Highlights
-
•
Arachnoid cysts should be included in the differential diagnosis of sellar cystic lesions.
-
•
Other sellar cystic lesions may present with similar clinical and radiological findings.
-
•
The definitive diagnosis is made on histopathologic examination and immunohistochemical staining.
-
•
Surgery is still the treatment of choice in lesions which are symptomatic, causing decompression and pituitary hypofunction.
Keywords: Sellar arachnoid cyst, Sellar cysts, Arachnoid cyst, Case report
Abstract
Introduction
Arachnoid cysts (ACs) are frequently found on intracranial imaging studies but intrasellar arachnoid cysts are rarely encountered.
Presentation of case
We present a 49-year old patient who had headaches for 6 months and cystic sellar mass was found in his cranial imaging. We operated him by transnasal transsphenoidal route. Our intraoperative diagnosis was an arachnoid cyst and pathologic studies verified our observation. He did well postoperatively and after a 1 year follow-up he was left free from future follow-ups.
Discussion
As common cystic lesions occupying the sellar region can simulate ACs both clinically and radiologically, neurosurgeon can fail to include ACs in making the initial diagnosis preoperatively.
Conclusion
Although a rare entity, arachnoid cysts should be considered in the differential diagnosis of sellar region.
1. Introduction
Intracranial arachnoid cysts (AC) are benign lesions of the arachnoid, forming nearly 1% of all intracranial space-occupying lesions [1]. Compared to other cystic lesions of the sellar region namely the cystic adenomas, craniopharyngiomas and Rathke's cleft cysts, they are rarely seen in this localization with few reports available in the English literature [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14]. ACs are most commonly found in the Sylvian fissure followed by the cerebellopontine angle, the supracollicular area and the vermian area. Intrasellar arachnoid cysts (IAC) constitute about 3% of all intracranial arachnoid cysts [15]. The discrimination of IACs from the cystic lesions of the sellar region remains a difficult preoperative problem because symptoms, signs and imaging characteristics can mimic each other [9], [14]. We describe a case of intrasellar arachnoid cyst, treated through transnasal transsphenoidal approach.
2. Case report
A 49-year-old man presented with 6 month history of headache. The results of the physical, neurologic and ophthalmologic examinations including visual acuity, fundoscopy and visual field studies were unremarkable. Cranial magnetic resonance imaging (MRI) revealed a sellar cystic lesion, and a hypophysis MRI including dynamic contrast enhanced studies were performed.
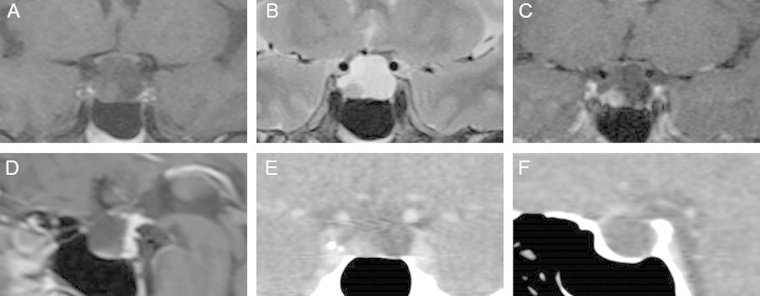
On the MRI a cystic lesion with a dimension of 18 × 14 × 14 mm, extending from the suprasellar cistern, traversing the diaphragma sellae and reaching the level of the dorsum sellae was seen. The optic chiasm was compressed. The lesion was hypointense in T1-weighted images and hyperintense in T2-weighted images. In contrast studies rim like enhancement of the periphery of the lesion was noted. The normal pituitary and pituitary stalk demonstrated a typical enhancement pattern, and were displaced laterally to the right by the lesion (Fig. 1). A computed tomography (CT) scan dedicated to the sellar region, with and without contrast, confirmed a cystic lesion, hypodense with no contrast enhancement (Fig. 1).
Fig. 1.
Preoperative MRI and CT images showing a cystic sellar lesion. A: Coronal T1 weighted MRI image, B: T2 weighted MRI image, C: Coronal Dynamic contrast enhanced T1 weighted MRI image, D: Sagittal dynamic contrast enhanced MRI image; E and F Coronal and sagittal contrast enhanced CT images.
