Abstract
Background
Malaria is one of the deadliest mosquito-borne diseases in the world. More than 80% of the total populations are at risk of malaria in the 22 countries in Asia and the Pacific. South Asia alone is home to an estimated 1.4 billion people at risk of contracting malaria. Despite the remarkable progress in reducing the burden of malaria, evidence of the disease based on knowledge of the social and cultural contexts from a South Asian perspective is limited. Our objective was to understand the knowledge, attitudes and beliefs about malaria in South Asian communities.
Methodology
We conducted a systematic literature review, searching six databases, between 1990 and 2015, focusing on knowledge, attitudes and beliefs about malaria in South Asia. Databases were searched using both ‘free terms’ and ‘index terms’ funnelled using Boolean operators and truncations. Inclusion and exclusion criteria were set, and included papers were scrutinised, employing a critical appraisal tool to find the best available evidences to support the study purpose.
Results and discussion
Evidence from 32 articles (26 quantitative, four qualitative and two mixed methods). General knowledge and awareness of the disease, its transmission, and control and preventative measures were generally found to be lacking amongst both the general public and healthcare professionals. In addition, the study shows that poor socio-economic factors – including limited access to services due to poor/limited availability – and issues of affordability are considered as major risk factors.
Conclusion
This review suggests the importance of increasing health awareness, mobilising the local or community healthcare professionals, for prevention as well as early detection and effective treatment of malaria among people who are at risk. Malaria is also a disease associated with poverty and socio-cultural factors; therefore, strong political will, wider partnerships between health and non-health sectors, and strengthening health systems’ technical and managerial capabilities at all level of primary healthcare systems, is inevitable.
Keywords: malaria, South Asia, primary healthcare, eradicating malaria, control and prevention, systematic review
Malaria is a public health problem as it kills more than 600,000 people every year. Over half of the population is known to be at risk of malaria globally, and most of them are children of under-five (1). Malaria is an acute febrile illness caused by the parasites of the genus Plasmodium, of which there are four species (P. vivax, P. ovale, P. malariae and P. falciparum) that infect humans, of which P. falciparum can be fatal if not treated immediately, and mixed species infections are common in endemic areas (2). Recently, Heymann (3) discussed that globally P. vivax and P. falciparum are the most common species, and P. falciparum is considered a serious public health threat because of its severity and often fatal outcome.
Africa accounts for 90% of the mortality burden of malaria, and South East Asia accounts for 10% of the burden (2, 4). World Health Organization (WHO) reports that in the Asia and Pacific region, which covers 22 countries, about 2.1 billion people (80% of the total population) are at risk of getting malaria. In this area, four countries – Afghanistan, Bangladesh, India and Pakistan have 1,000 or more cases per 100,000 population (5). As of writing this article, there was no aggregated data available for the cases of malaria in South Asia. This region covers eight countries India, Pakistan, Bhutan, Bangladesh, Sri Lanka, Nepal, Maldives and Afghanistan – which is also the scope of the article. Based on data extracted from each country from the World Health Report published in 2015 (2), this region alone has a reported point estimate of 19.5 million (19,464,050) malaria cases and 29 thousand (28,830) deaths, with 1.4 billion total population at risk (Table 1). Children below the age of five are most vulnerable, with approximately 86% of deaths from malaria being in this age group (6). Pregnant women were the second most vulnerable group due to anaemia, reduced immunity and increased vulnerability to infection and illness (7). At-risk categories include indigenous people, forest-related workers and settlers, subsistence farmers and migrant labourers working in mines, plantations, road construction, dams and irrigation.
Table 1.
Malaria in South Asia
| Country | Population | Population at risk | Reported cases (positive) | Reported deaths | Estimated cases | Estimated deaths |
|---|---|---|---|---|---|---|
| India | 1,295,300,000 | 1,178,700,000 | 1,102,205 | 561 | 17,000,000 | 26,000 |
| Pakistan | 185,044,286 | 181,918,666 | 275,149 | 56 | 1,500,000 | 1,100 |
| Bangladesh | 159,077,513 | 16,480,430 | 10,216 | 45 | 700,000 | 1,600 |
| Bhutan | 765,008 | 121,441 | 48 | 0 | 50 | – |
| Nepal | 28,174,724 | 13,509,780 | 1,469 | 0 | 14,000 | 10 |
| Sri Lanka | 20,618,991 | N/A | 49 | 0 | – | – |
| Maldives | – | – | 0 | 0 | – | – |
| Afghanistan | 31,627,506 | 23,902,611 | 61,362 | 32 | 250,000 | 120 |
| 1,720,608,028 | 1,414,632,928 | 1,450,498 | 694 | 19,464,050 | 28,830 |
WHO (2).
It is important to highlight Bhutan, a country which is in the elimination phase; the population living in active foci is the population at risk. There were no malaria deaths. Nepal has a current estimated malaria death rate of less than 10. Similarly, Sri Lanka has had no local transmission since October 2012; only cases imported from other countries were detected (2). Thus, there is no population at risk. Even though the number of confirmed malaria cases in the South East Asia region, including those in South Asia (SA), has generally decreased from 2.9 million in 2000 to 2 million in 2012, the disease still remains a significant threat to peoples’ lives and livelihoods (8).
WHO (2) recommends that every suspected case of malaria should receive a diagnostic test (2). There are several tests available (microscopy, serology, polymerase chain reaction (PCR)-based assay and lateral flow immunochromatographic antigen detection assays), with antigen detection assays being commonly known as ‘malaria rapid diagnostic tests’ (RDTs). This test is reliable and is often recommended to detect malaria parasites in the human body if microscopy is not available or not reliable (3).
Evidence suggests that key approaches to preventing malaria include regular use of long-lasting insecticidal nets, indoor spraying of homes with residual insecticides and treatment (2). Chloroquine is one popular drug and is still effective on P. vivax, but P. falciparum is resistant to it in many parts of the world. Artemisinin-based combination therapy (ACT) is considered as highly effective, not only as treatment for uncomplicated P. falciparum malaria, but also to help delay development of resistance (3).
SA had an estimate of reducing malaria cases and deaths by 75% by 2015 (from the year 2000) with a long-term goal of eliminating the disease, but this target is still far from being reached (9). Kumar et al. (10) argue that the ‘global malaria situation is increasingly being challenged owing to lack of credible malaria vaccine and the emergence of drug resistance to most of the available antimalarials’ (p. 2116).
There is a substantial body of literature in existence concerning malaria, but this evidence is often scattered and limited to establishing knowledge about malaria from the perspectives of vectors and environmental, economic, social and health-service features in SA communities (11–14). Similarly, several pieces of evidence suggest there is a gap between knowledge and understanding of the disease and its control and the implementation of that knowledge, largely due to socio-economic factors (the knowledge–implementation gap) (15–17). As Dash et al. (18) reported, people's understanding of malaria, its transmission, treatment and prevention is generally low and the neglect of SA, especially highly populated and malaria-endemic countries like India, would bring substantial challenges to the global reduction of malaria-related mortality and morbidity.
A comprehensive understanding of malaria exposure due to behavioural and social factors and gaps in knowledge would not only contribute to a better understanding of unexpected disease outbreaks and unpredicted disease presentations, but is also essential in developing and reflecting appropriate policies and guidelines into practice in line with malaria control and prevention (11). Therefore, it was justified and timely to conduct a systematic review of knowledge, attitudes and beliefs about malaria to support and inform further development of appropriate prevention and control interventions that may contribute to eradicate malaria transmission in SA.
Methodology
We conducted a systematic review of published literature, focusing on knowledge, attitudes and beliefs about malaria among the population of SA. Boland et al. (19) argue that a systematic review is considered as a gold standard method since it is ‘synthesising the findings of several studies investigating the same questions’ (p. 3) to provide high-quality evidence to inform healthcare policy on decision-making in practice (20, 21). In addition, a systematic review has a propensity to be more transparent when the selection of the studies for review is made carefully (22). Nevertheless, the Institute of Medicine (23) warns that systematic reviews might equally ‘fail to acknowledge or address the risk of reporting biases, neglect to appraise the quality of individual studies included in the review, and (they) are subject to errors during the data extraction and analysis’ (p. 82).
