Abstract
It is not known whether individuals successful at long term weight loss maintenance differ in chronotype (i.e., being a “morning” or “evening” person) or sleep habits compared to those who are overweight and obese. We compared Morningness-Eveningness Questionnaire (MEQ) and Pittsburgh Sleep Quality Index (PSQI) scores of 690 National Weight Control Registry (NWCR) members (73%female, 93%white, age=51.7±12.5, BMI=26.4±5.1) to 75 enrollees in two behavioral weight loss interventions (INT; 77%female, 88%white, age=55.7±10.4, BMI=36.2±4.7). Controlling for age, MEQ scores were higher in NWCR than INT, p=.004, such that more NWCR than INT were morning-types and fewer were evening types, p=.014. Further, NWCR participants reported better sleep quality, longer sleep duration, and shorter latency to sleep onset compared to INT, ps<.05, and fewer NWCR participants reported <6 or <7 hours of sleep, ps<.01. Future studies should examine if these factors change as a result of weight loss or are predictors of weight outcome.
Keywords: Obesity, Weight Loss Maintenance, Sleep, Chronotype, Morningness/Eveningness
Introduction
The difficulty experienced by many individuals in maintaining weight loss long-term (Jeffery et al., 2000; Kraschnewski et al., 2010) suggests the need for increased research on the factors associated with successful maintenance. Although prior studies have focused on the eating and physical activity patterns of successful weight loss maintainers, there has been no research to date on the chronotype or sleep habits of these individuals. This is surprising given the increasing emphasis on the impact of both chronotype (i.e., whether someone is a “morning” or an “evening” person) and sleep habits (e.g., sleep duration and quality) on health behaviors and health risks, including obesity.
Obesity has been associated with both shorter sleep duration (Cappuccio et al., 2008; Gangwisch et al., 2005) and poor sleep quality (Quick et al., 2013; Taheri et al., 2004; Tworoger et al., 2005). While the direction of this association remains unclear, some evidence suggests that there may be a reciprocal influence between sleep and obesity. Shorter sleep duration has been shown to lead to decreased levels of leptin (a protein hormone that signals satiety) and increased levels of ghrelin (a gut peptide associated with the sensation of hunger; Copinschi et al., 2014; Spiegel et al., 2004; Taheri et al., 2004), increased appetite for high-calorie, high-carbohydrate food (Spiegel et al., 2004), stimulation of brain regions sensitive to food stimuli (Copinschi et al., 2014), and insulin resistance (Broussard et al., 2012). Conversely, obesity has been associated with higher prevalence of sleep related problems, such as obstructive sleep apnea (Vgontzas et al., 1994), and weight loss in obese individuals has been shown to lead to clinically-relevant improvements in both sleep apnea (Foster et al, 2009) and overall sleep quality (Toor et al., 2012). It remains unknown whether sleep quality and duration differ between successful weight loss maintainers and overweight/obese individuals.
Compared to the research on sleep and obesity, relatively little research has investigated the association between chronotype and obesity. While a direct link between chronotype and weight status has yet to be demonstrated, evening-type chronotype has been associated with a wide variety of negative health outcomes, from behavioral dysregulation (Caci et al., 2004; Tonetti et al., 2010) to drug addiction (Adan, 1994), depression (Levandovski et al., 2011), and eating disorders (Natale et al., 2008) and evening-type individuals have been shown to be more likely to engage in eating behaviors that may negatively impact weight, such as increased fast food and soda consumption (Fleig & Randler, 2009). Similarly, morning-type individuals report higher dietary restraint and lower dietary disinhibition (Schubert & Randler, 2008), factors which have been demonstrated to differentiate obese and overweight individuals from normal weight individuals (Lindroos et al., 1997).
