Abstract
Background:
A previous hospital based study from Delhi revealed a high prevalence of hypothyroidism in pregnant women. Several other studies with small sample size also indicate a rising trend of prevalence of hypothyroidism during pregnancy in India.
Objective:
To assess prevalence of hypothyroidism in pregnant women from various states/cities across India.
Materials and Methods:
This was a cross-sectional multicenter study conducted at Allahabad (Uttar Pradesh), Bengaluru (Karnataka), Chennai (Tamil Nadu), Kolkata (West Bengal), Hyderabad (Telangana), Nasik (Maharashtra), Rohtak (Haryana), Pune (Maharashtra), New Delhi (Delhi), Srinagar (Kashmir), and Vizag (Andhra Pradesh) enrolling 2599 pregnant women. Estimation of thyroid stimulating hormone (TSH), free T4, and antithyroid peroxidase (TPO) antibodies was carried out using Roche modular kit using ECLIA technology in a central laboratory.
Results:
We found in our study population that 13.13% of pregnant women have hypothyroidism (n = 388), using a cutoff TSH level of 4.5 μIU/ml. This prevalence was much higher using the American Thyroid Association criteria. Anti-TPO antibodies were positive in 20.74% of all pregnant women (n = 613), whereas 40% (n = 155) of hypothyroid pregnant women were positive for anti-TPO antibodies.
Conclusion:
This study concludes that there is a high prevalence of hypothyroidism (13.13%), majority being subclinical in pregnant women during the first trimester from India and universal screening of hypothyroidism may be desirable in our country.
Keywords: Epidemiology, hypothyroidism, pregnancy
INTRODUCTION
Hypothyroidism during pregnancy has an adverse effect on both mother and child. Children born to untreated or undertreated mothers have profound effect on future intellectual development.[1] Pregnancy has a profound physiological impact on the thyroid gland and thyroid function. During pregnancy, the thyroid gland increases in size by 10% in iodine sufficient countries and to a greater extent in iodine deficiency countries.[2] Production of thyroid hormones and iodine requirement both increases by approximately 50% during pregnancy as part of physiology.[3] In addition, pregnancy is a stressful condition for the thyroid gland resulting in hypothyroidism in women with limited thyroid reserve or iodine deficiency.
Data from recently published studies have underscored the association between miscarriage and preterm delivery in women with normal thyroid function who test positive for thyroid peroxidase (TPO) antibodies.[4] Prenatal and postnatal adverse effects including attention deficit and hyperactivity syndrome have been reported in children born to hypothyroid mothers.[5,6] During the first trimester, approximately 1 in 10 pregnant women develop antibodies to TPO or thyroglobulin and hypothyroidism develops in roughly 16% of these women. The prevalence of hypothyroidism in pregnancy is around 2.5% according to the Western literature.[7] There are a few reports of prevalence of hypothyroidism during pregnancy from India with prevalence rates ranging from 4.8% to 11%.[8,9] Therefore, this study was carried out in a larger cohort of pregnant women during the first trimester from a government hospital setting catering to majority of women from lower socioeconomic status.
MATERIALS AND METHODS
This was a cross-sectional multicenter study conducted at Allahabad, Bengaluru, Rohtak, Chennai, Kolkata, Hyderabad, Nasik, Pune, New Delhi, Srinagar, and Vizag to assess the incidence of hypothyroidism in pregnant women. The study was conducted at secondary and tertiary public hospitals. The study was conducted from July 2011 to December 2012. All consecutive pregnant women who gave written consent were included in the study. All women were subjected to detailed history and clinical examination using a predesigned performa. Blood samples were collected in outpatient department settings. Complete blood count (hemogram), total cholesterol, triglycerides, serum creatinine, and blood urea nitrogen were evaluated for all subjects. Estimation of thyroid stimulating hormone (TSH), free T4, and anti-TPO antibodies was carried out using Roch modular kit using ECLIA technology. The intra-assay precision of TSH and free T4 was 3 and 2, whereas interassay precision was 7.2 and 4.8, respectively.
