1. Introduction
Ischemic heart disease is caused by atherosclerotic and/or thrombotic obstruction of coronary arteries. Clinical spectrum of ischemic heart disease expands from asymptomatic atherosclerosis of coronary arteries to acute coronary syndromes (ACS) including unstable angina, acute myocardial infarction (non-ST elevation myocardial infarction and ST elevation myocardial infarction). Stable ischemic heart disease (SIHD) refers to patients with known or suspected SIHD who have no recent or acute changes in their symptomatic status, suggesting no active thrombotic process is underway. These patients include those with (1) recent-onset or stable angina or ischemic equivalent symptoms, such as dyspnea or arm pain with exertion; (2) post-ACS stabilized after revascularization or medical therapy; and (3) asymptomatic SIHD diagnosed by abnormal stress tests or imaging studies. This review summarizes clinical features and management of SIHD in the older adult. ACS in older adults is not considered in this review.
Age is a strong independent risk factor for the development of atherosclerotic arterial disease. In the coming decades, tremendous increase of the prevalence of SIHD in the older adults is projected for the following reasons: (1) The world's population is aging, with those aged 80 and older expanding most rapidly. (2) The elderly population makes up the majority of new angina pectoris patients. In the USA, the annual rates per 1000 population of new episodes of angina pectoris of nonblack men were reported to be 28.3 for those 65 to 74 years of age, 36.3 for 75 to 84 years of age and 33.0 for ≥ 85 years of age; and 14.1, 20.0 and 22.0 for nonblack women in the same age groups; 22.4, 33.8 and 39.5 for black women; 15.3, 23.6 and 35.9 for black women, respectively.[1] (3) The acute myocardial infarction (AMI) survival rate has improved dramatically under current ACS care, so large numbers of AMI patients become SIHD patients. (4) The increased use of non-invasive (coronary artery calcium score, coronary CT angiography, etc) and invasive diagnostic modalities adds significantly to the number diagnosed with SIHD. SIHD in the older adult presents unique challenges to the healthcare community with predictable increasing burden but less clinical evidence to guide practice.
In the older adults, SIHD has equal prevalence in men and women. Obstructive coronary artery disease (CAD) is often more diffuse and severe anatomically. These patients have higher prevalence of left main stenosis, multi-vessel disease and impaired left ventricular function than in younger patients. In this population, other pathophysiological mechanisms may also cause myocardial ischemia and contribute to SIHD clinical presentation. These include microvascular dysfunction, endothelial dysfunction, vascular spasm or micro-embolism, left ventricular hypertrophy associated microvascular insufficiency or other factors contributing to supply-demand imbalance.[2] Microvascular and endothelial dysfunction are common in the older adult population. Therefore, SIHD in the older adult requires a comprehensive approach, not only diagnosing and treating obstructive CAD, but also managing other potential etiologies.
2. Clinical presentations and general evaluation
A thorough history and physical examination is strongly indicated for the evaluation of patients suspected of having SIHD. It provides critical information regarding typical versus atypical angina, cardiac versus non-cardiac symptoms, high risk vs. non-high risk features, as well as contributing non-cardiac etiologies. However, obtaining information accurately in older adults may be challenged by declining activity level, presence of comorbid conditions, cognitive impairment and atypical symptoms. Only a minority of older adults with ischemic heart disease complain of typical angina. Ischemia presentations are often characterized by lack of energy, exertional fatigue and dyspnea, epigastric or back discomfort. The origins of many of these symptoms are difficult to differentiate from chronic anemia, arthritis, gastric dysfunction, chronic lung disease, and overall physical inactivity. Post-prandial or emotional stress triggers may be common. Careful physical examination often leads to important clues of significant rhythms abnormalities (e.g., atrial fibrillation, bradycardia), valvular diseases, and peripheral arterial disease (e.g., carotid bruits, abdominal aorta aneurysm bruit and diminished pedal pulse).
The prevalence of resting electrocardiographic (ECG) abnormalities is significantly higher in older asymptomatic women and men, such as the prevalence of large or intermediate Q-waves, left axis deviation, T-wave inversions, left ventricular hypertrophy, bundle branch block and atrial fibrillation/flutter.[3] Many of these abnormalities confound the use of ECG in risk stratification and guide modality for non-invasive ischemia workup. Transthoracic echocardiography is informative in the diagnosis and management of SIHD in the older adults, providing information on left ventricular function, segmental ventricular contractility, left ventricular hypertrophy, diastolic function, valvular disease, and aortic root condition.
