Abstract
Local anesthesia forms the backbone of pain control techniques and is necessary for a painless dental procedure. Nevertheless, administering a local anesthetic injection is among the most anxiety-provoking procedures to children. This study was performed to compare the efficacy of different distraction techniques (passive, active, and passive-active) on children’s pain perception during local anesthesia administration. A total of 90 children aged four to nine years, requiring inferior alveolar nerve block for primary molar extraction, were included in this study and randomly divided into three groups according to the distraction technique employed during local anesthesia administration. Passive distraction group: the children were instructed to listen to a song on headphones; Active distraction group: the children were instructed to move their legs up and down alternatively; and Passive-active distraction group: this was a combination between both techniques. Pain perception during local anesthesia administration was evaluated by the Sounds, Eyes, and Motor (SEM) scale and Wong Baker FACES® Pain Rating Scale. There was an insignificant difference between the three groups for SEM scale and Wong Baker FACES Pain Rating Scale at P = 0.743 and P = 0.112 respectively. The examined distraction techniques showed comparable results in reducing pain perception during local anesthesia administration.
Keywords: Active; Children; Distraction; Local anesthesia; Pain perception; Passive, Passive-active
Introduction
Effective pain control during dental treatment of a pediatric patient is the cornerstone for successful behavior guidance [1]. Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage [2]. Prevention of pain can nurture the relationship between the dentist and the child, build trust, allay fear and anxiety, and enhance positive dental attitudes for future visits. However, the subjective nature of pain perception, and lack of use of accurate pain assessment scales may oppose successful pain management procedures [3].
Local anesthesia forms the backbone of pain control techniques and is necessary for a painless dental procedure. Nevertheless, administering a local anesthetic injection is among the most anxiety-provoking procedures to children [4]. Thus, several methods have been suggested to reduce pain caused by administration of local anesthetic agents, and these include application of topical analgesic, distraction techniques, counter irritation, warming the anesthetic agents, adjusting the rate of injection, and buffering the local anesthetic agent [5], [6], [7].
Distraction is a behavior management technique that successfully reduces pain and behavioral distress by diverting children’s attention away from painful stimuli during invasive dental procedures. It is most effective when adapted to the developmental level of the child. Distraction appears to be safe and inexpensive; moreover, it can lead to the reduction in procedure duration, and the number of staff required for the procedure [8], [9], [10].
Distraction is divided into two main categories: passive distraction, which calls for the child to remain quiet while the dental health care professional is actively distracting him. Passive distraction includes watching videos, listening to music on headphones, reading a book to the child, or telling him a story. Active distraction, on the other hand, encourages the child’s participation in the activities during the procedures. Active techniques include singing songs, squeeze balls, relaxation breathing, and playing with electronic devices [9], [11].
Thus, this study was conducted to compare the efficacy of different distraction techniques (passive, active, and passive-active) on children’s pain perception during local anesthesia administration.
Methodology
This study was carried out in Pediatric Dentistry and Dental Public Health Department, Faculty of Oral and Dental Medicine, Cairo University. The ethical clearance for the study was obtained from the ethical committee of the institution. The parents were informed about the aim of the study and associated procedures. The written informed consents were obtained from the parents prior to the study.
Sample size was estimated based on a previous study [12]. The minimum required sample size was calculated to be 87 (29 in each group) to be sufficient to detect effect size of f = 0.432, a power of 95%, and a significance level of 5%. Sample size estimation was done by PASS 2008 (Version 0.8.0.15, For Windows).
A total of 90 children aged four to nine years, requiring inferior alveolar nerve block for the purpose of mandibular primary molar extraction, and who had demonstrated “positive” to “definitely positive” behavior (Frankl 3 or 4), were included in this study, regardless their previous dental experiences.
The study sample was randomly divided into three equal groups 30 children each: Passive distraction group: the children were instructed to listen to the same song on headphones; Active distraction group: the children were instructed to move their legs up and down alternatively as a sort of playing a game together; and Passive-active distraction group: this was a combination between passive and active distraction (the children were instructed to listen to a song on headphones while moving their legs up and down alternatively). The distraction techniques were employed during the administration of local anesthesia.
