Abstract
Objective
Adherence to pediatric traumatic brain injury (TBI) guidelines has been associated with improved survival and better functional outcome. However, the relationship between guideline adherence and hospitalization costs has not been examined. To evaluate the relationship between adherence to pediatric severe TBI guidelines, measured by acute care clinical indicators, and the total costs of hospitalization associated with severe TBI.
Design
Retrospective cohort study
Setting
Five regional pediatric trauma centers affiliated with academic medical centers.
Patients
Demographic, injury, treatment, and charge data were included for pediatric patients (age under 17 years) with severe traumatic brain injury.
Measurements
Percent adherence to clinical indicators was determined for each patient. Cost-to-charge ratios were used to estimate ICU and total hospital costs for each patient. Generalized linear models evaluated the association between healthcare costs and adherence rate.
Main Results
Cost data for 235 patients were examined. Estimated mean adjusted hospital costs were $103,485 (95% CI: 98,553–108,416); adjusted ICU costs were $82,071 (95% CI: 78,559–85,582). No association was found between adherence to guidelines and total hospital or ICU costs, after adjusting for patient and injury characteristics. Adjusted regression model results provided cost ratio equal to 1.01 for hospital and ICU costs (95% CI: 0.99–1.03 and 0.99–1.02, respectively).
Conclusions
Adherence to severe pediatric traumatic brain injury guidelines at these 5 leading pediatric trauma centers was not associated with increased hospitalization and ICU costs. Therefore, cost should not be a factor as institutions and providers strive to provide evidence based guideline driven care of children with severe TBI.
Keywords: childhood injury, traumatic injury, costs, guidelines, health care costs, pediatrics, quality of care, trauma, injury
INTRODUCTION
Traumatic brain injury (TBI) is a leading cause of morbidity and mortality in children.(1) Outcomes after pediatric TBI depend on factors such as age, injury severity and intent of injury,(2–4) but timely and high quality acute care is also of vital importance.(5–8) Publication of the 2003 and 2012 pediatric TBI guidelines represent important interdisciplinary efforts to provide guidance on provision of evidence-based acute care for infants and children with severe TBI.(9) Adherence to acute care clinical indicators in guidelines (9, 10) is associated with improved discharge survival and Glasgow outcome score.(11)
A recent multicenter study has shown that there is a 6% increase in discharge survival for each percentage point increase in adherence rate to the severe pediatric TBI guidelines.(11) This overall protective effect examined adherence to acute care indicators across locations, including the emergency department (ED), operating room (OR) and intensive care unit (ICU). Some indicators were found to be associated with a reduction in mortality across more than one treatment location (e.g., maintenance of cerebral perfusion pressure > 40 mmHg in both the OR and ICU). Increasing adherence to the pediatric TBI guidelines may, however, increase hospital costs if equipment and staffing needs are greater. Currently, no information exists indicating whether guideline adherence increases hospital costs and concern for the need of additional expenses may actually hamper guideline adherence. The purpose of this study was to evaluate the relationship between adherence to the 2003 Pediatric TBI Guidelines, measured by acute care clinical indicators, and the total costs of hospitalization and ICU care associated with severe pediatric TBI.
METHODS
Study Design
This study utilized data from a large, multi-site cohort study that included five geographically dispersed, regional pediatric trauma centers affiliated with academic medical centers. The primary purpose of the parent study was to examine the association between adherence to guidelines for management of pediatric severe TBI and discharge survival. Human Subjects Committee approval was obtained from each respective institution.
Study Sample
Demographic, injury, treatment, and charge data were included for pediatric patients aged 0 to 17 years old with severe TBI. Consistent with prior literature,(11) severe TBI was defined as an injury with one or more of the following ICD-9 discharge diagnosis codes: 800.0–801.9, 803.0–804.9, 850.0–854.1, 959.01, 950.1–950.3, 995.55, minimum head abbreviated injury scale (AIS) ≥ 3, admission Glasgow Coma Scale (GCS) score ≤ 8, alive with tracheal intubation for at least 48 hours in the ICU, history of trauma, and abnormal admission head computed tomography exam. Patients with extracranial injuries and those transferred from another hospital immediate following injury were also included. Patient recruitment occurred between 1/1/2007 and 12/31/2011.
