Abstract
Background Burnout is common in internal medicine (IM) trainees and is associated with depression and suboptimal patient care. Facilitated group discussion reduces burnout among practicing clinicians.
Objective We hypothesized that this type of intervention would reduce incident burnout among first-year IM residents.
Methods Between June 2013 and May 2014, participants from a convenience sample of 51 incoming IM residents were randomly assigned (in groups of 3) to the intervention or a control. Twice-monthly theme-based discussion sessions (18 total) led by expert facilitators were held for intervention groups. Surveys were administered at study onset and completion. Demographic and personal characteristics were collected. Burnout and burnout domains were the primary outcomes. Following convention, we defined burnout as a high emotional exhaustion or depersonalization score on the Maslach Burnout Inventory.
Results All 51 eligible residents participated; 39 (76%) completed both surveys. Initial burnout prevalence (10 of 21 [48%] versus 7 of 17 [41%], P = .69), incidence of burnout at year end (9 of 11 [82%] versus 5 of 10 [50%], P = .18), and secondary outcomes were similar in intervention and control arms. More residents in the intervention group had high year-end depersonalization scores (18 of 21 [86%] versus 9 of 17 [53%], P = .04). Many intervention residents revealed that sessions did not truly free them from clinical or educational responsibilities.
Conclusions A facilitated group discussion intervention did not decrease burnout in resident physicians. Future discussion-based interventions for reducing resident burnout should be voluntary and effectively free participants from clinical duties.
Introduction
Burnout is common among resident physicians with grave potential consequences, including depression, suicidality,1,2 and suboptimal patient care.3 Factors predisposing residents to develop burnout include personality type, lack of performance feedback,4,5 and lack of a supportive work environment.6 Increased emotional support during training has the potential to prevent burnout in residents.
Potential benefits of physician support groups include promotion of personal awareness,7 improved teamwork and patient-caregiver relationships,8 emotional and spiritual support,9 and improved well-being related to coworker support.10 Facilitated discussion groups have also been shown to decrease burnout among practicing physicians.11 We hypothesized that a facilitated discussion group intervention could reduce burnout incidence among first-year internal medicine (IM) residents.
Methods
Setting
The study was performed in the IM residency program at the Icahn School of Medicine at Mount Sinai in New York. All incoming first-year IM residents were eligible to enter the study, which was conducted between June 2013 and May 2014. Power calculations based on prior research indicated that 60 participants would be necessary to minimize the likelihood of a Type I error to 0.05 when comparing burnout rates between the test and control groups. After participating residents consented to enroll, we clustered them into groups of 3 (“triplets”) based on clinical rotation schedule and randomly assigned the resulting triplets to the intervention or control arm.
Intervention
We based the intervention on a program in which practicing physician groups who met regularly with trained discussion group leaders to discuss topics related to stress, balance, and job satisfaction experienced decreased job burnout.11 Leaders assigned to each intervention arm triplet (9 groups) were psychotherapists with expertise in facilitating group discussion; psychotherapy was not part of the intervention. We purposely chose non-IM faculty to avoid any perception of evaluation or inhibition of discussion around sensitive topics. We asked groups to meet twice monthly on average between August 2013 and May 2014 for a total of 18 one hour-long sessions. Due to residency program requirements, we were unable to hold sessions in place of existing educational meetings. Each session was organized around a theme (eg, death and dying, coping mechanisms) with an accompanying session guide for group leaders that included teaching points, discussion questions, and associated readings. Group leaders were compensated $100 per session. Participating residents were provided a complimentary lunch and had no clinical duties during the sessions (though they carried pagers). Control arm residents were provided lunch vouchers.
Study Outcomes
Survey questions included basic demographic and personal characteristics, which were limited to maintain anonymity. We used the Maslach Burnout Inventory to measure 3 domains of burnout: emotional exhaustion (EE), depersonalization (DP), and feelings of decreased personal accomplishment (PA).12 Following convention, we defined burnout as a high EE or DP score.3
We administered the initial survey at intern orientation in June 2013, and the postsurvey following the completion of the intervention in May 2014. All residents in the intervention arm also met with study investigators after final surveys were completed to provide additional informal feedback.
The study received approval by the Icahn School of Medicine Institutional Review Board.