The study was conducted by two pediatric dentists. One of them gave all explanations, spoke with the children and carried out the anesthesia procedure and the other was observing and assessing the children’s pain perception.
Prior to inferior alveolar nerve block administration, topical anesthetic cream (PRILA 5% cream containing lidocaine 2.5%w/w and prilocaine 2.5%w/w, Middle East Pharmaceutical Industries Co. Ltd., Avalon Pharma, Riyadh-KSA, Saudi Arabia) was applied to the injection site approximately 30 s before the procedure. The technique used for administration of the anesthesia involved gradual injection of 1 mL of anesthetic agent Mepecaine-L (Mepivacaine 31.36 mg/1.8 mL and Levonordefrin 0.09 mg/1.8 mL, Alexandria Co., for Pharmaceuticals & Chemical Industries, Alexandria, Egypt) using a short needle (length: 32 mm, gauge: 27) over a period of one minute. Subsequently, extraction of the indicated primary molar was performed.
Pain perception during administration of local anesthesia was assessed by the Sounds, Eyes, and Motor (SEM) scale [13] and Wong Baker FACES Pain Rating Scale [14]. Sounds, Eyes, and Motor (SEM) scale shown in Table 1 was used to assess the observed pain. It is divided into two categories of comfort and discomfort. The discomfort response is further divided into three subscales: mild pain, moderate pain and severe pain.
Table 1.
The Sounds, Eyes, and Motor (SEM) scale for measuring the comfort or discomfort.
| Observations | Comfort | Discomfort |
||
|---|---|---|---|---|
| Mild pain | Moderate pain | Severe pain | ||
| Sounds | No sounds indicating pain | Nonspecific sounds; possible pain indication | Specific verbal complaints, e.g., “OW”, raises Voice | Verbal complaint indicates intense pain, e.g., scream, sobbing |
| Eyes | No eye signs indicating discomfort | Eyes wide, show of concern, no tears | Watery eyes, eyes flinching | Crying, tears running down face |
| Motor | Hands relaxed; no apparent body tension | Hands show some distress or tension, grasps chair due to discomfort, muscular tension | Random movement of arms or body without aggressive intention of physical contact, grimace, twitch | Movement of hands to make aggressive physical contact, e.g., punching, pulling head away |
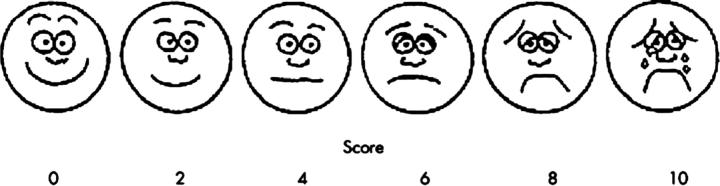
Wong Baker FACES Pain Rating Scale is a self-reported pain scale, and consists of a number of faces ranging from happy to crying. The scale was explained and shown to the children then they were asked to point out the face which indicated the pain level they experienced during administration of local anesthesia as illustrated in Fig 1.
Fig. 1.
Wong Baker FACES Pain Rating Scale.
Statistical analysis
Data were statistically described in terms of mean, standard deviation (±SD), frequency (n) and Percentage (%) when appropriate. One way ANOVA was used to compare between tested groups on mean Age. A non-parametric Kruskal Wallis test was used to compare between tested groups for SEM Score and Face pain Score. Spearman’s rho correlation between SEM Scale and Face pain Scale. Statistical analysis was performed with IBM® SPSS® (SPSS Inc., IBM Corporation, NY, USA) Statistics Version 22 for Windows.
Results
90 children were enrolled in this study with age range from four to nine years. The means of age in passive, active, and passive-active groups were 7.18 ± 1.94, 7.02 ± 2.2 and 7.65 ± 1.8 years, respectively. There was no significant difference in children’s age among the three groups (P = 0.444).
