Abstract
The purpose of this study was to identify fecal bacterial microbiome changes in patients with chronic human immunodeficiency virus (HIV) infection in China. Bacterial 16S rRNA genes were amplified, sequenced (454 pyrosequencing), and clustered into operational taxonomic units using the QIIME software. Relative abundance at the phylum and genus levels were calculated. Alpha diversity was determined by Chao 1 and observed-species indices, and beta diversity was determined by double principal component analysis using the estimated phylogeny-based unweighted Unifrac distance matrices. Fecal samples of the patients with chronic HIV-infection tended to be enriched with bacteria of the phyla Firmicutes (47.20%±0.43 relative abundance) and Proteobacteria (37.21%±0.36) compared with those of the non-HIV infected controls (17.95%±0.06 and 3.81%±0.02, respectively). Members of the genus Bilophila were exclusively detected in samples of the non-HIV infected controls. Bacteroides and arabacteroides were more abundant in the chronic HIV-infected patients. Our study indicated that chronic HIV-infected patients in China have a fecal bacterial microbiome composition that is largely different from that found in non-HIV infected controls, and further study is needed to evaluate whether microbiome changes play a role in disease complications in the distal gut, including opportunistic infections.
Keywords: antiretroviral treatment, feces, HIV, microbiome, 16S rRNA
INTRODUCTION
The human gut is home to a complex microbial ecosystem or microbiome that is composed of thousands of species. The total bacterial population in the gut exceeds 1 × 1014 cells, which is approximately ten times greater than the number of human cells.1 This large and diverse community of bacteria is known to play key roles in modulating host metabolism and immunity.2 To better understand the role of these microbes in the human body and to determine the potential effects of fecal bacterial microbiome composition on disease susceptibility, extensive microbial diversity surveys have been conducted.3 With the recent development of next-generation sequencing methods, these surveys have revealed a number of global patterns of bacterial diversity in human intestinal ecosystems.4
The composition of the fecal microbial microbiome is unique for each individual, depending, to some extent, on the environment and diet of the host. Although this ecosystem can evolve, a stable balance must be maintained.5 Using barcode pyrophosphate sequencing technology, Young et al.6 found that the intestinal microbiome is clearly different among the South Koreans, Americans, Chinese and Japanese; however, these individuals were all considered healthy, indicating that a stable or a balanced fecal bacterial microbiome is likely a greater indicator of intestinal health than the actual composition of the biome. Notably, this delicate balance of the microbiome can be disrupted in a number of situations, including illness.7 For example, in a recent high-throughput diversity and functional analysis, Zoetendal et al.8 observed that opportunistic infections may be associated with detrimental changes in the intestinal microbiome. Furthermore, through analysis of >400 species of microbes, Rajilić-Stojanović et al.9 found that the most abundant microbes present in the gut were also the most susceptible to change. In addition, various profiles have been shown to be present in the microbiome of elderly individuals with low immunity and people with chronic diseases, further highlighting a link between altered gut bacteria and health complications in the host. However, a thorough analysis of the fecal bacterial microbiome in patients with chronic human immunodeficiency virus (HIV) infection, particularly Chinese patients, has not been performed to date.
Acquired immune deficiency syndrome is a serious chronic infectious disease caused by HIV. Although the survival rate for Acquired immune deficiency syndrome/HIV patients has significantly improved since the introduction of antiretroviral therapy (ART),10, 11 persistent disease progression and clinical complications in virally suppressed individuals are suggestive of the contributions of factors other than HIV replication alone. Notably, a recent study indicated that antibacterial treatment can affect the normal fecal microbiome of chronic HIV-infected patients, which may provide an opportunity for pathogenic bacteria to multiply and trigger infection and other complications.11 Similar studies have primarily focused on patients in Europe and the United States,12, 13, 14 whereas the role of the fecal bacterial microbiome in disease progression in Chinese chronic HIV-infected patients is largely undocumented. In recent years, we have observed an increase in the number of patients living with HIV in the Shanghai Public Health Clinical Center. Many of these patients complain of abdominal discomfort, intermittent diarrhea and even persistent diarrhea after ART, which are complications that tend to occur repeatedly and do not appear to have a common cause. We suspect that these abdominal issues are related to changes in the intestinal microbiome of chronic HIV-infected patients. To test this hypothesis, we employed 454 pyrosequencing and the QIIME pipeline to explore microbial diversity in chronic HIV-infected patients and non-HIV infected controls and to determine the possible role of the gut ecosystem in the global health of the host during ART.
