Abstract
Primary bone tumors around the elbow represent <1% of all the skeletal tumors. Surgery with or without adjuvant therapy (radiotherapy, chemotherapy) is the treatment of choice for malignant tumors. Reconstruction of the elbow and forearm in malignant tumors is challenging as it involves a complex interplay between multiple joints which need to be stabilized for the optimal functional outcome. We describe a new technique for the reconstruction of the elbow after resection of a proximal ulna tumor with articular radio-ulnar synostosis with the creation of a single bone forearm. We attempted to achieve a mobile elbow and stable wrist joint with the radio-ulnar union at the proximal articular surface of the ulna resulting in a single bone forearm. The procedure involves an oblique osteotomy preserving the olecranon process (after taking adequate margins based on oncological principles) and its articular cartilage along with the attachment of the triceps tendon. Then the radial head was partially denuded of its cartilage using a burr, leaving cartilage only on the volar side, and then fused to the remnant olecranon. Osteosynthesis was done using compression screw and tension band wiring. The advantages of this procedure are that the mobility at wrist and elbow are retained, it requires minimal hardware and allows for primary closure of the wound.
Keywords: Biological reconstruction, elbow joint, Ewing sarcoma, osteosynthesis, single bone forearm, synostosis
INTRODUCTION
Primary bone tumors around the elbow represent <1% of all the skeletal tumors.[1] Among these, Ewings sarcoma is the most common primary bone tumor in children. Ewings sarcoma is treated with multimodality management where surgery forms the cornerstone of treatment sandwiched between neoadjuvant and adjuvant chemotherapy. Radiotherapy may be used as an adjuvant in cases with large disease volume, poor response to chemotherapy, close or involved surgical margins and as a definitive option where function-preserving surgery is not feasible. Surgery with or without radiotherapy has been successful in achieving higher local control as compared to definitive radiotherapy, which translates to better survival as well.[2] The treatment of tumors of the proximal ulna poses a unique challenge as reconstruction is difficult with limited options described in the literature. The primary aim in this case, is to have a mobile and stable elbow joint to provide optimal wrist and hand functions. We describe a new technique for the reconstruction of the elbow after resection of a proximal ulna tumor with articular radio-ulnar synostosis thereby creating a single bone forearm.
CASE REPORT
An 11-year-old boy presented with complaints of pain and swelling over the right forearm since 4 months. Examination revealed a 10 cm × 5 cm bony hard mass arising from the diaphysis of the ulna. Elbow and wrist range of movements were normal, pronation and supination were restricted due to pain, no distal neurovascular deficiency was noted. The plain radiograph of the forearm in two perpendicular planes revealed a permeative destructive lesion with a wide zone of transition involving the middle and lower third ulna with periosteal reaction and cortical breach [Figure 1a]. Magnetic resonance imaging (MRI) revealed the involvement of almost the entire ulna except for the proximal part sparing the olecranon and articular surface (T1-weighted images). It was associated with a large soft tissue component with the displacement of ulnar vessels (T2-weighted images) [Figure 1b and c].
Figure 1.
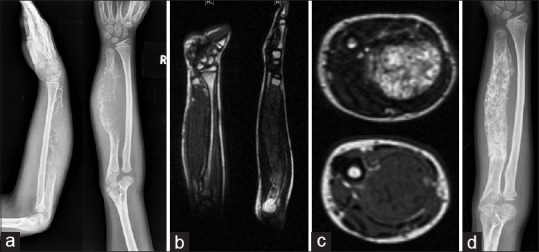
(a) Plain radiograph of forearm showing aggressive lesion of ulna with cortical destruction and soft tissue component. (b and c) Magnetic resonance imaging showing craniocaudal extent of the disease in ulna and the relation of the tumor with the neurovascular bundle. (d) Plain radiograph of forearm after neoadjuvant chemotherapy showing a good response
The clinico-radiological diagnosis of Ewings sarcoma was confirmed histopathologically with core needle biopsy. The patient was staged with computed tomography of the chest, a bone scan and multiple-site bone marrow aspiration, which did not reveal metastasis. The patient was evaluated in a multidisciplinary clinic and was started on multi-agent chemotherapy. He was reassessed after induction chemotherapy with plain radiography and an MRI of the forearm for planning local treatment [Figure 1d]. The MRI revealed a substantial decrease in the soft tissue component of the disease. Local treatment options (limb salvage surgery with complex reconstruction vs definitive radiotherapy) were discussed with the patient and attendants, who opted for surgical treatment.
Technique
A limb salvage surgical procedure was planned with wide excision of the ulna except the proximal 2 cm, which includes partial articular surface as this was uninvolved by the disease. This ensured a narrow 1 cm tumor-free margin proximally. Reconstruction was planned with medialization of the radius with its proximal articular surface to this retained fragment creating a one-bone forearm. Detailed preoperative surgical planning was done with appropriate drawings [Figure 2].
