Abstract
We recently identified a genome-wide genetic association of eosinophilic esophagitis (EoE) at 2p23 spanning the calpain 14 (CAPN14) gene, yet the causal mechanism has not been elucidated. We now show that recombinant CAPN14 cleaves a calpain-specific substrate and is inhibited by 4 classical calpain inhibitors: MDL-28170, acetyl-calpastatin, E-64, and PD151746. CAPN14 is specifically induced (>100-fold) in esophageal epithelium after IL-13 treatment. Epithelial cells overexpressing CAPN14 display impaired epithelial architecture, characterized by acantholysis, epidermal clefting, and epidermolysis. CAPN14 overexpression impairs epithelial barrier function, as demonstrated by decreased transepithelial resistance (2.1-fold) and increased FITC-dextran flux (2.6-fold). Epithelium with gene-silenced CAPN14 demonstrates increased dilated intercellular spaces (5.5-fold) and less organized basal cell layering (1.5-fold) following IL-13 treatment. Finally, CAPN14 overexpression results in loss of desmoglein 1 (DSG1) expression, whereas the IL-13–induced loss of DSG1 is normalized by CAPN14 gene silencing. Importantly, these findings were specific to CAPN14, as they were not observed with modulation of CAPN1 expression. These results, along with the potent induction of CAPN14 by IL-13 and genetic linkage of EoE to the CAPN14 gene locus, demonstrate a molecular and cellular pathway that contributes to T helper type 2 responses in mucosal epithelium.
The protease calpain 14 is induced by IL-13 and promotes esophageal epithelial barrier impairment through loss of desmoglein-1 expression.
Introduction
Eosinophilic esophagitis (EoE) is a chronic inflammatory disorder associated with allergic hypersensitivity to food. We recently interrogated >1.5 million genetic variants in EoE and identified the strongest genome-wide association at 2p23 spanning the calpain 14 (CAPN14) gene (P = 2.5 × 10–10) (1), a finding that has already been replicated by an independent group (2). CAPN14 is a member of the calpain family — a group of intracellular, calcium-activated proteases. Yet, there have been no publications about the functional role of CAPN14.
Calpains are considered to be regulatory proteases, which alter both the structure and function of their substrates (3, 4). The human calpain family consists of 16 members defined by their inclusion of the two main protease domains that compose the protease core. CAPN14 is part of the classical calpain subfamily, defined by its similar domain structure to the most extensively studied calpains, CAPN1 and CAPN2 (5). Calpains have been demonstrated to carry out a number of functions, including restructuring cytoskeletal and membrane proteins, modifying molecules involved in signal transduction pathways, and inactivating enzymes controlling cell cycle progression, gene expression, and apoptosis (6).
CAPN14 is most highly expressed in the esophagus, providing a potential explanation for the tissue specificity of EoE (1). In addition, CAPN14 expression is dynamically regulated as a function of EoE disease activity and genetic haplotype and after exposure of epithelial cells to IL-13. In addition, CAPN14 is located in an epigenetic hot spot modified by IL-13 (1). Furthermore, CAPN14 expression is upregulated by IL-4 and IL-13 (1, 7). Notably, IL-13 is overexpressed in EoE and induces loss of barrier integrity in epithelial cells, mediated in part by loss of desmoglein 1 (DSG1) expression (8).
Herein, we aimed to determine the function of CAPN14 in esophageal squamous epithelium. We first demonstrated that CAPN14 has calpain protease activity and is inhibited by classical calpain inhibitors. Overexpression of CAPN14 in esophageal epithelial cells was sufficient to induce disruption of epithelial cell architecture and impair barrier function, properties not induced by CAPN1. Mechanistically, CAPN14 overexpression reduced DSG1 expression, a process that has already been demonstrated to contribute to EoE via functional and genetic analyses (8, 9). Thus, we have identified CAPN14 as a functional protease that induces esophageal epithelial barrier impairment and loss of DSG1 expression and regulates IL-13–induced epithelial changes, providing insight into the recent genetic linkage of EoE to the CAPN14 and DSG1 loci (1).
Results
CAPN14 is a functional protease.
Recombinant CAPN14 (rCAPN14) and a short form that only included the protease core (domains IIa and IIb; Supplemental Figure 1; supplemental material available online with this article; doi:10.1172/jci.insight.86355DS1) were produced in HEK293 cells. rCAPN14 demonstrated a linear, dose-dependent protease activity in the range of 0.25 to 250 nM of protein using a classical calpain-specific cleavage assay measured by luminescence (10); in contrast, the short form containing only the protease core, which was purified in the same manner as rCAPN14, did not show enzymatic activity (Figure 1A). The classical reversible (MDL-28170, acetyl-calpastatin, and PD151746) and irreversible (E-64) calpain inhibitors preferentially affected rCAPN1 over rCAPN14 (Figure 1, B and C). rCAPN1 showed faster cleavage of the substrate SucLLVY-AMC than rCAPN14, but CAPN14 showed continued reaction progress beyond 112 minutes, whereas the activity of rCAPN1 reached a plateau after 20 minutes upon introduction of the substrate (Figure 1D).
Figure 1. Recombinant calpain 14 has protease activity.
Data from calpain activity assays comparing enzymatic activity of recombinant calpain 1 (rCAPN1), recombinant calpain 14 (rCAPN14), and rCAPN14 protease core are shown. (A) Calpain activity of rCAPN14 and rCAPN14 protease core as a function of protein amount (0.25–250 nM). (B) Calpain activity of rCAPN1 and rCAPN14 in the presence and absence of known reversible calpain inhibitors (n = 3). (C) Calpain activity of rCAPN1 and rCAPN14 in the presence and absence of known irreversible calpain inhibitor E-64. Data are representative of 3 independent experiments. Data are expressed as the mean ± SEM; ****P < 0.0001; statistical significance determined using a 2-tailed t test. (D) Reaction progress curves for cleavage of Suc-LLVY-AMC by rCAPN1 and rCAPN14 in the absence of inhibitors.
