Abstract
Objective
To investigate the effects of hippotherapy on psychosocial and emotional parameters in children with cerebral palsy (CP) and their caregivers.
Methods
Eight children with CP were recruited (three males and five females; mean age, 7.3 years; Gross Motor Function Classification System levels 1–3). Hippotherapy sessions were conducted for 30 minutes once weekly for 10 consecutive weeks in an indoor riding arena. The Gross Motor Function Measure (GMFM), Pediatric Balance Scale (PBS), and the Korean version of the Modified Barthel Index were evaluated. All children were evaluated by the Children's Depression Inventory, Trait Anxiety Inventory for Children, State Anxiety Inventory for Children, Rosenberg Self Esteem Scale, and the Korean-Satisfaction with Life Scale (K-SWLS). Their caregivers were evaluated with the Beck Depression Inventory, the Beck Anxiety Inventory, and the K-SWLS. We assessed children and their caregivers with the same parameters immediately after hippotherapy.
Results
Significant improvements on the GMFM, dimension E in the GMFM, and the PBS were observed after hippotherapy compared with the baseline assessment (p<0.05). However, no improvements were detected in the psychosocial or emotional parameters in children with CP or their caregivers. None of the participants showed any adverse effects or accidents during the 10 weeks hippotherapy program.
Conclusions
Hippotherapy was safe and effectively improved gross motor and balance domains in children with CP. However, no improvements were observed in psychosocial or emotional parameters.
Keywords: Hippotherapy, Cerebral palsy, Psychosocial aspects
INTRODUCTION
Cerebral palsy (CP) is a neurological disease that occurs in 2–3/1,000 newborns [1] and causes movement and postural disorders due to non-progressive damage that occurs in the immature fetal or infant brain [2], leading to chronic neurological abnormalities and developmental disorders that require lifelong movement therapy [3]. An early diagnosis and various treatments, such as therapeutic exercise, braces, and surgical treatment, should be applied for comprehensive rehabilitation therapy [4].
Hippotherapy is a field of rehabilitation therapy to achieve physical, social, and psychological well-being through horse riding, which is a whole-body exercise. Subjects ride horses under the prescription of a professional faculty. Hippotherapy provides a new stimulus related to gait and helps balance and postural control in children with CP because the pelvic movements of a horse rider are similar to that of the pelvis during gait [5]. Hippotherapy is a good strategy to increase functioning in children with CP who need continued, varied, and repetitive treatment [6]. The physical effects and functional improvements after hippotherapy improve spatiotemporal parameters, such as gait speed, rhythm, width, and bilateral symmetry [7], as well as improve gross motor function and balance parameters [8].
However, hippotherapy lacks a scientific basis regarding psychosocial effects. McGibbon et al. [9] reported that hippotherapy applied twice weekly for 8 weeks in children with CP increases social activities, enables hobbies, and reduces energy expenditure during walking. Casady et al. [10] reported that hippotherapy once weekly for 10 weeks improves self-esteem and motivation for activities and that this fun increases participation by children with CP. However, their study was not based on objective results but on the study subject's opinion that they were very interested in participating in more hippotherapy and the author's view that hippotherapy motivates these children to actively participate in social activities [9,10]. Most caregivers of children with CP have psychological and emotional difficulties, such as inferiority and guilt, and experience limitations in time use and their home, conflicts with nondisabled children, and are isolated from neighbors [11].
Thus, in this study, we examined not only functional and balance improvements but also increases in motivation, confidence, concentration, and the sense of accomplishment in children with CP after hippotherapy. We also examined the psychological and emotional effects on the caregivers of the children participating in hippotherapy.
MATERIALS AND METHODS
Subjects
Children who were able to sit with the little assistance or without any help, who had not experienced hippotherapy, and who were spastic hemiplegic, paraplegic, or triplegic patients with disabilities in gait among the children with CP who visited the rehabilitation medical center of Wonkwang University Hospital, were recruited. Those who could not control extreme head movements during hippotherapy, who could not maintain their head position against gravity with a helmet on, who had too much pain or limited joint range of motion to continue hippotherapy, uncorrectable alignment of the spine, pelvis, or lower limbs, or uncontrolled epilepsy, and who were vulnerable to fracture after a fall due to serious osteoporosis were excluded for safety. All patients underwent a physical examination, a horse riding test, and a radiological examination.