Measurement
Adherence to guidelines
Percent adherence to clinical indicators was determined for each patient. Methods for the calculation of adherence scores have been described previously.(11) Briefly, 14 clinical indicators represented measures of adherence with recommendations within the 2003 Pediatric TBI Guidelines, most of which were retained in the 2012 revision. In some instances, procedures and processes involved more than one clinical indicator, which resulted in an imprecise mapping to the TBI guidelines. When appropriate, clinical indicators were examined for conditionality; indicators were considered relevant for patients with underlying conditions that would have qualified for given treatments.(11) For each patient in this study, a total hospital adherence rate (0–100 scale) and an ICU adherence rate (0–100 scale) across all locations were utilized as primary and secondary independent variables, respectively, in separate analyses. Details of the analysis on adherence and outcomes for study patients are given elsewhere.(11)
Patient characteristics
Each study center provided the following patient demographic information: age, gender (male, female), race (White, Black/African American, Hispanic/Latino, Asian or Pacific Islander, Other). Information on cardiac, pulmonary, neurological, endocrine, or other medical conditions was represented as a dichotomous (presence or absence) variable. Injury mechanism was categorized as motor vehicle crash, fall, struck by vehicle, abusive TBI, gunshot, or other. Injury severity information included GCS score at admission, head AIS, and highest non-head AIS. The AIS distinguishes injuries based on the likelihood of survival and is scored on a range from 1 to 6.(12) ICU length of stay (LOS) was also calculated.
Healthcare costs
Total hospital and ICU charges for each patient were converted to cost estimates using institution-specific cost-to-charge ratios (CCRs). When available, CCRs were obtained from the 2009 Healthcare Cost and Utilization Project Kids Inpatient Database (HCUP-KID; n=2). However, participation in HCUP-KID is voluntary (not every hospital provides data) and approximately 11% of HCUP-KID hospitals lack CCR data. Two institutions in our study did not participate in HCUP in 2009, and another did not provide CCR data. For these three sites, we obtained CCRs from the institution’s billing office. Hospital costs covered the full length of the patient’s hospital stay from admission to discharge, including ICU costs. ICU costs covered all expenses from ICU admission to discharge. ICU costs were analyzed separately because a large proportion of pediatric severe TBI care takes place in the ICU. Costs included room charges, supplies, nursing and personnel services, OR time, diagnostic procedures, medications, and therapies. Costs for these individual components were not available. Separately billed, individual provider charges for inpatient services provided in hospital facilities were (e.g., anesthesiologist charges) not available to study sites and therefore cost estimates did not include these fees. All costs were adjusted for inflation to 2012 US dollars using the Consumer Price Index (CPI) for Medical Care.(13) Patients who received care in two calendar years were assigned the CPI for the admission year.
Analysis
Patient characteristics were tabulated across adherence rate quartiles and evaluated for statistical significance of trend across quartiles using a non-parametric trend test (nptrend in STATA, an extension of the Wilcoxon rank-sum test) for categorical variables and variance-weighted least-squares (VWLS) regression for continuous variables. We evaluated the trend in unadjusted (crude) mean hospital and ICU costs across adherence rate quartiles using VWLS regression. We used generalized linear models (GLMs) to evaluate the association between estimated health care costs and adherence to guidelines (adherence rate). GLMs are versatile models often used in analyzing right-skewed and over-dispersed health care cost data.(14) Box-Cox and modified Park Tests were used to determine model specifications and take into account the skewness of cost data. We created separate regression models to estimate cost ratios for total hospital costs and ICU costs. Based on these tests, log link and inverse Gaussian family were chosen for both cost models. Regression models adjusted for the following demographic and injury characteristics that could influence costs: age, gender, race, presence of other medical conditions, highest non-head AIS, and admission GCS score. As a sensitivity analysis, we conducted separate models with and without groups of variables (patient demographics, clinical characteristics). All models accounted for clustering by institution. We used STATA/MP 13.1 for Macintosh (Stata Corp., College Station, TX, USA) for all analyses.