MATERIALS AND METHODS
Subjects and sample collection
In this study, we enrolled 13 patients with chronic HIV infection who had recently been admitted to the Shanghai Public Health Clinical Center. All patients except two received ART. Of the 13 participants, pulmonary infection was found in six; combined pulmonary infection, CMV infection and non-tuberculosis mycobacteria, in one; combined pulmonary infection and non-tuberculosis mycobacteria, in one; amebiasis combined with pyogenic liver abscess, in one; lymphoma, in one; fungal infection combined with pulmonary infection, in one; combined pulmonary infection and syphilis, in one; and pyogenic liver abscess, in one (Table 1). Of these, 69.2% were male (nine subjects) and 30.8% were female (four subjects). The median age was 47 years (range: 22–72 years). The diagnosis of chronic HIV-infection was made according to known diagnostic standards.
Table 1. Demographic and clinical characteristics of the study subjects who provided fecal specimens.
| Sample ID | Gender | Age | ARTa | CD4 (cell/mm3) | Viral load (copy/mL)b | Antibiotic usec | Complicationsd | |
|---|---|---|---|---|---|---|---|---|
| Chronic HIV-infected patients (n=13) | HIV3 | M | 24 | HAART | 788 | 66100 | Yes | PLA |
| HIV4 | F | 22 | HAART | 222 | ND | Yes | PI/Syp | |
| HIV5 | M | 30 | No | 11 | ND | No | PI/ NTM | |
| HIV6 | F | 48 | No | 756 | ND | Yes | No | |
| HIV7 | M | 54 | HAART | 30 | ND | No | PI/NTM/CMVI | |
| HIV8 | M | 72 | HAART | 75 | ND | No | Lymp | |
| HIV9 | M | 47 | HAART | 26 | ND | No | PI | |
| HIV10 | M | 58 | HAART | 158 | 46400 | Yes | PLA/CDA | |
| HIV11 | M | 24 | HAART | 38 | 71 | No | PI | |
| HIV12 | F | 27 | HAART | 36 | 716 | Yes | PI/FI | |
| HIV13 | F | 34 | HAART | 414 | 731 | Yes | No | |
| HIV14 | M | 32 | HAART | 484 | 1720 | No | No | |
| HIV15 | M | 38 | HAART | 328 | 2500 | No | No | |
| NT10 | M | 46 | No | NDe | ND | No | No | |
| Non-HIV controls (n=7) | NT5 | M | 46 | No | ND | ND | No | No |
| NT7 | M | 46 | No | ND | ND | No | No | |
| NT9 | M | 46 | No | ND | ND | No | No | |
| DB3 | F | 29 | No | ND | ND | No | Diar | |
| DP3 | F | 66 | No | ND | ND | No | Diar | |
| DP4 | M | 71 | No | ND | ND | No | Diar |
antiretroviral therapy, ART; number of sequence reads, Read No.
Viral load: copy/mL.
Antibiotic use four weeks prior to fecal sampling.
pulmonary infection, PI; syphilis, Syp; pyogenic liver abscess, PLA; non-tuberculosis mycobacteria, NTM; CMV infection, CMVI; lymphoma, Lymp; clinical diagnosis of amoeba, CDA; fungal infection, FI; diarrhea, Diar.
not done, ND.
In addition, four non-HIV infected controls ranging from 29 to 71 years of age were enrolled in this study. Of these control subjects, three patients (DB3, DP3 and DP4) were suffering from diarrheal disease diagnosed at the outpatient services at Shanghai Tongji Hospital, whereas a single healthy control was referred from the Institute of Medicine Science, Shanghai Tongji Hospital. A basic outline of the patient characteristics can be found in Table 1.
One fecal sample was obtained from each subject. From the healthy subject, three additional samples were obtained (four total), one per week over the course of a month, for use as internal quality controls. All of the fecal samples were properly handled and collected in disposable plastic sterile dung cups. All samples arrived at the laboratory within 24 h and were immediately frozen at -20 °C and stored until analysis. This study was approved by the Ethics Committee of the Shanghai Public Health Clinical Center affiliated with Fudan University, China.
DNA extraction
DNA isolation with the QIAamp DNA Stool Mini Kit (Qiagen, Duesseldorf, Germany) was performed in accordance with the manufacturer's instructions (QIAamp DNA Stool Handbook 04/2010, Germany). DNA concentrations were measured at 260 nm with a NanoDrop 2000 spectrophotometer (Thermo Scientific, Waltham, MA, USA).
PCR enrichment of the V3–V4 region, pyrosequencing and statistical analysis
Details concerning the PCR methodology utilized in this study can be found in Chakravorty et al.15 Twenty pairs of barcoded primers were used for the enrichment of the bacterial 16S rRNA gene V3–V4 hypervariable regions.15, 16, 17, 18 The enriched V3–V4 regions were pooled, mixed and sequenced using the 454 FLX pyrosequencing platform (Roche 454 GS FLX, Basel, Switzerand).
