Abstract
Aim:
A previous study has shown that physcion 8-O-β-glucopyranoside (PG) derived from Rumex japonicusHoutt causes apoptosis and blocks cell cycle progression in human lung cancer cells. In the present study we investigated the molecular mechanisms underlying PG-induced cancer cell apoptosis.
Methods:
Human OSCC-derived cell line KB was treated PG (10, 20, 50 μg/mL). Cell apoptosis was detected with flow cytometry. Mitochondrial membrane potential (MMP) and release of cytochome C from mitochondria were measured; the expression of relevant signaling proteins was analyzed using Western blotting or qRT-PCR. For evaluation of in vivo anticancer action, nude mice grafted with KB cells were treated with PG (10, 20, 40 mg·kg−1·d−1, ip) for 24 days.
Results:
PG dose-dependently suppressed cell proliferation and induced apoptosis in KB cells. PG-induced apoptosis was mediated via the intrinsic mitochondrial pathway, as evidenced by the decreased Bcl-2, increased Bax and Bax/Bcl-2 ratio, as well as the loss of MMP, caspase-9 activation, and increased cytosolic cytochrome c. Furthermore, PG suppressed the expression of survivin, whereas overexpression of survivin markedly attenuated PG-induced apoptosis. Meanwhile PG increased the expression of tumor suppressor PTEN, and decreased p-Akt, p-GSK3β and miR-21 levels. Pharmacological activation of Akt/GSK3β signaling or transfection with miR-21 mimic abolished PG-induced survivin reduction and cell apoptosis. Similar results were observed in PG-treated nude mice grafted with KB cells.
Conclusion:
Physcion 8-O-β-glucopyranoside induces mitochondria-dependent apoptosis of human OSCC cells by suppressing survivin expression via miR-21/PTEN/Akt/GSK3β signaling pathway.
Keywords: physcion 8-O-β-glucopyranoside, human oral squamous cell carcinoma, mitochondria-dependent apoptosis, survivin, miR-21, PTEN, Akt/GSK3β
Introduction
Oral squamous cell carcinoma (OSCC), a common type of malignant tumor, accounts for approximately >90% of diagnosed patients with oral cancer1,2. Currently, the principal methods for the treatment of OSCC are radiotherapy and surgery, but recurrences are common with further resistance to therapy, leading to a poor prognosis with a 5-year survival rate less than 50%3. Therefore, the discovery and development of effective chemotherapeutic agents for OSCC might result in an improvement in the survival rate of OSCC patients.
Survivin, a 142-residue protein belonging to the inhibitor of apoptosis proteins (IAP) family, is overexpressed in a variety of human malignancies but not normal adult tissues4. Mechanically, survivin inhibits apoptosis by interfering with the activation of caspase-3 and caspase-75. It has also been suggested that survivin overexpression might provide a favorable environment for the accumulation of mutations in transformed cells and thereby, promote tumor progression. In the context of OSCC, survivin is overexpressed in OSCC patients. Patients with low survivin expression have significantly higher survival rates than those with high survivin expression; moreover survivin plays an important role during oral carcinogenesis6,7. An early study by Xu et al has shown that the knockdown of survivin by shRNA or siRNA induces apoptosis in tongue squamous cell carcinoma cell lines8. All of this evidence indicates that survivin might serve as a potentially important therapeutic target in the treatment of OSCC9.
Recently, natural products have attracted much attention in the context of cancer chemotherapy because of their potential to effectively suppress tumor growth without harming healthy human tissues. Rumex japonicus Houtt, a member of the family Polygonaceae, is widely distributed in China (known as Yang-Ti, in Chinese). Rumex japonicus Houtt contains a large number of compounds, including anthraquinones, oxanthrones, and flavones10,11. In folk medicine, Rumex japonicus Houtt has been used as an anti-microorganic, a purgative, and an anti-inflammatory agent, and also has been used in anti-tumor therapy for many years10,11,12. Interestingly, recent research has shown that one of the main active ingredients, physcion 8-O-β-glucopyranoside (PG), causes apoptosis and blocks cell cycle progression in the human lung cancer cell line A54913. However, little is known about the mechanism by which PG induces apoptosis in cancer cells. In present study, the OSCC cell line KB was used as model to examine whether PG induces apoptosis and to determine the underlying mechanism. In addition to showing the pro-apoptotic effect of PG in the KB cell line, data from this study demonstrated that survivin plays a key role in the apoptosis-inducing effect of PG, and PG modulates survivin through miR-21/PTEN/Akt/GSK3β signaling.