Figure 2.
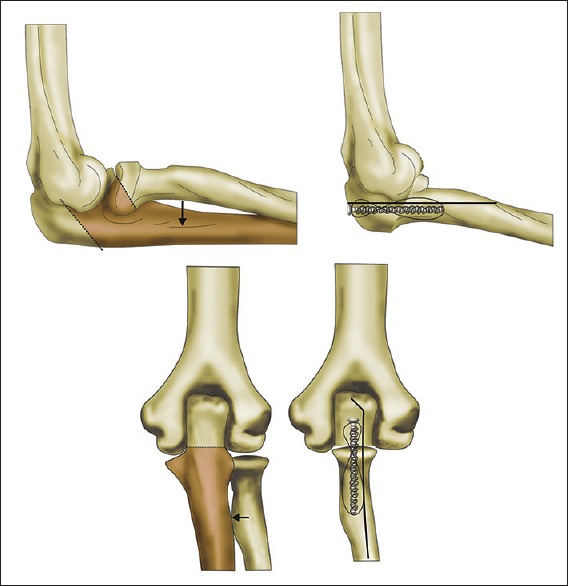
Illustration of oblique osteotomy at the base of coronoid process, medialization of radius after denuding articular cartilage and stabilization with remnant of olecranon using tension band wire technique
The patient was operated in the supine position with a tourniquet. A dorsolateral incision was taken. The needle biopsy scar and the tract were excised along with the tumor. The ulnar neurovascular bundle was identified and protected. The planned site of osteotomy was identified at the base of the coronoid process. An oblique osteotomy was done at this level to preserve the olecranon process and its articular cartilage along with the attachment of the triceps tendon [Figure 3a–c]. The osteotomy was done obliquely through the elbow joint at the level of the radial head. Distally, the ulna was dislocated and gradually released from the interosseous membrane, leaving a layer of uninvolved muscle on the ulna, as the oncological margin. Proximal radius was released from the tendinous attachments and mobilised medially. The radial head was partially denuded of its cartilage using a burr, leaving cartilage only on the volar side. Osteosynthesis was done between the radius and the ulna with the help of 3.5 mm cortical screw, directed from the olecranon into the radius. Tension band wiring was done to further secure the fixation [Figure 3d]. The forearm was fixed in a neutral position. The elbow was immobilized in the above elbow slab for 4 weeks [Figure 4a]. Postoperative period was uneventful. Elbow range of motion was initiated after 4 weeks. The final histopathology report confirmed Ewing sarcoma of the ulna with free margins and 95% tumor necrosis. Adjuvant radiotherapy was given in view of the large disease volume at presentation. The patient also completed adjuvant chemotherapy as per hospital protocol.
Figure 3.
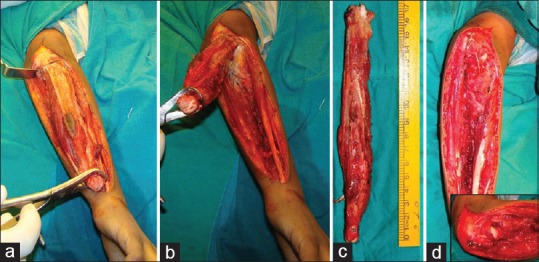
Intra-operative picturing showing (a and b) mobilization of the distal ulna and oblique olecranon osteotomy at the base of the coronoid process. (c) Excised specimen. (d) Fixation of the radius to the remaining olecrenon with compression screw and tension band wiring
Figure 4.

(a) Postoperative radiographs. (b) Plain radiograph at 5 years follow-up showing union at the osteotomy site and consolidation
Twelve months after the index surgery, the patient sustained a traumatic fracture of the shaft the radius, which was treated with closed reduction and fixation with a Kirschner wire. The patient underwent implant removal after 3 years of surgery, in view of prominence of the implant over the elbow. The patient was last reviewed at 5 years post index surgery with plain radiography [Figure 4b]. The patient is disease-free. He has 5 cm shortening of his forearm, 10° of fixed flexion deformity at the elbow, with a further range of movement up to 130° [Figure 5]. The patient is able to do most of the activities of daily living with the operated limb. He functionally fares well with a Musculoskeletal Tumor Society Score of 27 out of 30.
Figure 5.
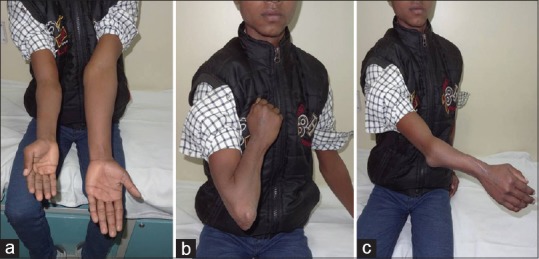
(a) Clinical picture showing shortening in the operated forearm. (b and c) Good elbow range of movement (10–130°) at 5 years follow-up
DISCUSSION
Reconstruction of the elbow and forearm in malignant tumors is challenging, as it involves a complex interplay between the multiple joints, which need to be stabilised for optimal functional outcomes. Postoperative radiation, young age, limited soft tissue in forearm and proximity to neurovascular structures add to the problems in achieving a good hand and elbow function.
