Abstract
Background
Urban children represent a group at high risk for asthma development and adverse asthma outcomes. Although rural children also encounter sociodemographic disparities that might be expected to worsen asthma, asthma in the rural US is poorly studied.
Objectives
To determine rural-urban differences in childhood asthma diagnosis and morbidity.
Methods
We studied a statewide population of 117,080 children continuously enrolled in Tennessee Medicaid from birth through the sixth year of life, using linked Tennessee Medicaid, vital records, and pharmacy claims databases to determine asthma diagnosis and residence.
Results
The cohort was 45% urban, 23% suburban, and 33% rural. Compared with urban children, rural children were more likely to be white, have a history of bronchiolitis, and have mothers who smoked. Eleven percent of urban, 12% of suburban, and 13% of rural children met study criteria for asthma diagnosis (adjusted odds ratio [OR] for rural children 1.16, 95% confidence interval [CI] 1.09–1.24, and for suburban children adjusted OR 1.22, 95% CI 1.14–1.30, with urban as referent, P<0.001). Rural children had greater utilization of outpatient asthma care, whereas urban children had greater utilization of inhaled corticosteroids. Compared with urban children, rural children had fewer asthma ED visits, but were hospitalized for asthma at similar rates. Others markers of asthma control, including oral corticosteroid and short acting beta agonist usage, were similar between rural and urban children.
CONCLUSION
In this pediatric Medicaid population, rural children had increased asthma prevalence, similar asthma morbidity, and differences in patterns of asthma care and resource utilization compared with urban children.
Introduction
Urban children, particularly those who are members of disadvantaged minority groups, are well understood to represent a group with high asthma prevalence and increased asthma morbidity.1–3 In contrast, little information about the burden of asthma among rural children is available, even though 21% of the US population lives in rural areas4, and residents of the rural US encounter many of the same socioeconomic disparities seen in inner city urban populations that might be expected to worsen asthma outcomes.5–6 Compared with the non-rural US population, residents of the rural US have lower median family income, lower educational attainment, a higher rate of uninsurance, greater reliance on government insurance programs when insured, and a lower supply of physicians, particularly subspecialists, per capita.5–6 Asthma prevalence and morbidity are directly proportional to poverty independent of race7–11, and indeed, in Tennessee, both poverty and yearly hospitalization rates for asthma are increased in rural counties compared with urban and suburban counties.4 A rural, poor, heavily African-American cohort of children in Arkansas was found to have a high asthma prevalence (28%), among whom 79% had persistent asthma symptoms.12 A comparison of rural and urban schoolchildren in Arkansas revealed similar asthma prevalence by residence, but increased prevalence of symptoms of uncontrolled asthma among the rural children.13 An analysis of hospital discharge information from Mississippi found an increased rate of emergency department care and hospitalization for asthma among residents of the rural Mississippi delta compared with metropolitan Jackson, and this difference persisted after controlling for covariates.14
However, there are few additional published studies comparing health outcomes for asthma in rural versus urban US populations, even though residents of the rural US represent a disadvantaged, medically underserved population5–6 that might be expected to have differences in asthma outcomes and healthcare utilization. We hypothesized t hat rural children represent a group with significant asthma prevalence and morbidity, and different patterns of healthcare resource utilization based on available services. To address this question, we studied 117,080 children born between 1995 and 2000 who were enrolled continuously in Tennessee Medicaid until age 5.5, to determine the prevalence of asthma in rural versus urban children in this cohort; furthermore, among those children with asthma, we identified differences in outpatient care utilization and adverse asthma outcome measures.
Methods
This is a population based birth cohort study of 117,080 children born in Tennessee between 1995–2000 continuously enrolled in TennCare (Tennessee Medicaid) until age 5.5 years, with no more than 60 days of non-enrollment between age 3.5–5.5. This cohort represented approximately 25% of all live births in Tennessee during the study period.15
Linked Tennessee Medicaid database, pharmacy, and vital records files were used to obtain data on maternal and child demographics, atopic disease diagnosis, and medication usage. Using the child’s county of residence and the current Office of Management and Budget classification of counties16, children were classified as urban (residing in a central county within one of Tennessee’s four standard metropolitan statistical areas [SMSAs]), suburban (residing in a non-central county within an SMSA), or rural (residing in a county outside of an SMSA).
