Abstract
Background
Thoracic injury rule out criteria (TIRC) were first introduced as a decision instrument for selective chest radiography in blunt thoracic trauma in 2014. However, the validity of this model has not been assessed in other studies. In this regard, the present survey evaluates the validity of TIRC model in a multi-center setting.
Methods
In this cross-sectional study, clinical presentations and chest radiograms of multiple trauma patients referring to 6 educational hospitals in Iran were evaluated. Data were gathered prospectively during 2015. In each center, data collection and interpretation of radiograms were conducted by two different emergency medicine specialists. Measures were then taken for assessment of discriminatory power and calibration of the model.
Results
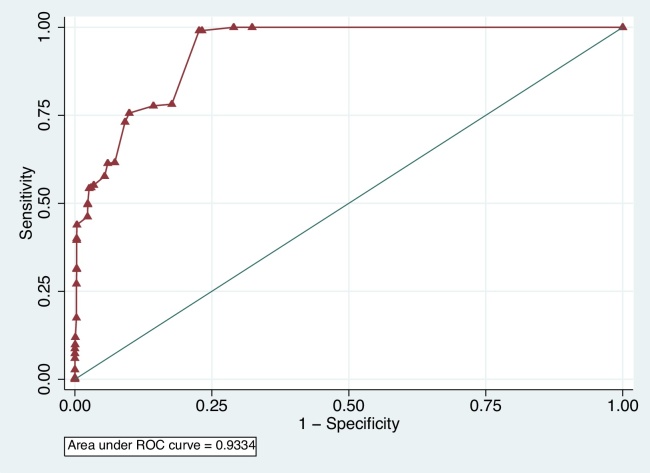
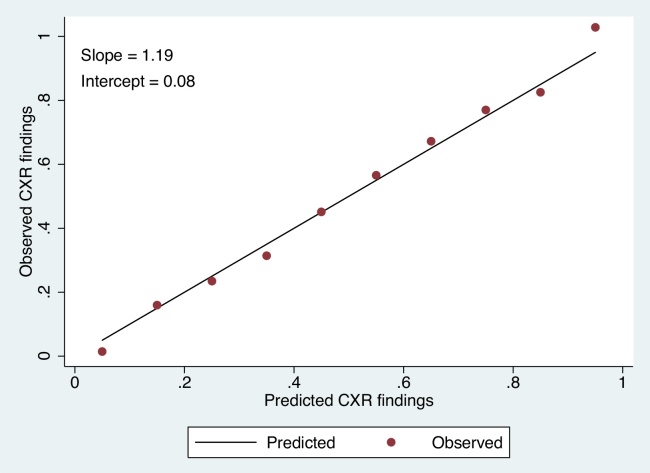
Data from 2905 patients were gathered (73.17% were male; the mean age was 33.53 ± 15.42 years). Area under the receiver operating characteristics curve of the TIRC model for detection of thoracic traumatic injuries was 0.93 (95%CI: 0.93–0.94). Sensitivity and specificity of the model were 100 (98.91–100) and 67.65 (65.76–69.45), respectively. The intercept of TIRC calibration plot was 0.08 (95%CI: 0.07–0.09), and its slope was 1.19 (95%CI: 1.15–1.24), which are indicative of the model being perfect in detecting presence or absence of lesions in chest radiograms.
Conclusion
The findings are corroborative of external validation, good discrimination, and proper calibration of TIRC model in screening of multiple trauma patients for obtaining chest radiograms.
