Abstract
Purpose
Anabolic steroid misuse is a growing concern among adolescent boys, and chronic misuse is associated with multisystemic health consequences. However, little is known about weight related predictors of anabolic steroid misuse. We examined the prediction of lifetime anabolic steroid misuse as a function of self-perceived weight status among US adolescent boys.
Methods
Analysis was undertaken using the 2013 Youth Risk Behavior Survey, a nationally representative data set sampling public and private high school students throughout the United States. Data from a total of 6,000 US adolescent boys were used in the present study.
Results
The prevalence of ever misusing anabolic androgenic steroids was 12.6% among boys who viewed themselves as very underweight, 11.9% for boys who viewed themselves as very overweight, compared with 3.8% for boys who viewed themselves as about the right weight. Compared to boys who viewed themselves as about the right weight, boys who self-perceived themselves as very underweight (adjusted odds ratio = 6.9, 95% confidence interval: 2.7–17.7, p < .001) and very overweight (adjusted odds ratio = 3.8, 95% confidence interval: 1.8–7.7, p < .001) were significantly associated with increased risk of anabolic androgenic steroid misuse.
Conclusions
Large effect size estimates were revealed, suggesting that anabolic androgenic steroid misuse is not solely a function of boys desiring increased mass; boys who desire leanness are also likely to misuse anabolic androgenic steroids. Future prevention efforts should target not only boys who view themselves as underweight but also those who perceive themselves as overweight.
Keywords: Anabolic steroids, Adolescent boys, Body image, Weight
Androgenic anabolic steroids (AAS) refer to a family of hormones and synthetic derivatives, inclusive of testosterone, that facilitate muscle development and fat loss [1,2]. Evidence linking AAS to adverse health outcomes is rapidly accumulating [3]. AAS appear to have a particularly deleterious effect on cardiovascular functioning, including greater cardiac mass [4], abnormal contraction and dilation of the heart, reduced peak systolic strain [5], and atherosclerosis [6]. Evidence is also mounting that AAS misuse has long-term adverse effects on the neuroendocrine system [2]. AAS misuse has been implicated in the etiology and maintenance of muscle dysmorphia [7] and forms the basis for a recently proposed psychiatric condition called androgen dependence syndrome, in which sufferers use AAS despite prominent adverse medical, psychological, and social effects [8]. Other adverse psychiatric effects, including aggression, violence, and hypomania, have also been documented, although recent studies to substantiate these effects are lacking [2]. In addition, AAS sold over the Internet or on the street are often fake, contaminated, or counterfeit, potentially exposing the purchaser to dangerous substances [9]. Although adolescents may constitute a minority of AAS users [10], they also are a particularly important group to study given that they biologically may be more vulnerable to the effects of AAS, due to their still developing brain and body [11].
Published prevalence rates of AAS misuse are highly variable, particularly among adolescents. Data from longitudinal studies indicate a lifetime prevalence rate of 1.7% among adolescent boys living in the United States [12]. The prevalence of lifetime steroid use among Australian adolescents was recently reported to be 2.4% [13]. Cross-sectional research from a large sample of American college students found a prevalence rate of 1% [14]. However, a recent nationally representative study of US adolescents found lifetime misuse prevalence at 7% in 2013, up from 5% in 2012 [15]. To date, it is unclear what is accounting for the variation in prevalence rates between studies, although it is possible that it is due to unclear operationalization of what constitutes AAS versus other appearance and performance enhancing drugs. In addition, adolescents may confuse illegal anabolic steroids with legal nonanabolic steroids. Corticosteroids, for example, are widely prescribed for a range of physical conditions and may potentially lead to overestimates of AAS use. Despite the lack of clarity around an established prevalence rate of AAS misuse, even the most conservative figures are comparable to the rate of anorexia nervosa among adolescent females.
Body dissatisfaction is a robust risk factor for AAS misuse among adolescent boys [16–18]. The current Western “ideal” form for the male body emphasizes both leanness and muscularity [18], with empirical evidence illustrating a curvilinear relationship between body weight and body satisfaction, in that greatest body dissatisfaction occurs in males with both low and high body mass index (BMI) [19]. Given that AAS misuse is often used as a means to approach this often highly unattainable body [20,21], it stands to reason that boys who perceive their bodies as distal from this ideal, whether in regard to body fat, muscle mass, or both, may experience greater body dissatisfaction and thus be at greater risk for AAS misuse. In partial support of this, a recent study of approximately 8,000 adolescent high school boys living in the United States found that perceiving oneself as very underweight was significantly predictive of AAS misuse [22].