RESULTS
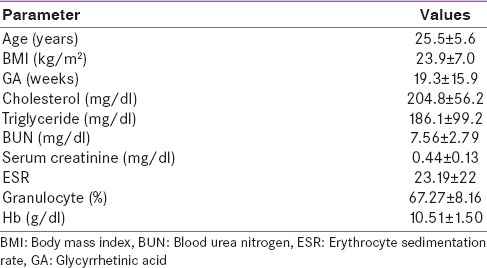
The baseline characteristics of the study population are given in Table 1. The mean age of the study population was 25.5 ± 5.6 years with a mean gestational age of 19.3 ± 15.9 weeks.
Table 1.
Demographic characteristics of the study population (n=2955)
Keeping upper normal limit of TSH < 4.5, we found in our study population 13.13% of pregnant women to be hypothyroid (n = 388). Anti-TPO antibodies were positive in 20.74% of all pregnant women (n = 613), whereas 40% (n = 155) of hypothyroid pregnant women were positive for anti-TPO antibodies. A total of 36.07% (n = 816) of pregnant women were found to be hypothyroid when we used trimester-specific TSH reference ranges as suggested by the American Thyroid Association (ATA) [Table 2].
Table 2.
Thyroid profile of pregnant women
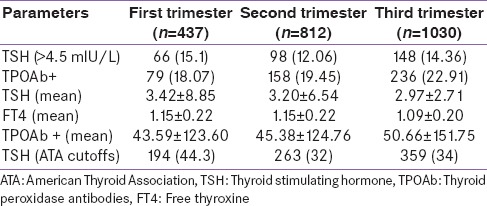
The prevalence of hypothyroidism was 15.1%, 12.06%, and 14.36% in the first, second, and third trimester, respectively, whereas anti-TPO antibody positivity was seen in 18.07%, 19.45%, and 22.91% in each trimester [Table 2].
Following trimester-specific TSH cutoffs of <2.5 mIU/L for the first trimester and <3.0 mIU/L for the second and third trimester as suggested by ATA, we found 44.3%, 32.0%, and 34% women were found to have hypothyroidism in the first, second, and third trimester, respectively [Table 2].
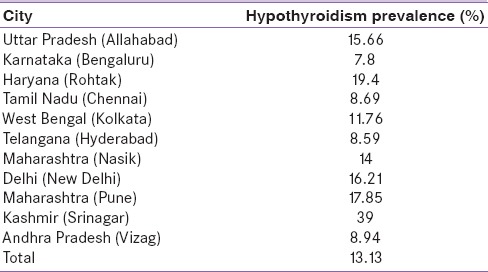
When we analyzed prevalence of hypothyroidism in individual states/cities, Srinagar (Kashmir), reported unusually high prevalence of hypothyroidism of (39%) and the lowest prevalence was reported from Bengaluru (Karnataka) (7.8%) [Table 3].
Table 3.
Prevalence of hypothyroidism among pregnant women in different states across India
DISCUSSION
This study was aimed to evaluate thyroid function during different trimesters of pregnancy in a large cohort across India. The major findings are that 13.3% women attending secondary and tertiary public hospitals have hypothyroidism majority being subclinical. A significant number of these women also have evidence of thyroid autoimmunity.
The prevalence of hypothyroidism has been reported from different countries very recently.[10,11,12] On analysis, results of this study are consistent with recently published data from India and other countries. Previous studies conducted in Delhi reported a 14.3% prevalence of hypothyroidism during the first trimester.[13] There are at least two small-scale published studies from the South, one from Chennai, and another from Hyderabad. Rao et al. included 163 nonpregnant women with recurrent pregnancy loss in a gestational age up to 12 weeks (2006) in Hyderabad.[14] Similarly, in a community-based large-scale study involving over 500,000 pregnant women from the USA showed a 15.5% prevalence of hypothyroidism.[15] Hypothyroidism was found in 7 (4.12%) women with recurrent pregnancy loss and one in the control group. The study demonstrates that hypothyroidism has a statistically significant relationship with recurrent pregnancy loss in the first trimester. Another study examined 500 pregnant women attending two Government Obstetrics and Gynecology Hospitals in Chennai for a period of 5 months in 2007 for thyroid function. Subclinical hypothyroidism was detected in 2.8%, among them, TPO antibodies positivity was seen in 57.1%, whereas euthyroid women had significantly lower positivity (7%).[16] In another study, Sahu et al. have done thyroid function during the second trimester in high-risk pregnant women and reported that prevalence of thyroid disorders, especially overt and subclinical hypothyroidism was 6.47%.[9] Further, in this study, significant adverse effects on maternal and fetal outcomes were observed emphasizing the importance of routine antenatal thyroid screening. Therefore, findings of our study are consistent with other previously reported data from India and this study also shows a rising trend of hypothyroidism among the Indian pregnant women.