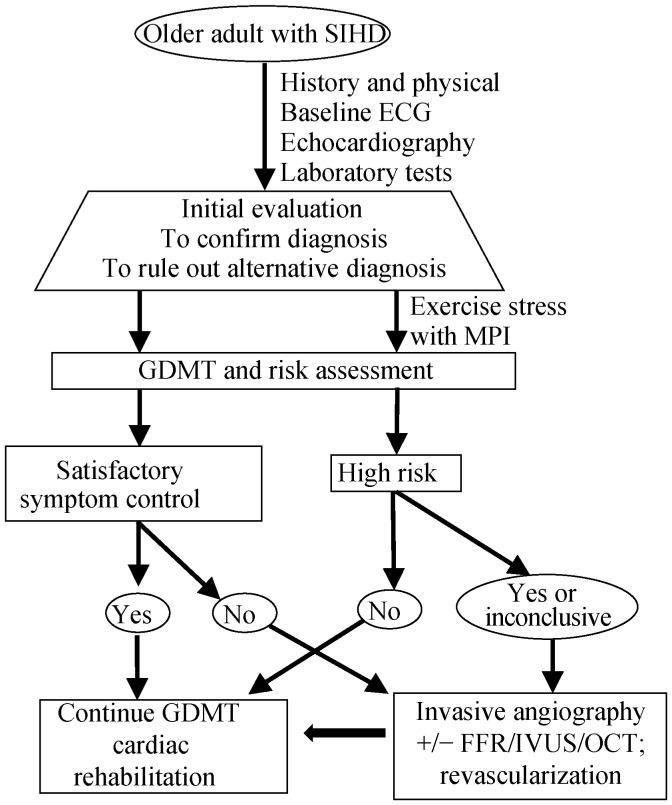
In contrast to an older adult with an acute presentation of coronary artery disease, an older adult who is asymptomatic or has stable symptoms benefits from CAD risk modification and guideline directed preventive therapy. Additional ischemic workup may be warranted if symptoms are not managed with initial attempts at medical therapy. Figure 1. is the flow chart of assessment and management of SIHD in the elderly.
Figure 1. Flow chart of assessment and management of SIHD in the elderly.
The corner stone of caring for SIHD is risk assessment and optimizing GDMT. SIHD older adult have high risk of ischemic events and refactor symptoms despite optimized GDMT may be recommended by invasive coronary angiography and revascularization. FFR: fractional flow reserve; GDMT: guideline directed medical therapy; OCT: optical coherence tomography; MPI: myocardial perfusion imaging; SIHD: stable ischemia heart disease; IVUS: intravascular ultrasound.
3. Risk assessment and ischemia workup
Clinical risk assessment is an important part of the SIHD workup in older adults. Prolonging survival with optimal quality of life is the main goal, and is informed by the patient's underlying risk of adverse outcome and symptom status. Risk assessment incorporates socio-demographics, symptoms and signs, risk factors, comorbid conditions, laboratory data, ECG and other non-invasive or invasive ischemic workup results. Existing models used to assess the risk are derived from populations aged ≤ 70 years, so their specificity and sensitivity in the older adult are less certain. The selection of ischemic testing modalities should be based on an estimation of the pre-test probability of ischemic heart disease or obstructive CAD.[4] When pre-test probability of ischemic heart disease is low (< 20%), further workup is not recommended due to a concern of false positive rate exceeding the true positive rate. When the pre-test probability is high (> 80%), negative non-invasive test results may not exclude obstructive CAD, so an invasive approach may provide a more definitive answer. Patients with intermediate pre-test likelihood benefit most from stress testing.
3.1. Exercise treadmill test
Whereas exercise treadmill testing (ETT) is often used in the assessment of CAD, the diagnostic and prognostic sensitivity and specificity of ETT is often questioned in older adults.[5] Lower exercise capacity associated with aging (i.e., effects of reduced peak heart rate, reduced muscle mass, as well as deconditioning) may limit exercise workload such that it is insufficient to provoke ischemic ECG changes or symptoms. Comorbidities associated with aging also often additionally impede exercise, and baseline ECG abnormalities often diminish specificity of any exercise-induced ECG changes.
