Abstract
Mucinous neoplasms of the urinary tract are very rare. We present a 63-year-old-women who had a sessile papillary villous tumor in urinary bladder. Although transurethral resection of the bladder tumor (TURBT) was performed, the villous tumor repetitively recurred and gradually spread to the entire surface of bladder lumen. Histopathologic and immunohistochemical examination showed that the lesion was very similar to low-grade mucinous neoplasm arising in appendix vermiformis. There are no reports on appendiceal metaplasia of urinary bladder mucosa. In this case, we describe this unprecedented neoplasm as “villous tumor of the urinary bladder resembling low-grade mucinous neoplasm of the appendix.”
Keywords: Urinary bladder tumor, Mucinous neoplasm, Villous tumor, Appendiceal-type
Introduction
Villous adenomas are benign glandular neoplasm, and rarely arise in urinary tract. Morphology of this lesion is similar to the colonic counterpart, and when the tumor is resected completely, that rarely recur.1 Here, we present a case of recurrent “villous tumor of the urinary bladder resembling low-grade mucinous neoplasm of the appendix” which was treated as villous adenoma.
Case presentation
A 63-year-old woman with sponge kidney disease and had undergone extracorporeal shock wave lithotripsy (ESWL) for several times due to nephrolithiasis. She manifested intermittent asymptomatic gross hematuria since 7 years ago. Cystoscopy showed a sessile papillary tumor covered with abundant mucus involving the left lateral wall of the urinary bladder (Fig. 1). Transurethral resection of the bladder tumor (TURBT) was performed and the tumor was resected completely.
Figure 1.
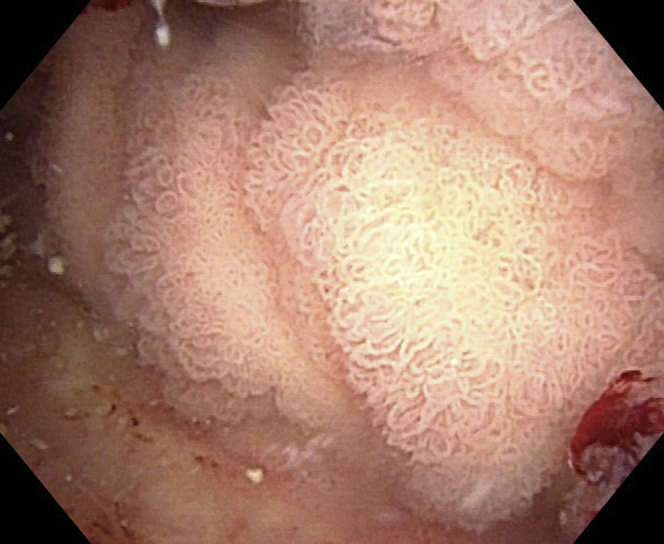
Cystoscopy showed a sessile papillary tumor covered with abundant mucus.
Histopathologic diagnosis was a villous tumor with no malignant transformation to adenocarcinoma. One year after the TURBT, cystoscopy showed the recurrence of the sessile papillary tumor spreading more than half of bladder wall. Patients underwent re-TURBT, however, tumor recurred 9 months later. Computed tomography (CT) revealed an irregular thickening of urinary bladder without any extravesical extension and distant metastasis.
On microscopic examination, the neoplasm was characterized by a papillary architecture with central fibrovascular cores. The epithelial cells displayed nuclear stratification, nuclear crowding (Fig. 2A and B). There was no appearance of submucosal invasion. Immunohistochemistry revealed that the neoplasm cells were stained strongly positive with CK7, CK20, MUC2, MUC5AC and CDX2, while MUC1, MUC6 staining was negative. Ki-67 labeling index was very high (80%), and p53 was focal positive. Cytoplasm was stained strongly positive with d-PAS and Alcian Blue. Expression of mutated protein BRAF V600E was negative, and K-RAS codon13 was positive.