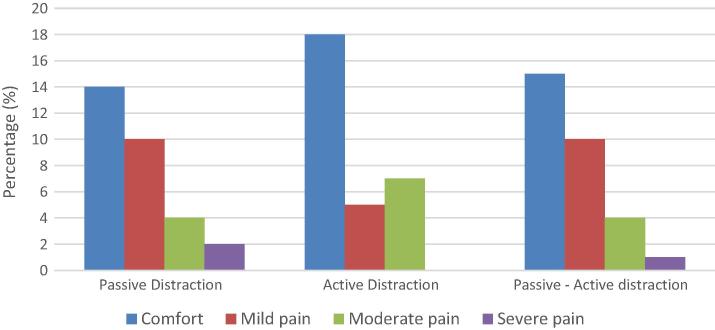
SEM scale findings are presented in Table 2. Children in active distraction group exhibited the greatest percentage (60%) of comfort score, followed by passive-active distraction group (50%) while passive distraction group demonstrated the least percentage of comfort score (46.7%). However, there was no statistically significant difference between the three groups for SEM scale scores at P = 0.743 as shown in Table 2 and Fig 2.
Table 2.
Sounds, Eyes, and Motor (SEM) Scale scores for the three distraction groups.
| SEM scale (n [%]) | Passive distraction (n = 30) | Active distraction (n = 30) | Passive-active distraction (n = 30) | P-value |
|---|---|---|---|---|
| Comfort | 14 (46.7%) | 18 (60%) | 15 (50%) | 0.743 NS |
| Mild pain | 10 (33.3%) | 5 (16.7%) | 10 (33.3%) | |
| Moderate pain | 4 (13.3%) | 7 (23.3%) | 4 (13.3%) | |
| Severe Pain | 2 (6.7%) | 0 (0.0%) | 1 (3.3%) |
P-value: 0.743 NS (non-significant).
Fig. 2.
Sounds, Eyes, and Motor (SEM) Scale scores for the three distraction groups.
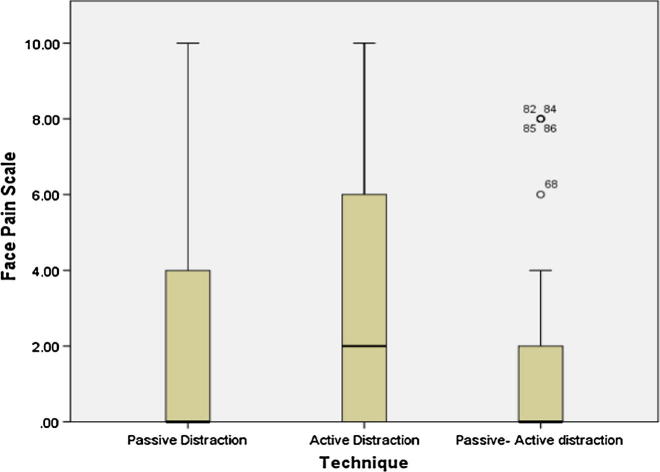
Wong Baker FACES Pain Rating Scale findings are presented in Table 3. Passive-active distraction group showed the lowest mean of the face pain scale which was 1.67 ± 2.93. There was no significant difference between the three groups for Wong Baker FACES Pain Rating Scale at P = 0.112 as shown in Table 3 and Fig 3.
Table 3.
Mean, standard deviation (SD), median, percentiles for the Wong Baker FACES Pain Rating Scale in the three groups.
| Technique |
P-value | ||||
|---|---|---|---|---|---|
| Passive distraction | Active distraction | Passive-active distraction | |||
| Wong Baker FACES Pain Rating Scale | Mean | 2.07 | 3.33 | 1.67 | 0.112 NS |
| SD | 2.70 | 3.73 | 2.93 | ||
| SE | 0.49 | 0.68 | 0.53 | ||
| Median | 0.00 | 2.00 | 0.00 | ||
| Percentiles (25) | 0.00 | 0.00 | 0.00 | ||
| Percentiles (50) | 0.00 | 2.00 | 0.00 | ||
| Percentiles (75) | 4.00 | 6.00 | 2.00 | ||
| Mode | 0.00 | 0.00 | 0.00 | ||
| Min. | 0.00 | 0.00 | 0.00 | ||
| Max. | 10.00 | 10.00 | 8.00 | ||
P-value: 0.112 NS (non-significant).
