Abstract
Objective
To assess the influence of age on the error of estimate (EE) of maximal oxygen uptake (VO2max) using sex and population specific-equations in cycle ergometer exercise testing, since estimated VO2 max is associated with a substantial EE, often exceeding 20%, possibly due to intrinsic variability of mechanical efficiency.
Methods
1850 adults (68% men), aged 18 to 91 years, underwent maximal cycle ergometer cardiopulmonary exercise testing. Cardiorespiratory fitness (CRF) was assessed relative to sex and age [younger (18 to 35 years), middle-aged (36 to 60 years) and older (> 60 years)]. VO2max [mL·(kg·min)−1] was directly measured by assessment of gas exchange and estimated using sex and population specific-equations. Measured and estimated values of VO2max and related EE were compared among the three age- and sex-specific groups.
Results
Directly measured VO2max of men and women were 29.5 ± 10.5 mL·(kg·min)−1 and 24.2 ± 9.0 mL·(kg·min)−1 (P < 0.01). EE [mL·(kg·min)−1] and percent errors (%E) for men and women had similar values, 0.5 ± 3.2 and 0.4 ± 2.9 mL·(kg·min)−1, and −0.8 ± 13.1% and −1.7 ± 15.4% (P > 0.05), respectively. EE and %E for each age-group were, respectively, for men: younger = 1.9 ± 4.1 mL·(kg·min)−1 and 3.8 ± 10.5%, middle-aged = 0.6 ± 3.1 mL·(kg·min)−1 and 0.4 ± 10.3%, older = −0.2 ± 2.7 mL·(kg·min)−1 and −4.2 ± 16.6% (P < 0.01); and for women: younger = 1.2 ± 3.1 mL·(kg·min)−1 and 2.7 ± 10.0%, middle-aged = 0.7 ± 2.8 mL·(kg·min)−1 and 0.5 ± 11.1%, older = -0.8 ± 2.3 mL·(kg·min)−1 and −9.5 ± 22.4% (P < 0.01).
Conclusion
VO2max were underestimated in younger age-groups and were overestimated in older age groups. Age significantly influences the magnitude of the EE of VO2max in both men and women and should be considered when CRF is estimated using population specific equations, rather than directly measured.
Keywords: Aging, Cardiopulmonary exercise testing, Error of measurement
1. Introduction
Cardiorespiratory fitness (CRF) is an important health indicator that is typically expressed as maximal oxygen uptake (VO2max).[1]–[3] Accordingly, VO2max is routinely used as a diagnostic and prognostic index.[4]–[10] Ideally, VO2max is directly measured during maximal cardiopulmonary exercise testing (CPX), as it provides the most valid and reliable assessment of aerobic fitness.[11] Nevertheless, for varied reasons, most clinical exercise testing labs do not regularly perform ventilatory gas analyses and CPX. Consequently, clinicians often rely on estimated VO2max values using equations which combine exercise duration and maximal workload achieved during standard electrocardiographic (ECG) exercise stress testing.[12],[13] Estimated VO2max assessments have been validated relative to directly measured VO2max values, but for a given subject there may be a large magnitude of error, signified by the error of estimate (EE).[14],[15] The associated EE has been reported to often exceed 20%.[1] The imprecision of these estimates may negatively impact related clinical decisions regarding patient management and risk stratification.
Large EE may be partially attributed to differences in mechanical efficiency, as reflected by the ability to perform work through the utilization of oxygen consumption.[13] Sex is one variable that may also influence mechanical efficiency and the associated EE.[14]–[17] Considering the growing number of elderly subjects worldwide, it is of critical importance to delineate factors affecting peak or symptom-limited exercise testing and the key assessments it provides.[18] Furthermore, as the majority of the equations used to estimate VO2max were developed based in young and middle-age individuals, it is important to assess the outcome of estimating VO2max in older ones. Therefore, in this study, we hypothesized that older age exacerbates the EE when using population-specific equations to estimate VO2max, due to intrinsic variability of mechanical efficiency. Therefore, we assessed EE underlying the estimation of VO2max in progressive age groups (i.e., younger, middle-aged, older) of men and women.
2. Methods
2.1. Sample
Our study population included voluntary adult subjects in a private clinic who underwent maximal cycle ergometer CPX between January 2008 and December 2014. All subjects provided informed consent and authorized the de-identified use of their collective data for research purposes. The study protocol and retrospective data analysis were approved by the institutional ethics committee.
