Abstract
Rotator cuff tears have been reported to be uncommon following total shoulder arthroplasty (TSA). Postoperative rotator cuff tears can lead to pain, proximal humeral migration, and glenoid component loosening. The purpose of this paper was to evaluate the incidence of post-TSA rotator cuff tears or dysfunction in osteoarthritic patients. A systematic review of multiple databases was performed using preferred reporting items for systematic reviews and meta-analyses guidelines. Levels I-IV evidence clinical studies of patients with primary osteoarthritis with a minimum 2-year follow-up were included. Fifteen studies with 1259 patients (1338 shoulders) were selected. Student's t-tests were used with a significant alpha value of 0.05. All patients demonstrated significant improvements in motion and validated clinical outcome scores (P < 0.001). Radiographic humeral head migration was the most commonly reported data point for extrapolation of rotator cuff integrity. After 6.6 ± 3.1 years, 29.9 ± 20.7% of shoulders demonstrated superior humeral head migration and 17.9 ± 14.3% migrated a distance more than 25% of the head. This was associated with an 11.3 ± 7.9% incidence of postoperative superior cuff tears. The incidence of radiographic anterior humeral head migration was 11.9 ± 15.9%, corresponding to a 3.0 ± 13.6% rate of subscapularis tears. We found an overall 1.2 ± 4.5% rate of reoperation for cuff injury. Nearly all studies reported indirect markers of rotator cuff dysfunction, such as radiographic humeral head migration and clinical exam findings. This systematic review suggests that rotator cuff dysfunction following TSA may be more common than previously reported. IV, systematic review of Levels I-IV studies.
Keywords: Glenohumeral, humeral head migration, osteoarthritis, rotator cuff, rupture, total shoulder arthroplasty
INTRODUCTION
The number of total shoulder arthroplasties (TSAs) performed has increased over three-fold from 2000 to 2008.[1] Prolonged life expectancy and increased physical activity in older populations are among many reasons we have seen a greater prevalence of shoulder osteoarthritis (OA). Results following TSA have demonstrated a low complication rate, excellent pain relief, and return of function in a majority of patients.[2,3]
When complications do arise postoperatively, component loosening, nerve injuries, instability, periprosthetic fractures, and rotator cuff tears have been reported.[4,5] Glenoid loosening has typically been the primary concern with regard to TSA longevity, but recent reports have indicated that rotator cuff tears may be more prevalent.[6,7] Bohsali et al. reported a 1.3% incidence of rotator cuff tear following TSA, with a majority of these tears occurring in the subscapularis tendon.[5] Others have reported a 2-4% incidence of rotator cuff tear following the procedure.[4,8] Young et al. reported a much higher 16.8% incidence of rotator cuff dysfunction following TSA, with “dysfunction” defined as >25% superior migration of the humeral component on a true anterior-posterior radiograph of the glenohumeral joint.[6] Post-TSA rotator cuff tearing or dysfunction is associated with proximal migration of the humeral component, which can accelerate polyethylene wear and loosening of the glenoid component through the rocking-horse phenomenon.[9]
The literature on rotator cuff dysfunction after TSA remains limited. Furthermore, most studies do not differentiate patients with OA from those with other forms of arthritis. Posttraumatic and inflammatory arthritis predispose patients to cuff tears, thus confounding any post-TSA cuff complications. We are not aware of any systematic reviews examining the incidence of rotator cuff tears following total shoulder replacement for primary OA. The purpose of this investigation is to determine the incidence of rotator cuff tears after TSA for primary glenohumeral arthritis. We hypothesized that the rate of overall rotator cuff pathology would be significantly higher than the 20-4% rate of rotator cuff tears reported in earlier investigations.
MATERIALS AND METHODS
Search strategy
We conducted a systematic review of the available literature according to preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines using the PRISMA checklist.[10] Searches were completed in February 2013 using the PubMed Medline database and the Cochrane Central Register of Clinical Trials. The keyword selection was designed to capture all Levels I-IV evidence (according to the Oxford Centre for Evidence-Based Medicine) English-language studies that reported clinical and/or radiographic outcomes. This was accomplished using the keywords “shoulder” and “arthroplasty” and a series of “NOT” phrases designed to match our exclusion criteria.* Study exclusion criteria consisted
of cadaveric, biomechanical, histological, and kinematic results as well as any analyses of nonoperative management, hemiarthroplasty, or reverse TSA. Studies were excluded if they did not report any clinical and/or radiographic data relating to rotator cuff pathology. Patient populations were further excluded if their diagnosis was not primary OA; patients with inflammatory arthritis, posttraumatic arthritis, and postcapsulorrhaphy arthritis were excluded. Conversions from hemiarthroplasty to TSA were also excluded. Inclusion criteria consisted of a minimum of 2 years follow-up. This search yielded 178 initial results.