Search strategy
A search strategy was developed by the research team, led by one of the lead authors (KR). Through identifying and examining primary researches in the topic area, six major electronic databases – MEDLINE, Global Health, PsycINFO, CINAHL, EMBASE and AMED – were searched using both ‘free terms’ and ‘index terms’, focusing on the studies related to malaria – knowledge, attitudes and beliefs amongst South Asian communities. Additional grey literatures – OpenGrey, Ethos and British Library Catalogue – were also searched. Following the formulation of research questions, inclusion and exclusion criteria were set. The search strategy to address this question involved searching these electronic databases in four groups (Table 2).
Table 2.
Word groups used to identify relevant articles
| Word group 1 – Population | Word group 2 – Intervention | Word group 3 – Disease or conditions, context or setting | Word group 4 – Outcomes |
|---|---|---|---|
| ‘Male’ OR ‘Female’ OR ‘Adult’ OR ‘Child*’ OR ‘Elderly’ |
‘Insecticide treated bed net’ OR ‘ITNs’ OR ‘LLIN’ OR ‘bed net’ OR ‘Indoor Residual Spray’ OR ‘IRS’ OR ‘Intermittent’ OR ‘Prevent*’ OR ‘Treat*’ OR ‘Artemisinin-based Combination Theory’ OR ‘ACT’ OR ‘community education’ or ‘health promotion’ OR ‘public health’ OR ‘primary care’ OR ‘prevent*’ OR ‘control*’ OR ‘Preventative care’ |
‘Malaria’ OR ‘mosquito’ OR ‘febrile patients’ OR ‘South Asia[*1]’ OR ‘SAARC’ OR ‘Afghanistan’ OR ‘Afghanistan[*1]’ OR ‘Bhutan’ OR ‘Bhutan[*3]’ OR ‘Nepal’ OR ‘Nepal[*3]’ OR ‘India’ OR ‘India[*1]’ OR ‘Pakistan’ OR ‘Pakistan[*1]’ OR ‘Bangladesh’ OR ‘Maldives’ OR ‘Sri Lanka’ OR ‘Sri Lanka[*1]’ | ‘Improv*’ OR ‘improvement’ OR ‘access*’ OR ‘utilization’ OR ‘utilization’ OR ‘utilis*’ OR ‘utilize*’ OR ‘aware’ OR ‘prevent*’ OR ‘control*’ OR ‘mortality and morbidity’ OR ‘quality of life’ ‘Health need’ OR ‘outcome’ OR ‘results’ OR ‘quality’ OR ‘impact’ OR ‘effective’ OR ‘change’ ‘Knowledge’ OR ‘awareness’ OR ‘attitude’ OR ‘beliefs’ OR ‘behavior’ ‘community knowledge’ OR ‘community response’ |
Inclusion criteria (limit):
| |||
All groups are combined using Boolean operators.
Screening strategy
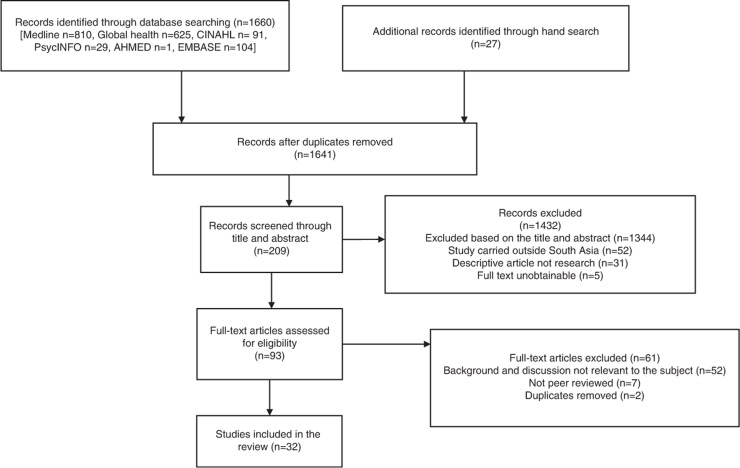
Screening was undertaken in two phases in this review. Firstly, the titles and abstracts of the retrieved literature were reviewed by the two authors in order to identify if the literature met the set inclusion criteria. During this process, some studies were excluded due to the fact that they did not meet the set inclusion criteria. Secondly, the full texts of the selected articles were retrieved, more articles were excluded and the studies that passed the screening criteria were included in the study. Manual screening of the articles was also considered through the references list for further articles relevant to the study. The PRISMA flow diagram was followed in a stepwise process, and the final 33 articles were screened and identified for the review (Fig. 1).
Fig. 1.
PRISMA flow diagram.
Results
In this study, 1,660 studies were identified from the initial search of the chosen six major databases, with an additional 27 studies being identified as relevant to the topic area through hand-searching in other sources, which made a total of 1,687. Articles from both types of searching were screened and 1,641 studies were retrieved after 46 duplicates were removed. Of the 1,641 articles, 1,432 articles were excluded based on title and abstract not being relevant to the research question, the study being carried out outside South Asia and some articles not being in academic journals. Therefore, 209 articles were selected and the full texts of those articles were retrieved. All articles were examined based on set inclusion and exclusion criteria, and finally, 93 articles were found to be eligible. A further 61 articles were excluded since the backgrounds and discussions of some articles were not relevant to the study, some articles were not peer-reviewed, and further duplicates were removed. Overall, 32 publications were included in this study. The primary evidence base is comprised of quantitative (n=26) followed by qualitative (n=4) and mixed methods (n=2). Most of the studies were conducted in India (n=19) followed by Bangladesh (n=4), Sri Lanka (n=3), Pakistan (n=2), Bhutan (n=2), Afghanistan (n=1) and Nepal (n=1). Although all studies were published after 1990, the study periods ranged from 2000 to 2012 with a total sample size of 42,393 (ranging from 73 to 7,117). It is noted that one study did not provide sample size, and two studies did not report study periods (Table 3).
Table 3.