However, boys who perceive themselves as overweight may also be at risk for AAS misuse. It is important to note that some forms of AAS are used primarily for purposes of achieving leanness versus excessive muscle mass. For instance, one increasingly used synthetic agent—clenbuterol—is used specifically for its fat burning properties [23]. Thus, adolescent boys who perceive themselves as overweight may also be at risk for misusing AAS—perhaps for reasons similar to those of boys who perceive themselves as underweight—to achieve a highly lean and muscular body. The notion that there exist various groups of boys at risk for misusing AAS—underweight boys and overweight boys—is supported by research. Hildebrandt et al. [24] modeled heterogeneity among a sample of 400 regular AAS users and found evidence for distinct classes—including those who used predominantly fat burning substances to effect a reduction in body fat and body weight and those who used predominantly anabolic or muscle building substances to effect an increase in muscle mass and body weight. However, to date, no known studies have simultaneously examined the role of perceived underweight and overweight status in predicting AAS misuse among adolescent boys. With this limitation in mind, we hypothesized that boys who perceive themselves as distal to the ideal male body—that is, both underweight and overweight males—would be more likely than their average weight peers to engage in AAS misuse.
Methods
Participants and procedure
The present study is a secondary data analysis from the publically available 2013 National Youth Risk Behavior Survey (YRBS) [25,26]. For the purposes of the present study, we examined select variables (described in the following section) from the YRBS, based on the present study hypotheses. The YRBS is a nationally representative survey that monitors the health behaviors among US high school students and used a 3-stage cluster sample design that yielded a representative sample of ninth through 12th grade students. Students included all public, catholic, and other private school students enrolled in grades nine through 12. Student participation in the study was voluntary and anonymous. In 2013, the survey included 92 items, and the Institutional Review Board of the Centers for Disease Control and Prevention approved the national YRBS. A total of 13,583 students responded to the survey (88% return rate), from 148 schools (77% return rate). For the purposes of the present study, only participants who indicated their sex was male were included (N = 6,000; see Table 1 for sample characteristics) given the sex disparities noted in the prevalence of AAS misuse. Additional information regarding the methodology and validity of the YRBS is discussed in detail elsewhere [25].
Table 1.
Sample characteristics
| Variable | M (SD)/N (%) |
|---|---|
| Age | 16 (1.2) |
| Grade level | |
| 9th Grade | 1,819 (26) |
| 10th Grade | 1,606 (23) |
| 11th Grade | 1,671 (24) |
| 12th Grade | 1,798 (26) |
| Race/Ethnicity | |
| White | 2,844 (48) |
| Nonwhite | 3,050 (52) |
| Hispanic/Latino | 1,744 (26) |
| Non-Hispanic/Latino | 5,065 (74) |
M = mean; SD = standard deviation.
Measures
AAS misuse
Lifetime AAS misuse was assessed with the following item, “During your life, how many times have you taken steroid pills or shots without a doctor’s prescription?” The response options for this item were: 0 times, 1 or 2 times, 3–9 times, 10–19 times, 20–39 times, or 40 or more times. To denote any lifetime misuse, a dichotomous score was created by coding no use as “0” and all other responses as “1.” Two additional dichotomous variables were created to assess moderate and severe levels of AAS misuse. Moderate use was defined as using AAS 10 or more times versus 10 times, and severe use was defined as using AAS 40 or more times versus 40 times. This is an approach that has been used in past research on AAS misuse [27].
Self-perceived weight
Self-perceived weight was obtained via the self-report item “how do you describe your weight?” The response options for this item were: very underweight, slightly underweight, about the right weight, slightly overweight, and very overweight. Four dummy variables were created for analyses, with “about the right weight” set as the referent group for all other self-perceived weight responses.
Demographics
Demographic data were assessed on the survey, which included questions on age, grade level, sex, ethnicity, and race. Participants completed survey questions to indicate their ethnicity as Hispanic/Latino or Non Hispanic/Latino, as well as questions to indicate their race as American Indian or Alaskan Native, Asian, Black, or African-American, Native Hawaiian or Other Pacific Islander, or White. For the purposes of the present study, ethnicity was coded as either Hispanic/Latino or Non Hispanic/Latino, whereas race was coded dichotomously as white versus nonwhite.
Self-reported height and weight
BMI was calculated based on participants’ self-reported height and weight. Self-reported height and weight were converted to meters and kilograms, respectively, and then a BMI score was calculated using the formula: kg/m2. These scores were in turn converted into percentiles based on age- and sex-specific reference data from the 2000 Centers for Disease Control and Prevention growth charts.