RESULTS
As previously described,(11) 236 pediatric patients with severe TBI were admitted to five sites during the study period. Hospital cost data were unavailable for one patient, so the final sample size was 235 patients. Ages ranged from less than 1 year to 17 years at the time of injury (Table 1). There was evidence of a significant trend for age (p=0.02) and discharge mortality (p=0.02) across adherence rate quartiles.
Table 1.
Characteristics of study sample
| Total (N=235) | Overall adherence rate quartile 1 (40–68.2%) (N=60) | Overall adherence rate quartile 2 (68.4–73.3%) (N=60) | Overall adherence rate quartile 3 (73.7–77.3%) (N=58) | Overall adherence rate quartile 4 (77.8–92.9%) (N=58) | |
|---|---|---|---|---|---|
| Age (years), mean [SD] | 8.0 [6.3] | 6.9 [6.4] | 7.7 [6.2] | 8.0 [6.3] | 9.5 [5.9] |
| Gender | |||||
| Male | 163 (69.1) | 41 (68.3) | 42 (70.0) | 41 (70.7) | 39 (67.2) |
| Female | 73 (30.9) | 19 (31.7) | 18 (30.0) | 17 (29.3) | 19 (32.8) |
| Race | |||||
| White | 117 (49.6) | 27 (45.0) | 31 (51.7) | 30 (51.7) | 29 (50.0) |
| Latino/Hispanic | 47 (19.9) | 12 (20.0) | 8 (13.3) | 15 (25.9) | 12 (20.7) |
| Black/African American | 55 (23.3) | 15 (25.0) | 17 (28.3) | 9 (15.5) | 14 (24.1) |
| Other | 17 (7.2) | 6 (10.0) | 4 (6.7) | 4 (6.9) | 3 (5.2) |
| Other medical condition(s) | |||||
| No | 46 (19.5) | 53 (88.3) | 46 (76.7) | 43 (74.1) | 48 (82.8) |
| Yes | 190 (80.5) | 7 (11.7) | 14 (23.3) | 15 (25.9) | 10 (17.2) |
| Injury mechanism | |||||
| Fall | 37 (15.7) | 13 (21.7) | 13 (21.7) | 13 (21.7) | 12 (20.7) |
| Motor vehicle crash | 51 (21.6) | 12 (20.0) | 7 (11.7) | 7 (12.1) | 11 (19.0) |
| Struck by vehicle | 50 (21.2) | 10 (16.7) | 14 (23.3) | 12 (20.7) | 14 (24.1) |
| Abusive TBI | 60 (25.4) | 16 (26.7) | 16 (26.7) | 20 (34.5) | 8 (13.8) |
| Gunshot | 14 (5.9) | 5 (8.3) | 3 (5.0) | 0 (-) | 6 (10.3) |
| Other | 24 (10.2) | 4 (6.7) | 7 (11.7) | 6 (10.3) | 7 (12.1) |
| Highest non-head AIS | |||||
| None (isolated TBI) | 54 (22.9) | 13 (21.7) | 6 (10.0) | 20 (34.5) | 15 (25.9) |
| 1,2 | 94 (39.8) | 25 (41.7) | 27 (45.0) | 20 (34.5) | 22 (37.9) |
| 3,4 | 82 (34.8) | 19 (31.7) | 26 (43.3) | 17 (29.3) | 20 (34.5) |
| 5,6 | 6 (2.5) | 3 (5.0) | 1 (1.7) | 1 (1.7) | 1 (1.7) |
| Head AIS | |||||
| 3,4 | 108 (45.8) | 26 (43.3) | 27 (45.0) | 30 (52.7) | 25 (43.1) |
| 5,6 | 128 (54.2) | 34 (56.7) | 33 (55.0) | 28 (48.3) | 33 (56.9) |
| Discharge mortality | |||||
| No | 206 (87.3) | 48 (80.0) | 50 (83.3) | 55 (94.8) | 53 (91.4) |
| Yes | 30 (12.7) | 12 (20.0) | 10 (16.7) | 3 (5.2) | 5 (8.6) |
| ICU LOS (days), mean [SD] | 14.8 [12.2] | 13.1 [11.6] | 16.2 [16.1] | 13.9 [9.0] | 15.9 [10.8] |
Unless otherwise indicated, values refer to N (%). Values may not sum to 100% due to rounding.