Statistical Analysis
We compared intervention and control group demographic data using univariate analyses. All metrics (eg, DP, EE) were dichotomized into high level versus all others; prevalues and postvalues were compared using chi-square analyses. Fisher exact test was utilized when cell sizes were small (n < 5). When comparing changes in scores, we analyzed data using analysis of variance techniques. SAS version 9.2 (SAS Institute Inc, Cary, NC) was used for data analysis.
Results
Response Rate
All 51 first-year residents entering the 2013–2014 IM residency program participated in the study. Twenty-seven belonged to triplet groups that were randomized to the intervention arm. A total of 39 (76%) residents completed the presurveys and postsurveys. Group leaders voluntarily and anonymously reported attendance for 85% of sessions. Mean individual resident attendance was 9 sessions (range, 7 to 15); however, this number modestly underestimates actual attendance in light of the incomplete attendance records.
Demographics
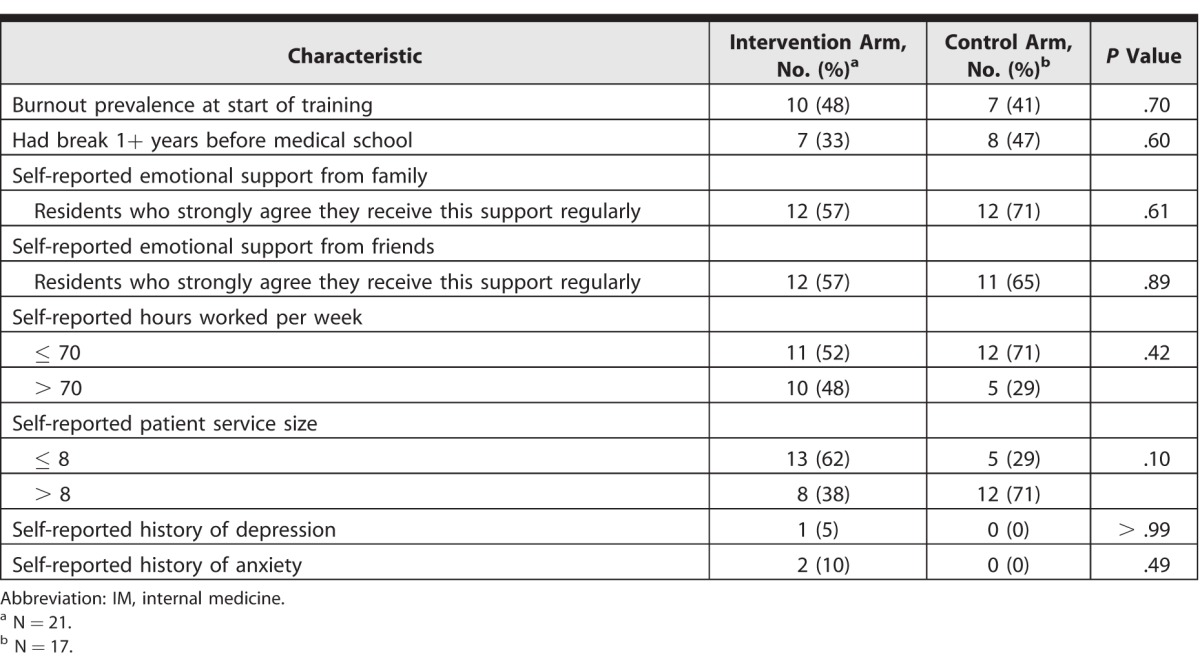
Groups were similar in terms of burnout prevalence at the start of training, break between undergraduate and medical school studies, self-reported emotional support, self-reported duty hours, service size, and history of depression or anxiety (table 1).
table 1.