Study selection
Studies with the above-stated exclusion criteria were not immediately excluded but rather reviewed for any differentiation of patient population. For instance, if outcomes from a TSA population were compared to or isolated from those of hemiarthroplasty patients, the clinical outcomes from the TSA population were included in our review. If a study separated outcomes by diagnosis, only those for patients with primary OA were included. If a study could not be deconstructed as such or was entirely devoted to one of our exclusion criteria, that study was excluded from our review. To ensure that no patients were counted twice, each study's authors, data collection period, and ethnic population were reviewed and compared to those of the other studies. If there was any overlap in authorship, period, and place, only the study with the most relevant (i.e., rotator cuff outcomes) or comprehensive data was included. After accounting for all inclusion and exclusion criteria, 15 studies with 1259 patients (1338 shoulders) were selected for inclusion [Figure 1].[2,6,7,11,12,13,14,15,16,17,18,19,20,21,22]
Figure 1.
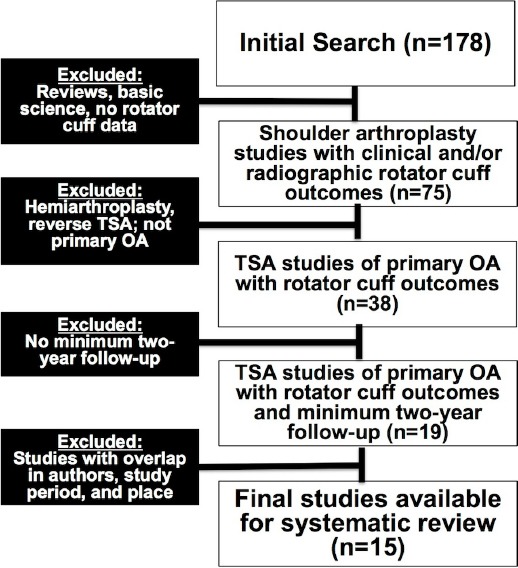
CONSORT diagraph demonstrating study selection criteria
Data extraction
We extracted data from studies that satisfied the eligibility criteria. Details of study design, sample size, and patient demographics, including age, sex, hand dominance, and primary diagnosis were recorded. Surgical factors such as the approach, presence of preoperative rotator cuff tears, biceps treatment, use of cement, and prosthesis design were abstracted. Clinical outcomes included physical examination findings, functional assessment scores (patient satisfaction, Western Ontario OA score, Constant-Murley, Shoulder Outcome score [constant], American Shoulder and Elbow Surgeons [ASES] score, the visual analog score, and Neer patient satisfaction), the number of revisions, changes in range of motion, and subscapularis-specific tests, such as belly press and lift-off. Radiographic outcomes focused on anterior or superior migration of the humeral head, which suggested subscapularis or supraspinatus/infraspinatus pathology, respectively. Those reporting superior migration of the humeral head were classified according to Torchia et al.:[12] superior migration of ≤25% of the prosthetic humeral head diameter is graded as mild subluxation; moderate subluxation involves migration of 25-50% of the diameter; severe subluxation involves proximal migration >50% of the humeral head diameter [Figure 2].
Figure 2.

Computed tomography arthrogram of the right shoulder in a 67-year-old male demonstrating superior migration of the humeral component as well as contrast extravasation in the subacromial space indicative of a full-thickness tear of the superior rotator cuff
Statistical analysis
We reported our data as weighted means with data ranges. A mean was calculated for each study reporting on a respective data point, and each mean was then weighed according to its study sample size. This calculation was performed by multiplying one study's individual mean by the number of patients enrolled in that study and dividing the sum of these weighted data points by the number of eligible patients in all relevant studies. In this way, the nonweighted means from studies with a smaller sample size did not carry as much weight as those from larger studies. Comparisons were made with Student's t-test (SPSS version 18, IBM Inc., Armonk, NY, USA), and an alpha value of 0.05 was set as statistically significant.