Abbreviations: TBI, traumatic brain injury; SD, standard deviation; ICU, intesive care unit; AIS, abbreviated injury score, LOS, length of stay.
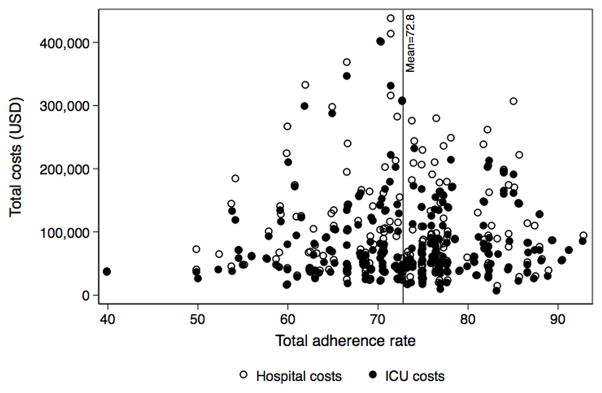
Among pediatric patients in this study, total hospital costs ranged from $13,859 to $437,749 and total ICU costs ranged from $5,776 to $400,663. The median estimated per-patient hospital cost was $73,742 (USD) (interquartile range, IQR=$90,050) and the median ICU cost was $59,358 (IQR=69,810) (Table 2). Overall, median ICU costs accounted for 89.1% of median hospital costs. For 37 patients (15.7%), total hospital costs were equal to ICU costs, indicating patients who were discharged directly from the ICU, transferred to rehabilitation facilities or long-term acute care centers associated with hospitals not included in this study, or expired before discharge from the ICU (N=30). There was no statistically significant trend in hospital or ICU costs across adherence rate quartiles (p=0.87 and p=0.78, respectively). The relationship between adherence rate and total hospital and ICU costs is shown in Figure 1.
Table 2.
Unadjusted hospital and ICU costs across quartiles of adherence to pediatric severe TBI guidelines.
| Total (N=235) | Overall adherence rate quartile 1 (40–68.2%) (N=60) | Overall adherence rate quartile 2 (68.4–73.3%) (N=60) | Overall adherence rate quartile 3 (73.7–77.3%) (N=58) | Overall adherence rate quartile 4 (77.8–92.9%) (N=58) | |
|---|---|---|---|---|---|
| Median (IQR), USD | |||||
| Hospital | 73,742 (90,050) | 70,827 (82,062) | 60,980 (73,203) | 75,832 (89,036) | 87,457 (93,329) |
| ICU | 59,358 (69,810) | 61,495 (73,273) | 49,978 (61,915) | 56,711 (70,545) | 70,857 (64,967) |
| Estimated costs, Mean (95% CI), USD | |||||
| Hospital | 102,525 (92,352–112,697) | 103,133 (83,257–123,009) | 101,350 (75,782–126,918) | 99,673 (81,557–117,788) | 106,023 (87,704–124,342) |
| ICU | 81,318 (73,192–89,445) | 85,396 (67,853–102,939) | 82,023 (61,896–102,151) | 73,553 (60,856–86,249) | 84,187 (69,678–98,695) |
Costs are converted from total charged amounts using cost to charge ratios, are reported in USD ($), and inflation adjusted to 2012 equivalents, based on Medical Consumer Price Index. No significant differences across quartile groups (variance-weighted least-squares regression, p=0.87 for hospital costs and p=0.78 for ICU costs).
Abbreviations: CI, confidence interval; IQR, interquartile range; ICU, intensive care unit; USD, US dollars.
Figure 1.
Total adherence rate (0–100 scale) for each pediatric severe TBI patient across five institutions and associated hospital and ICU costs (USD).
