Abstract
Orthopedic prosthetic infections are potentially devastating complications. Plastic surgeons are frequently consulted to aid in the management of the soft tissue defects that are created by these infections. A review of the existing literature was performed to identify established treatment methods for soft tissue coverage of orthopedic hardware infections for a variety of anatomic locations. The following treatment guidelines and soft tissue reconstructive options were identified as viable options for the management of exposed or infected orthopedic hardware. This review provides descriptions of the various soft tissue reconstructive options available as well as adjunctive treatment methods.
Keywords: orthopedic prosthetic infections, plastic surgery
Plastic surgery expertise is sought in cases of orthopedic hardware infections when the soft tissues surrounding the site of infection become compromised. At the time of consultation, the diagnosis has been established and treatment has begun. The degree to which the surgeon must ascend the reconstructive ladder depends upon the degree of soft-tissue devitalization as the presence of well-vascularized tissue is essential for wound healing.1 Important considerations in operative planning include the size, depth, and location of the wound, and the quality of the surrounding soft tissue. Deep wounds with the exposure of bone, joint capsule, prosthesis, or other hardware require immediate, aggressive management involving flap coverage. On the other hand, superficial wounds are frequently treated with local wound care.1
Coverage with muscle flaps is the gold standard to repair soft tissue defects associated with infected joint prosthesis.2 3 Local and free flaps are excellent reconstructive options for many reasons. They provide a robust blood supply to regional tissues,1 4 thereby improving oxygen and nutrient delivery and allowing for adequate antibiotic distribution, exposure to humoral defenses, and vascular drainage to reduce the probability of failure due to recurrent infection.3 4 Not only does the augmented blood supply reduce infection, it also reduces the ischemia-induced breakdown of the surroundings tissues that cover the hardware.4 These flaps also provide bulk to eliminate the dead space created by the infection and debridement that follows.1 By incorporating muscle flap coverage into the dogma of early debridement and irrigation, the prosthesis can often be salvaged despite bone or hardware exposure.4 In a study of total knee arthroplasties with implant exposure, 100% limb salvage and 91% prosthesis salvage were accomplished with coverage by microvascular free tissue transfer,4 and Nahbedian et al demonstrated an 83% salvage rate using pedicle or free flap coverage of knee wounds with exposed prosthetic.5 Functional muscle flaps should be considered to replace function deficits arising when nearby muscle is damaged.4 The type of flap depends upon the location of the wound, the quality of local tissue, volume requirements, and surgeon preference.1 Further explanation of this decision will follow. Early plastic surgery consultation and the subsequent use of muscle flaps help provide definitive closure, salvage the prosthesis, maintenance of limb function, and decrease length-of-stay and cost of hospitalization.1
Beyond joint prostheses, soft tissue coverage is still the management of choice for exposed orthopedic hardware, as inconsistent results have plagued secondary closure and skin grafting.6 In trauma, wounds extending to the tendons, joint hardware, or other deep structures dictate flap reconstruction.7 Muscle and musculocutaneous flaps are suitable for reconstruction of soft tissue defects complicated by implant exposure because of their rich blood supply and anti-infective properties. Valenti et al reported a 75% salvage rate utilizing a sural fasciomusculocutaneous flap to treat infected distal leg implants with hardware exposure.8 Though soft tissue coverage is definitive management, Cho et al found that prophylactic or simultaneous soft tissue coverage did not reduce the frequency of wound-healing complications in patients undergoing elective orthopedic foot or ankle surgery when compared with postoperative plastic surgery management.7
Choosing a Flap
After deciding to use soft tissue transfer to reconstruct the soft tissue defect, the surgeon must then select the proper flap. The anatomical location of the wound largely determines the donor site from which the flap will be harvested and whether the flap will be pedicled or free. Both pedicle flaps and microvascular free flaps provide a robust local blood supply conferring all of the anti-infective benefits described above.4 Free flaps are frequently turned to if local muscle flaps are unavailable (i.e., after multiple prior procedures, extensive local tissue damage), or if the defect is too large to reconstruct with local or regional tissue.4 The latissimus dorsi is a commonly used free flap as its broad, flat shape provides sufficient surface area to cover many wounds.