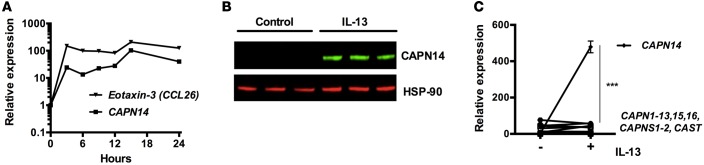
IL-13 specifically induces CAPN14 in esophageal epithelium.
We sought to determine the kinetics of IL-13–induced CAPN14 mRNA in an esophageal epithelial progenitor cell line (EPC2). CAPN14 mRNA expression increased within 3 hours of IL-13 stimulation and remained elevated for at least 24 hours (Figure 2A). Corresponding to the mRNA increase, there was an increase in CAPN14 protein expression, as shown by Western blot (Figure 2B). Of all calpain family members, CAPN14 was the only member that increased with IL-13 stimulation (Figure 2C). CAPN14 mRNA induction mirrored that of another classical IL-13–stimulated gene product, CCL26 (eotaxin-3) (Figure 2A).
Figure 2. IL-13 induces calpain 14 in esophageal epithelial cells.
(A) Expression of calpain 14 (CAPN14) mRNA relative to GAPDH mRNA by quantitative PCR reaction in EPC2 cells exposed to IL-13 (100 ng/ml) for the indicated times. Eotaxin-3 is a positive control for IL-13 stimulation. (B) Western blot analysis of CAPN14 protein in air-liquid interface–cultured (ALI–cultured) EPC2 cells with or without (control) IL-13 for 96 hours; data are representative of 3 independent experiments, and HSP-90 is a loading control. (C) mRNA levels of calpain family members in ALI-cultured EPC2 cells with and without IL-13 treatment; data are derived from RNA-sequencing analysis, expressed as fragments per kilobase of exon per million, and representative of 3 independent experiments. For A and C, data are expressed as the mean or mean ± SEM; ***P < 0.001; statistical significance determined using a 2-tailed t test. CAST, calpastatin; CAPNS1, calpain small subunit 1.
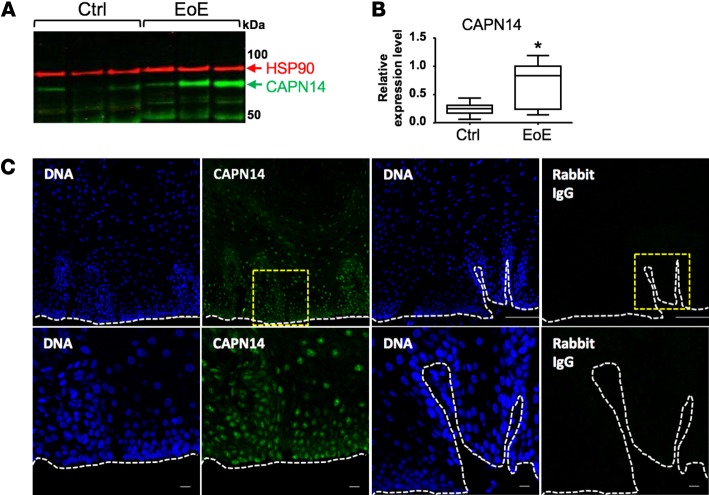
Expression of CAPN14 in esophageal biopsies.
We next examined CAPN14 expression in esophageal biopsies. We observed a considerable increase in CAPN14 protein in EoE compared with that of normal controls, as defined by Western blot analysis (Figure 3, A and B). Immunofluorescent staining revealed that CAPN14 protein expression was specific to the epithelium in the basal and suprabasal regions of the esophagus (Figure 3C).
Figure 3. Expression of calpain 14 in esophageal biopsies.
(A) A representative Western blot analysis of esophageal biopsies obtained from control and active patients with EoE. Each lane represents a separate patient. (B) Calpain 14 (CAPN14) band intensity was quantified in control (n = 10) and active EoE biopsies (n = 8) relative to HSP-90. *P < 0.05; statistical significance determined using Mann-Whitney test. (C) Immunofluorescence of esophageal biopsies from control individuals. Nuclei are indicated by DAPI (DNA) staining (blue). Green indicates staining with anti-CAPN14 antibody (second column) or rabbit IgG (fourth column). The bottom row contains high-powered views of the area enclosed in yellow square above. The dashed white line indicates basement membrane. Scale bar: 100 μm (top row); 10 μm (bottom row).
CAPN14 overexpression in esophageal epithelium results in membranous and nuclear staining.
Overexpression of CAPN14 in a CAPN14-transduced EPC2 cell line was demonstrable by immunofluorescent staining, which showed diffuse staining in the cytoplasm and nucleus (Figure 4A). Even though control cells had baseline calpain activity, likely from constitutive expression of CAPN1 and CAPN2, the CAPN14-overexpressing cells demonstrated increased calpain activity compared with that of control cells (Figure 4B). After 6 days of culture at air-liquid interface (ALI) (Figure 4C), overexpression transcript levels were similar to IL-13–induced expression levels (Figure 4D) and protein was detectable by Western blot analysis (Figure 4E). CAPN14 immunofluorescent staining was increased at the periphery of the cell and was more intense on the apical side of the cells grown at the ALI (Figure 4F).
Figure 4. Characterization of calpain 14 overexpression.