Summary of the articles included
| Quality appraisal [from Smith et al., 2009 (24)] | |||||||
|---|---|---|---|---|---|---|---|
| First author (year) | Title and journal (impact factor) | Country | Study design (study period) | Population group/sample size | Qualitative | Quantitative | Overall quality rating* |
| Ahmed et al. 2009 (25) | Knowledge on the transmission, prevention and treatment of malaria among two endemic populations of Bangladesh and their health- seeking behavior. Malar J [IF: 3.11] | Bangladesh | Survey, semi-structured questionnaire/face-to-face interview (July–November 2007) |
General population (9,750) | NA | 1,2,7,10 | weak |
| Ahmed et al. 2014 (26) | Conventional or interpersonal communication: which works best in disseminating malaria information in an endemic rural Bangladeshi community? PloS One [IF 3.23] | Bangladesh | Cross-sectional survey, pretested, semi-structured questionnaire (July–November 2007 & January–February 2012) |
General population (750 households) | NA | 1,2,4,5,6,7,9,10 | Strong |
| Ahmed et al. 2011 (27) | Free distribution of insecticidal bed nets improves possession and preferential use by households and is equitable: findings from two cross-sectional surveys in 13 malaria endemic districts of Bangladesh. Malar J [IF: 3.11] | Bangladesh | Cross-sectional surveys, structured interviews (2008 and 2011) |
General population (3,760 in 2008 and 7,895 in 2011) | NA | 1,2,3,4,5,6,7,9,10 | Strong |
| Anand et al. 2014 (28) | Knowledge and use of personal protective measures against mosquito borne diseases in a resettlement colony of Delhi. Ann Med Health Sci Res [IF: 0.00] | India | Cross-sectional study, pre-tested, pre-designed, semi-structured questionnaire (June 2011–July 2011) |
General population (100) | NA | 1,2,4,5,7,10 | Moderate |
| Bashar et al. 2012 (29) | Socio-demographic factors influencing knowledge, attitude and practice (KAP) regarding malaria in Bangladesh. BMC Public Health [IF: 2.264] | Bangladesh | Survey, structured questionnaires and the interviews, (July–October 2011) | General population (468) | NA | 1,2,4,7,10 | Weak |
| Chourasia et al. 2014 (30) | Household training vs. mass campaigns: a better method of health communication for preventing malaria. Trop Doct [IF: 0.48) | India | Interviewer-administered structured questionnaire (September–December 2012) | General population (218) | NA | 1,2,4,5,7,10 | Moderate |
| Dambhare et al. 2012 (31) | Knowledge, attitude and practice of malaria transmission and its prevention among the school going adolescents in Wardha District, Central India. Glob J Health Sci [IF: 0.00] | India | Cross sectional study, pre-designed, pre-tested questionnaire (October–December 2010) |
School going adolescents (1,096) | NA | 1,2,4,5,6,7,10 | Moderate |
| Das and Ravindran 2010 (32) | Factors affecting treatment-seeking for febrile illness in a malaria endemic block in Boudh district, Orissa, India: policy implications for malaria control. Malar J [IF: 3.11] | India | Cross-sectional community-based survey, using structured interviews (2006) |
General population (323) [300-service users and 23 – service providers] | 1,2,3,4,5,7,8,9,10 | 1,2,7,8,9,10 | Moderate |
| Das and Ravindran 2011 (33) | Community knowledge on malaria among febrile patients in an endemic district of Orissa, India. J Vector Borne Dis [IF: 0.806] | India | Cross-sectional community-based survey, structured interviews (June–August 2006) |
General population (300) | NA | 1,2,4,5,7,9,10 | Moderate |
| Dhawan et al. 2014 (34) | Malaria-related knowledge and prevention practices in four neighborhoods in and around Mumbai: a cross sectional study. Malar J [IF: 3.11] | India | Quantitative – cross-sectional, structured interviewers-administered questionnaire (December 2010–January 2011) |
General population (119) | NA | 1,4,7,10 | Weak |
| Fernando et al. 2008 (35) | Community factors affecting long-lasting impregnated mosquito net use for malaria control in Sri Lanka. Trans R Soc Trop Med Hyg [IF: 1.931] | Sri Lanka | Community-based cross-sectional survey among (June–July 2007) |
General population (2,467) | NA | 1,2,4,5,7,10 | Moderate |
| Howard et al. 2010 (36) | Malaria control under the Taliban regime: insecticide-treated net purchasing, coverage, and usage among men and women in eastern Afghanistan. Mala J[IF: 3.11] | Afghanistan | Mixed methods – focus group discussions, in-depth and quantitative household survey (February–September 2000) |
General population (566) [Fifteen focus group discussions (82+40) and 30 in-depth interviews, 414 households] | 1,2,3,4,5,6,7,8,9,10 | 1,2,4,5,7,9,10 | Strong |
| Hussain et al. 2013 (37) | Public health system readiness to treat malaria in Odisha State of India. Malar J [IF: 3.11] | India | Cross-sectional study, key informant interviews, semi-structured interviews and health facility assessments (February–July 2012) | Auxiliary nurse midwives and accredited social health activists (455) | NA | 1,2,7,10 | Weak |
| Joshi and Banjara 2008 (38) | Malaria related knowledge, practices and behaviour of people in Nepal. J Vector Borne Dis [IF: 0.806] | Nepal | Cross-sectional study using structured questionnaire and focus group discussions (December 2004–April 2005) | General population (1,330) | NA | 1,2,4,7,10 | Weak |
| Kirkby et al. 2013 (39) | Knowledge, attitudes and practices relevant to malaria elimination amongst resettled populations in a post-conflict district of northern Sri Lanka. Trans R Soc Trop Med Hyg [IF: 1.931] | Sri Lanka | Descriptive cross-sectional, structured questionnaire. Questionnaire (2011) | General population (300) | NA | 1,2,4,5,6,7,10 | Moderate |
| Kumar et al. 2014 (40) | Spatial trend, environmental and socioeconomic factors associated with malaria prevalence in Chennai. Malar J [IF: 3.11] | India | Questionnaire, field survey (2005–2011) | Not provided | NA | 1,2,7,10 | Weak |
| Lwin et al. 2014 (41) | ‘It's effective but should I bother?’ A study of personal protection measures against Malaria in urban India. Public Health [IF: 1.434] | India | Quantitative – survey, interview questionnaire (March–June, 2012) |
General population (1,000) | NA | 1,2,7,10 | Weak |
| Nandwani et al. 2014 (42) | Clinical profile of severe malaria: study from a tertiary care center in north India. J Parasit Dis [IF: 0.00] | India | Retrospective observational study (August 2010 to October 2010) |
Patients (160) | NA | 1,2,7,10 | Weak |
| Pandit et al. 2010 (43) | Awareness and practice about preventive method against mosquito bite in Gujarat. Healthline [IF: 0.00]. | India | Quantitative – cross-sectional, questionnaire (June 2009) | General population (311) | NA | 1,7,10 | weak |
| Qayum et al. 2012 (44) | SPHERE-based assessment of knowledge and preventive measures related to malaria among the displaced population of Jalozai, Pakistan. J Pak Med Assoc [IF 0.414] | Pakistan | Descriptive cross-sectional, structured questionnaire (March–November 2010) |
General population (116) | NA | 1,2,4,5,7,10 | Moderate |
| Sabin et al. 2010 (45) | Attitudes, knowledge, and practices regarding malaria prevention and treatment among pregnant women in Eastern India. Am J Trop Med Hyg [IF: 2.699] | India | Qualitative using in-depth interviews and focus group discussions (April–May 2007) |
Pregnant women (73) [32 in-depth interviews and six focus group discussions] | 1,2,3,4,5,6,7,8,9,10 | NA | Strong |
| Saha et al. 2015 (46) | Establishing communication mechanism for malaria prevention in Baiga tribal villages in Baiga chak area of Dindori district, Madhya Pradesh. Indian J Med Res [IF: 1.4] | India | Quasi experimental design using questions (November 2011–February 2012) |
General population (2,350) | NA | 1,2,3,4,5,6,7,9,10 | Strong |
| Sarkar et al. 2009 (47) | Risk factors for malaria deaths in Jalpaiguri district, West Bengal, India: evidence for further action. Malar J [IF: 3.11] | India | Quantitative – using pre-tested structured questionnaire (2007–2008) | Total population (168) | NA | 1,2,3,4,5,6,7,9,10 | Strong |
| Sharma et al. 2015 (48) | Socio-economic & household risk factors of malaria in tribal areas of Madhya Pradesh, central India. Indian J Med Res [IF: 1.4] | India | Baseline survey using interviews (May 2005–June 2008) | General population (7,117) | NA | 1,2,4,5,6,7,9,10 | Strong |
| Sood et al. 2010 (49) | Community awareness, perceptions, acceptability and preferences for using LLIN against malaria in villages of Uttar Pradesh, India. J Vector Borne Dis [IF: 0.806] | India | Community-based survey, structured questionnaire (April–May 2009) |
General population (596) | NA | 1,2,7,10 | weak |
| Sundararajan et al. 2013 (50) | Barriers to malaria control among marginalized tribal communities: a qualitative study. PloS One [IF: 3.234] | India | Qualitative data using multiple key informants and groups. (July 2012) |
General population (84) [76-focus groups, and 8- individual interviews] | 1,2,3,4,5,6,7,8,9,10 | NA | Strong |
| Tobgay and Lhazeen 2010 (51) | Malaria perceptions and practices in Bhutan. Southeast Asian J Trop Med Public Health. [IF: 0.719]. | Bhutan | Qualitative using focus group discussions and interviews (July–August 2007) |
Eight focus group discussions (n=80) [three with medical profession, three with community members, and two with village health workers] |
1,2,3,4,6,7,8(partly),9,10 | NA | Strong |
| Tobgay et al. 2013 (52) | Community-directed educational intervention for malaria elimination in Bhutan: quasi-experimental study in malaria endemic areas of Sarpang district. Malar J [IF: 3.11] | Bhutan | Quasi-experimental study, both qualitative and quantitative data collection methods (Study period – not provided) | General population (25+560) [13 in-depth interviews and 12 focus group discussions] & 560 households interviewed | NA | 1,2,3,4,5,6,7,9,10 | Strong |
| Vijayakumar et al. 2009 (53) | Knowledge, attitude and practice on malaria: a study in a tribal belt of Orissa state, India with reference to use of long lasting treated mosquito nets. Acta Trop [IF: 2.519] | India | Mixed methods: quantitative (questionnaire) and qualitative (key informant interview and focus group discussions) (2002) | General population (656) | 1,3,7 | 1,2,4,7,10 | Moderate |
| Yadav et al. 2013 (54) | Knowledge, treatment-seeking behaviour and socio-economic impact of malaria in the desert of Rajasthan, India. South African India. South Afr J Epidemiol Infect [IF: 0.00] | India | Quantitative – cross-sectional, community-based study, questionnaire (Study period: not provided) |
General population (540) | NA | 4,7,10 | weak |
| Yasuoka et al. 2006 (55) | Impact of education on knowledge, agricultural practices, and community actions for mosquito control and mosquito-borne disease prevention in rice ecosystems in Sri Lanka. Am J Trop Med Hyg [IF: 2.7] | Sri Lanka | Cross-sectional, – two surveys before and after the intervention (2003) | General population (75 households) | NA | 1,2,4,5,7,8,9,10 | Moderate |
| Zaidi et al. 2015 (56) | The quantitative evidence of malarial transmission and its associates in Bahawalpur, Pakistan. J Ayub Med Coll Abbottabad (IF: 0.00) | Pakistan | Cross-sectional, semi-structured questionnaires (January–June, 2008) | General population (1,623) | NA | 1,2,4,5,7,10 | Moderate |
(i) Some studies did not report sufficient details about the quality, so missing quality appraisal criteria/question(s) mean not particular appraisal question(s) applicable or not reported. (ii) Overall quality rating scale: strong (9–10 criteria/questions of yes); moderate (6–8 criteria/question of yes); weak (1–5 criteria/question of yes).