For mothers of children in the cohort who were also enrolled in TennCare, maternal asthma was determined utilizing an algorithm that incorporates capture of International Classification of Diseases revision 9 (ICD-9) diagnosis 493 for hospital care and outpatient visits, as well as asthma medication utilization, as has been previously described.17
For children in the study, the prevalence of asthma was determined from age 4–5.5 years. An 18-month window was chosen to capture at least one well visit for minimally symptomatic children presenting once a year for routine preventive care to their physician. Asthma diagnosis was defined using a validated algorithm18 that required an ICD-9 diagnosis of 493 in any field for outpatient, emergency room, or inpatient care, or usage of one or more asthma specific anti inflammatory medications. This algorithm has been shown to be 90% sensitive and 95% specific for identifying asthma compared with a gold standard of known physician diagnosis.18 Allergic rhinitis was defined by the presence of one or more ICD-9 diagnoses, and atopic dermatitis by the presence of 2+ ICD-9 diagnoses, from age 3.5–5.5. Other illnesses and co-morbidities were determined using ICD-9 codes, including infant bronchiolitis, which was defined by the presence of ICD-9 codes 466.1 and/or 480.1 during the first year of life, or after the first year of life, if the appropriate ICD-9 diagnosis was present on a day when an ICD-9 diagnosis for asthma was not also submitted. Chronic comorbidities, including congenital heart, lung, and airway abnormalities, cystic fibrosis, diabetes, chronic kidney disease, neuromuscular disorders, and immunodeficient states were determined by ICD-9 codes submitted during the first 3.5 years of life.
To assess utilization of outpatient healthcare, the number of outpatient visits children with asthma made for any reason was determined. Also, outpatient visits for asthma care were identified, and pharmacy claims data were used to determine filling of inhaled corticosteroid prescriptions from age 4.5–5.5 (this age range was chosen to use the oldest available one year interval for each child, to minimize misclassification of childhood post-viral wheezing as asthma).
To measure asthma morbidity, yearly rates from age 4.5–5.5 of episodes of asthma care (ICD-9 493) that occurred in the emergency department (ED) or that required observation admission or inpatient hospital care were determined. Prescriptions for rescue medications (oral corticosteroids and short acting beta agonists) were determined from pharmacy claims data. The protocol was approved by the Institutional Review Boards of Vanderbilt University and the Tennessee Department of Health. Informed consent of subjects was waived since this was de-identified administrative data.
Asthma prevalence and morbidity were presented as frequency and proportion, mean and standard deviation (SD), or median and interquartile range as appropriate. Asthma morbidity variables were compared by residence status using the Kruskal-Wallis test for continuous measures and Chi-square test for proportions. The main independent variable was child residence (urban, suburban, or rural, as defined above). Outcomes included the prevalence of asthma from age 4–5.5 years by residence, and asthma morbidity as measured by acute care visits for asthma and asthma rescue medication usage. Odds ratios (ORs) were calculated to assess the association of rural versus urban residence with the outcome of asthma diagnosis at age 4–5.5 years using a multivariable logistic regression model. Separate multivariable logistic regression models were used to calculate ORs for the association of child residence with the outcomes of allergic rhinitis, eczema, and usage of any inhaled corticosteroid (ICS), oral corticosteroid, or short acting beta agonist. Separate multivariable Poisson regression analyses were performed to calculate risk ratios for the association of child residence status and the number of outpatient visits, ED visits, asthma-related inpatient and 23 hour admissions, ICS prescriptions, oral corticosteroid courses and short acting beta agonists per child. The Huber-White robust sandwich estimator was used for estimating standard errors.19 Child and maternal covariates included in adjusted statistical models were birth weight, gender, child race/ethnicity, number of siblings, history of bronchiolitis, presence of chronic conditions (listed above) that might affect measures of asthma severity, maternal smoking during pregnancy, maternal asthma (determined as discussed above), and maternal education level. Statistical analysis was performed using SAS version 9.1 (Cary, North Carolina) and R version 2.10.1 (http://www.R-project.org).
Results
A total of 117,080 children met eligibility requirements and were studied. Forty-five percent were urban, 23% suburban, and 33% rural. Key demographic features of this cohort are presented in Table 1. The majority of the urban group was African-American (69%), while the majority of the suburban and rural groups was white (73% of the suburban group and 81% of the rural group). Urban children were somewhat more likely to have low birth weight. Rural children were more likely to have a history of bronchiolitis, and their mothers were more likely to smoke and have a history of asthma. The prevalence of one or more chronic health conditions, including congenital disorders of the heart and lungs, was similar in the three groups.
Table 1.