The impact of thyroid dysfunction on pregnancy outcomes appears to manifest with a TSH threshold of >2.5 mIU/L in the first trimester rather than with a TSH range based on percentiles cutoff derived from apparently “normal” pregnant women. ATA recommends >2.5 and >3.0 µIU/ml as cutoff range for diagnosis of hypothyroidism during the first and later part of pregnancy, respectively. However, we have taken 4.5 µIU/ml as cutoff for diagnosis of hypothyroidism in different trimesters. This was based on the study published by Reh et al.[ 16] In addition, Marwaha et al. have reported that normal range of thyroid hormones in the Indian pregnant women are higher as compared to international cutoffs.[17] The large burden of subclinical hypothyroidism in pregnancy may prove to be a major public health burden in India, once it becomes clear that adverse outcomes can be corrected with screening and early replacement of levothyroxine. Children born to hypothyroid mothers have a poor intellectual function during the later part of their life.[18] Therefore, majority of the developed countries have the National Neonatal Screening Program in place and routinely screen all newborn for hypothyroidism. The question whether to screen all pregnant women for hypothyroidism is still not resolved.[19] ATA in its recently published guidelines has stated against the universal screening of pregnant women for hypothyroidism.[1]
Some of these studies have shown an adverse effect on fetal and maternal health outcomes. However, these studies are too small, and it is advisable that a large-scale study is done in this regard from India.
The strong point of this study is that we have included the largest number of subjects in this study from different parts of India. All the samples have been analyzed at a central laboratory. Further, the study population belongs to different socioeconomic strata and therefore, represents probably the pregnant population of India. This study also demonstrates a secular trend in prevalence of hypothyroidism in India, when data from other previous studies was analyzed. However, there are few limitations of this study. We have not carried out clinical and radiological thyroid examination including ultrasound, and apart from autoimmunity, we have not evaluated other causes of hypothyroidism in these women. Urinary iodine in the study population was also not measured.
This study concludes that there is a high prevalence of hypothyroidism in pregnancy (13.13%). Majority of these hypothyroid pregnant women have subclinical hypothyroidism. Further studies are required to evaluate impact of thyroid disorders during pregnancy in the Indian population to decide whether universal screening is needed for Indian pregnant women.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Stagnaro-Green A, Abalovich M, Alexander E, Azizi F, Mestman J, Negro R, et al. Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and postpartum. Thyroid. 2011;21:1081–125. doi: 10.1089/thy.2011.0087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van Raaij JM, Vermaat-Miedema SH, Schonk CM, Peek ME, Hautvast JG. Energy requirements of pregnancy in The Netherlands. Lancet. 1987;2:953–5. doi: 10.1016/s0140-6736(87)91431-0. [DOI] [PubMed] [Google Scholar]
- 3.Glinoer D. The regulation of thyroid function in pregnancy: Pathways of endocrine adaptation from physiology to pathology. Endocr Rev. 1997;18:404–33. doi: 10.1210/edrv.18.3.0300. [DOI] [PubMed] [Google Scholar]