Fig. 3.
Box-plot for the Wong Baker FACES Pain Rating Scale scores for three distraction groups.
In this study the correlations between the SEM scale (observed pain) and Wong Baker FACES Pain Rating Scale (self-reported pain) presented in Fig 4 revealed that there was a significant positive relationship between SEM Scale and Face Pain Scale scores with rs = 0.357, P (2-tailed) = 0.001.
Fig. 4.
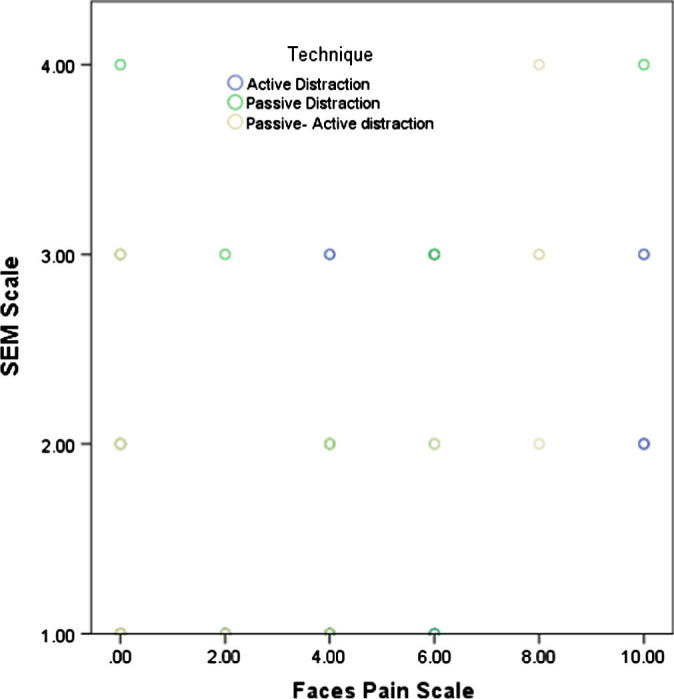
Scatterplot for the correlation between SEM Scale and Face Pain Scale.
Discussion
Pain control is one of the most important aspects in administration of local anesthesia in dental practice particularly in children [15]. Thus, several procedural, behavioral, and pharmacological strategies have been proposed to alleviate pain and discomfort during pediatric dental treatment.
This study was conducted to compare the effect of different distraction techniques (passive, active, and combination) on children’s pain perception during local anesthesia administration.
The children included in this study demonstrated positive or definitely positive behavior during pretreatment evaluation (ranking 3 or 4 in the Frankl scale). The choice of the children was based on their present behavior regardless of their previous dental experiences.
Child dental fear and anxiety are considered multifactorial in nature. Different factors have been proposed that can stimulate, provoke and promote dental anxiety in children. These factors include and not limited to parent–child relationship, parental dental anxiety, parental attitudes and perceptions regarding child’s behavior, parent’s past dental experiences, parental presence in the dental operatory, chronological age of the child, intellectual development of the child, medical and dental history of the child, child’s awareness of dental problem, and behavior of dental team. All these factors interact together affecting the child behavior, as we were examining the efficacy of distraction techniques rather than the psychological background of the children in this study; thus, the children were selected based on their cooperation and present behavior [16], [17].
The children were not selected based on their gender as gender was not discussed by Wright [17] as a factor affecting the children behaviors in dental clinic. Moreover, many studies proved that there was no significant difference between boys and girls in pain perception in children [4], [8], [18].
In this study, local anesthesia administration in all children was performed by the same operator while pain perception was assessed by another pediatric dentist in order to provide optimal standard conditions for accurate comparison between the distraction techniques.
In the present study, inferior alveolar nerve block was chosen to compare the distraction techniques as blocking the inferior alveolar nerve in children was claimed to be one of the most painful and stressful procedures in pediatric dentistry [19].