Following sequencing, the reads were de-multiplexed into samples according to the barcodes using the QIIME software (Denver, CO, USA) pipeline,19 with the default parameters. Primer and barcode sequences were removed. Operational taxonomic unit clustering was performed at a 97% similarity threshold using the QIIME pipeline. The relative abundance of the taxa at the phylum and genus levels were calculated. The diversity was estimated with Chao 1 and observed-species indices calculations (alpha or within-sample diversity) and double principal component analysis (DPCoA; beta or between-sample diversity) using the phylogeny-based unweighted Unifrac distance matrices. The difference between specific taxa was analyzed using analysis of variance (ANOVA) followed by post-hoc t-tests, with Bonferroni and Benjamini-Hochberg false discovery rate (FDR) corrections for multiple testing. P<0.05 and q<0.1 were considered significant. Linear discriminant analysis effect size (LEfSe) analysis was used to identify different taxa between the cases and the controls.20
RESULTS
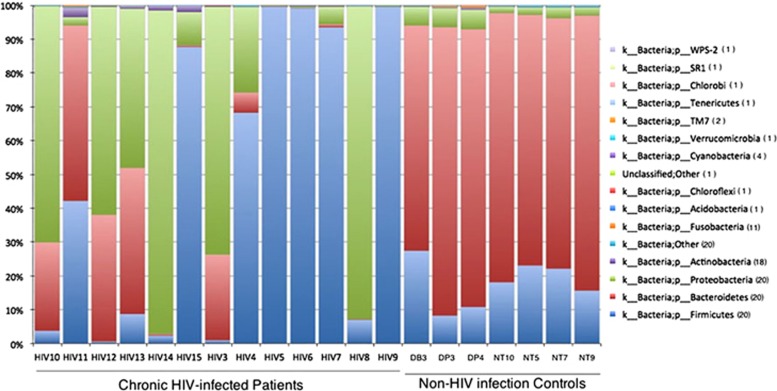
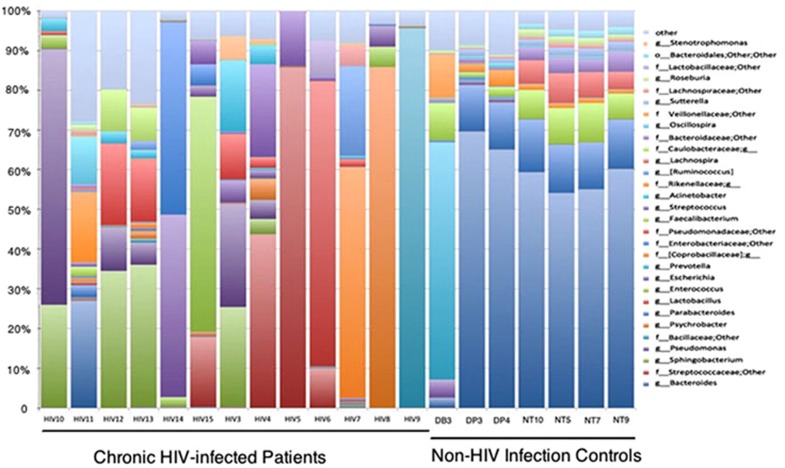
The 20 fecal samples yielded 376 627 high-quality reads. On average, each sample yielded ~18 811 sequences, ranging from 1393 to 76 583. Overall, 16 unique bacterial phyla (Figure 1) or 273 genera were identified in the 20 samples, with an average of 61 genera in each sample (Figure 2).
Figure 1.
Phylum-level taxon distribution in chronic HIV-infected patients and non-HIV infected controls. Stacked columns for each of the 20 samples from the 17 subjects enrolled in this study show the abundance of a given phylum as a percentage of the total bacterial sequences in the sample. All 16 phyla (one unclassified) with an abundance of at least 0.1% in at least one subject were included. Numbers in parentheses in the legend indicate the number of samples containing the taxon.
Figure 2.
Genus-level taxon distribution in chronic HIV-infected patients and non-HIV infected controls. Stacked columns for each of the 20 samples from the 17 subjects enrolled in this study show the abundance of a given genus as a percentage of the total bacterial sequences in the sample. All 31 genera with an abundance of at least 0.1% in at least one subject were included.
