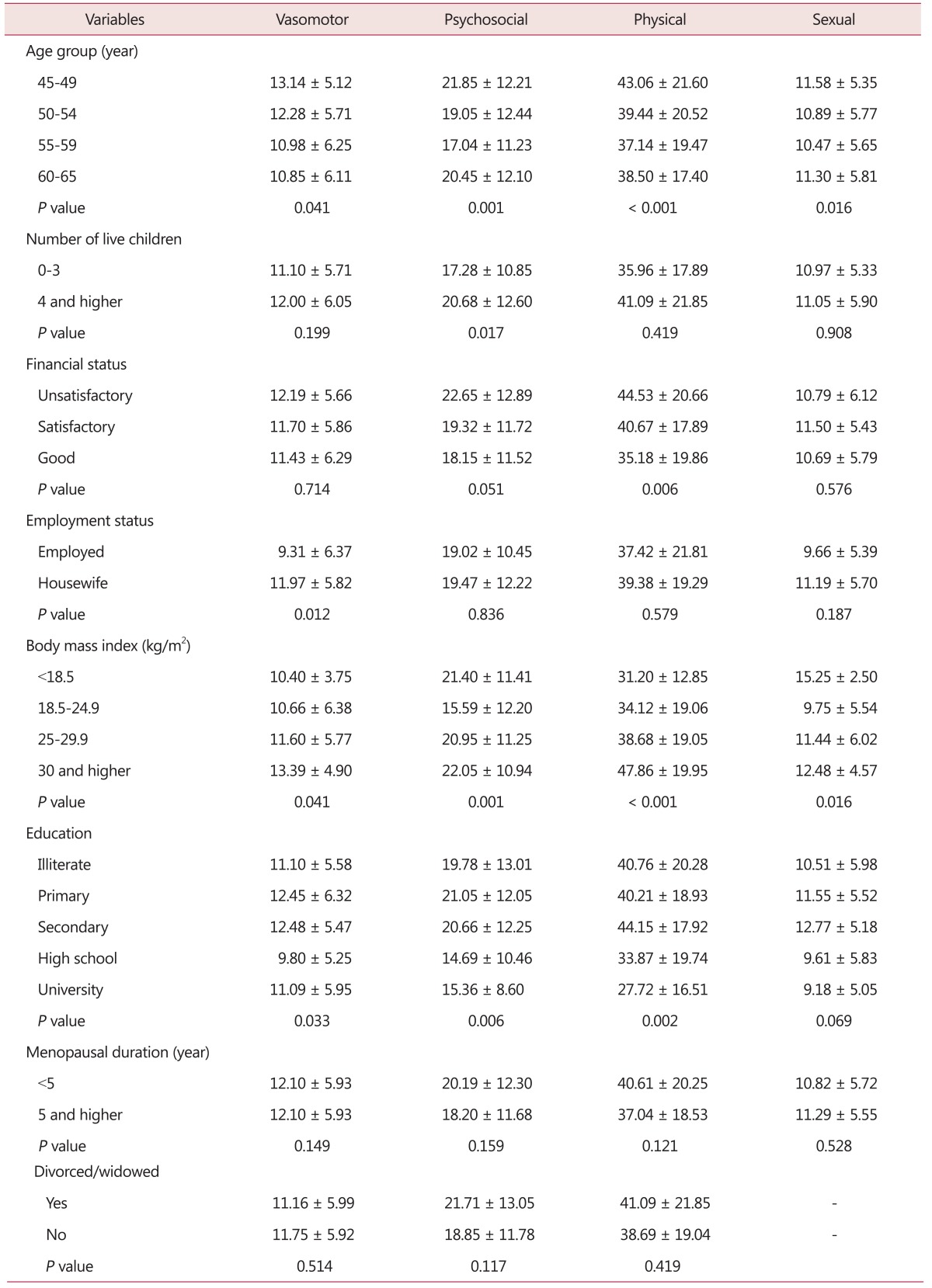
The mean score of QOL in four domains have been presented in Table 2. Sixty to 65 years old women had significantly lower QOL scores (better QOL) in psychosocial, physical and sexual domains compared with the other age group and 45 to 49 years old women had significantly higher scores in all the domains of QOL.
Table 2. Mean scores of quality of life per item in postmenopausal women.
Women with university degrees had the lowest scores in the physical domain and the highest scores of sexual, physical and vasomotor domains belonged to women with guidance school degrees.
Women with fewer than four live children had lower QOL scores in psychosocial domain (P = 0.017). Compared to married women, divorced/widowed women did not affect all the domains of QOL.
Financial status was associated with physical domain and women with higher incomes had lower scores in QOL compared with other groups.