Materials and methods
Cell culture
The human OSCC-derived cell line KB (ATCC, Shanghai. China) was cultured in Dulbecco's modified Eagle's medium (DMEM) (Sigma Chemical Co, St Louis, MO, USA) containing 10% heat-inactivated FBS (fetal bovine serum), 50 U/ml penicillin and streptomycin. The cell cultures were maintained at 37 °C in a humidified atmosphere of 5% CO2.
Cell viability test
Cell viability was determined via a commercial kit (WST-8 Cell Counting Kit-8, Beyotime, Nantong, China). According the manufacturer's instructions, cells at a density of 3×104 were placed in 96-well culture plates and cultured for the indicated time. Then, 10 μl of the CCK-8 solution was added to each well and the cells were cultured at 37 °C for another hour. Cell viability was assessed by measuring absorbance at 450 nm (ELX-800, Bio-Tek Instruments, Winooski, USA).
Cell apoptosis assay
The proapoptotic effect of PG was determined by flow cytometry (FITC Annexin V apoptosis kit, BD Pharmingen, NJ, USA). Briefly, the cells were rinsed with ice-cold PBS buffer before being resuspended in binding buffer at a final density of 1×106 cells/ml. The cells were then stained with annexin V-FITC and propidium iodide (PI) for 15 min in the dark, and the apoptosis rate was analyzed (Beckman Coulter Inc, FL, USA). Annexin V-FITC positive cells were regarded as undergoing apoptosis, and those negative for FITC were regarded as living cells.
Determination of miRNA and mRNA expression
Gene expression was determined by quantitative real time PCR (qPCR) using gene-specific primers as described previously14. In brief, total RNA was extracted using a commercial kit (RNeasy Mini kit, Qiagen, Dusseldorf, Germany). For miRNA expression, 40 ng of cDNA, which was obtained by reverse-transcription, was used as a template for the PCR reaction14. mRNA expression was detected using a master mix that included a SYBR GREEN master mix (Solarbio Co, Beijing, China), a forward primer, a reverse primer, and template cDNA (10 ng), on a BioRad iCycler. Gene expression was analyzed by using U6 or GAPDH as an internal standard.
Construction of plasmids and cell transfection
To investigate the role of survivin in PG-induced apoptosis in KB cells, survivin was overexpressed as previously described15. Briefly, a full-length cDNA fragment, encoding human survivin, was obtained by reverse transcription and PCR with the survivin primers15 and was inserted into the pEGFP-N1 vector (Takara Biomedical Technology Co, Ltd, Beijing, China). The resulting plasmid was named pEGFP-N1-survivin. Then, the pEGFP-N1-survivin vector was cloned into KB cells to produce survivin overexpression. KB cells were transfected with an empty pEGFP-N1 vector that used as a control. Forty-eight hours after transfection, a G418 solution was used to select the stable clones.
Knockdown of survivin in KB cells
Survivin knockdown was performed by using survivin specific siRNA (Santa Cruz, CA, USA). A scrambled siRNA was used as a control. The siRNA transfection was performed according to the manufacturer's instructions (Lipofectamine-2000, Invitrogen, Carlsbad, CA, USA). Sixteen hours after transfection, the culture medium was changed, and survivin expression was examined 24 h after transfection.
miR-21 transfection
The lentiviral constructs miR-21 mimic and miR-con, and the miR-21 inhibitor were obtained from Qiagen (Dusseldorf, Germany). KB cells were seeded into each well of a 96-well plate, incubated overnight, and then, were transfected with either miR-21 mimic, miR-21 inhibitor or control miRNA according to the manufacturer's instructions (Lipofectamine-2000, Invitrogen, Carlsbad, CA, USA). The transfection efficiency was confirmed by qPCR analysis.
Western blotting analysis
Following treatment, the cells were collected and incubated with ice-cold lysis buffer for 30 min on ice before being centrifuged at 4 °C at 12 000 r/min for 5 min Then, 50 μg of the lysate protein was subjected to a 10% SDS-PAGE before being transferred onto PVDF membranes (Millipore, MA, USA). Specific antibodies were used to probe the proteins. The blots were examined using a chemiluminescent substrate (KPL, Guildford, UK). The protein quantity was determined using BandScan software (Glyko, Novato, CA).
