Abstract
Aim:
To assess the level of adherence to diabetes care processes, and associated clinic and patient factors at general practices in Delhi, India.
Methods:
We interviewed physicians (n = 23) and patients with diabetes (n = 406), and reviewed patient charts at general practices (government = 5; private = 18). We examined diabetes care processes, specifically measurement of weight, blood pressure (BP), glycated hemoglobin (HbA1c), lipids, electrocardiogram, dilated eye, and a foot examination in the last one year. We analyzed clinic and patient factors associated with a number of care processes achieved using multilevel Poisson regression model.
Results:
The average number of clinic visits per patient was 8.8/year (standard deviation = 5.7), and physicians had access to patient's previous records in only 19.7% of patients. Dilated eye exam, foot exam, and electrocardiogram were completed in 7.4%, 15.1%, and 29.1% of patients, respectively. An estimated 51.7%, 88.4%, and 28.1% had ≥1 measurement of HbA1c, BP, and lipids, respectively. Private clinics, physician access to patient's previous records, use of nonphysicians, patient education, and the presence of diabetes complication were positively associated with a number of care processes in the multivariable model.
Conclusion:
Adherence to diabetes care processes was suboptimal. Encouraging implementation of quality improvement strategies like Chronic Care Model elements at general practices may improve diabetes care.
Keywords: Diabetes, India, primary care, quality of care
INTRODUCTION
Strong evidence has shown that controlling risk factors reduce complications among people with diabetes.[1,2,3,4,5,6,7] The evidence is clearly conveyed in clinical practice guidelines recommended by professional organizations such as the American Diabetes Association (ADA),[8] the International Diabetes Federation,[9] and others that set the standard for assessing the quality of care delivery and outcomes among patients. Implementing these guidelines in real life with complex health care systems is a challenge but doable. Undertaking processes of care (monitoring metabolic markers and screening for complications) may be an important step in the pathway to better diabetes management. Data from countries such as the United States and the United Kingdom suggest that measuring the quality of care – both processes and risk factor control – and implementing approaches to deliver high-quality care can improve diabetes processes and outcomes.[10,11,12]
Such data are scarce in India, which is home to 66.8 million individuals with diabetes mellitus.[13] Most of these individuals are young- or middle-aged[14] and unless managed efficiently are at risk for devastating complications of diabetes and premature mortality.[15] Further, the majority of people with diabetes in India are managed by general practitioners or nonspecialists. For example, a survey of middle- and high-income residents of Delhi reported that 80% of patients with diabetes are managed by nonspecialists.[16] Assessments of the quality of care delivered in these settings help to identify care gaps and promotes accountability such that strategies for improvement are considered and achieved in the long-term. Documenting the current status of diabetes care using clinic audits or surveys is the necessary first step. The DiabCare India cross-sectional studies in 2001 and 2011 documented inadequate control of risk factors at specialist centers.[17] However, there is a little knowledge regarding diabetes care at general practices in India, and less documented evidence regarding process measures.
As a start, we surveyed 23 primary care clinics providing care to patients with diabetes in National Capital Region-Delhi (NCR-Delhi) to document processes of diabetes care. We also aimed to identify clinic and patient factors associated with achievement of care processes.
METHODS
Recruitment
We recruited general practitioners practicing in NCR-Delhi who voluntarily enrolled in a Certificate Course in Evidence Based Diabetes Care (CCEBDM) at the Public Health Foundation of India (PHFI) in 2011 and 2012. The details of CCEBDM are provided in Box 1. We included physicians who were providing outpatient care to patients with diabetes ≥1 year; do not hold a specific qualification in diabetes (such as diploma or degree in endocrinology or diabetes); whose clinics had at least 20% of the patients with diabetes (as reported by physicians themselves); and consented to participate in the study. We excluded physicians practicing in a setting which included a specialist in diabetes.
Box 1.
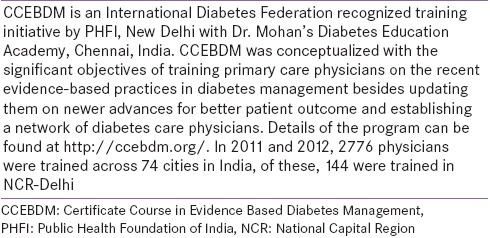
Certificate Course in Evidence Based Diabetes Management
From each clinic, up to 20 consecutive patients with diagnosed diabetes were recruited for the study. Patients were eligible for inclusion if: Diagnosed with diabetes for ≥1 year, treated for diabetes at the same clinic for ≥1 year, and consented to participate in the study.