After excluding subjects that were previously tested at this clinic, those who had undergone treadmill testing, individuals who did not meet criteria for a maximal CPX, and additional subjects with incomplete data, the final study population included 1850 subjects.
2.2. Anthropometric measurements
Body weight was measured without shoes to the nearest 0.1 kg in subjects wearing light clothing. Height was measured to the nearest 0.1 cm. Body mass index (BMI) was calculated by the ratio of body weight and the square of height (kg/m2).
2.3. Maximal cardiopulmonary exercise testing
Maximal CPX was conducted using an electromagnetically-braked cycle ergometer (Inbrasport CG-04, Inbrasport, Brazil) following a ramp protocol that was tailored to each individual's clinical history, body habitus and exercise habits to achieve volitional exhaustion between 8 and 12 min.[19],[20] All CPXs were performed under direct medical supervision in a properly equipped laboratory.[21] Subject seat height, body position and leg extension were carefully adjusted on the cycle ergometer to provide a standardized, natural and comfortable cycling movement.
One lead CM5 or CC5 digital ECG continuous monitoring (ErgoPC Elite, Micromed, Brazil) was obtained at rest, during exercise and throughout the 5-min recovery period. Resting, exercise and post exercise measurements of heart rate (HR) and blood pressure were obtained during each minute, respectively, from ECG recordings and by auscultation of the right brachial artery.
During CPX, subjects wore a nose clip and breathed through a mouthpiece with an embedded Prevent pneumotachograph (MedGraphics, United States) to provide respiratory measurements. Ventilatory gases were analyzed with a VO2000 Medgraphics metabolic cart (MedGraphics, United States) that was calibrated prior to each study. Throughout the CPX, expired gases were initially averaged at 10 s intervals and later consolidated minute-by-minute for further analysis. VO2max was signified by the highest oxygen uptake value attained, expressed as mL·(kg·min)−1.
CPX was defined as maximal if it was terminated due to fatigue, despite strong verbal encouragement, rather than having been prematurely stopped due to abnormal signs or symptoms, or by having fulfilled selected physiological criteria,[22] such as a peak respiratory exchange ratio (RER) ≥ 1.05 and/or exceeding the ventilatory threshold.[23] Additionally, measures of perceived exertion were obtained to assess somatic exhaustion, including a 10-score on the 0–10 Borg scale,[24] which was further substantiated by the inability to maintain the required pedal cadence (65–75 rev/min).
2.4. Predicted VO2max and HR
To better characterize the study's sample, VO2max values were predicted by sex-specific equations: 60 − 0.55 × age (years) for men and 48 − 0.37 × age (years) for women.[25] Maximum values of HR were age-predicted by a previously validated equation derived from a similar population, where HRmax (beats/min) = 208 − 0.7 × age (years).[26]
2.5. Estimated VO2max
VO2max [mL·(kg·min)−1] was estimated by sex-specific equations that were previously validated in our exercise lab.[17] For men and women, VO2max was estimated as [maximal workload (watts)/weight (kg)] ×10.79 + 7 and [maximal workload (watts)/weight (kg)] ×9.82 + 7, respectively.
2.6. Comparing measured and estimated VO2max
To compare measured versus estimated VO2max values, adults were categorized by both sex and age as: younger (18 to 35 years), middle-aged (36 to 60 years) and older (> 60 years). VO2max per kilogram of body weight, EE (measured VO2max − estimated VO2max) in mL·(kg·min)−1 and percent error (%E) − [(measured VO2max − estimated VO2max)/measured VO2max] × 100 − were calculated. Negative values of EE and %E signified that estimated VO2max was higher than directly measured VO2max.
2.7. Data analysis
Descriptive statistics were expressed as mean ± SD or as percent. Results for demographic and CPX variables as well as EE and %E were compared by one-way ANOVA-Bonferroni test (three age-groups), t-test (male and female subjects) or chi-square test depending of the nature of variable distribution. Pearson product-moment correlation coefficients were also calculated for measured and estimated VO2max in men and women. Statistical analysis employed Prism software 6.02 (GraphPad, USA), having < 5% probability as the criterion for statistical significance.