Local Flaps Used for Coverage of Knee Defects
Coverage of the knee joint can be accomplished with local fasciocutaneous flaps in patients with delayed wound healing and significant skin loss in the absence of deep infection and implant exposure.2 Muscle and musculocutaneous flaps are reserved for complex soft tissue defects associated with bone or hardware exposure.2 As the knee joint is located in the proximal third of the distal lower extremity, the medial gastrocnemius muscle flap (followed by the lateral gastrocnemius) is the gold standard for reconstructing soft tissue defects (Fig. 1).2 3 If the defect is lower, the soleus flaps present additional reconstructive options (Fig. 1).3 Turnover flaps from the thigh, such as a distal based anterolateral thigh flap (ALT), can be used in the gastrocnemius muscle is not available. If local flap coverage options are not available, free muscle flaps such as latissimus dorsi, rectus abdominis, or vastus lateralis free flaps may be used (Fig. 2). Free perforator flaps, such as the free ALT, present a valid alternative to muscle flaps with their low donor-site morbidity and long pedicles. They are ideally used for large skin and soft tissue defects associated with excess fibrosis and scarring.2
Fig. 1.
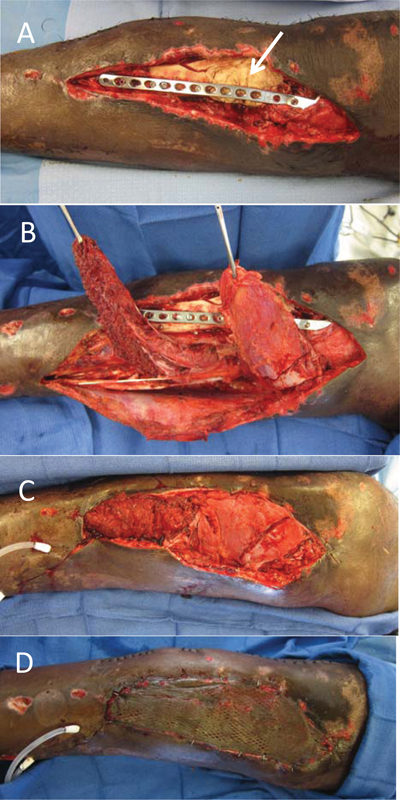
(A) A 43-year-old with exposed hardware with antibiotic spacer (arrow). (B,C) Coverage with gastrocnemius and soleus flap. (D) Coverage with split thickness skin graft.
Fig. 2.
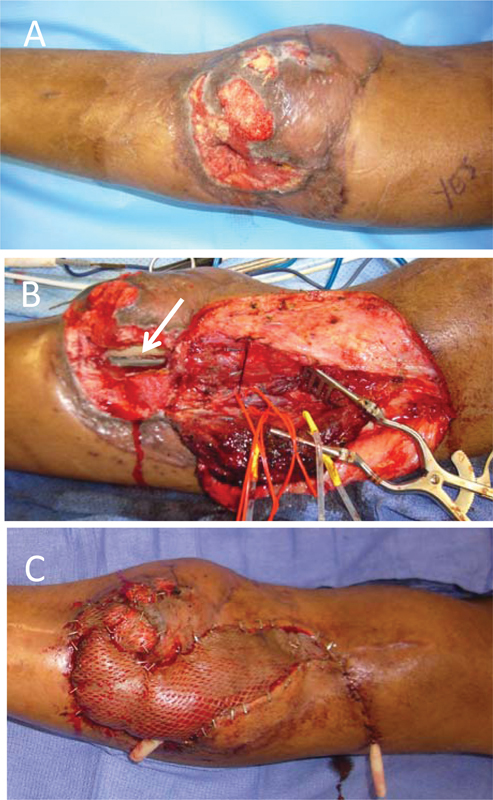
(A) A 45-year-old with a knee wound after failed gastrocnemius flap and (B) exposed hardware (arrow). (C) Coverage with free rectus abdominis and split thickness skin graft.