Adjusted regression model results yielded cost ratios equal to 1.01 for hospital and ICU costs (95% CI: 0.99–1.03 and 0.98–1.02, respectively), indicating no significant association between estimated costs and patient-level adherence rate, after adjusting for age, gender, race, presence of other medical conditions, head AIS, highest non-head AIS, admission GCS, and clustering by institution. The cost ratio provides an estimate of the relative difference in costs for a 1% increase in guideline adherence rate. The regression results show a 1% increase in guideline adherence is associated with 1% higher hospital costs and no (0%) higher ICU costs; these results are not statistically significant (p=0.22 for hospital costs; p=0.47 for ICU costs). The multivariable models therefore suggest that change in guideline adherence is not associated with a significance increase in costs. Adjustment for varying levels of covariates did not appreciably change cost ratios or result in statistical significance for hospital or ICU costs (Supplemental Table 1). Estimated mean per-patient costs, adjusted for covariates, were $103,485 (95% CI: 98,553–108,416) for total hospital costs and $82,071 (95% CI: 78,559–85,582) for costs associated with ICU admission.
DISCUSSION
This study found that across five geographically dispersed, regional pediatric trauma centers affiliated with academic medical centers, improvements in adherence to severe pediatric TBI acute care guidelines was not associated with changes in ICU or total hospital costs in the time period from 2007 to 2011 at participating pediatric trauma centers. This result, together with the finding that adherence to pediatric TBI guidelines is associated with significantly better patient outcomes,(11) provides strong evidence supporting the use of and adherence to evidence-based guidelines for the care of children with severe TBI.(9, 10) For institutions with limited resources, the potential investment required to improve adherence to pediatric TBI guidelines may not be associated with long-term increases in cost, but may result in improved outcomes. In addition, the relationship between guideline adherence and age, also reported in the parent study (11), warrants investigation in future research.
Healthcare costs may be attributed to capital, personnel, treatment, technology, and administrative costs.(15) Some of these costs are fixed such as facility costs, whereas other costs, like staffing, are variable. Theoretically, the cost of adhering to guideline recommendations may increase due to an increase in costly resources, such as staffing. For example, if maintenance of cerebral perfusion pressure above 40mmHg or early initiation of nutrition during the first 72 hours of admission (two acute care indicators associated with reduction in mortality) necessitates hiring additional staff for purposes of monitoring and providing care in these domains, then the value of adherence in these areas must consider these additional costs. Our finding, however, suggests that adherence to severe pediatric TBI guidelines may not significantly impact hospital or ICU costs. A formal cost-effectiveness analysis may be warranted to investigate this relationship further.
Our findings suggest that greater adherence to guidelines may be achieved without a statistically significant increase in cost, potentially by considering workflow characteristics of organizations where children with severe TBI receive care. For example, guideline adherence in the ED could require consideration of trauma team composition and functionality, which considers number and complexity of tasks and waste times. In the case of severe pediatric TBI, time from ED to OR may be reduced by optimizing communication paradigms, and handoffs from ED to OR or from these locations to the ICU may improve quality of care and reduce errors without concomitant increases in cost. The outcome and cost benefits of care coordination, through care pathways or creation of medical homes are similarly described;(16, 17) better organization of care services for children with severe TBI could contribute to similar findings. As recently described, there may also be a role for facility-level systems analysis and improvement interventions designed to maximize cost-effectiveness in severe TBI care.(18)
Recent research on the patient-centered medical home shows no significant changes in costs from adopting a model that increases care coordination.(19) Researchers have discussed the concept that “if care is to be of higher quality and lower cost the key to improvement lies in better organizational structures and processes”.(20) In order to achieve this, we must better understand the intersection of evidence-based medicine with evidence-based management.(21) This study points us in that general direction: for pediatric patients with severe TBI, improved outcomes can be sought, without increased costs.
This study has limitations. First, our study contains data from five select centers and average national costs for acute severe pediatric care may be overestimated or underestimated. Second, there may be differences in organizational characteristics between centers that we did not capture in this study. Third, it is possible that CCRs changed over the study period and are not sufficiently captured in the analysis. Fourth, provider-level charges may vary between institutions or by region and were not available for analyses. It is unclear how those differences may impact pediatric severe TBI costs. Fifth, we excluded patients who failed to survive at least 48 hours from ICU admission. The main purpose of this study was to examine adherence and inclusion of early deaths would have not allow for examination of adherence attempts or success. Finally, all sites in this study had the necessary infrastructure, supplies, equipment, or staffing to strive toward optimal guideline adherence with limited additional costs. Institutions with limited resources may have to invest more “up front” to achieve the level of guideline adherence.