While ETT is less useful to diagnose ischemia in older adults, it may still provide insights for clinical management. Symptoms, chronotropic responses, arrhythmias, hemodynamics, exercise capacity, cardiorespiratory fitness, and other parameters can often by ascertained by exercise testing. Furthermore, ETT can be coupled with cardiopulmonary assessments and imaging assessments (e.g., myocardial perfusion imaging or echocardiography) to increase sensitivity and specificity to detect ischemia, and to also ascertain additional insights regarding pulmonary hypertension, valvular heart disease, and other pertinent aspects of disease and management.[6]
3.2. Imaging modalities
Both SPECT myocardial perfusion imaging (MPI) and echocardiology can be coupled with ETT to improve ischemic specificity and sensitivity.[7],[8] The diagnostic/prognostic utilities of both modalities are similar to one other, and often depends on particular expertise and/or equipment that is available at different hospital centers.
For older patients who are unable to exercise, pharmacological stress can be coupled with MPI or echocardiography (i.e., pharmacological stress tests) to still enable diagnostic and risk stratification of SIHD in the older adult.[9] For MPI, vasodilating agents are usually the preferred pharmacological stress option as they facilitate sensitive ischemic assessments that are generally well tolerated. For both MPI and echocardiographic pharmacologic studies, dobutamine can also be used to provoke stress. Since dobutamine is relatively more likely to provoke arrhythmias and hemodynamic lability than vasodilating agents, it is used relatively less frequently for SPECT imaging, but it remains the primary pharmacological stimulus for pharmacologic echocardiographic stress tests.
3.3. Coronary calcium score and coronary CT angiography
Older adults have high prevalence of coronary calcification. For asymptomatic individuals 70 years of age or older, electron beam tomography (EBT) derived coronary artery calcium (CAC) score was found to improve prediction of coronary events based on cardiovascular risk factors in a population-based study, in particular, elderly persons with no or very low CAC have a lower mortality rate.[10] However, the value of CAC score in symptomatic elderly patients with suspected SIHD is limited. Coronary CT angiography (CCTA) is another commonly used imaging modality in detecting obstructive CAD and is found beneficial in younger adults. However, due to high prevalence of significant coronary calcification, and inability to perform satisfactory breath-hold for the scan, CCTA may be less accurate and less feasible for some older patients.[11]
3.4. Invasive coronary angiography
Coronary angiography remains the “gold standard” for definitive evaluation of epicardial CAD. It provides information for assessment of risk of death and future cardiovascular events. It is a prerequisite for ascertaining the feasibility and selection of revascularization approaches if indicated. In general, coronary angiography is recommended for patients whose clinical characteristics and/or results noninvasive testing indicate a high likelihood of severe IHD at high risk of coronary events or death. Coronary angiography is also recommended for patients with moderate clinical risk profile who have decreased left ventricular contractile function, inconclusive prognostic information after non-invasive testing, or unsatisfactory quality of life thought to be due to IHD.[12] Coronary angiography is generally safe in the older adults. However, increased risks of bleeding, stroke, contrast-induced kidney injury and increased prevalence of peripheral arterial disease and tortuosity, chronic kidney disease, and decreased tolerance of sedative and narcotics, are factors requiring attention. Despite some risks, older adults may benefit from coronary angiography due to higher prevalence of multi-vessel and left main CAD, atypical presentations and inconclusive non-invasive testing.