Demographic Characteristics of IM Residents in Study Examining Impact of Facilitated Discussion on Burnout
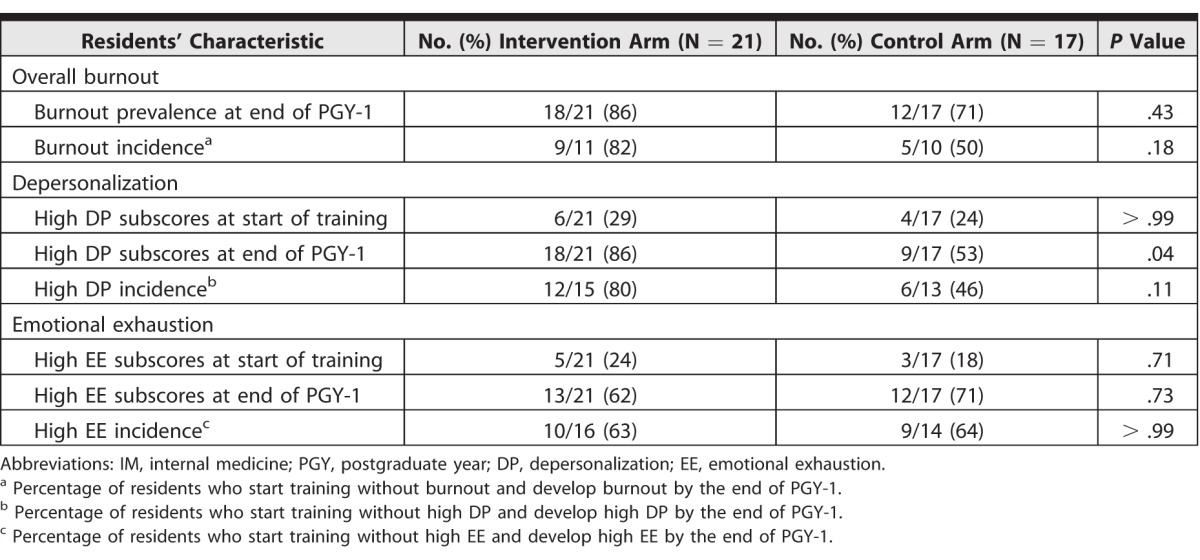
Development of Burnout
Rates of incident burnout as measured on the postsurvey did not differ between the study and control groups. The only significant difference was that more residents from the intervention arm had high depersonalization scores at study end, compared with the control arm (table 2).
table 2.
Burnout Incidence of IM Residents Participating in Study Examining Impact of Facilitated Discussion
Informal Feedback
Several consistent remarks emerged in the informal debriefing sessions held after the completion of the study. First, sessions did not effectively free residents from clinical responsibilities; instead they created an added burden. Some reported that the group discussion did not suit their personality style or that they did not form a connection with their group leader.
Discussion
We postulated that facilitated group discussion would decrease job burnout in resident physicians, but our study found no such benefit. Plausible explanations for the ineffectiveness of the intervention could relate to the intervention design, unique challenges of residency training, underpowered enrollment, or novel factors related to the structure of our residency training program.
Our intervention differed in important ways from the model on which it was based.11 The successful model randomized self-selected participants, whereas our participants were randomly selected from a convenience sample (the incoming resident class). Self-selected participants might be more engaged in facilitated discussion and therefore may derive greater benefit from it, suggesting that the success of interventions13 to decrease burnout could be related to an individual's initial desire to participate. Unlike the model, we chose psychotherapist group leaders rather than IM physicians as group facilitators. Our rationale was that resident physicians, who work with and are evaluated by IM faculty, may be less inclined to confide in them. It is possible, however, that some of our participants were not inclined to communicate with therapists.
Other factors may also have limited our success. Despite our effort to liberate time from the residency schedule for the intervention, we were unable to substitute the sessions for other educational requirements. As a result, our intervention added to participants' already full schedules. Prior to the study, power calculations assumed 30 participants each in the test and control groups; however, the actual incoming class size was 9 short of the anticipated number of 60. The finite size of the residency class precluded enrolling additional subjects, regardless of power needs. Finally, although statistically similar, the 2 study arms had differences that could have biased the results.
The failure of the intervention to reduce burnout may be due to fundamental differences in job stress in residents and posttraining physicians. Both groups experience intense work demands and work-life interference; however, resident physicians likely experience a greater lack of autonomy.14,15 The structure of residency minimizes residents' control over work responsibilities.16 Indeed, high measured levels of residents' internal locus of control correlated with better tolerance of intense work demands.17 Facilitated discussion likely alleviates burnout in practicing physicians by reframing their perspective on work-life balance.18 At the same time, it may be ineffective in residents because the lack of autonomy may interfere with their ability to make meaningful change.
Given that lack of autonomy16 may make residents refractory to interventions to mitigate burnout, future studies should evaluate resident-driven interventions. Resident burnout persists and may contribute to severe consequences. We must continue to explore potential interventions to protect both trainees and their patients.
Conclusion
A facilitated discussion intervention modeled after a successful program used to decrease job burnout in practicing physicians was not found to be effective in resident trainees, possibly due to the limitations of the design of the intervention in this population or the unique challenges of residency training compared with posttraining practice, particularly reduced autonomy and control of schedules and workload.