Caspase-3 and caspase-9 activity analysis
To analyze the activity of caspase-3 and caspase-9, the cytosolic protein from the cells were extracted in a hypotonic cell lysis buffer. The cytosolic extracts from 30 μg of protein were analyzed using a colorimetric assay kit specific for caspase-3 and caspase-9 (Ray Biotech, Guangzhou, China).
Mitochondrial Membrane Potential (MMP) assay
The changes in MMP were examined using fluorochrome dye JC-1 following a standard protocol. Briefly, KB cells were challenged with the indicated dose of PG for 48 h before the cells were harvested and incubated with JC-1. The cells were then gently rinsed with PBS to remove excessive dye before the fluorescence signal was quantitatively analyzed by flow cytometry.
Anticancer effect in vivo
To determine whether PG exerts an anti-cancer effect in vivo, 60 male Balb/c nude mice (4–6 weeks old) were injected with KB cells (1.5×106 cells per mouse) in the dorsal flank to create subcutaneous tumors. Once palpable tumor masses were established, the mice were randomly allocated into 4 groups (n=15 in each group). Mice in the different groups were then intraperitoneally (IP) injected with different dosages of PG (dissolved in 0.9% saline containing 1% DMSO). Group (A) received vehicle, and groups (B), (C) and (D) were administered with 10 mg/kg, 20 mg/kg or 40 mg/kg of PG, respectively per day. As a control, the same amount of saline was injected. Tumors were examined every 3 days, and the tumor volumes were calculated using the formula V=1/2ab2 (where a is the largest diameter and b is the smallest diameter). The animals were observed for 24 days. At the end of the study, the animals were sacrificed, and the tumors were harvested to prepare the RNA and measure the expression of survivin, PTEN and miR-21 using qRT-PCR. All of the manipulations involving living mice were approved by the Animal Care and Use Committee of the Affiliated Hospital of Qingdao University.
Statistical analysis
All of the experiments in this study were conducted in triplicate and were performed three times unless stated otherwise. The data are presented in the form of the mean±SD (standard deviation). Comparisons were conducted by a one-way ANOVA using SPSS 13.0 software. P<0.05 was regarded as statistically significant.
Results
PG decreases the viability of KB cells in a time- and concentration-dependent manner
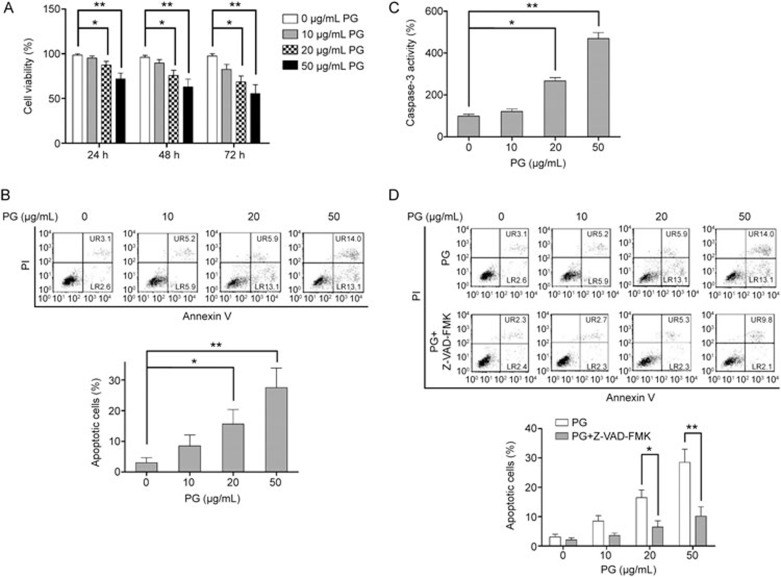
To assess the effect of PG on cell viability, KB cells were exposed to various concentrations (0, 10, 20, 50 μg/ml) of PG for 24, 48 or 72 h. As shown in Figure 1A, PG suppresses the proliferation of KB cells in a time- and concentration-dependent manner. Treatment with PG for 24 h at concentrations of 10, 20 and 50 μg/ml reduced the viability of KB cells by 4.7%±0.9%, 12.5%±4.2% and 27.9%±6.3%, respectively. Following treatment with PG for 48 h, the cell viability was reduced by 10.3%±1.4%, 24.2%±5.9% and 37.1%±5.6%, respectively. Following PG treatment for 72 h, PG caused a further decrease in cell viability, and cell viability was reduced to 44.6%±5.4%. Given the ability of PG to suppress cell proliferation at 48 h, we chose 48 h for the subsequent experiments.