Despite increased research on long-term maintenance of weight loss, successful maintenance remains a challenge for many individuals (Kraschnewski et al., 2010); investigating the behaviors that differ between those who are successful at weight loss and maintenance and those who are overweight and obese may provide clues to understanding this challenge. Findings from the National Weight Control Registry (NWCR), a registry of individuals who have lost at least 13.6 kg and have maintained this weight loss for at least 1 year, have provided insight into the characteristics and behaviors of highly successful weight loss maintainers (Klem et al., 1997). For example, studies from the NWCR have demonstrated that individuals successful at weight loss maintenance report continued consumption of a reduced calorie, low fat diet, regular engagement in high levels of physical activity, and frequent self-weighing (Klem et al., 1997; McGuire et al., 1999). The current study focused on identifying chronotype and characterizing sleep habits in a group of successful weight loss maintainers (NWCR), and compared them to overweight and obese individuals enrolling in two behavioral weight loss interventions (INT). Compared to INT participants, we hypothesized that more NWCR would be categorized as morning-type chronotype. Further, we hypothesized that NWCR participants would have better sleep quality and longer sleep duration compared to INT participants.
Methods and Procedures
Participants
Participants were recruited for the NWCR through national and local television, radio, magazine, and newspaper advertisements. Eligibility requirements for participation in the NWCR included weight loss of ≥ 13.6 kg and duration of weight loss maintenance ≥ 1 year. Those interested in joining the NWCR were mailed a consent form and questionnaire packet and asked to report their maximum weight, current weight, and weight loss and to provide verification of their weight loss by photographs, physician report, or collateral testimony. There was no compensation for participation in the registry. For the present study, 1,000 NWCR participants who had consented to complete on-line questionnaires and had completed their most recent year’s follow-up questions were emailed a link to use for this study.
INT participants were recruited from two behavioral weight management programs at the Weight Control and Diabetes Research Center in Providence, RI. For each study, participants responded to newspaper or Internet advertisements and were screened by phone for basic eligibility criteria (BMIs > 25 kg/m2, no current medical conditions affecting safety of the program, not using any medications that affect weight, and not currently enrolled in another weight management program). Participants who met basic eligibility criteria were invited to attend an in-person orientation visit, where they completed informed consent and baseline study measures. Participants were not compensated for completion of this assessment.
Measures
Demographics
Age, gender, race/ethnicity, marital status, and educational attainment were assessed via self-report questionnaire.
Height and weight
Height and weight were collected from NWCR participants using a self-report questionnaire; previous studies have demonstrated good accuracy of the self-report weight data in the NWCR.(McGuire et al., 1999) Height and weight were measured for INT participants at an in-person assessment. Height was measured using a wall-mounted stadiometer, without shoes, to the nearest .1 cm. Weight was measured in one layer of light indoor clothing, without shoes, to the nearest .1 kg using a calibrated digital scale. Height and weight for each participant were used to calculate body mass index (BMI).
Morningness/Eveningness
Chronotype was assessed using the Morningness-Eveningness Questionnaire (MEQ), a 19-item questionnaire developed by Horne and Ostberg (1975) to assess chronotype via self-reported habitual bed and wake times, alertness at waking and bedtimes, and preferred times of physical and mental performance. The MEQ has acceptable internal reliability (Smith et al., 1989), and chronotype categorization from the MEQ has been validated by objectively measured sleep/wake times in adults (Carrier et al., 1997), physiological indicators such as body temperature (Kerkhof et al., 1980; Kerkhof & Van Dongen, 1996) and electrocortical activity (Ishihara et al., 1987; Kerkhof et al., 1980), and cognitive measure such as alertness (Natale & Cicogna, 2002) and performance tasks (Horne et al., 1980; Kerkhof et al., 1980).
Sleep Quality
Sleep quality and duration were measured using the Pittsburgh Sleep Quality Index (PSQI; Buysse et al., 1989). This measure has been demonstrated to have high reliability and good validity for assessing impaired sleep (Backhaus et al., 2002). Both the PSQI total score and subscale scores were used, including the subscales assessing duration of sleep, sleep disturbance, sleep latency, day dysfunction due to sleepiness, sleep efficiency, and need for sleep medications.
Statistical Analyses
All analyses were conducted using SAS v9.3 for Windows (SAS Institute Inc., 2011). Of the 797 NWCR participants who completed the online questionnaire, 67 were excluded from analyses for no longer meeting registry entry requirements (no longer maintaining a weight loss ≥ 13.6 kg), and 40 were excluded due to missing items on the chronotype and sleep measures that prevented calculation of scale and total summary scores, leaving a total sample of 690. Data from four INT participants were excluded due to missing items on the sleep measures, leaving a total sample of 75. Participants in both INT studies were asked to complete the PSQI at their first study assessment, but only those in the second study (N=52) were asked to complete the MEQ.