Demographic characteristics of a birth cohort of 117,080 children born from 1995–2000 and enrolled in Tennessee Medicaid (TennCare) who were followed through the sixth year of life. Unless otherwise noted, data are presented as N (%).
| Urban, N=52168 |
Suburban, N=26493 |
Rural, N=38317 |
P value† | |
|---|---|---|---|---|
| Male sex (%) | 26608 (51) | 13447 (51) | 19830 (52) | 0.037 |
| Child race | <0.001 | |||
| White (%) | 11847 (23) | 19269 (73) | 31219 (81) | |
| African-American (%) | 36213 (69) | 5507 (21) | 4892 (13) | |
| Hispanic (%) | 1268 (2) | 458 (2) | 718 (2) | |
| Other (%) | 2840 (5) | 1259 (5) | 1488 (4) | |
| Gestational age (weeks ± SD) | 38.4 ± 2.9 | 38.7 ± 2.6 | 38.8 ± 2.6 | <0.001 |
| Birth weight <2500 gm (%) | 7240 (14) | 2969 (11) | 4053 (11) | <0.001 |
| History of 1+ chronic medical conditions other than asthma* (%) |
3248 (6) | 1859 (7) | 2442 (6) | <0.001 |
| History of bronchiolitis before age 1 (%) | 9057 (17) | 5317 (20) | 8527 (22) | <0.001 |
| Maternal cigarettes/day during pregnancy |
<0.001 | |||
| Non-smoker (%) | 43225 (83) | 17261 (66) | 24707 (65) | |
| <10 (%) | 2713 (5) | 1939 (7) | 2560 (7) | |
| ≥10 (%) | 5961 (11) | 7063 (27) | 10787 (28) | |
| Maternal education | <0.001 | |||
| <12 years (%) | 23173 (45) | 11287 (43) | 17065 (45) | |
| 12 years (%) | 21699 (42) | 11935 (45) | 17680 (46) | |
| >12 years (%) | 7191 (14) | 3242 (12) | 3493 (9) | |
| Maternal asthma (%) | 2199 (6) | 1101 (8) | 1759 (9) | <0.001 |
Chi-square test was used for comparing proportions and Kruskal-Wallis test for comparing continuous variables.
comorbid conditions in addition to asthma, including congenital heart, lung, and airway abnormalities; cystic fibrosis; diabetes; neuromuscular disorders; chronic kidney disease; immunodeficient states.
The prevalence of asthma and allergic rhinitis was higher in rural areas. Eleven percent of urban, 12% of suburban, and 13% of rural children met study criteria for asthma diagnosis from age 4–5.5 (P<0.001), while 9% of urban, 11% of suburban, and 13% of rural children met study criteria for allergic rhinitis diagnosis from age 3.5–5.5 (P<0.001). The prevalence of atopic dermatitis, defined as 2+ ICD-9 diagnoses from age 3.5–5.5, was low (1%) in all three groups.
Among the subgroup of children with prevalent asthma, several measures of outpatient healthcare utilization were examined (Table 2). From age 3.5–5.5, rural and suburban children with asthma made a greater number of total outpatient visits for any reason compared with urban children. Rural and suburban children had a similar rate of making one or more outpatient asthma visits from age 4.5–5.5 compared with urban children, and had a somewhat greater number of visits per child. In contrast, urban children were somewhat more likely to have been prescribed an inhaled corticosteroid from age 4.5–5.5 (31% of rural children, 32% of suburban children, and 35% of urban children, p<0.001). Notably, among those children who were prescribed an inhaled corticosteroid, each child only filled a median of 2 (urban children) or 1 (other children) one-month prescriptions per year.
Table 2.
Measures of outpatient and inpatient healthcare utilization and asthma morbidity among 13,775 Medicaid-enrolled children with asthma, by urban-rural residence. Means with standard deviation or medians with interquartile range are presented as appropriate. Data were determined for the 1 year age interval from 4.5-5.5 years old, except as indicated.
