Abstract
Objectives:
This study aimed to evaluate the effect of different ceramic surface treatments after machining grinding on the biaxial flexural strength (BFS) of machinable dental ceramics with different crystalline phases.
Materials and Methods:
Disk-shape specimens (10mm in diameter and 1.3mm in thickness) of machinable ceramic cores (two silica-based and one zirconia-based ceramics) were prepared. Each type of the ceramic surfaces was then randomly treated (n=15) with different treatments as follows: 1) machined finish as control, 2) machined finish and sandblasting with alumina, and 3) machined finish and hydrofluoric acid etching for the leucite and lithium disilicate-based ceramics, and for the zirconia; 1) machined finish and post-sintered as control, 2) machined finish, post-sintered, and sandblasting, and 3) machined finish, post-sintered, and Nd;YAG laser irradiation. The BFS were measured in a universal testing machine. Data based were analyzed by ANOVA and Tukey’s multiple comparisons post-hoc test (α=0.05).
Results:
The mean BFS of machined finish only surfaces for leucite ceramic was significantly higher than that of sandblasted (P=0.001) and acid etched surfaces (P=0.005). A significantly lower BFS was found after sandblasting for lithium disilicate compared with that of other groups (P<0.05). Sandblasting significantly increased the BFS for the zirconia (P<0.05), but the BFS was significantly decreased after laser irradiation (P<0.05).
Conclusions:
The BFS of the machinable ceramics was affected by the type of ceramic material and surface treatment method. Sandblasting with alumina was detrimental to the strength of only silica-based ceramics. Nd:YAG laser irradiation may lead to substantial strength degradation of zirconia.
Keywords: Strength, Zirconia, Lasers, Ceramics, CAD-CAM
INTRODUCTION
The increasing demand for precise and well-looking dental restorations has led to development and employment of new materials and techniques for tooth restoration or replacement. High-strength ceramic materials for core construction necessitate the use of grinding mechanisms to fabricate desired structures. Today, the application of computer-aided design/computer-aided manufacturing (CAD/CAM) technology in dentistry significantly affected the laboratory and clinical procedures. The advantages of CAD/CAM technology for dental applications are the possibility of applying new materials for fabrication of restorations, reduced labor, cost effectiveness and quality control [1].
The ability to use new materials made it feasible to fabricate all-ceramic restorations with superior esthetics [2]. Different types of ceramic materials are now available as CAD-CAM blocks for chair-side and laboratory applications. Feldspathic-based ceramics are composed of fine-grained powders that produce a relatively high strength and nearly pore-free structure with fine crystals [3]. The strength of these ceramics has been approximated to be about 160MPa [3] and provides esthetics in combination with the ability of acid-etching and bonding to resin [4].
IPS e.max CAD is a lithium disilicate glass-ceramic with the strength of about 320 MPa which is partially crystallized to facilitate machining. After milling, the restoration is fired at 850°C for 30 minutes to complete the crystallization. The final microstructure is composed of a glass matrix, containing a fine-grained size of approximately 1.5μm.
Zirconia-based ceramics are widely used for dental prosthetic restorations because of good physical, chemical and mechanical properties. As a polymorphic material, zirconia has three allotropes: monoclinic, tetragonal, and cubic. At room temperature, pure zirconia is monoclinic, which transforms to tetragonal at high temperature. The tetragonal zirconia can be retained at room temperature if stabilized with yttria, which is called yttria tetragonal stabilized zirconia polycrystalline (Y-TZP) and it is the proposed mechanism for high fracture toughness for this type of ceramic materials [5]. However, grinding procedure during machining the ceramic blocks may cause inevitable damage accumulation that occurs at the surface of restoration and within the machined material [6]. Although the ceramic restorations that are produced by machining ceramic blocks may optimize and improve the structural reliability, but the effect of the machining process on the long-term stability of the restorations must be taken under consideration [7,8].