Keywords: Thoracic trauma, Chest radiography, Scoring system
1. Background
Thoracic trauma as one of the most important causes of morbidity and mortality in the first four decades of life1, 2 is the cause for 25% of trauma-related deaths.3 Early diagnosis of these injuries can significantly decrease their burden. Radiology plays an important role in the assessment of trauma patients. In the past, the Advanced Trauma Life Support recommended that radiograms should be obtained from the chest, pelvis, and neck of all multiple trauma patients. However, recently it has limited the neck and pelvis radiograms to hemodynamically unstable patients or subjects with positive findings in their physical examinations.4 These changes are made based on the findings that suggest plain radiograms present little information useful for making decisions about the hemodynamically stable patients or subjects with negative cervical and pelvic physical examinations.5, 6, 7, 8, 9
Recently similar attempts have been made to decrease the burden of obtaining unnecessary radiograms in thoracic trauma. In this regard two different scoring systems of NEXUS chest and thoracic injury rule out criteria (TIRC) have been proposed by two separate research teams.10, 11 NEXUS chest, developed based on the data from 2628 patients referring to three trauma centers, is a 7-item scoring system that includes age of more than 60 years old, rapid deceleration mechanism (falling from a height of more than 20 ft or a motor vehicle accident with a speed of more than 40 mph), chest pain, intoxication, altered mental status, distracting painful injury and tenderness to chest wall palpitation as factors predictive of thoracic trauma. The validation study of this scoring system was conducted on 9905 patients.11 However, information about the rapid deceleration criterion is rarely available to the physicians. This is mainly due to inaccurate recording of information about the accidents by emergency medical services, particularly in developing countries, which can limit the application of this scoring system.
In 2014 Forouzanfar et al. develop the TIRC model based on the data gathered from 2608 patients referring to one trauma center. According to this model any of these factors can predict a thoracic lesion: age over 60, hemodynamic instability, Glasgow Coma Scale (GCS) lower than 15, crepitation, decrease in pulmonary sounds, pain and tenderness of the chest wall, thoracic skin abrasion, and dyspnea.10 As can be seen, this model does not have the limitations of NEXUS chest scoring system. However, the validity of the TIRC model has not been evaluated in another survey. Accordingly, in the present study, we aimed to assess the validity of TIRC model in a multi-center survey.
2. Methods
2.1. Study setting
In this cross-sectional survey conducted during 2015, clinical presentations and chest radiograms of multiple trauma patients referring to 6 educational hospitals in Iran were evaluated. The study protocol was approved by the ethics committee of Tehran University of Medical Sciences. All the researchers were committed to the principles of Helsinki's Declaration and informed written consent was obtained from all the included patients or their legal guardians.
2.2. Participants
Hemodynamically stable multiple trauma patients aged over 15 years were included through a consecutive sampling method. Exclusion criteria included being the subject of penetrating traumas and not willing to participate. These criteria were based on the study carried out by Forouzanfar et al.10
2.3. Data collection
Prospectively gathered data included information about demographic characteristics of the patients (age, gender, trauma mechanism) and findings of their physical examinations. Data were collected by the emergency medicine specialists. Subsequently chest radiograms were obtained from the subjects in two views of anteroposterior and lateral.
Physical examination of the patients further focused on presence of painful distracting injuries, altered mental status (GCS < 15), tachypnea, pain or tenderness in thoracic region, dyspnea, abrasion or wound caused by the trauma in chest region, deformity of the thorax, tenderness in upper abdominal region, crepitation in palpation, diminished pulmonary sounds, and subcutaneous emphysema.
Final diagnosis of thoracic injury was made based on chest radiography. Computed tomography scan (CT scan) was performed in 3.2% of patients, which were demanded by other specialists such as surgeons or internal medicine specialists. In these patients, final diagnosis was based on CT scan findings. Chest radiograms were interpreted by another emergency medicine specialist, blinded to the survey's objectives. Verification of these interpretations was done for 3% of the radiograms by a radiologist. The inter-tater agreement was calculated to be 98%. Abnormal findings of the chest-X rays (CXR) included pneumothorax, hemothorax, pulmonary contusion, pneumomediastinum, mediastinal widening, subcutaneous emphysema, and fractures of the ribs, sternum, clavicles and scapulas.
2.4. Statistical analysis
Sample size calculation was based on a 6.5% prevalence of thoracic lesions in multiple trauma patients12 considering a confidence interval of 95% (α = 0.05), a power of 90% (β = 0.1), and a maximum error of 1.5% (d = 0.015). The minimum number of patients required as the sample population was estimated to be 1038 subjects.