The research was heterogeneous; therefore, overall synthesis using meta-analysis was inappropriate (57). We, therefore, utilised a thematic analysis as a framework for analysis. Thematic analysis involves ‘discovering, interpreting and reporting patterns and clusters of meaning within the data’ (58, p. 27). As Joff (59) described, following reading and re-reading of the included articles, we identified themes, and these themes were further examined for their similarities, differences and contradictions. From the review, six major themes emerged: 1) knowledge and awareness about malaria, 2) socio-economic and cultural factors, 3) malaria prevention practice, 4) local concepts and perceptions regarding malaria and 5) health-seeking behaviour factors.
Knowledge and awareness about malaria
Nineteen studies reported that knowledge and awareness are major risk factors in malaria control and prevention in SA, mainly in some parts of India, Bangladesh and Sri Lanka (25–28, 30–33, 35, 36, 38, 39, 45, 47, 48, 51, 52, 55, 56). However, very few studies correctly reported the malaria parasite as a causative agent for malaria disease (28, 33, 36, 38), as well as the modes of transmission (30, 31, 44, 55). One study conducted in 2010 among school adolescents reported that only 8.6% (of 1,096 samples) students were aware of the causative agent. There were still some misconceptions about the mode of malaria transmission. The same study reported that over 33% of the students responded that houseflies were implicated in malaria (31). Another study reported that dirty water and food, person-to-person transfer and rain were considered as modes of malaria transmission, while only 24% of people correctly reported that mosquitoes transmit malaria (30). Similarly, a qualitative study conducted among pregnant women in India reported the mode of transmission:
If anyone eats leftover food, they will get a fever and maybe malaria …. Mosquitoes that had made contact with potentially unclean items such as drains, dirty water, bushes, or food, and mosquitoes born ‘due to dirtiness’ or ‘in garbage’ were listed as causes of malaria … If a mosquito defecates in water that is stored for household drinking then this can also cause malaria. (30, p. 1012)
Ten studies (29, 30, 32, 33, 38, 42, 48, 49, 52, 53) highlighted that some participants could not even figure out the symptoms of malaria and its treatment. Likewise, one study carried out in India (Orissa) (33) reported that only about 86% of the participants (male 92.8%; female 78.3%) had ever heard of the term ‘malaria’, and another study conducted in Pakistan (Jalozai) reported over 42% of the participants were not aware of malaria (44). The study further noted that participants knew or heard about malaria from multiple sources, that is, from health workers (doctors), neighbours, family members or community leaders. In five studies, it was reported that the media – television, radio, newspaper, internet and posters – were the main source of awareness and knowledge among the participants (28, 31, 34, 38, 43). The findings of this review noted that generally the level of knowledge and awareness about malaria was not only limited among the general public, but also limited among private healthcare professionals (47). A survey among Indian private practitioners carried out in 2006 reported that the knowledge of malaria treatment and danger signs was very low among private practitioners; therefore, there were some concerns of malaria deaths of those receiving private healthcare treatment (60, 61).
Various symptoms and complications regarding malaria, such as jaundice, acute kidney injury, generalised tonic–clonic convulsions, severe anaemia, shock, metabolic acidosis, hypoglycaemia and hyperpyrexia were found among the patients with P. vivax in a study carried out by Nandwani et al. (42), for which the symptoms are known to have been related with P. falciparum malaria in recent times. Despite the level of knowledge and awareness in diagnosing and treating malaria by auxiliary nurse midwives (ANMs) and accredited social health activists (ASHAs) with the use of RDT and ACT, malaria was still not treated on time due to unavailability of drugs (26, 32, 38, 46).
Socio-economic and cultural factors
Eight studies have reported the gap between the gender (male and female) and health-seeking behaviours in SA, where patriarchal norms, beliefs and perceptions still exist (26, 29, 32, 40, 44, 46, 50, 51). It was reported that female participants were generally less knowledgeable as compared to male participants about the cause and transmission of malaria (33, 45). However, a study conducted in Afghanistan reported that Afghan women were surprisingly knowledgeable (over 75%) about cause and prevention of malaria (36).
Eight studies highlighted socio-economic factors as barriers to malaria control and prevention in SA (25, 29, 38, 40, 47, 48, 54, 55). Yadav et al. (54) reported that the majority of people visited government healthcare facilities for blood examination, diagnosis and treatment, as compared to private healthcare facilities. One study, conducted in India, reported that about 51.7% of the participants were aware that governments were taking some initiatives for the prevention and control of malaria (31). Yet not every participant could take advantage of the facilities like follow-up, blood examination and medicines for the disease; this is mainly due to the affordability of travelling long distances and insufficient availability of public transport. In addition, four studies reported that the efforts of government health authorities against malaria are generally poor or inadequate mainly due to poor infrastructure, less qualified healthcare practitioners, lack of faith in government medicines, expensive and poor quality treatment, non-compliant or incomplete treatment (irrational and inappropriate treatment, lack of efficacy of drugs, inadequate surveillance and resource-poor health systems) (28, 32, 38, 50).
Seven studies reported that socio-economic factors led to an increase in malaria cases in several parts of SA (26, 27, 29, 40, 48, 50, 54). Therefore, there has been a clear emphasis that the government should focus on socio-economic factors in order to decrease the adverse effects of socio-economic factor attributes, including climate change, in vulnerability to malaria in this region. It was interesting to highlight that in most of the studies, it was reported that the majority of people knew about the use and importance of bed nets, which are considered as one of the potential protective interventions against malaria, but there was no relationship with their use due to affordability of bed nets within poor SA communities (25, 36, 39, 49, 55).