Measures
We used study tools from the Translating Research Into Action for Diabetes (TRIAD) study, a multicenter study of diabetes in managed care in the United States.[18] In addition to chart reviews as in TRIAD study, we also used patient questionnaire to obtain data on diabetes care processes.
We interviewed the physicians and collected personal details (age, sex, professional degrees, and experience), and clinic characteristics (government/private, cluster visits for diabetes [a specific day or time of the week in the clinic when only patients with diabetes are treated], availability of specialists, laboratory, record system, involvement of nonphysicians, and presence of diabetes education facilities).
Patients were interviewed either in the clinic waiting area or another room (based on facility available) before they met the physician. The questionnaire included demographic characteristics, duration of diabetes, comorbidities and complications, whether they had tests to screen for diabetes complications (dilated eye examination, foot examination, electrocardiogram, weight measurement, fasting plasma glucose [FPG]/random plasma glucose [RPG], glycated hemoglobin [HbA1c], blood pressure [BP], and serum lipids) in the past year and if they had the total number of tests in that period. The tests were described to the patients in common words for better understanding [Box 2]. The reported data were cross-verified with patient latest records whenever available. In addition, values of risk factors (HbA1c, BP, and lipids) were also noted from the patient records available with patients or clinic. In the case, these records were not available in the clinic or with patient at the time of visit, we either requested patients to bring the record from home or the study coordinator visited the homes of the patients (if they consented) to obtain these records. After several attempts to obtain the information of risk factor control, we could access 82–93% records of (FPG - 82%, HbA1c - 84%, lipids - 84%, and BP - 93%) of measurements that patient reported they had undergone in last 1 year.
Box 2.
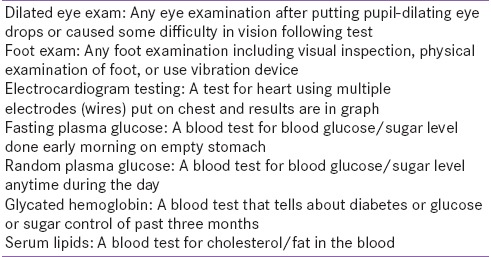
Explanations for the tests
We defined “physician's access to patient's record during current visit,” as positive if either the patient carried or the clinic maintained at least one previous record of diabetes prescription and laboratory values during the current visit. We considered seven process quality indicators, three monitoring indicators (dilated eye exam, foot exam, and electrocardiography [ECG]), and four risk factor measurements (HbA1c, BP, lipids, and body weight).[19] We defined adherence to each of the care processes as positive if the particular test had been done at least once in the previous year.
Ethical issues
The protocol was approved by ethics committees of Centre for Chronic Disease Control and PHFI. Written informed consent was obtained from physicians and patients with diabetes to conduct in-person interviews.
Data analysis
We used Stata version 12.1 (Serial number: 3012046778; Manufacturer: 4905 Lakeway Drive College Station, Texas 77845 USA) descriptive statistics were used to characterize clinics and patients. Means and standard deviation (SD) (median and interquartile range [IQR], if not normally distributed) were used to describe continuous variables and percentages for categorical variables.
To assess the factors associated with adherence to care processes, we used multilevel poison regression models. The outcome of interest was the number of care processes completed in last 1 year (out of seven) and patient-, physician-, and clinic-level characteristics were exposures. We used bivariate models to assess the relationships first. We used forward stepwise multivariable models with patient's age and sex as a priori exposure factors. Other variables were added to the model based on the strength of association from bivariate models, starting with the strongest. The variables were retained in the model only if it improved goodness of fit, measured by likelihood ratio test at P < 0.05.
RESULTS
Clinic level factors
Of the 144 physicians enrolled in CCEBDM (2011 and 2012 batches), 77 were practicing in specialist or tertiary care centers, and 35 practices had fewer than 20% of their patients with diabetes. Of the remaining 32 physician clinics, three were practicing outside NCR, and six did not respond to the invitation, leaving 23 physicians recruited for the study.