Sports participation
Sports participation was assessed via the following item, “During the past 12 months, on how many sports teams did you play? (Count any teams run by your school or community groups).” Response options were: 0 teams, 1 team, 2 teams, or 3 or more teams. This variable was treated continuously in analyses.
Weight change attempts
Weight change attempts were assessed via the following item: “Which of the following are you trying to do about your weight?” Response options were: lose weight, gain weight, stay the same weight, or not trying to do anything about weight. Three dummy variable were created for analyses, with “not trying to do anything about weight” set as the referent group for all other weight change attempt responses.
History of asthma
History of asthma was assessed via the self-report item: “Has a doctor or nurse ever told you that you have asthma?” This item was controlled for analyses, as some forms of steroids (e.g., prednisone, methylprednisolone) are used to treat asthma, and we wished to parcel out the effects of some participants misinterpreting the AAS misuse item to include treatment for asthma.
Statistical analyses
The primary analyses aimed to estimate AAS misuse as a function of self-perceived weight status among a nationally representative sample of adolescent boys. Given the complex sampling design inherent to the YRBS administration, the complex samples module of SPSS 22.0 (IBM Corp., Armonk, NY) was used in conducting the primary analyses. In doing so, SPSS complex samples module incorporates the weight, stratum, and primary sampling units variables provided in the public data set, when executing statistical significance tests. Accordingly, three separate binary logistic regressions were used, with each AAS misuse severity variable (i.e., any, moderate, and severe) set as the criterion variable. Additionally, relevant sociodemographic, (i.e., age, ethnicity, and race) and other covariates that have been previously associated with AAS misuse (i.e., asthma diagnosis, sports participation, weight change attempts, and body mass index) were controlled for. Adjusted odds ratios (AOR) and their 95% confidence intervals (CIs) are reported for all models. We also estimated prevalence rates of AAS misuse, across the three severity levels, as a function of self-perceived weight category.
Results
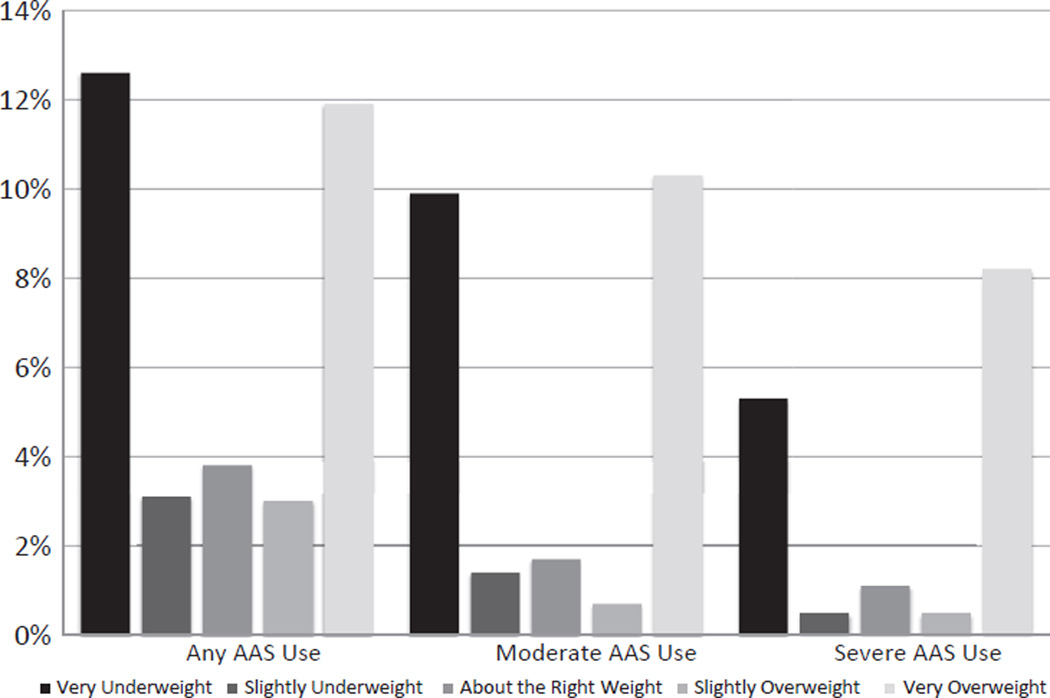
Please see Table 1 for characteristics of sample demographics. In regard to prevalence of AAS misuse, as a function of self-perceived weight category, for any lifetime misuse, very underweight (12.6%) and very overweight (11.9%) were the most elevated, followed by about the right weight (3.8%), underweight (3.1%), and overweight (3%). For moderate misuse, the prevalence rates were: very overweight (10.3%), very underweight (9.9%), about the right weight (1.7%), underweight (1.4%), and overweight (1%). Finally, for severe misuse, the prevalence rates were: very overweight (8.2%), very underweight (5.3%), about the right weight (1.1%), overweight (1%), and underweight (.5%). See Figure 1 for a graphical display.