(A) Calpain 14 (CAPN14) (green) immunofluorescence in EPC2 cells transduced with either empty vector (EV) or CAPN14 overexpression vector (CAPN14). (B) Data shown are from calpain activity assays of lysates from EPC2 cells transduced and selected for EV and CAPN14 overexpression lentivirus uptake (n = 3). (C) A model of the overexpression system is shown. Cells were transduced with either EV or CAPN14 overexpression vector by lentiviral transduction. Differentiated EPC2 esophageal epithelial cells were grown for 11 days in high-calcium media starting at day 2. Cells were brought to the air-liquid interface (ALI) starting at day 7 in the presence or absence of IL-13 treatment (100 ng/ml). Images of H&E-stained cells correspond to the time points above. Original magnification, ×20. (D) Expression of CAPN14 mRNA relative to GAPDH mRNA by quantitative PCR in ALI-cultured EPC2 cells. IL-13 stimulation is a positive control (n = 3). (E) Western blot analysis of CAPN14 protein overexpression in ALI-cultured EPC2 cells. (F) Immunofluorescence of CAPN14 (green) overexpression in ALI-cultured EPC2 cells. DAPI is shown in blue. Original magnification, ×20 (top and middle); ×100 (bottom). Scale bar: 10 μm. Data are representative of 3 independent experiments. For B and D, data are expressed as the mean ± SEM; ***P < 0.001, ****P < 0.0001; statistical significance determined using a 2-tailed t test.
CAPN14 overexpression impairs epithelial cell architecture.
CAPN14 overexpression caused disruption of the epithelial architecture, including separation of neighboring cells (acantholysis), separation of the epithelium from its underlying substrate (epidermolysis), and intraepidermal clefting (Figure 5A). This disruption occurred despite normal growth of the transduced cells compared with that of control cells in monolayer culture (B.P. Davis, unpublished observations).
Figure 5. Calpain 14 overexpression alters barrier function.
(A) Cultures of EPC2 cells transduced with empty vector (EV) or calpain 14 overexpression vector (CAPN14) and grown at air-liquid interface (ALI) for 6 days were analyzed by H&E stain. These ALI-cultured cells were analyzed by (B) transepithelial resistance (Rt, n = 3) and (C) FITC-dextran flux assay (n = 3). Data are representative of 3 independent experiments. Scale bar: 10 μm. For B and C, data are expressed as the mean ± SEM; ***P < 0.001; statistical significance determined using a 2-tailed t test.
CAPN14 overexpression impairs barrier function.
Cultures overexpressing CAPN14 had decreased transepithelial resistance (2.1-fold, P < 0.0001) and increased FITC-dextran flux through the epithelial layer (2.6-fold, P < 0.0001) (Figure 5, B and C). Interestingly, when CAPN1 was overexpressed in the same system, it did not affect barrier function or ALI architecture, although CAPN1 was enzymatically active (Supplemental Figure 2). Taken together, these data demonstrate that CAPN14 overexpression specifically induces impaired barrier function in esophageal epithelial cells.
CAPN14 gene silencing dysregulates the IL-13–induced epithelial changes in ALI cultures.
To test whether CAPN14 may be involved in the IL-13–induced impaired barrier function pathway, we developed a CAPN14 gene-silencing approach using the EPC2-ALI system. As above, we performed lentiviral transduction of EPC2 cells with a CAPN14 gene-silencing construct. We verified that the CAPN14 gene was silenced at both the mRNA and protein level (Figure 6, A and B). Additionally, the silencing effect was specific to CAPN14 (Supplemental Figure 3). CAPN14 gene silencing showed sustained barrier and architectural changes after IL-13 stimulation compared with the nonsilencing control (NSC) (Figure 6, C, F, and G), but gene silencing increased the disorder of IL-13–mediated epithelial changes, including dilated intercellular spaces, 5.5-fold (P < 0.001) and the disarray of basal cell organization, as quantified by nuclei lining the basolateral edge, by 1.5-fold (P < 0.05) (Figure 6, C–E). This occurred despite similar cell growth rates (B.P. Davis, unpublished observations).
Figure 6. Effect of calpain 14 gene silencing on epithelial cell responses to IL-13.
EPC2 cells transduced with either a nonsilencing control (NSC) or calpain 14 (CAPN14) gene silencing (KD-1 and KD-2) vector were grown at the air-liquid interface (ALI) with and without IL-13 and analyzed by (A) quantitative PCR of CAPN14 mRNA relative to GAPDH mRNA and normalized to NSC without IL-13 (n = 3). (B) Western blot analysis of CAPN14 protein in ALI culture (n = 3) with HSP-90 as a loading control. (C) H&E staining of ALI-cultured EPC2 cells. (D) Quantification of the percentage of total area of dilated intercellular spaces. (E) Quantification of nuclei of basal cells in contact with basolateral edge of ALI epithelium. (F) Transepithelial resistance (Rt, n = 3) and (G) FITC-dextran flux (n = 3) of ALI system. Data are representative of 3 independent experiments. Scale bar: 10 μm. For A and D–G, data are represented as the mean ± SEM; *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001; statistical significance determined using a 2-tailed t test.
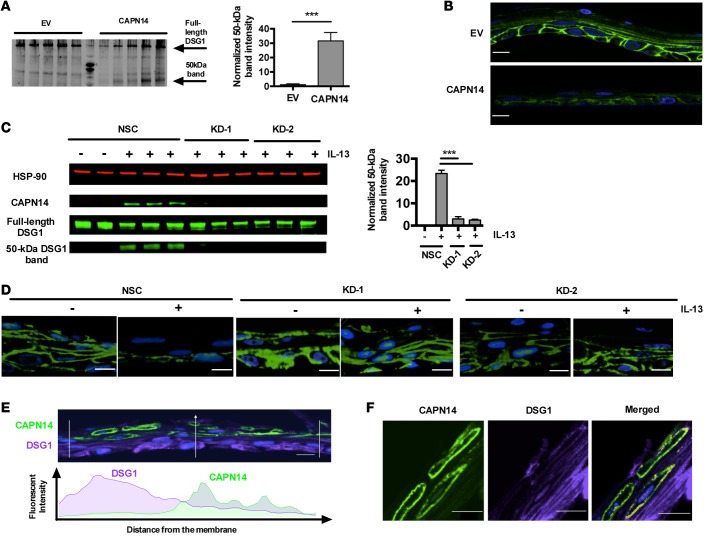
CAPN14 overexpression disrupts DSG1 expression.
