Abstract
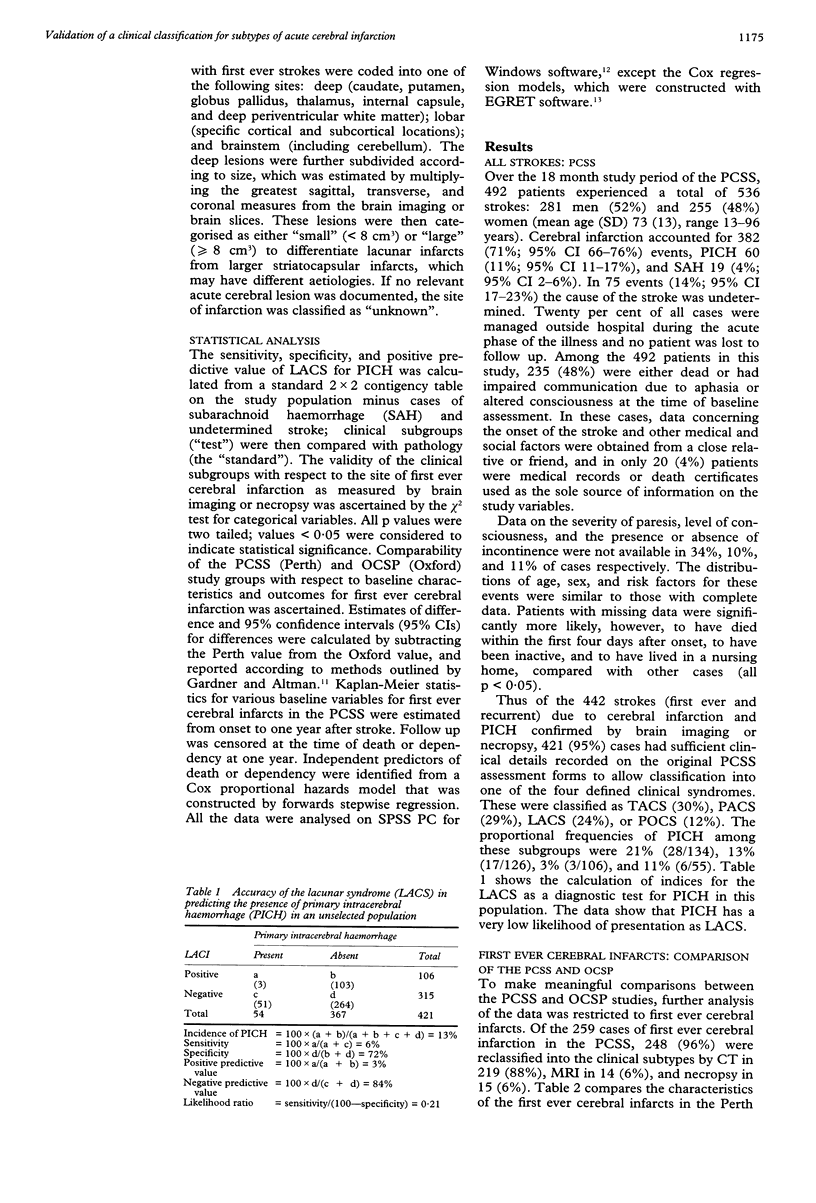
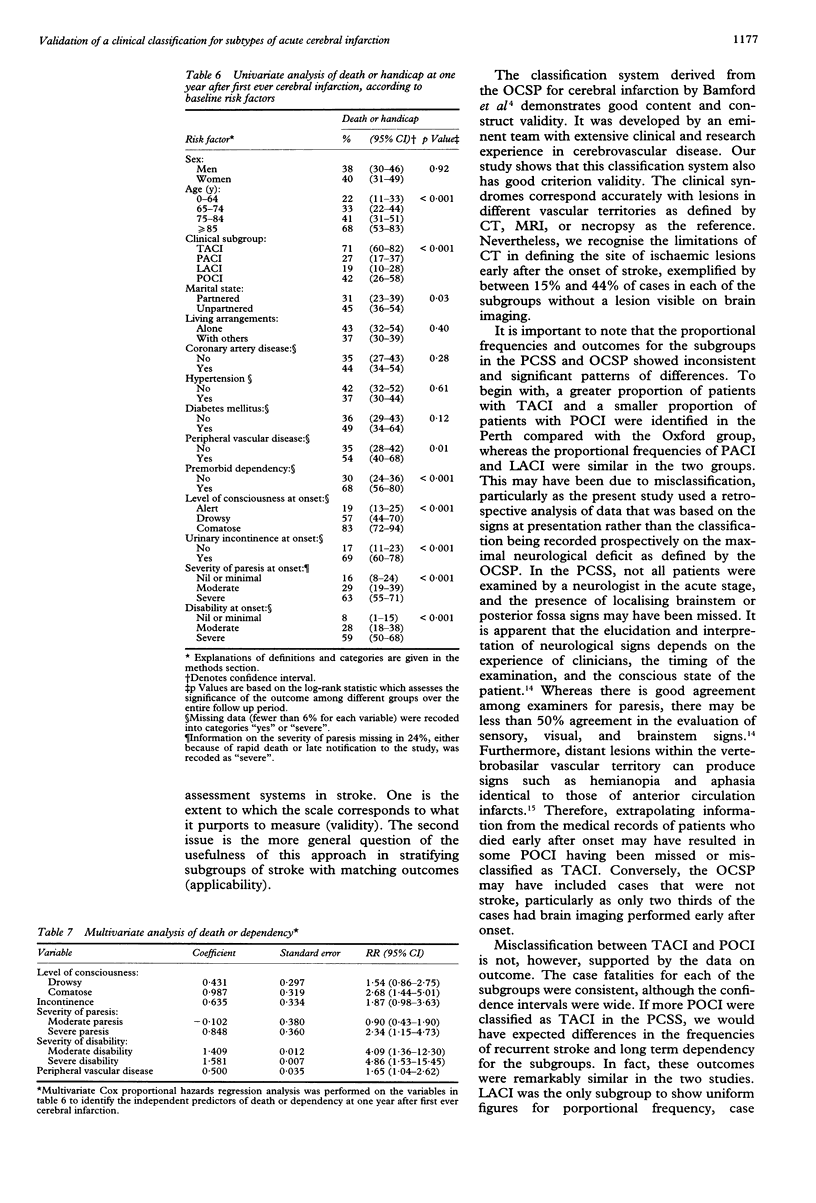
The validity of a clinical classification system was assessed for subtypes of cerebral infarction for use in clinical trials of putative stroke therapies and clinical decision making in a population based stroke register (n = 536) compiled in Perth, Western Australia in 1989-90. The Perth Community Stroke Project (PCSS) used definitions and methodology similar to the Oxfordshire Community Stroke Project (OCSP) where the classification system was developed. In the PCSS, 421 cases of cerebral infarction and primary intracerebral haemorrhage (PICH), confirmed by brain imaging or necropsy, were classified into the subtypes total anterior circulation syndrome (TACS), partial anterior circulation syndrome (PACS), lacunar syndrome (LACS), and posterior circulation syndrome (POCS). In this relatively unselected population, relying exclusively on LACS for a diagnosis of PICH had a very low sensitivity (6%) and positive predictive value (3%). Comparison of the frequencies and outcomes (at one year after the onset of symptoms) for each subgroup of first ever cerebral infarction in the PCSS (n = 248) with the OCSP (n = 543) registers showed uniformity only for LACI. For example, there were 27% of cases of TACI in the PCSS compared with 17% in the OCSP (difference = 10%; 95% confidence interval (95% CI) 4% to 16%) and 15% of cases in the PCSS compared with 24% in the OCSP were POCI (difference = 9%; 95% CI 3% to 15%). Case fatalities and long-term handicap across the subgroups were not significantly different between studies, but the frequencies of recurrent stroke were significantly greater for POCI in the OCSP compared with the PCSS. Although this classification system defines subtypes of stroke with different outcomes, simple clinical measures-level of consciousness, paresis, disability, and incontinence at onset-are more powerful predictors of death or dependency at one year. It is concluded that simple clinical measures that reflect the severity of the neurological deficit should complement this classification system in clinical trials and practice.