His blood studies including complete blood count, routine biochemistry and pituitary hormone levels, and urinalysis were within normal limits.
A presumptive diagnosis of Rathke’s cleft cyst was made based on the MRI findings.
The patient was operated by transnasal transsphenoidal route. Intraoperatively, after the dural incision, cerebrospinal fluid began to leak and when the opening was widened the lesion was found to have an arachnoidal membrane and when the membrane was opened watery, colorless, CSF like liquid was seen. The membrane was excised totally and normal pituitary, pituitary stalk and the sellar diaphragm were observed.
Postoperative 24-hour hypophysis MRI revealed that cyst was decompressed and optic chiasm and hypophysis were in normal location with no compression (Fig. 2).
Fig. 2.
Postoperative Day 1 coronal MRI images showing cyst excised and the normal hypophysis. A: T1 weighted, B: T2 weighted and C: Dynamic contrast enhanced studies.
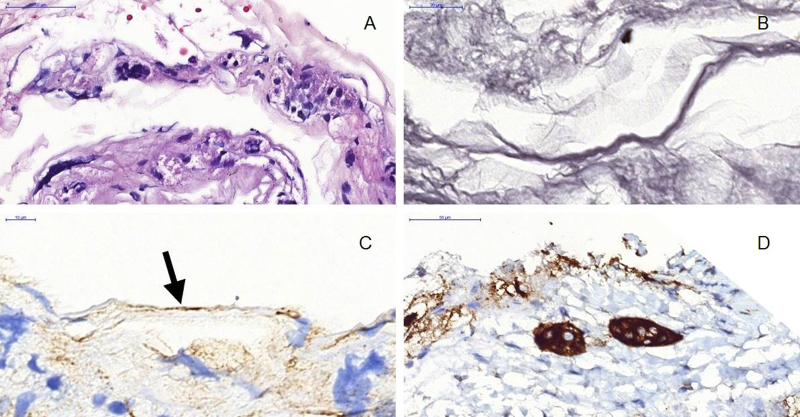
On pathologic examination, monolayered and flattened meningothelial cap cells were observed in the fibrous cyst wall (Fig. 3A). The subepithelial stroma was composed of a thin, non-vascular connective tissue rich in reticulin fibers (Fig. 3B). Perilesional anterior hypophyseal cells were present. Immunohistochemically overlying cells revealed, EMA positivity (Fig. 3C), while GFAP, Ki-67, synaptophysin, S-100 were negative. The anterior hypophyseal cells were observed Pan-ck (5/6/8/18) and synaptophysin (Fig. 3D) positive. Thus, the histological examination established a diagnosis of arachnoid cyst.
Fig. 3.
Histopathology and immunohistochemistry. A: Flattened arachnoid cells lined on thin basement membrane (H&E, x59.7). B: Basement membrane rich in reticulin fibers in cyst wall (Gomori’s reticulum stain, x113.2). C: Cyst wall overlined by flattened arachnoidal cells reacting with EMA (arrow) (Biotinylated streptavidin complement, EMA, x127.5) D: Anterior pituitary cell cluster in close neighbourhood of cyst wall (Biotinylated streptavidin complement, Synaptophysin, x61.0).
The patient was discharged on the postoperative fourth day with no complications and morbidity. In his neurosurgical and endocrinological follow-up of 1 year, no abnormality was observed.
3. Discussion
The pathophysiology of the development of IACs remains controversial. It has been suggested that IACs result from a defective diaphragma sellae through which basal arachnoid membrane herniates. This defect may close as a result of meningitis, hemorrhage, or inflammatory event creating a non-communicating cyst [11], [16]. Meyer et al. proposed that the IACs develop between the arachnoid layers as other intracranial ACs. This diverticulum would either originate above the diaphragm and expand through its aperture or develop from a subdiaphragmatic arachnoid layering [17].
IACs clinically resemble that of a nonfunctional pituitary adenoma. Compared to other intracranial ACs, IACs present at older ages. Headache and visual disturbances are the most commonly presenting symptoms associated with IACs. Headaches may result from dura distension, while compression of optic chiasm leads to visual symptoms. Endocrine symptoms are observed to be less common, mostly involving gonadotrophic axis [7], [11], [14]. Our case presented with headache with no accompanying endocrinological complaints and signs.