Local Flaps Used for Coverage of Hip Defects
A multitude of flap options to manage hip wounds exist. The rectus abdominis, vastus lateralis, vastus medialis, and rectus femoris flaps have all been described in the literature. Pedicled vastus medial and vastus lateral flaps may present good reconstructive options after resection arthroplasty.3 9 The vastus lateralis is supported by a reliable vascular pedicle, has a wide arc of rotation, and provides sufficient volume to fill dead space. Its integrity is not compromised by prior procedures, and no secondary function deficits are created by its harvest.1 In cases of traumatic injury, inferiorly based rectus abdominis flaps provide a reconstructive option in which the vascular pedicle originates safely outside the zone of injury.1
Local Flaps Used for Coverage of Ankle/Foot Defects
Soft tissue deficits of the foot and ankle pose unique reconstructive challenges given the complex anatomical variations and functional demands of this area. As such, addressing each area as a distinct subunit may allow surgeons to better understand the reconstructive goals for a given wound. Hollenbeck et al constructed a map of the foot dividing it into seven distinct subunits. The flap donor site is chosen based upon the unique functional and aesthetic demands of the given subunit.10 Some of the free flaps utilized include radial forearm, ALT, latissimus dorsi, and rectus abdominis flaps.
Local Flaps Used for Coverage of Elbow Defects
The treatment of elbow wounds is guided by the size of the defect and the location of the wound relative to the olecranon (Table 1).11 Local muscle flap donors include the anconeus, flexor carpi ulnaris, and triceps, but they often lie in the zone of injury rendering them unusable. The radial forearm flap is a major reconstructive option in elbow coverage, as it possesses a flexible arc of rotation, reliable vascularity, and possible sensory innervation.11 Most large deficits are managed with the latissimus dorsi muscle flap. The distal end of the flap can become tenuous in a pedicled flap is extended beyond the olecranon, so it is preferred to use free tissue transfer for defects distal to the olecranon.11
Table 1. Treatment protocol for soft tissue coverage of the elbow11 .
| Defect size | Defect location (relative to olecranon) | Recommended coverage options |
|---|---|---|
| Small (< 40 cm2) | Proximal | Pedicled latissimus dorsi flap, local fasciocutaneous flap |
| Distal | Local muscle flap, radial forearm flap, local fasciocutaneous flap | |
| Large (< 40 cm2) | Proximal | Pedicled latissimus dorsi flap, free flap |
| Distal | Radial forearm flap, free flap |
A regional approach described by Hochberg et al guides coverage of spine-associated wounds (Fig. 3).12 Paraspinal and trapezius muscle flaps are the flaps of choice for defects occurring in the upper third of the spine (Fig. 4). Specifically regarding the cervical spine, the trapezius muscle flap is first-line treatment, though it is plagued by a high seroma rate.12 Mericli et al advocate for the paraspinous muscle flap as first-line citing lower seroma rates.13 For those in the middle third, the turnover paraspinal flap and latissimus dorsi (Fig. 5) or reverse latissimus dorsi are often utilized. Multiple options exist for the lower third including the turnover paraspinal, latissimus dorsi, bipedicled latissimus, or gluteus maximus muscle flaps.
Fig. 3.
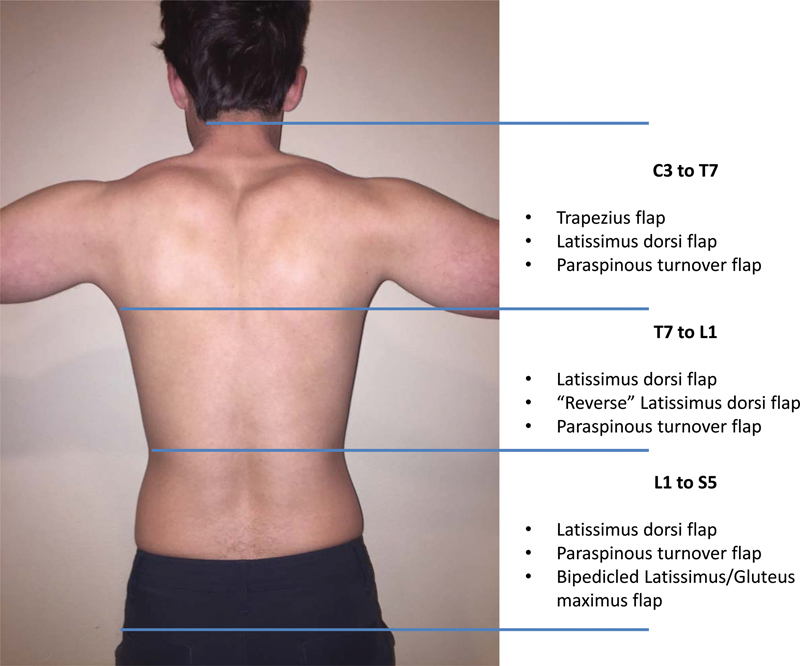
Regional approach to coverage of spine-associated wounds.14
Fig. 4.