Figure 1.
PG inhibits cell proliferation and induces apoptosis in KB cells. KB cells were incubated with PG at the indicated concentration for 48 h when no time is indicated. (A) PG inhibits cell proliferation in KB cells in a dose- and time-dependent manner. (B) PG induces apoptosis in a dose-dependent manner. (C) PG activates caspase-3 in a dose-dependent manner. (D) Z-VAD-FMK significantly blocks PG-induced apoptosis in KB cells. Mean±SD. n=3. *P<0.05, **P<0.01.
PG induces apoptosis in mitochondria-dependent pathway
Next, we investigated the apoptosis-inducing effect of PG at different concentrations. As shown in Figure 1B, PG induced apoptosis in KB cells in a dose-dependent manner. PG treatment at 10 μg/ml did not cause significant apoptosis in KB cells, whereas PG at 20 and 50 μg/ml induced a significant increase in apoptosis compared to the KB cells treated with vehicle. Because caspase-3 activation is a hallmark of cell apoptosis, the activation of caspase-3 was examined to confirm the apoptosis-inducing effect of PG on KB cells. Our results showed that PG increased caspase-3 activation in a dose-dependent manner (Figure 1C). Recently, a few studies have demonstrated the ability of a natural product to induce apoptosis in tumor cells via a caspase-independent pathway16. To fully appreciate the underlying mechanism of the apoptosis-inducing effect of PG, a caspase inhibitor (Z-VAD-FMK) was used. As shown in Figure 1D, Z-VAD-FMK treatment significantly abolished the apoptosis-inducing effect of PG, suggesting that PG treatment induced apoptosis in KB cells via activating the caspase cascade.
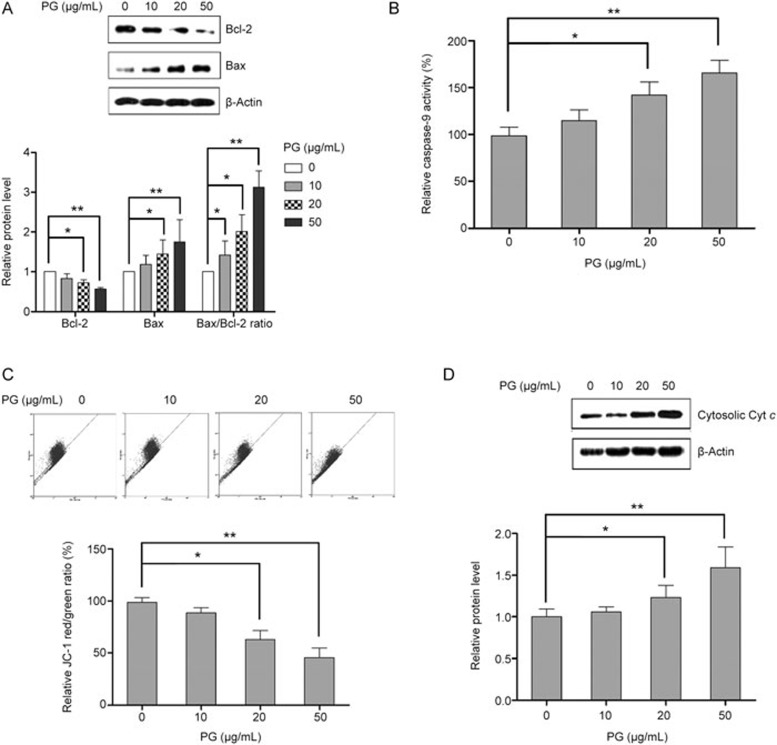
Apoptosis may occur through either an intrinsic or extrinsic pathway, corresponding to the mitochondria-dependent or mitochondria-independent pathway, respectively17. Mitochondria-mediated apoptosis or intrinsic apoptosis is controlled by the Bcl-2 family of proteins. As shown in Figure 2A, PG treatment decreased Bcl-2 and increased Bax expression with an increased Bax/Bcl-2 ratio, suggesting that PG induced apoptosis in KB cells via the mitochondrial pathway. Moreover, the mitochondrial apoptosis pathway was evidenced by the activation of caspase-9, a decrease in MMP and a cytochrome c shift from the mitochondria to the cytosol. Therefore, to further confirm the role of the mitochondria in PG-induced apoptosis, the changes in caspase-9 activity, MMP and the level of cytosolic cytochrome c were examined. Our results showed that PG treatment led to dose-dependent loss of MMP, activation of caspase-9 and increased cytosolic cytochrome c compared with the cells treated with vehicle (Figure 2B, 2C and 2D).