As described by Elliot et al. suprasellar ACs are characterized by a pure cystic lesion with no contrast enhancement and calcification with a typical CSF-like signal behavior, that is a hypointense T1-weighted signal and a hyperintense T2-weighted signal on the MRI images [18]. Complementary to this, MRI findings showing a cystic intrasellar lesion with suprasellar extension, a balloon-shape, regular, isoor slightly hyper-intense to CSF, molding but no invasion to cavernous sinus may suggest a diagnosis of IAC [8], [11]. MRI findings were consistent with these features except the rim like contrast enhancement in our patient. However this finding was thought to be stretched, normal pituitary gland in our case. Rim like enhancement of the cyst wall was specifically reported in conjunction with Rathke’s cleft cysts and craniopharyngiomas [7], [18], [19]. In addition, both RCCs and craniopharyngiomas may show calcification. Solid, contrast-enhancing parts within the cyst are typical features of craniopharyngioma [9], [17]. Moreover the cystic fluid was of slightly higher intensity than CSF and isointense with CSF on T1- and T2-weighted sequences, respectively. This finding was thought to be caused by an elevated protein concentration in the fluid and has already been pointed out by previous publications [11], [17].
Arachnoid cysts are lined by one or several layers of nonciliated meningothelial cells. Rengachary and Watanabe described the structural features of arachnoid cysts after review of several hundred cases: (1) splitting of the arachnoid membrane at the margin of the cyst; (2) thickened collagen layer in the cyst wall; (3) absence of normal arachnoid trabeculations within the cyst; and (4) hyperplastic arachnoid cells in the cyst wall [15].
Immunohistochemical marker studies have been helpful in differentiating arachnoid cysts from epithelial cysts, a distinction that is sometimes difficult to achieve by routine light microscopy. Arachnoid cysts are positive for EMA, but are negative for cytokeratins, GFAP, S-100 protein, transthyretin, and CEA [20]. According to pathologic and immunohistochemical findings, the diagnosis was established as arachnoid cyst.
Surgical treatment indications of IACs are the same for a non-secreting adenoma i.e. pituitary dysfunction, signs of compressions and severe headaches. Transcranial or, more widely used transsphenoidal route can be used to establish the diagnosis and remove the lesion (Table 1). For the diagnosis and relief of the optochiasmatic compression, patient was operated through transsphenoidal approach without postoperative complications and recurrence on follow-up.
Table 1.
Studies and case reports of sellar arachnoid cysts.
| Authors | Case No | No of cases |
Mean Age (Yrs) | Sex | Surgical approach | Complications | Recurrence |
|---|---|---|---|---|---|---|---|
| Benedetti et al. [24] | 1 2 |
1 1 |
35 65 |
M M |
Subfrontal Subfrontal |
None | No recurrence at 12 months No recurrence at 6 m |
| Leo et al. [25] | 3 | 1 | 49 | F | Microscopic TS | Pituitary abscess at 3 weeks | Death |
| Harter et al. [26] | 4 | 1 | 60 | F | Microscopic TS | None | No recurrence at 8 months |
| Spaziente et al. [27] | 5 6 7 |
3 | 24 69 42 |
M M F |
Microscopic TS Microscopic TS Microscopic TS |
Blindness that required 2.operation None CSF leak&meningitis |
NA NA NA |
| Baskin et al. [28] | 8–15 | 8 | 58 | M | Microscopic TS | CSF leak&meningitis required 2nd operation | NA |