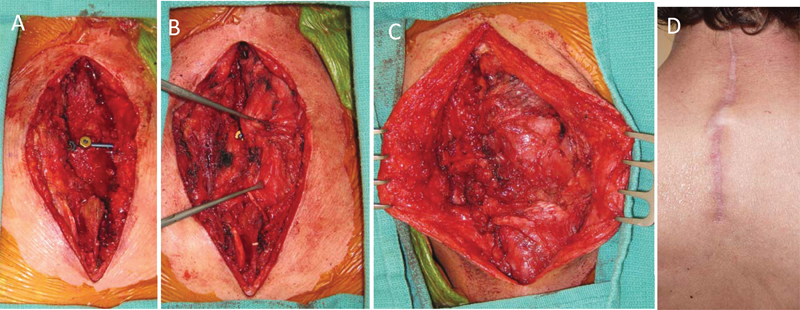
(A) A 58-year-old with prominent hardware. (B,C) Coverage with paraspinal flap. (D) At 9 months postoperative.
Fig. 5.
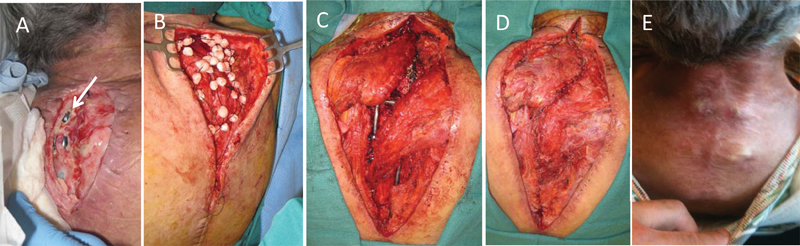
(A) A 64-year-old with lupus with exposed, unremovable hardware. (B) Salvaged with antibiotic beads. (C,D) Covered with bilateral latissimus dorsi flaps. (E) At 1 year postoperative.
Adjunctive Therapies
Another important, relatively new technology that facilitates management is negative-pressure therapy with vacuum-assisted closure (VAC). Negative-pressure therapy encourages healing by increasing wound blood flow and granulation tissue formation, resulting in reduced bacterial counts in the wound.14 Since its discovery, VAC therapy has been widely used to treat infected wounds as it has been proven to decrease the size of wounds and reduce flap requirements.14 Vacuum-assisted closure therapy combined with free tissue transfer can effectively treat exposed orthopedic hardware. Wen et al described an approach using VAC therapy followed by flap reconstruction of wound infections with hardware exposure after open reduction and internal fixation of distal tibia fractures. Utilizing this approach, bony consolidation was achieved in all seven patients.14 A prospective study by Lehner et al investigated the efficacy of negative-pressure wound therapy with instillation (NPWTi) in the treatment of infected orthopedic implants. Treatment consisted of surgical debridement, lavage, systemic antibiotics therapy, and NPWTi. Using this approach, 19 of 22 (86%) and 8 of 10 (80%) implants were retained in acutely and chronically infected implants, respectively.15
Conclusion
With the continued increase in orthopedic surgeries involving the use of prosthetic materials and the associated infections of these devices, management of the sequelae of these infections is expected to remain an active area of practice for plastic surgeons. Once the infection has been eradicated through the collaborative efforts of the infectious disease and orthopedic surgery teams, often plastic surgeons are consulted to manage the remaining complex wounds with the goals of (1) providing stable wound coverage with vascularized tissue, and (2) avoiding hardware exposure. Although each wound is unique and should be treated as such, here we have provided a summary of frequently employed coverage options for various anatomical locations.