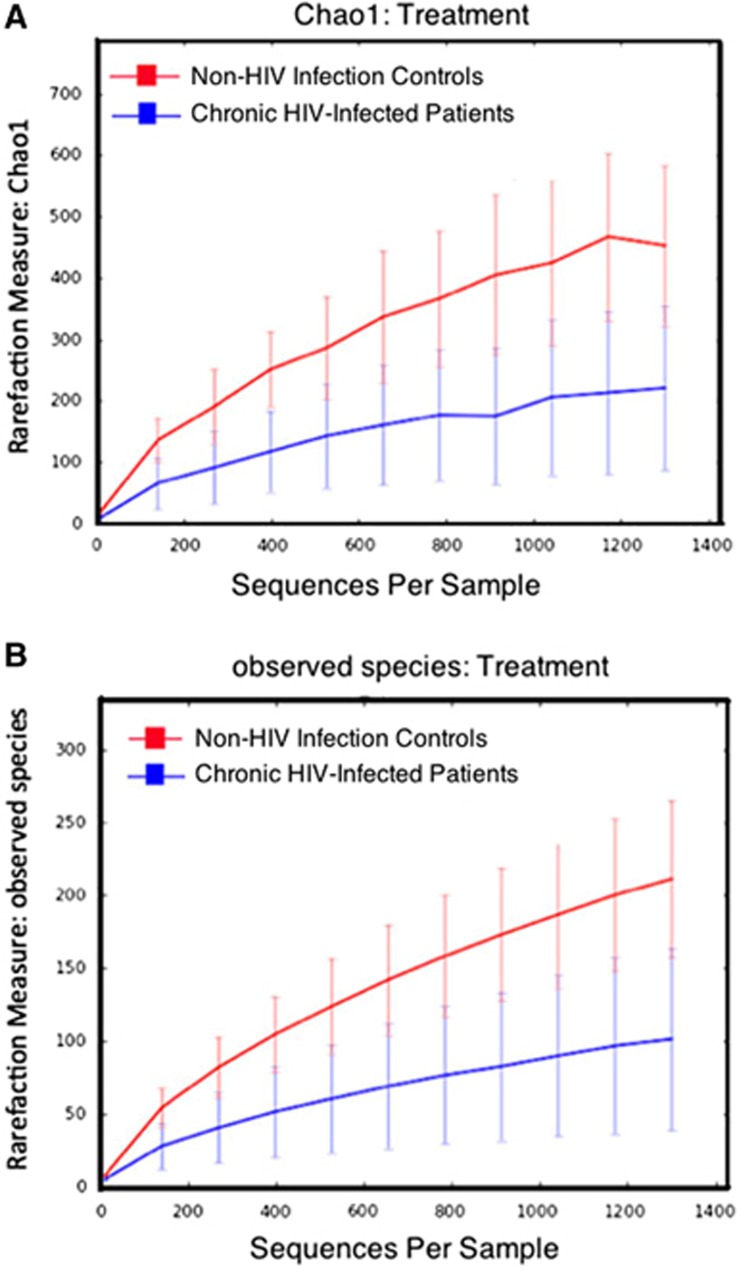
Diversity indices
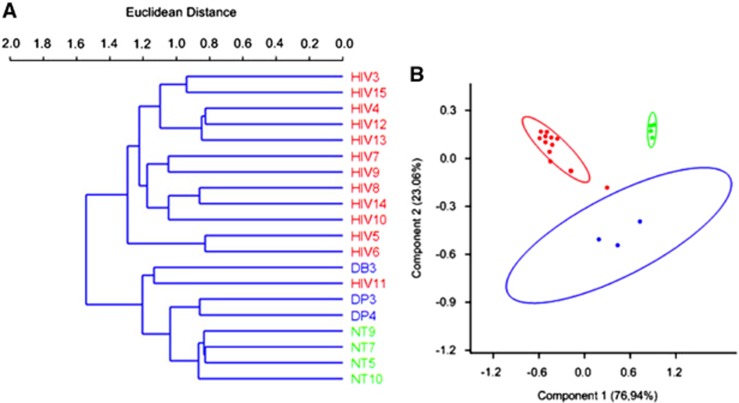
Alpha diversity was determined using Chao 1 and observed-species index calculations (Figure 3, panels A and B, respectively). These data indicated that HIV infection was associated with a decrease in microbiome diversity. Beta diversity was determined using DPCoA with the phylogeny-based unweighted Unifrac distance matrices and revealed a clear separation in bacterial community composition between the controls and the HIV-infected patients (Figure 4).
Figure 3.
Analysis of alpha diversity in chronic HIV-infected patients. Diversity indices in chronic HIV-infected patients (blue) versus non-HIV infected controls (red) predicted diversity by Chao 1 (A) and observed diversity (B).