Figure 1.
Anabolic androgenic steroid use as a function of self-perceived weight status among adolescent boys.
For the model predicting any lifetime AAS misuse, both self-perceived very underweight (AOR = 6.9, 95% CI: 2.7–17.7, p < .001) and very overweight status (AOR = 3.8, 95% CI: 1.8–7.7, p < .001) were significantly associated with increased risk of AAS misuse. Similar results were revealed for moderate AAS misuse, with both self-perceived very underweight (AOR = 13.9, 95% CI: 4.7–40.6, p < .001) and very overweight status (AOR = 6.4, 95% CI: 2.1–19.2 p < .001) emerging as significant predictors of misuse. Finally, both self-perceived very underweight (AOR = 11.2, 95% CI: 3.3–37.9, p < .001) and very overweight status (AOR = 6.2, 95% CI: 2.0–19.3, p < .001), were significant predictors of severe AAS misuse (see Tables 2–4 for full regression models).
Table 2.
Logistic regression model: Any steroid use
| Variable | B | SE | AOR | 95% CI |
|---|---|---|---|---|
| Hispanic | .464 | .205 | 1.59* | 1.05–2.41 |
| White | .233 | .251 | 1.26 | .760–2.09 |
| Asthma | .436 | .154 | 1.55** | 1.13–2.11 |
| Very underweighta | 1.93 | .467 | 6.93** | 2.69–17.81 |
| Underweighta | .054 | .384 | 1.05 | .486–2.29 |
| Overweighta | .135 | .373 | 1.15 | .539–2.43 |
| Very overweighta | 1.34 | .351 | 3.82** | 1.88–7.76 |
| Lose weightb | −.867 | .295 | .42** | .232–.761 |
| Gain weightb | .487 | .280 | 1.63 | .925–2.86 |
| Stay the same weightb | .381 | .263 | 1.46 | .860–2.49 |
| Age | .190 | .073 | 1.21* | 1.04–1.40 |
| Sports participation | .205 | .078 | 1.23* | 1.04–1.44 |
| BMI percentile | .014 | .005 | 1.01** | 1.00–1.02 |
AOR = adjusted odds ratio; BMI = body mass index; CI = confidence interval; SE = standard error.
As compared to referent group “about the right weight.”
As compared to referent group “not trying to do anything about weight.”
p < .05;
p < .01.
Table 4.
Logistic regression model: Severe steroid use
| Variable | B | SE | AOR | 95% CI |
|---|---|---|---|---|
| Hispanic | .113 | .472 | 1.12 | .432–2.90 |
| White | .284 | .377 | 1.328 | .620–2.85 |
| Asthma | .573 | .348 | 1.774 | .879–3.58 |
| Very underweighta | 2.417 | .604 | 11.21** | 3.31–37.98 |
| Underweighta | −.681 | .575 | .506 | .158–1.62 |
| Overweighta | −.814 | .702 | .443 | .107–1.83 |
| Very overweighta | 1.831 | .560 | 6.24** | 2.01–19.34 |
| Lose weightb | −.550 | .564 | .577 | .185–1.80 |
| Gain weightb | .948 | .441 | 2.58* | 1.06–6.29 |
| Stay the same weightb | .457 | .608 | 1.579 | .463–5.39 |
| Age | .272 | .131 | 1.31* | 1.01–1.71 |
| Sports participation | .050 | .139 | 1.05 | .794–1.39 |
| BMI percentile | .021 | .007 | 1.02** | .1.01–1.04 |
AOR = adjusted odds ratio; BMI = body mass index; CI = confidence interval; SE = standard error.
As compared to referent group “about the right weight.”
As compared to referent group “not trying to do anything about weight.”
p < .05;
p < .01.
Discussion
The present study reports the first known data illustrating the relationship between self-perceived weight status and AAS misuse among adolescent boys. The results revealed very large effect sizes indicating that the risk for AAS misuse is significantly elevated in those who self-reported a very underweight and very overweight status. This stands in marked contrast to the prevalence of AAS misuse among those who self-reported being underweight, overweight, or “at about the right weight”, who consistently demonstrated lower rates of AAS misuse.