| Children with asthma, N=13,775 | ||||
|---|---|---|---|---|
| Urban, N=5639 |
Suburban, N=3308 |
Rural, N=4818 |
P value† | |
| Mean outpatient visits per asthmatic child for any reason, age 3.5–5.5 |
11.0 ± 8.2 | 14.6 ± 9.4 | 15.7 ± 9.9 | <0.001 |
| Children making 1+ outpatient asthma visits per year (%) |
40% | 39% | 41% | 0.520 |
| Of those making 1+ outpatient asthma visits, mean number of visits per child per year |
2.0 ± 1.5 | 2.1 ± 1.7 | 2.2 ± 1.9 | <0.001 |
| Children filling 1+ inhaled corticosteroid prescriptions per year (%) |
35% | 32% | 31% | <0.001 |
| Of those filling 1+ ICS prescriptions, median number filled per child per year |
2.0 (1.0–3.0) | 1.0 (1.0–3.0) | 1.0 (1.0–3.0) | 0.050 |
| Children making 1+ ED visits for asthma per year (%) | 29% | 23% | 20% | <0.001 |
| Among those making 1+ ED asthma visits, mean number of visits per child per year |
1.4 ± 1.0 | 1.4 ± 0.9 | 1.4 ± 0.9 | 0.072 |
| Children having 1+ 23 hour observation admissions for asthma per year (%) |
4% | 3% | 4% | 0.020 |
| Among those having 1+ 23 hour observation admissions for asthma, median number of admissions per child per year |
2.0 (1.0–3.0) | 2.0 (1.0–4.0) | 3.0 (2.0–3.0) | <0.001 |
| Children having 1+ inpatient admissions for asthma per year (%) |
6% | 5% | 6% | 0.020 |
| Among those having 1+ inpatient admissions for asthma, mean number of admissions per child per year |
1.2 ± 0.5 | 1.1 ± 0.6 | 1.1 ± 0.4 | 0.130 |
| Children having 1+ ED, 23 hour observation, or inpatient visits for asthma per year (%) |
30% | 25% | 23% | <0.001 |
| Children who filled 1+ oral corticosteroid courses per year (%) |
41% | 41% | 43% | 0.029 |
| Among those who filled 1+ oral corticosteroid courses, mean number of courses per child per year |
1.1 ± 1.0 | 1.0 ± 1.0 | 1.1 ± 1.1 | 0.098 |
| Children who filled 1+ short acting beta agonist prescriptions per year (%) |
79% | 77% | 76% | 0.006 |
| Among those who filled 1+ short acting beta agonist prescriptions, mean number of fills per child per year |
2.0 (1.0–3.0) | 2.0 (1.0–3.0) | 2.0 (1.0–3.0) | <0.001 |
Chi-square test was used for comparing proportions and Kruskal-Wallis test for comparing continuous variables.
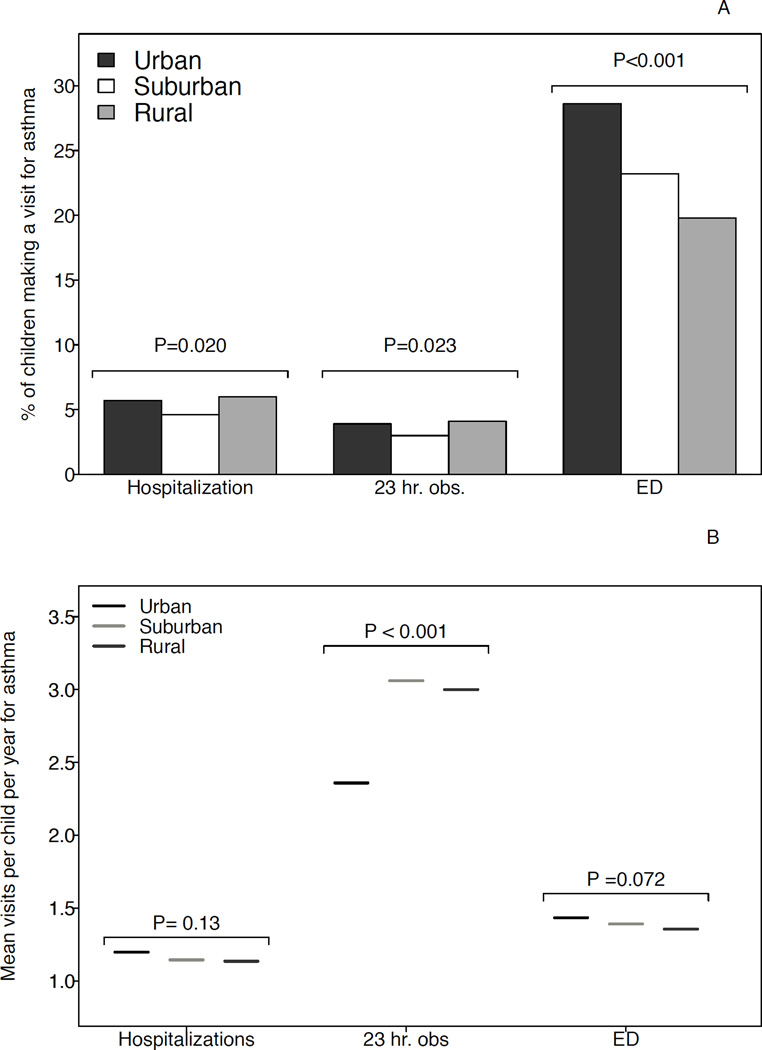
There were several differences in measures of asthma morbidity by urban-rural residence (Table 2 and Figure 1). Rural and suburban children with asthma had a lower yearly rate of making one or more emergency department visits for asthma compared with urban children. However, rural children had similar yearly rates of inpatient and observation asthma admissions, and had a larger number of asthma observation admissions per child from age 4.5–5.5, compared with urban children.