According to the grinding mechanism of ceramic materials, analysis of the chipped fragments and cutting forces showed that ceramic material removal is dominantly a brittle fracture mechanism [9]. On the other hand, before cementation of ceramic restorations, different surface treatments methods such as airborne particle abrasion (sand-blasting) with aluminum oxide, hydrofluoric (HF) acid etching, or laser irradiation are employed to improve the resin-ceramic bond strength.
It has been shown that these surface treatments which increase the irregularities on the ceramic surface [10] might be the source of future failure and adversely affect the fracture resistance of the ceramic restorations [11].
The aim of this study was to evaluate the effect of different ceramic surface treatments after machining grinding on the biaxial flexural strength (BFS) of CAD/CAM machinable dental ceramics with different crystalline phases.
MATERIALS AND METHODS
Three different commercial CAD/CAM machinable ceramic core materials (two silica-based and one zirconia-based ceramics) were employed in this study; lithium disilicate-based glass ceramic (IPS e.max CAD, Ivoclar Vivadent, Schaan, Liechtenstein), leuicte-based feldspathic ceramic (VITABLOCS Mark II, VITA, Bad Säckingen, Germany), and zirconia-based ceramic (Cercon, DeguDent GmbH, Hanau, Germany) blocks. The materials information are provided in Table 1. The as-received ceramic blocks were worked on a diamond wheel point using a micromotor handpiece to make 10mm-diameter cylindrical rods. For the zirconia-based ceramic (Cercon), a cylindrical acrylic resin pattern was used for the milling of the pre-sintered zirconia blocks by an authorized dental laboratory. The cylinders were cut oversized considering an approximate of 24% shrinkage during post-sintering of zirconia-based ceramics according to the manufacturer’s instructions.
Table 1.
Description of ceramic materials used
| Ceramic Core Material | Description | Manufacturer |
|---|---|---|
| Vitablocks® Mark II | Leucite-based feldspathic ceramic | Vita Zahnfabrik,Bad Säckingen, Germany |
| IPS e.max CAD | Lithium disilicate glass-ceramic | Ivoclar Vivadent, Schaan, Liechtenstein |
| Cercon | Yttrium tetragonal zirconia polycrystals | Degussa Dental, Hanau, Germany |
The cylindrical ceramic rods were then cut into 1.3-mm thick disk-like specimens using a water-cooled low speed diamond saw (Isomet, Buehler, Lake Bluff, IL, USA). For the Cercon ceramic, 1.6 mm thick specimens were cut to compensate the 24% shrinkage during the sintering procedure. The Cercon and IPS e.max CAD ceramic specimens were then sintered to complete the crystallization according to the manufacturer’s instructions.
One side of each disk was polished slightly using 800 to 1200 grit wet silicon carbide papers and cleaned ultrasonically in distilled water for 10 minutes. The other side of each type of the ceramic specimen was then randomly treated with different surface treatment methods as follows (15 specimens in each subgroup):
Vitablocks Mark II and IPS e.max CAD ceramic specimens:
Machined finish as control using a 60 μm diamond bur (D&Z, DIAMANT GmbH, Lemgo, Germany) at high–speed hand piece (NSK Dental, Kanuma, Japan) with water spray coolant. After 2 preparations, the bur was replaced with a new one. This surface finish was used to simulate the machining process of the CAD/CAM technology [12]. (VM-1 and e.CAD-1)
Machined finish and sandblasting with 50 μm aluminum oxide particles (Bego, Easy Blast, Bremen, Germany) at a pressure of 2.8 bar, distance of 10 mm, and perpendicular to the ceramic surface for 20 s. (VM-2 and e.CAD-2)
Machined finish and acid etching with HF acid (Ultradent Porcelain Etch 9.5% Buffered, Ultradent Products, South Jordan, UT, USA) for 20 s and one minute for IPS e.max CAD and Vitablocks Mark II ceramics, respectively as recommended by the manufacturer. Then the specimens were rinsed and air dried for one minute. (VM-3 and e.CAD-3)
Cercon ceramic specimens:
Machined finish as control using a 60 μm diamond bur and then post-sintered according to the manufacturer’s instructions. (Cer-1)
Machined finish, post-sintered, and sandblasted with 50 μm aluminum oxide particles at a pressure of 2.8 bar, distance of 10 mm, and perpendicular to the ceramic surface for 20 s. (Cer-2).