Malaria prevention practice
Six studies reported various measures to prevent malaria which exist in different parts of SA and that the success of these measures depends on the knowledge of, access to and utilisation of services, as well as a combination of users’ behaviours and healthcare access and quality issues (28, 35, 36, 38, 47, 51). These studies also highlighted that, despite people's knowledge and awareness about the use of bed nets and their effectiveness, not everyone used them because of the costs, concerns about safety (for pregnant women) and lack of availability (ITN), as well as promotion and pricing, including preferential treatment, as there were some strong perceptions that clinics and salesman prefer to sell these ITNs to their relatives or for profit (36). Though bed nets in general, and insecticide-treated nets in particular, generally reduce the burdens of malaria, the role of the protective effects of bed nets was not clear when comparing malaria deaths with malaria survivors (47). The same study explored two possibilities for protective effects: ‘one possibility could be that bed nets reduced the intensity of infection. The other possibility could be that ownership of bed net was a surrogate marker of socio-economic status, through residual confounding’ (p. 5).
Some studies reported that people used repellent coils, proper clothing that covers the whole body, spray and removal of stagnant water from the environment as preventive practices (28, 39, 46, 56). However, some ethnic groups in some parts of SA equally preferred traditional methods, like making bonfires, burning grass, rubbing lamp or motor oil on the skin, and sleeping wrapped in wet chadors and applying herbal oil to avoid mosquito bites, practices which were quite prevalent (30, 36, 45, 53). One study conducted in Afghanistan reported that people often use cooling drinks, such as dough or lassie (from yoghurt), or various plants, the most common of which was a tea from shamaki roots. Shamaki is a Pashtu term for a plant used locally in traditional medicine, and such traditional medicine is usually chosen due to cost (36). One respondent said:
We usually resort to traditional treatment rather than clinical treatment unless the traditional treatment doesn't work. It is due to poverty and people can't afford to cover doctor's and transportation costs. (36)
Similarly, another study conducted in Nepal reported that 16.3% (of 1,130) respondents did not consult anywhere and 16.1% consulted with traditional healers, with the reasons provided being lack of time to go to the health services, absence of health professionals in the health services and lack of knowledge of where to go when getting a fever with chills (38).
Concepts and perceptions
Several studies reported that local people perceived and defined malaria differently, and the perceived symptoms presented by the participants in the study were common cold, typhoid, tuberculosis, skin disease and diarrhoea (53, 54). Studies carried out by Das and Ravindran (32, 33) stated that people defined malaria using the term ‘meleria’ and that was equated with the meaning of ‘common disease’ in the community. Likewise, in a study carried out in India, it was found the community called malaria kakar jwar or Pali jwar, which was the concept often used to describe the symptoms of malaria among the tribes (54). However, despite the fact that the community gave their own name to the malarial symptoms, the participants clearly understood the term ‘malaria’, and most of the participants were aware that malaria is a serious public health issue (32, 38, 45, 54). This concept was no different between the LLIN users and non-users. However, people often reported that the degree of the seriousness of the disease was determined by the amount of physical suffering, the degree of daily activities being hindered and having to spend more money on treatment (32, 36, 38, 51, 55).
Health-seeking behaviour
Seven studies reported that delays in the diagnosis and treatment of malaria, even for a few days, would lead to a fatal outcome (25, 32, 34, 38, 47, 53, 54). It has been discussed that the community people who suffered from malaria would rather wait for a few more days and help themselves with home remedies. When the disease did not seem to get better, then the adults within the community would seek help from traditional healers (38, 45, 51). Four studies reported that the delayed treatment and delays in health-seeking practices were mainly due to the long walking distances to access the health facilities, long waiting time, unfriendly health workers, lack of money, loss of faith in the medical profession, lack of people to accompany patients to health services – primarily with small children of those parents who might be busy farming – compounded by difficult terrain, especially during monsoon (32, 39, 50, 51). Sometimes, it was simply due to some misconceptions; for example, one study conducted in Bhutan reported that still ‘people believe that malaria is caused by bad air, by staying in rain and long hours in sun, by local spirits, and taking fruits with sour taste’ (51, p. 276; 52, p. 2).
The responses in the study by Ahmed et al. (25) showed that the participants wished to go for allopathic treatment rather than seeking modern medicines. This led to delays in seeking healthcare, even when fever was noticed. Similarly, another study reported that people often seek treatment from traditional healers, and this was mainly due to the fact that the community lacks public transport, leading to the need to walk long distances in order to obtain essential healthcare at primary healthcare facilities (53).
Discussion and conclusion
This review examined the knowledge, attitudes and beliefs about malaria in SA. Although problems or concerns represented a diverse list of issues as SA is reasonably heterogeneous in terms of multi-cultural setups, variances in socio-cultural, economic, and demographic profiles, and dissimilar environments which are considered as suitable settings for mosquito-breeding (56), this study has added significantly to the literature on understanding and practices of prevention and control of malaria in this region. As far as the authors are aware, this is perhaps the first of its kind in terms of research to determine the knowledge, attitudes and beliefs about malaria in this region.
We found that appropriate understanding and awareness of malaria are considered essential components before taking any informed action for the prevention and treatment of malaria (26). The study also revealed that factors associated with cost (travel, treatment), distance to access/utilise health services, and perceptions of the healthcare expected from health services have been identified as major determinants that influence people's health-seeking behaviours, as has been clearly documented in other studies (62, 63).
Similarly, the findings of the study highlighted that though the knowledge of malaria among some participants was found to be generally high, which was similar to the previous studies conducted in Nigeria (64), Zimbabwe (65) and Sudan (66), the barriers seem mostly to be at the implementation step, largely due to socio-economic and cultural factors. This study has also revealed that those people who were most at risk – mainly children and pregnant women – were not given priority when dealing with preventive and treatment measures at both healthcare and household levels. This was consistent with the findings from Ethiopia's studies (67, 68) as they reported that malaria mostly affected poor and underserved tribal populations, who lived in remote forest areas, as these people are deprived in terms of access to adequate modern treatment facilities.
In SA, most of the people are poor and marginalised, their level of education is relatively poor and they mostly live in the remote villages, often deprived of modern healthcare facilities. Several studies supported similar findings stating that people – mainly the tribal or indigenous communities – were less able to obtain appropriate and timely treatment, even for minor illness, and as a result, they not only rely upon unproven traditional methods (30), but are also obliged to seek inappropriate care due to their low level of knowledge and awareness about the symptoms and seriousness of malaria (32). That may ultimately lead them to delay treatment. A previous study reported that in 2006, four out of six deaths from malaria occurred due to delayed treatment (69).
Evidence suggests that to better understand the challenges or barriers to the prevention and control of malaria, it is important to consider people's geographical and socio-cultural contexts (50). Malaria is very much linked with environmental determinants, including climate, agriculture, irrigation and forests, which significantly contribute to the variations in malaria incidence (48). It is, therefore, important to develop intersectoral co-operation or collaboration, working modally in terms of developing environmentally sound mosquito control activities with appropriate community participation (70, 71). Roll Back Malaria (RBM), an initiative launched jointly in Geneva by the United Nations Children's Emergency Fund (UNICEF), the United Nations Development Programme (UNDP), the World Bank and the WHO, is a people-oriented programme that emphasises community participation (44).
The findings of this review have clearly identified that even when there were health services available to people, the cost related to cure and prevention treatment for malaria has prevented the poor from seeking healthcare. Besides that, the cost of malaria prevention intervention measures was found to be more costly in rural areas as compared to urban areas (45). Similarly, this study noted that the use of bed nets was relatively poor and limited among the participants (32, 36). Bed nets, mainly ITNs, are reasonably cost-effective and are now considered as an integral component of global malaria control initiatives to decrease malaria cases and malarial mortality, if properly used and maintained (72). A study conducted in Uganda reported that the prevalence of malaria cases is significantly lower in households with ITNs compared to non-users (9% vs. 14%) (73). It is, therefore, important to distribute insecticidal nets in a more equitable manner (74–76), which is also one of the strategies for global malaria control in terms of achieving the malaria-related Millennium Development Goal (MDG) and RBM targets (77–79).