3. Results
A total of 1850 subjects, including 1262 men and 588 women, were studied. Our subjects ranged in age from 18 to 91 years, and men and women averaged 53 ± 15 and 50 ± 15 years (P < 0.01), respectively. Using BMI criteria, 41.1% of the subjects were overweight (BMI 25.0−29.9 kg/m2) and 23.5% were classified as obese (BMI ≥ 30.0 kg/m2). Accordingly, 27.2% of the men and 22.1% of the women were obese, whereas 1.6% and 1.2% of all men and women, respectively, were morbidly obese (BMI ≥ 40.0 kg/m2). In men, all three age-groups had similar BMIs (P > 0.05), whereas in women BMI was higher in older subjects (P < 0.05). Major demographic characteristics and selected CPX results are shown in Tables 1 and 2. Associated clinical conditions and regularly prescribed medications for men and women are depicted in Tables 3 and 4.
Table 1. Major demographics and CPX results according to age-groups - men (n = 1262).
| Age groups | Younger (n = 155) | Middle-aged (n = 683) | Older (n = 424) | P |
| Characteristics | ||||
| Age (yrs) | 29 ± 5 | 49 ± 7 | 69 ± 7 | < 0.01 |
| Weight (kg) | 86.1 ± 16.6 | 88.3 ± 15.0 | 82.2 ± 13.6 | < 0.01 |
| Height (cm) | 177.2 ± 6.5 | 176.9 ± 6.2 | 171.9 ± 6.9 | < 0.01* |
| BMI (kg/m2) | 27.4 ± 5.0 | 28.2 ± 4.3 | 27.8 ± 3.9 | > 0.05 |
| Predicted VO2max [mL·(kg·min)−1] | 44.1 ± 2.6 | 33.2 ± 4.0 | 21.8 ± 3.7 | < 0.01 |
| Predicted HRmax (bpm) | 188 ± 3 | 174 ± 5 | 159 ± 5 | < 0.01 |
| β -blocker usage (%) | 6.5 | 21.2 | 41.3 | |
| CPX Results | ||||
| Duration (min) | 10 ± 2 | 10 ± 2 | 9 ± 3 | < 0.01# |
| HRmax (bpm) | 184 ± 11 | 166 ± 18 | 135 ± 24 | < 0.01 |
| HRmax measured/predicted (%) | 98.0 ± 6.0 | 95.3 ± 9.5 | 84.9 ± 14.0 | < 0.05 |
| Maximum workload (Watts) | 229 ± 57 | 199 ± 5.9 | 110 ± 43 | < 0.01 |
| Maximum RER | 1.14 ± 0.10 | 1.14 ± 0.09 | 1.11 ± 0.13 | < 0.01* |
| Measured VO2max [mL·(kg·min)−1] | 38.3 ± 9.5 | 32.5 ± 9.2 | 21.4 ± 7.0 | < 0.01 |
| Measured/predicted VO2max (%) ) | 86.9 ± 21.9 | 98.1 ± 26.1 | 98.5 ± 28.7 | < 0.01€ |
| Estimated VO2max [mL·(kg·min)−1] | 36.4 ± 8.2 | 28.4 ± 7.2 | 21.6 ± 5.7 | < 0.01 |
| Error of estimate [mL·(kg·min)−1] | 1.9 ± 4.1 | 0.6 ± 3.1 | -0.2 ± 2.7 | < 0.01 |
| Percent error (%E) | 3.8 ± 10.5 | 0.4 ± 10.3 | -4.2 ± 16.6 | < 0.01 |
*non significant when comparing Younger and Middle-aged groups; #significant when comparing Middle-aged and Older groups; €non significant when comparing Middle-aged and Older groups. BMI: Body Mass Index; CPX: cardiopulmonary exercise testing; HR: heart rate; RER: respiratory exchange ratio.
Table 2. Major demographics and CPX results according to age-groups – women (n = 588).