| Meyer et al. [17] | 16–28 | 13 | 46 | 5 M, 8 F | Microscopic TS | Meningitis resulting in death | Mean follow-up 4.5 years with no recurrence |
| Hasegawa et al. [29] | 29 | 1 | 53 | M | Microscopic TS | CSF leak&meningitis | Recurrence at day 42 required TCS |
| Hornig and Zervas [16] | 30 | 1 | 57 | M | Microscopic TS | None | No recurrence at 6 years |
| Iida et al. [4] | 31 | 1 | 44 | M | Microscopic TS | Not mentioned | NA |
| Nomura et al. [30] | 32 | 1 | 44 | M | Microscopic TS | CSF leak&meningitis required 2nd operation | NA |
| Dietemann et al. [31] | 33 34 |
2 | 57 45 |
M F |
Microscopic TS endoscopic exploration Microscopic TS |
None None |
NA |
| Saeki et al. [5] | 35 | 1 | 50 | F | Microscopic TS | CSF leak that required 2nd operation | NA |
| Miyamoto et al. [6] | 36 37 |
1 | 59 67 |
M F |
Microscopic TS Frontotemporal Craniotomy |
None | NA NA |
| Shin et al. [9] | 38–42 | 5 | 53 ± 12 | 2 M, 3 F | Microscopic TS | None | Mean follow-up 33 ± 17 months with one recurrence at 99 months |
| Weil [2] | 43 | 1 | 74 | F | Sublabial transseptal transnasal | Not mentioned | No recurrence at 6 months |
| Murakami et al. [3] | 44 | 1 | 48 | M | Microscopic TS | None | Recurrence at 52 months |
| Yasuda et al., [32] | 45 | 1 | 57 | M | Endonasal TS | None | No recurrence at 6 months |
| Dubuisson et al. [11] | 46–54 | 9 | 45 | 5 M, 4 F | Microscopic TS | CSF leak in 2 patients that required reoperation | No recurrence at a mean of 11 years |
| Cavallo et al. [10] | 55–64 | 10 | 48.6 | 4 M, 6 F | Endoscopically assisted microscopic TS or endonasal endoscopic | CSF leak in 2 patients (one with meningitis) that required reoperation | Mean follow-up 36.9 months with one recurrence at 16 months |
| McLaughlin et al. [13] | 65–72 | 8 | 57 | 2 M, 6 F | Endoscopically assisted microscopic TS or endonasal endoscopic | None | Mean follow-up 32 months with 2 recurrences at 29 and 43 months |
| Park et al. [21] | 73 | 1 | 53 | F | Microscopic TS | CSF leak | No recurrence at 1 year |
| Shim et al. [22] | 74–79 | 6 | 2 M, 4 F | Transventricular endoscopic fenestration | No recurrence at a mean follow–up 10 months | ||
| Oyama et al. [8] | 80–85 | 6 | 59 | 3 M, 3 F | TS cyst cisternostomy with a keyhole | One transient CSF leak | No recurrence at a mean follow-up 42.2 months |
| Su et al. [23] | 86 87 88 |
1 1 1 |
64 37 53 |
F M F |
Endoscopically endonasal, cyst drainage cisternostomy |
None | Follow-up 4–50 months (mean not specified) with 1 recurrence (time not specified) |
Less than 100 IAC cases were reported in the English literature. Compared to other cystic lesions of sellar region ACs are rarely seen in this localization and should be kept in mind in the differential diagnosis of sellar cystic lesions.
References
- 1.Starkman S.P., Brown T.C., Linell E.A. Cerebral arachnoid cysts. J. Neuropathol. Exp. Neurol. 1958;17(3):484–500. doi: 10.1097/00005072-195807000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Weil R.J. Rapidly progressive visual loss caused by a sellar arachnoid cyst: reversal with transsphenoidal microsurgery. South Med. J. 2001;94(11):1118–1121. doi: 10.1097/00007611-200111000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Murakami M., Okumura H., Kakita K. Recurrent intrasellar arachnoid cyst. Neurol. Med. Chir. 2003;43(6):312–315. doi: 10.2176/nmc.43.312. [DOI] [PubMed] [Google Scholar]