In and of itself, the finding that AAS misuse is elevated among those self-reporting a very underweight body may not be surprising. The self-reported deeming of oneself to be inadequately muscular is an important construct in the body dissatisfaction of males [28], which in turn is centrally implicated in the drive for muscularity and a number of potentially adverse behavioral correlates including disordered eating, compulsive exercise, and AAS use [28–30]. However, the elevated risk of AAS misuse in those self-reporting a very overweight body status may appear somewhat counterintuitive, given that males with high body weight typically evidence behavioral strategies to lose weight [31]. Nonetheless, these data may reflect the changing nature of the male body ideal, with males being increasingly encouraged to pursue both muscular and lean body types [32]. Indeed, the ideal male body portrayed to males is often characterized by a high degree of muscularity, in addition to the absence of body fat, which is thought to obscure the visibility of muscularity. As such, many males pursuing the muscular ideal simultaneously evidence the drive for muscularity and the drive for leanness [32]. Boys who self-perceive themselves to be very overweight may both (1) desire a reduction of body fat which obscures the visibility of muscularity, and simultaneously (2) desire a greater degree of muscularity. Reflecting this, recent evidence depicts distinct profiles of AAS misuse among males, oriented toward both fat loss and muscular development, respectively [24]. Indeed, body image in boys typically runs along two dimensions; muscularity and leanness [33,34], with both muscularity and body fat dissatisfaction representing dual pathways into muscularity-oriented sequelae [35]. The present findings illustrate that it may not be just self-perceived very underweight status that predicts AAS misuse among this population but also self-reported very overweight status.
In accounting for this greater preponderance of AAS misuse in very underweight and very overweight groups, one explanation might posit that those at dimensional extremes of body composition are most likely to engage in AAS misuse. These trends prevailed after controlling for any variance because of self-reported height and weight, suggesting that boys who misuse AAS may inaccurately assess their weight status. However, because the YRBS does not collect objective markers of height and weight, we cannot conclude with certainty that participants were necessarily misperceiving their weight, although somewhat mitigating this concern, both self-reported and physician measured BMI correlate similarly to health risk estimates. Indeed, marked differences in AAS misuse emerged between those who self-reported being very underweight versus underweight and between those who self-report being very overweight versus overweight, suggesting that even a moderate recalibration of self-reported body image may exact large reductions in the risk of AAS misuse in those most vulnerable. To this end, broader research suggests that among those with eating disorders, self-reported body image may drive a myriad of pathological body image behaviors [36,37], with much evidence documenting the value of restructuring core body perception as a key intervention in those with eating disorders [38]. Evidence suggests that cognitive behavioral techniques such as mirror exposure training have yielded promising findings for the recalibration of body image disturbance [39]. The present findings therefore support the application of similar cognitive restructuring techniques in recalibrating distorted body image in those most at risk for AAS misuse. Alongside a direct impact in clinical practice, these findings may also impact the ongoing development of preventative measures, with the clear delineation of the differential impact of self-reported weight status likely augmenting efforts to identify those most at risk for AAS misuse.
However, it is important to note that one’s subjective perception of weight and one’s actual body weight may differ significantly. Thus, in identifying those most at risk for AAS misuse, clinicians may not rely on physical dimensions alone and should seek to ascertain a subjective determination of one’s body image. Furthermore, clinicians ought to be familiar with the full spectrum of body image concerns among boys, with ostensibly opposing dimensional extremes of self-reported body image being similarly associated with increased AAS misuse. Clinicians concerned about a client potentially using AAS may enquire about other muscularity-oriented body change and eating disordered behaviors, including supplement use, compulsive exercise or over-exercise, and negative affect–associated with interruptions to training and dieting.