Demographic differences between the NWCR and INT samples were assessed using independent samples t-tests and chi-square analyses. As morningness/eveningness scores have been shown to increase with age (Carrier et al., 1997; Monk & Kupfer, 2007), age was controlled as a covariate in the primary analyses for morningness/eveningness and sleep.
Morningness/Eveningness
An ANCOVA using SAS proc GLM was used to investigate differences in total MEQ scores by group (NWCR vs. INT) after controlling for participant age. The original cut-offs recommended by Horne & Ostberg (1975) were developed using data from college students and have been criticized for misclassifying chronotype in middle-aged adults; thus, in our analyses we used cut-offs for morningness/eveningness that were developed specifically for use with middle-aged adults (Taillard et al., 2004), participants who scored above 69 on the MEQ were categorized as ‘definitely morning type,’ those who scored 65–69 as ‘moderately morning type,’ those who scored 53–64 as ‘neither type,’ those who scored 52–47 as ‘moderately evening type,’ and those who scored less than 47 as ‘definitely evening type.’ A chi-square analysis was used to investigate differences in MEQ categorization between the NWCR and INT groups. To investigate significant differences following this analysis, ‘definitely morning type’ and ‘moderately morning type’ were collapsed into a general ‘morning type’ category, and ‘definitely evening type’ and ‘moderately evening type’ were collapsed into ‘evening type’(Horne et al., 1980; Horne & Ostberg, 1975). We further replicated this analysis using the cut-offs originally developed by Horne and Ostberg (1975).
Sleep Quality
Analyses of covariance (ANCOVAs; using SAS proc GLM) were used to investigate differences in PSQI total score and subscale scores between NWCR and INT, after adjusting for age. Two chi-square analyses were used to assess differences between NWCR and INT in proportion of participants reporting less than six hours and less than seven hours of sleep each night. Finally, participants were categorized using established cut-offs for “good sleep quality” (total PSQI score ≤ 5) and “poor sleep quality” (total PSQI score > 5; Buysse et al., 1989) and differences in categorization were assessed using a chi-square analysis.
Results
The NWCR participants reported an average weight loss of −33.91 ± 17.21 kg at the time the questionnaire was administered (representing a −29.93 ± 9.63% reduction from maximum lifetime weight), and reported maintaining this loss for an average of 7.26 ± 6.05 years. Demographic data, by study, are presented in Table 1. There were no significant differences between the NWCR and INT samples in terms of gender or marital status, all ps > .05. As anticipated, the NWCR participants had lower BMIs compared to INT participants, t(763) = 15.94, p < .0001. NWCR participants were significantly younger than INT participants, t(763) = 2.63, p = .009, and there was a significant difference between samples in terms of race/ethnicity, Fisher’s exact p = .04, and education, χ2(4) = 42.16, p < .001, such that the NWCR participants were more likely identify as non-Hispanic Caucasian and to report a college or graduate/professional degree compared to INT participants.
Table 1.
Baseline demographic characteristics of NWCR and INT participants.