Machined finish, post-sintered, and Nd;YAG laser (Fotona, M001-10F, Ljubljana, Slovenia) irradiation (Cer-3). The laser optical fiber (320 μm in diameter) was kept one mm from the surface and the entire ceramic area was manually scanned perpendicularly for two minutes. The parameters of the applied laser are listed in Table 2.
Table 2.
The parameters of the applied Nd:YAG laser
| Output power | 2 w |
| Frequency | 20 Hz |
| Exposure time | 2 minutes |
| Pulse duration | 100 μsec |
| Pulse energy | 100 mj/pulse |
| Energy density | 124.40 j/cm2 |
| Optical fiber diameter | 320 μm |
| Angle of exposure | Perpendicular |
| Distance from surface | 1 mm |
After surface treatment, the specimens were cleansed in distilled water in an ultrasonic device for 15 minutes. The piston-on-three-ball test (ASTM Standard F394-78) [13] was used to determine the BFS of 15 disk specimens per test group. We selected a specimen with a smaller diameter in order to promote a more realistic sample fabrication and to simulate dental restoration dimensions more closely. The thickness of the specimen center was measured with a digital micrometer before testing. Three steel spheres (3.18 mm in diameter) placed on a circle (10 mm in diameter) arranged 120° apart were used to center and support the disk specimens.
The load was applied to the specimen center by a right circular cylinder of hardened steel having a diameter of 1.58 mm with the flat end perpendicular to the axis. In order to achieve a uniform load distribution, we placed a thin plastic sheet between the flat-ended loading cylinder and specimen surface. The specimens were loaded in a universal testing machine (Zwick, Z100, Ulm, Germany) at a crosshead speed of 0.5 mm/min until fracture. Testing was performed at room conditions. The maximum tensile stress (MPa), which corresponded to the biaxial flexure strength, was calculated according to the equation suggested by the test standard (ASTM F394-78) [13] as follows:
S = −0.2387P(X − Y)/d2 where S is the maximum tensile stress (MPa), P is the load at fracture (N), and d is the specimen thickness (mm) at fracture origin. X and Y were determined as follows:
where ν is the Poisson’s ratio, A is the radius of the support circle (mm), B is the radius of the tip of the piston (mm), and C is the radius of the specimen (mm).
The value for Poisson’s ratio was assumed as 0.25 (if the value for the ceramic concerned is not known, Poisson’s ratio of 0.25 is used [14]). Data were analyzed by Analysis of Variance and Tukey’s multiple comparisons post hoc test at a significance level of p<0.05, using the Statistical Package for Social Sciences (SPSS for Windows 11.5, SPSS, Inc., Chicago, IL).
The microstructure of each ceramic material after different surface treatment methods was evaluated using a field emission scanning electron microscope (SEM) (Hitachi SEM S-4160, Tokyo, Japan).
RESULTS
The mean BFS values (BFS) for different ceramic surface treatments in each group are reported in Table 3. For each ceramic type, Kolmogorov-Smirnov analysis showed normal distribution of data. One-way analysis of variance for each ceramic type showed that different surface treatments significantly affected the mean BFS values in each group.
Table 3.
Mean biaxial flexural strength data (MPa) for different ceramic surface treatments
| 1 | 2 | 3 | ||||
|---|---|---|---|---|---|---|
| Mean | SD* | Mean | SD* | Mean | SD* | |
| Vitablocks Mark II | 68.52 | 11.36 | 54.76 | 3.76 | 57.20 | 4.54 |
| IPS e.max CAD | 89.56 | 12.77 | 63.01 | 7.12 | 84.39 | 19.74 |
| Cercon | 336.50 | 54.68 | 443.20 | 114.03 | 211.42 | 41.54 |
Machined finish: Groups VM-1 (Vitablock Mark II) and e.CAD-1 (IPS e.max CAD), and machined finish & post-sintered: group Cer-1 (Cercon).