RESULTS
A total of 15 studies representing 1259 patients were included in the final dataset.[2,6,7,11,12,13,14,15,16,17,18,19,20,21,22] Demographic characteristics of the included patients are presented in Table 1. Nine of the fifteen studies consist of Level IV Evidence. Only one study reported Level I Evidence.[20]
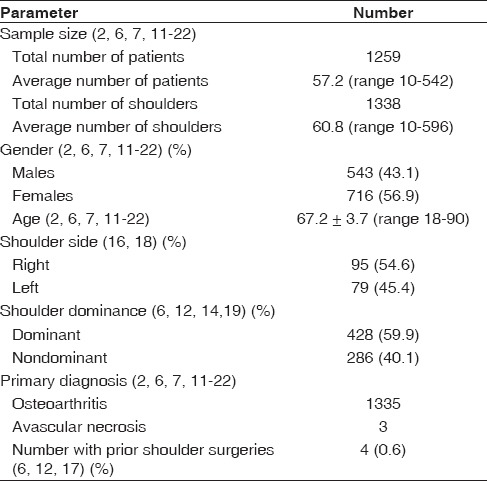
Table 1.
Demographics and clinical diagnoses for the final cohort of included patients
The incidence of preoperative rotator cuff tears, as well as details of the surgical procedure, including the type of components utilized, is presented in Table 2. Seven studies commented on the preoperative condition of the rotator cuff and whether or not a concomitant repair was performed. Of these seven studies, 59 shoulders (6.4%) had a complete supraspinatus tear, 39 of which (4.0%) underwent a supraspinatus repair at the time of arthroplasty. The technique of repair was not specified in any study.
Table 2.
Operative findings, techniques, and implants for the final cohort of included patients
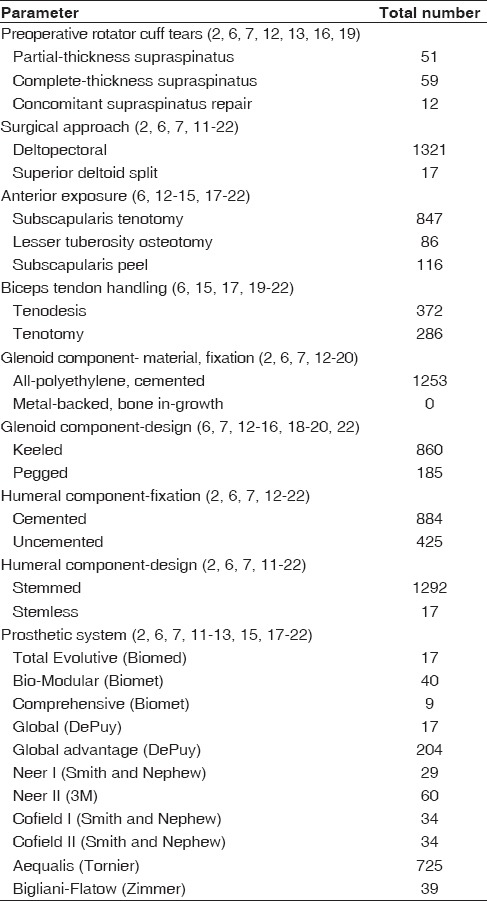
Table 3 reports the clinical and radiographic outcomes from the included studies. The average length of follow-up to the final physical exam was 6.8 ± 3.2 years. Eleven studies documented changes in forward elevation and external rotation pre- and post-operatively, all of which demonstrated statistically significant improvements at final follow-up (P < 0.001). The belly-press test was found to be abnormal in 20% of patients postoperatively. Each clinical outcome score was utilized in no more than five studies. When reported, clinical outcome scores improved significantly, after more than 6 years of follow-up (P < 0.001).
Table 3.