- 4.Stagnaro-Green A. Thyroid antibodies and miscarriage: Where are we at a generation later? J Thyroid Res 2011. 2011:841949. doi: 10.4061/2011/841949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghassabian A, Bongers-Schokking JJ, de Rijke YB, van Mil N, Jaddoe VW, de Muinck Keizer-Schrama SM, et al. Maternal thyroid autoimmunity during pregnancy and the risk of attention deficit/hyperactivity problems in children: The generation R study. Thyroid. 2012;22:178–86. doi: 10.1089/thy.2011.0318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Männistö T, Vääräsmäki M, Pouta A, Hartikainen AL, Ruokonen A, Surcel HM, et al. Perinatal outcome of children born to mothers with thyroid dysfunction or antibodies: A prospective population-based cohort study. J Clin Endocrinol Metab. 2009;94:772–9. doi: 10.1210/jc.2008-1520. [DOI] [PubMed] [Google Scholar]
- 7.LeBeau SO, Mandel SJ. Thyroid disorders during pregnancy. Endocrinol Metab Clin North Am. 2006;35:117–36. doi: 10.1016/j.ecl.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 8.Nambiar V, Jagtap VS, Sarathi V, Lila AR, Kamalanathan S, Bandgar TR, et al. Prevalence and impact of thyroid disorders on maternal outcome in Asian-Indian pregnant women. J Thyroid Res 2011. 2011:429097. doi: 10.4061/2011/429097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sahu MT, Das V, Mittal S, Agarwal A, Sahu M. Overt and subclinical thyroid dysfunction among Indian pregnant women and its effect on maternal and fetal outcome. Arch Gynecol Obstet. 2010;281:215–20. doi: 10.1007/s00404-009-1105-1. [DOI] [PubMed] [Google Scholar]
- 10.Qian W, Zhang L, Han M, Khor S, Tao J, Song M, et al. Screening for thyroid dysfunction during the second trimester of pregnancy. Gynecol Endocrinol. 2013;29:1059–62. doi: 10.3109/09513590.2013.829448. [DOI] [PubMed] [Google Scholar]
- 11.Habimana L, Twite KE, Daumerie C, Wallemacq P, Donnen P, Kalenga MK, et al. High prevalence of thyroid dysfunction among pregnant women in Lubumbashi, Democratic Republic of Congo. Thyroid. 2014;24:568–75. doi: 10.1089/thy.2013.0261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moreno-Reyes R, Glinoer D, Van Oyen H, Vandevijvere S. High prevalence of thyroid disorders in pregnant women in a mildly iodine-deficient country: A population-based study. J Clin Endocrinol Metab. 2013;98:3694–701. doi: 10.1210/jc.2013-2149. [DOI] [PubMed] [Google Scholar]
- 13.Dhanwal DK, Prasad S, Agarwal AK, Dixit V, Banerjee AK. High prevalence of subclinical hypothyroidism during first trimester of pregnancy in North India. Indian J Endocrinol Metab. 2013;17:281–4. doi: 10.4103/2230-8210.109712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rao VR, Lakshmi A, Sadhnani MD. Prevalence of hypothyroidism in recurrent pregnancy loss in first trimester. Indian J Med Sci. 2008;62:357–61. [PubMed] [Google Scholar]
- 15.Blatt AJ, Nakamoto JM, Kaufman HW. National status of testing for hypothyroidism during pregnancy and postpartum. J Clin Endocrinol Metab. 2012;97:777–84. doi: 10.1210/jc.2011-2038. [DOI] [PubMed] [Google Scholar]
- 16.Reh A, Grifo J, Danoff A. What is a normal thyroid-stimulating hormone (TSH) level?. Effects of stricter TSH thresholds on pregnancy outcomes after in vitro fertilization. Fertil Steril. 2010;94:2920–2. doi: 10.1016/j.fertnstert.2010.06.041. [DOI] [PubMed] [Google Scholar]
- 17.Marwaha RK, Chopra S, Gopalakrishnan S, Sharma B, Kanwar RS, Sastry A, et al. Establishment of reference range for thyroid hormones in normal pregnant Indian women. BJOG. 2008;115:602–6. doi: 10.1111/j.1471-0528.2008.01673.x. [DOI] [PubMed] [Google Scholar]
- 18.Negro R, Schwartz A, Gismondi R, Tinelli A, Mangieri T, Stagnaro-Green A. Universal screening versus case finding for detection and treatment of thyroid hormonal dysfunction during pregnancy. J Clin Endocrinol Metab. 2010;95:1699–707. doi: 10.1210/jc.2009-2009. [DOI] [PubMed] [Google Scholar]
- 19.Vila L, Velasco I, González S, Morales F, Sánchez E, Torrejón S, et al. Controversies in endocrinology: On the need for universal thyroid screening in pregnant women. Eur J Endocrinol. 2013;170:R17–30. doi: 10.1530/EJE-13-0561. [DOI] [PubMed] [Google Scholar]