Machined finish & sandblasted: Groups VM-2 (Vitablock Mark II) and e.CAD-2 (IPS e.max CAD), and machined finish & post-sintered & sandblasted: group Cer-2 (Cercon).
Machined finish & acid etched: Groups VM-3 (Vitablock Mark II) and e.CAD-3 (IPS e.max CAD), and machined finish & post-sintered & laser irradiated: group Cer-3 (Cercon).
Standard Deviation
Tukey’s multiple comparisons for the Vitablocks Mark II ceramic revealed that VM-1 specimens (machined finish) had significantly higher mean BFS value than that of VM-2 (machined finish and sandblasted, P=0.001) and VM-3 (machined finish and acid etched, P=0.005) groups.
No significant difference in the mean BFS values was observed between VM-2 and VM-3 specimens (P=0.742). For the IPS e.max CAD ceramic, a significantly lower mean BFS value for the e.CAD-2 specimens (machined finish and sandblasted) than that of e.CAD-1 (machined finish, P=0.001) and e.CAD-3 (machined finish and acid etched, P=0.009) was found. No significant difference in the mean BFS values was observed between e.CAD-1 and e.CAD-3 groups (P=0.70). For the Cercon ceramic, Cer-2 specimens (machined finish, post-sintered, and sandblasted) showed a significantly higher mean value than that of Cer-1 (machined finish and post-sintered, P=0.02) and Cer-3 (machined finish, post-sintered, and Nd;YAG laser irradiation, P<0.001) specimens. The lowest mean BFS value was found for Cer-3 specimens which was significantly different from those of Cer-1 (P=0.007) and Cer-2 (P<0.001) specimens.
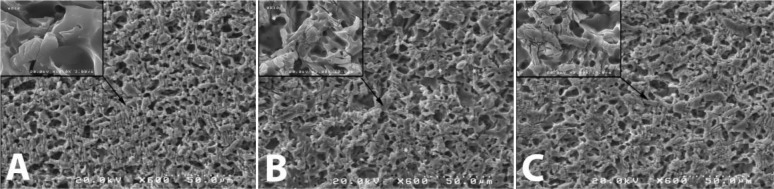
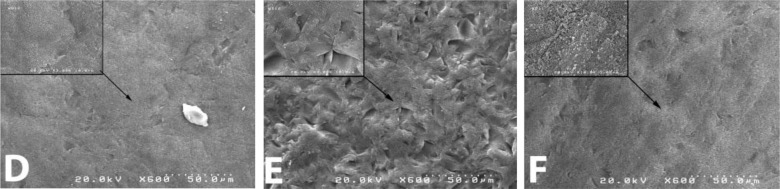
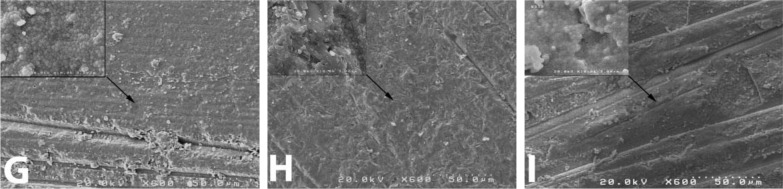
In Vitablocks Mark II ceramic specimens, scanning electron micrographs showed clearly that all the surface treatment methods altered the ceramic surfaces. As shown in Figs 1.A, B and C, crack formation took place. Surface treatment in the VM-2 specimens led to more surface porosity in combination with more crack formation (Fig. 1.B). Scanning electron micrographs in Figs 2.D, E and F showed that for the e.max CAD ceramic, machined finish surfaces in combination with sandblasting with 50 μm aluminum oxide particles (e.CAD-2) altered the ceramic surfaces followed by e.CAD-3 specimens receiving machined finishing and etching with HF acid. With regard to the Cercon ceramic specimens, SEM analysis revealed an alteration in the grain structure of zirconia as shown in Figs 3.G, H, and I. Sandblasting with alumina (Cer-2) did not alter the grain structure as shown in Fig. 3.H, in comparison with the specimens which had only machined finish and post-sintered surfaces (Cer-1, Fig. 3.G). Crack formation was also detected in micrographs (Fig. 3.I) after Nd:YAG laser irradiation (Cer-3).