Pre- and post-operative clinical outcome data and postoperative radiological outcomes for all patients included in the final analysis
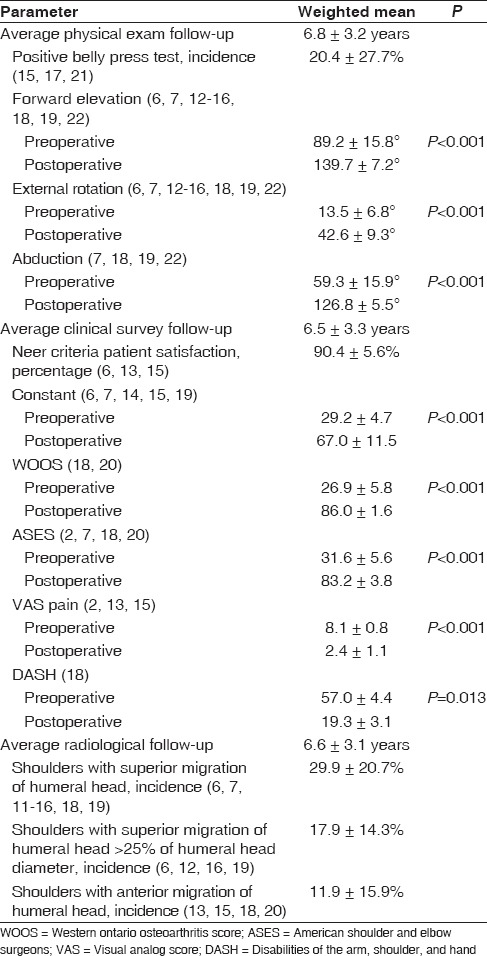
Radiographic data were reported in a majority of investigations [Table 3]. Ten studies reported on the proximal migration of the humeral head prosthesis. In these ten studies, the percentage of shoulders with superior migration was nearly 30% after 6.6 ± 3.1 years. Among the four studies using the Torchia et al. classification scheme,[12]18% of shoulders demonstrated moderate or severe migration. These ten studies were further subdivided into those reporting an average of greater than or <15% of shoulders with superior migration. When comparing these two groups of studies, there was no significant difference in preoperative constant scores (P = 0.74), but there was a significant difference in postoperative scores, with lower scores in those studies reporting more than 15% of patients with superior migration (P = 0.049). Anterior humeral head migration was not specifically defined in any of the four studies in which it was reported. As such, the percentage of shoulders with anterior migration ranged widely from 0% to 36% for a mean of 12%.
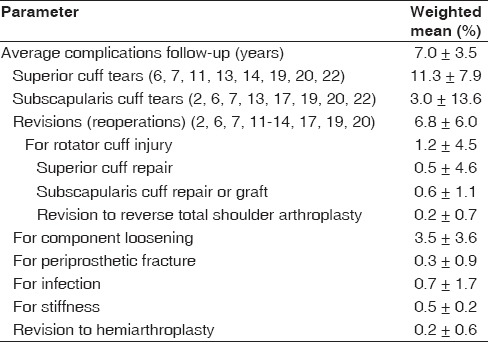
Complications data were reported after a weighted mean of 7.0 ± 3.5 years of follow-up [Table 4]. Overall revision rate for any reason was 6.8 ± 6.0%, while the independent reoperation rate for rotator cuff injury was 1.2 ± 4.5%. Among the eight studies with documented rotator cuff tears, the weighted mean of superior cuff tears (supraspinatus or infraspinatus) was 11.3 ± 7.9%, and that of subscapularis tears was 3.0 ± 13.6%.
Table 4.
Incidence of postoperative rotator cuff tears and reoperations
DISCUSSION
The goal of this systematic review was to report the incidence of rotator cuff tears following TSA for primary OA. Nearly all of the 15 analyzed studies (over 1,300 shoulders) reported indirect markers of rotator cuff dysfunction, such as radiographic humeral head migration and/or positive exam findings. Only one study utilized nonroentographic imaging (ultrasonography).[17] We found that nearly 30% of shoulders demonstrated radiographic superior migration and 12% showed anterior migration of the humeral head at a final mean follow-up of 6.6 ± 3.1 years.