| Age groups | Younger (n = 101) | Middle-aged (n = 338) | Older (n = 149) | P |
| Characteristics | ||||
| Age (yrs) | 28 ± 5 | 48 ± 7 | 70 ± 7 | < 0.01 |
| Weight (kg) | 63.5 ± 12.8 | 66.7 ± 12.2 | 69.6 ± 12.8 | < 0.05* |
| Height (cm) | 164.0 ± 5.6 | 163.7 ± 6.2 | 158.9 ± 5.9 | < 0.01* |
| BMI (kg/m2) | 23.5 ± 4.4 | 24.9 ± 4.5 | 27.6 ± 5.0 | < 0.05 |
| Predicted VO2max [mL·(kg·min)−1] | 38.2 ± 3.2 | 30.4 ± 2.8 | 22.1 ± 2.8 | < 0.01 |
| Predicted HRmax (bpm) | 188 ± 4 | 174 ± 5 | 159 ± 5 | < 0.01 |
| β -blocker usage (%) | 4.0 | 42.6 | 33.6 | |
| CPX Results | ||||
| Duration (min) | 9 ± 2 | 10 ± 3 | 7 ± 2 | < 0.01* |
| HRmax (bpm) | 184 ± 10 | 166 ± 17 | 137 ± 24 | < 0.01 |
| HRmax measured/predicted (%) | 97.6 ± 4.9 | 95.0 ± 9.3 | 86.1 ± 13.7 | < 0.01* |
| Maximum workload (Watts) | 136 ± 34 | 123 ± 42 | 67 ± 22 | < 0.01 |
| Maximum RER | 1.15 ± 0.08 | 1.15 ± 0.12 | 1.15 ± 0.11 | > 0.05 |
| Measured VO2max [mL·(kg·min)−1) | 29.9 ± 7.3 | 26.2 ± 8.4 | 15.8 ± 4.5 | < 0.01 |
| Measured/predicted VO2max (%) | 78.7 ± 20.6 | 86.4 ± 26.5 | 71.5 ± 17.8 | < 0.05¢ |
| Estimated VO2max [mL·(kg·min)−1] | 28.6 ± 5.9 | 25.6 ± 6.8 | 16.6 ± 3.2 | < 0.01 |
| Error of estimate (EE) [mL·(kg·min)−1] | 1.2 ± 3.1 | 0.7 ± 2.8 | −0.8 ± 2.3 | < 0.01* |
| Percent error (%E) | 2.7 ± 10.0 | 0.5 ± 11.1 | −9.5 ± 22.4 | < 0.01* |
Data are expressed as mean ± SD. *non significant when comparing Younger and Middle-aged groups; ¢non significant when comparing Younger and Older groups. BMI: Body Mass Index; CPX: cardiopulmonary exercise testing; HR: heart rate; RER: respiratory exchange ratio.
Table 3. Major clinical conditions and prescribed medications - men (n = 1262).
| Age Groups | Younger (n = 155) | Middle-aged (n = 683) | Older (n = 424) |
| Major clinical conditions (%) | |||
| Coronary artery disease | 1.9 | 14.3 | 40.1 |
| Acute myocardial infartion | 1.3 | 7.8 | 18.4 |
| Percutaneous coronary intervention | 1.3 | 10.1 | 23.8 |
| Coronary artery bypass graft | 0.0 | 4.1 | 17.0 |
| Hypertension | 7.7 | 30.5 | 55.4 |
| Dyslipidemia | 12.3 | 38.7 | 56.1 |
| Obesity | 12.3 | 17.6 | 17.2 |
| Diabetes | 0.6 | 7.5 | 17.0 |
| Medication use (%) | |||
| β-blockers | 6.5 | 21.2 | 41.3 |
| Calcium channel blocker | 1.9 | 6.4 | 16.7 |
| Angiotensin-converting enzyme inhibitor | 3.9 | 8.5 | 16.0 |
| Angiotensin receptor antagonist | 5.8 | 26.1 | 42.0 |
| Diuretic | 3.9 | 10.0 | 29.5 |
| Vasodilator | 0.6 | 3.8 | 14.2 |
| Cholesterol lowering | 6.5 | 39.5 | 67.9 |
| Antiplatelet | 3.2 | 23.7 | 59.2 |
| Antiarrhythmic | 0.6 | 3.5 | 15.6 |
Table 4. Major clinical conditions and prescribed medications – women (n = 588).