Eight children (three males and five females) with CP were recruited. The mean age was 7.3±3.11 years. Four had spastic paraplegia, three had spastic hemiplegia, and one had spastic triplegia. All children were Gross Motor Function Classification System (GMFCS) levels 1–3 (Table 1).
Table 1. General characteristics of participants.
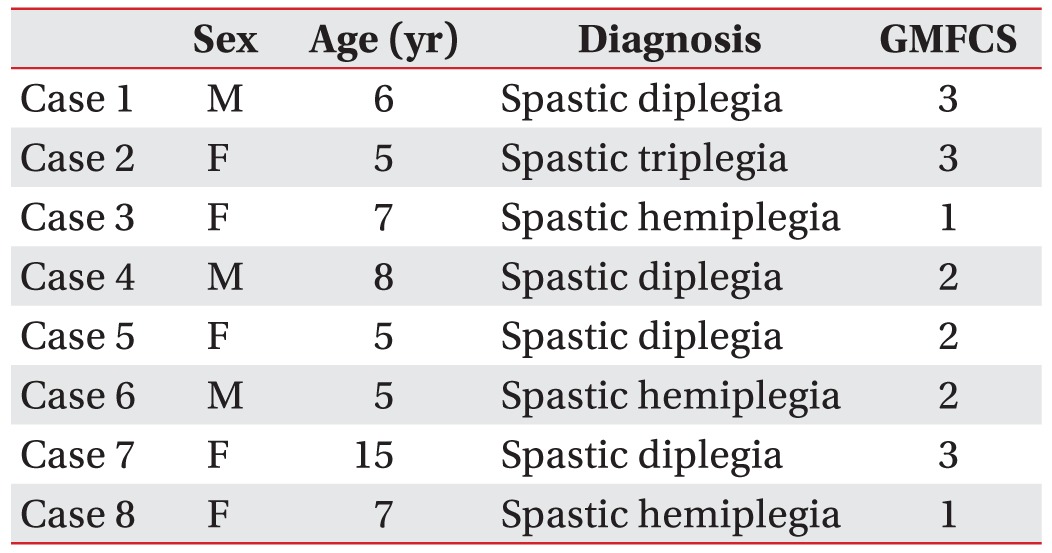
GMFCS, Gross Motor Function Classification System.
The mean age of the caregivers was 34.62±6.12 years (range, 33–40 years), all of whom were the mothers and all but one were married. Three were college graduates, and four were high school graduates. Two of the caregivers had jobs besides being a housewife. The mean amount of caregiving time per day was 18 hours, and none had a history of psychotropic drug use, such as antidepressants.
Methods
Hippotherapy
This study was approved by the Institutional Review Board of Wonkwang University Hospital ethics committee. Hippotherapy was explained to the caregivers of the children, and informed consent was provided prior to the study. Hippotherapy was performed on a rehabilitation horse riding course affiliated with Jeonju Kijeon College. Seven well-domesticated horses were chosen, including two Welsh ponies, three Jeju horses, and two Halflingers. Six miniature ponies were also used for communication activities when the children were riding.
The children wore protective helmets. A leader pulled the horse reins in front, and two side walkers prevented patients from falling by holding their legs and helped the movement of the patients on the horse.
Hippotherapy was done once weekly for 30 minutes for 10 weeks. During each session, physical therapists coordinated many of the movements to improve sensationrelated and cognition-related movement abilities. The movements were variously chosen according to the methods of Developmental Riding Therapy by Spink [12].
All children continued neurodevelopmental and occupational therapy sessions once or twice weekly for about 2 hours per session. Three of eight patients were taking medications for spasticity and maintained medications during hippotherapy. No chemodenervation was done for at least 3 months before hippotherapy.
Functional evaluation of the therapeutic effect
The Gross Motor Function Measure (GMFM-88) was used to assess functional activity and gross motor function development. Among the five dimensions on the gross motor function evaluation, scores for (C) crawling and kneeling, (D) standing, (E) walking, running, and jumping were checked separately. Balance ability was evaluated with the Korean version of the Pediatric Balance Scale (PBS) [13], and the Korean version of the Modified Barthel Index (K-MBI) was used to assess activities of daily living. All assessments were conducted by the same researcher before and after the 10 weeks hippotherapy.