Five were government clinics, and 18 were private for-profit clinics. Twelve clinics had an in-house laboratory. Five had electronic records (only two clinics had database information accessible during the patient visit) and three clinics had a diabetes-specific booklet (patient record book updated at every visit). Three clinics had cluster visits for diabetes, three sent reminders to patients with diabetes when their visit or laboratory testing were due. Nine clinics either held diabetes group education classes or referred patients to such classes. Four clinics provided standardized diabetes education materials [Table 1].
Table 1.
Details of study clinics, health care personnel, and diabetes education activities
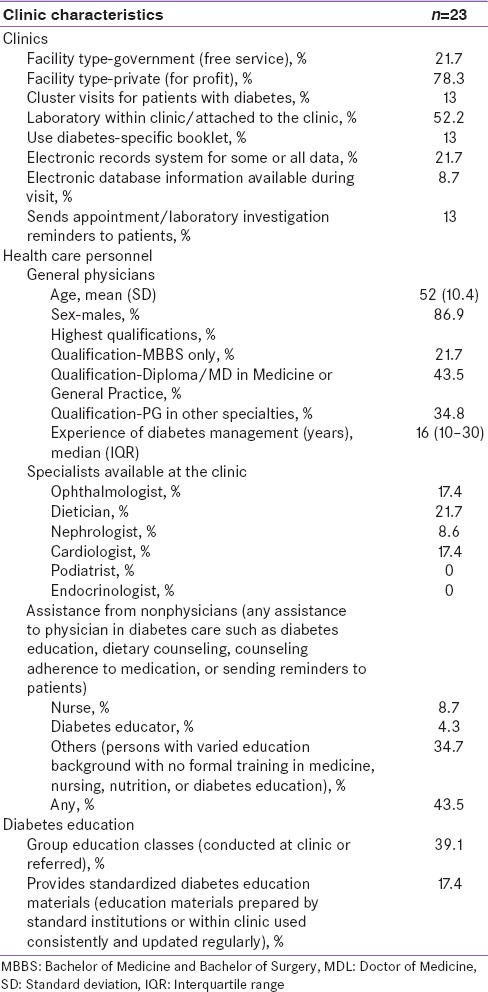
Twenty of the primary care physicians were men, and 18 had done specialization (masters’ degree or diploma) of some sort after bachelor of medicine and bachelor of surgery. Physicians had a median of 16 (range: 6–44) years of experience in managing diabetes. Ophthalmologists were available in four clinics, cardiologists in four, nephrologists in two, and dieticians in five clinics. Ten clinics had nonphysicians involved in diabetes care at some level.
Patient level factors
A total of 406 (response rate = 98.7%) patients with diabetes were recruited for the study. Fifty-one percent of the participants were men, mean age was 56.3 (SD = 11.2) years, 87.4% were married, and median duration of diabetes was seven (IQR; 3–12) years. Patients had mean schooling of 9.8 (SD = 5.6) years, 29.6% were graduates, and 37% had income ≥20,000 Indian rupees/month [Table 2].
Table 2.
Characteristics of diabetes patients recruited from general practitioner's clinics in National Capital Region-Delhi
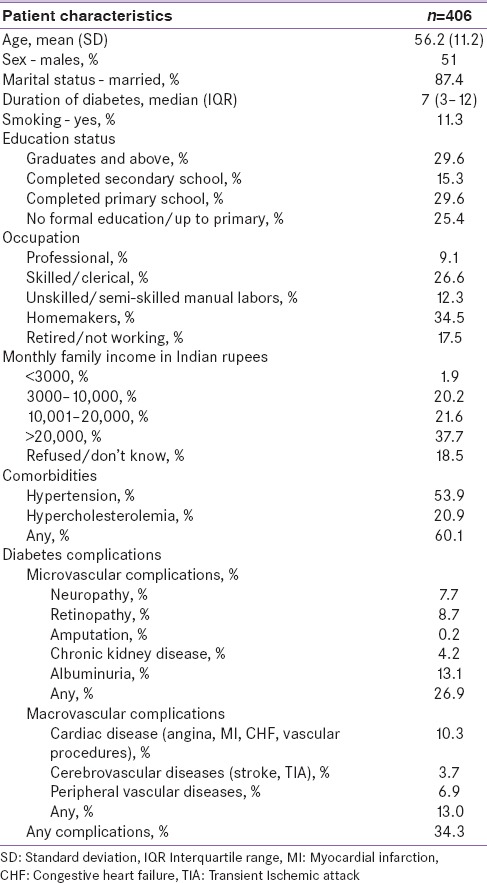
Comorbidities were present in 66.0% of patients with diabetes; hypertension was the most common and was present in 53.9%. Cardiac diseases including a history of angina, myocardial infarction, congestive heart failure, vascular procedures were present in 10% and cerebrovascular diseases including a history of transient ischemic attack or stroke in 3.7%. One or more diabetes complications-history of retinopathy, neuropathy, albuminuria or chronic kidney disease, and amputation was present in 26.8% of participants [Table 2].