Various reconstruction options after proximal and shaft ulna resections mentioned in the literature include arthrodesis, use of autografts or allografts and endoprosthetic replacements.[3,4,5] En bloc resection of the proximal ulna and fibular reconstruction with joint fusion is a simple and very effective method without the involvement of too much metal or prosthesis. However, this technique of resection and reconstruction are more suitable for cases with complete involvement of proximal ulna with articular surface. Total elbow arthroplasty is more suitable for small resection lengths. Its usage in patients with large defects may, however, result in poor function and instability.[5] In addition, these nonbiological methods of reconstruction have higher rates of long-term complications such as implant loosening and failure. The rate of postoperative infection is also higher with nonbiological methods of reconstruction where the large metallic prosthesis is used.
The aim of the procedure was to provide a durable and stable reconstruction after complete tumor excision. Preservation of the proximal portion of the ulna with triceps attachment provides the necessary stability required for the elbow joint. This may be difficult to achieve if the total ulna is excised. Authors have published methods to reconstruct the proximal ulna with fibular transfer or with allograft ulna, but these procedures have their inherent problems.[6] It is extremely difficult to find a size matched proximal ulnar allograft in a country like ours, where organ donation program is not very popular. Another method of reconstruction may include the use of sterilised tumor bone and its reimplantation. Alhough very popular with intercalary resections and reconstructions, this procedure is not very suitable for osteoarticluar resections as the high dosage of radiation leads to cartilage damage and subsequent osteoarthritis of the joint.[7]
We attempted to achieve a mobile elbow with the proximal radio-ulnar union at the articular surface resulting in a single bone forearm. A single bone forearm with a stable hand was our goal for good function. The advantages of this procedure are that the mobility at the wrist and elbow are retained, it requires minimal hardware thus reducing the incidence of infection and obviates complex microvascular surgeries (required if vascularized grafts are used). Creation of a one-bone forearm also reduces the residual forearm volume allowing for good soft tissue coverage with reduced wound morbidity. Disadvantages of this procedure include loss of prono-supination and inferior cosmoses.
CONCLUSION
Articular radioulnar synostosis and a single bone forearm retaining the articular cartilage of the proximal ulna provides a good elbow, wrist and hand function. It is an alternative procedures that can be used in the ulna tumors where we can preserve the olecranon.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Sewell MD, Hanna SA, Pollock RC, Aston WJ, Skinner JA, Blunn GW, et al. Proximal ulna endoprosthetic replacement for bone tumours in young patients. Int Orthop. 2012;36:1039–44. doi: 10.1007/s00264-012-1483-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daecke W, Ahrens S, Juergens H, Martini AK, Ewerbeck V, Kotz R, et al. Ewing's sarcoma and primitive neuroectodermal tumor of hand and forearm. Experience of the Cooperative Ewing's Sarcoma Study Group. J Cancer Res Clin Oncol. 2005;131:219–25. doi: 10.1007/s00432-004-0637-9. [DOI] [PubMed] [Google Scholar]
- 3.Kimura K, Tatezaki S, Ishii T, Yonemoto T, Shigehara T, Takenouchi T. Hemiarthroplasty of the elbow with a vascularized fibular graft after excision of Ewing's sarcoma of the proximal ulna: A case report. Jpn J Clin Oncol. 2002;32:430–4. doi: 10.1093/jjco/hyf088. [DOI] [PubMed] [Google Scholar]
- 4.Urbaniak JR, Black KE., Jr Cadaveric elbow allografts. A six-year experience. Clin Orthop Relat Res. 1985;197:131–40. [PubMed] [Google Scholar]
- 5.Sperling JW, Pritchard DJ, Morrey BF. Total elbow arthroplasty after resection of tumors at the elbow. Clin Orthop Relat Res. 1999;367:256–61. [PubMed] [Google Scholar]
- 6.Aberg M, Rydholm A, Holmberg J, Wieslander JB. Reconstruction with a free vascularized fibular graft for malignant bone tumor. Acta Orthop Scand. 1988;59:430–7. doi: 10.3109/17453678809149397. [DOI] [PubMed] [Google Scholar]
- 7.Puri A, Gulia A, Jambhekar N, Laskar S. The outcome of the treatment of diaphyseal primary bone sarcoma by resection, irradiation and re-implantation of the host bone: Extracorporeal irradiation as an option for reconstruction in diaphyseal bone sarcomas. J Bone Joint Surg Br. 2012;94:982–8. doi: 10.1302/0301-620X.94B7.28916. [DOI] [PubMed] [Google Scholar]