Psychosocial and emotional evaluation of the therapeutic effect
One skilled clinical psychologist conducted evaluations before and after therapy. The subjects were able to communicate and understand the questionnaire questions or they were excluded from the study.
The Children's Depression Inventory (CDI-K) [14], Trait Anxiety Inventory for Children (TAIC) [15], State Anxiety Inventory for Children (SAIC) [15], Rosenberg Self-Esteem Scale (RSES) [16,17], and the Satisfaction with Life Scale (K-SWLS) [18] were used for the psychosocial and emotional evaluation of subjects. The psychosocial and emotional evaluation of the caregivers was performed using the Beck Depression Inventory (BDI) [19,20], the Beck Anxiety Inventory (BAI) [21,22], and the Korean version of the Satisfaction with Life Scale (K-SWLS) [18].
Statistical analysis
SPSS ver. 19.0 software (IBM, Armonk, NY, USA) was used for the analysis. The Kolmogorov-Smirnov test was used to test the normality of the data distribution and the paired sample t-test and Wilcoxon signed-rank test were used to compare the results before and after hippotherapy. Statistical significance was set at p<0.05.
RESULTS
Balance, function, and activities of daily living parameters
The balance parameter on the PBS was 34.87±17.29 before hippotherapy and increased by 4 points on average after therapy (38.12±15.79). The GMFM was 86.62±11.77 before hippotherapy and increased by 2.4 points on average after therapy (89.00±11.64; p<0.05). Among the GMFM score, the dimension (E) of walking, running, and jumping was 54.49±32.73 before and increased to 66.45±32.73 after therapy (p<0.05). However, although the K-MBI showed tendency to increase from 51.37±23.10 to 59.75±16.33, the change was not significant (p=0.109) (Table 2).
Table 2. Functional assessment before and after hippotheray.
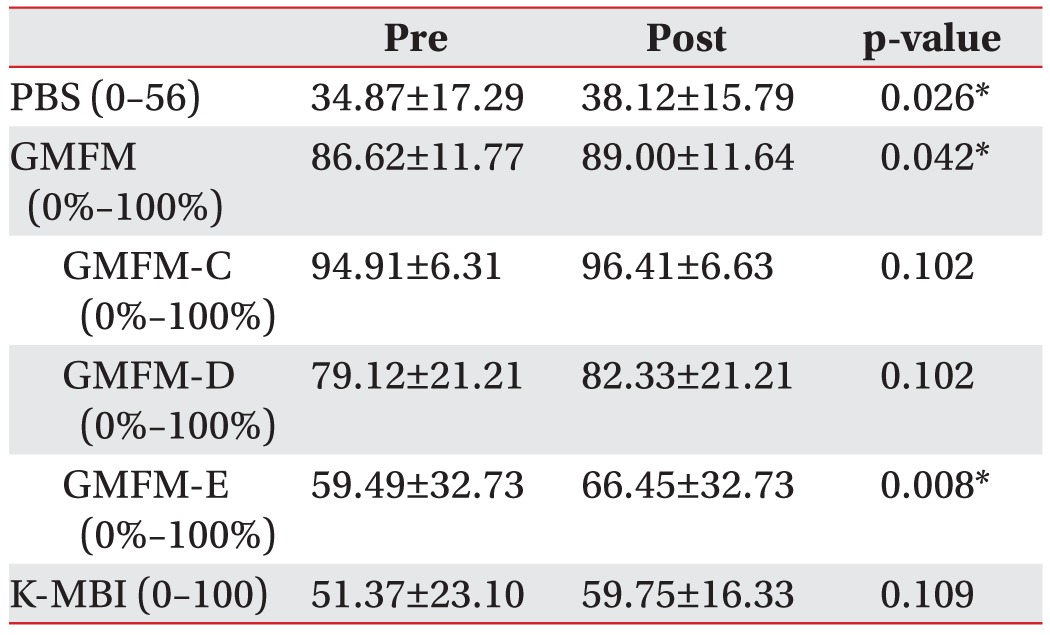
Values are presented as mean±standard deviation.