- 4.Iida S., Fujii H., Tanaka Y., Hayashi S., Nagareda T., Moriwaki K. An intrasellar cystic mass and hypopituitarism. Postgrad. Med. J. 1996;72(849):441–442. doi: 10.1136/pgmj.72.849.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saeki N., Tokunaga H., Hoshi S., Sunada S., Sunami K., Uchino F., Yamaura A. Delayed postoperative CSF rhinorrhea of intrasellar arachnoid cyst. Acta Neurochir. (Wien) 1999;141(2):165–169. doi: 10.1007/s007010050281. [DOI] [PubMed] [Google Scholar]
- 6.Miyamoto T., Ebisudani D., Kitamura K., Ohshima T., Horiguchi H., Nagahiro S. Surgical management of symptomatic intrasellar arachnoid cysts–two case reports. Neurol. Med. Chir. 1999;39(13):941–945. doi: 10.2176/nmc.39.941. [DOI] [PubMed] [Google Scholar]
- 7.Shim K.W., Park E.K., Lee Y.H., Kim S.H., Kim D.S. Transventricular endoscopic fenestration of intrasellar arachnoid cyst. Neurosurgery. 2013;72(4):520–528. doi: 10.1227/NEU.0b013e318282a6e3. [DOI] [PubMed] [Google Scholar]
- 8.Oyama K., Fukuhara N., Taguchi M., Takeshita A., Takeuchi Y., Yamada S. Transsphenoidal cyst cisternostomy with a keyhole dural opening for sellar arachnoid cysts: technical note. Neurosurg. Rev. 2014;37(2):261–267. doi: 10.1007/s10143-013-0496-4. [DOI] [PubMed] [Google Scholar]
- 9.Shin J.L., Asa S.L., Woodhouse L.J., Smyth H.S., Ezzat S. Cystic lesions of the pituitary: clinicopathological features distinguishing craniopharyngioma, Rathke's cleft cyst, and arachnoid cyst. J. Clin. Endocrinol. Metab. 1999;84(11):3972–3982. doi: 10.1210/jcem.84.11.6114. [DOI] [PubMed] [Google Scholar]
- 10.Cavallo L.M., Prevedello D., Esposito F., Laws E.R., Jr., Dusick J.R., Messina A., Jane J.A., Jr., Kelly D.F., Cappabianca P. The role of the endoscope in the transsphenoidal management of cystic lesions of the sellar region. Neurosurg. Rev. 2008;31(1):55–64. doi: 10.1007/s10143-007-0098-0. [DOI] [PubMed] [Google Scholar]
- 11.Dubuisson A.S., Stevenaert A., Martin D.H., Flandroy P.P. Intrasellar arachnoid cysts. Neurosurgery. 2007;61(3):505–513. doi: 10.1227/01.NEU.0000290896.69825.40. [DOI] [PubMed] [Google Scholar]
- 12.Al-Holou W.N., Terman S., Kilburg C., Garton H.J., Muraszko K.M., Maher C.O. Prevalence and natural history of arachnoid cysts in adults. J. Neurosurg. 2013;118(2):222–231. doi: 10.3171/2012.10.JNS12548. [DOI] [PubMed] [Google Scholar]
- 13.McLaughlin N., Vandergrift A., Ditzel Filho L.F., Shahlaie K., Eisenberg A.A., Carrau R.L., Cohan P., Kelly D.F. Endonasal management of sellar arachnoid cysts: simple cyst obliteration technique. J Neurosurg. 2012;116(4):728–740. doi: 10.3171/2011.12.JNS11399. [DOI] [PubMed] [Google Scholar]
- 14.Iqbal J., Kanaan I. Al Homsi M Non-neoplastic cystic lesions of the sellar region presentation, diagnosis and management of eight cases and review of the literature. Acta Neurochir. (Wien) 1999;141(4):389–397. doi: 10.1007/s007010050315. [DOI] [PubMed] [Google Scholar]
- 15.Rengachary S.S., Watanabe I. Ultrastructure and pathogenesis of intracranial arachnoid cysts. J. Neuropathol. Exp. Neurol. 1981;40(1):61–83. [PubMed] [Google Scholar]
- 16.Hornig G.W., Zervas N.T. Slit defect of the diaphragma sellae with valve effect: observation of a slit valve. Neurosurgery. 1992;30(2):265–267. doi: 10.1227/00006123-199202000-00022. [DOI] [PubMed] [Google Scholar]
- 17.Meyer F.B., Carpenter S.M., Laws E.R., Jr. Intrasellar arachnoid cysts. Surg. Neurol. 1987;28(2):105–110. doi: 10.1016/0090-3019(87)90081-4. [DOI] [PubMed] [Google Scholar]