Fig. 1.
Scanning electron micrographs of Vitablocks Mark II ceramic specimens after surface treatment; A: Machined finish; B: Machined finish and sandblasted; C: Machined finish and HF acid etched (×600).
Fig. 2.
Scanning electron micrographs of IPS e.max CAD ceramic specimens after surface treatment; D: Machined finish, E: Machined finish and sandblasted, F: Machined finish and HF acid etched (×600).
Fig. 3.
Scanning electron micrographs of Cercon ceramic specimens after surface treatment; G: Machined finish and post-sintered, H: Machined finish, post-sintered, and sandblasted, I: Machined finish, post-sintered, and Nd;YAG laser irradiated (×600).
DISCUSSION
New CAD/CAM ceramic materials have been developed to satisfy the outspreading demand for strong as well as esthetic dental restorations [1,15].
The optimum strength of ceramic materials is dependent on the fabrication procedures and content of flaws.
Furthermore, several factors may influence the definitive strength of ceramics, including dimension of specimens, test environment, rate of stressing area of specimen subjected to the stresses, and testing methods [16]. The BFS test was used in this study since the measurement of the strength of brittle materials under biaxial flexure conditions rather than uniaxial flexure (3 or 4-point flexural tests) is often considered more reliable. This is because specimen fracture is not influenced by edge failures and maximum tensile stresses occurring within central loading [17]. However, in biaxial flexural testing, the small loading piston induces concentrated stress at the opposite surface of a disk-like specimen. The experiment setup is so that this test is quite sensitive to surface condition [18].
In the present study, the machined surface treatment using a 60 μm diamond bur represents the ceramic surface finishing that is created by the CAD/CAM milling process with no other surface treatment [12]. The results showed that for the Vitablocks Mark II with leucite crystalline phase content, sandblasting or HF acid etching significantly decreased the BFS of the material compared with machined finish only surfaces.
SEM analysis also demonstrated the appearance of surface cracks and destruction after sandblasting or acid etching of leucite-based ceramic surfaces (Figs 1.B and C). It is proved that surface roughness negatively affects the mechanical properties in dental ceramics, since a decrease in surface roughness generally improves the mechanical properties of this ceramic [19]. In addition, our results showed that the BFS for Vitablocks Mark II was similarly decreased by either sandblasting or HF acid etching surface treatment. This is in agreement with another study by Chen et al. who reported that similar periods of HF acid etching or sandblasting may lead to similar pattern of surface damage in machinable leucite-based feldspathic ceramics [20].
Surface damage and weakening effect of acid etching or sandblasting on the strength of leucite-based ceramics could be due to the modification of the resident surface flaw population.