PBS, Pediatric Balance Scale; GMFM, Gross Motor Function Measure; GMFM-C, GMFM dimension C Crawling & kneeling; GMFM-D, GMFM dimension D standing; GMFM-E, GMFM dimension E gait, running, & jumping; K-MBI, Korean version of Modified Barthel index.
*p<0.05, significant difference between the pre and post groups.
Psychosocial and emotional parameters
The CDI-K score changed from 14.38±8.90 to 12.25±7.32, the TAIC score changed from 38.38±7.90 to 35.13±7.20, and the SAIC score changed from 33.75±6.54 to 33.13±4.64, suggesting that depression and anxiety tended to decrease but no significant differences were detected. The RSES score changed from 25.75±3.06 to 26.25±4.50 and the K-SWLS score changed from 16.63±8.63 to 16.63±6.00, indicating no significant improvements in self-esteem or quality of life parameters (Table 3).
Table 3. Psychosocial assessments before and after hippotherapy, in children with cerebral palsy.
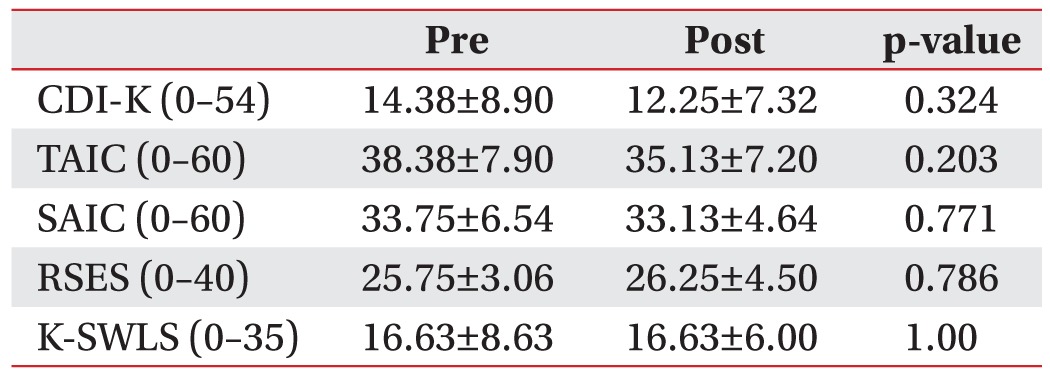
Values are presented as mean±standard deviation.
CDI-K, Children's Depression Inventory – Korean form; TAIC, Trait Anxiety Inventory for Children; SAIC, State Anxiety Inventory for Children; RES, Rosenberg Self-Esteem Scale; K-SWLS, Korean version of Satisfaction with Life Scale.
The BDI score for the caregivers changed from 16.50±11.97 to 15.12±4.99, and the BAI score changed from 14.75±15.15 to 14.50±1.39, suggesting that depression and anxiety tended to decrease. The K-SWLS score changed from 15.37±6.63 to 15.62±5.55. All the psychological parameters of caregivers did not improve significantly (p>0.05) (Table 4).
Table 4. Psychosocial assessments before and after hippotherapy in caregivers.
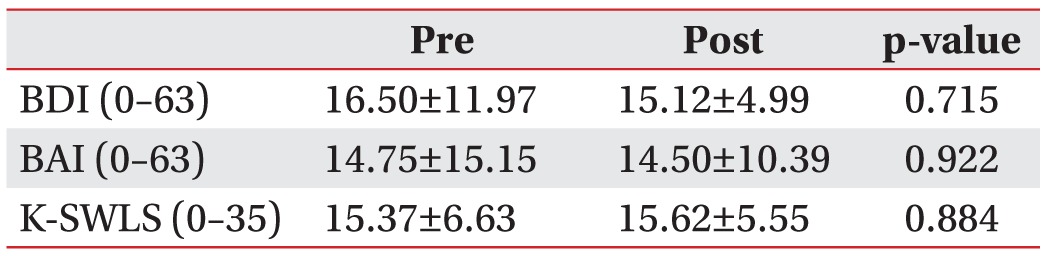
Values are presented as mean±standard deviation.
BDI, Beck Depression Inventory; BAI, Beck Anxiety Inventory; K-SWLS, Korean version of Satisfaction with Life Scale.