In summary, increased hospital cost does not appear to be a reason for non-adherence to best health care practice in severe pediatric TBI at five leading pediatric trauma centers. Future studies investigating workflow and organization may reveal cost-neutral mechanisms that facilitate guideline adherence at all centers which care for children with severe TBI.
Supplementary Material
Acknowledgments
The source of support for this work including design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript was NINDS R01 NS072308-03. The following staff have contributed to data collection reported in the manuscript and were compensated as project staff and we have obtained permission from them, and they have been sent the manuscript under review: Rachelle Bell, RN University of Pittsburgh Medical Center, Pittsburgh, PA; Kristi Schmidt, MD, Ann & Robert H. Lurie Children’s Hospital, Chicago, IL; Alma Ramirez, Los Angeles BioMedical Research Institute, Harbor-UCLA Medical Center, Torrance, CA; Sheila Giles, RN, Nationwide Children’s Hospital, Columbus, OH. Authors would like to thank Harriet A. Saxe, JD, Research Coordinator at Harborview Injury Prevention and Research Center, for her assistance throughout this project.
Footnotes
Address for reprints: (Same as corresponding author)
Institution where work was performed: College of Nursing-Spokane, Washington State University
Conflict of interest statement: Authors have no conflicts of interest to declare.
AUTHOR CONTRIBUTIONS
The study was conceived by Janessa M. Graves, PhD MPH and Monica S. Vavilala, MD. Dr. Graves led the analysis, interpretation, and intial drafting of the manuscript. Dr. Graves had full access to all cost data and takes responsibility for its integrity of the data and the accuracy of the data analysis. All authors read, provided feedback on, and approved all manuscript drafts.
There are no conflicts of interests, including relevant financial interests, activities, relationships, and affiliations.
References
- 1.Faul M, Xu L, Wald M, Coronado V. Traumatic brain injury in the United States: Emergency department visits, hospitalizations and deaths 2002–2006. Atlanta, GA: Centers for Disease Control and Prevention; National Center for Injury Prevention and Control; 2010. [Google Scholar]
- 2.Kouznetsov E, Brennan M, Vassilyadi M. Towards development of a survival prediction tool for pediatric head injury. Pediatr Neurosurg. 2012;48(1):1–5. doi: 10.1159/000340068. [DOI] [PubMed] [Google Scholar]
- 3.Rivara FP, Koepsell TD, Wang J, Temkin N, Dorsch A, Vavilala MS, Durbin D, Jaffe KM. Disability 3, 12, and 24 months after traumatic brain injury among children and adolescents. Pediatrics. 2011;128(5):e1129–38. doi: 10.1542/peds.2011-0840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sills MR, Libby AM, Orton HD. Prehospital and in-hospital mortality: a comparison of intentional and unintentional traumatic brain injuries in Colorado children. Arch Pediatr Adolesc Med. 2005;159(7):665–70. doi: 10.1001/archpedi.159.7.665. [DOI] [PubMed] [Google Scholar]
- 5.Franschman G, Peerdeman SM, Greuters S, Vieveen J, Brinkman AC, Christiaans HM, Toor EJ, Jukema GN, Loer SA, Boer C. Prehospital endotracheal intubation in patients with severe traumatic brain injury: guidelines versus reality. Resuscitation. 2009;80(10):1147–51. doi: 10.1016/j.resuscitation.2009.06.029. [DOI] [PubMed] [Google Scholar]
- 6.Hesdorffer DC, Ghajar J. Marked improvement in adherence to traumatic brain injury guidelines in United States trauma centers. J Trauma. 2007;63(4):841–7. doi: 10.1097/TA.0b013e318123fc21. discussion 7–8. [DOI] [PubMed] [Google Scholar]