| Age Groups | Younger | Middle-aged | Older |
| (n = 101) | (n = 338) | (n = 149) | |
| Major clinical conditions (%) | |||
| Coronary artery disease | 0.0 | 4.1 | 18.1 |
| Acute myocardial infartion | 0.0 | 3.0 | 6.0 |
| Percutaneous coronary intervention | 0.0 | 3.6 | 8.1 |
| Coronary artery bypass graft | 0.0 | 0.6 | 6.0 |
| Hypertension | 5.0 | 15.7 | 44.3 |
| Dyslipidemia | 4.0 | 22.5 | 46.3 |
| Obesity | 4.0 | 9.5 | 19.5 |
| Diabetes | 0.0 | 3.6 | 12.1 |
| Medications in use (%) | |||
| Β-blockers | 4.0 | 13.0 | 33.6 |
| Calcium channel blocker | 2.0 | 2.7 | 18.8 |
| Angiotensin-converting enzyme inhibitor | 1.0 | 2.1 | 8.1 |
| Angiotensin receptor antagonist | 3.0 | 13.6 | 50.3 |
| Diuretic | 4.0 | 5.3 | 34.2 |
| Vasodilator | 0.0 | 0.6 | 8.7 |
| Cholesterol lowering | 0.0 | 19.8 | 61.7 |
| Antiplatelet | 0.0 | 8.3 | 40.3 |
| Antiarrhythmic | 0.0 | 5.0 | 14.8 |
The duration of CPX averaged 10 ± 2 min with 70.1% of all tests lasting between 8 and 12 min. Maximal attained workload averaged 173 ± 71 and 111 ± 45 watts, respectively, in men and women (P < 0.01), with the sex-differences persisting when values were expressed relative to body weight ― 2.04 ± 0.86 watts/kg for men and 1.71 ± 0.75 watts/kg for women (P < 0.01). Directly measured VO2max values of men and women were 29.5 ± 10.5 mL·(kg·min)−1 and 24.2 ± 9.0 mL·(kg·min)−1 (P < 0.01), ranging from 5.8 to 73.3 mL·(kg·min)−1 in men and from 4.1 to 60.1 mL·(kg·min)−1 in women. When related to age-predicted values, men achieved higher values (96.9% ± 26.8%) of VO2max as compared with women (81.3% ± 24.5%) (P < 0.01). Younger men achieved the lowest value (86.9% ± 21.9%, P < 0.01) with middle-aged and older men attaining similar relative values ― 98.1% ± 26.1% and 98.5% ± 28.7%, respectively (P > 0.05). Different results were observed in women; the middle-aged cohort achieved the highest values of percent of age-predicted VO2max (86.4% ± 26.5%; P < 0.05) whereas younger and older women demonstrated similar values, 78.7% ± 20.6 and 71.5% ± 17.8% (P > 0.05), respectively.
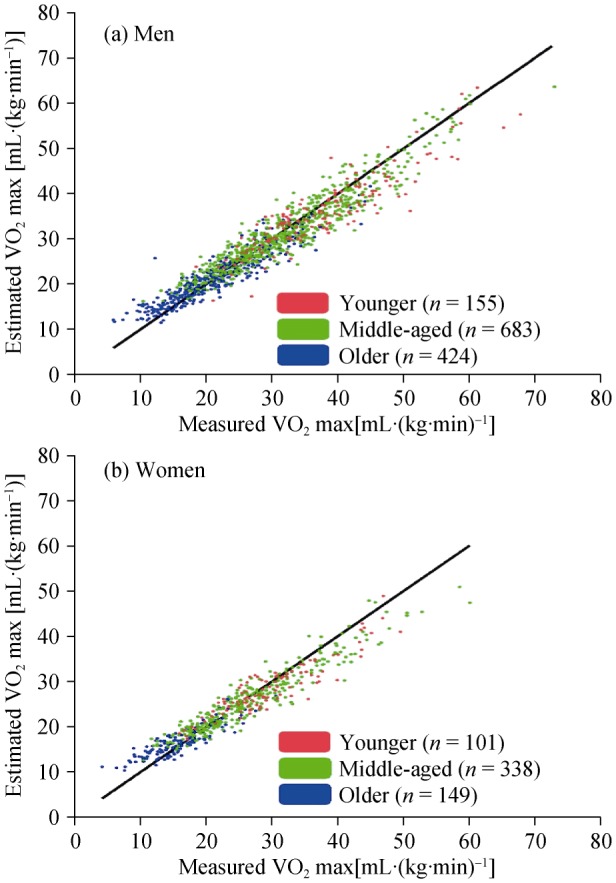
Relative to the EE and %E of VO2max, men and women had similar values, 0.5 ± 3.2 mL·(kg·min)−1 and 0.4 ± 2.9 mL·(kg·min)−1 (P > 0.05) and −0.8 ± 13.1% and −1.7 ± 15.4% (P > 0.05), respectively. In reference to the age-groups for both men and women, VO2max was similarly underestimated in the younger age-groups ― %E 3.8 ± 10.5% and 2.7 ± 10.0% (P > 0.05), and generally overestimated in the older male and female subjects, −4.2 ± 16.6% and −9.5 ± 22.4% (P < 0.01). Men and women had similar results for EE in the middle-aged group, 0.6 ± 3.1 mL·(kg·min)−1 and 0.7 ± 2.8 mL·(kg·min)−1 (P > 0.05) and for %E, 0.4 ± 10.3% and 0.5 ± 11.1% (P > 0.05) (Figure 1).