DISCUSSION
Previous studies on the effects of hippotherapy targeting children with CP mostly focused on trunk balance, gait, and balancing ability [23]. Shurtleff and Engsberg [24] reported that six patients showed improved neck and trunk balance after 12 weeks of hippotherapy, and Kwon et al. [8] reported that not only gross motor functions including gait but balance ability improved after 8 weeks of hippotherapy conducted twice weekly in a controlled clinical trial of 32 children with CP. In our study, PBS, which measures balance, improved by an average of 4 points, and the GMFM score increased by an average of 2.4 points, suggesting significant improvements after hippotherapy. This result was particularly dramatic in the dimension (E) of walking, running, and jumping. However, this was a pilot study without a comparison group and we only targeted a few patients, so the results are limited for demonstrating the effect of hippotherapy on improvements on the PBS and GMFM. However, Kwon et al. [8] showed a similar result in a controlled clinical trial in which the PBS increased 4.1 points, and the GMFM increased 1.7 points. Improvements in balance and gross motor function can be expected to some degree after once weekly hippotherapy for 10 weeks but additional study is required.
The improvements in physical ability caused by hippotherapy are related to the sensory inputs from the soft and rhythmical movements of the horse that are conveyed to the rider [12]. Static and kinetic movements, changes in center of gravity, and rotational movements all occur between the trunk and pelvis of a rider when the horse walks slowly, which is a new stimulus for children with CP who have not experienced normal gait [3]. Furthermore, the temperature of a horse is 1℃ higher than that of humans, allowing the rider to relax [25]. Patients were expected to maintain upright posture only using the reins without handles between sessions 6 and 10 when the horse's gait was increased, which contributed to improve balance. The children learned the horse's reactions during trotting by sitting and standing rapidly, which improved lower extremity muscle strength, perception of their body center, and balance ability.
We found no significant improvement on the K-MBI, which assesses activities of daily living. A previous study of 29 children with CP who were assessed using the WeeFIM after 10 weeks of hippotherapy showed no significant improvements [3]. In addition, no improvements on the K-MBI were observed in a study that applied hippotherapy targeting patients with a chronic brain disorder [26]. In contrast, activities of daily living improved after hippotherapy in patients with multiple sclerosis [27]. Improvement of independence in activities of daily living after hippotherapy may depend on age, diseases of the subjects, and hippotherapy duration.
Until now, only improvements in gait and balance ability were confirmed after hippotherapy in children with CP but a scientific basis for other psychosocial effects is lacking. Snider et al. [28] and Sterba [29] pointed out the absence of participation field results on the International Classification of Functioning, Disability, and Health (ICF) among study results on the effects of hippotherapy. Since then, one case about self-esteem and participation after hippotherapy was reported. A 6-year-old patient with mild ataxic CP and GMFCS level 1 showed improved self-esteem and participation measured by the Pictorial Scale of Perceived Competence and Social Acceptance for Young Children, as well as functional gross motor function after 8 weeks of twice weekly therapy [30].
We expected that hippotherapy would improve emotional stability through interactions between the horse and children, the special experience in a natural environment, fun during therapy, and participation in a sports activity. However, we found no significant improvement on the psychological parameters. It may be that 10 weeks of once-weekly hippotherapy was insufficient compare to that in a prior study [30]. If we increased the frequency and duration of therapy, children would be expected to achieve physical improvements and fun activities.
Parents of children with CP are in the center of children's lives and therapies [31]. Most parents of disabled children show depressive symptoms [32] and this is consistently shown in studies targeting children with CP [33,34]. In our study, the BDI score of the caregivers was 16.50±11.97, which was consistent with a prior study [31]. Usually mothers of children with CP have high rates of depression and a low quality of life, so understanding the psychological and emotional state of mothers during rehabilitation therapy and improving their psychological and emotional status by improving quality of life and self-esteem of the patients provides psychological support. However, we found no psychological or emotional improvements in mothers of children with CP. Future study targeting more children with CP with more intensive hippotherapy is required.
This study had the following limitations. First, it only targeted children who underwent hippotherapy and did not compare children who did not participate in hippotherapy. Second, reliability was low because we only enrolled a few patients. Third, the same researcher who was not blinded conducted the functional evaluations before and after hippotherapy children, so we cannot exclude bias.