The active distraction technique employed in this study is a modification of a similar technique utilized by Kamath [20]. This technique appears to be simple, time saving, inexpensive and gives rise to an effective relaxed experience in short painful dental procedure (local anesthesia administration). Moreover, this technique can be easily used on the large number of children attending the clinic of Pediatric Dentistry and Dental Public Health Department, Faculty of Oral and Dental Medicine, Cairo University.
The perceived pain during local anesthesia administration was compared using observed ratings of pain and behavioral distress (SEM scale) as well as self-reports of pain (Wong-Baker FACES Pain Scale) [21]. Observing children’s behavior during dental treatment is essential in pain evaluation, as their facial expressions, crying, complaining, and body movements are important diagnostic criteria [3], [14].
The use of a self-reported pain intensity scale is also beneficial for children, as this scale features facial expressions to help the children to express how they feel. Wong-Baker FACES Pain Scale was used according to guidelines of American Academy of Pediatric Dentistry (2014–2015) which recommends its use for children over three years of age due to its well established reliability and validity [3].
The results of the present study showed that there was no statistically significant difference between the compared distraction techniques neither in SEM scale scores nor in Wong-Baker FACES Pain Scale scores, and this may be related to either the operator experience, or the effectiveness of distraction as a behavioral management technique in minimizing procedural pain, fear, and distress by reducing the sensory and affective components of pain [17].
However, active distraction demonstrated the greatest percentage (60%) of comfort score as evaluated using the SEM scale, and this is because active distraction involves multiple sensory modalities (auditory, and kinesthetic), active emotional involvement, and participation of the patient to compete with the signals from the noxious stimuli [8].
Though, active–passive distraction combines active engagement of the children in the distraction process together with listening to music, this group showed a lesser percentage of comfort score (50%) when compared to active distraction group using SEM scale (observed pain), and this may be due to the children’s confusion and inability to give full attention to the employed distraction techniques. However, this technique revealed the lowest mean of the Wong-Baker FACES Pain Scale (self-reported pain) which indicates that the children enjoyed the dual effect of active–passive distraction by being actively involved in moving their legs together with listening to music.
The overall correlation of SEM scale (observed pain), and Wong-Baker FACES Pain Scale (self-reported pain) in the three groups showed a significant positive relationship between the two scales. Children’s ratings of their pain were directly related to the scores recorded by the observing pediatric dentist, thereby strengthening the validity of the scales utilized to assess the observed and the self-reported pain.
Conclusions
The examined distraction techniques showed comparable results in reducing pain perception during local anesthesia administration. Both SEM scale (observed pain), and Wong-Baker FACES Pain Scale (self-reported pain) revealed similar presentation of children’s pain perception during local anesthesia administration.
Conflict of interest
The authors have declared no conflict of interest.
Acknowledgment
The authors would like to thank Dr. Ahmed Abdulrahman for his statistical assistance.
Footnotes
Peer review under responsibility of Cairo University.
References
- 1.Ashkenazi M., Blumer S., Eli I. Effectiveness of computerized delivery of intrasulcular anesthetic in primary molars. J Am Dent Assoc. 2005;136:1418–1425. doi: 10.14219/jada.archive.2005.0056. [DOI] [PubMed] [Google Scholar]
- 2.Second Y.L.K., Neelakantan P. Local anesthetics in dentistry-newer methods of delivery. Int J Pharm Clin Res. 2014;6(1):4–6. [Google Scholar]
- 3.American Academy of Pediatric Dentistry. Guideline on behavior guidance for the pediatric dental patient. Reference Manual; Pediatr Dent 2014–2015;36(6):180–90.