In SA, there is long experience of using vector control for the prevention and control of malaria (47). Vector control can help in prevention and control by ‘reducing the vector density or abundance, reducing longevity, and preventing human-vector contact’ (47, p. 1). The World Health Assembly (48) has called for support in developing countries’ capacities in expanding the use of effective interventions for malaria control. Indoor residual spraying was the main approach for controlling vector in most parts of SA, but its effectiveness was an issue due to insecticide resistance (46). Rowland et al. (14) argue that the standard method of malaria control in SA is indoor spraying of houses with residual insecticide, which is becoming prohibitively expensive to implement. Recently, it has been reported that drug-resistant parasites are prevalent in SA, which would threaten the control and elimination of malaria globally (2, 33, 38, 47).
This study was not without some limitations, and it was acknowledged that this study should be evaluated to be certain about the reliability and validity of the conclusion. Hence, any limitation encountered in the research literature studied could also affect the validity of the current study. Our study was not externally funded, and therefore, time and resources were severe constraints. Nonetheless, careful consideration was given to selection of the material for the systematic literature review, on the reliability and validity of the methodologies employed.
Despite these limitations, we believe that this study has been clearly recognised for its ability to identify the socio-cultural gaps in the research, which is often a neglected area in malaria research in general and the SA population in particular. The study emphasises that control and prevention of malaria prevention would be possible when the social and cultural factors need to be addressed, along with the other factors and the challenges. The regional director, WHO South-East Asia, emphasised that ‘successful and sustainable malaria control would need strong political will, participation of communities at risk of malaria, partnerships between the public, private, health and non-health sectors, and strong technical and management capacities for malaria control at all levels of the public health system’ (61). Strong disease surveillance, including monitoring and evaluation as well as early diagnosis and proper treatment of malaria, is the major approach, not only in reducing morbidity and mortality caused by malaria, but also leading to the pre-elimination phase of malaria (61). In addition, given the nature of the findings of the study, it is important to focus on the need to develop appropriate strategies to improve individual and community practices for the prevention and control of malaria through engaging social scientists in terms of conducting formative research as a basis for behaviour-change communications in various socio-cultural settings, as well as addressing other determinants to improve access to malaria interventions. Therefore, there is a need to invest more in social science research to support policy and practices to accelerate progress towards malaria elimination.
This study concludes that there is a need for changes in people's beliefs, attitudes and behaviours towards using long-lasting insecticide nets and indoor spraying with residual insecticides, as well as seeking early, effective diagnosis, treatment, vector control and personal protection. Adherence to treatment is equally important in bringing lasting change in people's health and livelihoods, which would ultimately accelerate to eliminating malaria. All of this requires training and education, public–private partnerships, and community awareness from SA (2, 80, 81).
Acknowledgements
The present article is based on the research undertaken for a public health project at the University of Bedfordshire, UK.
Authors’ contributions
AK and KR conceived and designed the study with advice from LO; KR, AK and LO reviewed, analysed and interpreted the data and contributed to drafting and finalising the manuscript.
Conflicts of interests and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
Disclaimer
The findings and conclusions in this article are by the authors and views expressed in this publication do not necessarily represent the decisions, policy or views of their institutions.
References
- 1.World Health Organization. Geneva: WHO; 2014. Factsheet: vector borne disease. Factsheet #387. [Google Scholar]
- 2.World Health Organization. World malaria report. Geneva: WHO; 2015. [Google Scholar]
- 3.Heymann D. Washington, DC: American Public Health Association; 2015. Control of communicable diseases manual. [Google Scholar]
- 4.World Health Organization. Geneva: WHO; 2015. South Asian Association for Regional Cooperation: partnership, interagency coordination and resource mobilization. [Google Scholar]
- 5.Asian Development Bank. Metro Manila: ADB; 2013. Malaria data in Asia and the pacific: by the numbers. [Google Scholar]
- 6.World Health Organization. World malaria report. Geneva: WHO; 2013. [Google Scholar]
- 7.Rijken MJ, McGready R, Boel ME, Poespoprodjo R, Singh N, Syafruddin D, et al. Malaria in pregnancy in the Asia-Pacific region. Lancet Infect Dis. 2012;12:75–88. doi: 10.1016/S1473-3099(11)70315-2. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. India: WHO-South East Asia Region; 2013. WHO calls for greater investment to eliminate malaria. [Google Scholar]
- 9.Grietens KP, Xuan XN, Ribera JM, Duc TN, Bortel WV, Ba NT. Low perception of malaria risk among the Ra-glai ethnic minority in south-central Vietnam: implications for forest malaria control. Malar J. 2010;9:23. doi: 10.1186/1475-2875-9-23. doi: http://dx.doi.org/10.1186/1475-2875-9-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kumar D, Kumar M, Kumar A, Singh SK. Chalcone and curcumin derivatives: a way ahead for malarial treatment. Mini Rev Med Chem. 2013;13:2116–33. doi: 10.2174/13895575113136660101. [DOI] [PubMed] [Google Scholar]
- 11.Kumar A, Chery L, Biswas C, Dubhashi N, Dutta P, Kumar V, et al. Malaria in South Asia: prevalence and control. Acta Trop. 2012;121:246–55. doi: 10.1016/j.actatropica.2012.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leslie T, Mayan MI, Hasan MA, Safi MH, Klinkenberg E, Whitty CJM, et al. Sulfadoxine-pyrimethamine, chlorproguanil-dapsone, or chloroquine for the treatment of plasmodium vivax malaria in Afghanistan and Pakistan: a randomized controlled trial. JAMA. 2007;297:2201–9. doi: 10.1001/jama.297.20.2201. [DOI] [PubMed] [Google Scholar]
- 13.Khatoon L, Khan IU, Shah SA, Jan MI, Ullah F, Malik SA. Genetic diversity of Plasmodium vivax and Plasmodium falciparum in Kohat district, Pakistan. Braz J Infect Dis. 2012;16:184–7. [PubMed] [Google Scholar]
- 14.Rowland M, Durrani N, Kenward M, Mohammed N, Urahman H, Hewitt S. Control of malaria in Pakistan by applying deltamethrin insecticide to cattle: a community-randomised trial. Lancet. 2001;357:1837–41. doi: 10.1016/S0140-6736(00)04955-2. [DOI] [PubMed] [Google Scholar]
- 15.Sharma R, Thakor H, Saha K, Sonal G, Dhariwal A, Singh N. Malaria situation in India with special reference to tribal areas. Indian J Med Res. 2015;141:537–45. doi: 10.4103/0971-5916.159510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dhillon HS, Kar SB. Geneva: WHO; 1963. Investigation of cultural patterns and beliefs among tribal populations in Orissa with regard to malaria eradication activities. [Google Scholar]
- 17.Bates I, Fenton C, Gruber J, Lalloo D, Lara AM, Medina Lara A, et al. Vulnerability to malaria, tuberculosis, and HIV/AIDS infection and disease. Part 1: determinants operating at individual and household level. Lancet Infect Dis. 2004;4:267–77. doi: 10.1016/S1473-3099(04)01002-3. [DOI] [PubMed] [Google Scholar]