| NWCR
|
INT
|
|
|---|---|---|
| n = 690 | n = 75 | |
| Age (SD), years | 51.72 (12.54) | 55.67 (10.43)a |
| BMI (SD), kg/m2 | 26.37 (5.07) | 36.19 (4.66)a |
| Gender (%) | ||
| Female | 72.61 | 77.33 |
| Male | 27.39 | 22.67 |
| Ethnicity (%) | ||
| African American | 2.0% | 4.0%b |
| Asian | 1.5% | 0.0% |
| Caucasian | 92.7% | 88.0% |
| Hispanic | 2.8% | 1.3% |
| Other/Multiple | 1.6% | 6.7% |
| Marital Status (%) | ||
| Single | 14.8% | 17.3% |
| Married or living with a partner | 72.3% | 62.7% |
| Separated/Divorced | 13.0% | 20.0% |
| Education (%) | ||
| High school or less | 2.6% | 10.7%a |
| Vocational Training | 1.9% | 5.3% |
| Some college | 11.2% | 29.3% |
| College or university degree | 35.1% | 26.7% |
| Graduate degree | 49.1% | 28.0% |
p < .01
p< .05
Morningness/Eveningness
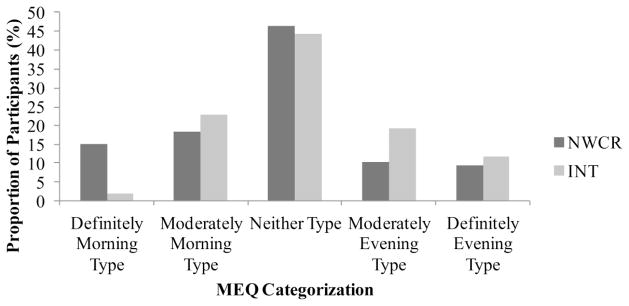
After controlling for age, NWCR participants had significantly higher MEQ scores than INT participants (see Table 2), suggesting that NWCR participants were more likely to be “morning type” compared to INT, Cohen’s d = .38. Adjusting for education did not affect the results. Using the “morning-type” and “evening-type” categorizations developed for middle aged adults (Taillard et al., 2004), there was a significant difference between NWCR and INT, Fisher’s exact p = .014 (see Figure 1), such that more NWCR participants were categorized as morning type (definitely or moderately) compared to INT (33.8% compared to 25.0%) and less as evening types (19.7% vs. 30.8%). Analyses completed using the original cut-offs developed by Horne and Ostberg (1975) demonstrated the same pattern of results.
Table 2.
PSQI total and subscale scores and MEQ total scores, by group.
| NWCR
|
INT
|
p | |||
|---|---|---|---|---|---|
| M | SE | M | SE | ||
| PSQI Total1 | 5.02 | 0.11 | 6.05 | 0.34 | .005 |
| PSQI Subscales | |||||
| Duration | 0.37 | 0.03 | 0.67 | 0.08 | < .001 |
| Sleep Disturbance | 1.21 | 0.02 | 1.31 | 0.06 | .073 |
| Sleep Latency | 0.80 | 0.03 | 1.19 | 0.10 | < .001 |
| Day Dysfunction | 0.75 | 0.03 | 0.81 | 0.08 | .503 |
| Sleep Efficiency | 0.33 | 0.03 | 0.48 | 0.08 | .069 |
| Sleep Quality | 0.93 | 0.03 | 1.13 | 0.08 | .015 |
| Need Meds to Sleep | 0.63 | 0.04 | 0.47 | 0.13 | .232 |
| MEQ Total2 | 59.82 | 0.35 | 56.00 | 1.27 | .004 |
Lower scores = Better sleep.
Higher scores = Higher morningness tendencies
Figure 1.
Morningness/Eveningness categorization by group, using cut-offs developed for middle-aged adults.
Sleep Quality and Duration
PSQI total scores and subscale scores are presented by group in Table 2. After adjusting for age, the NWCR participants had significantly lower total PSQI scores compared to INT participants, indicating that they reported better overall sleep quality than INT participants, Cohen’s d = .35. Further, on the PSQI subscales, NWCR participants reported significantly better duration of sleep, less sleep latency (time to fall asleep), and better self-reported sleep quality. There were no differences between the NWCR and INT groups in terms of sleep disturbance, day dysfunction due to sleepiness, sleep efficiency, or needing medications to sleep.
On average, NWCR participants reported taking approximately (mean ± SE) 17.4 ± 0.7 minutes to fall asleep, compared to 23.6 ± 2.0 minutes reported by INT participants, F(1,763) = 8.80, p = .003, ȵ2partial = .011. Significantly fewer participants in the NWCR group reported <6 hours (7.0% for NWCR compared to 18.7% of INT χ2(1) = 12.46, p < .001) or <7 hours of sleep each night (29.6% for NWCR compared to 45.3% INT, χ2(1) = 7.85, p = .005). Using established cut-offs for assessing “good sleep quality” compared to “poor sleep quality,” NWCR participants were significantly more likely to report “good sleep quality,” (66.4% NWCR compared to 52.0% INT), χ2(1) = 6.14, p = .013.
Discussion
Results from the current study demonstrated that individuals who have been highly successful at both weight loss and long-term maintenance were more likely to be categorized as a “morning type” chronotype and reported longer sleep duration and better sleep quality compared to treatment-seeking overweight and obese participants. Further, these NWCR participants were more likely to report shorter sleep latency (time required to fall asleep) and were less likely to report short sleep, defined as either <6 or <7 hours of sleep per night, than INT participants. Effect sizes for differences between total MEQ and PSQI scores indicate small to moderate effect of group on chronotype and sleep quality.