Figure 1. Relationship between measured and estimated VO2max in three age-groups (younger, middle-aged, older) in men (a) and women (b).
4. Discussion
Although the use of CPX has increased in recent years, for the vast majority of exercise testing labs VO2max is still indirectly estimated by applying equations that rely on the workloads achieved, and their duration.[27] In our study, by using specific equations for our population of men and women, VO2max was consistently overestimated in older subjects and underestimated in the younger cohort, with the largest %E observed in the former.
There are some plausible physiologic mechanisms to explain our findings. One possibility is related to net VO2, that is, the oxygen uptake associated with a given exercise bout.[28] Because the percentage of type I fibers influences mechanical efficiency during cycling, changes in fiber type may alter the linear relationship between workload and oxygen consumption.[29] According to Tevald, et al.[30] and Venturelli, et al.,[31] the loss of muscle fibers with aging is fiber specific, occurring primarily with type II fibers or fast-twitch fibers, with an increase in percentage of type I fibers, or slow-twitch fibers, contributing to differences in mechanical efficiency seen between younger and older subjects.
In addition, equations commonly used to estimate VO2max often employ the added constant value of 7 mL·(kg·min)−1 to represent the oxygen consumption at rest [3.5 mL·(kg·min)−1] plus the energy cost of unloaded pedaling [also 3.5 mL·(kg·min)−1]. However, in one study, values of oxygen consumption at rest between 2.0 and 4.4 mL·(kg·min)−1 were reported in 125 healthy men aged 17 to 38 years.[32] Kwan, et al.[33] found that resting VO2 was significantly lower in elderly people, suggesting that the conventional value of 3.5 mL·(kg·min)−1 probably overestimates their energy expenditure at rest. In accordance with this latter study, a recent review of 397 reports noted that the resting value of VO2 decreased with age in both sexes, leading to its systematic overestimation in older subjects.[34] Therefore, it is possible that differences in resting VO2 may have contributed to the increasing EE of VO2max seen in our study comparing three progressive age groups.
Likewise, the value of oxygen consumption of unloaded pedaling used in our sex-specific equations was derived from a study of 60 healthy men aged 19 to 39 years.[14] With respect to net VO2, it is also possible that the oxygen consumption for pedaling an unloaded cycle ergometer is age dependent and, therefore, influences the EE of VO2max mostly in older subjects. Thus, routinely using a constant added value of 7 mL·(kg·min)−1 to our prediction equations may have influenced our observed EE for VO2max.
Because this was a retrospective study, we were not able to assess values of resting VO2 nor VO2 for pedaling an unloaded cycle ergometer, as these measurements are not routinely obtained in our lab or others. Moreover, there remain controversies regarding the accurate assessment of resting VO2, making it difficult to incorporate this variable when equations to estimate VO2max are used in clinical practice.[28]
Our study has some methodological limitations. First, we did not evaluate the previous or current history of physical activity, exercise and sports practice of our subjects. Admittedly, regular physical activity can alter skeletal muscle fiber typing, thus influencing our subject's mechanical efficiency, regardless of age. As previously reported, older individuals (mean age, 62 years) that participated in a supervised exercise program showed greater improvement in functional capacity, as measured by the workload (watts)/weight (kg) ratio, than in VO2max, suggesting that regular exercise may improve mechanical efficiency.[35] Moreover, it remains unclear whether some co-morbid conditions, such as cardiovascular diseases, and commonly prescribed medications, including statins, can influence mechanical efficiency.[36],[37] Accordingly, future studies are needed to address these potential confounding variables.
In conclusion, the magnitude of EE of VO2max is directly influenced by age in both men and women. The EE is probably related to age-related differences in mechanical efficiency, oxygen cost of unloaded cycling, basal metabolic rate, or combinations thereof. Thus, estimating VO2max simply based on the peak workload achieved during CPX may lead to larger errors in older subjects.
Acknowledgments
Partial financial support for this study was provided by CNPq and FAPERJ.