Figure 2.
PG induces apoptosis in KB cells via the mitochondrial pathway. KB cells were challenged with PG at different doses for 48 h. (A)PG increases the Bax/Bcl-2 ratio in a concentration-dependent manner. (B) PG activates caspase-9 in a concentration-dependent manner. (C) PG causes the loss of mitochondrial membrane potential. (D) PG treatment results in an increase in cytosolic cyt c. Mean±SD. n=3. *P<0.05, **P<0.01.
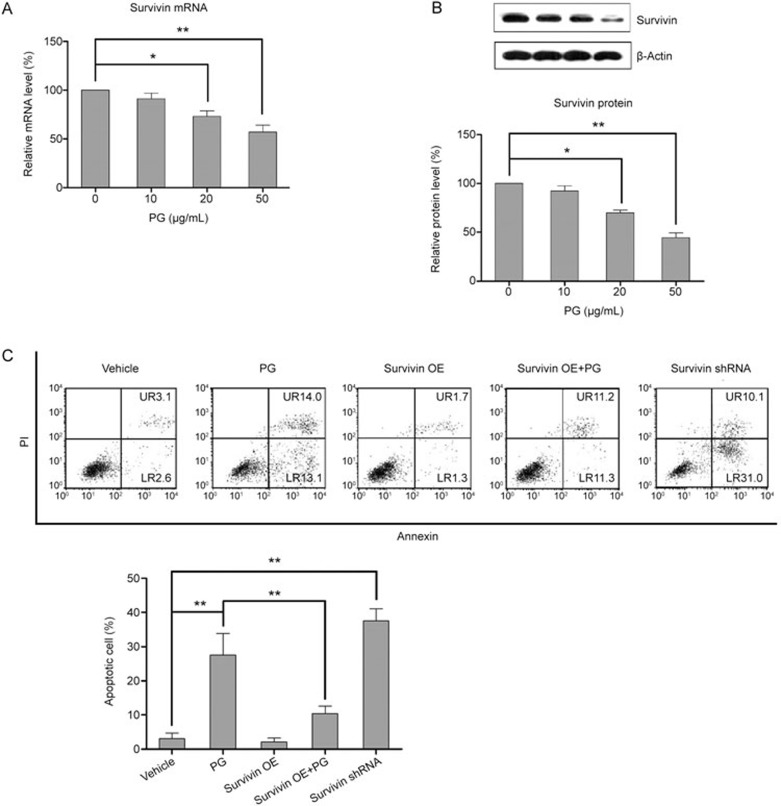
PG induces apoptosis in KB cells by modulating survivin
Research by Pennati et al has highlighted the role of survivin in apoptosis18. Therefore, we investigated whether PG induced apoptosis by modulating survivin. As shown in Figure 3A and 3B, PG led to a dose-dependent decrease in both survivin mRNA and protein levels. To further appreciate the role of survivin in PG-induced apoptosis, KB cells were transfected with a survivin overexpression plasmid. As shown in Figure 3C, overexpressing survivin significantly blocked PG-induced apoptosis in KB cells. In contrast, as shown in Figure 3C, survivin silenced by shRNA led to a significantly increased apoptotic population, supporting the role of survivin in mediating apoptosis. Together, our results suggest that PG induces apoptosis in KB cells, at least partly, by modulating survivin.
Figure 3.
PG induces apoptosis in KB cells by targeting survivin. KB cells were challenged with PG at the indicated concentration (50 μg/ml if not indicated) for 48 h. (A) PG suppresses the mRNA expression of survivin in a concentration-dependent manner. (B) PG concentration-dependently suppresses survivin protein expression. (C) Flow cytometric analysis showing the apoptosis-inducing effect of PG in survivin overexpressing KB cells. Mean±SD. n=3. *P<0.05, **P<0.01.
