Abstract
Ureteral strictures arising from radiotherapy for the treatment of prostate cancer are rare. We describe four cases of these ureteral strictures emphasizing pre-operative factors that may have contributed to development of the strictures, their ultimate surgical management, and the patients' short-term outcomes.
Keywords: Ureter, Stricture, Radiotherapy, Prostate cancer
Introduction
In the United States there are around 3 million survivors of prostate cancer.1 Definitive radiotherapy (XRT) treatment of localized prostate cancer is used in approximately 37% of newly diagnosed men.2 Severe urinary adverse events (AEs) are rare and some estimates are as low as 0.1%.3 AEs are increased with combined modality treatment, e.g. radical prostatectomy (RP) with XRT.4 Urethral obstruction is the most common severe AE, but obstruction can also occur within the pelvic ureter.4
Jarosek et al analyzed Surveillance, Epidemiology and End Results (SEER)-Medicare data to examine long-term AEs of XRT for prostate cancer. They found that ureteral stricture was an uncommon high-grade AE, with a 10 year propensity-weighted cumulative incidence of only 2.7% in men treated with RP and external beam radiotherapy (EBRT) compared to 1.2% in controls.4 The authors, however, were unable to describe management of this AE with the limitations of SEER-Medicare analysis.
Understanding AEs associated with XRT used to treat prostate cancer is essential for counseling patients and alerts urologists to monitor for rare AEs like ureteral stricture. We undertook this study in order to describe how these ureteral strictures were managed surgically. We hypothesized that urinary tract reconstruction was feasible in these cases.
Case presentation
Patient characteristics
We identified 4 men from our prospective database of 80 men with high-grade AEs from XRT for the treatment of prostate cancer. All of the patients were treated with combined modality therapy consisting of salvage EBRT after RP in 3 cases and high-dose-rate brachytherapy and EBRT in the remaining case. Mean latency period between XRT and ureteral stricture was 2.75 years (range 1–6 years). Three patients had urolithiasis, requiring ureteroscopy, which preceded clinically evident ureteral stricture. The mean age and Charlson Comorbidity Index was 72.8 (range 64–79) and 4.8 (range 4–6), respectively. At the time of diagnosis with ureteral stricture, mean serum creatinine was 2.2 mg/dL, glomerular filtration rate (GFR) was 38.3 mL/min and all men had no evidence of prostate cancer (Table 1).