Despite these novel findings, the present study is not without limitations. For instance, while the overall sample size represents a strength of the study, the cross-sectional design precludes any temporal inferences over time. Indeed, with increasing evidence supporting the notion of AAS dependence in some users [8], a temporal assessment of the impact of self-perceived weight status over time may offer important insights into the pathways into dependent versus nondependent AAS misuse. In addition, AAS misuse may occur among a constellation of other pathological body image–related behaviors, including disordered eating practices [40] and compulsive exercise, although it is important that the present findings are not extrapolated to infer risk of disordered eating and compulsive exercise practices. Further research may benefit from examining the impact of self-perceived weight status on AAS misuse over time and also in assessing the impact of self-perceived weight status on previously noted behavioral correlates of AAS misuse. Additionally, with recent evidence highlighting disparities in AAS misuse among boys as a function of sexual orientation [27], future research ought to control for sexual orientation in further indexing the impact of self-perceived weight status on AAS misuse. The parent YRBS study does not include measures of body dissatisfaction or internalization of the muscular ideal, thus, results from the present study cannot address whether these variables are accounting for variance in the relationship between self-perceived weight and AAS misuse; however, this would be an important inclusion in future studies. Finally, clinical interpretation of these findings must take into account the well-documented potential for over inclusive reporting on self-report measures of AAS misuse [22,27], as well as relying on self-report height and weight in lieu of objective markers.
After controlling for a range of relevant covariates, both self-perceived very underweight and very overweight status are significantly associated with greater risk of AAS misuse among adolescent boys. Thus, the drive for increased body mass alone may not entirely predict increased AAS misuse among adolescent boys, and the drive for leanness may also predict AAS misuse in this population. In addition, the potential discrepancy between actual weight and self-perceived weight in adolescent boys, when taken alongside the striking impact of self-perceived weight, underscores the importance of targeting body image cognition/perceptual distortions in those at risk for AAS misuse. Findings should be couched within the limitations of the study design—relying on cross-sectional, self-report data.
Table 3.
Logistic regression model: Moderate steroid use
| Variable | B | SE | AOR | 95% CI |
|---|---|---|---|---|
| Hispanic | .132 | .276 | 1.14 | .501–1.53 |
| White | .021 | .346 | 1.02 | .508–2.05 |
| Asthma | .544 | .219 | 1.72* | 1.11–2.68 |
| Very underweighta | 2.635 | .530 | 13.94** | 4.79–40.62 |
| Underweighta | .117 | .549 | 1.12 | .371–3.41 |
| Overweighta | −.833 | .597 | .44 | .13–1.45 |
| Very overweighta | 1.865 | .541 | 6.45** | 2.17–19.24 |
| Lose weightb | −.315 | .498 | .73 | .267–1.99 |
| Gain weightb | 1.065 | .355 | 2.9** | 1.42–5.94 |
| Stay the same weightb | .730 | .481 | 2.08 | .786–5.48 |
| Age | .326 | .109 | 1.39** | 1.11–1.73 |
| Sports participation | .170 | .122 | 1.19 | .921–1.52 |
| BMI percentile | .018 | .005 | 1.02** | 1.01–1.03 |
AOR = adjusted odds ratio; BMI = body mass index; CI = confidence interval; SE = standard error.
As compared to referent group “about the right weight.”
As compared to referent group “not trying to do anything about weight.”
p < .05;
p < .01.
IMPLICATIONS AND CONTRIBUTION.
This study examines the role of both underweight and overweight self-perceptions in predicting anabolic androgenic steroid use among adolescent boys. The findings suggest that steroid prevention efforts should examine extreme distortions in self-perceived weight—both very underweight and very overweight.
Acknowledgments
The funding source had no involvement in the study design, collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication. A.J.B. conceptualized and designed the study, conducted the analyses, and supervised the writing of the manuscript. S.G. drafted the introduction section of the manuscript. S.B.M. drafted the discussion section of the manuscript. J.D.J. drafted the methods section of the manuscript, and assisted in conceptualization of the study. A.J.B., the corresponding author, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. A.J.B. also affirms that everyone who has significantly contributed to this study is listed in the Acknowledgments section. This manuscript was originally presented as an abstract at the 2015 Association for Behavioral and Cognitive Therapies (ABCT) conference.
Funding Sources
Investigator time was supported by NIH grant K23MH096647 (A.J.B.).
Footnotes
Conflicts of Interest: No authors of this study have any conflicts of interest, including relevant financial interests, activities, relationships, or affiliations.