Figure 4.
Analysis of beta diversity in chronic HIV-infected patients. Cluster dendrogram (A) illustrating the bacterial diversity of chronic HIV-infected patients (red) compared with non-HIV infected controls (blue and green). Double principal component analysis (B) of fecal microbiome composition in chronic HIV-infected patients (red) compared with non-HIV infected controls (blue for the non-HIV subjects with diarrhea and green for the healthy controls).
Difference in specific taxa between chronic HIV-infected patients and non-HIV infected controls
To examine these differences more closely, we investigated microbial distributions at the phylum and genus levels. At the phylum level, the data indicated that the chronic HIV-infected patients tended to be enriched with Firmicutes (47.20 versus 17.94% q=0.16, P=0.10) and Proteobacteria (37.21 versus 3.81% q=0.06, P=0.03) and depleted in Bacteroidetes (17.48 versus 77.58% q=9.13E-07, P=1.52E-07) (Figure 1 and Supplementary Table S1) compared with the non-HIV infected controls. The distribution of bacteria according to the genus in each sample showed that several genera were different in abundance between the two groups (Figure 2). We further investigated intergroup differences by using ANOVA and post-hoc tests, and post-hoc P-values were FDR-corrected (q-values) (Table 2). The data indicated a high level of variability between the fecal microbiome compositions of the chronic HIV-infected patients and the non-HIV infected controls at the genus level (P=0.001, R=0.7813). The control subjects appeared to have significantly higher levels of bacteria from the genera Bacteroides (52.30% versus 2.16% q=3.17E-05, P<0.0001), Parabacteroides (10.50 versus 0.25% q=2.76E-05, P<0.0001), Faecalibacterium (6.54 versus 0.19% q=5.67E-05, P<0.0001), Sutterella (1.52 versus 0.02% q=1.96E-05, P<0.0001), Phascolarctobacterium (7.96 versus 9.81E-03% q=2.40E-05, P<0.0001), Roseburia (1.17% versus 1.36E-01% q=3.90E-03, P<0.001), Lachnospira (3.57% versus 5.73E-02% q=6.76E-03, P<0.05) and unclassified Bacteroidaceae (2.37 versus 6.84E-02% q=5.66E-03, P<0.05) compared with the chronic HIV-infected patients (Table 2, Figure 5). It is also worth noting that bacteria of the genus Bilophila appeared only in the non-HIV infected controls.
Table 2. Genus-level differences between chronic HIV-infected patients and non-HIV infected controls.
| OTU | P-value | Bonferroni-corrected | FDR-corrected | Control mean | HIV+mean |
|---|---|---|---|---|---|
| Parabacteroides | 3.00E-07 | 2.76E-05 | 2.76E-05 | 1.05E-01 | 2.51E-03 |
| Bacteroides | 6.89E-07 | 6.34E-05 | 3.17E-05 | 5.23E-01 | 2.16E-02 |
| Lachnospiraceae-unclassified | 8.42E-07 | 7.74E-05 | 2.58E-05 | 6.85E-03 | 4.43E-04 |
| Sutterella | 8.52E-07 | 7.84E-05 | 1.96E-05 | 1.52E-02 | 1.61E-04 |
| Phascolarctobacterium | 1.30E-06 | 1.20E-04 | 2.40E-05 | 7.96E-02 | 9.81E-05 |
| Faecalibacterium | 3.70E-06 | 3.40E-04 | 5.67E-05 | 6.54E-02 | 1.96E-03 |
| Clostridia-unclassified | 4.57E-06 | 4.20E-04 | 6.00E-05 | 1.30E-03 | 2.00E-05 |
| Bacteroidales-unclassified | 2.77E-04 | 2.55E-02 | 3.18E-03 | 1.07E-02 | 5.21E-04 |
| Roseburia | 3.82E-04 | 3.51E-02 | 3.90E-03 | 1.17E-02 | 1.36E-03 |
| Bacteroidaceae-unclassified | 6.15E-04 | 5.66E-02 | 5.66E-03 | 2.37E-02 | 6.84E-04 |
| Lachnospira | 8.08E-04 | 7.43E-02 | 6.76E-03 | 3.57E-02 | 5.73E-04 |
| Bacteroidetes-unclassified | 2.01E-03 | 1.85E-01 | 1.54E-02 | 9.20E-05 | 9.96E-06 |
| Clostridiales-unclassified | 4.57E-03 | 4.21E-01 | 3.24E-02 | 1.52E-03 | 2.88E-04 |
| Streptococcus | 2.12 E-01 | 19.52 | 4.76 E-01 | 6.12 E-04 | 3.58 E-02 |
| Pseudomonas | 2.32 E-01 | 21.31 | 4.63 E-01 | 4.88E-06 | 8.67 E-02 |
| Sphingobacterium | 1.00 E-01 | 9.26 | 4.20 E-01 | 4.48E-05 | 9.69 E-02 |
| Bilophila | 7.13E-03 | 6.56E-01 | 4.69E-02 | 2.78E-03 | 0 |
Abbreviation: OTU, Operational taxonomic unit.