Full text
PDF




Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson C. S., Jamrozik K. D., Burvill P. W., Chakera T. M., Johnson G. A., Stewart-Wynne E. G. Ascertaining the true incidence of stroke: experience from the Perth Community Stroke Study, 1989-1990. Med J Aust. 1993 Jan 18;158(2):80–84. doi: 10.5694/j.1326-5377.1993.tb137528.x. [DOI] [PubMed] [Google Scholar]
- Bamford J. M., Sandercock P. A., Warlow C. P., Slattery J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1989 Jun;20(6):828–828. doi: 10.1161/01.str.20.6.828. [DOI] [PubMed] [Google Scholar]
- Bamford J., Sandercock P., Dennis M., Burn J., Warlow C. Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet. 1991 Jun 22;337(8756):1521–1526. doi: 10.1016/0140-6736(91)93206-o. [DOI] [PubMed] [Google Scholar]
- Barer D. H., Mitchell J. R. Predicting the outcome of acute stroke: do multivariate models help? Q J Med. 1989 Jan;70(261):27–39. [PubMed] [Google Scholar]
- Brott T., Adams H. P., Jr, Olinger C. P., Marler J. R., Barsan W. G., Biller J., Spilker J., Holleran R., Eberle R., Hertzberg V. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989 Jul;20(7):864–870. doi: 10.1161/01.str.20.7.864. [DOI] [PubMed] [Google Scholar]
- Côté R., Battista R. N., Wolfson C., Boucher J., Adam J., Hachinski V. The Canadian Neurological Scale: validation and reliability assessment. Neurology. 1989 May;39(5):638–643. doi: 10.1212/wnl.39.5.638. [DOI] [PubMed] [Google Scholar]
- Demeurisse G., Demol O., Robaye E. Motor evaluation in vascular hemiplegia. Eur Neurol. 1980;19(6):382–389. doi: 10.1159/000115178. [DOI] [PubMed] [Google Scholar]
- Gardner M. J., Altman D. G. Confidence intervals rather than P values: estimation rather than hypothesis testing. Br Med J (Clin Res Ed) 1986 Mar 15;292(6522):746–750. doi: 10.1136/bmj.292.6522.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindley R. I., Warlow C. P., Wardlaw J. M., Dennis M. S., Slattery J., Sandercock P. A. Interobserver reliability of a clinical classification of acute cerebral infarction. Stroke. 1993 Dec;24(12):1801–1804. doi: 10.1161/01.str.24.12.1801. [DOI] [PubMed] [Google Scholar]
- Lyden P. D., Lau G. T. A critical appraisal of stroke evaluation and rating scales. Stroke. 1991 Nov;22(11):1345–1352. doi: 10.1161/01.str.22.11.1345. [DOI] [PubMed] [Google Scholar]
- Sandercock P. A., Allen C. M., Corston R. N., Harrison M. J., Warlow C. P. Clinical diagnosis of intracranial haemorrhage using Guy's Hospital score. Br Med J (Clin Res Ed) 1985 Dec 14;291(6510):1675–1677. doi: 10.1136/bmj.291.6510.1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandercock P. A., van den Belt A. G., Lindley R. I., Slattery J. Antithrombotic therapy in acute ischaemic stroke: an overview of the completed randomised trials. J Neurol Neurosurg Psychiatry. 1993 Jan;56(1):17–25. doi: 10.1136/jnnp.56.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandercock P., Molyneux A., Warlow C. Value of computed tomography in patients with stroke: Oxfordshire Community Stroke Project. Br Med J (Clin Res Ed) 1985 Jan 19;290(6463):193–197. doi: 10.1136/bmj.290.6463.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teasdale G., Murray G., Parker L., Jennett B. Adding up the Glasgow Coma Score. Acta Neurochir Suppl (Wien) 1979;28(1):13–16. doi: 10.1007/978-3-7091-4088-8_2. [DOI] [PubMed] [Google Scholar]