Process indicators
In the preceding 12 months, patients with diabetes had an average of 8.9 (SD = 5.7) visits to outpatient clinics for diabetes; 83.9% of patients made four or more visits. However, in only 19.7% of visits did the physician have access to patient's previous records during the current visit and 13.5% had access to three or more previous records [Table 3].
Table 3.
Diabetes patients achieving targets for process indicators of diabetes care in the previous year in general practitioners clinics
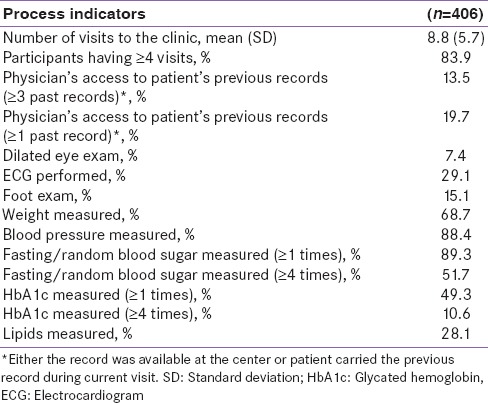
Seventy percent of patients reported that their weight was monitored in the preceding year, and 88.4% reported BP was measured. In terms of monitoring metabolic parameters, fasting/random blood sugar, HbA1c, and lipids were measured at least once in 89.3%, 49.3%, and 28.8%, respectively. In terms of annual screenings for diabetes complications, ECG was done in 29.1%, 15% had foot exams, and dilated eye examination was done in only 7.4% as reported by the patients [Table 3].
The percentage of number of processes completed in the last one year by various subgroups is provided in Table 4. In the total sample, only 0.7% of patients had undergone all seven processes in the last year while 4.7% had none. One, two, three, four, five, and six were completed in 15.5%, 27.6%, 15%, 21.7%, 10.3%, and 4.4%, respectively.
Table 4.
Percentage of diabetes patients completing processes of care* in the last 1 year
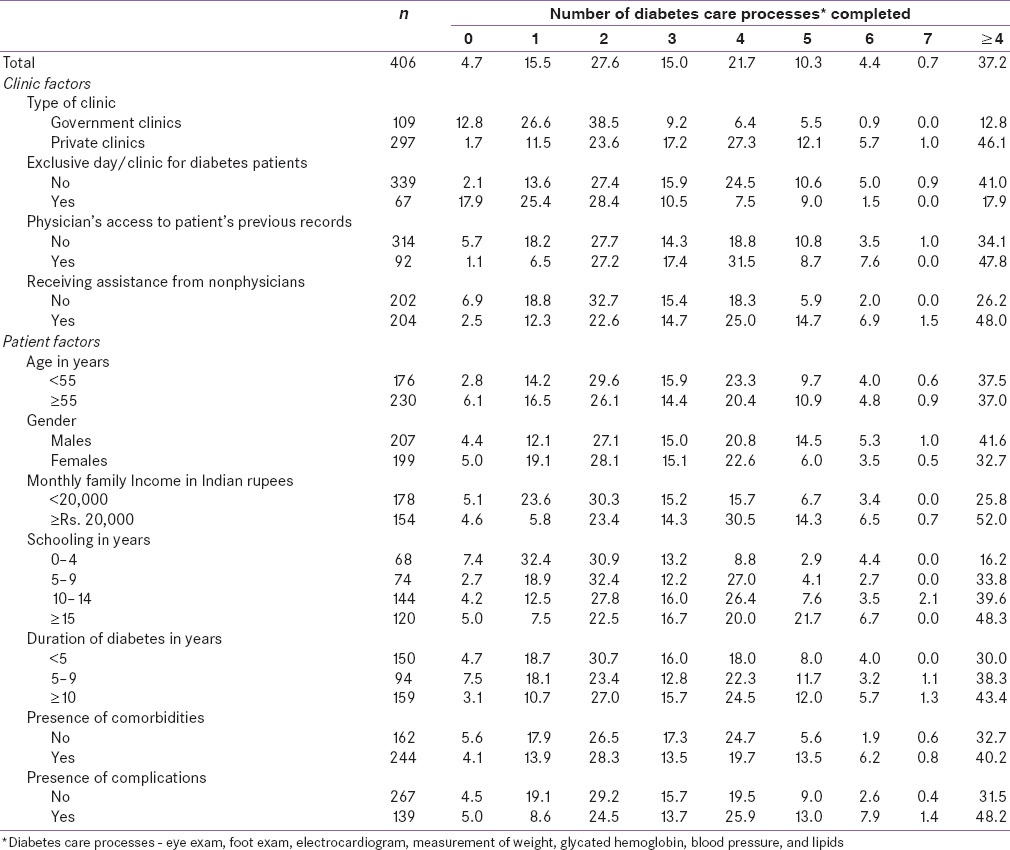
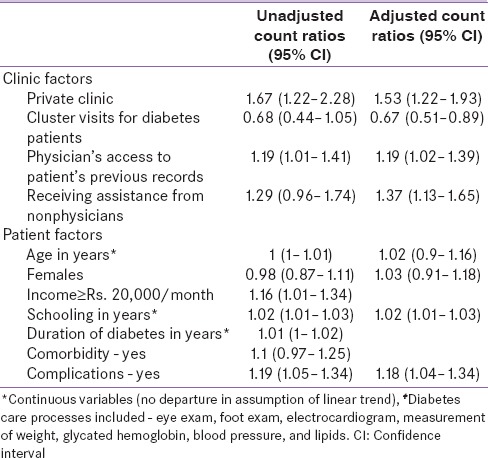
In unadjusted analysis, private for-profit clinics had a higher number of processes of care with count ratio 1.67 (95% confidence interval 1.22, 2.28) compared to government-free services clinics. Physicians’ access to patients’ previous records (count ratio 1.19 [1.01, 1.41]) and receiving assistance from nonphysicians (1.29 [0.96, 1.74]) also were associated with better process of care achievement. Patients monthly income ≥20,000 Indian rupees (1.16 [1.01, 1.34]) and having diabetes complications (1.19 [1.05, 1.34]) were significantly positively associated with the outcome. For every addition of year in schooling among patients, the number of process of care was higher by 1.02 (1.01, 1.03) times.