The taxonomic classification (genus level) and taxa abundance matrix were analyzed with the QIIME pipeline. Differences between the two experimental groups were analyzed by ANOVA followed by post-hoc tests with Bonferroni correction and FDR correction (q-values). P<0.05 and q<0.1 were considered significant.
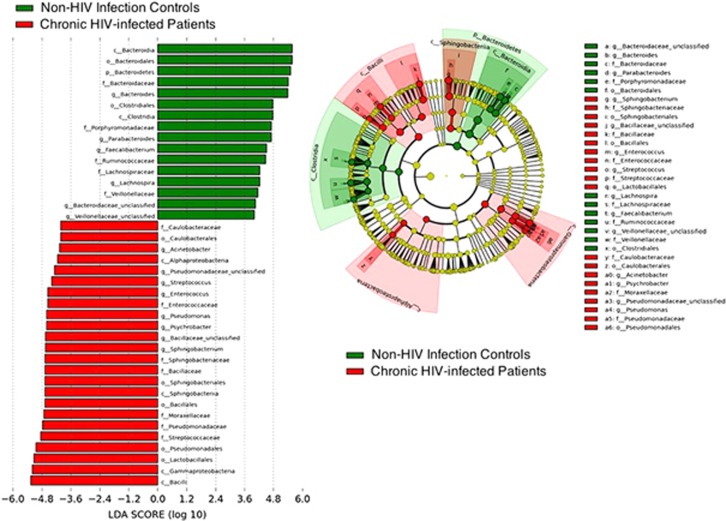
Figure 5.
Differential representation of bacterial lineages by LEfSe between chronic HIV-infected patients and controls. Histograms of enriched bacterial taxa in HIV-infected patients are displayed in red, and in controls, in green.
These findings are shown in the LEfSe analysis (Figure 5). Taken together, these results imply that an entirely different bacterial ecosystem is present in the feces of chronic HIV-infected patients compared with non-HIV infected controls with gastrointestinal illnesses and healthy individuals (Supplementary Table S2).
DISCUSSION
To elucidate the potential role of the fecal microbiome in HIV disease progression, we compared the fecal bacterial microbiome of chronic HIV-infected patients with that of non-HIV infected controls. We found that chronic HIV-infected patients tended to be enriched with bacteria of the phyla Firmicutes and Proteobacteria. Our observations are consistent with those of a recent meta-analysis showing that the phylum Proteobacteria is highly abundant in the intestinal lumen of patients suffering from chronic HIV infection.21
The observed phylum level changes can be traced to lower ranked taxa. Within Firmicutes, a phylum dominated by Gram-positive bacteria, the changes in relative abundance were most prominent for the genera Phascolarctobacterium, Faecalibacterium, Roseburia and Lachnospira, as well as for taxa within the Veillonellaceae, Ruminococcaceae and Lachnospiraceae families in the order Clostridiales, class Clostridia. Within the Proteobacteria, a phylum of Gram-negative bacteria, the difference in relative abundance between the chronic HIV-infected patients and the non-HIV infected controls was most prominent for the genera Bilophila and Sutterella, which belong to the class Betaproteobacteria, as well as for others from the class Deltaproteobacteria, including taxa in the Alcaligenaceae and Desulfovibrionaceae families in the orders Burkholderiales and Desulfovibrionales, respectively.
In addition to the bacterial enrichment observed in the chronic HIV-infected patients, several bacterial taxa were depleted in the HIV-infected patients compared with the controls. For example, the control subjects appeared to have higher levels of bacteria of the Bacteroidetes (77.58% relative abundance) than the chronic HIV-infected patients (14.78%). Within this phylum, the change in relative abundance was most prominent for the genera Parabacteroides, Bacteroides and others belonging to the class Bacteroidia, including taxa in Porphyromonadaceae, Bacteroidaceae and others in the order Bacteroidales.