References
- 1.Bhasin S, Woodhouse L, Casaburi R, et al. Testosterone dose-response relationships in healthy young men. Am J Physiol Endocrinol Metab. 2001;281:E1172–E1181. doi: 10.1152/ajpendo.2001.281.6.E1172. [DOI] [PubMed] [Google Scholar]
- 2.Kanayama G, Pope HG. Illicit use of androgens and other hormones: Recent advances. Curr Opin Endocrinol Diabetes Obes. 2012;19:211–219. doi: 10.1097/MED.0b013e3283524008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kanayama G, Hudson JI, Pope HG. Culture, psychosomatics and substance abuse: The example of body image drugs. Psychother Psychosom. 2012;81:73–78. doi: 10.1159/000330415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Far HR, Ågren G, Thiblin I. Cardiac hypertrophy in deceased users of anabolic androgenic steroids: An investigation of autopsy findings. Cardiovasc Pathol. 2012;21:312–316. doi: 10.1016/j.carpath.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 5.D’Andrea A, Caso P, Salerno G, et al. Left ventricular early myocardial dysfunction after chronic misuse of anabolic androgenic steroids: A Doppler myocardial and strain imaging analysis. Br J Sports Med. 2007;41:149–155. doi: 10.1136/bjsm.2006.030171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Santora LJ, Marin J, Vangrow J, et al. Coronary calcification in body builders using anabolic steroids. Prev Cardiol. 2006;9:198–201. doi: 10.1111/j.1559-4564.2006.05210.x. [DOI] [PubMed] [Google Scholar]
- 7.Rohman L. The relationship between anabolic androgenic steroids and muscle dysmorphia: A review. Eat Disord. 2009;17:187–199. doi: 10.1080/10640260902848477. [DOI] [PubMed] [Google Scholar]
- 8.Kanayama G, Brower KJ, Wood RI, et al. Anabolic–androgenic steroid dependence: An emerging disorder. Addiction. 2009;104:1966–1978. doi: 10.1111/j.1360-0443.2009.02734.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Graham MR, Ryan P, Baker JS, et al. Counterfeiting in performance- and image-enhancing drugs. Drug Test Anal. 2009;1:135–142. doi: 10.1002/dta.30. [DOI] [PubMed] [Google Scholar]
- 10.Cohen J, Collins R, Darkes J, Gwartney D. A league of their own: Demographics, motivations and patterns of use of 1,955 male adult nonmedical anabolic steroid users in the United States. J Int Soc Sports Nutr. 2007;4:1–14. doi: 10.1186/1550-2783-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lumia AR, McGinnis MY. Impact of anabolic androgenic steroids on adolescent males. Physiol Behav. 2010;100:199–204. doi: 10.1016/j.physbeh.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 12.vandenBerg P, Neumark-Sztainer D, Cafri G, Wall M. Steroid use among adolescents: Longitudinal findings from Project EAT. Pediatrics. 2007;119:476–486. doi: 10.1542/peds.2006-2529. [DOI] [PubMed] [Google Scholar]
- 13.Dunn M, White V. The epidemiology of anabolic–androgenic steroid use among Australian secondary school students. J Sci Med Sport. 2011;14:10–14. doi: 10.1016/j.jsams.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 14.McCabe SE, Brower KJ, West BT, et al. Trends in non-medical use of anabolic steroids by U.S. college students: Results from four national surveys. Drug Alcohol Depend. 2007;90:243–251. doi: 10.1016/j.drugalcdep.2007.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Partnership for a Drug-Free America. The partnership attitude tracking study. New York: Partnership for a Drug-Free America; 2013. [Accessed May 2015]. Available at: http://www.drugfree.org/wp-content/uploads/2014/07/PATS-2013-FULL-REPORT.pdf. [Google Scholar]
- 16.Field AE, Sonneville KR, Crosby RD, et al. Prospective associations of concerns about physique and the development of obesity, binge drinking, and drug use among adolescent boys and young adult men. JAMA Pediatr. 2014;168:34–39. doi: 10.1001/jamapediatrics.2013.2915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parent MC, Moradi B. His biceps become him: A test of objectification theory’s application to drive for muscularity and propensity for steroid use in college men. J Couns Psychol. 2011;58:246–256. doi: 10.1037/a0021398. [DOI] [PubMed] [Google Scholar]
- 18.Ricciardelli LA, McCabe MP. A biopsychosocial model of disordered eating and the pursuit of muscularity in adolescent boys. Psychol Bull. 2004;130:179–205. doi: 10.1037/0033-2909.130.2.179. [DOI] [PubMed] [Google Scholar]