Weiner and Macnab first described the superior migration of the humeral head in native shoulders.[23] They found that 50% of patients with rotator cuff tears had proximal humeral migration, and subsequent clinical and cadaveric studies confirmed this finding.[24,25,26] Deutsch et al. later described the mechanism by which this migration occurs.[27] The rotator cuff functions as a dynamic stabilizer of the glenohumeral joint and counteracts the upward pull of the deltoid muscle by depressing the humeral head during abduction. When the rotator cuff is torn or deficient, the deltoid is unopposed, leading to chronic superior subluxation of the humeral head. In a native shoulder, this can progress to impingement syndrome or cuff tear arthropathy. In a prosthetic shoulder, proximal migration may accelerate arthroplasty failure through one of the two mechanisms. Greater humeral head translation diminishes the relative contact area of the glenohumeral joint and thus transmits higher contact stress to the glenoid component, leading to polyethylene deformation and wear.[28,29,30] In addition, humeral head migration can lead to eccentric loading and glenoid component loosening via a “rocking-horse phenomenon.”[9,29,30,31,32,33] Anterior migration theoretically could engender the same mechanisms of polyethylene wear and eccentric loading. Just as superior humeral head migration is associated with supraspinatus and infraspinatus tears, anterior subluxation may indicate a tear of the subscapularis tendon.[5] Inadequate subscapularis repair, humeral component malrotation, the use of oversized components, anterior glenoid and/or capsular deficiency, and deltoid dysfunction all have been associated with anterior instability after TSA.[8,34,35]
The clinical consequences of superior or anterior humeral migration remain controversial. The rocking-horse phenomenon of glenoid component loosening has been clearly described in patients with severe preoperative rotator cuff tears,[9] but it has not been proven in patients without preexisting tears. Young et al. found that superior migration was significantly associated with glenoid radiolucencies,[6] and Miller et al. reported lower ASES and patient satisfaction scores in patients with subscapularis tears.[36] However, the former also showed no difference in glenoid revisions between patients with and without superior migration. Moreover, Wirth et al. found no association between rotator cuff tears and activity-altering pain,[8] and Khan et al. showed that rotator cuff pathology did not adversely impact mean shoulder survey scores.[7]
Of the studies that reported postoperative rotator cuff tears, there was an 11% rate of superior cuff tears and 3% rate of subscapularis tears, confirming this investigation's hypothesis. Unfortunately, only a few authors specified their method of diagnosis.[6,7,14,17] Khan et al. clinically diagnosed rotator cuff failure if the patient was pseudoparalytic or had a positive Jobe test, elevation of the humeral head on resisted cuff action, and serial radiographs with increasing proximal migration of at least 5 mm.[7] Scalise et al. defined an abnormal subscapularis tendon through ultrasonography.[17] An attenuated tendon had a focal decrease of ≥50% of the normal tendon thickness, and a full-thickness tear was defined as a gap in the tendon substance with retraction. The lack of objective data and the nature of aggregate data in a systematic review precluded direct correlation of the presence of rotator cuff tears with clinical outcomes. However, while nearly 7% of patients underwent reoperation, only 1.2% of patients did so for a rotator cuff injury.
Proximal migration of the humeral head was the most consistently reported data point that was used as an approximation of rotator cuff dysfunction. Ten studies (1,012 shoulders) commented on proximal migration. Four of these studies employed the proximal migration grading system of Torchia et al.[12] One study defined proximal migration as an acromiohumeral distance ≤7 mm,[14] and another study defined it as >5 mm of migration over the follow-up period.[7] The other four studies did not define their parameters for superior migration of the humeral head. Only three studies in this review were dedicated specifically to post-TSA rotator cuff function, and all three used radiographic humeral head migration as their primary outcomes instrument.[6,11,12] This review's reported rate of 17.9% moderate or severe superior subluxation after 6.6 years was similar to the 16.8% rate Young et al. reported after 8.6 years.
Limitations of this systematic review are imposed by the studies analyzed. There was a relative paucity of clinical and radiographic data relating to rotator cuff pathology. Magnetic resonance imaging serves as the current gold standard for diagnosis of rotator cuff tears, but its use postoperatively is limited by metal artifact. Therefore, most outcomes studies rely on indirect measures of rotator cuff quality. Proximal humeral migration may not be a reliable indicator of rotator cuff pathology, as Boyd et al. showed that the incidence of cuff tears did not differ significantly between groups with and without proximal migration.[11] In addition, the belly press test has demonstrated low sensitivity, low specificity, and low positive predictive value for diagnosis of subscapularis tears after TSA so may be an unreliable indicator of subscapularis dysfunction.[37] Finally, because only a handful of studies described their actual clinical method of diagnosing rotator cuff tears, we accepted radiographic measurements of humeral head migration as a proxy of rotator cuff dysfunction. Selection bias was minimized in this review due to the inclusive nature of studies with Levels of evidence I-IV, but this created a study design bias in that most studies consisted of Level IV evidence and only one study cited Level I evidence.