4. Treatment
4.1. Treatment goals
The goals for SIHD treatment include maximizing survival, minimizing risk of cardiovascular events and achieving nearly complete elimination of symptoms with return to normal activities. Older adults with declined baseline activity level, multiple serious coexisting conditions, may be satisfied with a reduction in symptoms that permits continuation of some limited activities of daily living. Therefore, individualized discussion about goals of treatments, risk and benefit of therapeutic approaches, especially revascularization of obstructive CAD by either percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) surgery, is important. Patients' preferences can vary as a function of age. Improvement of quality of life, eliminating symptoms and maintenance of independency in daily life become more important than prolonging length of life in the decision-making of the older adults.[13]
4.2. Guideline-directed medical therapy and risk factor modification
More than 30% SIHD patients are aged 75 years and older, and these patients have higher mortality. Guideline-directed medical therapy (GDMT) is as effective as compared to younger groups, with favorable benefit and risk ratio.[14],[15] GDMT should be the initial approach in treating most patients with SIHD, including older adults. A comprehensive GDMT for SIHD would include: (1) patient education and counseling to promote lifestyle changes, i.e., smoking cessation, maintaining healthy weight, engaging physical activity, adopting healthy diet, achieving psychosocial well-being and increasing medication adherence and involvement of self-monitoring; (2) pharmacological therapy to optimize risk factor modification, i.e., blood pressure, glucose and cholesterol control and treating other comorbid conditions; (3) medical therapy to prevent MI with anti-platelet therapy and other agents; and (4) medical therapy to relieve ischemic symptoms. All agents proven to be beneficial to younger groups with SIHD may be used in the older adults, with cautions to be paid due to alteration of cardiovascular physiology and their response to each medication (Table 1). These approaches/agents decrease SIHD patient's vulnerability, partially by its plaque stabilizing effects via reducing inflammation, lipid content, and thrombotic potential and improving endothelial dysfunction. Selection of agents for older adults might be also individualized according to comorbidities, contra-indications, adverse effects, drug and costs, and personal preference.
Table 1. Categories of pharmacotherapy for management of SIHD.
| GDMT agents | Risk factor modification | MI risk reduction | Symptom relief | Mortality reduction | Cautions for older adults |
| Aspirin | No | Yes | Yes | Yes | Increased risk of bleeding |
| BBs | Yes | Yes | Yes | Yes | High prevalence of adrenergic dysfunction, bradycardia and hypotension |
| CCBs | Yes | Yes | Yes | No | High incidence of bradycardia and hypotension |
| ACEi/ARB | Yes | Yes | No | Yes | Vulnerable kidney function, high prevalence of renal artery stenosis |
| Statin | Yes | Yes | No | Yes | High rate of intolerance and adverse effects |
| Nitroglycerin | No | No | Yes | No | Less hemodynamic reserve, hypotension |
| Ranolazine | No | No | Yes | No | Increased rate of non-specific adverse effects |
| Nicorandil | Yes | Yes | Yes | No | Comparable to isosorbide mononitrate, no special adverse effect reported |
ACEi: angiotensin-converting-enzyme inhibitor; ARB: angiotensin receptor blockers; BBs: beta-adrenergic blocking agents; CCBs: calcium channel blocking agents; MI: myocardial infarction; SIHD: stable ischemic heart disease.
4.3. Revascularization therapy
Older adults are known to have increased mortality and morbidity undergoing PCI and CABG revascularization comparing to younger patients. Revascularization and its approach should be carefully planned after considerations of coronary anatomy, technical feasibility, risks of complication, patient preferences, functional capacity, goal of care, quality-of-life, life-expectancy, and end-of-life issues, as well as alternative therapies. Nevertheless, SIHD patients with refractory symptoms despite GDMT, particularly if evidence of moderate or severe ischemia in non-invasive diagnostic tests, should be considered for invasive coronary angiographic and optimal revascularization. In the TIME study, faster symptom relief and improved exercise capacity were achieved by revascularization in comparison to GDMT alone in elderly SIHD patients (aged ≥ 75 years with mean 80 years).[16] Revascularization also reduces hospitalization, non-fatal MI and improves survival in the elderly population.