Figure 1.
Yearly episodes of acute care for asthma among 13,775 Medicaid-enrolled children with asthma, by urban-rural residence, age 4.5–5.5. Panel A: percent of asthmatic children making 1+ of each visit type for asthma-related care per year. Panel B: number of visits per child among those making 1+ visit.
All three groups had a similar yearly rate of filling one or more courses of oral rescue corticosteroids (about 40% of children in all three groups), and filled a similar number of prescriptions per child. The three groups also had a similar yearly rate of filling one or more short acting beta agonists (about 75% in each group), and filled a similar number of prescriptions per child.
In multivariable analysis (Table 3) controlling for demographic variables specific to the child (birth weight, sex, race, presence of chronic health conditions, and history of bronchiolitis) and to the mother (maternal smoking, education, and history of asthma), increased asthma prevalence in rural and suburban children persisted, as did increased allergic rhinitis in rural but not in suburban children, compared with urban as referent. Rural children, but not suburban children, had a marginally statistically significant decreased odds of receiving one or more inhaled corticosteroid prescriptions (rural versus urban, OR=0.87, 95% CI 0.77–0.99). Decreased emergency room visits among rural but not suburban children versus urban children persisted in multivariable analysis. There was no significant difference by residence in asthma-related inpatient or 23 hour observation admissions, or in utilization of short acting beta agonists or oral corticosteroids.
Table 3.
Asthma prevalence, outpatient healthcare utilization, and asthma morbidity among Medicaid-enrolled children in Tennessee. Outcomes are measured from age 4.5–5.5 unless otherwise specified.
|
Outcome, entire cohort (N=117,080) |
Suburban (N=26493) Referent: urban |
Rural (N=38317) Referent: urban |
|
|
Atopic disease prevalences |
Asthma diagnosis* | 1.22 (1.14–1.30) | 1.16 (1.09–1.24) |
| Allergic rhinitis, age 3.5–5.5* | 0.96 (0.89–1.04) | 1.14 (1.06–1.22) | |
| Atopic dermatitis, age 3.5–5.5* | 1.13 (0.90–1.43) | 1.07 (0.85–1.34) | |
|
Outcome, children with asthma (N=13,775) |
Suburban (N=3308) Referent: urban |
Rural (N=5639) Referent: urban |
|
|
Outpatient healthcare utilization |
Outpatient asthma visits per child** |
1.07 (0.96–1.20) | 1.15 (1.03–1.28) |
| ICS prescriptions, any use vs. no use* |
0.92 (0.81–1.05) | 0.87 (0.77–0.99) | |
| ICS prescriptions per child filling 1+ prescription** |
0.86 (0.73–1.00) | 0.77 (0.65–0.90) | |
|
Asthma acute care and rescue medication usage |
Rescue steroid courses, any use vs. no use* |
1.00 (0.88–1.14) | 1.09 (0.96–1.23) |
| Short acting beta agonists, any use vs. no use, age 3.5–5.5* |
0.89 (0.77–1.04) | 0.88 (0.76–1.01) | |
| ED visits for asthma per child** |
0.93 (0.82–1.07) | 0.78 (0.68–0.89) | |
| 23 hour observation admissions for asthma per child** |
1.12 (0.70–1.80) | 1.32 (0.97–1.83) | |
| Inpatient hospitalizations for asthma per child** |
0.85 (0.64–1.13) | 1.00 (0.78–1.29) | |
| Number of oral corticosteroid courses per child** |
0.99 (0.93–1.05) | 1.02 (0.96–1.08) | |
| Number of short acting beta agonist inhalers filled per child** |
0.97 (0.91–1.03) | 0.96 (0.89–1.02) |
Multiple logistic regression models were used, controlling for child birth weight, sex, race, chronic medical conditions, history of bronchiolitis, maternal smoking, maternal education, and maternal history of asthma, to calculate adjusted odds ratios and 95% confidence intervals.
Poisson regression models were used to estimate risk ratios and 95% confidence intervals controlling for the covariates mentioned above.