Rotator cuff dysfunction following TSA may be more common than previously reported. It remains unknown, however, whether rotator cuff dysfunction, as defined by clinical or radiographic examination of humeral head migration, leads to inferior outcomes. We hope that this review encourages researchers to design clinical and basic science studies that assess the impact of shoulder arthroplasty on the rotator cuff.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
(((((((((((((((((((((((((((((((((((((((((((((((((((total[Title/Abstract]) AND shoulder[Title/Abstract]) AND arthroplasty[Title/Abstract] AND (English[lang]))) NOT reverse[Title/Abstract]) NOT hemiarthroplasty[Title/Abstract]) NOT fixation[Title/Abstract]) NOT nonoperative[Title/Abstract]) NOT nonsurgical[Title/Abstract] AND (English[lang]))) NOT revision[Title/Abstract]) NOT elbow[Title/Abstract]) NOT wrist[Title/Abstract]) NOT hip[Title/Abstract]) NOT knee[Title/Abstract]) NOT ankle[Title/Abstract] AND (English[lang]))) NOT biomechanical[Title/Abstract]) NOT cadaveric[Title/Abstract]) NOT laboratory[Title/Abstract] AND (English[lang]))) NOT resurfacing[Title/Abstract]) NOT surface[Title/Abstract]) NOT interphalangeal[Title/Abstract] AND (English[lang]))) NOT anesthesia[Title/Abstract]) NOT anesthesia[Title/Abstract]) NOT finite[Title/Abstract] AND (English[lang]))) NOT interscalene[Title/Abstract]) NOT radiostereometric[Title/Abstract] AND (English[lang]))) NOT cmc[Title/Abstract]) NOT carpometacarpal[Title/Abstract]) NOT cervical[Title/Abstract]) NOT anesthesiology[Title/Abstract] AND (English[lang]))) NOT rehabilitation[Title/Abstract] AND (English[lang]))) NOT histology[Title/Abstract]) NOT histological[Title/Abstract]) NOT collagen[Title/Abstract] AND (English[lang]))) NOT kinematic[Title/Abstract]) NOT kinematics[Title/Abstract] AND (English[lang]))) NOT vitro[Title/Abstract] AND (English[lang]))) NOT inverted[Title/Abstract]) NOT grammont[Title/Abstract]) NOT arthrodesis[Title/Abstract]) NOT fusion[Title/Abstract] AND (English[lang])
REFERENCES
- 1.Kim SH, Wise BL, Zhang Y, Szabo RM. Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am. 2011;93:2249–54. doi: 10.2106/JBJS.J.01994. [DOI] [PubMed] [Google Scholar]
- 2.Norris TR, Iannotti JP. Functional outcome after shoulder arthroplasty for primary osteoarthritis: A multicenter study. J Shoulder Elbow Surg. 2002;11:130–5. doi: 10.1067/mse.2002.121146. [DOI] [PubMed] [Google Scholar]
- 3.Godenèche A, Boileau P, Favard L, Le Huec JC, Lévigne C, Nové-Josserand L, et al. Prosthetic replacement in the treatment of osteoarthritis of the shoulder: Early results of 268 cases. J Shoulder Elbow Surg. 2002;11:11–8. doi: 10.1067/mse.2002.120140. [DOI] [PubMed] [Google Scholar]
- 4.Chin PY, Sperling JW, Cofield RH, Schleck C. Complications of total shoulder arthroplasty: Are they fewer or different? J Shoulder Elbow Surg. 2006;15:19–22. doi: 10.1016/j.jse.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 5.Bohsali KI, Wirth MA, Rockwood CA., Jr Complications of total shoulder arthroplasty. J Bone Joint Surg Am. 2006;88:2279–92. doi: 10.2106/JBJS.F.00125. [DOI] [PubMed] [Google Scholar]
- 6.Young AA, Walch G, Pape G, Gohlke F, Favard L. Secondary rotator cuff dysfunction following total shoulder arthroplasty for primary glenohumeral osteoarthritis: Results of a multicenter study with more than five years of follow-up. J Bone Joint Surg Am. 2012;94:685–93. doi: 10.2106/JBJS.J.00727. [DOI] [PubMed] [Google Scholar]