Women with higher BMI had significantly higher scores in all the QOL domains. Menopausal duration was not associated with all the domains of the QOL. In vasomotor domain employed women had lower scores than housewives (P = 0.012).
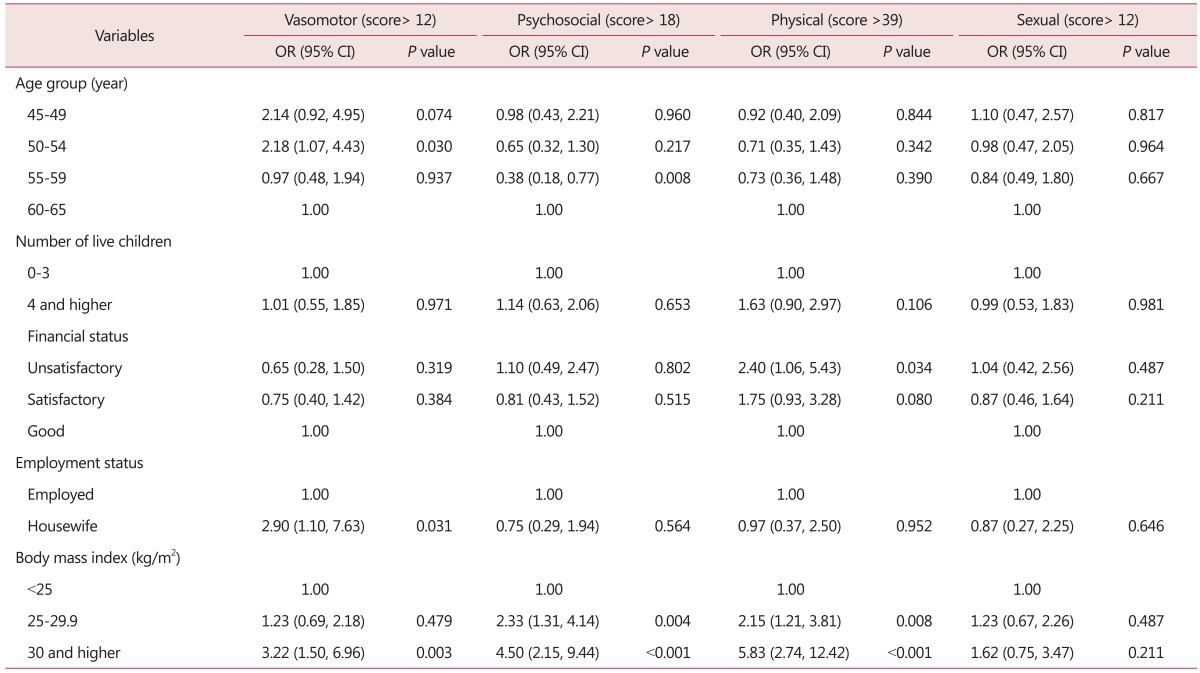
According to the results of the logistic regression analysis after adjusted variables, obesity increased scores of physical, psychosocial and vasomotor above the median. Employment and incoming decreased the risk of vasomotor and physical scores above the median, respectively (Table 3).
Table 3. The multivariate predictors of different items of the quality of life of associated with presenting higher score (above the median) in postmenopausal women.
OR: odds ratio, CI: confidence interval
Discussion
In our study, 45 to 49 years old women had significantly higher scores in all the QOL domains. Aging in women decreased the scores of QOL except for 60 to 65 years old women whose scores increased again in psychosocial, physical and sexual domains. Aging in vasomotor domain decreased QOL scores. Fallahzadeh's study16 shows the lowest scores for 60 to 65 years old women in the vasomotor domain which is in agreement with our study, while Blumel et al.'s study18 in Chile could not show a significant relation between aging and QOL. Some studies have shown that age is a predictor of reduction in QOL.19,20
In our study, women with university degrees had lower scores in all domains but this association was significant in vasomotor, psychological and physical domains. Similar results have been reported in different studies.21,22,23 In contrast, Fallahzadeh's study16 showed that women with university degrees had the highest mean scores in vasomotor domain. These studies show that knowledge and education are the reason for having fewer problems and a better QOL. Having an education makes a positive contribution to women's lives in that they reach a higher level of income.
In this study, employed women had lower scores in QOL in vasomotor domain. This is similar to the study of Blumel et al.18 Another study13 reported that working women had lower scores of QOL compared to housewives which was not significant. The employed women seemed that had better social support.