A previous population study of morningness/eveningness found that approximately 24.7% of middle-aged adults were categorized as morning-type (Taillard et al., 2004); Categorization of MEQ scores in the INT participants closely mirrored these population estimates, at 25.0%, whereas 33.8% of the NWCR sample were categorized as morning type. These results suggest that individuals who are successful at long-term weight maintenance may be especially likely to morning-type chronotype. In addition, NWCR members were far less likely to be short sleepers, with only 7% reporting sleep duration of <6 hours compared to 19% of INT. What remains unknown is the direction of these associations. Does morning chronotype or better sleep predict success at long-term maintenance, or does success at weight loss maintenance alter chronotype and sleep? Previous studies with NWCR participants suggest several health behaviors that could feasibly impact both chronotype and sleep, such as high levels of physical activity (Klem et al., 1997) and regular breakfast consumption (Wyatt et al., 2002), and weight loss has been shown to lead to improvements in both sleep apnea (Foster et al., 2009) and sleep quality and duration (Toor et al., 2012). Conversely, both genetic markers for evening-type chronotype (Garaulet et al., 2012) and short sleep duration/poor sleep quality (Thomson et al., 2012) have been shown to predict smaller weight losses following intervention. Indeed, although the correlational nature of the current study precludes causal inferences, they are interesting in relation to results by Thomson and colleagues (2012), who demonstrated that better sleep quality increased the likelihood of weight loss success by 33%. A third possibility may be that there is a reciprocal relationship between these factors. While it is unknown whether intervention can affect chronotype, effective interventions for improving sleep quality exist (Edinger et al., 2001; Sivertsen et al., 2006; Vitiello et al., 2009); thus, future research should focus on measuring both chronotype and sleep before, during, and after weight loss to examine the direction of these effects and to examine whether attempts to intervene on these factors may impact success at weight loss and maintenance.
The current study represents the first investigation into the chronotype classification and sleep habits of successful weight loss maintainers. Strengths of the current study included the examination of novel correlates of weight loss maintenance, the collection of data from a large sample of successful weight loss maintainers, and the comparison of these data from successful weight loss maintainers to treatment-seeking obese and overweight individuals at enrollment for a weight management program.
Despite these strengths, the current study had several limitations. First, all sleep data (from both NWCR and INT) were self-reported, which may introduce bias. The methods of data collection utilized were not suited to the use of actigraphy to measure sleep; however, the PSQI has been widely used to assess sleep in both population and intervention studies, and has demonstrated validity for assessing impaired sleep (Backhaus et al., 2002). As discussed previously, the cross-sectional nature of the current data prevents causal interpretation of the results. Further, it is unknown whether individuals without a lifetime history of overweight/obesity differ in chronotype or sleep from individuals successful at long-term weight loss maintenance. Future studies should compare successful weight loss maintainers to normal weight individuals to assess whether these differences may be associated with current weight status rather than history of weight loss/maintenance. Finally, the current study did not assess nor adjust for sleep apnea. As prevalence of sleep apnea is associated with obesity (Vgontzas et al., 1994), future research should investigate symptoms of sleep apnea when investigating sleep quality and duration.
Conclusion
In summary, the current results establish an association between successful weight loss maintenance and morning-type chronotype. Further, we demonstrated that successful weight loss maintainers were more likely to report longer sleep duration and improved sleep quality compared to treatment-seeking overweight and obese adults. Future research should investigate whether chronotype categorization and sleep quality change as a result of weight loss, or if morning-type chronotype and better sleep quality predict later success at weight loss and long-term maintenance.