We next investigated the effect of CAPN14 overexpression on junctional protein integrity. We first interrogated junctional protein expression by Western blot analysis of 14 junctional proteins (Supplemental Figure 4) and found a specific decrease in DSG1 expression (Figure 7A). CAPN14 overexpression produced a lower-molecular-weight band (50 kDa) not seen with the empty vector control using anti-DSG1 antibody (Figure 7A). Immunofluorescent staining for DSG1 of CAPN14-overexpressing cells grown at the ALI had decreased staining intensity and a loss of the defined membranal staining pattern (Figure 7B). We did not observe this same effect with CAPN1 overexpression (Supplemental Figure 5). To further examine the CAPN14-mediated loss of DSG1, we examined the effect of CAPN14 gene silencing on DSG1 expression. We found that the 50-kDa DSG1 band seen with CAPN14 overexpression could also be induced with IL-13 stimulation and that the IL-13–stimulated 50-kDa band was specifically blocked with CAPN14 gene silencing (Figure 7C). DSG1 immunofluorescence was decreased by IL-13 stimulation, but this effect was partially rescued by CAPN14 gene silencing (Figure 7D). Next, we observed that the immunofluorescent signal of CAPN14 and DSG1 showed an inverse localization relationship, which was particularly evident when the fluorescent intensity was plotted according to distance from the membrane (Figure 7E); the two signals overlapped in the middle of the ALI-cultured cells, where there was colocalization (Figure 7F). Finally, we found that DSG1 was not the only epithelial differentiation gene product affected by CAPN14 expression (Supplemental Figure 6).
Figure 7. Effect of calpain 14 overexpression on desmoglein 1 expression.
EPC2 cells transduced with empty vector (EV), calpain 14 overexpression vector (CAPN14), nonsilencing control (NSC), or CAPN14 gene-silencing (KD-1 and KD-2) vectors were grown at the air-liquid interface (ALI) and analyzed by (A) Western blot analysis for desmoglein 1 (DSG1). Quantitation of the 50-kDa DSG1 band intensity normalized to the full-length DSG1 band intensity is shown. (B) Immunofluorescence of DSG1 (green) in ALI culture; DAPI is shown in blue. (C) Western blot analysis of the CAPN14 gene-silencing effect on IL-13–mediated appearance of a DSG1 immunoreactive molecular species (50-kDa band) and quantitation of the 50-kDa DSG1 band intensity normalized to full-length DSG1 band intensity. (D) Immunofluorescence of DSG1 (green) in ALI-cultured EPC2 cells with and without IL-13 stimulation and CAPN14 gene silencing; DAPI is shown in blue. (E) ALI immunofluorescence intensity relationship of CAPN14 (green) and DSG1 (purple) and (F) colocalization of CAPN14 (green) and DSG1 (purple); DAPI is shown in blue. Data are representative of 3 independent experiments performed with replicates (n = 3–6). For A and C, data are expressed as the mean ± SEM; ***P < 0.001; statistical significance determined using a 2-tailed t test. Original magnification, ×20. Scale bar: 10 μm.
Discussion
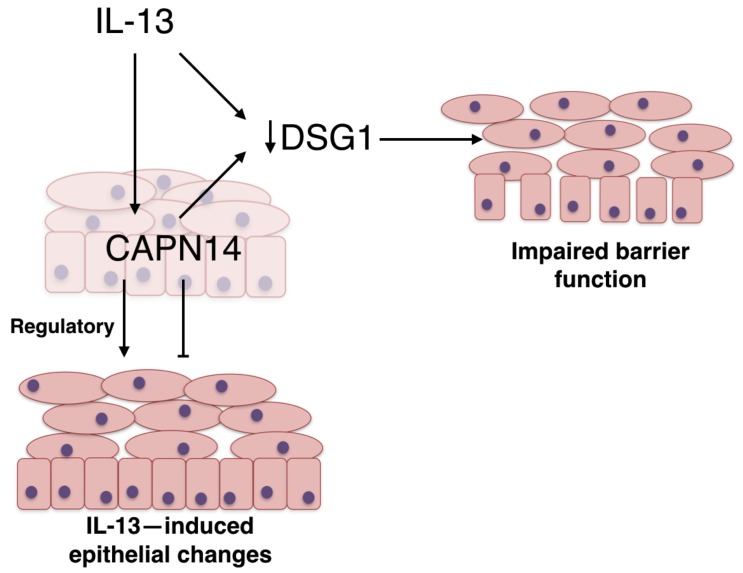
Herein, we report what we believe is the first description of the biochemical and functional properties of CAPN14. First, we identified CAPN14 as a functional enzyme that is blocked by known inhibitors of classical calpains. Second, we reported that CAPN14 is the only member of the calpain family substantially induced by IL-13 in esophageal epithelium in vitro. Third, we showed that CAPN14 protein expression is increased in EoE and is specifically expressed in the basal and suprabasal regions of the epithelium. Fourth, we showed that CAPN14 has dynamic subcellular localization depending on cell-culturing conditions, a cytoplasmic and nuclear localization in submerged cells, and an apical localization in ALI-cultured cells, likely representing increased stability in the apical epithelium. Fifth, CAPN14 overexpression was sufficient to induce disruption of the epithelial architecture. Notably, these CAPN14-induced changes are reminiscent to those seen in biopsies of patients with EoE, including acantholysis. Sixth, we reported that CAPN14 overexpression induces loss of epithelial barrier function, as assessed by transepithelial cell resistance and paracellular flux. Seventh, mechanistically, we associated CAPN14 overexpression with loss of DSG1 expression, likely by a degradative mechanism, a process already shown to occur in EoE. Finally, we made the observation that lack of CAPN14 disturbs IL-13–induced epithelial cell changes, as demonstrated by increased dilated intercellular spaces and basal cell disorder in the presence of CAPN14 gene silencing. These findings suggest a key role for CAPN14 in regulating the effector phase of epithelial pathology and in repair to cell injury (Figure 8). This latter finding also offers an explanation for the observation that the EoE risk allele is associated with reduced esophageal CAPN14 expression, even though CAPN14 is generally overexpressed in EoE compared with controls, and supports the view that CAPN14 may be involved in multiple aspects of the disease, including susceptibility, induction, and repair. Collectively, we have elucidated a mechanism contributing to T helper type 2–associated responses in the epithelium, and this contributes to our understanding of the genetic association of EoE with the CAPN14 gene (2p23).