Women with more than three children obtained higher scores of QOL compared to those who had fewer than four children, this difference was significant in psychosocial domain. This is similar to other studies.13 Fallahzadeh16 in Iran reported that the number of children had a significant impact on physical domain scores. A study defined that higher number children could increased parental stress and responsibility as well as financial problems.24
Women with lower incomes had significantly higher mean scores in physical and psychosocial domains. This is similar to Fallahzadeh's study.16
Daley et al.25 reported that obese women had significantly higher vasomotor and somatic symptoms than women of normal weight. A review study reported that obesity was associated with a poor health-related QOL in postmenopausal women.26 In our study, a high BMI predictor higher scores in vasomotor, psychosocial and physical domains of QOL. Obesity is a health problem that can decrease QOL in postmenopausal women.22
Based on the present study, duration of menopause did not have any impact on QOL, and this finding has been confirmed by another study.13 In contrast, Caylan et al.27 reported that duration of menopause was associated with higher scores in psychosocial, physical and sexual domains in QOL. It seems that low QOL more than four years after menopausal duration may be due to various factors such as race, age and culture.28
This study assessed QOL and related factors in postmenopausal women in Iran. Our study had a few limitations: (a) the women self-reported their weight and height. The literature shows that overweight and obese women are more likely to under-report their weight while those who are underweight are more likely to over-report their weight.29,30 (b) Our design was a cross-sectional study. We had no information about the women's QOL in their premenopausal period which could affect their postmenopausal QOL. Therefore, more evidence based on large prospective cohort studies is required for a more precise investigation of effective factors on postmenopausal women's QOL.
Conclusion
Menopause causes a decrease in QOL, which is dependent to age, work, BMI, financial status and number of children variables. Therefore, it is necessary to develop effective intervention programs to improve QOL in postmenopausal women.
Acknowledgement
We would like to thank the University's vice-chancellor of education and vice-chancellor of research and technology for their financial support to carry out the study.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported. This article is part of a PhD thesis supported by Hamadan University of Medical Sciences.
References
- 1.Izetbegovic S, Stojkanovic G, Ribic N, Mehmedbasic E. Features of postmenopausal uterine haemorrhage. Med Arch. 2013;67:431–434. doi: 10.5455/medarh.2013.67.431-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Souza Santos CA, Dantas EE, Moreira MH. Correlation of physical aptitude; functional capacity, corporal balance and quality of life (QoL) among elderly women submitted to a post-menopausal physical activities program. Arch Gerontol Geriatr. 2011;53:344–349. doi: 10.1016/j.archger.2010.12.019. [DOI] [PubMed] [Google Scholar]
- 3.Park S, Yang MJ, Ha SN, Lee JS. Effective anti-aging strategies in an era of super-aging. J Menopausal Med. 2014;20:85–89. doi: 10.6118/jmm.2014.20.3.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Silva Filho CR, Baracat EC, Conterno Lde O, Haidar MA, Ferraz MB. Climacteric symptoms and quality of life: validity of women's health questionnaire. Rev Saude Publica. 2005;39:333–339. doi: 10.1590/s0034-89102005000300002. [DOI] [PubMed] [Google Scholar]
- 5.Roush K. What nurses know... Menopause: the answers you need from the people you trust. New York, NY: Demos Health; 2011. [Google Scholar]
- 6.Nelson HD. Menopause. Lancet. 2008;371:760–770. doi: 10.1016/S0140-6736(08)60346-3. [DOI] [PubMed] [Google Scholar]
- 7.Kwak EK, Park HS, Kang NM. Menopause knowledge, attitude, symptom and management among midlife employed women. J Menopausal Med. 2014;20:118–125. doi: 10.6118/jmm.2014.20.3.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim HK, Kang SY, Chung YJ, Kim JH, Kim MR. The recent review of the genitourinary syndrome of menopause. J Menopausal Med. 2015;21:65–71. doi: 10.6118/jmm.2015.21.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Orley J, Kuyken W, editors. Quality of life assessment: international perspectives. Berlin, DE: Springer Berlin Heidelberg; 1994. [Google Scholar]
- 10.Mousavi SA, Masoumi SZ, Keramat A, Pooralajal J, Shobeiri F. Assessment of questionnaires measuring quality of life in infertile couples: a systematic review. J Reprod Infertil. 2013;14:110–119. [PMC free article] [PubMed] [Google Scholar]