Acknowledgments
Funding: This study was funded by the National Cancer Institute (National Institutes of Health) under award number 5U01CA150387 awarded to RRW, and by the National Institute of Diabetes Digestive and Kidney Diseases (National Institutes of Health) under award number F32DK100069 awarded to KMR. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
References
- Adan A. Chronotype and personality factors in the daily consumption of alcohol and psychostimulants. Addiction. 1994;89(4):455–462. doi: 10.1111/j.1360-0443.1994.tb00926.x. http://doi.org/10.1111/j.1360-0443.1994.tb00926.x. [DOI] [PubMed] [Google Scholar]
- Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test–retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. Journal of Psychosomatic Research. 2002;53(3):737–740. doi: 10.1016/s0022-3999(02)00330-6. http://doi.org/10.1016/S0022-3999(02)00330-6. [DOI] [PubMed] [Google Scholar]
- Broussard JL, Ehrmann DA, Van Cauter E, Tasali E, Brady MJ. Impaired insulin signaling in human adipocytes after experimental sleep restriction: A randomized, crossover study. Annals of Internal Medicine. 2012;157(8):549–557. doi: 10.7326/0003-4819-157-8-201210160-00005. http://doi.org/10.7326/0003-4819-157-8-201210160-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. http://doi.org/10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Caci H, Robert P, Boyer P. Novelty seekers and impulsive subjects are low in morningness. European Psychiatry. 2004;19(2):79–84. doi: 10.1016/j.eurpsy.2003.09.007. http://doi.org/10.1016/j.eurpsy.2003.09.007. [DOI] [PubMed] [Google Scholar]
- Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, Miller MA. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619–626. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrier J, Monk TH, Buysse DJ, Kupfer DJ. Sleep and morningness-eveningness in the “middle” years of life (20–59y) Journal of Sleep Research. 1997;6(4):230–237. doi: 10.1111/j.1365-2869.1997.00230.x. http://doi.org/10.1111/j.1365-2869.1997.00230.x. [DOI] [PubMed] [Google Scholar]
- Copinschi G, Leproult R, Spiegel K. The important role of sleep in metabolism. Frontiers of Hormone Research. 2014;42:59–72. doi: 10.1159/000358858. http://doi.org/10.1159/000358858. [DOI] [PubMed] [Google Scholar]
- Edinger JD, Wohlgemuth WK, Radtke RA, Marsh GR, Quillian RE. Cognitive behavioral therapy for treatment of chronic primary insomnia: A randomized controlled trial. JAMA. 2001;285(14):1856–1864. doi: 10.1001/jama.285.14.1856. http://doi.org/10.1001/jama.285.14.1856. [DOI] [PubMed] [Google Scholar]
- Fleig D, Randler C. Association between chronotype and diet in adolescents based on food logs. Eating Behaviors. 2009;10(2):115–118. doi: 10.1016/j.eatbeh.2009.03.002. http://doi.org/10.1016/j.eatbeh.2009.03.002. [DOI] [PubMed] [Google Scholar]
- Foster GD, Borradaile KE, Sanders MH, Millman R, Zammit G, Newman AB Sleep AHEAD Research Group of Look AHEAD Research Group. A randomized study on the effect of weight loss on obstructive sleep apnea among obese patients with type 2 diabetes: The Sleep AHEAD study. Archives of Internal Medicine. 2009;169(17):1619–1626. doi: 10.1001/archinternmed.2009.266. http://doi.org/10.1001/archinternmed.2009.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005;28(10):1289–1296. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- Garaulet M, Esteban Tardido A, Lee YC, Smith CE, Parnell LD, Ordovás JM. SIRT1 and CLOCK 3111T>C combined genotype is associated with evening preference and weight loss resistance in a behavioral therapy treatment for obesity. International Journal of Obesity. 2012;36(11):1436–1441. doi: 10.1038/ijo.2011.270. http://doi.org/10.1038/ijo.2011.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne J, Brass CG, Petitt AN. Circadian performance differences between morning and evening “types. Ergonomics. 1980;23(1):29–36. doi: 10.1080/00140138008924715. http://doi.org/10.1080/00140138008924715. [DOI] [PubMed] [Google Scholar]