- 18.Dash AP, Valecha N, Anvikar AR, Kumar A. Malaria in India: challenges and opportunities. J Biosci. 2008;33:583–92. doi: 10.1007/s12038-008-0076-x. [DOI] [PubMed] [Google Scholar]
- 19.Boland A, Cherry M, Dickson R. London: Sage; 2014. Doing a systematic review: a student's guide. [Google Scholar]
- 20.Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Policy. 2005;10:6–20. doi: 10.1258/1355819054308576. [DOI] [PubMed] [Google Scholar]
- 21.Guyatt G, Rennie D. Chicago, IL: American Medical Association; 2002. User's guides to the medical literature: a manual for evidence-based clinical practice. [Google Scholar]
- 22.Garg AX, Hackam D, Tonelli M. Systematic review and meta-analysis: when one study is just not enough. Clin J Am Soc Nephrol. 2008;3:253–60. doi: 10.2215/CJN.01430307. [DOI] [PubMed] [Google Scholar]
- 23.Institute of Medicine. Washington, DC: The National Academic Press; 2011. Finding what works in healthcare: standards for systematic review. [Google Scholar]
- 24.Smith KE, Bambra C, Joyce KE, Perkins N, Hunter DJ. Partners in health? A systematic review of the impact of organizational partnerships on public health outcomes in England between 1997 and 2008. J Public Health (Oxf) 2009;1:210–21. doi: 10.1093/pubmed/fdp002. [DOI] [PubMed] [Google Scholar]
- 25.Ahmed SM, Haque R, Haque U, Hossain A. Knowledge on the transmission, prevention and treatment of malaria among two endemic populations of Bangladesh and their health-seeking behavior. Malar J. 2009;8:173. doi: 10.1186/1475-2875-8-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ahmed SM, Hossain SM, Kabir M. Conventional or interpersonal communication: which works best in disseminating malaria information in an endemic rural Bangladeshi community? PLoS One. 2014;9:e90711. doi: 10.1371/journal.pone.0090711. doi: http://dx.doi.org/10.1371/journal.pone.0090711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ahmed SM, Hossain S, Kabir MM, Roy S. Free distribution of insecticidal bed nets improves possession and preferential use by households and is equitable: findings from two cross-sectional surveys in thirteen malaria endemic districts of Bangladesh. Malar J. 2011;10:357. doi: 10.1186/1475-2875-10-357. doi: http://dx.doi.org/10.1186/1475-2875-10-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anand T, Kumar R, Saini V, Meena G, Ingle G. Knowledge and use of personal protective measures against mosquito borne diseases in a resettlement colony of Delhi. Ann Med Health Sci Res. 2014;4:227–32. doi: 10.4103/2141-9248.129048. doi: http://dx.doi.org/10.4103/2141-9248.129048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bashar K, Al-Amin HM, Reza MS, Islam M, Asaduzzaman, Ahmed TU. Socio-demographic factors influencing knowledge, attitude and practice (KAP) regarding malaria in Bangladesh. BMC Public Health. 2012;12:1084. doi: 10.1186/1471-2458-12-1084. doi: http://dx.doi.org/10.1186/1471-2458-12-1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chourasia MK, Abraham VJ, John J. Household training vs. mass campaigns: a better method of health communication for preventing malaria. Trop Doct. 2014;44:196–200. doi: 10.1177/0049475514545201. [DOI] [PubMed] [Google Scholar]
- 31.Dambhare DG, Nimgade SD, Dudhe JY. Knowledge, attitude and practice of malaria transmission and its prevention among the school going adolescents in Wardha District, Central India. Glob J Health Sci. 2012;4:76–82. doi: 10.5539/gjhs.v4n4p76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Das A, Ravindran TS. Factors affecting treatment-seeking for febrile illness in a malaria endemic block in Boudh district, Orissa, India: policy implications for malaria control. Malar J. 2010;9:377. doi: 10.1186/1475-2875-9-377. doi: http://dx.doi.org/10.1186/1475-2875-9-377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Das A, Ravindran TS. Community knowledge on malaria among febrile patients in an endemic district of Orissa, India. J Vector Borne Dis. 2011;48:46–51. [PubMed] [Google Scholar]
- 34.Dhawan G, Joseph N, Pekow PS, Rogers CA, Poudel KC, Bulzacchelli MT. Malaria-related knowledge and prevention practices in four neighborhoods in and around Mumbai: a cross sectional study. Malar J. 2014;13:303. doi: 10.1186/1475-2875-13-303. doi: http://dx.doi.org/10.1186/1475-2875-13-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fernando SD, Abeyasinghe RR, Galappaththy GN, Gunawardena N, Rajapakse LC. Community factors affecting long-lasting impregnated mosquito net use for malaria control in Sri Lanka. Trans R Soc Trop Med Hyg. 2008;102:1081–8. doi: 10.1016/j.trstmh.2008.06.007. [DOI] [PubMed] [Google Scholar]
- 36.Howard N, Shafi A, Jones A, Rowland M. Malaria control under the Taliban regime: insecticide-treated net purchasing, coverage, and usage among men and women in eastern Afghanistan. Malar J. 2010;9:7. doi: 10.1186/1475-2875-9-7. doi: http://dx.doi.org/10.1186/1475-2875-9-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hussain MA, Dandona L, Schellenberg D. Public health system readiness to treat malaria in Odisha State of India. Malar J. 2013;12:351. doi: 10.1186/1475-2875-12-351. doi: http://dx.doi.org/10.1186/1475-2875-12-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Joshi A, Banjara MR. Malaria related knowledge, practices and behaviour of people in Nepal. J Vector Borne Dis. 2008;45:44–50. [PubMed] [Google Scholar]
- 39.Kirkby K, Galappaththy GN, Kurinczuk JJ, Rajapakse S, Fernando SD. Knowledge, attitudes and practices relevant to malaria elimination amongst resettled populations in a post-conflict district of northern Sri Lanka. Trans R Soc Trop Med Hyg. 2013;107:110–18. doi: 10.1093/trstmh/trs015. [DOI] [PubMed] [Google Scholar]
- 40.Kumar DS, Andimuthu R, Rajan R, Venkatesan MS. Spatial trend, environmental and socioeconomic factors associated with malaria prevalence in Chennai. Malar J. 2014;13:14. doi: 10.1186/1475-2875-13-14. doi: http://dx.doi.org/10.1186/1475-2875-13-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lwin MO, Vijaykumar S, Lim G, Theng YL, Foo S. ‘It's effective but should I bother?’ A study of personal protection measures against malaria in urban India. Public Health. 2014;128:654–64. doi: 10.1016/j.puhe.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 42.Nandwani S, Pande A, Saluja M. Clinical profile of severe malaria: study from a tertiary care center in north India. J Parasit Dis. 2014;38:11–15. doi: 10.1007/s12639-012-0208-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pandit N, Patel Y, Bhavsar B. Awareness and practice about preventive method against mosquito bite in Gujarat. Healthline. 2010;1:16–20. [Google Scholar]
- 44.Qayum M, Zahur H, Ahmad N, IIyas M, Khan A, Khan S. SPHERE-based assessment of knowledge and preventive measures related to malaria among the displaced population of Jalozai, Pakistan. J Pak Med Assoc. 2012;62:344–6. [PubMed] [Google Scholar]
- 45.Sabin LL, Rizal A, Brooks MI, Singh MP, Tuchman J, Wylie BJ, et al. Attitudes knowledge, and practices regarding malaria prevention and treatment among pregnant women in Eastern, India. Am J Trop Med Hyg. 2010;82:1010–16. doi: 10.4269/ajtmh.2010.09-0339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Saha KB, Sharma RK, Mishra R, Verma R, Tiwart BK, Singh N. Establishing communication mechanism for malaria prevention in Baiga tribal villages in Baiga Chak area of Dindori district, Madhya Pradesh. Indian J Med Res. 2015;141:576–83. doi: 10.4103/0971-5916.159516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sarkar J, Murhekar MV, Shah NK, van Hutin Y. Risk factors for malaria deaths in Jalpaiguri district, West Bengal, India: evidence for further action. Mala J. 2009;8:133. doi: 10.1186/1475-2875-8-133. doi: http://dx.doi.org/10.1186/1475-2875-8-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sharma RK, Singh MP, Saha KB, Bharti PK, Jain V, Singh PP, et al. Socio-economic & household risk factors of malaria in tribal areas of Madhya Pradesh, central India. Indian J Med Res. 2015;141:567–75. doi: 10.4103/0971-5916.159515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sood RD, Mittal PK, Kapoor N, Razdan RK, Dua VK, Dash AP. Community awareness, perceptions, acceptability and preferences for using LLIN against malaria in villages of Uttar Pradesh, India. J Vector Borne Dis. 2010;47:243–8. [PubMed] [Google Scholar]