Figure 8. Model of calpain 14 function.
IL-13 stimulates calpain 14 (CAPN14) expression and desmoglein 1 (DSG1) downregulation. In addition, CAPN14 leads to the loss of DSG1 expression, which, together with IL-13–mediated effects, causes an impaired barrier function. In addition, CAPN14 has a regulatory role on the epithelial structure, as CAPN14 gene silencing induces disorder of the IL-13–mediated changes. We propose that CAPN14 acts as a regulator of IL-13–induced epithelial restructuring. The activity of CAPN14 is likely finely tuned to effect proper restructuring. If CAPN14 is overactive, there is a gross disruption of epithelial integrity. If CAPN14 is underactive, the restructuring process is likely constrained, leading to a disordered epithelial response to IL-13.
CAPN14 belongs to the classical subfamily of the calpain family, which includes calpains 1–3, 8, 9, and 11–14 on the basis of similar domain structure. CAPN14’s activity appears to be distinct compared with that of CAPN1, based on the assay utilized, suggesting different substrate specificities between these two calpains, which is supported by the observed differential effects of these calpains on DSG1. Interestingly, although CAPN1 and CAPN14 have distinct tissue specificities and functions (as defined by our findings), CAPN1 has been reported to cleave profilaggrin and filaggrin 2 (11, 12), central molecules in atopic dermatitis whose expression is reduced in atopic dermatitis and EoE (13). Additionally, mucin processing in the lung, a process that is directly related to IL-13 and is a cardinal characteristic of asthma (14), has been shown to be calpain dependent (15). CAPN1 and CAPN2 have been shown to cleave several barrier-related proteins, including E-cadherin (16). So, it is important that CAPN14 appears to have a specific role in regulating DSG1 expression in contrast to the other classic calpains. Our findings mechanistically place CAPN14 upstream of DSG1 loss, which is a notable process in EoE, as DSG1 is normally markedly reduced in the esophagus of patients with EoE, and its loss is sufficient to induce impaired barrier function in esophageal epithelial cells. DSG1 deficiency leads to an esophageal epithelial transcript signature that includes increased gene expression of the proinflammatory extracellular matrix molecule POSTN and TSLP production (8). These findings have been reinforced by the existence of a human condition induced by homozygous mutations in the DSG1 gene, which cause a severe atopy syndrome that includes EoE (17). Additionally, IL-13 leads to both decreased DSG and barrier dysregulation. In addition, we have preliminary evidence that CAPN14 activity in the epithelium is affecting a differentiation program. Finally, we have evidence demonstrating increased CAPN14 protein expression in EoE that is epithelial specific. Together, this evidence, along with the finding that IL-13 induces CAPN14, suggests that IL-13 and CAPN14 may have a cooperative role in epithelial barrier function.
Importantly, eosinophilic myositis (also known as limb-girdle muscular dystrophy type IIa) is caused by recessive mutations in CAPN3, a skeletal muscle–specific calpain that has been shown to cleave sarcomere proteins in response to cellular injury (18–20). The eosinophilia of eosinophilic myositis has been postulated to be a part of a repair response to intracellular oxidative stress (21). Therefore, our collective data raise the possibility that EoE could be another calpainopathy.
Finally, although we do not yet know whether gain or loss of CAPN14 activity leads to EoE risk, there are already data supporting the usefulness of current medical therapies in both the inhibition and activation of calpain systems that directly affect epithelial regenerative properties and may therefore be future possible EoE therapies (22–24).
In summary, we have shown that CAPN14 encodes a functional protease with potent capacity to induce cellular changes in epithelial cells and that these cellular and resulting tissue alterations are reminiscent of those occurring in EoE, including acantholysis, epidermal clefting, epidermolysis, and impaired barrier function. We functionally link CAPN14 overexpression with loss of DSG1 expression, a process that has already been shown to be causal in EoE (17). Interestingly, loss of DSG1 function occurs in pemphigus foliaceus, a disease also associated with eosinophilia (25). Our data offer a functional explanation of the strong linkage of EoE susceptibility to the CAPN14 gene locus. Notably, IL-33, an epithelial-derived proallergic cytokine, has been shown to be processed in a calpain-dependent manner (26); yet, whether CAPN14 can mediate a similar effect has not yet been demonstrated. The CAPN14 gene-silencing studies provide early evidence that the function of CAPN14 may not be limited to the induction of disease pathogenesis, as CAPN14 gene-silenced cells had exacerbated IL-13–induced pathology (dilated intercellular spaces), providing early evidence that CAPN14 is also involved in regulating repair responses to acute, T helper type 2–associated injury (Figure 7). Our collective data identify CAPN14 as a functional regulatory protease that induces esophageal epithelial barrier impairment and loss of DSG1 expression while supporting possible repair from IL-13–mediated changes. These findings highlight a potential central role of CAPN14 in EoE pathogenesis and thereby implicate EoE as a calpainopathy.
Collectively, we are reporting that CAPN14 is a functional enzyme that induces disruptive effects on esophageal epithelium. These findings, along with the potent induction of CAPN14 by IL-13 and genetic linkage of EoE to the CAPN14 gene locus, demonstrate a molecular and cellular pathway that contributes to T helper type 2 responses in mucosal epithelium.