In multivariable analyses, private clinics, physician's access to patient's previous records, receiving assistance from nonphysicians, patient's schooling, and diabetes complications were positively associated with a number of process of care. Cluster visits for diabetes was negatively associated with the process of care with count ratio 0.67 (0.51, 0.89) [Table 5].
Table 5.
Multilevel poison regression model of factors associated with processes of care# completed in last 1 year*
Risk factor control
Among the participants whose records could be accessed, 16.8%, 39.4%, and 55.2% had achieved ADA-2012 targets for BP <130/80, glucose control (HbA1c <7%), and low-density lipoprotein cholesterol (<100 mg/dl), respectively [Supplementary Table 1 (133.7KB, tif) ].
Diabetes patients meeting risk factor control targets at general practitioners clinics in National Capital Region-Delhi
DISCUSSION
The number of people living with diabetes has reached to epidemic proportions in India. General practitioners are increasingly managing diabetes in their clinic. This study is the first to document diabetes care processes at this level and analyze how and if clinic and patient factors are associated with better care.
We found suboptimal levels of diabetes care processes at the general practitioners’ clinics in NCR-Delhi. Our findings are similar to low levels of diabetes care processes found elsewhere in low- and middle-income countries of Asia and the Middle East.[19] There is limited published literature documenting processes of care in India. The only comparable published research comes from the Delhi Diabetes Community (DEDICOM) survey, a community-based representative sample survey of diabetes quality of care from middle- and high-income residents of Delhi in 2005–2006.[16] Compared to DEDICOM, the frequency of HbA1c testing was higher in our study (13% vs. 49.3%) indicating improvements in HbA1c monitoring. We also found a higher percentage of annual foot exams (15.1%) reported compared to the DEDICOM survey (3.1%). However, this may have been because DEDICOM survey included only monofilament testing while our study assessed any physical foot exam. We found a very low frequency of dilated eye examinations (7.4%) compared to DEDICOM (16.2%). Among the patients whose data could be accessed, the risk factor control was poor except for lipids [Supplementary Table 1 (133.7KB, tif) ]. Since only lipids records were obtained from less than quarter of the patients, commenting on lipid control will be biased.