STATA software version 11.0 was used for data analysis. Qualitative variables are presented as frequencies and percentages and quantitative factors are presented as means and standard deviations. Validation of the model was performed using the methods proposed by recent review articles.13, 14 These methods assess the discriminatory power, calibration of a predictive model, or a combination of these two criteria. The discriminatory power was evaluated through calculating area under the curve of the receiver operating characteristic curve (ROC) and presenting the result as sensitivity, specificity and likelihood ratios. Based on TIRC cut off (presence of at least one criteria),10 data were presented as true positive (true prediction of presence of thoracic injury in CXR), true negative (true prediction of absence of thoracic injury in CXR), false positive (false prediction of presence of thoracic injury in CXR), and false negative (false prediction of absence of thoracic injury in CXR).
General calibration of the model was also evaluated through drawing a calibration plot, in which the numbers of observed and predicted CXR findings per decile of the linear predictor of the TIRC model were compared. In this plot, the perfect calibration is the reference line with an intercept of zero and a slope of 1. The overall performance was eventually assessed via the brier score in order to evaluate predictive accuracy and predictive reliability of the model.
3. Results
3.1. Baseline characteristics
Data were collected from a total of 2905 patients (73.17% were male; the mean age was 33.53 ± 15.42 years). The most prevalent trauma mechanisms were pedestrian (37.81%), car accidents (31.23%), motorcycle accidents (12.34%) and falling (14.03%). 312 patients (10.74%) presented with some levels of altered mental status, 732 subjects (25.20%) had thoracic pain, chest tenderness was found in 581 patients (20.0%) and 451 cases had thoracic skin abrasions (Table 1).
Table 1.
Baseline characteristics of studied patients.
| Variable | N (%) |
|---|---|
| Age (years) | |
| <60 | 2650 (91.22) |
| ≥60 | 255 (8.78) |
| Gender | |
| Male | 2125 (73.17) |
| Female | 779 (26.83) |
| Mechanism of traumaa | |
| Motorcycle accident | 358 (12.34) |
| Pedestrian | 1097 (37.81) |
| Car accident | 906 (31.23) |
| Falls | 407 (14.03) |
| Other | 133 (4.58) |
| Glasgow Coma Scale | |
| 15 | 2593 (89.26) |
| Less than 15 | 312 (10.74) |
| Dyspnea | |
| Yes | 458 (15.77) |
| No | 2447 (84.23) |
| Distracting pain | |
| Yes | 1162 (40.0) |
| No | 1743 (60.0) |
| Thoracic skin abrasion | |
| Yes | 451 (15.52) |
| No | 2454 (84.48) |
| Chest deformity | |
| Yes | 50 (1.72) |
| No | 2855 (98.28) |
| Chest wall tenderness | |
| Yes | 581 (20.0) |
| No | 2324 (80.0) |
| Crepitation | |
| Yes | 122 (4.20) |
| No | 2783 (95.8) |
| Abdominal tenderness | |
| Yes | 444 (15.28) |
| No | 2461 (84.72) |
| Decrease in pulmonary sounds | |
| Yes | 172 (5.92) |
| No | 2733 (94.08) |
| Chest wall pain | |
| Yes | 732 (25.20) |
| No | 2173 (74.80) |
Motorcycle accident: including motorcycle–car accident and motorcycle–motorcycle accident. Pedestrian: including accident of pedestrian with motorcycle of car. Car accident: including car–car accident and car rollover.
3.2. Discrimination
Area under the ROC curve of the TIRC model in predicting thoracic injuries was 0.93 (95%CI: 0.93–0.94) (Fig. 1). Table 2 presents the sensitivity and specificity of this rule out criteria in different cut-off points. Considering the presence of at least one of the criteria proposed by TIRC model resulted in 435 true positive, 1671 true negative and 799 false positive cases. No cases were false negative. Accordingly, the sensitivity and specificity were calculated to be 100 (98.91–100) and 67.65 (65.76–69.45), respectively. Positive and negative likelihood ratios for the TIRC model were also found to be 3.09 and 0.
Fig. 1.
Area under the curve of the TIRC model.
Table 2.