Discussion
Residents of the rural US face a wide variety of economic and healthcare disparities that might be expected to impact asthma outcomes, but there are few studies conducted in the US comparing either asthma prevalence or morbidity in rural versus urban populations.13–14, 20 Of these, one report used state surveillance data on asthma ED visits and therefore offers no data on prevalence14, and another was a non-peer reviewed work group report.20 This report20 analyzed Behavioral Risk Factor Surveillance System data, and found a national prevalence of self-reported asthma in urban areas of 12% versus 11% in rural areas (N=264,684, p<0.001). The present study is the first to use administrative data to compare urban and rural asthma prevalence and morbidity outcomes in a large, statewide, population-based cohort of Medicaid-enrolled children. Because 32.5% of urban children (under age 18) and 40.7% of rural children in Tennessee were enrolled in Medicaid as of 2008–2009, the study population represents a large portion of children in the state, and is likely to be similarly representative of the overall urban and rural pediatric populations in Tennessee.21Compared with urban children, rural children in this Medicaid cohort have increased asthma and allergic rhinitis prevalence, similar usage of asthma rescue medications, similar asthma hospitalization rates, and increased receipt of healthcare in the outpatient setting, underscoring the need for improved understanding of asthma management and care patterns among Medicaid-enrolled rural children, in order to improve outcomes for this high risk population of children.
Several features of the rural cohort might serve as a basis for further study regarding optimal interventions to benefit rural asthmatic children. Rural children were more likely to have smoking mothers and to have a history of bronchiolitis, both of which are associated with increased asthma risk22–23, and so efforts to reduce second hand smoke exposure and to reduce winter viral infection transmission might have a greater impact on asthma among rural children. Rural children have a higher prevalence of allergic rhinitis, and so measures to treat this condition and reduce allergen exposure may help to improve asthma control in this population. The percentage of asthmatic children filling an inhaled corticosteroid per year (which only slightly exceeded the percentage of asthmatic children who made an ED visit for asthma per year) is low, and among those who filled one or more prescriptions, who should therefore be on the medication continuously, rural children filled a median of 1 month, and urban children a median of 2 months of medication in a 1 year period. This suggests that achieving improved adherence to inhaled corticosteroids is likely to improve asthma control in this population, regardless of residence. Finally, rural children made a greater number of outpatient visits for any reason as well as for asthma, and made fewer emergency department asthma visits, compared with urban children. This difference in healthcare delivery suggests that, in rural areas, interventions to reduce asthma morbidity might be most effectively targeted to the primary care realm.
The abovementioned decreased number of asthma ED visits by rural children might have several explanations. First, this might represent a decreased frequency and/or severity of asthma exacerbations among rural children. However, the similar rate of asthma hospitalization for urban and rural children (implying that rural children are more likely to be hospitalized each time they present to the ED for asthma) argues against this (although could be explained by a lower level of comfort managing asthma among rural EDs, leading to a higher admission rate), as does the similar pattern in rescue medication usage by residence. A second explanation for decreased asthma ED visits among rural versus urban children is that urban families may have a lower threshold to present to the ED for asthma, given closer proximity and greater convenience. Indeed, the lower numbers of outpatient visits for any reason as well as for asthma among urban versus rural children suggest that for urban children, the ED may partially supplant the role of the primary care physician, as has been observed in previous studies.24–25 In contrast, rural children may be less likely to present to the ED for asthma unless truly sick, given a greater distance to travel.
We separated children into three groups, based on the Office of Management and Budget system of Standard Metropolitan Statistical Areas, which for ease of understanding we termed urban, suburban, and rural. The urban children live in urban central counties within SMSAs, the suburban children in non-central (but by definition, economically interrelated) counties within SMSAs, and the rural children in all other counties. As can be readily observed from Table 1, the demographic features of the “suburban” cohort are quite similar to those of the rural cohort. In general, Tennessee’s cities are medium sized, and counties surrounding urban counties tend to be rural. The “suburban” group, therefore, should be thought of as a rural population that has improved access to metropolitan resources compared with the “rural” group, which represents a group economically and geographically separate from the nearest cities. One related issue is that truly suburban (i.e. more advantaged) neighborhoods are located within the urban central counties, and therefore are included under the “urban” heading. However, since this is a Medicaid population, it is unlikely that many more highly advantaged children are included in the urban cohort, and therefore the observed urban asthma prevalence is unlikely to be falsely low. Other commonly used rural-urban classification systems, including urban influence codes and rural urban continuum codes, similarly divide populations at the county level. Systems that divide at the level of the census tract (e.g. rural urban commuting area) exist, but require the subject’s home address, whereas we retained only ZIP codes in our dataset. Dividing children by ZIP code would require cross-referencing with an existing classification scheme, likely one of the county-based systems (i.e. ZIP codes would be used to determine county of residence, which would be the ultimate determiner of urbanicity, and so no additional detail would be gained).26
One limitation of this study is that, like all administrative database studies, it relies on the completeness of the submitted data. For example, it seems unlikely that the observed prevalence of atopic dermatitis (1% of urban, suburban, and rural children with 2+ ICD-9 diagnoses from age 3.5–5.5) captures all children of this age with the condition; perhaps this condition is under coded when a child presents with several issues, or perhaps children with minimally symptomatic atopic dermatitis only present for their well visits and are only coded as a well visit by their pediatrician
However, this study has a number of strengths. First, the use of a Medicaid administrative database design allows us to capture a very large, statewide, population based cohort of vulnerable children, with adequate representation of patient subgroups. Secondly, there is little published information about asthma in the rural United States, and this study presents some of the first evidence for significant asthma prevalence, morbidity, and differential healthcare utilization practices in a rural versus urban US population. Future work should expand our understanding of asthma care and morbidity in the rural US and identify appropriate
Acknowledgments
The authors wish to thank the Bureau of TennCare and the Tennessee Department of Health for providing the data.