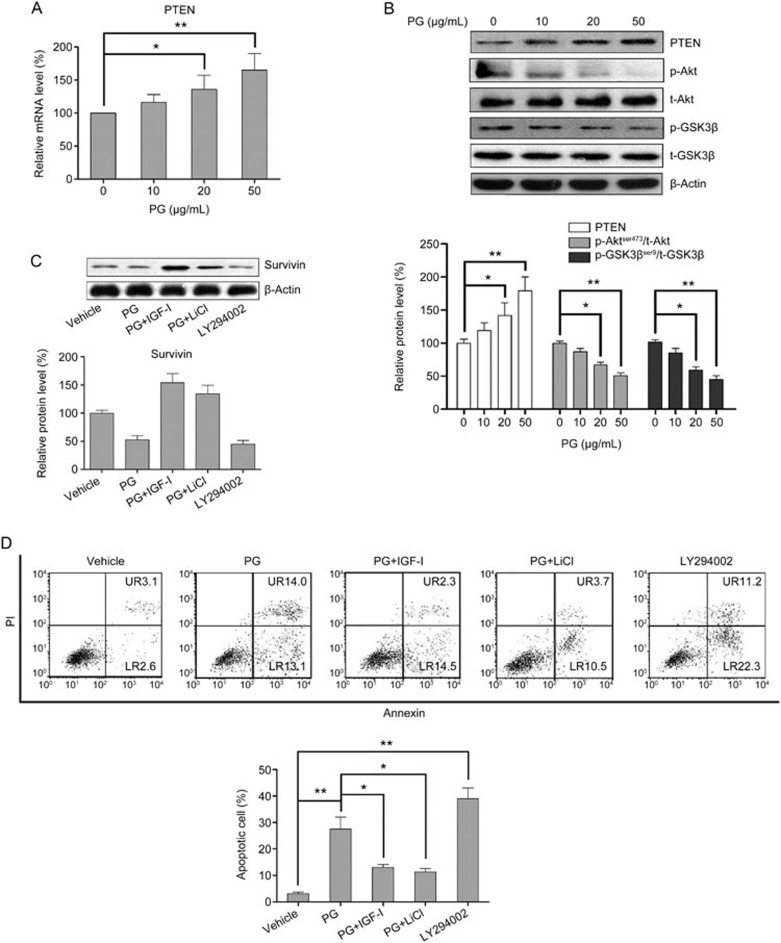
PG modulates survivin expression via miR-21/PTEN/Akt/GSK3β signaling
PTEN/Akt/GSK3β signaling has been proposed to regulate a number of biological activities in cancer cells, including apoptosis19,20. In addition, a recent study has shown that the anthraquinone derivative exerts an anti-cancer effect via PTEN/Akt signaling21. Therefore, we postulated that PG might modulate survivin and induce apoptosis in KB cells by modulating PTEN/Akt/GSK3β signaling. As shown in Figure 4A and 4B, PG increased the expression of PTEN mRNA and protein in a concentration-dependent manner. Our results also showed that PG inactivated Akt/GSK3β signaling by decreasing the phosphorylation of Akt and GSK3β (Ser9) (Figure 4B). To further demonstrate the involvement of Akt/GSK3β signaling in the pro-apoptotic effect of PG, the Akt/GSK3β pathway was inhibited or activated by using a pharmacological inhibitor or activator. As shown in Figure 4C, suppressing Akt phosphorylation with 10 μmol/L LY294002 (a specific Akt inhibitor) downregulated the expression of survivin. Meanwhile, activating Akt or inactivating GSK3β signaling by 10 ng/ml IGF-I or 5 mmol/L LiCl significantly attenuated the suppressive effects of PG on survivin expression (Figure 4C). Our results revealed that IGF-I or LiCl significantly attenuated the apoptosis-inducing effect of PG on KB cells, to an extent corresponding to the expression level of survivin.
Figure 4.
PG modulates survivin levels via regulating PTEN/Akt/GSK3β signaling in KB cells. KB cells were incubated with PG at the indicated concentrations (50 μg/ml if not indicated) for 48 h. (A) PG treatment results in increased PTEN mRNA levels in a dose-dependent manner. (B) PG treatment results in increased PTEN protein levels and the inhibition of Akt/GSK3β signaling. (C) The activation of Akt/GSK3β signaling abolishes the suppressive effect of PG on survivin expression. (D) The activation of Akt/GSK3β signaling abolishes the apoptosis-inducing effect of PG in KB cells. Mean±SD. n=3. *P<0.05, **P<0.01.