We are not the first to consider the relationship between HIV infection and the fecal bacterial microbiome. A recent report by Dinh et al.,21 which compared the fecal microbial community composition of patients suffering from HIV with that of healthy controls, presented results that are somewhat different from ours. In that study, the relative abundances of Proteobacteria, Gammaproteobacteria, Enterobacteriales, Enterobacteriaceae, Erysipelotrichi, Erysipelotrichales, Erysipelotrichaceae and Barnesiella were significantly higher in HIV patients, whereas those of Rikenellaceae and Alistipes were lower. The lack of corroboration between this prior study and the current study is surprising as similar methodologies with regard to subject enrollment, sample DNA extraction, 16S rRNA gene amplification and 454 pyrosequencing were used in both studies. However, these two studies differed primarily in terms of the patient populations recruited for evaluation. The present study focused on Chinese subjects, whereas Dinh et al.21 enrolled American subjects. Lozupone et al.22 also sought to determine the association between HIV infection and characteristic fecal bacterial microbiome changes and found that the microbiome of HIV-infected individuals in the United States was similar to that of healthy individuals residing in the agrarian cultures of Malawi and Venezuela. The researchers related this phenomenon to the diets of these individuals, which are carbohydrate-rich and poor in protein and fat. Overall, these findings indicate that the bacterial composition and balance in the fecal bacterial microbiome is dependent not only on the health status of the individual but also on their environment and diet, which may partially explain the difference in the observed microbiome changes between American and Chinese subjects with HIV infection.
Additional factors affecting the fecal microbiome, including alcohol use, lean body mass, nutritional factors, and the intake of carbohydrate-rich, protein-poor and fat-poor diets, have also been investigated.23, 24, 25, 26, 27 Volpe et al.23 focused on cocaine-induced differences in the relative abundance of major phyla in the fecal bacterial microbiome of HIV-infected patients, as well as on markers of inflammation and microbial translocation. In that study, HIV-infected individuals similar to the Chinese subjects in our study had a higher relative abundance of Proteobacteria, whereas cocaine users had a higher relative abundance of Bacteroidetes. Furthermore, HIV-infected cocaine users had the highest interferon levels indicating that drug use may further alter the microbiome and exacerbate inflammation.
We present the first epidemiologic study comparing the fecal bacterial microbiome of chronic HIV-infected patients with that of non-HIV infected controls in China. Chinese HIV-infected patients are similar to the subjects in other parts of the world in that HIV infection reduces microbiome diversity and enriches Proteobacteria. However, the affected lower ranked taxa in Proteobacteria were different between the two populations. Because most of our control subjects had diarrhea, the difference could be caused by diarrhea. Dietary factors may also play a role. Because the enrichment of Proteobacteria is also a common finding in inflammatory states,28 similar changes in HIV infection may play a functional role in regulating innate immunity, inflammation and disease progression. The unique microbiome change in Chinese HIV-infected patients should be further investigated to better understand its impact on disease progression and response to ART. An increased understanding of the correlations between the proinflammatory bacterial community composition in the human fecal bacterial microbiome and chronic HIV infection-related health complications will contribute to improved and holistic management of this disease.
Our study was limited by a small sample size. In particular, our study was subject to type-II error (that is, failing to detect an effect that is present in a small scale study). The power of this study was further weakened by a heterogeneous study population that varied in gender, antibiotic use and HIV progression. Thus, a large-scale study is needed to confirm our findings.
Acknowledgments
This work was supported by the National High Technology Research and Development (863) Program (no. 2014AA021403) and the Twelfth Five-Year Plan for National Economic and Social Development of the People's Republic of China (no. 2012ZX10001001-007). We thank Dr Jijian Yu (Shanghai Sangon Biological Engineering Technology & Service Co., Ltd., Shanghai, China) for providing excellent technical assistance.