- 4.Lee S.H., Lee N.Y. An alternative local anaesthesia technique to reduce pain in paediatric patients during needle insertion. Eur J Paediatr Dent. 2013;14(2):109–112. [PubMed] [Google Scholar]
- 5.Aminabadi N.A., Farahani R.M.Z. The effect of pre-cooling the injection site on pediatric pain perception during the administration of local anesthesia. J Contemp Dent Pract. 2009;10(3):1–9. [PubMed] [Google Scholar]
- 6.Yesilyurt C., Bulut G., Taşdemir T. Pain perception during inferior alveolar injection administered with the Wand or conventional syringe. Br Dent J. 2008;E10:1–4. doi: 10.1038/sj.bdj.2008.757. [DOI] [PubMed] [Google Scholar]
- 7.Leyda A.M., Liena C. Comparison of eutectic mixture of lidocaine/prilocain versus benzocaine gel in children. Open J Stomat. 2011;1:84–91. [Google Scholar]
- 8.Aminabadi N.A., Erfanparast L., Sohrabi A., Oskouei S.G., Naghili A. The impact of virtual reality distraction on pain and anxiety during dental treatment in 4–6 year-old children: a randomized controlled clinical trial. J Dent Res Dent Clin Dent Prospect. 2012;6(4):117–124. doi: 10.5681/joddd.2012.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Srouji R., Ratnapalan S., Schneeweiss S. Pain in children: assessment and nonpharmacological management. Int J Pediatr. 2010:1–11. doi: 10.1155/2010/474838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh H., Rehman R., Kadtane S., Dalai D.R., Jain C.D. Techniques for the behaviors management in pediatric dentistry. Int J Sci Stud. 2014;2(7):269–272. [Google Scholar]
- 11.Law E.F., Dahlquist L.M., Sil S., Weiss K.E., Herbert L.J., Wohlheiter K. Videogame distraction using virtual reality technology for children experiencing cold pressor pain: the role of cognitive processing. J Pediatr Psychol. 2011;36(1):84–94. doi: 10.1093/jpepsy/jsq063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aitken J.C., Wilson S., Coury D., Moursi A.M. The effect of music distraction on pain, anxiety and behavior in pediatric dental patients. Pediatr Dent. 2002;24(2):114–118. [PubMed] [Google Scholar]
- 13.Wright G.Z., Weinberger S.J., Marti R., Plotzke O. The effectiveness of infiltration anesthesia in the mandibular primary molar region. Pediatr Dent. 1991;13:278–283. [PubMed] [Google Scholar]
- 14.Wong L.D., Baker C.M. Pain in children: comparison of assessment scales. Pediatr Nurs. 1988;14(1):9–17. [PubMed] [Google Scholar]
- 15.Shahidi Bonjar A.H. Syringe micro vibrator (SMV) a new device being introduced in dentistry to alleviate pain and anxiety of intraoral injections, and a comparative study with a similar device. Ann Surg Innov Res. 2011:1–5. doi: 10.1186/1750-1164-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Suprabha B.S., Rao Arathi. Role of parent in behavior guidance of children in dental operatory: current trends. Int J Adv Res. 2015;3(1):466–470. [Google Scholar]
- 17.Wright G.Z. Psychologic management of children’s behaviors. In: McDonald R.E., Avery D.R., editors. Dentistry for the child and adolescent. 7th ed. Mosby; 2000. pp. 34–51. [Google Scholar]
- 18.Versloot J., Veerkamp J.S.J., Hoogstraten J. Assessment of pain by the child, dentist, and independent observers. Pediatr Dent. 2004;26:445–449. [PubMed] [Google Scholar]
- 19.Costa R.S.M., Ribeiro S.N., Cabral E.D. Determinants of painful experience during dental treatment. Rev Dor São Paulo. 2012;13(4):365–370. [Google Scholar]
- 20.Kamath P.S. A novel distraction technique for pain management during local anesthesia administration in pediatric patients. J Clin Pediatr Dent. 2013;38(1):45–47. doi: 10.17796/jcpd.38.1.265807t236570hx7. [DOI] [PubMed] [Google Scholar]
- 21.Windich-Biermeier A., Sjoberg I., Dale J.C., Eshelman D., Guzzetta C.E. Effects of distraction on pain, fear, and distress during venous port access and venipuncture in children and adolescents with cancer. J Pediatr Oncol Nurs. 2007;24(1):8–19. doi: 10.1177/1043454206296018. [DOI] [PubMed] [Google Scholar]