- 50.Sundararajan R, Kalkonde Y, Gokhale C, Greenough PG, Bang A. Barriers to malaria control among marginalized tribal communities: a qualitative study. PLoS One. 2013;8:e81966. doi: 10.1371/journal.pone.0081966. doi: http://dx.doi.org/10.1371/journal.pone.0081966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tobgay T, Lhazeen K. 2010 malaria perceptions and practices in Bhutan. Southeast Asian J Trop Med Public Health. 2010;41:274–9. [PubMed] [Google Scholar]
- 52.Tobgay T, Pem D, Dophu U, Dumre SP, Na-Bangchang K, Torres CE. Community-directed educational intervention for malaria elimination in Bhutan: quasi-experimental study in malaria endemic areas of Sarpang district. Malar J. 2013;12:132. doi: 10.1186/1475-2875-12-132. doi: http://dx.doi.org/10.1186/1475-2875-12-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vijayakumar KN, Gunasekaran K, Sahu SS, Jambulingam P. Knowledge, attitude and practice on malaria: a study in a tribal belt of Orissa State, India with reference to use of long lasting treated mosquito nets. Acta Trop. 2009;112:137–42. doi: 10.1016/j.actatropica.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 54.Yadav SP, Yadav S, Kuma P, Yadav S. Knowledge, treatment-seeking behaviour and socio-economic impact of malaria in the desert of Rajasthan, India. South Afr J Epidemiol Infect. 2013;28:41–7. [Google Scholar]
- 55.Yasuoka J, Mangione TW, Spielman A, Levins R. Impact of education on knowledge, agricultural practices, and community actions for mosquito control and mosquito-borne disease prevention in rice ecosystems in Sri Lanka. Am J Trop Med Hyg. 2006;74:1034–42. [PubMed] [Google Scholar]
- 56.Zaidi SA, Kokab F, Bukhari IA, Nasir JA. The quantitative evidence of malarial transmission and its associates in Bahawalpur, Pakistan. J Ayub Med Coll Abbottabad. 2015;27:164–7. [PubMed] [Google Scholar]
- 57.Thomas J, Harden A. Methods for the thematic analysis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:45. doi: 10.1186/1471-2288-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ritchie J, Lewis J, Nicholas CM, Ormston R. London: Sage; 2014. Qualitative research practice: a guide for social science student and researchers. [Google Scholar]
- 59.Joff H. Thematic analysis. In: Harper D, Thompson A, editors. Qualitative research methods in mental health and psychotherapy: an introduction for students and practitioners. Chichester: Wiley-Blackwell; 2012. pp. 209–24. [Google Scholar]
- 60.Sharma PK, Sen TK, Ramakrishnan R, Hutin Y, Gupte MD. Lack of access to public health care, shift towards unqualified private providers and malaria deaths in Jalpaiguri district, West Bengal, India, 2006; Poster presented at the Bi-regional Tephinet conference in Taiwan; 2007. Nov, [Google Scholar]
- 61.Mishra SK, Mohanty S, Das BS. The influence of healthcare facilities on malarial mortality in and around Rourkela, India. Ann Trop Med Parasitol. 2002;96:835–37. doi: 10.1179/000349802125002248. [DOI] [PubMed] [Google Scholar]
- 62.Konradsen F, van der Hoek W, Amerasinghe PH, Amerasinghe FP, Fonseka KT. Household responses to malaria and their costs: a study from rural Sri Lanka. Trans R Soc Trop Med Hyg. 1997;91:127–30. doi: 10.1016/s0035-9203(97)90194-2. [DOI] [PubMed] [Google Scholar]
- 63.Williams HA, Jones CO. A critical review of behavioral issues related to malaria control in sub-Saharan Africa: what contributions have social scientists made? Soc Sci Med. 2004;59:501–23. doi: 10.1016/j.socscimed.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 64.Udonwa NE, Gyuse AN, Etokidem AJ. Malaria: knowledge and prevention practices among school adolescents in a coastal community in Calabar, Nigeria. Afr J Prm Health Care Fam Med. 2010;2:103. [Google Scholar]
- 65.Midzi N, Mtapuri-Zinyowera S, Mapingure MP, Paul NH, Sangweme D, Hlerema G, et al. Knowledge attitudes and practices of grade three primary schoolchildren in relation to schistosomiasis, soil transmitted helminthiasis and malaria in Zimbabwe. BMC Infect Dis. 2011;11:169. doi: 10.1186/1471-2334-11-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Erhun WO, Agbani EO, Adesanya SO. Malaria prevention: knowledge, attitude and practice in a Southwestern Nigerian community. Afr J Biomed Res. 2005;8:25–9. [Google Scholar]
- 67.Loha E, Tefera K, Lindtjørn B. Freely distributed bed-net use among Chano Mille residents, south Ethiopia: a longitudinal study. Malar J. 2013;12:23. doi: 10.1186/1475-2875-12-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Deribew A, Birhanu Z, Sena L, Dejene T, Reda AA, Sudhakar M, et al. The effect of household heads training on long-lasting insecticide-treated bed nets utilization: a cluster randomized controlled trial in Ethiopia. Malar J. 2012;11:99. doi: 10.1186/1475-2875-11-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Vector-borne Disease Control Programme. Thimphu, Bhutan: VBDCP, Ministry of Health; 2006. Annual malaria report. [Google Scholar]
- 70.Konradsen F, Amerasinghe FP, van der Hoek W, Amerasinghe PH. Battaramulla, Sri Lanka: International Water Management Institute; 2000. Malaria in Sri Lanka, current knowledge on transmission and control. [Google Scholar]
- 71.Silva KT. “Public health” for whose benefit? Multiple discourses on malaria in Sri Lanka. Med Anthropol. 1997;17:195–214. doi: 10.1080/01459740.1997.9966137. [DOI] [PubMed] [Google Scholar]
- 72.UNICEF. Malaria. 2013. UNICEF. Available from: http://www.unicef.org/health/index_malaria.html [cited 2 April 2016]
- 73.Spencer S, Grant AD, Piola P, Tukpo K, Okia M, Gracia M, et al. Malaria in camps for internally-displaced persons in Uganda: evaluation of an insecticide treated bednet distribution programme. Trans R Soc Trop Med Hyg. 2004;98:719–27. doi: 10.1016/j.trstmh.2004.01.012. [DOI] [PubMed] [Google Scholar]
- 74.Tekelehaimanot A, Sachs JD, Curtis C. Malaria control needs mass distribution of insecticidal bednets. Lancet. 2007;369:2143–6. doi: 10.1016/S0140-6736(07)60951-9. [DOI] [PubMed] [Google Scholar]
- 75.Curtis C, Maxwell C, Leminge M, Kilama WL, Steketee RW, Hawley WA, et al. Scaling up coverage with insecticide-treated nets against malaria in Africa: who should pay? Lancet Infect Dis. 2003;3:304–7. doi: 10.1016/s1473-3099(03)00612-1. [DOI] [PubMed] [Google Scholar]
- 76.Noor AM, Mutheu JJ, Tatem AJ, Hay SI, Snow RW. Insecticide-treated net coverage in Africa: mapping progress in 2000–07. Lancet. 2009;373:58–67. doi: 10.1016/S0140-6736(08)61596-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.RBM Partnership. Geneva: WHO; 2008. The Global Malaria Action Plan: for a malaria-free world. [Google Scholar]
- 78.RBM Partnership Secretariat. Geneva: WHO; 2005. RBM global strategy 2005–2015. [Google Scholar]
- 79.Hill J, Lines J, Rowland M. Insecticide-treated nets. Adv Parasitol. 2006;61:77–128. doi: 10.1016/S0065-308X(05)61003-2. [DOI] [PubMed] [Google Scholar]
- 80.World Health Organization. Geneva: WHO; 2015. Guidelines for the treatment of malaria. [PubMed] [Google Scholar]
- 81.National Vector Borne Disease Control Programme, National Institute of Malaria Research. Guidelines for diagnosis and treatment of malaria in India. India: Government of India; 2009. Available from: http://www.nvbdcp.gov.in/Doc/Guidelines-Diagnosis-Treatment-Mal-2009.pdf [cited 2 April 2016] [Google Scholar]