In conclusion, this was a pilot study that compared motor function and psychosocial parameters of children with CP before and after hippotherapy. Hippotherapy showed a positive effect on gross motor function and improved balance but we could not verify improvement in psychosocial parameters, such as depression, anxiety, and quality of life, in children and their caregivers as a result of the therapy.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Morris C. Definition and classification of cerebral palsy: a historical perspective. Dev Med Child Neurol Suppl. 2007;109:3–7. doi: 10.1111/j.1469-8749.2007.tb12609.x. [DOI] [PubMed] [Google Scholar]
- 2.Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;109:8–14. [PubMed] [Google Scholar]
- 3.Kim HS, Lee KW, Hwang JH, Kim EJ, Lee YT, Chung SH, et al. Therapeutic effects of horseback riding (hippotherapy) on motor development of children with cerebral palsy. Korean J Sports Med. 2005;23:278–283. [Google Scholar]
- 4.Yim SY, Dung IY, Kwuan BS. Cerebral palsy: etiology and evaluation, clinical feature and management. In: Sung IY, editor. Pediatric rehabilitation. 1st ed. Seoul: Koonja; 2006. pp. 173–212. [Google Scholar]
- 5.Glasow BL. Hippotherapy: the horse as a therapeutic modality. People Anim Environ. 1986;4:30–31. [Google Scholar]
- 6.Cunningham B. The effect of hippotherapy on functional outcomes for children with disabilities: a pilot study. Pediatr Phys Ther. 2009;21:137. doi: 10.1097/PEP.0b013e318197a60d. [DOI] [PubMed] [Google Scholar]
- 7.Manikowska F, Jozwiak M, Idzior M, Chen PJ, Tarnowski D. The effect of a hippotherapy session on spatiotemporal parameters of gait in children with cerebral palsy: pilot study. Ortop Traumatol Rehabil. 2013;15:253–257. doi: 10.5604/15093492.1058420. [DOI] [PubMed] [Google Scholar]
- 8.Kwon JY, Chang HJ, Lee JY, Ha Y, Lee PK, Kim YH. Effects of hippotherapy on gait parameters in children with bilateral spastic cerebral palsy. Arch Phys Med Rehabil. 2011;92:774–779. doi: 10.1016/j.apmr.2010.11.031. [DOI] [PubMed] [Google Scholar]
- 9.McGibbon NH, Andrade CK, Widener G, Cintas HL. Effect of an equine-movement therapy program on gait, energy expenditure, and motor function in children with spastic cerebral palsy: a pilot study. Dev Med Child Neurol. 1998;40:754–762. doi: 10.1111/j.1469-8749.1998.tb12344.x. [DOI] [PubMed] [Google Scholar]
- 10.Casady RL, Nichols-Larsen DS. The effect of hippotherapy on ten children with cerebral palsy. Pediatr Phys Ther. 2004;16:165–172. doi: 10.1097/01.PEP.0000136003.15233.0C. [DOI] [PubMed] [Google Scholar]
- 11.Kim YM. A study on stresses and coping behaviors of the mothers with cerebral palsied children [master's thesis] Seoul: Ewha Womans University; 1990. [Google Scholar]
- 12.Spink J. Developmental riding therapy: a team approach to assessment and treatment. Tucson: Therapy Skill Builders; 1993. [Google Scholar]
- 13.Franjoine MR, Gunther JS, Taylor MJ. Pediatric balance scale: a modified version of the berg balance scale for the school-age child with mild to moderate motor impairment. Pediatr Phys Ther. 2003;15:114–128. doi: 10.1097/01.PEP.0000068117.48023.18. [DOI] [PubMed] [Google Scholar]
- 14.Cho SC, Lee YS. Development of the Korean form of the Kovecs' Children's Depression Inventory. J Korean Neuropsychiatr Assoc. 1990;29:943–956. [Google Scholar]
- 15.Choi JS, Cho SC. Reliability and validity of revised children's manifest anxiety scale: assessment of anxiety in children. J Korean Neuropsychiatr Assoc. 1990;29:691–702. [Google Scholar]
- 16.Rosenberg M. Society and the adolescent self-image. Princeton: Princeton University Press; 1965. [Google Scholar]