References
- 1. van der Heijden F, Dillingh G, Bakker A, Prins J. Suicidal thoughts among medical residents with burnout. Arch Suicide Res. 2008; 12 4: 344– 346. [DOI] [PubMed] [Google Scholar]
- 2. Dyrbye LN, Thomas MR, Massie FS, Power DV, Eacker A, Harper W, et al. Burnout and suicidal ideation among US medical students. Ann Intern Med. 2008; 149 5: 334– 341. [DOI] [PubMed] [Google Scholar]
- 3. Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002; 136 5: 358– 367. [DOI] [PubMed] [Google Scholar]
- 4. Ripp J, Babyatsky M, Fallar R, Bazari H, Bellini L, Kapadia C, et al. The incidence and predictors of job burnout in first-year internal medicine residents: a five-institution study. Acad Med. 2011; 86 10: 1304– 1310. [DOI] [PubMed] [Google Scholar]
- 5. Ripp J, Fallar R, Babyatsky M, David R, Reich L, Korenstein D. Prevalence of resident burnout at the start of training. Teach Learn Med. 2010; 22 3: 172– 175. [DOI] [PubMed] [Google Scholar]
- 6. Eckleberry-Hunt J, Lick D, Boura J, Hunt R, Balasubramaniam M, Mulhem E, et al. An exploratory study of resident burnout and wellness. Acad Med. 2009; 84 2: 269– 277. [DOI] [PubMed] [Google Scholar]
- 7. Novack DH, Suchman AL, Clark W, Epstein RM, Najberg E, Kaplan C. Calibrating the physician. Personal awareness and effective patient care. Working Group on Promoting Physician Personal Awareness, American Academy on Physician and Patient. JAMA. 1997; 278 6: 502– 509. [DOI] [PubMed] [Google Scholar]
- 8. Lown BA, Manning CF. The Schwartz Center Rounds: evaluation of an interdisciplinary approach to enhancing patient-centered communication, teamwork, and provider support. Acad Med. 2010; 85 6: 1073– 1081. [DOI] [PubMed] [Google Scholar]
- 9. Zeckhausen W. Why are doctors so unhappy? Doctor support groups can be a lifeline. BMJ. 2001; 322 7298: 1364– 1365. [PubMed] [Google Scholar]
- 10. Wallace JE, Lemaire J. On physician well being—you'll get by with a little help from your friends. Soc Sci Med. 2007; 64 12: 2565– 2577. [DOI] [PubMed] [Google Scholar]
- 11. West CP, Dyrbye LN, Rabatin JT, Call TG, Davidson JH, Multari A, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014; 174 4: 527– 533. [DOI] [PubMed] [Google Scholar]
- 12. Maslach C, Jackson SE, Leiter MP, Schaufeli WB, Schwab RL. Maslach Burnout Inventory Manual. 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996. [Google Scholar]
- 13. Krasner MS, Epstein RM, Beckman H, Suchman AL, Chapman B, Mooney CJ, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009; 302 12: 1284– 1293. [DOI] [PubMed] [Google Scholar]
- 14. Thomas NK. Resident burnout. JAMA. 2004; 292 23: 2880– 2889. [DOI] [PubMed] [Google Scholar]
- 15. Linzer M, BaierManwell L, Mundt M, Williams E, Maguire A, McMurray J, et al. Organizational climate, stress, and error in primary care: the MEMO study. : Henriksen K, Battles JB, Marks ES. Advances in Patient Safety: From Research to Implementation (Volume 1: Research Findings). Rockville, MD: Agency for Healthcare Research and Quality; 2005. [PubMed] [Google Scholar]
- 16. Geurts S, Rutte C, Peeters M. Antecedents and consequences of work-home interference among medical residents. Soc Sci Med. 1999; 48 9: 1135– 1148. [DOI] [PubMed] [Google Scholar]
- 17. Saksvik IB, Bjorvatn B, Hetland H, Sandal GM, Pallesen S. Individual differences in tolerance to shift work—a systematic review. Sleep Med Rev. 2011; 15 4: 221– 235. [DOI] [PubMed] [Google Scholar]
- 18. Epstein RM. Mindful practice. JAMA. 1999; 282 9: 833– 839. [DOI] [PubMed] [Google Scholar]