The comparative effectiveness of PCI and CABG for SIHD are an ongoing topic of debate which continues to evolve as new approaches, stents and understanding of complete revascularization enter the discussion. Selection of approach should consider CAD lesion complexity (SYNTAX score as a surrogate), surgical risk (STS score, EuroScore), comorbid conditions, functional capacity, and patient's preference. Limited data suggests comparable mortality and symptom relief between CABG and PCI, but very few patients aged ≥ 75 years were included in these studies. CABG may result in a higher rate of complete revascularization, lower recurrence of symptoms and better long term mortality. However, CABG requires longer recovery, higher risk of stroke and peri-procedural neurological complications (60% post CABG elderly patients experience short term and 20% long term cognitive impairment), as well as higher costs for the index hospitalization and lifetime.[17],[18] To many older adults, improving quality of life, eliminating adverse symptoms and maintaining independence in daily life becomes more important than prolonging the length of life in the decision-making process. It is understandable that a less invasive approach with PCI is preferable among older adults. Advancement of PCI techniques (i.e., increased use of radial artery approach, more sophisticated devices and balloon/stent designs) and rigorous and standardized professional training and regulations, adjunctive pharmacotherapy and post procedure dual antiplatelet therapy contribute to steadily declined procedural complications.[19] However, comparing with younger patients, PCI has higher rate of complications including bleeding, stroke, contrast-induced kidney injury and post-procedural MI in older adults.[20] Drug eluting stents reduce the rates of in-stent restenosis compared with bare metal stents but require longer duration of dual antiplatelet therapy associated increased risk of bleeding.
5. Follow-up care and cardiac rehabilitation
Considering that older adults with SIHD often have multiple comorbidities, it is essential to have appropriate clinical follow-up to ensure regular communication. Secondary prevention in the elderly has been addressed extensively in previous review.[20] Comprehensive, exercise-centered cardiac rehabilitation is effective in reducing mortality, decreasing hospitalization and improving quality-of-life in older SIHD patients. Exercise training improves exercise tolerance and functional capacity, and education and counseling reduces the risk of further cardiac events by optimizing pharmacological therapy (e.g., monitoring and encouraging concordance with medication). Other important outcomes of patient education include promotion of a healthy lifestyle (e.g., smoking cessation, dietary advice, increasing physical activity) and identifying and counseling of post cardiac event psychological stresses.
6. Future opportunities and clinical pearls
There are opportunities for research: (1) comparative effectiveness of GDMT alone and GDMT plus revascularization in the older adult with SIHD; (2) comparative effectiveness of multivessel PCI with new generation drug eluting stents or CABG for older adults with left main or complex multi-vessel CAD; and (3) optimizing risk assessment of SIHD in older adults with invasive (angiography) or non-invasive (CCTA and echo) testing.
Clinical pearls include: (1) SIHD is common in older adults with equal prevalence in men and women. (2) Older adults with SIHD have more comorbidities and higher risk profiles. They have a high prevalence of multi-vessel CAD, left main disease and left ventricular dysfunction. (3) Exercise stress test with and without pharmacological stress combined with myocardial perfusion imaging is often used for risk assessment. (4) Invasive coronary angiography is reserved for older adults with SIHD and high likelihood of severe IHD in non-invasive testing, or moderate risk with depressed left ventricular function, or inconclusive non-invasive testing and unsatisfactory symptom controls despite optimized GDMT. (5) GDMT is the first line therapy for older adult with SIHD. This modality includes lifestyle modification and pharmacotherapy with the goals of risk factor modification, reduction of MI risk, symptoms relief and prolonging of life. (6) Older adults with refractory symptoms affecting quality of life despite optimized GDMT should be referred for revascularization. (7) Clinic follow-up and cardiac rehabilitation are integrative components of care for SIHD in the older adults.