References
- 1.Araújo CG, Herdy AH, Stein R. Maximum oxygen consumption measurement: valuable biological marker in health and in sickness. Arq Bras Cardiol. 2013;100:51–53. [PubMed] [Google Scholar]
- 2.Taylor HL, Buskirk E, Henschel A. Maximal oxygen intake as an objective measure of cardio-respiratory performance. J Appl Physiol. 1995;8:73–80. doi: 10.1152/jappl.1955.8.1.73. [DOI] [PubMed] [Google Scholar]
- 3.Hawkins MN, Raven PB, Snell PG, et al. Maximal oxygen uptake as a parametric measure of cardiorespiratory capacity. Med Sci Sports Exerc. 2007;39:103. doi: 10.1249/01.mss.0000241641.75101.64. [DOI] [PubMed] [Google Scholar]
- 4.Bruce RA, Hornsten TR. Exercise stress testing in evaluation of patients with ischemic heart disease. Prog Cardiovasc Dis. 1969;11:371–390. doi: 10.1016/0033-0620(69)90027-9. [DOI] [PubMed] [Google Scholar]
- 5.Bhatia LC, Singal R, Jain P, et al. Detection of silent myocardial ischaemia in asymptomatic diabetic patients during treadmill exercise testing. High Blood Press Cardiovasc Prev. 2012;19:137–142. doi: 10.1007/BF03262463. [DOI] [PubMed] [Google Scholar]
- 6.Barry VW, Baruth M, Beets MW, et al. Fitness vs. fatness on all-cause mortality: a meta-analysis. Prog Cardiovasc Dis. 2014;56:382–390. doi: 10.1016/j.pcad.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 7.Kavanagh T, Mertens DJ, Hamm LF, et al. Prediction of long-term prognosis in 12 169 men referred for cardiac rehabilitation. Circulation. 2002;106:666–671. doi: 10.1161/01.cir.0000024413.15949.ed. [DOI] [PubMed] [Google Scholar]
- 8.Kavanagh T, Mertens DJ, Hamm LF, et al. Peak oxygen intake and cardiac mortality in women referred for cardiac rehabilitation. J Am Coll Cardiol. 2003;42:2139–2143. doi: 10.1016/j.jacc.2003.07.028. [DOI] [PubMed] [Google Scholar]
- 9.Kodama S, Saito K, Tanaka S, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301:2024–2035. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- 10.Myers J, Prakash M, Froelicher V, et al. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801. doi: 10.1056/NEJMoa011858. [DOI] [PubMed] [Google Scholar]
- 11.Balady GJ, Arena R, Sietsema K, et al. Clinician's guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation. 2010;122:191–225. doi: 10.1161/CIR.0b013e3181e52e69. [DOI] [PubMed] [Google Scholar]
- 12.Bruce RA, Kusumi F, Hosmer D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am Heart J. 1973;85:546–562. doi: 10.1016/0002-8703(73)90502-4. [DOI] [PubMed] [Google Scholar]
- 13.Whipp BJ, Wasserman K. Efficiency of muscular work. J Appl Physiol. 1969;26:644–648. doi: 10.1152/jappl.1969.26.5.644. [DOI] [PubMed] [Google Scholar]
- 14.Lang PB, Latin RW, Berg KE, et al. The accuracy of the ACSM cycle ergometry equation. Med Sci Sports Exerc. 1992;24:272–276. [PubMed] [Google Scholar]
- 15.Latin RW, Berg KE. The accuracy of the ACSM and a new cycle ergometry equation for young women. Med Sci Sports Exerc. 1994;26:642–646. [PubMed] [Google Scholar]
- 16.Londeree BR, Moffitt-Gerstenberger J, Padfield JA, et al. Oxygen consumption of cycle ergometry is nonlinearly related to work rate and pedal rate. Med Sci Sports Exerc. 1997;29:775–780. doi: 10.1097/00005768-199706000-00007. [DOI] [PubMed] [Google Scholar]
- 17.de Souza e Silva CG, Araújo CGS. Sex-specific equations to estimate maximum oxygen uptake in cycle ergometry. Arq Bras Cardiol. 2015;105:381–389. doi: 10.5935/abc.20150089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ferrucci L, Giallauria F, Guralnik JM. Epidemiology of aging. Radiol Clin North Am. 2008;46:643–652. doi: 10.1016/j.rcl.2008.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buchfuhrer MJ, Hansen JE, Robinson TE, et al. Optimizing the exercise protocol for cardiopulmonary assessment. J Appl Physiol Respir Environ Exerc Physiol. 1983;55:1558–1564. doi: 10.1152/jappl.1983.55.5.1558. [DOI] [PubMed] [Google Scholar]