Table 1.
Patient characteristics
| Variable | Mean | Range |
|---|---|---|
| Age (years) | 72.8 | 68–74 |
| Charlson comorbidity index | 4.75 | 4–7 |
| XRT treatment (n) | RP + EBRT = 3 HDR + EBRT = 1 |
|
| Time from XRT (years) | 2.75 | 1–6 |
| Stricture length (cm) | 7 | 2–13 |
| Hospital stay (days) | 4 | 3–5 |
| GFR improvement after surgery (mL/min) | 6 | 4–7 |
| Creatinine improvement after surgery (mg/dL) | 0.29 | 0.1–0.4 |
XRT (radiation therapy), RP (radical prostatectomy), EBRT (external beam radiotherapy), HDR (high-dose-rate brachytherapy).
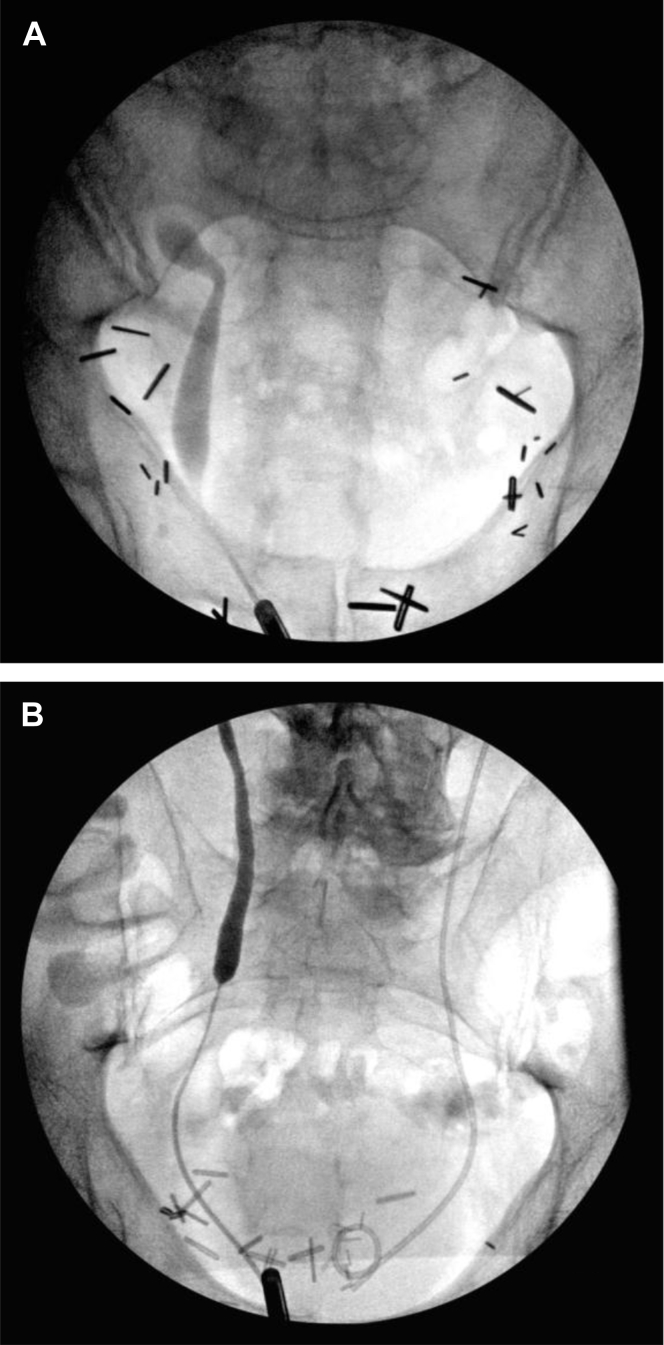
Patients had ureteral strictures of the left side in 2, right side in 1 and bilateral in 1, and the strictures were all within the pelvis (Fig. 1). The mean stricture length was 7 cm (range 2–13 cm). Patients had attempts at endoscopic management in all cases with an average of 3.5 procedures prior to surgical management. One patient was temporized with a stent, two with percutaneous nephrostomy tubes, and one did not have kidney drainage prior to surgery. Nuclear medicine MAG-3 renogram was performed on the 3 patients with unilateral obstruction and showed a mean function of 22% (range 12–28) prior to surgery.
Figure 1.
Pre-operative retrograde ureteropyelograms showing relatively short stricture of the distal ureter (A) versus pelvic obliteration of the lower ureter (B).
Management
All patients underwent hyperbaric oxygen therapy, either before or after ureteral reconstruction. Three patients with unilateral strictures had a ureteral re-implantation; 2 with a Boari flap and 1 with a psoas hitch. The patient with bilateral ureteral strictures required bilateral ileal ureteral substitution. Omental flaps were used in all of the cases to either wrap the anastomosis of the ureter or ileal limb with the bladder. The mean hospital stay was 4 days (range 3–5). There were no peri-operative complications within 6 weeks of surgery.
Follow up
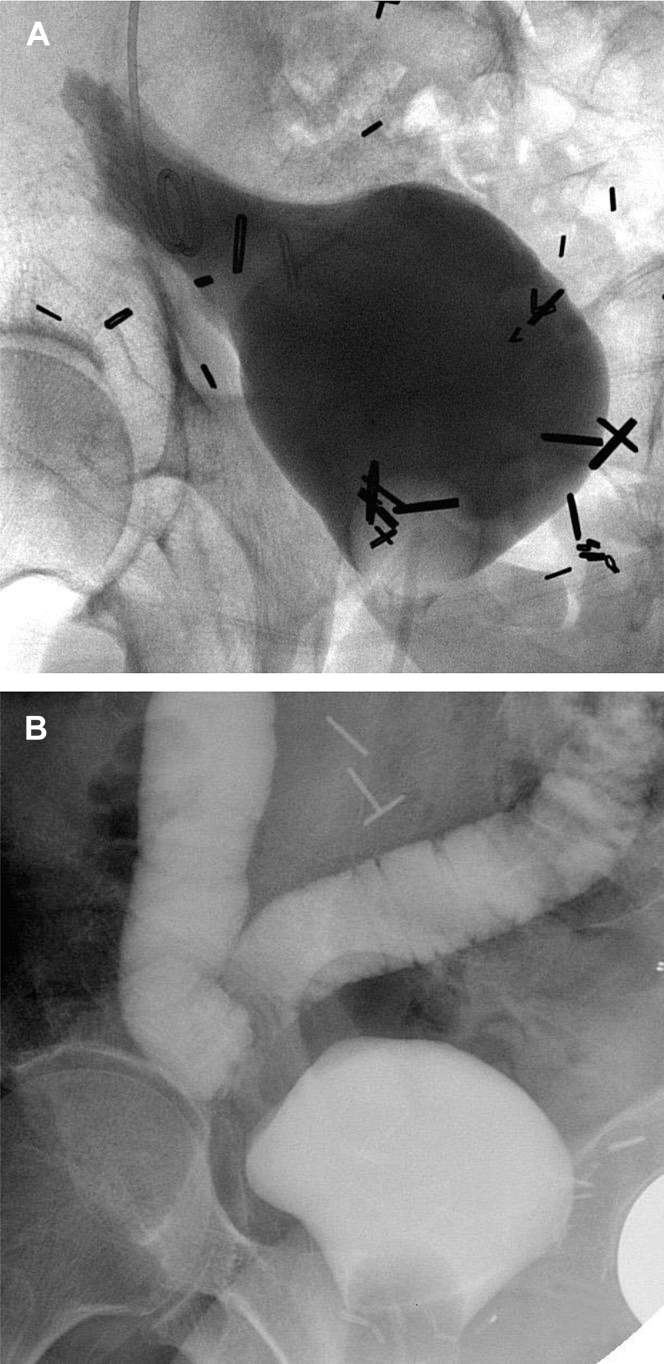
The median follow up was 5 months (range 3–12 months). Patients had a post-operative cystogram at 4 weeks (Fig. 2) prior to ureteral stent and Foley catheter removal. Long-term follow up imaging consisted of renal ultrasound in all 4 patients, which showed resolved hydronephrosis in all patients. The mean improvement of serum creatinine after surgery was 0.29 mg/dL and GFR was 6 mL/min. Improved or stable renal function was noted in all patients. None of the patients has had recurrent ureteral stricture.