References
- 1.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics-2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marzilli M, Merz CN, Boden WE, et al. Obstructive coronary atherosclerosis and ischemic heart disease: an elusive link! J Am Coll Cardiol. 2012;60:951–956. doi: 10.1016/j.jacc.2012.02.082. [DOI] [PubMed] [Google Scholar]
- 3.Molander U, Dey DK, Sundh V, et al. ECG abnormalities in the elderly: prevalence, time and generation trends and association with mortality. Aging Clin Exp Res. 2003;15:488–493. doi: 10.1007/BF03327371. [DOI] [PubMed] [Google Scholar]
- 4.Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med. 1979;300:1350–1358. doi: 10.1056/NEJM197906143002402. [DOI] [PubMed] [Google Scholar]
- 5.Katsikis A, Theodorakos A, Kouzoumi A, et al. Prognostic value of the Duke treadmill score in octogenarians undergoing myocardial perfusion imaging. Atherosclerosis. 2014;236:373–380. doi: 10.1016/j.atherosclerosis.2014.07.028. [DOI] [PubMed] [Google Scholar]
- 6.Fletcher GF, Ades PA, Kligfield P, et al. Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation. 2013;128:873–934. doi: 10.1161/CIR.0b013e31829b5b44. [DOI] [PubMed] [Google Scholar]
- 7.Hachamovitch R, Kang X, Amanullah AM, et al. Prognostic implications of myocardial perfusion single-photon emission computed tomography in the elderly. Circulation. 2009;120:2197–2206. doi: 10.1161/CIRCULATIONAHA.108.817387. [DOI] [PubMed] [Google Scholar]
- 8.Rai M, Baker WL, Parker MW, et al. Meta-analysis of optimal risk stratification in patients > 65 years of age. Am J Cardiol. 110:1092–1099. doi: 10.1016/j.amjcard.2012.05.048. [DOI] [PubMed] [Google Scholar]
- 9.Makaryus AN, Diamond JA. Nuclear stress testing in elderly patients: a review of its use in the assessment of cardiac risk, particularly in patients undergoing preoperative risk assessment. Drugs Aging. 2007;24:467–479. doi: 10.2165/00002512-200724060-00003. [DOI] [PubMed] [Google Scholar]
- 10.Tota-Maharaj R, Blaha MJ, McEvoy JW, et al. Coronary artery calcium for the prediction of mortality in young adults < 45 years old and elderly adults > 75 years old. Eur Heart J. 33:2955–2962. doi: 10.1093/eurheartj/ehs230. [DOI] [PubMed] [Google Scholar]
- 11.Chan W, Liew C, Chin S, et al. Feasibility and accuracy of coronary imaging in elderly patients using the 64-row muIti-detector computed tomography:a correlation study with conventionaI coronary angiography. J Geriatric Cardiology. 2006;3:9–14. [Google Scholar]
- 12.Niebauer J, Sixt S, Zhang F, et al. Contemporary outcome of cardiac catheterizations in 1085 consecutive octogenarians. Int J Cardiol. 2004;93:225–230. doi: 10.1016/S0167-5273(03)00216-X. [DOI] [PubMed] [Google Scholar]
- 13.Singh M, Alexander K, Roger VL, et al. Frailty and its potential relevance to cardiovascular care. Mayo Clin Proc. 2008;83:1146–1153. doi: 10.4065/83.10.1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maron DJ, Spertus JA, Mancini GB, et al. Impact of an initial strategy of medical therapy without percutaneous coronary intervention in high-risk patients from the Clinical Outcomes Utilizing Revascularization and Aggressive DruG Evaluation (COURAGE) trial. Am J Cardiol. 2009;104:1055–1062. doi: 10.1016/j.amjcard.2009.05.056. [DOI] [PubMed] [Google Scholar]
- 15.Pfisterer M, Buser P, Osswald S, et al. Outcome of elderly patients with chronic symptomatic coronary artery disease with an invasive vs. optimized medical treatment strategy: one-year results of the randomized TIME trial. JAMA. 2003;289:1117–1123. doi: 10.1001/jama.289.9.1117. [DOI] [PubMed] [Google Scholar]
- 16.Pfisterer M. Long-term outcome in elderly patients with chronic angina managed invasively versus by optimized medical therapy: four-year follow-up of the randomized Trial of Invasive versus Medical therapy in Elderly patients (TIME) Circulation. 2004;110:1213–1218. doi: 10.1161/01.CIR.0000140983.69571.BA. [DOI] [PubMed] [Google Scholar]
- 17.Newman MF, Kirchner JL, Phillips-Bute B, et al. Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med. 2001;344:395–402. doi: 10.1056/NEJM200102083440601. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Z, Kolm P, Grau-Sepulveda MV, et al. Cost-effectiveness of revascularization strategies: the ASCERT study. J Am Coll Cardiol. 2015;65:1–11. doi: 10.1016/j.jacc.2014.09.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang TY, Gutierrez A, Peterson ED. Percutaneous coronary intervention in the elderly. Nat Rev Cardiol. 2011;8:79–90. doi: 10.1038/nrcardio.2010.184. [DOI] [PubMed] [Google Scholar]
- 20.Damluji A, Ramireddy A, Otalvaro L, et al. Secondary cardiovascular prevention in older adults: an evidence based review. J Geriatric Cardiology. 2015;12:459–464. doi: 10.11909/j.issn.1671-5411.2015.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]