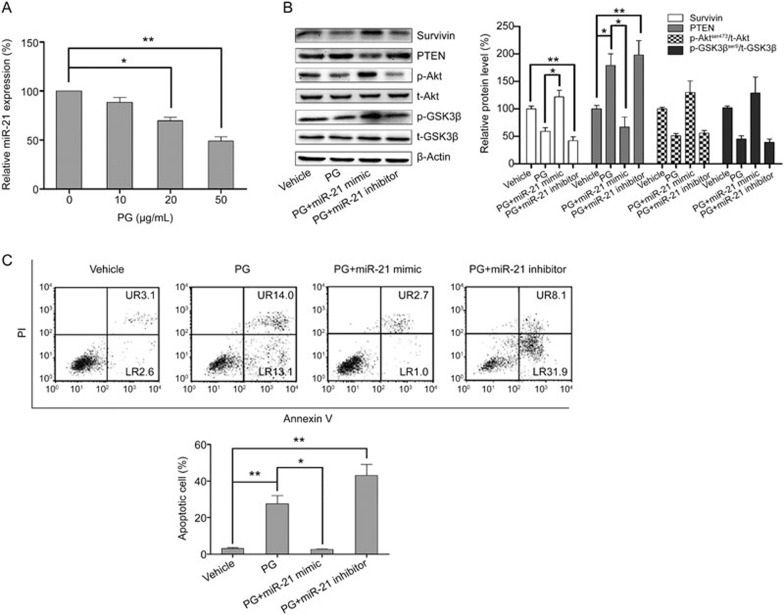
Next, we conducted experiments to explore the upstream signaling that regulates the inactivation of PTEN/Akt/GSK3β signaling by PG. A number of studies have shown that miR-21 is an important modulator involved in a variety biological activities of cancer cells by acting upstream of the PTEN/Akt pathway22,23. In our study, PG decreased the expression of miR-21 in a dose-dependent manner (Figure 5A). Then, to verify the role of miR-21 as an upstream regulator of the PTEN/Akt/GSK3β pathway and a regulator of the expression of survivin, a miR-21 mimic and a miR-21 inhibitor were used. As shown in Figure 5B, the miR-21 inhibitor exerted a similar effect on PTEN/Akt/GSK3β signaling as PG, whereas the miR-21 mimic significantly abolished the effect of PG on PTEN/Akt/GSK3β signaling. Meanwhile, the miR-21 mimic significantly abrogated the suppressive effect of PG on survivin. The effect of the miR-21 mimic or inhibitor on cell apoptosis was also examined to confirm the involvement of miR-21 in the apoptosis-inducing effect of PG. As shown in Figure 5C, the miR-21 mimic significantly attenuated PG-induced apoptosis in KB cells. Collectively, our results demonstrate that PG induces apoptosis in KB cells, at least in part by modulating survivin via miR-21/PTEN/Akt/GSK3β signaling.
Figure 5.
PG regulates PTEN/Akt/GSK3β signaling by targeting miR-21. KB cells were incubated with PG at the indicated concentrations (50 μg/ml if not marked) for 48 h. (A) PG inhibits the expression of miR-21 in a dose-dependent manner. (B) The PG-mediated suppression of survivin expression via PTEN/Akt/GSK3β signaling is abrogated in miR-21 overexpressing KB cells. (C) Flow cytometric analysis showing the apoptosis-inducing effect of PG in the survivin overexpressing KB cells. Mean±SD. n=15. *P<0.05, **P<0.01.
In vivo anticancer effect of PG
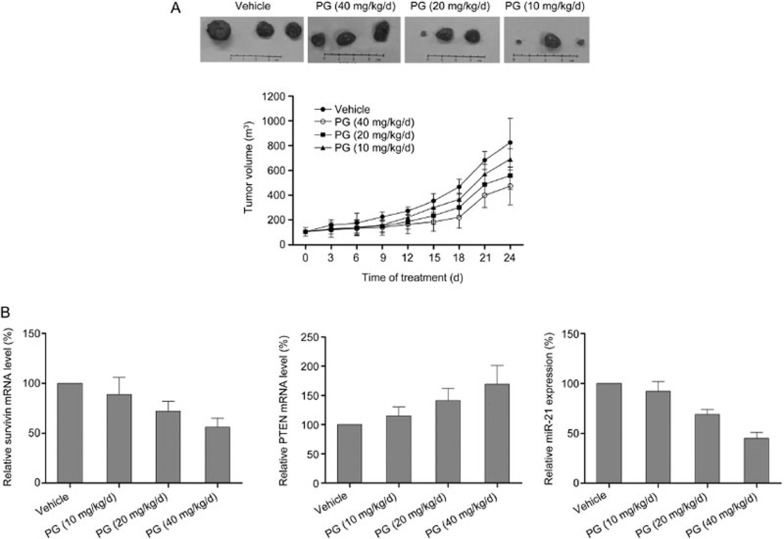
After obtaining encouraging results from the in vitro experiments, we sought to investigate the in vivo effect of PG. Nude mice were grafted with KB cells, and the tumors were allowed to grow to 100 mm3. Then, the mice were treated with different dosages of PG (40, 20, and 10 mg/kg/day). The effectiveness of the treatment was evaluated by examining the tumor volume. As shown in Figure 6A, PG inhibited tumor growth dose-dependently, and the anti-tumor effect was significant at a dosage of 20 mg/kg/day (P<0.05 vs vehicle). Moreover, the PCR results showed that PG caused a marked and significant decrease in the transcription of survivin mRNA (P< 0.05), suggesting the in vivo effectiveness of this compound in inhibiting tumor growth by suppressing survivin (Figure 6B). Moreover, the inhibiting effect of PG on tumor growth was associated with a significantly decreased expression of miR-21 and a significantly increased expression of PTEN, further supporting our in vitro findings.