Sensitivity, specificity, positive likelihood ratio (LR+) and negative likelihood ratio (LR−) of the thoracic injury rule out criteria (TIRC) at various cut-off points.
| Cut point | Sensitivity | Specificity | LR+ | LR− |
|---|---|---|---|---|
| ≥0 | 100.0 | 0.0 | 1.0 | – |
| ≥0.5 | 100.0 | 67.7 | 3.1 | 0.0 |
| ≥1 | 100.0 | 71.0 | 3.4 | 0.0 |
| ≥2 | 99.1 | 77.3 | 4.4 | 0.0 |
| ≥3 | 77.7 | 85.7 | 5.4 | 0.3 |
| ≥4 | 73.1 | 90.9 | 8.0 | 0.3 |
| ≥5 | 61.4 | 94.0 | 10.2 | 0.4 |
| ≥6 | 55.2 | 96.6 | 16.0 | 0.5 |
| ≥7 | 54.3 | 97.4 | 20.9 | 0.5 |
| ≥8 | 49.7 | 97.7 | 21.1 | 0.5 |
| ≥9 | 43.9 | 99.6 | 120.5 | 0.6 |
| ≥10 | 39.5 | 99.7 | 122.1 | 0.6 |
| ≥11 | 31.3 | 99.7 | 96.5 | 0.7 |
| ≥12 | 17.5 | 99.7 | 61.6 | 0.8 |
| ≥13 | 9.9 | 100.0 | 244.2 | 0.9 |
| ≥15 | 6.0 | 100.0 | – | 0.9 |
| ≥16 | 0.5 | 100.0 | – | 1.0 |
3.3. Calibration
Fig. 2 presents the calibration plot for the TIRC model and shows the observed and predicted CXR positive findings per decile of the linear predictor of the model. The perfect calibration is the reference line with an intercept of zero and a slope of 1, which is indicated by a continuous black line in Fig. 2. The TIRC calibration plot (scatter plot) had an intercept equal to 0.08 (95%CI: 0.07–0.09) and a slope of 1.19 (95%CI: 1.15–1.24). As can be seen the TIRC model showed a close adherence to the reference line, which indicates that the model is perfect in predicting the presence or absence of a lesion in CXRs.
Fig. 2.
The calibration plot for the TIRC model.
3.4. Overall performance
Brier score for the TIRC model was 0.07 and its scaled reliability was calculated to be 0.002. These figures are indicative of the high predictive accuracy and reliability of the model.
4. Discussion
The findings of this study confirm the external validation, good discrimination, and good calibration of the TIRC model in screening the multiple trauma patients for obtaining chest radiograms. The present survey was the first to evaluate the validity of the TIRC model in a multi-center setting, while its derivation study was conducted on 2600 subjects referring to a single center.10 Therefore, generalization of the model was considered as one of the limitations in their study10 till the present survey found a similar validity for the model through a multi-center approach.
In comparison, both the NEXUS chest and the TIRC model have acceptable sensitivities in detection of thoracic traumatic injuries. In the NEXUS chest validation study, Rodriguez et al. reported its sensitivity to be 98.8%.11 The present survey found a sensitivity of 100% for the TIRC model. The present survey found a sensitivity of 100% for the TIRC model. Therefore, it seems that obtaining CXR is not necessary in stable multiple blunt trauma patients, who are conscious, under 60 years, or have no decrease in pulmonary sounds, dyspnea, thoracic skin abrasions, and crepitation. Although the sample size of this survey is far less than the sample population included the study of Rodriguez et al.; however, the very fitting calibration of the TIRC model presented in this study indicates that the model can perfectly detect the presence or absence of injuries.
Few studies have aimed to develop scoring systems for detection of blunt thoracic injuries. In the most important one, Bokhari et al. stated that patients with blunt traumas to the thoracic region, who are hemodynamically stable and their physical examinations are normal there is no need for chest radiography. In the rest of their study these researchers show that abnormal breath sounds in pulmonary auscultation, pain or tenderness of the chest wall and tachypnea have sensitivities of 100%, 57.1% and 42.8% in detection of hemopneumothorax, respectively. Although the negative predictive values of the two latter factors are more than 99%.15 Wisbach et al. also showed that in hemodynamically stable patients with normal physical examination of the thorax, chest radiography is unnecessary. This study declared that chest radiography should only be performed, if an evident clinical indication is present, similar to the way that cervical and pelvic radiographies are approached.12 On the other hand, Dubinsky and Low believed that clinical presentation of the patient is not a suitable prognostic factor for detection of thoracic injuries in blunt traumas. However, most of the injuries in their study were rib fractures, and none of the patients had hemopneumothorax; therefore, their results might be subject to selection bias.16 Based on the results of the present study and other surveys on this matter, it can be concluded that in most cases scoring systems can be utilized in order to avoid unnecessary radiographies. In this regard, TIRC as an accurate scoring system is recommended to be used to order CXR for multiple trauma patients.