- 7.Khan A, Bunker TD, Kitson JB. Clinical and radiological follow-up of the Aequalis third-generation cemented total shoulder replacement: A minimum ten-year study. J Bone Joint Surg Br. 2009;91:1594–600. doi: 10.1302/0301-620X.91B12.22139. [DOI] [PubMed] [Google Scholar]
- 8.Wirth MA, Rockwood CA., Jr Complications of total shoulder-replacement arthroplasty. J Bone Joint Surg Am. 1996;78:603–16. doi: 10.2106/00004623-199604000-00018. [DOI] [PubMed] [Google Scholar]
- 9.Franklin JL, Barrett WP, Jackins SE, Matsen FA., 3rd Glenoid loosening in total shoulder arthroplasty. Association with rotator cuff deficiency. J Arthroplasty. 1988;3:39–46. doi: 10.1016/s0883-5403(88)80051-2. [DOI] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J Clin Epidemiol. 2009;62:1006–12. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 11.Boyd AD, Jr, Aliabadi P, Thornhill TS. Postoperative proximal migration in total shoulder arthroplasty. Incidence and significance. J Arthroplasty. 1991;6:31–7. doi: 10.1016/s0883-5403(06)80154-3. [DOI] [PubMed] [Google Scholar]
- 12.Torchia ME, Cofield RH, Settergren CR. Total shoulder arthroplasty with the Neer prosthesis: Long-term results. J Shoulder Elbow Surg. 1997;6:495–505. doi: 10.1016/s1058-2746(97)90081-1. [DOI] [PubMed] [Google Scholar]
- 13.Mileti J, Sperling JW, Cofield RH, Harrington JR, Hoskin TL. Monoblock and modular total shoulder arthroplasty for osteoarthritis. J Bone Joint Surg Br. 2005;87:496–500. doi: 10.1302/0301-620X.87B4.15558. [DOI] [PubMed] [Google Scholar]
- 14.Merolla G, Paladini P, Campi F, Porcellini G. Efficacy of anatomical prostheses in primary glenohumeral osteoarthritis. Chir Organi Mov. 2008;91:109–15. doi: 10.1007/s12306-007-0019-y. [DOI] [PubMed] [Google Scholar]
- 15.Lafosse L, Schnaser E, Haag M, Gobezie R. Primary total shoulder arthroplasty performed entirely thru the rotator interval: Technique and minimum two-year outcomes. J Shoulder Elbow Surg. 2009;18:864–73. doi: 10.1016/j.jse.2009.03.017. [DOI] [PubMed] [Google Scholar]
- 16.Throckmorton TW, Zarkadas PC, Sperling JW, Cofield RH. Pegged versus keeled glenoid components in total shoulder arthroplasty. J Shoulder Elbow Surg. 2010;19:726–33. doi: 10.1016/j.jse.2009.10.018. [DOI] [PubMed] [Google Scholar]
- 17.Scalise JJ, Ciccone J, Iannotti JP. Clinical, radiographic, and ultrasonographic comparison of subscapularis tenotomy and lesser tuberosity osteotomy for total shoulder arthroplasty. J Bone Joint Surg Am. 2010;92:1627–34. doi: 10.2106/JBJS.G.01461. [DOI] [PubMed] [Google Scholar]
- 18.Razmjou H, Holtby R, Christakis M, Axelrod T, Richards R. Impact of prosthetic design on clinical and radiologic outcomes of total shoulder arthroplasty: A prospective study. J Shoulder Elbow Surg. 2013;22:206–14. doi: 10.1016/j.jse.2012.04.016. [DOI] [PubMed] [Google Scholar]
- 19.Raiss P, Schmitt M, Bruckner T, Kasten P, Pape G, Loew M, et al. Results of cemented total shoulder replacement with a minimum follow-up of ten years. J Bone Joint Surg Am. 2012;94:e1711–10. doi: 10.2106/JBJS.K.00580. [DOI] [PubMed] [Google Scholar]
- 20.Lapner PL, Sabri E, Rakhra K, Bell K, Athwal GS. Comparison of lesser tuberosity osteotomy to subscapularis peel in shoulder arthroplasty: A randomized controlled trial. J Bone Joint Surg Am. 2012;94:2239–46. doi: 10.2106/JBJS.K.01365. [DOI] [PubMed] [Google Scholar]