Figure 2.
Post-operative cystogram showing Boari Flap reconstruction (A), and creation of a Y-type bilateral ileal ureter (B).
Discussion
There is little data about the treatment of ureteral strictures arising from XRT for prostate cancer. The condition is low risk according to SEER-Medicare analysis,4 however, in our prospective patient registry of men with high-grade urologic complications post XRT, the incidence was 5%.
Ureteral strictures are often managed with stenting and periodic stent exchanges. In our series, 2 of the patients could not have stents placed, because the scarring of the ureter was too severe and 1 had persistent asymptomatic hydronephrosis with a stent.
In our cases, all of the men had combined modality therapy and 3 out of 4 men had EBRT for salvage therapy after RP. Similar to these findings, Jarosek et al found that ureteral strictures were most common in patients who received RP + EBRT. Anatomically, after RP the ureters are pulled medially and the bladder neck inferiorly, and it has been hypothesized that this is the mechanism for ureteral obstruction with subsequent EBRT.5 Interestingly 75% of our patients had ureteroscopy for ureteral stones, prior to developing significant ureteral stenosis. One could propose a two hit hypothesis to explain the development of stricture in these men; one hit – RP + EBRT, second hit – ureteral manipulation. Additionally, the ureteral stones could be an indicator of sub-clinical ureteral narrowing and surgeons should be aware of possible further surgical trauma that might lead to complete obstruction.
All of the men in our series were reconstructed with the aid of omental flaps, and had hyperbaric oxygen treatments peri-operatively. Omental flaps provide two-fold benefit in the reconstructed radiated pelvis: (1) to augment blood flow and (2) help seal radiated anastomoses. Hyperbaric oxygen may theoretically improve tissue quality in marginal areas of collateral radiation damage and aid in healing, improving outcomes.
There are limitations to this study. The sample size of four patients limits our comments to observational. In addition, the limited median follow up of 5 months is too short to comment about long-term outcomes.
Conclusion
Ureteral strictures caused by pelvic radiation are more common in patients who have been treated with RP and subsequent salvage EBRT. These strictures appear to be high risk when patients have ureteral manipulation after XRT and urologists should avoid this if possible. Patients may have limited recovery of their kidney function, however, the need for indwelling stents or percutaneous nephrostomy drainage is eliminated with successful ureteral reconstruction.
Conflicts of interest
Authors have no conflict of interest.
Acknowledgments
The authors received funding from three anonymous patient donors with high-grade radiation injury to fund publication of this report.
References
- 1.DeSantis C.E., Lin C.C., Mariotto A.B. Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin. 2014;64:252–271. doi: 10.3322/caac.21235. [DOI] [PubMed] [Google Scholar]
- 2.Elliott S.P., Malaeb B.S. Long-term urinary adverse effects of pelvic radiotherapy. World J Urol. 2011;29:35–41. doi: 10.1007/s00345-010-0603-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Keyes M., Miller S., Pickles T. Late urinary side effects 10 years after low-dose-rate prostate brachytherapy: population-based results from a multiphysician practice treating with a standardized protocol and uniform dosimetric goal. Int J Radiat Oncol Biol Phys. 2014;90:570–578. doi: 10.1016/j.ijrobp.2014.06.037. [DOI] [PubMed] [Google Scholar]
- 4.Jarosek S.L., Virnig B.A., Chu H., Elliott S.P. Propensity-weighted long-term risk of urinary adverse events after prostate cancer surgery, radiation, or both. Eur Urol. 2014;67:273–280. doi: 10.1016/j.eururo.2014.08.061. [DOI] [PubMed] [Google Scholar]
- 5.Cohen K.H., Teh B.S., Paulino A.C., Butler E.B. Ureteral stenosis after postprostatectomy intensity-modulated radiotherapy. Am J Clin Oncol. 2010;33:108. doi: 10.1097/COC.0b013e31802b30cb. [DOI] [PubMed] [Google Scholar]