- 19.Austin SB, Haines J, Veugelers PJ. Body satisfaction and body weight: Gender differences and sociodemographic determinants. BMC Public Health. 2009;9:313. doi: 10.1186/1471-2458-9-313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ip EJ, Barnett MJ, Tenerowicz MJ, Perry PJ. The anabolic 500 survey: Characteristics of male users versus nonusers of anabolic-androgenic steroids for strength training. Pharmacotherapy. 2011;31:757–766. doi: 10.1592/phco.31.8.757. [DOI] [PubMed] [Google Scholar]
- 21.Leit RA, Gray JJ, Pope HG. The media’s representation of the ideal male body: A cause for muscle dysmorphia? Int J Eat Disord. 2002;31:334–338. doi: 10.1002/eat.10019. [DOI] [PubMed] [Google Scholar]
- 22.Blashill AJ. A dual pathway model of steroid use among adolescent boys: Results from a nationally representative sample. Psychol Men Masc. 2014;15:229–233. doi: 10.1037/a0032914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brett J, Dawson AH, Brown JA. Clenbuterol toxicity: A NSW poisons information centre experience. Med J Aust. 2014;200:219–221. doi: 10.5694/mja13.10982. [DOI] [PubMed] [Google Scholar]
- 24.Hildebrandt T, Langenbucher JW, Carr SJ, Sanjuan P. Modeling population heterogeneity in appearance- and performance-enhancing drug (APED) use: Applications of mixture modeling in 400 regular APED users. J Abnorm Psychol. 2007;116:717–733. doi: 10.1037/0021-843X.116.4.717. [DOI] [PubMed] [Google Scholar]
- 25.Brener ND, Kann L, Kinchen S, et al. Methodology of the Youth Risk Behavior Surveillance System-2013. MMWR Recomm Rep. 2013;62:1–20. [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Methodology of the Youth Risk Behavior Surveillance System. MMWR Recomm Rep. 2004;53:1–13. [PubMed] [Google Scholar]
- 27.Blashill AJ, Safren SA. Sexual orientation and anabolic-androgenic steroids in US adolescent boys. Pediatrics. 2014;33:469–475. doi: 10.1542/peds.2013-2768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Olivardia R, Pope HG, Borowiecki JJ, III, Cohane GH. Biceps and body image: The relationship between muscularity and self-esteem, depression, and eating disorder symptoms. Psychol Men Masc. 2004;5:112–120. [Google Scholar]
- 29.Bergeron D, Tylka TL. Support for the uniqueness of body dissatisfaction from drive for muscularity among men. Body Image. 2007;4:288–295. doi: 10.1016/j.bodyim.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 30.Tod D, Edwards C. Predicting drive for muscularity behavioural engagement from body image attitudes and emotions. Body Image. 2013;10:135–138. doi: 10.1016/j.bodyim.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 31.McCabe MP, Ricciardelli LA. Body image and body change techniques among young adolescent boys. Eur Eat Disord Rev. 2001;9:335–347. [Google Scholar]
- 32.Griffiths S, Murray SB, Touyz S. Disordered eating and the muscular ideal. J Eat Disord. 2013;1:15. doi: 10.1186/2050-2974-1-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brunet J, Sabiston CM, Dorsch KD, McCreary DR. Exploring a model linking social physique anxiety, drive for muscularity, drive for thinness and self-esteem among adolescent boys and girls. Body Image. 2010;7:137–142. doi: 10.1016/j.bodyim.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 34.Kelley CC, Neufeld JM, Musher-Eizenman DR. Drive for thinness and drive for muscularity: Opposite ends of the continuum or separate constructs? Body Image. 2010;7:74–77. doi: 10.1016/j.bodyim.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 35.Tylka TL. Refinement of the tripartite influence model for men: Dual body image pathways to body change behaviors. Body Image. 2011;8:199–207. doi: 10.1016/j.bodyim.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 36.Cattarin JA, Thompson JK. A three-year longitudinal study of body image, eating disturbance, and general psychological functioning in adolescent females. Eat Disord. 1994;2:114–125. [Google Scholar]
- 37.Rosen JC. Body-image disturbances in eating disorders. In: Cash TF, Pruzinsky T, editors. Body Images: Development, Deviance, and Change. New York, NY: Guilford Press; 1990. pp. 190–214. [Google Scholar]
- 38.Waller G, Cordery H, Corstorphine E, et al. Cognitive behavioral therapy for eating disorders: A comprehensive treatment guide. New York, NY: Cambridge University Press; 2007. [Google Scholar]
- 39.Delinsky SS, Wilson GT. Mirror exposure for the treatment of body image disturbance. Int J Eat Disord. 2006;39:108–116. doi: 10.1002/eat.20207. [DOI] [PubMed] [Google Scholar]
- 40.Pisetsky EM, May Chao Y, Dierker LC, et al. Disordered eating and substance use in high-school students: Results from the Youth Risk Behavior Surveillance System. Int J Eat Disord. 2008;41:464–470. doi: 10.1002/eat.20520. [DOI] [PubMed] [Google Scholar]