Footnotes
Supplementary Information for this article can be found on the Emerging Microbes & Infections website (http://www.nature.com/emi)
Supplementary Material
References
- Bengmark S. Ecological control of the gastrointestinal tract. The role of probiotic flora. Gut 1998; 42: 2–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Keefe SJ. Nutrition and colonic health: The critical role of the microbiota. Curr Opin Gastroenterol 2008; 24: 51–58. [DOI] [PubMed] [Google Scholar]
- Zhao L, Shen J. Whole-body systems approaches for gut microbiota-targeted, preventive healthcare. J Biotechnol 2010; 149: 183–190. [DOI] [PubMed] [Google Scholar]
- Qin J, Li R, Raes J et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature 2010; 464: 59–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lozupone CA, Stombaugh JI, Gordon JI et al. Diversity, stability and resilience of the human gut microbiota. Nature 2012; 489: 220–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nam Y-D, Jung M-J, Roh SW et al. Comparative analysis of Korean human gut microbiota by barcoded pyrosequencing. PLoS One 2011; 6: e22109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maccaferri S, Biagi E, Brigidi P. Metagenomics: Key to human gut microbiota. Dig Dis 2011; 29: 525–530. [DOI] [PubMed] [Google Scholar]
- Zoetendal EG, Rajilic-Stojanovic M, de Vos WM. High-throughput diversity and functionality analysis of the gastrointestinal tract microbiota. Gut 2008; 57: 1605–1615. [DOI] [PubMed] [Google Scholar]
- Rajilić-Stojanović M, Smidt H, de Vos WM. Diversity of the human gastrointestinal tract microbiota revisited. Environ Microbiol 2007; 9: 2125–2136. [DOI] [PubMed] [Google Scholar]
- Lu HZ. The rule of conventional diagnosis and treatment for HIV/AIDS and its related diseases. Shanghai: The press of Shanghai science and technology, 2009: 1–61. [Google Scholar]
- Le Nguyen H, Pitakpolrat P, Sirivichayakul S et al. Minority HIV-1 resistant variants in recent infection and in patients who failed first-line antiretroviral therapy with no detectable resistance-associated mutations in Thailand. J Med Virol 2012; 84: 713–720. [DOI] [PubMed] [Google Scholar]
- Mutlu EA, Keshavarzian A, Losurdo J et al. A compositional look at the human gastrointestinal microbiome and immune activation parameters in HIV infected subjects. PloS Pathog 2014; 10: e1003829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park SY, Goeken N, Lee HJ et al. Developing high-throughput HIV incidence assay with pyrosequencing platform. J Virol 2014; 88: 2977–2990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellecave P, Recordon-Pinson P, Papuchon J et al. Detection of low-frequency HIV type 1 reverse transcriptase drug resistance mutations by ultradeep sequencing in naive HIV type 1-infected individuals. AIDS Res Hum Retroviruses 2014; 30: 170–173. [DOI] [PubMed] [Google Scholar]
- Chakravorty S, Helb D, Burday M et al. A detailed analysis of 16S ribosomal RNA gene segments for the diagnosis of pathogenic bacteria. J Microbiol Methods 2007; 69: 330–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas BJ, Gevers D, Earl AM et al. Chimeric 16S rRNA sequence formation and detection in Sanger and 454-pyrosequenced PCR amplicons. Genome Res 2011; 21: 494–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nossa CW, Oberdorf WE, Yang L et al. Design of 16S rRNA gene primers for 454 pyrosequencing of the human foregut microbiome. World J Gastroenterol 2010; 16: 4135–4144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakamoto M, Umeda M, Ishikawa I et al. Comparison of the oral bacterial flora in saliva from a healthy subject and two periodontitis patients by sequence analysis of 16S rDNA libraries. Microbiol Immunol 2000; 44: 643–652. [DOI] [PubMed] [Google Scholar]
- Caporaso JG, Kuczynski J, Stombaugh J et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods 2010; 7: 335–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segata N, Izard J, Waldron L et al. Metagenomic biomarker discovery and explanation. Genome Biol 2011; 12: R60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinh DM, Volpe GE, Duffalo C et al. The intestinal microbiota, microbial translocation, and systemic inflammation in chronic HIV infection. J Infect Dis 2015; 211: 19–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lozupone CA, Li M, Campbell TB et al. Alterations in the gut microbiota associated with HIV-1 infection. Cell Host Microbe 2013; 14: 329–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volpe GE, Ward H, Mwamburi M et al. Associations of cocaine use and HIV infection with the intestinal microbiota, microbial translocation and inflammation. J Stud Alcohol Drugs 2014; 75: 347–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelder T, Stroeve JH, Bijlsma S et al. Correlation network analysis reveals relationships between diet-induced changes in human gut microbiota and metabolic health. Nutr Diabetes 2014; 4: e122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nwosu FC, Avershina E, Wilson R et al. Gut microbiota in HIV infection: implication for disease progression and management. Gastroenterol Res Pract 2014; 2014: 803185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gori A, Tincati C, Rizzardini G et al. Early impairment of gut function and gut flora supporting a role for alteration of gastrointestinal mucosa in human immunodeficiency virus pathogenesis. J Clin Microbiol 2008; 46: 757–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis CL, Ma Z-M, Mann SK et al. Molecular characterization of stool microbiota in HIV-infected subjects by panbacterial and order-level 16S ribosomal DNA (rDNA) quantification and correlations with immune activation. J Acquir Immune Defic Syndr 2011; 57: 363–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marnie P, Janette B, Douglas B. Kell, Etheresia Pretorius. The dormant blood microbiome in chronic inflammatory diseases. FEMS Microbiol Rev 2015; 39: 567–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.