Financial disclosure: TVH received support from NIH F32 HL086048, NIH U01 HL 072471, and the Thrasher Research Fund.
Abbreviations
- ED
emergency department
- ICD-9
International Classification of Diseases revision 9
- ICS
inhaled corticosteroid
- IQR
interquartile range
- OR
odds ratio
- SD
standard deviation
- SMSA
standard metropolitan statistical area.
Footnotes
Conflicts of interest:
Robert S Valet MD: no conflict of interest to report.
Tebeb Gebretsadik MPH: no conflict of interest to report.
Kecia N. Carroll MD, MPH: no conflict of interest to report.
Pingsheng Wu PhD: no conflict of interest to report.
William D. Dupont PhD: no conflict of interest to report.
Edward F. Mitchel MS: no conflict of interest to report.
Tina V. Hartert MD, MPH: no conflict of interest to report.
References
- 1.Togias A, Fenton MJ, Gergen PJ, Rotrosen D, Fauci AS. Asthma in the inner city: the perspective of the National Institute of Allergy and Infectious Diseases. J Allergy Clin Immunol. 2010;125(3):540–544. doi: 10.1016/j.jaci.2010.01.040. [DOI] [PubMed] [Google Scholar]
- 2.Bryant-Stephens T. Asthma disparities in urban environments. J Allergy Clin Immunol. 2009;123(6):1199–1206. doi: 10.1016/j.jaci.2009.04.030. [DOI] [PubMed] [Google Scholar]
- 3.Byrd RS, Joad JP. Urban asthma. Curr Opin Pulm Med. 2006;12(1):68–74. doi: 10.1097/01.mcp.0000199001.68908.45. [DOI] [PubMed] [Google Scholar]
- 4.Valet RS, Perry TT, Hartert TV. Rural health disparities in asthma care and outcomes. J Allergy Clin Immunol. 2009;123(6):1220–1225. doi: 10.1016/j.jaci.2008.12.1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Kaiser Commission on Medicaid and the Uninsured. [Accessed November 4, 2010];Health Insurance Coverage in Rural America, Chartbook. 2003 Sep; Available at http://www.kff.org/uninsured/upload/Health-Insurance-Coverage-in-Rural-America-PDF.pdf. [Google Scholar]
- 6.United States Department of Agriculture Economic Research Service. [Accessed November 4, 2010];Rural Labor and Education: Nonmetro Education. Available at http://www.ers.usda.gov/Briefing/LaborAndEducation/education.htm.