Though the average number of clinic visits was more than twice the recommended number of annual visits for people with diabetes, physicians had limited access to patients’ previous records as they were not maintained at the clinic and relied on patients to bring their own records to the clinic. This is clearly a situation where patient unreliability can affect care – more than 80% of patients did not bring previous records to the clinic. Inadequate HbA1c and lipids monitoring but reasonable frequency of FPG/RPG and BP measurements indicates that clinicians relied on tests that are available and accessible during the time of each patient's visit. The lack of access to patients’ previous records may have resulted in poor tracking of frequency of screening for complications and monitoring of risk factors. As such, for those where there was access to patients’ records, odds of receiving multiple processes doubled.
Ten out of 23 clinics used nonphysicians to assist with various aspects of diabetes care. The nature of assistance could involve helping with treatment of diabetes, patient reminders for tests, or conveying diet, and physical activity advice to patients. Clinics with nonphysician assistants in diabetes care performed better. This is similar to other studies in the United States where they found practices involving nurse practitioners in diabetes care had better HbA1c[20] compared to the physician along practices. We found a negative relation between cluster visits and care processes. This is in contrary to evidence from randomized control studies[21] where this strategy has shown to be beneficial. The reasons for this conflicting finding could not be ascertained from the current study. It is possible that cluster visits in the clinics involved in the current study were not co-occurring with group health education and interdisciplinary team as seen in a trial setting.[21] Another speculation is prescribing cluster visits for a particular day of a week may have caused loss of flexibility to diabetes patients. This, however, needs further exploration in future studies in India.
General practitioners in India still use the acute episodic care delivery model to manage chronic conditions like diabetes.[22] Management of diabetes at primary care needs a systematic approach as has been seen in other countries. The Chronic Care Model (CCM)[23,24] developed by Wagner and colleagues is one such example. The use of CCM was significantly associated with improved diabetes outcomes and better control of HbA1c, BP, and cholesterol.[25,26] Our study also confirmed that the two elements of CCM that we studied tracking care of diabetes patients (patient records) and involving nonphysician staff in reminding patients and other services (nonphysician assistance) was positively associated with the better process of care. The simple changes in general practice such as ensuring access to previous records of patients by either keeping the copy in the clinics or even better, incorporating electronic records may improve the adherence to processes of care. Nonphysician staff helps in both managing the records and reminding physicians and patients regarding required processes of care.
Adherence to prescribed processes of care may not translate directly to the control of risk of factors as many other patient factors such as behavioral (e.g., adherence to treatment and lifestyle) and psychological factors (e.g., depression) also influence the control of risk factors.[27] As such, identifying barriers and also what patients themselves would be willing to take on toward achieving better care needs to be considered. This may be another role that nonphysician assistants can take on – talking to the patient and using behavioral activation approaches to achieve better and more patient-centered care. In addition, the offer of a recommended monitoring and screening visit tends to be physician directed and can be objectively measured; as such, updating physicians on evidence-based practices may be an important first step toward better diabetes care.
Further, improving outcomes of diabetes care is a challenging task but is achievable. For example, recent trend analysis using national level data in the United States showed significantly improved risk factor control[10] and reduced incidence of diabetes complication[28] in previous decades and was attributed to the combined efforts of patient education and improved performances of health systems including team approaches to care at all levels of care.[28] Incorporating evidence-based practices into routine practices does have many systemic impediments in India such as lack of standard treatment protocol, lack of systemic coordination, and poor regulation of the private sector.[22] These systemic barriers at the general practices need to be addressed to improve diabetes and other chronic disease care.
This is the first study to report processes of diabetes care at general practitioners clinics in India and identify both clinic- and patient-level factors that are associated with quality indicators. The study included a large group of clinics and volume of patients with very few missing data.