- 17.Lee J, Nam S, Lee MK, Lee JH, Lee SM. Rosenberg' Self-Esteem Scale: analysis of item-level validity. Korean J Couns Psychother. 2009;21:173–189. [Google Scholar]
- 18.Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life Scale. J Pers Assess. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- 19.Beck AT. Depression: clinical, experimental and theoretical aspects. J R Coll Gen Pract. 1969;18:249. [Google Scholar]
- 20.Lee YH, Song JY. A study of the reliability and the validity of the BDI, SDS, and MMPI-D scales. Korean J Clin Psychol. 1991;10:98–113. [Google Scholar]
- 21.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 22.Yook SP, Kim ZS. A clinical study on the Korean version of Beck Anxiety Inventory: comparative study of patient and non-patient. Korean J Clin Psychol. 1997;16:185–197. [Google Scholar]
- 23.Meregillano G. Hippotherapy. Phys Med Rehabil Clin N Am. 2004;15:843–854. doi: 10.1016/j.pmr.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 24.Shurtleff TL, Engsberg JR. Changes in trunk and head stability in children with cerebral palsy after hippotherapy: a pilot study. Phys Occup Ther Pediatr. 2010;30:150–163. doi: 10.3109/01942630903517223. [DOI] [PubMed] [Google Scholar]
- 25.Sterba JA, Rogers BT, France AP, Vokes DA. Horseback riding in children with cerebral palsy: effect on gross motor function. Dev Med Child Neurol. 2002;44:301–308. doi: 10.1017/s0012162201002122. [DOI] [PubMed] [Google Scholar]
- 26.Sunwoo H, Chang WH, Kwon JY, Kim TW, Lee JY, Kim YH. Hippotherapy in adult patients with chronic brain disorders: a pilot study. Ann Rehabil Med. 2012;36:756–761. doi: 10.5535/arm.2012.36.6.756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hammer A, Nilsagard Y, Forsberg A, Pepa H, Skargren E, Oberg B. Evaluation of therapeutic riding (Sweden)/ hippotherapy (United States): a single-subject experimental design study replicated in eleven patients with multiple sclerosis. Physiother Theory Pract. 2005;21:51–77. doi: 10.1080/09593980590911525. [DOI] [PubMed] [Google Scholar]
- 28.Snider L, Korner-Bitensky N, Kammann C, Warner S, Saleh M. Horseback riding as therapy for children with cerebral palsy: is there evidence of its effectiveness? Phys Occup Ther Pediatr. 2007;27:5–23. [PubMed] [Google Scholar]
- 29.Sterba JA. Does horseback riding therapy or therapist-directed hippotherapy rehabilitate children with cerebral palsy? Dev Med Child Neurol. 2007;49:68–73. doi: 10.1017/s0012162207000175.x. [DOI] [PubMed] [Google Scholar]
- 30.Frank A, McCloskey S, Dole RL. Effect of hippotherapy on perceived self-competence and participation in a child with cerebral palsy. Pediatr Phys Ther. 2011;23:301–308. doi: 10.1097/PEP.0b013e318227caac. [DOI] [PubMed] [Google Scholar]
- 31.Cho YK, Kim EJ, Park JW, Cho KE, Lee SH, Kang EY, et al. Assessment of quality of life in parents of children with cerebral palsy. J Korean Acad Rehabil Med. 2008;32:682–688. [Google Scholar]
- 32.Smith TB, Innocenti MS, Boyce GC, Smith CS. Depressive symptomatology and interaction behaviors of mothers having a child with disabilities. Psychol Rep. 1993;73(3 Pt 2):1184–1186. doi: 10.2466/pr0.1993.73.3f.1184. [DOI] [PubMed] [Google Scholar]
- 33.Kim HW, Ko YJ, Lee BN, Lee KA, Choi YJ. Depression and anxiety in mothers of children with cerebral palsy. J Korean Acad Rehabil Med. 2001;25:941–947. [Google Scholar]
- 34.Ones K, Yilmaz E, Cetinkaya B, Caglar N. Assessment of the quality of life of mothers of children with cerebral palsy (primary caregivers) Neurorehabil Neural Repair. 2005;19:232–237. doi: 10.1177/1545968305278857. [DOI] [PubMed] [Google Scholar]