- 18.Elliott R.E., Tanweer O., Rubin B.A., Koslow M., Mikolaenko I., Wisoff J.H. Suprasellar hamartoma and arachnoid cyst. World Neurosurg. 2013;80(6):e401–e407. doi: 10.1016/j.wneu.2012.01.058. [DOI] [PubMed] [Google Scholar]
- 19.Bender B., Honegger J.B., Beschorner R., Ernemann U., Horger M. MR imaging findings in colloid cysts of the sellar region: comparison with colloid cysts of the third ventricle and Rathke’s cleft cysts. Acad. Radiol. 2013;20(11):1457–1465. doi: 10.1016/j.acra.2013.08.014. [DOI] [PubMed] [Google Scholar]
- 20.Gregory Fuller N., Arie Perry . Practical Surgical Neuropathology: A Diagnostic Approach. In: Gregory Fuller N., Arie Perry, editors. Churchill Livingstone/Elsevier; Philadelphia: 2010. pp. 287–313. [Google Scholar]
- 21.Park K.H., Gwak H.S., Hong E.K., Lee S.H. Inflamed symptomatic sellar arachnoid cyst: case report. Brain Tumor Res. Treat. 2013;1(1):28–31. doi: 10.14791/btrt.2013.1.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shim K.W., Park E.K., Lee Y.H., Kim S.H., Kim D.S. Transventricular endoscopic fenestration of intrasellar arachnoid cyst. Neurosurgery. 2013;72(4):520–528. doi: 10.1227/NEU.0b013e318282a6e3. [DOI] [PubMed] [Google Scholar]
- 23.Su Y., Ishii Y., Lin C.M., Tahara S., Teramoto A., Morita A. Endoscopic transsphenoidal cisternostomy for nonneoplastic sellar cysts. Biomed. Res. Int. 2015;2015:389474. doi: 10.1155/2015/389474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Benedetti A., Carbonin C., Colombo F. Possible aetiopathogenetic correlation between primary empty sella and arachnoid cyst. Acta Neurochir. (Wien) 1977;38(3):269–278. doi: 10.1007/BF01401097. [DOI] [PubMed] [Google Scholar]
- 25.Leo J.S., Pinto R.S., Hulvat G.F., Epstein F., Kricheff I.I. Computed tomography of arachnoid cysts. Radiology. 1979;130:675–680. doi: 10.1148/130.3.675. [DOI] [PubMed] [Google Scholar]
- 26.Harter L.P., Silverberg G.D., Brant-Zawadzki M. Intrasellar arachnoid cyst: case report. Neurosurgery. 1980;7:387–390. doi: 10.1227/00006123-198010000-00013. [DOI] [PubMed] [Google Scholar]
- 27.Spaziante R., Cirillo S., Constans J.P., de Divitiis E., Donzelli R., Stella L. Arachnoid cyst of the quadrigeminal cistern. Neurochirurgia. 1986;29:117–123. doi: 10.1055/s-2008-1054152. [DOI] [PubMed] [Google Scholar]
- 28.Baskin D.S., Wilson C.B. Transsphenoidal treatment of non-neoplastic intrasellar cysts. A report of 38 cases. J. Neurosurg. 1984;60(1):8–13. doi: 10.3171/jns.1984.60.1.0008. [DOI] [PubMed] [Google Scholar]
- 29.Hasegawa M., Yamashima T., Yamashita J., Kuroda E. Symptomatic intrasellar arachnoid cyst: case report. Surg. Neurol. 1991;35:355–359. doi: 10.1016/0090-3019(91)90044-a. [DOI] [PubMed] [Google Scholar]
- 30.Nomura M., Tachibana O., Hasegawa M., Kohda Y., Nakada M., Yamashima T., Yamashita J., Suzuki M. Contrast-enhanced MRI of intrasellar arachnoid cysts: relationship between the pituitary gland and cyst. Neuroradiology. 1996;38(6):566–568. doi: 10.1007/BF00626100. [DOI] [PubMed] [Google Scholar]
- 31.Dietemann J.L., Guessoum M., Schultz A., Zollner G., Sanoussi S., Maitrot D., Buchheit F. Intrasellar arachnoid cysts: computed tomography and MRI. Apropos of 2 cases. J. Neuroradiol. 1997;24(2):168–173. [PubMed] [Google Scholar]
- 32.Yasuda K., Saitoh Y., Okita K., Morris S., Moriwaki M., Miyagawa J., Yoshimine T. Giant intrasellar arachnoid cyst manifesting as adrenal insufficiency due to hypothalamic dysfunction—case report. Neurol. Med. Chir (Tokyo) 2005;45:164–167. doi: 10.2176/nmc.45.164. [DOI] [PubMed] [Google Scholar]