- 7.Pronovost PJ, Rinke ML, Emery K, Dennison C, Blackledge C, Berenholtz SM. Interventions to reduce mortality among patients treated in intensive care units. J Crit Care. 2004;19(3):158–64. doi: 10.1016/j.jcrc.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 8.Rusnak M, Janciak I, Majdan M, Wilbacher I, Mauritz W. Severe traumatic brain injury in Austria VI: effects of guideline-based management. Wien Klin Wochenschr. 2007;119(1–2):64–71. doi: 10.1007/s00508-006-0765-0. [DOI] [PubMed] [Google Scholar]
- 9.Adelson PD, Bratton SL, Carney NA, Chesnut RM, du Coudray HE, Goldstein B, Kochanek PM, Miller HC, Partington MP, Selden NR, et al. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents. Pediatr Crit Care Med. 2003;4(3 Suppl):S1–75. doi: 10.1097/01.CCM.0000066600.71233.01. [DOI] [PubMed] [Google Scholar]
- 10.Kochanek PM, Carney N, Adelson PD, Ashwal S, Bell MJ, Bratton S, Carson S, Chesnut RM, Ghajar J, Goldstein B, et al. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents--second edition. Pediatr Crit Care Med. 2012;13(Suppl 1):S1–82. doi: 10.1097/PCC.0b013e31823f435c. [DOI] [PubMed] [Google Scholar]
- 11.Vavilala MS, Kernic MA, Wang J, Kannan N, Mink RB, Wainwright MS, Groner JI, Bell MJ, Giza CC, Zatzick DF, et al. Acute Care Clinical Indicators Associated With Discharge Outcomes in Children With Severe Traumatic Brain Injury. Crit Care Med. 2014;42(10):2258–66. doi: 10.1097/CCM.0000000000000507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Copes WS, Champion HR, Sacco WJ, Lawnick MM, Gann DS, Gennarelli T, MacKenzie E, Schwaitzberg S. Progress in characterizing anatomic injury. J Trauma. 1990;30(10):1200–7. doi: 10.1097/00005373-199010000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Bureau of Labor Statistics. Consumer price index for medical care. [cited 2015 08 July]. Available from: http://www.bls.gov/cpi/cpi_dr.htm.
- 14.Diehr P, Yanez D, Ash A, Hornbrook M, Lin DY. Methods for analyzing health care utilization and costs. Annu Rev Public Health. 1999;20:125–44. doi: 10.1146/annurev.publhealth.20.1.125. [DOI] [PubMed] [Google Scholar]
- 15.Penner SJ. Introduction to Health Care Economics and Financial Management: Fundamental Concepts with Practical Applications. Philadelphia: Lippincott Williams & Wilkins; 2004. [Google Scholar]
- 16.Letton C, Cheung C, Nordin A. Does an enhanced recovery integrated care pathway (ICP) encourage adherence to prescribing guidelines, accelerate postoperative recovery and reduce the length of stay for gynaecological oncology patients? J Obstet Gynaecol. 2013;33(3):296–7. doi: 10.3109/01443615.2012.758693. [DOI] [PubMed] [Google Scholar]
- 17.Wagner EH, Coleman K, Reid RJ, Phillips K, Sugarman JR. Guiding Transformation: How Medical Practices Can Become Patient-Centered Medical Homes. Vol. 2012. The Commonwealth Fund; Feb 27, 2012. Report No. [Google Scholar]
- 18.Sherr K, Gimbel S, Rustagi A, Nduati R, Cuembelo F, Farquhar C, Wasserheit J, Gloyd S. Systems analysis and improvement to optimize pMTCT (SAIA): a cluster randomized trial. Implement Sci. 2014;9:55. doi: 10.1186/1748-5908-9-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hebert PL, Liu CF, Wong ES, Hernandez SE, Batten A, Lo S, Lemon JM, Conrad DA, Grembowski D, Nelson K, et al. Patient-centered medical home initiative produced modest economic results for Veterans Health Administration, 2010–12. Health Aff (Millwood) 2014;33(6):980–7. doi: 10.1377/hlthaff.2013.0893. [DOI] [PubMed] [Google Scholar]
- 20.Koeck C. Time for organisational development in healthcare organisations. Improving quality for patients means changing the organisation. BMJ. 1998;317(7168):1267–8. doi: 10.1136/bmj.317.7168.1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shortell SM, Rundall TG, Hsu J. Improving patient care by linking evidence-based medicine and evidence-based management. JAMA. 2007;298(6):673–6. doi: 10.1001/jama.298.6.673. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.