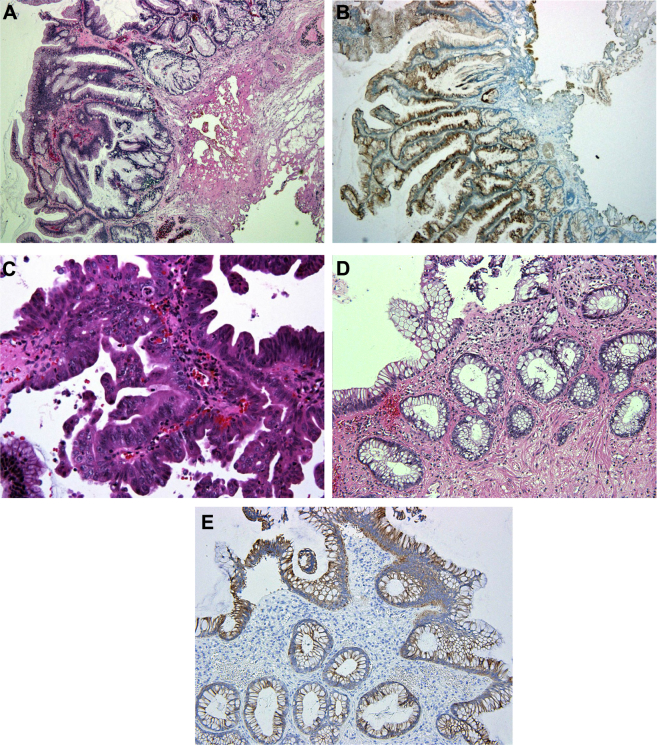
Figure 2.
Microscopic characteristics of the tumor (A–E). A) The tumor was characterized by a papillary or villous architecture (hematoxylin-eosin). B) Immunohistochemically, neoplastic cells are diffusely positive for cytokeratin 7. C) The histological examination showed the focal fusion of basement membrane. D) The histological examination of normal bladder mucosa. The mucosa is not urothelial epithelium, but resembles normal appendix or colon. E) The mucosa shows the diffuse positivity for cytokeratin 7 by immunostaining. This phenotype is uncommon in normal colonic mucosa.
Despite thorough resection of tumors at each recurrence, the neoplasm recurred and finally spread to the entire surface of bladder lumen. Histological examination of bladder tumor showed the similar nature to the previous tumors. However, the fusion of basement membrane was focally identified that suggested malignant potential of the tumor (Fig. 2C). Furthermore, biopsy specimens of normally appeared bladder mucosa which was obtained at follow-up cystoscopy showed the immunophenotype similar to normal appendix vermiformis (Fig. 2D and E).
Discussion
Villous adenomas in urinary bladder are benign glandular neoplasm, and the morphology is similar to the colonic counterpart. Although we treated this patient as villous tumor at first, the clinical course of recurrent tumor was not inconsistent with its feature. Therefore, we performed additional immunohistochemical examination; the findings were similar to those of the low-grade mucinous neoplasm of appendix.
The low-grade mucinous neoplasm arising in the appendix is also rare, and potentially malignant as the precursor to disseminated pseudomyxoma peritonei.2 We suggest that this case may be a low-grade mucinous neoplasm arising in appendiceal metaplasia of urinary bladder with following three reasons.
First, the immunohistochemistry pattern of this case; CK7+, CK20+, MUC1−, MUC2+, MUC5AC+, MUC6−, CDX2+, coincide with the pattern of five appendiceal mucinous neoplasms or normal appendiceal mucosa of these tumors3 (Table 1). The immunophenotype of colonic mucosa typically exhibits the pattern of CK7−, CK20+ and CDX2+. Additionally, only 10% of colonic adenocarcinoma shows the positivity for CK7.
Table 1.
Special stain and immunohistochemical findings of normal appendix vermiformis, five appendiceal mucinous neoplasms and villous tumor of the urinary bladder resembling low-grade mucinous neoplasm of the appendix.
| D-PAS | Alcian blue | CK7 | CK20 | MUC1 | MUC2 | MUC5AC | MUC6 | CDX2 | |
|---|---|---|---|---|---|---|---|---|---|
| Normal appendix | Cytoplasm, ++ | Cytoplasm, ++ | f+ | d+ | − | d++ | f++ | − | d++ |
| Appemdiceal mucinous neoplasm | |||||||||
| Case1 | Cytoplasm, ++ | Cytoplasm, ++ | f++ | d+ | − | d++ | d++ | − | d++ |
| Case2 | Cytoplasm, ++ | Cytoplasm, ++ | d++ | d+ | − | d++ | d++ | − | d++ |
| Case3 | Cytoplasm, ++ | Cytoplasm, ++ | f++ | d+ | − | d++ | f++ | − | d++ |
| Case4 | Cytoplasm, ++ | Cytoplasm, ++ | d+ | d+ | − | d++ | d++ | − | d++ |
| Case5 | Cytoplasm, ++ | Cytoplasm, ++ | − | d+ | − | d++ | d++ | − | d++ |
| Present tumor | Cytoplasm, ++ | Cytoplasm, ++ | d++ | d++ | − | d++ | d++ | − | d++ |
−: negative, +: positive, ++: strongly positive, f: focal, d: diffuse.