For the IPS e.max CAD ceramic with lithium disilicate crystalline phase, a significantly decreased in the BFS was found by sandblasting compared with acid etched or machined finish only ceramic surfaces. This may be due to excessive destruction of crystals and glass of machinable lithium disilicate ceramic by sandblasting which was observed on scanning electron micrographs (Fig. 2.E) and revealed more surface damage after sandblasting compared to HF acid etching. Our study showed that after machine grinding of the e.max CAD ceramic surfaces, the BFS was not significantly decreased by HF acid etching for 20 s. SEM analysis also showed slight changes in the surface topography of the acid etched e.max CAD ceramic surfaces (Fig. 2.F). This finding was in consistent with another study by Pollington et al. [12] who reported that the mean surface roughness (Ra) of both fluorocanasite and lithium disilicate glass-ceramics after HF acid etching was lower in comparison to the sandblasted surfaces. On the other hand, our previous study showed that surface HF acid etching for 2 minutes could have a weakening effect on the BFS of two hot-pressed leucite or lithium disilicate-based glass ceramic systems [21]. This observation might be due to the selected longer etching time compared with that of used in this study. As it has been also shown, HF acid etching for 60 s decreased the flexural strength of e.max CAD ceramic in a time-dependent manner in comparison with untreated ceramic surfaces [22]. HF acid dissolves the glassy or crystalline phases of the ceramic and thus changes the microstructure of ceramic surface. This creates microporosity on the ceramic surface, increases the surface area and allows the formation of micro-mechanical retention with resin composites [23].
The results obtained from the present study showed that the machinable leucite-based ceramic surfaces were more susceptible to acid attack than the lithium disilicate ceramic. This might be due to the change in the microstructure of the leucite-based ceramic surface, resulting in the surface being considerably weakened by the HF acid etching. Sandblasting was destructive on both machinable silica-based ceramic surfaces with leucite and lithium disilicate crystalline phases. For the Cercon ceramics with zirconia crystalline phase, a significantly increased (32%) in the BFS was found by sandblasting compared with laser-irradiated or machined finish only surfaces. Our finding is consistent with other studies that reported sandblasting increased the strength of dental Y-TZP ceramics [24–26]. The explanation for this finding might be that air abrasion of zirconia by alumina particles can introduce residual surface compressive stresses because of surface phase transformation from the metastable tetragonal phase (t) to the more stable monoclinic (m) phase [24]. With 50-μm alumina air abrasion, the compressive fields created by this transformation could increase the strength of the zirconia ceramic [27]. Sandblasting may cause surface flaws; however, it appears that these flaws have surpassed the compressive surface layer thickness since material strength increased instead of showing reduction [24].
In addition, weakly attached surface grains could be removed and other imperfections concentrating stresses that could act as crack initiation sites might be eliminated. On the other hand, the mean BFS was significantly dropped by 34% of that of the machined finish surfaces after Nd:YAG laser irradiation. SEM micrographs also showed that laser beam may melt the zircnoia ceramic surfaces (Fig. 3.I). This observation was similar to that of another investigation [28] in which many cracks appeared at the subsurface layer of Cercon ceramic after Nd:YAG laser irradiation. They also mentioned that the crack formation happens during cooling process. It might be due to the volume change during the solidification of melted ceramic as well as phase transformation from cubic to tetragonal. These changes may adversely affect the mechanical properties of zirconia [28]. In addition, Akyil et al. have reported that Nd:YAG laser induces thermal degradation of superficial layer of zirconia ceramic [29].
Finally, it should be noted that the BFSs reported in this in vitro study will not reflect the actual fracture strengths in the clinical situation because of different environmental and loading conditions. Some limitations of the present study are defect driven failure and limitations in producing a precise stress-free cutting in the specimens. Further in vitro and in vivo studies evaluating the effect of other variables on the mechanical strength of machinable dental ceramic systems are needed.
CONCLUSIONS
Within the limitations of this study, it can be concluded that the BFS of the machinable ceramics evaluated in the present study was affected by the type of ceramic material and surface treatment method. HF acid etching considerably decreased the strength of machined leucite-based ceramic system.
Sandblasting with alumina was detrimental to the strength of both machinable silica-based ceramics systems. In contrast, alumina sand-blasting considerably increased the strength of Y-TZP-based ceramic after machining. Nd:YAG laser irradiation of machined Y-TZP ceramic surfaces may lead to substantial strength degradation and cannot be recommended as a reliable surface treatment method. Finally, careful selection of the surface treatment method for resin bonding which does not induce further surface damage, is a prerequisite for the success of machinable ceramics restorations.