It should also be kept in mind that overall the diagnostic yield of chest radiography is not very high in detection of thoracic traumatic injuries. In this regard, the 5 meta-analyses performed by the authors of this survey showed that ultrasonography has higher sensitivity and specificity in detection of pneumothorax, hemothorax, pulmonary contusion, fracture, and pleural effusion compared to chest radiography.17, 18, 19, 20 Accordingly, the application of chest radiography in detection of thoracic injuries might be better re-evaluated and replaced with ultrasonography. However, studies with larger sample populations are needed to make decisions regarding this issue.
The large sample population and the multi-center setting can be pointed out as strengths of the present study. The number of included patients was approximately three times the minimum number required for the survey, which warrants the power of the study. Moreover, the included subjects are from four different cities that confirms that the results could be generalized to the total population. However, presence of selection bias is not fully avoidable. Furthermore, the event of radiograms having been interpreted by multiple physicians rather than a single one was another limitation of this study. Nevertheless, in order to verify these interpretations, 5% of the CXRs were evaluated and interpreted by a blinded radiologist for the second time. The inter-rater reliability was calculated to be 98%, which was congruent with the results of other similar surveys confirming the validity of CXR interpretations made by emergency medicine specialists.21 Finally, the presence of occult pneumothorax in our study was unavoidable, because not all of our patients received CT scan.
5. Conclusion
The findings confirmed the external validation, good discrimination, and good calibration of the TIRC model in screening of multiple trauma patents for chest radiography. The present survey was the first to validate the TIRC model in a multi-center setting that warrants its applicability in all the patients with thoracic traumatic injuries.
Author contributions
Study design and concerting: S.S., M.Y., M.H., V.R.-M.; data gathering: S.A., N.M., A.M.J., A.T.; data analysis: M.H., M.B., P.Gh., S.S.; drafting: M.Y., M.B., P.Gh.; other authors critically revised the manuscript.
Funding
This research has been supported by Tehran University of Medical Sciences & Health Services grant number: 93-02-38-25619.
Conflicts of interest
The authors have none to declare.
Acknowledgments
We appreciate very much Dr. Abolfazl Darafarin and Dr. Ahmadreza Sabouri for their invaluable cooperation in data collection.
References
- 1.Hill A., Fowler R., Pinto R., Nathens A. Epidemiology of major trauma: a Canadian perspective. Can J Surg. 2011;54(3):S45. [Google Scholar]
- 2.Søreide K. Epidemiology of major trauma. Br J Surg. 2009;96(7):697–698. doi: 10.1002/bjs.6643. [DOI] [PubMed] [Google Scholar]
- 3.Heron M. vol. 60. 2012. pp. 1–94. (Deaths: Leading Causes for 2008. National Vital Statistics Reports: From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System). [PubMed] [Google Scholar]
- 4.Kool D.R., Blickman J.G. Advanced Trauma Life Support®. ABCDE from a radiological point of view. Emerg Radiol. 2007;14(3):135–141. doi: 10.1007/s10140-007-0633-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abedi Khorasgani M., Shahrami A., Shojaee M., Alimohammadi H., Amini A., Hatamabadi H.R. The accuracy of plain radiography in detection of traumatic intrathoracic injuries. Emergency. 2015;4 [in press] [PMC free article] [PubMed] [Google Scholar]