- 20.Myers J, Buchanan N, Walsh D, et al. Comparison of the ramp versus standard exercise protocols. J Am Coll Cardiol. 1991;17:1334–1342. doi: 10.1016/s0735-1097(10)80144-5. [DOI] [PubMed] [Google Scholar]
- 21.Sociedade Brasileira de Cardiologia III Guidelines of Sociedade Brasileira de Cardiologia on the exercise test. Arq Bras Cardiol. 2010;95:1–26. doi: 10.1590/S0066-782X2010000800001. [DOI] [PubMed] [Google Scholar]
- 22.Ramos PS, Sardinha A, Nardi AE, et al. Cardiorespiratory optimal point: a submaximal exercise variable to assess panic disorder patients. PLoS One. 2014;9:e104932. doi: 10.1371/journal.pone.0104932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Howley ET, Bassett DR, Welch HG. Criteria for maximal oxygen uptake: review and commentary. Med Sci Sports Exerc. 1995;27:1292–1301. [PubMed] [Google Scholar]
- 24.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–381. [PubMed] [Google Scholar]
- 25.Jones NL, Campbell EKM, Edwards RHT, et al. Clinical Exercise Testing. Philadelphia, USA: WB Saunders; 1995. p. 202. [Google Scholar]
- 26.Duarte CV, Araujo CG. Cardiac vagal index does not explain age-independent maximal heart rate. Int J Sports Med. 2013;34:502–506. doi: 10.1055/s-0032-1323818. [DOI] [PubMed] [Google Scholar]
- 27.Arena R, Sietsema KE. Cardiopulmonary exercise testing in the clinical evaluation of patients with heart and lung disease. Circulation. 2011;123:668–680. doi: 10.1161/CIRCULATIONAHA.109.914788. [DOI] [PubMed] [Google Scholar]
- 28.Cunha FA, Midgley AW, Monteiro W, et al. How long does it take to achieve steady state for an accurate assessment of resting VO2 in healthy men? Eur J Appl Physiol. 2013;113:1441–1447. doi: 10.1007/s00421-012-2571-x. [DOI] [PubMed] [Google Scholar]
- 29.Coyle EF, Sidossis LS, Horowitz JF, et al. Cycling efficiency is related to the percentage of type I muscle fibers. Med Sci Sports Exerc. 1992;24:782–788. [PubMed] [Google Scholar]
- 30.Tevald MA, Foulis SA, Lanza IR, et al. Lower energy cost of skeletal muscle contractions in older humans. Am J Physiol Regul Integr Comp Physiol. 2010;298:729–739. doi: 10.1152/ajpregu.00713.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Venturelli M, Schena F, Scarsini R, et al. Limitations to exercise in female centenarians: evidence that muscular efficiency tempers the impact of failing lungs. Age. 2013;35:861–870. doi: 10.1007/s11357-011-9379-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cunha FA, Midgley AW, Montenegro R, et al. Metabolic equivalent concept in apparently healthy men: a re-examination of the standard oxygen uptake value of 3.5 mL·kg(-1)· min(-1) Appl Physiol Nutr Metab. 2013;38:1115–1119. doi: 10.1139/apnm-2012-0492. [DOI] [PubMed] [Google Scholar]
- 33.Kwan M, Woo J, Kwok T. The standard oxygen consumption value equivalent to one metabolic equivalent (3.5 mL/min/kg) is not appropriate for elderly people. Int J Food Sci Nutr. 2004;55:179–182. doi: 10.1080/09637480410001725201. [DOI] [PubMed] [Google Scholar]
- 34.McMurray RG, Soares J, Caspersen CJ, et al. Examining variations of resting metabolic rate of adults: a public health perspective. Med Sci Sports Exerc. 2014;46:1352–1358. doi: 10.1249/MSS.0000000000000232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Signorelli GR, Duarte CV, Ramos PS, et al. Improvement in functional capacity exceeds that of aerobic fitness: data from 144 patients in an exercise program. Rev Bras Cardiol. 2012;25:299–308. [Google Scholar]
- 36.Gosker HR, Wouters EF, van der Vusse GJ, et al. Skeletal muscle dysfunction in chronic obstructive pulmonary disease and chronic heart failure: underlying mechanisms and therapy perspectives. Am J Clin Nutr. 2000;71:1033–1047. doi: 10.1093/ajcn/71.5.1033. [DOI] [PubMed] [Google Scholar]
- 37.Mikus CR, Boyle LJ, Borengasser SJ, et al. Simvastatin impairs exercise training adaptations. J Am Coll Cardiol. 2013;62:709–714. doi: 10.1016/j.jacc.2013.02.074. [DOI] [PMC free article] [PubMed] [Google Scholar]