Our study does have several limitations. One, the selected clinics may not be representative of general practitioner's clinics in NCR-Delhi. These were physicians that were interested in diabetes care (and therefore were motivated and enrolled in CCEBDM training program) and had good proportions of patients with diabetes; therefore, we believe that the diabetes care processes would be either similar or possibly worse in other clinics. Two, we did not measure proportions of patients with diabetes having an annual urine microalbumin measurement; preventive screening test for diabetes nephropathy is an important process quality indicator. However, since patients may not be able to differentiate between regular urine (dip test) and microalbumin testing, this was considered an unreliable measure. Three, other than clinic, physician, and patient factors measured in the study, factors related to the patient-physician-system relationship such as communication, trust, access to care, and cost of care also influence receipt of care processes and could not be accounted for in our study.[27] Finally, we recruited the physicians at the beginning of training in CCEBDM, therefore this study did not capture the effect of training on diabetes care at these settings.
CONCLUSIONS
Despite the fact that patients with diabetes in Delhi visited general practitioner clinics in high frequency over the preceding year, their receipt of diabetes care processes was inadequate. Inadequate use of patient records may have led to poor decision making on the periodicity of monitoring of risk factors and screening for complications. Being a private clinic and involvement of nonphysicians in assisting with aspects of diabetes care were the two clinic factors found to be associated with processes of care. These associations and their implications need further exploration. Encouraging implementation of quality of improvement strategies like CCM elements at general practices may improve diabetes care.
Financial support and sponsorship
The study was funded by and the first author (RS) and her mentors (KMV and MKA) were supported by D43 Training Program (Award No. 1D43HD05249 of the Eunice Kennedy Shriver National Institute of Child Health and Human Development and Fogarty International Center) and National Heart, Lung, and Blood Institute and United Health, USA (Contract Award No. HHSN26820090026C).
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We acknowledge the contribution of Arun Kumar, Harshit Singh Thapa in data collection and Naveen Kumar and Praggya Sharma in data management.
REFERENCES
- 1.Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352:837–53. [PubMed] [Google Scholar]
- 2.Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: Results of the HOPE study and MICRO-HOPE substudy. Heart Outcomes Prevention Evaluation Study Investigators. Lancet. 2000;355:253–9. [PubMed] [Google Scholar]
- 3.Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ. 1998;317:703–13. [PMC free article] [PubMed] [Google Scholar]
- 4.Colhoun HM, Betteridge DJ, Durrington PN, Hitman GA, Neil HA, Livingstone SJ, et al. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): Multicentre randomised placebo-controlled trial. Lancet. 2004;364:685–96. doi: 10.1016/S0140-6736(04)16895-5. [DOI] [PubMed] [Google Scholar]
- 5.Heart Protection Study Collaborative Group. Collins R, Armitage J, Parish S, Sleigh P, Peto R. MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: A randomised placebo-controlled trial. Lancet. 2003;361:2005–16. doi: 10.1016/s0140-6736(03)13636-7. [DOI] [PubMed] [Google Scholar]
- 6.ADVANCE Collaborative Group. Patel A, MacMahon S, Chalmers J, Neal B, Billot L, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560–72. doi: 10.1056/NEJMoa0802987. [DOI] [PubMed] [Google Scholar]
- 7.Tuomilehto J, Rastenyte D, Birkenhäger WH, Thijs L, Antikainen R, Bulpitt CJ, et al. Effects of calcium-channel blockade in older patients with diabetes and systolic hypertension. Systolic Hypertension in Europe Trial Investigators. N Engl J Med. 1999;340:677–84. doi: 10.1056/NEJM199903043400902. [DOI] [PubMed] [Google Scholar]
- 8.American Diabetes Association. Standards of medical care in diabetes-2014. Diabetes Care. 2014;37(Suppl 1):S14–80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- 9.International Diabetes Federation Guideline Development Group. Global guideline for type 2 diabetes. Diabetes Res Clin Pract. 2014;104:1–52. doi: 10.1016/j.diabres.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 10.Ali MK, Bullard KM, Saaddine JB, Cowie CC, Imperatore G, Gregg EW. Achievement of goals in U.S. diabetes care, 1999-2010. N Engl J Med. 2013;368:1613–24. doi: 10.1056/NEJMsa1213829. [DOI] [PubMed] [Google Scholar]