- 11.Jenabi E, Shobeiri F, Hazavehei SM, Roshanaei G. Assessment of questionnaire measuring quality of life in menopausal women: a systematic review. Oman Med J. 2015;30:151–156. doi: 10.5001/omj.2015.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jafari F, Hadizadeh MH, Zabihi R, Ganji K. Comparison of depression, anxiety, quality of life, vitality and mental health between premenopausal and postmenopausal women. Climacteric. 2014;17:660–665. doi: 10.3109/13697137.2014.905528. [DOI] [PubMed] [Google Scholar]
- 13.Mohammad-Alizadeh-Charandabi S, Rezaei N, Hakimi S, Montazeri A. Predictors of health-related quality of life in postmenopausal women: a population-based study. J Caring Sci. 2012;1:201–208. doi: 10.5681/jcs.2012.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Makvandi S, Bastami A, Shoushtari SZ, Yazdizadeh H, Etemadpour Y, Taghavifar SA. Quality of life and its related factors in postmenopausal women referred to Ahvaz East Health Center, Iran, 2012. Iran J Obstet Gynecol Infertil. 2013;16:6–13. [Google Scholar]
- 15.Lewis JE, Hilditch JR, Wong CJ. Further psychometric property development of the menopause-specific quality of life questionnaire and development of a modified version, MENQOL-intervention questionnaire. Maturitas. 2005;50:209–221. doi: 10.1016/j.maturitas.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 16.Fallahzadeh H. Quality of life after the menopause in Iran: a population study. Qual Life Res. 2010;19:813–819. doi: 10.1007/s11136-010-9644-2. [DOI] [PubMed] [Google Scholar]
- 17.Avraham Y, Nachum S. Management of obesity in menopause: lifestyle modification, medication, bariatric surgery and personalized treatment. In: Dvornyk V, editor. Current topics in menopause. Oak Park, IL: Bentham Science Publishers; 2013. pp. 143–162. [Google Scholar]
- 18.Blumel JE, Castelo-Branco C, Binfa L, Gramegna G, Tacla X, Aracena B, et al. Quality of life after the menopause: a population study. Maturitas. 2000;34:17–23. doi: 10.1016/s0378-5122(99)00081-x. [DOI] [PubMed] [Google Scholar]
- 19.Aghamolaei T, Tavafian SS, Zare S. Health related quality of life in elderly people living in Bandar Abbas, Iran: a population-based study. Acta Med Iran. 2010;48:185–191. [PubMed] [Google Scholar]
- 20.Shobeiri F, Nazari M. Age at menopause and its main predictors among Iranian women. Int J Fertil Steril. 2014;8:267–272. [PMC free article] [PubMed] [Google Scholar]
- 21.Ceylan B, Özerdoğan N. Menopausal symptoms and quality of life in Turkish women in the climacteric period. Climacteric. 2014;17:705–712. doi: 10.3109/13697137.2014.929108. [DOI] [PubMed] [Google Scholar]
- 22.Ghazanfarpour M, Abdolahian S, Zare M, Shahsavari S. Association between anthropometric indices and quality of life in menopausal women. Gynecol Endocrinol. 2013;29:917–920. doi: 10.3109/09513590.2013.819078. [DOI] [PubMed] [Google Scholar]
- 23.Yanikkerem E, Koltan SO, Tamay AG, Dikayak S. Relationship between women's attitude towards menopause and quality of life. Climacteric. 2012;15:552–562. doi: 10.3109/13697137.2011.637651. [DOI] [PubMed] [Google Scholar]
- 24.Guallar-Castillón P, Sendino AR, Banegas JR, López-García E, Rodríguez-Artalejo F. Differences in quality of life between women and men in the older population of Spain. Soc Sci Med. 2005;60:1229–1240. doi: 10.1016/j.socscimed.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 25.Daley A, Macarthur C, Stokes-Lampard H, McManus R, Wilson S, Mutrie N. Exercise participation, body mass index, and health-related quality of life in women of menopausal age. Br J Gen Pract. 2007;57:130–135. [PMC free article] [PubMed] [Google Scholar]
- 26.Jones GL, Sutton A. Quality of life in obese postmenopausal women. Menopause Int. 2008;14:26–32. doi: 10.1258/mi.2007.007034. [DOI] [PubMed] [Google Scholar]
- 27.Caylan A, Aydemir I, Dagdeviren N, Akturk Z, Set T, Oztora S, et al. Evaluation of health related quality of life among perimenopausal Turkish women. Health Med. 2011;5:741–752. [Google Scholar]
- 28.Cheng MH, Wang SJ, Wang PH, Fuh JL. Attitudes toward menopause among middle-aged women: a community survey in an island of Taiwan. Maturitas. 2005;52:348–355. doi: 10.1016/j.maturitas.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 29.Lawlor DA, Bedford C, Taylor M, Ebrahim S. Agreement between measured and self-reported weight in older women. Results from the British Women's Heart and Health Study. Age Ageing. 2002;31:169–174. doi: 10.1093/ageing/31.3.169. [DOI] [PubMed] [Google Scholar]
- 30.Taylor AW, Dal Grande E, Gill TK, Chittleborough CR, Wilson DH, Adams RJ, et al. How valid are self-reported height and weight? A comparison between CATI self-report and clinic measurements using a large cohort study. Aust N Z J Public Health. 2006;30:238–246. doi: 10.1111/j.1467-842x.2006.tb00864.x. [DOI] [PubMed] [Google Scholar]