Methods
Quantitative PCR analysis.
RNA samples were prepared as previously described (27). Briefly, total RNA (250–500 ng) was DNAase treated, and complementary DNA was generated using the iScript complementary DNA synthesis kit (Bio-Rad Laboratories). Quantitative PCR was performed, and SYBR Green (Bio-Rad Laboratories) incorporation was analyzed using iQ5 software (Bio-Rad Laboratories). Relative expression was calculated using a standard curve method. Results were normalized to GAPDH, and fold induction was compared with controls. Primers (Integrated DNA Technologies) used are listed in Supplemental Table 1.
Western blot.
Total cellular protein was extracted from esophageal biopsies with TRIzol (Invitrogen) according to the manufacturer’s instructions. Cell cultures were lysed with RIPA buffer with protease inhibitor cocktail. Loading buffer (Life Technologies) was added, and samples were sonicated, heated to 95°C for 10 minutes, and spun at 15,294 g for 10 minutes to separate the desired supernatant from the insoluble pellet. Samples were subjected to electrophoresis on 4% to 12% NuPAGE Bis-Tris gels (Life Technologies) and transferred to nitrocellulose membranes using the novex iblot system (Life Technologies) and a LI-COR Odyssey CLx imager (LI-COR). Primary antibodies were used at a 1:1,000 dilution and included the following: anti-DSG1 (sc-20114, Santa Cruz Biotechnology), anti-CAPN14 (HPA035720, Sigma-Aldrich), anti-HSP-90 (61014, BD Biosciences), anti-CAPN1 (HPA005992, Sigma-Aldrich), and anti–β-actin (A5441, Sigma-Aldrich). Secondary antibodies were used at 1:10,000 and included the following: goat anti-mouse (926-68070, LI-COR) and goat anti-rabbit (926-3221, LI-COR). Blots were visualized using the Odyssey CLx system (LI-COR) and were quantified using Image Studio (LI-COR).
RNA sequencing and bioinformatic analyses.
RNA isolated from ALI cultures was subjected to RNA sequencing at the CCHMC Gene Discovery and Genetic Variation Core as previously described (28). The paired-end sequencing reads were aligned against the GRCh37 genome model using TopHat 2.04 with Bowtie 2.03 (29, 30). The separate alignments were then merged using Cuffmerge, with RefSeq gene models as a reference. The aligned reads were then quantified for differential expression analysis using Cuffdiff (31). Statistical significance was determined using a t test with a threshold of P < 5 × 10–2 and a 2-fold cutoff filter in GeneSpring 11.5 (Agilent Technologies Incorporated). The GEO accession number for this data set is GSE65335.
EPC2 cell culture.
The esophageal epithelial cell line (human telomerase reverse transcriptase–immortalized EPC2 cell line) was a gift from Anil Rustgi (University of Pennsylvania, Philadelphia, Pennsylvania, USA) (32). EPC2 cells were cultured in keratinocyte serum–free media (Life Technologies) supplemented with bovine pituitary extract, epidermal growth factor, and amphotericin (Life Technologies).
ALI culture system.
For the ALI culture system, EPC2 cells were grown to confluence while fully submerged in low-calcium ([Ca2+] = 0.09 mM), keratinocyte, serum-free media (Life Technologies) on permeable supports with 0.4-mm pores (Corning Incorporated). Confluent monolayers were then switched to high-calcium ([Ca2+] = 1.8 mM), keratinocyte, serum-free media for an additional 5 days. To induce epithelial stratification and differentiation, the culture medium was removed from the inner chamber of the permeable support in order to expose the cell monolayer to the air interface. Differentiated esophageal epithelial equivalents were analyzed 5 to 7 days after exposure.
Lentiviral transduction.
EPC2 cells were transduced with shRNA targeting the 3′ UTR of CAPN14 or a NSC shRNA using the Mission RNAi system (SHCLNG-NM_001145122, Sigma-Aldrich) or overexpression constructs (CAPN1, CAPN14, empty vector) using the PLVX-puro vectors (Clontech). Lentiviral particles were prepared at the CCHMC Viral Vector Core facility. Forty-eight hours after transduction, cells were selected for stable integration using puromycin (1 mg/ml). Overexpression and gene silencing efficiency, as compared with NSC shRNA– or empty vector–transduced cells, was assessed by quantitative PCR, Western blot, and immunofluorescent staining, as described herein.
Immunofluorescent histochemical microscopy.
For immunohistochemical staining, formalin-fixed, paraffin-embedded distal esophageal biopsies and ALI-cultured epithelium were serially sectioned and deparaffinized using xylene followed by graded ethanol washes. Heat-induced epitope retrieval in sodium citrate buffer (10 mM sodium citrate, 0.05% Tween 20, pH 6.0) was used, and endogenous peroxidase activity was quenched in 2% H2O2. Slides were blocked in phosphate-buffered saline with 3% goat serum for 1 hour followed by overnight incubation at 4°C in the following primary antibodies (2 mg/ml): mouse anti-DSG1 (sc-2011; Santa Cruz Biotechnology) and rabbit anti-CAPN14 (HPA035720, Sigma-Aldrich). Slides were then washed and incubated for 1 hour at room temperature with either anti-rabbit Alexa Fluor 488 (A11008, Life Technologies) or anti-mouse (A11012, Life Technologies) (1:250). Nuclei were stained with DAPI. Histochemical staining of slides was performed with H&E stain. Cross-sectional area of H&E-stained sections was calculated using image processing with ImageJ (NIH).
Transepithelial resistance and paracellular flux assays.
Transepithelial resistance measurements and paracellular flux assays using FITC-dextran (average molecular weight 4 kDa) were performed as previously described (33). In vitro measurements for transepithelial resistance following ALI culture were assessed using an EVOM (World Precision Instruments Inc.). Fluorescence was read using the Biotek Synergy2 Multi-Mode microplate reader.
Calpain activity assay.