- 11.Saaddine JB, Cadwell B, Gregg EW, Engelgau MM, Vinicor F, Imperatore G, et al. Improvements in diabetes processes of care and intermediate outcomes: United States, 1988-2002. Ann Intern Med. 2006;144:465–74. doi: 10.7326/0003-4819-144-7-200604040-00005. [DOI] [PubMed] [Google Scholar]
- 12.Khunti K, Gadsby R, Millett C, Majeed A, Davies M. Quality of diabetes care in the UK: Comparison of published quality-of-care reports with results of the Quality and Outcomes Framework for Diabetes. Diabet Med. 2007;24:1436–41. doi: 10.1111/j.1464-5491.2007.02276.x. [DOI] [PubMed] [Google Scholar]
- 13.6th ed. Brussels, Belgium: International Diabetes Federation; 2003. International Diabetes Federation. IDF Diabetes Atlas. [PubMed] [Google Scholar]
- 14.Mohan V, Madan Z, Jha R, Deepa R, Pradeepa R. Diabetes-social and economic perspectives in the new millennium. Int J Diabetes Dev Ctries. 2004;24:29–35. [Google Scholar]
- 15.Nathan DM. Long-term complications of diabetes mellitus. N Engl J Med. 1993;328:1676–85. doi: 10.1056/NEJM199306103282306. [DOI] [PubMed] [Google Scholar]
- 16.Nagpal J, Bhartia A. Quality of diabetes care in the middle- and high-income group populace: The Delhi Diabetes Community (DEDICOM) survey. Diabetes Care. 2006;29:2341–8. doi: 10.2337/dc06-0783. [DOI] [PubMed] [Google Scholar]
- 17.Mohan V, Shah SN, Joshi SR, Seshiah V, Sahay BK, Banerjee S, et al. Current status of management, control, complications and psychosocial aspects of patients with diabetes in India: Results from the DiabCare India 2011 Study. Indian J Endocrinol Metab. 2014;18:370–8. doi: 10.4103/2230-8210.129715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Triad Study Group. The Translating Research Into Action for Diabetes (TRIAD) study: A multicenter study of diabetes in managed care. Diabetes Care. 2002;25:386–9. doi: 10.2337/diacare.25.2.386. [DOI] [PubMed] [Google Scholar]
- 19.Shivashankar R, Kirk K, Kim WC, Rouse C, Tandon N, Narayan KM, et al. Quality of diabetes care in low- and middle-income Asian and Middle Eastern countries (1993-2012): 20-year systematic review. Diabetes Res Clin Pract. 2015;107:203–23. doi: 10.1016/j.diabres.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 20.Jackson GL, Lee SY, Edelman D, Weinberger M, Yano EM. Employment of mid-level providers in primary care and control of diabetes. Prim Care Diabetes. 2011;5:25–31. doi: 10.1016/j.pcd.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 21.Housden L, Wong ST, Dawes M. Effectiveness of group medical visits for improving diabetes care: A systematic review and meta-analysis. CMAJ. 2013;185:E635–44. doi: 10.1503/cmaj.130053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bhojani U, Devedasan N, Mishra A, De Henauw S, Kolsteren P, Criel B. Health system challenges in organizing quality diabetes care for urban poor in South India. PLoS One. 2014;9:e106522. doi: 10.1371/journal.pone.0106522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the chronic care model in the new millennium. Health Aff (Millwood) 2009;28:75–85. doi: 10.1377/hlthaff.28.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: Translating evidence into action. Health Aff (Millwood) 2001;20:64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 25.Nutting PA, Dickinson WP, Dickinson LM, Nelson CC, King DK, Crabtree BF, et al. Use of chronic care model elements is associated with higher-quality care for diabetes. Ann Fam Med. 2007;5:14–20. doi: 10.1370/afm.610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Siminerio L, Zgibor J, Solano FX. Implementing the chronic care model for improvements in diabetes practice and outcomes in primary care: The university of pittsburgh medical center experience. Clin Diabetes. 2004;22:54–8. [Google Scholar]
- 27.Triad Study Group. Health systems, patients factors, and quality of care for diabetes: A synthesis of findings from the TRIAD study. Diabetes Care. 2010;33:940–7. doi: 10.2337/dc09-1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gregg EW, Li Y, Wang J, Burrows NR, Ali MK, Rolka D, et al. Changes in diabetes-related complications in the United States, 1990-2010. N Engl J Med. 2014;370:1514–23. doi: 10.1056/NEJMoa1310799. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Diabetes patients meeting risk factor control targets at general practitioners clinics in National Capital Region-Delhi