ACKNOWLEDGEMENT
This study was supported by Research Center for Science and Technology in Medicine (Tehran University of Medical Sciences).
REFERENCES
- 1-. Miyazaki T, Hotta Y, Kunii J, Kuriyama S, Tamaki Y. A review of dental CAD/CAM: current status and future perspectives from 20 years of experience. Dent Mater J. 2009. January; 28( 1): 44– 56. [DOI] [PubMed] [Google Scholar]
- 2-. Mormann WH. The evolution of the CEREC system. J Am Dent Assoc. 2006. September; 137 Suppl: 7S– 13S. [DOI] [PubMed] [Google Scholar]
- 3-. Seghi RR, Sorensen JA. Relative flexural strength of six new ceramic materials. Int J Prosthodont. 1995. May-Jun; 8( 3): 239– 46. [PubMed] [Google Scholar]
- 4-. Giordano R. Materials for chairside CAD/CAM-produced restorations. J Am Dent Assoc. 2006. September; 137 Suppl: 14S– 21S. [DOI] [PubMed] [Google Scholar]
- 5-. Kelly JR, Denry I. Stabilized zirconia as a structural ceramic: an overview. Dent Mater. 2008. March; 24( 3): 289– 98. [DOI] [PubMed] [Google Scholar]
- 6-. Sreejith PS, Ngoi BK. Material removal mechanisms in precision machining of new materials. Int J Mach Tool Manufact. 2001. September 30; 41( 12): 1831– 43. [Google Scholar]
- 7-. Tinschert J, Zwez D, Marx R, Anusavice KJ. Structural reliability of alumina-, feldspar-, leucite-, mica- and zirconia-based ceramics. J Dent. 2000. September; 28( 7): 529– 35. [DOI] [PubMed] [Google Scholar]
- 8-. Işeri U, Ozkurt Z, Yalnız A, Kazazoğlu E. Comparison of different grinding procedures on the flexural strength of zirconia. J Prosthet Dent. 2012. May; 107( 5): 309– 15. [DOI] [PubMed] [Google Scholar]
- 9-. Malkin S, Hwang TW. Grinding mechanisms for ceramics. CIRP Annals-Manufact Technol. 1996. December 31; 45( 2): 569– 80. [Google Scholar]
- 10-. Borges GA1, Sophr AM, de Goes MF, Sobrinho LC, Chan DC. Effect of etching and airborne particle abrasion on the microstructure of different dental ceramics. J Prosthet Dent. 2003. May; 89( 5): 479– 88. [DOI] [PubMed] [Google Scholar]
- 11-. Zhang Y1, Lawn BR, Rekow ED, Thompson VP. Effect of sandblasting on the long-term performance of dental ceramics. J Biomed Mater Res B Appl Biomater. 2004. November 15; 71( 2): 381– 6. [DOI] [PubMed] [Google Scholar]
- 12-. Pollington S, Fabianelli A, van Noort R. Microtensile bond strength of a resin cement to a novel fluorcanasite glass-ceramic following different surface treatments. Dent Mater 2010. September 30; 26( 9): 864– 72. [DOI] [PubMed] [Google Scholar]
- 13-. ASTM F394-78: Standard test method for biaxial flexural strength (modulus of rupture) of ceramic substrates. 1996: 1– 5. [Google Scholar]
- 14-. Yilmaz H, Aydin C, Gul BE. Flexural strength and fracture toughness of dental core ceramics. J Prosthet Dent. 2007. August; 98( 2): 120– 8. [DOI] [PubMed] [Google Scholar]
- 15-. Rekow ED. A review of the developments in dental CAD/CAM systems. Curr Opin Dent. 1992. June; 2: 25– 33. [PubMed] [Google Scholar]
- 16-. Ban S, Anusavice KJ. Influence of test method on failure stress of brittle materials. J Dent Res. 1990. December; 69( 12): 1791– 9. [DOI] [PubMed] [Google Scholar]
