Key Clinical Message
Transforaminal lumbar interbody fusion (TLIF) is a popular posterior spinal fusion technique, but sometimes require salvage surgery when implant failure occurs, which involves possible neural damage due to postoperative adhesion. The current report deals with successful anterior transperitoneal salvage surgery for failed L5‐S TLIF with less neural invasiveness.
Keywords: Lumbosacral fusion, revision surgery, transforaminal lumbar interbody fusion, transperitoneal anterior approach
Introduction
Lumbar interbody fusion has become a popular technique for treating pathological spinal conditions such as spondylolisthesis, degenerative disk disease, recurrent disk herniation, and spinal deformity 1. However, failed spinal intervertebral fusion sometimes requires salvage surgery when symptomatic 2. Posterior revision surgery sometimes causes severe perioperative complications such as a dural tear, nerve injury, and symptomatic neurologic disorders, especially in those with lumbosacral lesions 3.
The current report describes a safe revision option for a case of failed posterior transforaminal lumbar interbody fusion (TLIF) at the lumbosacral level treated using the anterior approach.
Case Report
A 72‐year‐old man was referred to our clinic for robust lower back pain and radicular pain in his right leg. The pain was refractory to any analgesic agents, including opioids and nerve root infiltration, which was temporarily effective for a couple of days. He had neurological intermittent claudication at <50 m. Radiological evaluation using magnetic resonance imaging indicated foraminal stenosis at the L5‐S level (Fig. 1A,B), and neurological findings showed left L5 spinal nerve‐related radiculopathy with a positive straight leg raising (SLR) test of 60°. Muscle weakness (manual muscle testing level 4) was present in the right anterior tibial muscle and extensor digitorum longus muscle as well as distribution of painful numbness that coincided with the L5 dermatome with a visual analog scale (VAS) score of 6–7. Under the diagnosis of L5‐S lumbar foraminal stenosis, he underwent L5‐S TLIF surgery using unilateral posterior intervertebral cages (Stryker, Kalamazoo, MI) (Fig. 1C,D). Postoperatively, he was free from the radicular leg pain and neurological disorder.
Figure 1.
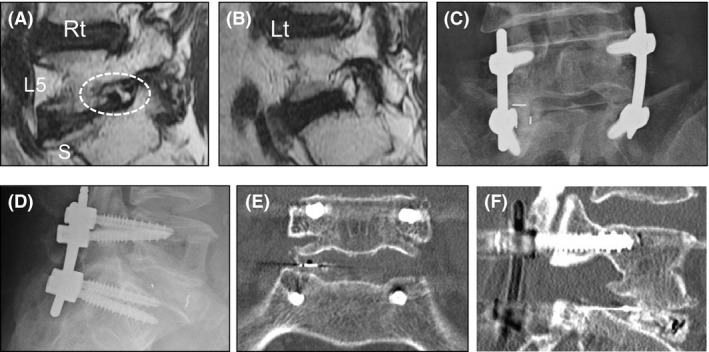
Representative images of the primary surgery. (A, B) The patient had complained of robust right leg pain from L5 radiculopathy due to L5‐S foraminal stenosis (dotted circle). (C–F) He had undergone L5‐S transforaminal lumbar interbody fusion using single posterior intervertebral cage. The intervertebral cage was more laterally installed than usual. Rt, right; Lt, left.
Three months postoperatively, he complained of recurrent right leg pain with L5 dermatomal distribution that was more robust than before the surgery, with a VAS score of 8–9 and a positive SLR test of 15°. Radiological examinations indicated right L5‐S foraminal stenosis due to subsidence of the intervertebral cage combined with a marginal fracture of the L5 vertebral body (Fig. 2A–C). The pain was refractory to any analgesic drugs, so we performed revision surgery. As the foraminal stenosis was severe, we planned to remove the intervertebral cage and replace it with another one. Considering major intra‐ and postoperative complications of severe damage to the foraminal space due to postoperative adhesion and scar tissues, and the predicted neural damage, we adopted the anterior transperitoneal approach to reach the lumbosacral junction to ensure clear and sufficient exposure of the intradiscal space.
Figure 2.