- 6.Heydari F., Esmailian M., Dehghanniri M. Diagnostic accuracy of ultrasonography in the initial evaluation of patients with penetrating chest trauma. Emergency. 2014;2(2):81–84. [PMC free article] [PubMed] [Google Scholar]
- 7.Holder Y., Organization WH . World Health Organization; Geneva: 2001. Injury Surveillance Guidelines. [Google Scholar]
- 8.Taghizadieh A., Ala A., Rahmani F., Nadi A. Diagnostic accuracy of chest X-ray and ultrasonography in detection of community acquired pneumonia: a brief report. Emergency. 2014;3(3):114–116. [PMC free article] [PubMed] [Google Scholar]
- 9.Vafaei A., Hatamabadi H.R., Heidary K., Alimohammadi H., Tarbiat M. Diagnostic accuracy of ultrasonography and radiography in initial evaluation of chest trauma patients. Emergency. 2016;4(1):29–33. [PMC free article] [PubMed] [Google Scholar]
- 10.Forouzanfar M.M., Safari S., Niazazari M. Clinical decision rule to prevent unnecessary chest X-ray in patients with blunt multiple traumas. Emerg Med Aust. 2014;26(6):561–566. doi: 10.1111/1742-6723.12302. [DOI] [PubMed] [Google Scholar]
- 11.Rodriguez R.M., Anglin D., Langdorf M.I. NEXUS chest: validation of a decision instrument for selective chest imaging in blunt trauma. JAMA Surg. 2013;148(10):940–946. doi: 10.1001/jamasurg.2013.2757. [DOI] [PubMed] [Google Scholar]
- 12.Wisbach G.G., Sise M.J., Sack D.I. What is the role of chest X-ray in the initial assessment of stable trauma patients? J Trauma. 2007;62(1):74–78. doi: 10.1097/01.ta.0000251422.53368.a3. discussion 8–9. [DOI] [PubMed] [Google Scholar]
- 13.Bouwmeester W., Zuithoff N.P., Mallett S. Reporting and methods in clinical prediction research: a systematic review. PLOS Med. 2012;9(5):1–12. doi: 10.1371/journal.pmed.1001221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cook N.R. Statistical evaluation of prognostic versus diagnostic models: beyond the ROC curve. Clin Chem. 2008;54(1):17–23. doi: 10.1373/clinchem.2007.096529. [DOI] [PubMed] [Google Scholar]
- 15.Bokhari F., Brakenridge S., Nagy K. Prospective evaluation of the sensitivity of physical examination in chest trauma. J Trauma Acute Care Surg. 2002;53(6):1135–1138. doi: 10.1097/00005373-200212000-00017. [DOI] [PubMed] [Google Scholar]
- 16.Dubinsky I., Low A. Non-life-threatening blunt chest trauma: appropriate investigation and treatment. Am J Emerg Med. 1997;15(3):240–243. doi: 10.1016/s0735-6757(97)90004-8. [DOI] [PubMed] [Google Scholar]
- 17.Ebrahimi A., Yousefifard M., Kazemi H.M. Diagnostic accuracy of chest ultrasonography versus chest radiography for identification of pneumothorax: a systematic review and meta-analysis. Tanaffos. 2014;13(4):29–40. [PMC free article] [PubMed] [Google Scholar]
- 18.Hosseini M., Ghelichkhani P., Baikpour M. Diagnostic accuracy of ultrasonography and radiography in detection of pulmonary contusion: a systematic review and meta-analysis. Emergency. 2015;3(4):127–136. [PMC free article] [PubMed] [Google Scholar]
- 19.Rahimi-Movagha V., Yousefifard M., Ghelichkhani P. Application of ultrasonography and radiography in detection of hemothorax: a systematic review and meta-analysis. Emergency. 2015;4 [in press] [PMC free article] [PubMed] [Google Scholar]
- 20.Yousefifard M., Baikpour M., Ghelichkhani P. Screening performance characteristic of ultrasonography and radiography in detection of pleural effusion: a meta-analysis. Emergency. 2016;4(1):1–10. [PMC free article] [PubMed] [Google Scholar]
- 21.Safari S., Baratloo A., Negida A.S., Taheri M.S., Hashemi B., Selkisari S.H. Comparing the interpretation of traumatic chest X-ray by emergency medicine specialists and radiologists. Arch Trauma Res. 2014;3(4):e22189. doi: 10.5812/atr.22189. [DOI] [PMC free article] [PubMed] [Google Scholar]