- 21.Jandhyala S, Unnithan A, Hughes S, Hong T. Subscapularis tenotomy versus lesser tuberosity osteotomy during total shoulder replacement: A comparison of patient outcomes. J Shoulder Elbow Surg. 2011;20:1102–7. doi: 10.1016/j.jse.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 22.Jost PW, Dines JS, Griffith MH, Angel M, Altchek DW, Dines DM. Total shoulder arthroplasty utilizing mini-stem humeral components: Technique and short-term results. HSS J. 2011;7:213–7. doi: 10.1007/s11420-011-9221-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weiner DS, Macnab I. Superior migration of the humeral head. A radiological aid in the diagnosis of tears of the rotator cuff. J Bone Joint Surg Br. 1970;52:524–7. [PubMed] [Google Scholar]
- 24.Poppen NK, Walker PS. Normal and abnormal motion of the shoulder. J Bone Joint Surg Am. 1976;58:195–201. [PubMed] [Google Scholar]
- 25.Poppen NK, Walker PS. Forces at the glenohumeral joint in abduction. Clin Orthop Relat Res. 1978;135:165–70. [PubMed] [Google Scholar]
- 26.Blasier RB, Guldberg RE, Rothman ED. Anterior shoulder stability: Contributions of rotator cuff forces and the capsular ligaments in a cadaver model. J Shoulder Elbow Surg. 1992;1:140–50. doi: 10.1016/1058-2746(92)90091-G. [DOI] [PubMed] [Google Scholar]
- 27.Deutsch A, Altchek DW, Schwartz E, Otis JC, Warren RF. Radiologic measurement of superior displacement of the humeral head in the impingement syndrome. J Shoulder Elbow Surg. 1996;5:186–93. doi: 10.1016/s1058-2746(05)80004-7. [DOI] [PubMed] [Google Scholar]
- 28.Flatow EL. Prosthetic design considerations in total shoulder arthroplasty. Semin Arthroplasty. 1995;6:233–44. [PubMed] [Google Scholar]
- 29.Wang VM, Krishnan R, Ugwonali OF, Flatow EL, Bigliani LU, Ateshian GA. Biomechanical evaluation of a novel glenoid design in total shoulder arthroplasty. J Shoulder Elbow Surg. 2005;14(1 Suppl S):129S–40. doi: 10.1016/j.jse.2004.09.029. [DOI] [PubMed] [Google Scholar]
- 30.Karduna AR, Williams GR, Williams JL, Iannotti JP. Glenohumeral joint translations before and after total shoulder arthroplasty. A study in cadavera. J Bone Joint Surg Am. 1997;79:1166–74. doi: 10.2106/00004623-199708000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Karduna AR, Williams GR, Williams JL, Iannotti JP. Kinematics of the glenohumeral joint: Influences of muscle forces, ligamentous constraints, and articular geometry. J Orthop Res. 1996;14:986–93. doi: 10.1002/jor.1100140620. [DOI] [PubMed] [Google Scholar]
- 32.Karduna AR, Williams GR, Iannotti JP, Williams JL. Total shoulder arthroplasty biomechanics: A study of the forces and strains at the glenoid component. J Biomech Eng. 1998;120:92–9. doi: 10.1115/1.2834312. [DOI] [PubMed] [Google Scholar]
- 33.Matsen FA, 3rd, Clinton J, Lynch J, Bertelsen A, Richardson ML. Glenoid component failure in total shoulder arthroplasty. J Bone Joint Surg Am. 2008;90:885–96. doi: 10.2106/JBJS.G.01263. [DOI] [PubMed] [Google Scholar]
- 34.Brems JJ. Complications of shoulder arthroplasty: Infections, instability, and loosening. Instr Course Lect. 2002;51:29–39. [PubMed] [Google Scholar]
- 35.Warren RF, Coleman SH, Dines JS. Instability after arthroplasty: The shoulder. J Arthroplasty. 2002;17((4 Suppl) 1):28–31. doi: 10.1054/arth.2002.32543. [DOI] [PubMed] [Google Scholar]
- 36.Miller BS, Joseph TA, Noonan TJ, Horan MP, Hawkins RJ. Rupture of the subscapularis tendon after shoulder arthroplasty: Diagnosis, treatment, and outcome. J Shoulder Elbow Surg. 2005;14:492–6. doi: 10.1016/j.jse.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 37.Armstrong A, Lashgari C, Teefey S, Menendez J, Yamaguchi K, Galatz LM. Ultrasound evaluation and clinical correlation of subscapularis repair after total shoulder arthroplasty. J Shoulder Elbow Surg. 2006;15:541–8. doi: 10.1016/j.jse.2005.09.013. [DOI] [PubMed] [Google Scholar]