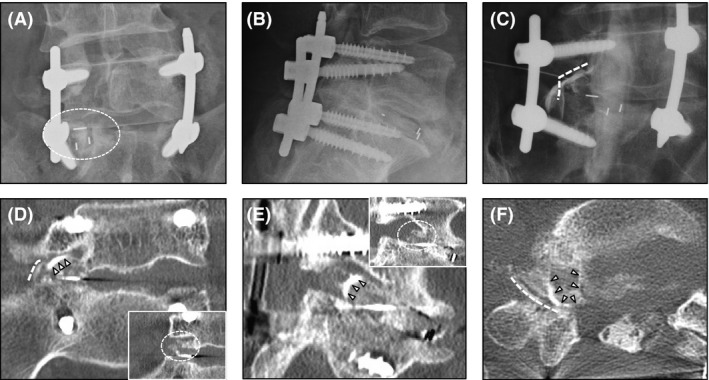
Radiological examinations 3 months after the primary surgery with right L5 radiculopathy. (A) Marked subsidence of the intervertebral cage is shown (dotted circle). (B) lateral X‐ray did not suggest apparent back‐out of the cage, nor subsidence to the S1 endplate. (C) Spinal nerve enhancement was performed just after the myelography. There was a rectangular‐shaped rim enhancement which knocked up the spinal nerve (dotted line). (D–F) Computed tomographic (CT) myelography. Enhanced rim of the cage (arrowheads) showed knocking up of spinal nerve (dotted line) at the foramen. Also, there was an obscure bone‐density mass in the foramen in the plain CT image (small images in (D) and (E)), indicating marginal fracture (dotted circle). Laterally installed intervertebral cage was considered to be knocking up the L5 spinal nerve with marginal fracture.
First, after the posterior rod was loosened in the prone position, the patient was placed in the supine position. A medial incision below the umbilicus was made followed by opening the peritoneal cavity. The bowels were retracted to expose the retroperitoneum at the bifurcation of the great vessels, and then the retroperitoneal space around the bifurcation and promontory were exposed. The ventral portion of the lumbosacral (IVD), including the anterior longitudinal ligament, was dissected to approach the disk. From the anterior opening portal, the primary intervertebral cage was identified at the edge of the endplates, and then, we carefully removed it to avoid intraoperative neurovascular injury. Then, the intervertebral space and vertebral fractured margin of the foraminal space were carefully and meticulously scraped to decompress the nerve under fluoroscopic guidance. Next, we installed an anterior cage (Century Medical, Tokyo, Japan) into the lumbosacral disk space followed by final rod fixation in the prone position (Fig. 3A–C). The operative duration was 4:31 (h:min) with only 10 mL of intraoperative bleeding.
Figure 3.
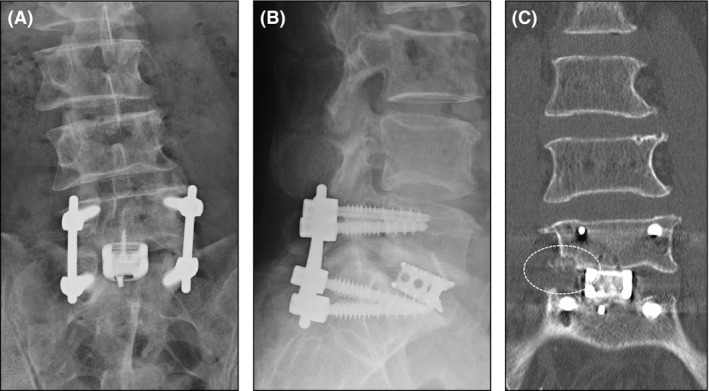
Representative postoperative radiological studies. (A, B) The lumbosacral anterior titanium cage was successfully installed. (C) The anterior cage recovered the disk height to resolve the right foraminal stenosis. Note that the marginal fracture was also resected (dotted circle).
Postoperatively, the leg pain resolved completely, with a VAS score of 0–1 and slight numbness in the right leg. Postoperative radiological studies showed enough recovery of the lumbosacral disk space, including the dorsal foraminal space. There have been no recurrence and/or exacerbation of pain and numbness without cage subsidence at 1.5 years after the revision surgery.
Discussion
The current report presented the effectiveness of the anterior approach for salvaging the posterior interbody to achieve safe removal of the posterior interbody cage and effective IVD height recovery under clear surgical site exposure at the lumbosacral junction via the transperitoneal approach.
Generally, posterior revision surgery requires extensive intracanal manipulation, which can cause epi‐ and endoneural fibrosis, resulting in a dural tear, nerve injury, and symptomatic neurologic disorders 3, although the TLIF procedure itself is reported to be relatively safe because the intervertebral cage will stay more lateral from the nerve even when it is dislodged 4. Thus, anterior salvage is reasonable that it prevents additional muscle damage and neurologic risks, and it is associated with much less blood loss achieved by blunt dissection 5. Moreover, anterior salvaging is quite effective considering that posterior adhesion/scar tissue can complicate the surgical procedure with a possible incidence of incidental durotomy. Previous studies have shown a higher rate of incidental durotomy in revision spinal surgery (8.1%) than with primary surgery (1–3.1%) 6. Furthermore, when durotomy cannot be identified at the time of surgery 7, it could result in postoperative pseudomeningocele. Among anterior approaches, the transperitoneal approach to the lumbosacral junction provides clearer and wider exposure than the retroperitoneal approach, and it is associated with an increased rate of potential complications such as retrograde ejaculation, impotence, retroperitoneal fibrosis, rectus muscle hematomas, pancreatitis, femoral nerve palsy, pseudomeningocele, or latissimus dorsi rupture 8, 9. Thus, complications may occur, and Gumbs et al. 9 suggested the following preoperative checklist for revision anterior spine surgery: repeat history and physical taking; repeat preoperative radiological evaluation, ureteral stents, angiogram/venogram; and preoperative sperm banking for male patients.