- Horne J, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. International Journal of Chronobiology. 1975;4(2):97–110. [PubMed] [Google Scholar]
- Ishihara K, Miyasita A, Inugami M, Fukuda K, Miyata Y. Differences in sleep-wake habits and EEG sleep variables between active morning and evening subjects. Sleep: Journal of Sleep Research & Sleep Medicine. 1987;10(4):330–342. doi: 10.1093/sleep/10.4.330. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, Epstein LH, Wilson GT, Drewnowski A, Stunkard AJ, Wing RR. Long-term maintenance of weight loss: Current status. Health Psychology. 2000;19(1, Suppl):5–16. doi: 10.1037/0278-6133.19.suppl1.5. http://doi.org/10.1037/0278-6133.19.Suppl1.5. [DOI] [PubMed] [Google Scholar]
- Kerkhof GA, Korving HJ, Geest HMMWd, Rietveld WJ. Diurnal differences between morning-type and evening-type subjects in self-rated alertness, body temperature and the visual and auditory evoked potential. Neuroscience Letters. 1980;16(1):11–15. doi: 10.1016/0304-3940(80)90093-2. http://doi.org/10.1016/0304-3940(80)90093-2. [DOI] [PubMed] [Google Scholar]
- Kerkhof GA, Van Dongen HPA. Morning-type and evening-type individuals differ in the phase position of their endogenous circadian oscillator. Neuroscience Letters. 1996;218(3):153–156. doi: 10.1016/s0304-3940(96)13140-2. http://doi.org/10.1016/S0304-3940(96)13140-2. [DOI] [PubMed] [Google Scholar]
- Klem ML, Wing RR, McGuire MT, Seagle H, Hill JO. A descriptive study of individuals successful at long-term maintenance of substantial weight loss. American Journal of Clinical Nutrition. 1997;66:239–246. doi: 10.1093/ajcn/66.2.239. [DOI] [PubMed] [Google Scholar]
- Kraschnewski JL, Boan J, Esposito J, Sherwood NE, Lehman EB, Kephart DK, Sciamanna CN. Long-term weight loss maintenance in the United States. International Journal of Obesity. 2010;34(11):1644–1654. doi: 10.1038/ijo.2010.94. http://doi.org/10.1038/ijo.2010.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levandovski R, Dantas G, Fernandes LC, Caumo W, Torres I, Roenneberg T, Allebrandt KV. Depression scores associate with chronotype and social jetlag in a rural population. Chronobiology International. 2011;28(9):771–778. doi: 10.3109/07420528.2011.602445. http://doi.org/10.3109/07420528.2011.602445. [DOI] [PubMed] [Google Scholar]
- Lindroos AK, Lissner L, Mathiassen ME, Karlsson J, Sullivan M, Bengtsson C, Sjöström L. Dietary intake in relation to restrained eating, disinhibition, and hunger in obese and nonobese Swedish women. Obesity Research. 1997;5(3):175–182. doi: 10.1002/j.1550-8528.1997.tb00290.x. http://doi.org/10.1002/j.1550-8528.1997.tb00290.x. [DOI] [PubMed] [Google Scholar]
- McGuire MT, Wing RR, Klem ML, Lang W, Hill JO. What predicts weight regain in a group of successful weight losers? Journal of Consulting and Clinical Psychology. 1999;67(2):177–185. doi: 10.1037//0022-006x.67.2.177. http://doi.org/10.1037/0022-006X.67.2.177. [DOI] [PubMed] [Google Scholar]
- Monk TH, Kupfer DJ. Which aspects of morningness-eveningness change with age? Journal of Biological Rhythms. 2007;22(3):278–280. doi: 10.1177/0748730407301054. http://doi.org/10.1177/0748730407301054. [DOI] [PubMed] [Google Scholar]
- Natale V, Ballardini D, Schumann R, Mencarelli C, Magelli V. Morningness–eveningness preference and eating disorders. Personality and Individual Differences. 2008;45(6):549–553. http://doi.org/10.1016/j.paid.2008.06.014. [Google Scholar]
- Natale V, Cicogna P. Morningness-eveningness dimension: is it really a continuum? Personality and Individual Differences. 2002;32(5):809–816. http://doi.org/10.1016/S0191-8869(01)00085-X. [Google Scholar]