- 7.Boudreaux ED, Emond SD, Clark S, Camargo CA., Jr Acute asthma among adults presenting to the emergency department: the role of race/ethnicity and socioeconomic status. Chest. 2003;124:803–812. doi: 10.1378/chest.124.3.803. [DOI] [PubMed] [Google Scholar]
- 8.Lynd LD, Sandford AJ, Kelly EM, Paré PD, Bai TR, Fitzgerald JM, et al. Reconcilable differences: a cross-sectional study of the relationship between socioeconomic status and the magnitude of short-acting beta-agonist use in asthma. Chest. 2004;126:1161–1168. doi: 10.1378/chest.126.4.1161. [DOI] [PubMed] [Google Scholar]
- 9.Higgins PS, Wakefield D, Cloutier MM. Risk factors for asthma and asthma severity in nonurban children in Connecticut. Chest. 2005;128:3846–3853. doi: 10.1378/chest.128.6.3846. [DOI] [PubMed] [Google Scholar]
- 10.Cesaroni G, Farchi S, Davoli M, Forastiere F, Perucci CA. Individual and area-based indicators of socioeconomic status and childhood asthma. Eur Respir J. 2003;22(4):619–624. doi: 10.1183/09031936.03.00091202. [DOI] [PubMed] [Google Scholar]
- 11.Basagaña X, Sunyer J, Kogevinas M, Zock JP, Duran-Tauleria E, Jarvis D, et al. Socioeconomic status and asthma prevalence in young adults: the European Community Respiratory Health Survey. Am J Epidemiol. 2004;160(2):178–188. doi: 10.1093/aje/kwh186. [DOI] [PubMed] [Google Scholar]
- 12.Perry TT, Vargas PA, McCracken A, Jones SM. Underdiagnosed and uncontrolled asthma: findings in rural schoolchildren from the Delta region of Arkansas. Ann Allergy Asthma Immunol. 2008;101:375–381. doi: 10.1016/S1081-1206(10)60313-4. [DOI] [PubMed] [Google Scholar]
- 13.Pesek RD, Vargas PA, Halterman JS, Jones SM, McCracken A, Perry TT. A comparison of asthma prevalence and morbidity between rural and urban schoolchildren in Arkansas. Ann Allergy Asthma Immunol. 2010;104(2):125–131. doi: 10.1016/j.anai.2009.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roy SR, McGinty EE, Hayes SC, Zhang L. Regional and racial disparities in asthma hospitalizations in Mississippi. J Allergy Clin Immunol. 2010;125(3):636–642. doi: 10.1016/j.jaci.2009.11.046. [DOI] [PubMed] [Google Scholar]
- 15.Tennessee Department of Health, Health Information Tennessee website. [Accessed November 4, 2010]; Available at http://hit.state.tn.us/BirthRateDetail.aspx. [Google Scholar]
- 16.US Census Bureau. Metropolitan and micropolitan statistical areas. [Accessed November 4, 2010]; Available at: http://www.census.gov/population/www/metroareas/aboutmetro.html.
- 17.Enriquez R, Griffin MR, Carroll KN, Wu P, Cooper WO, Gebretsadik T, et al. Effect of maternal asthma and asthma control on pregnancy and perinatal outcomes. J Allergy Clin Immunol. 2007;120(3):625–630. doi: 10.1016/j.jaci.2007.05.044. [DOI] [PubMed] [Google Scholar]
- 18.Wakefield DB, Cloutier MM. Modifications to HEDIS and CSTE algorithms improve case recognition of pediatric asthma. Pediatr Pulmonol. 2006;41:962–971. doi: 10.1002/ppul.20476. [DOI] [PubMed] [Google Scholar]
- 19.Freedman DA. On the so-called “Huber Sandwich Estimator” and “Robust Standard Errors”. Am Statistician. 2006;60:299–302. [Google Scholar]
- 20.Jackson JE, Doescher MP, Hart LG. A national study of lifetime asthma prevalence and trends in metro and non-metro counties, 2000–2003. [Accessed November 4, 2010];2007 Jan; Available at: http://depts.washington.edu/uwrhrc/uploads/RHRC_WP108_Jackson.pdf. [Google Scholar]
- 21.Cecil G Sheps Center for Health Services Research. Tennessee Medicaid Profile. [Accessed October 31, 2010]; Available at: http://www.shepscenter.unc.edu/medicaidprofiles/State%20Profile_Tennessee.pdf. [Google Scholar]
- 22.Wu P, Dupont WD, Griffin MR, Carroll KN, Mitchel EF, Gebretsadik T, et al. Evidence of a causal role of winter virus infection during infancy on early childhood asthma. Am J Respir Crit Care Med. 2008;178:1123–1129. doi: 10.1164/rccm.200804-579OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martinez FD, Cline M, Burrows B. Increased incidence of asthma in children of smoking mothers. Pediatrics. 1992;89:21–26. [PubMed] [Google Scholar]
- 24.Flores G, Snowden-Bridon C, Torres S, Perez R, Walter T, Brotanek J, et al. Urban minority children with asthma: substantial morbidity, compromised quality and access to specialists, and the importance of poverty and specialty care. J Asthma. 2009;46(4):392–398. doi: 10.1080/02770900802712971. [DOI] [PubMed] [Google Scholar]
- 25.Rand CS, Butz AM, Kolodner K, Huss K, Eggleston P, Malveaux F. Emergency department visits by urban African American children with asthma. J Allergy Clin Immunol. 2000;105:83–90. doi: 10.1016/s0091-6749(00)90182-9. [DOI] [PubMed] [Google Scholar]
- 26.Hall SA, Kaufman JS, Ricketts TC. Defining urban and rural areas in U.S. epidemiologic studies. J Urban Health. 2006;83(2):162–175. doi: 10.1007/s11524-005-9016-3. [DOI] [PMC free article] [PubMed] [Google Scholar]