References
- 1.Gusenoff J A, Hungerford D S, Orlando J C, Nahabedian M Y. Outcome and management of infected wounds after total hip arthroplasty. Ann Plast Surg. 2002;49(6):587–592. doi: 10.1097/00000637-200212000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Panni A S, Vasso M, Cerciello S, Salgarello M. Wound complications in total knee arthroplasty. Which flap is to be used? With or without retention of prosthesis? Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1060–1068. doi: 10.1007/s00167-010-1328-5. [DOI] [PubMed] [Google Scholar]
- 3.Suda A J, Cieslik A, Grützner P A, Münzberg M, Heppert V. Flaps for closure of soft tissue defects in infected revision knee arthroplasty. Int Orthop. 2014;38(7):1387–1392. doi: 10.1007/s00264-014-2316-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cetrulo C L Jr, Shiba T, Friel M T. et al. Management of exposed total knee prostheses with microvascular tissue transfer. Microsurgery. 2008;28(8):617–622. doi: 10.1002/micr.20578. [DOI] [PubMed] [Google Scholar]
- 5.Nahabedian M Y, Orlando J C, Delanois R E, Mont M A, Hungerford D S. Salvage procedures for complex soft tissue defects of the knee. Clin Orthop Relat Res. 1998;(356):119–124. doi: 10.1097/00003086-199811000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Viol A, Pradka S P, Baumeister S P. et al. Soft-tissue defects and exposed hardware: a review of indications for soft-tissue reconstruction and hardware preservation. Plast Reconstr Surg. 2009;123(4):1256–1263. doi: 10.1097/PRS.0b013e31819f2b5e. [DOI] [PubMed] [Google Scholar]
- 7.Cho E H, Garcia R, Pien I, Thomas S, Levin L S, Hollenbeck S T. An algorithmic approach for managing orthopaedic surgical wounds of the foot and ankle. Clin Orthop Relat Res. 2014;472(6):1921–1929. doi: 10.1007/s11999-014-3536-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vaienti L, Di Matteo A, Gazzola R, Randelli P, Lonigro J. Distally based sural fasciomusculocutaneous flap for treatment of wounds of the distal third of the leg and ankle with exposed internal hardware. J Orthop Traumatol. 2012;13(1):35–39. doi: 10.1007/s10195-011-0175-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choa R, Gundle R, Critchley P, Giele H. Successful management of recalcitrant infection related to total hip replacement using pedicled rectus femoris or vastus lateralis muscle flaps. J Bone Joint Surg Br. 2011;93(6):751–754. doi: 10.1302/0301-620X.93B6.25726. [DOI] [PubMed] [Google Scholar]
- 10.Hollenbeck S T, Woo S, Komatsu I, Erdmann D, Zenn M R, Levin L S. Longitudinal outcomes and application of the subunit principle to 165 foot and ankle free tissue transfers. Plast Reconstr Surg. 2010;125(3):924–934. doi: 10.1097/PRS.0b013e3181cc9630. [DOI] [PubMed] [Google Scholar]
- 11.Choudry U H, Moran S L, Li S, Khan S. Soft-tissue coverage of the elbow: an outcome analysis and reconstructive algorithm. Plast Reconstr Surg. 2007;119(6):1852–1857. doi: 10.1097/01.prs.0000259182.53294.67. [DOI] [PubMed] [Google Scholar]
- 12.Hochberg J Ardenghy M Yuen J et al. Muscle and musculocutaneous flap coverage of exposed spinal fusion devices Plast Reconstr Surg 19981022385–389., discussion 390–392 [DOI] [PubMed] [Google Scholar]
- 13.Mericli A F, Mirzabeigi M N, Moore J H Jr, Fox J W IV, Copit S E, Tuma G A. Reconstruction of complex posterior cervical spine wounds using the paraspinous muscle flap. Plast Reconstr Surg. 2011;128(1):148–153. doi: 10.1097/PRS.0b013e3182174075. [DOI] [PubMed] [Google Scholar]
- 14.Wen G, Wang C Y, Chai Y M, Cheng L, Chen M, Yi-Min L V. Distally based saphenous neurocutaneous perforator flap combined with vac therapy for soft tissue reconstruction and hardware salvage in the lower extremities. Microsurgery. 2013;33(8):625–630. doi: 10.1002/micr.22162. [DOI] [PubMed] [Google Scholar]
- 15.Lehner B, Fleischmann W, Becker R, Jukema G N. First experiences with negative pressure wound therapy and instillation in the treatment of infected orthopaedic implants: a clinical observational study. Int Orthop. 2011;35(9):1415–1420. doi: 10.1007/s00264-011-1274-y. [DOI] [PMC free article] [PubMed] [Google Scholar]