EPC2 cultures were lysed with Mammalian Protein Extraction Reagent lysis buffer (Pierce, 78501) in the presence of 1 mM EDTA and 1 mM dithiothreitol on ice. rCAPN14 used in this assay was obtained from Lifeome. It was produced as amino acids 43–684, with the predicted molecular weight of 78 kDa. Recombinant or purified protein was diluted in calpain activity buffer (100 mM Tris-HCl, pH 7.4, 10 mM CaCl2, 1 mM DTT) to 250 nM unless otherwise noted. Calpain activity was measured with the Promega Calpain-Glo protease assay according to the manufacturer’s instructions. Briefly, 25 μl of lysate or diluted protein was incubated for 15 minutes with reaction buffer, and the luminescence was read at 37°C using the GloMax-Multi+ Microplate Multimode Reader (Promega). For inhibitor studies, inhibitors were added prior to the start of the assay. Concentrations of inhibitors were as follows: 50 μM acetyl-calpastatin (2950, Tocris), 20 μM MDL-28170 (M6690, Sigma-Aldrich), 100 μM PD151746 (Santa Cruz Biotechnologies), and 100 μM E-64 (Sigma-Aldrich). Baseline measurements of Calpain-Glo buffer alone (Promega) were subtracted from results. For irreversible inhibitor E-64, fluorescence measurements were performed on the same instrument using irradiation λEx = 365 nm and reading aminomethylcoumarin signal at λEm = 410–460 nm.
Statistics.
Statistical significance was determined using a 2-tailed t test, and P < 0.05 was considered significant. All statistical analyses were performed using GraphPad Prism (GraphPad Software Incorporated).
Study approval.
The use of patient biopsies in this study was reviewed and approved by the CCHMC Institutional Review Board, Cincinnati, Ohio, USA. Subjects provided informed consent prior to their participation in the study.
Author contributions
MER conceived the project and supervised the study. BPD and MER wrote the manuscript. BPD performed the experiments with assistance from VAL, JKR, LCK, EMS, MEK, JT, and MR. All of the authors discussed the results and commented on the manuscript.
Supplementary Material
Acknowledgments
This work was supported in part by NIH grant U19 AI070235, NIH grant R01 AI124355, Public Health Service grant P30 DK078392, the Campaign Urging Research for Eosinophilic Disease Foundation, and the Sunshine Charitable Foundation and its supporters, Denise A. Bunning and David G. Bunning. The paper’s contents are solely the responsibility of the authors and do not necessarily represent the official view of the NIH. We thank S. Hottinger for editorial assistance and Margaret Collins for review of histological findings.
Footnotes
Conflict of interest: M.E. Rothenberg is a consultant for Celgene (formerly known as Receptos) and Akari Therapeutics (formerly known as Celsus Therapeutics); has received speaking honorarium from Merck; has an equity interest in Immune Pharmaceuticals and NKT Therapeutics; has royalty rights from reslizumab, a drug being developed by Teva Pharmaceuticals; and is an inventor on patents owned by CCHMC.
Reference information:JCI Insight. 2016;1(4):e86355. doi:10.1172/jci.insight.86355.
Contributor Information
Mark Rochman, Email: Mark.Rochman@cchmc.org.
Jared Travers, Email: jared.travers@cchmc.org.
Marc E. Rothenberg, Email: rothenberg@cchmc.org.
References
- 1.Kottyan LC, et al. Genome-wide association analysis of eosinophilic esophagitis provides insight into the tissue specificity of this allergic disease. Nat Genet. 2014;46(8):895–900. doi: 10.1038/ng.3033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sleiman PM, et al. GWAS identifies four novel eosinophilic esophagitis loci. Nat Commun. 2014;5:e86355. doi: 10.1038/ncomms6593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goll DE, Thompson VF, Li H, Wei W, Cong J. The calpain system. Physiol Rev. 2003;83(3):731–801. doi: 10.1152/physrev.00029.2002. [DOI] [PubMed] [Google Scholar]
- 4.Ono Y, Sorimachi H. Calpains: an elaborate proteolytic system. Biochim Biophys Acta. 2012;1824(1):224–236. doi: 10.1016/j.bbapap.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 5.Sorimachi H, Hata H, Ono O. Calpain chronicle — an enzyme family under multidisciplinary characterization. Proc Jpn Acad Ser B Phys Biol Sci. 2011;87(6):287–327. doi: 10.2183/pjab.87.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chakraborti S, Alam MN, Paik D, Shaikh S, Chakraborti T. Implications of calpains in health and diseases. Indian J Biochem Biophys. 2012;49(5):316–328. [PubMed] [Google Scholar]
- 7.Ueta M, Sotozono C, Kinoshita S. Expression of interleukin-4 receptor α in human corneal epithelial cells. Jpn J Ophthalmol. 2011;55(4):405–410. doi: 10.1007/s10384-011-0030-6. [DOI] [PubMed] [Google Scholar]
- 8.Sherrill JD, et al. Desmoglein-1 regulates esophageal epithelial barrier function and immune responses in eosinophilic esophagitis. Mucosal Immunol. 2014;7(3):718–729. doi: 10.1038/mi.2013.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blanchard C, et al. IL-13 involvement in eosinophilic esophagitis: transcriptome analysis and reversibility with glucocorticoids. J Allergy Clin Immunol. 2007;120(6):1292–1300. doi: 10.1016/j.jaci.2007.10.024. [DOI] [PubMed] [Google Scholar]
- 10.Calpain-Glo Protease Assay Technical Bulletin. [December 1, 2015]; [March 16, 2016];Promega Web site. https://www.promega.com/resources/protocols/technical-bulletins/101/calpain-glo-protease-assay-protocol/