- 17. Albakry M, Guazzato M, Swain MV. Biaxial flexural strength, elastic moduli and X-ray diffraction characterization of three pressable all-ceramic materials. J Prosthet Dent. 2003. April; 89( 4): 374– 80. [DOI] [PubMed] [Google Scholar]
- 18-. Yi YJ, Kelly JR. Failure responses of a dental porcelain having three surface treatments under three stressing conditions. Dent Mater 2011. December 31; 27( 12): 1252– 8. [DOI] [PubMed] [Google Scholar]
- 19-. Flury S, Peutzfeldt A, Lussi A. Influence of Surface Roughness on Mechanical Properties of Two Computer-aided Design/Computer-aided Manufacturing (CAD/CAM) Ceramic Materials. Oper Dent. 2012. Nov-Dec; 37( 6): 617– 24. [DOI] [PubMed] [Google Scholar]
- 20-. Chen JH, Matsumura H, Atsuta M. Effect of different etching periods on the bond strength of a composite resin to a machinable porcelain. J Dent. 1998. January; 26( 1): 53– 8. [DOI] [PubMed] [Google Scholar]
- 21-. Hooshmand T, Parvizi S, Keshvad A. Effect of surface acid etching on the biaxial flexural strength of two hot-pressed glass ceramics. J Prosthodont. 2008. July; 17( 5): 415– 9. [DOI] [PubMed] [Google Scholar]
- 22-. Zogheib LV, Bona AD, Kimpara ET, McCabe JF. Effect of hydrofluoric acid etching duration on the roughness and flexural strength of a lithium disilicate-based glass ceramic. Braz Dent J. 2011; 22( 1): 45– 50. [DOI] [PubMed] [Google Scholar]
- 23-. Peumans M, Van Meerbeek B, Yoshida Y, Lambrechts P, Vanherle G. Porcelain veneers bonded to tooth structure: an ultra-morphological FE-SEM examination of the adhesive interface. Dent Mater. 1999. March; 15( 2): 105– 19. [DOI] [PubMed] [Google Scholar]
- 24-. Kosmac T, Oblak C, Jevnikar P, Funduk N, Marion L. The effect of surface grinding and sandblasting on flexural strength and reliability of Y-TZP zirconia ceramic. Dent Mater. 1999. November; 15( 6): 426– 33. [DOI] [PubMed] [Google Scholar]
- 25-. Guazzato M, Quach L, Albakry M, Swain MV. Influence of surface and heat treatments on the flexural strength of Y-TZP dental ceramic. J Dent. 2005. January; 33( 1): 9– 18. [DOI] [PubMed] [Google Scholar]
- 26-. Souza RO, Valandro LF, Melo RM, Machado JP, Bottino MA, Oezcan M. Air– particle abrasion on zirconia ceramic using different protocols: Effects on biaxial flexural strength after cyclic loading, phase transformation and surface topography. J Mech Behav Biomed Mater 2013. October 31; 26: 155– 63. [DOI] [PubMed] [Google Scholar]
- 27-. Wang H, Aboushelib MN, Feilzer AJ. Strength influencing variables on CAD/CAM zirconia frameworks. Dent Mater. 2008. May; 24( 5): 633– 8. [DOI] [PubMed] [Google Scholar]
- 28-. Noda M, Okuda Y, Tsuruki J, Minesaki Y, Takenouchi Y, Ban S. Surface damages of zirconia by Nd:YAG dental laser irradiation. Dent Mater J. 2010. October; 29( 5): 536– 41. [DOI] [PubMed] [Google Scholar]
- 29-. Akyıl MŞ, Uzun İH, Bayındır F. Bond strength of resin cement to yttrium-stabilized tetragonal zirconia ceramic treated with air abrasion, silica coating, and laser irradiation. Photomed Laser Surg 2010. December 1; 28( 6): 801– 8. [DOI] [PubMed] [Google Scholar]