Another merit of the anterior approach for salvage surgery is that it does little harm to intracanal neural tissues by achieving indirect decompression followed by spontaneous recovery of the intervertebral and foraminal height. The current case demonstrated successful indirect decompression of the foramens by spontaneously recovering the disk height with little invasion.
The discussion regarding implant failure itself is beyond the current report, but the most commonly encountered reasons for failed interbody fusion derive from undersized constructs, single midline constructs, lateral cage placement with nerve root irritation, an anteriorly/posteriorly prominent cage, and pseudarthrosis 10. We have to mention that the placement of the cage in the current case was far lateral, that is suboptimal and why the subsidence occurred. The anterior cage installed in the current case overcame these issues because we inserted a much larger cage, which greatly reduces posterior irritation of the spinal nerve and results in a low rate of pseudarthrosis with robust circumference fusion. The cage also showed effective interbody fusion with its large opening and sufficient height, which posterior intervertebral cages fail to achieve. On the other hand, this is not with the current case, we have to realize that potentially approaching the nerve root via the ventral approach could lead to issues with nerve root traction when trying to remove a problematic TLIF cage that was scarred into the ventral nerve root area, especially after a long postoperative period. Furthermore, we have to discuss how to remove the cage removal when marginal fracture exists because treatment in the subsided space is sometimes destructive and disgusting to spinal nerve. In the current case, analysis using the multiply reconstructed images and detailed evaluation gave us the conclusion that the pathology of the radiculopathy was the foraminal stenosis due to the loss of foraminal height due to lateral marginal fracture, which did not directly interfere with the spinal nerve and foramen. Considering the possible damage to the foraminal space including the spinal nerve in the stenosed foramen via posterior revision, we made a decision to remove the cage via anterior approach.
In conclusion, we successfully performed a salvage revision surgery for a case of failed post‐TLIF at the L5‐S level using the transperitoneal anterior approach, and we replaced the failed intervertebral cage with an anterior cage that had enough height and bony union. Revision surgery has a higher rate of minor perioperative complications such as delayed wound healing and neurological disorders as well as incidental durotomy; thus, surgeons should practice the best salvaging strategy to avoid such perioperative complications similar to that in the current case.
Conflict of Interest
None declared.
Clinical Case Reports 2016; 4(5): 477–480
References
- 1. Silvestre, C. , Mac‐Thiong J. M., Hilmi R., and Roussouly P.. 2012. Complications and morbidities of mini‐open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine J. 6:89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kim, S. S. , and Michelsen C. B.. 1992. Revision surgery for failed back surgery syndrome. Spine 17:957–960. [DOI] [PubMed] [Google Scholar]
- 3. Wetzel, F. T. , and LaRocca H.. 1991. The failed posterior lumbar interbody fusion. Spine 16:839–845. [DOI] [PubMed] [Google Scholar]
- 4. Aoki, Y. , Yamagata M., Nakajima F., Ikeda Y., and Takahashi K.. 2009. Posterior migration of fusion cages in degenerative lumbar disease treated with transforaminal lumbar interbody fusion: a report of three patients. Spine 34:E54–E58. [DOI] [PubMed] [Google Scholar]
- 5. Aunoble, S. , Hoste D., Donkersloot P., Liquois F., Basso Y., and Le Huec J. C.. 2006. Video‐assisted ALIF with cage and anterior plate fixation for L5‐S1 spondylolisthesis. J. Spinal Disord. Tech. 19:471–476. [DOI] [PubMed] [Google Scholar]
- 6. Cammisa, F. P. Jr , Girardi F. P., Sangani P. K., Parvataneni H. K., Cadag S., and Sandhu H. S.. 2000. Incidental durotomy in spine surgery. Spine 25:2663–2667. [DOI] [PubMed] [Google Scholar]
- 7. Eichholz, K. M. , and Ryken T. C.. 2003. Complications of revision spinal surgery. Neurosurg. Focus 15:E1. [DOI] [PubMed] [Google Scholar]
- 8. Sasso, R. C. , Kenneth Burkus J., and LeHuec J. C.. 2003. Retrograde ejaculation after anterior lumbar interbody fusion: transperitoneal versus retroperitoneal exposure. Spine 28:1023–1026. [DOI] [PubMed] [Google Scholar]
- 9. Gumbs, A. A. , Hanan S., Yue J. J., Shah R. V., and Sumpio B.. 2007. Revision open anterior approaches for spine procedures. Spine J. 7:280–285. [DOI] [PubMed] [Google Scholar]
- 10. Heim, S. E. , and Abitbol J. J.. 2002. Complications and strategies for salvage of intervertebral fixation devices. Orthop. Clin. North America 33:393–402, vii. [DOI] [PubMed] [Google Scholar]