Second, the morphology and immunohistochemistry lesion of this case is not consistent with other mucinous neoplasm. Villous tumor rarely produces abundant mucin and large mucin vacuoles of columnar cells are uncommon in usual villous tumor. Undulating structure is uncommon in villous adenoma. Colonic sessile serrated adenoma/polyp (SSAP) may show the similar histological lesion. However, the boots-like dilatation of deep crypt is characteristic of SSAP and most SSAPs usually show the positive for MUC6.4 At contrast, low-grade mucinous neoplasm usually shows villous, serrated or undulating structure, often simulating adenoma. Furthermore, K-RAS mutation was positive in this case. This genetic result seems to show a close relationship to the malignant nature rather than benign tumor in this tumor, because the positive frequency of K-RAS mutation is higher in appendiceal mucinous carcinoma than appendiceal adenoma. Although colonic mucinous adenocarcinoma also produces abundant mucus, the morphology of this tumor is incompatible with typical colonic mucinous adenocarcinoma. Both cytological and structural atypia are prominent in mucinous adenocarcinoma.
Third, we performed cold punch biopsy of normal mucosa in urinary bladder. The lesion that the appendiceal metaplasia showing diffuse positivity for cytokeratin 7 was already confirmed in normal mucosa, as shown in Fig. 2D and E. It is well known that colonic metaplasia often occur in bladder mucosa. However, intestinal mucosa can occur in this site.5 Additionally, mucinous metaplasia has been previously described in urothelial tract. To the best of our knowledge, there is no description on appendiceal metaplasia of normal bladder mucosa. In conclusion, we suggest that this may be the first description of “villous tumor of the urinary bladder resembling low-grade mucinous neoplasm of the appendix.” However, it is possible that some of this tumor may have been included in the category of villous adenoma of urinary bladder. We speculate that this phenomenon may be caused by the transdifferentiation of normal bladder mucosa due to the long-term inflammatory stimulus attributed to sponge kidney and subsequent urinary tract stone.
Conclusion
Low-grade mucinous neoplasm in appendix is neither pure adenoma nor pure carcinoma but potentially malignant, because low-grade mucinous neoplasm occurring in the appendix may give rise to metastasis. In this case, in spite of focal structural atypia, no invasion to the submucosa has been showed. However, considering the significant structural atypia and RAS mutation, we regarded that the lesion should be diagnosed as potentially malignant neoplasm. Furthermore, it is possible that rupture to retroperitoneum and disseminated pseudomyxoma peritonei may occur in this patient in the future. Thus, this patient should be followed up intensively, and paid attention to the progression of true morphological malignant changes and invasive lesion.
Conflicts of interest
The authors declare that there are no conflicts of interest.
References
- 1.Cheng L., Ayala A.G. IARC; Lyons: 2004. Villous adenoma. WHO Classification of Tumors. Pathology & Gentics. Tumors of the Urinary System and Male Genital Organs; p. 134. [Google Scholar]
- 2.Misdraji J. Appendiceal mucinous neoplasm. Arch Pathol Lab Med. 2010;134:864–870. doi: 10.5858/134.6.864. [DOI] [PubMed] [Google Scholar]
- 3.Yajima N., Wada R., Yamagishi S. Immunohistochemical expressions of cytokeratins, mucin core proteins, and neuroendocrine cell markers in epithelial neoplasm of appendix. Hum Pathol. 2005;36:1217–1225. doi: 10.1016/j.humpath.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 4.Kabbani W., Houlihan P.S., Luthwa R. Mucinous and nonmucinous appendiceal adenocarcinomas: different clinicopathological features but similar genetic alterations. Mod Pathol. 2002;15:599–605. doi: 10.1038/modpathol.3880572. [DOI] [PubMed] [Google Scholar]
- 5.Clouston D., Lawrentschuk N. Metaplastic conditions of the bladder. BJU Int. 2013;112:27–31. doi: 10.1111/bju.12378. [DOI] [PubMed] [Google Scholar]