- 11.Hsu CY, et al. Deimination of human filaggrin-2 promotes its proteolysis by calpain 1. J Biol Chem. 2011;286(26):23222–23233. doi: 10.1074/jbc.M110.197400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yamazaki M, et al. Cytoplasmic processing of human profilaggrin by active mu-calpain. Biochem Biophys Res Commun. 1997;235(3):652–656. doi: 10.1006/bbrc.1997.6809. [DOI] [PubMed] [Google Scholar]
- 13.Palmer CN, et al. Common loss-of-function variants of the epidermal barrier protein filaggrin are a major predisposing factor for atopic dermatitis. Nat Genet. 2006;38(4):441–446. doi: 10.1038/ng1767. [DOI] [PubMed] [Google Scholar]
- 14.Wills-Karp M, et al. Interleukin-13: central mediator of allergic asthma. Science. 1998;282(5397):2258–2261. doi: 10.1126/science.282.5397.2258. [DOI] [PubMed] [Google Scholar]
- 15.Lampe WR, Park J, Fang S, Crews AL, Adler KB. Calpain and MARCKS protein regulation of airway mucin secretion. Pulm Pharmacol Ther. 2012;25(6):427–431. doi: 10.1016/j.pupt.2012.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Konze SA, et al. Cleavage of E-cadherin and β-catenin by calpain affects Wnt signaling and spheroid formation in suspension cultures of human pluripotent stem cells. Mol Cell Proteomics. 2014;13(4):990–1007. doi: 10.1074/mcp.M113.033423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Samuelov L, et al. Desmoglein 1 deficiency results in severe dermatitis, multiple allergies and metabolic wasting. Nat Genet. 2013;45(10):1244–1248. doi: 10.1038/ng.2739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ono Y, et al. Functional defects of a muscle-specific calpain, p94, caused by mutations associated with limb-girdle muscular dystrophy type 2A. J Biol Chem. 1998;273(27):17073–17078. doi: 10.1074/jbc.273.27.17073. [DOI] [PubMed] [Google Scholar]
- 19.Krahn M, et al. CAPN3 mutations in patients with idiopathic eosinophilic myositis. Ann Neurol. 2006;59(6):905–911. doi: 10.1002/ana.20833. [DOI] [PubMed] [Google Scholar]
- 20.Taveau M, Bourg N, Sillon G, Roudaut C, Bartoli M, Richard I. Calpain 3 is activated through autolysis within the active site and lyses sarcomeric and sarcolemmal components. Mol Cell Biol. 2003;23(24):9127–9135. doi: 10.1128/MCB.23.24.9127-9135.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rajakumar D, Alexander M, Oommen A. Oxidative stress, NF-κB and the ubiquitin proteasomal pathway in the pathology of calpainopathy. Neurochem Res. 2013;38(10):2009–2018. doi: 10.1007/s11064-013-1107-z. [DOI] [PubMed] [Google Scholar]
- 22.Liu L, Xing D, Chen WR, Chen T, Pei Y, Gao X. Calpain-mediated pathway dominates cisplatin-induced apoptosis in human lung adenocarcinoma cells as determined by real-time single cell analysis. Int J Cancer. 2008;122(10):2210–2222. doi: 10.1002/ijc.23378. [DOI] [PubMed] [Google Scholar]
- 23.Elias PM, et al. Epidermal vascular endothelial growth factor production is required for permeability barrier homeostasis, dermal angiogenesis, and the development of epidermal hyperplasia: implications for the pathogenesis of psoriasis. Am J Pathol. 2008;173(3):689–699. doi: 10.2353/ajpath.2008.080088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karlsson I, et al. Solenopsin A and analogs exhibit ceramide-like biological activity. Vasc Cell. 2015;7:e86355. doi: 10.1186/s13221-015-0030-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lin MS, et al. Desmoglein-1-specific T lymphocytes from patients with endemic pemphigus foliaceus (fogo selvagem) J Clin Invest. 2000;105(2):207–213. doi: 10.1172/JCI8075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hayakawa M, Hayakawa H, Matsuyama Y, Tamemoto H, Okazaki H, Tominaga S. Mature interleukin-33 is produced by calpain-mediated cleavage in vivo. Biochem Biophys Res Commun. 2009;387(1):218–222. doi: 10.1016/j.bbrc.2009.07.018. [DOI] [PubMed] [Google Scholar]
- 27.Zuo L, et al. IL-13 induces esophageal remodeling and gene expression by an eosinophil-independent, IL-13Rα 2-inhibited pathway. J Immunol. 2010;185(1):660–669. doi: 10.4049/jimmunol.1000471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lu TX, et al. MicroRNA signature in patients with eosinophilic esophagitis, reversibility with glucocorticoids, and assessment as disease biomarkers. J Allergy Clin Immunol. 2012;129(4):1064–1075. doi: 10.1016/j.jaci.2012.01.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Langmead B, Trapnell C, Pop M, Salzberg SL. Ultrafast and memory-efficient alignment of short DNA sequences to the human genome. Genome Biol. 2009;10(3):e86355. doi: 10.1186/gb-2009-10-3-r25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Trapnell C, Hendrickson DG, Sauvageau M, Goff L, Rinn JL, Pachter L. Differential analysis of gene regulation at transcript resolution with RNA-seq. Nat Biotechnol. 2013;31(1):46–53. doi: 10.1038/nbt.2450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Garber M, Grabherr MG, Guttman M, Trapnell C. Computational methods for transcriptome annotation and quantification using RNA-seq. Nat Methods. 2011;8(6):469–477. doi: 10.1038/nmeth.1613. [DOI] [PubMed] [Google Scholar]
- 32.Harada H, et al. Telomerase induces immortalization of human esophageal keratinocytes without p16INK4a inactivation. Mol Cancer Res. 2003;1(10):729–738. [PubMed] [Google Scholar]
- 33.Jovov B, Que J, Tobey NA, Djukic Z, Hogan BL, Orlando RC. Role of E-cadherin in the pathogenesis of gastroesophageal reflux disease. Am J Gastroenterol. 2011;106(6):1039–1047. doi: 10.1038/ajg.2011.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.