- Quick V, Byrd-Bredbenner C, White AA, Brown O, Colby S, Shoff S, Greene G. Eat, sleep, work, play: Associations of weight status and health-related behaviors among young adult college students. American Journal of Health Promotion. 2013;29:e64–e72. doi: 10.4278/ajhp.130327-QUAN-130. http://doi.org/10.4278/ajhp.130327-QUAN-130. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS Version 9.3. Cary, NC: 2011. [Google Scholar]
- Schubert E, Randler C. Association between chronotype and the constructs of the Three-Factor-Eating-Questionnaire. Appetite. 2008;51(3):501–505. doi: 10.1016/j.appet.2008.03.018. http://doi.org/10.1016/j.appet.2008.03.018. [DOI] [PubMed] [Google Scholar]
- Sivertsen B, Omvik S, Pallesen S, Bjorvatn B, Havik OE, Kvale G, Nordhus IH. Cognitive behavioral therapy vs zopiclone for treatment of chronic primary insomnia in older adults: A randomized controlled trial. JAMA. 2006;295(24):2851–2858. doi: 10.1001/jama.295.24.2851. http://doi.org/10.1001/jama.295.24.2851. [DOI] [PubMed] [Google Scholar]
- Smith CS, Reilly C, Midkiff K. Evaluation of three circadian rhythm questionnaires with suggestions for an improved measure of morningness. Journal of Applied Psychology. 1989;74(5):728–738. doi: 10.1037/0021-9010.74.5.728. http://doi.org/10.1037/0021-9010.74.5.728. [DOI] [PubMed] [Google Scholar]
- Spiegel K, Tasali E, Penev P, Cauter EV. Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Annals of Internal Medicine. 2004;141(11):846–850. doi: 10.7326/0003-4819-141-11-200412070-00008. http://doi.org/10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1(3):e62. doi: 10.1371/journal.pmed.0010062. http://doi.org/10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taillard J, Philip P, Chastang JF, Bioulac B. Validation of Horne and Ostberg Morningness-Eveningness Questionnaire in a middle-aged population of French workers. Journal of Biological Rhythms. 2004;19(1):76–86. doi: 10.1177/0748730403259849. http://doi.org/10.1177/0748730403259849. [DOI] [PubMed] [Google Scholar]
- Thomson CA, Morrow KL, Flatt SW, Wertheim BC, Perfect MM, Ravia JJ, Rock CL. Relationship between sleep quality and quantity and weight loss in women participating in a weight-loss intervention trial. Obesity. 2012;20(7):1419–1425. doi: 10.1038/oby.2012.62. http://doi.org/10.1038/oby.2012.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonetti L, Adan A, Caci H, De Pascalis V, Fabbri M, Natale V. Morningness-eveningness preference and sensation seeking. European Psychiatry. 2010;25(2):111–115. doi: 10.1016/j.eurpsy.2009.09.007. http://doi.org/10.1016/j.eurpsy.2009.09.007. [DOI] [PubMed] [Google Scholar]
- Toor P, Kim K, Buffington CK. Sleep quality and duration before and after bariatric surgery. Obesity Surgery. 2012;22(6):890–895. doi: 10.1007/s11695-011-0541-8. http://doi.org/10.1007/s11695-011-0541-8. [DOI] [PubMed] [Google Scholar]
- Tworoger SS, Davis S, Vitiello MV, Lentz MJ, McTiernan A. Factors associated with objective (actigraphic) and subjective sleep quality in young adult women. Journal of Psychosomatic Research. 2005;59(1):11–19. doi: 10.1016/j.jpsychores.2005.03.008. http://doi.org/10.1016/j.jpsychores.2005.03.008. [DOI] [PubMed] [Google Scholar]
- Vgontzas AN, Tan TL, Bixler EO, Martin LF, Shubert D, Kales A. Sleep apnea and sleep disruption in obese patients. Archives of Internal Medicine. 1994;154(15):1705–1711. http://doi.org/10.1001/archinte.1994.00420150073007. [PubMed] [Google Scholar]
- Vitiello MV, Rybarczyk B, Von Korff M, Stepanski EJ. Cognitive Behavioral Therapy for Insomnia Improves Sleep and Decreases Pain in Older Adults with Co-Morbid Insomnia and Osteoarthritis. Journal of Clinical Sleep Medicine: JCSM: Official Publication of the American Academy of Sleep Medicine. 2009;5(4):355–362. [PMC free article] [PubMed] [Google Scholar]
- Wyatt HR, Grunwald GK, Mosca CL, Klem ML, Wing RR, Hill JO. Long-term weight loss and breakfast in subjects in the National Weight Control Registry. Obesity Research. 2002;10(2):78–82. doi: 10.1038/oby.2002.13. http://doi.org/10.1038/oby.2002.13. [DOI] [PubMed] [Google Scholar]