Figure 6.
PG suppresses tumor growth in a xenograft mouse model. (A) PG treatment significantly inhibits tumor growth as evaluated by tumor volume. (B) The effect of PG on the gene transcription of survivin, PTEN, and miR-21. Mean±SD. n=3. *P<0.05, **P<0.01.
Discussion
Apoptosis, which is programmed cell death, can occur via the cell death receptor-mediated extrinsic pathway or the mitochondria-mediated intrinsic pathways. A number of stimuli trigger apoptosis, including cellular reactive oxygen species (ROS), reactive nitrogen species (RNS), hormones, cell–cell interaction, growth factor withdrawal, antigens and chemotherapeutics24,25. Cancer development correlates with decreased apoptosis and increased proliferation of cancer cells. Therefore, apoptosis induction has been proposed as an effective strategy in cancer therapy. In the present study, we found that PG time- and dose-dependently induced apoptosis in OSCC cell lines. In addition, we explored the signaling pathway that might play a role in PG-induced OSCC cell apoptosis. To our knowledge, this present study is the first to link survivin to the anti-neoplastic property of PG in OSCC cell lines, and it suggests that PG-mediated suppression of survivin is involved in the pro-apoptotic effect of PG.
Death receptor-triggered extrinsic apoptosis and mitochondrial-initiated intrinsic apoptosis are indicated by activation of caspase-8 and caspase-9, respectively26,27. In present study, the PG-mediated activation of caspase-9 and caspase-3, as well as the result that the caspase inhibitor Z-VAD-FMK significantly blocked PG-induced apoptosis in KB cells, indicated that PG induces apoptosis primarily via the mitochondrial-mediated caspase pathway. Furthermore, the PG-induced downregulation of Bcl-2, a powerful antagonist of the mitochondrial pathway of apoptosis, provided additional documentation that the proapoptotic effect of PG was related to the mitochondrial-mediated activation of the caspase cascade.
Survivin (BIRC5), a member of the inhibitor of apoptosis (IAP) family, plays an important role in apoptosis and cell division. In contrast to other IAP protein molecules, survivin is expressed in embryonic and fetal tissues but not in normal adult tissues28,29. Interestingly, survivin is highly expressed in human malignant cells. A number of preclinical studies have shown that survivin inhibition by a specific inhibitor or siRNA suppresses tumor cell proliferation and invasion and increases chemosensitivity to therapeutic agents30. Our finding that PG appears to downregulate survivin in OSCC directly suggests that it might be a useful agent in the therapeutic regimen of OSCC. In addition to its important role in apoptosis and cell division, survivin is also involved in the regulation of the metastasis of human malignancies. An in vivo study by Kogo et al has shown that survivin knockdown by siRNA significantly delays tumor development and lymph node metastasis in cervical cancer31. Directly silencing survivin by siRNA also inhibits invasion in neuroblastoma SH-SY5Y cells32. Another in vivo study by Zhang et al has found that the inhibition of survivin dramatically inhibits spontaneous metastasis in Dunning prostate cancer33. Moreover, clinical evidence has shown that the survivin level is associated with nodal metastasis in T1-T2 squamous cell carcinoma of the tongue34. Therefore, by downregulating survivin, PG might also exert an anti-metastatic effect in OSCC in addition to inducing apoptosis.
microRNAs (miRNAs) are short noncoding RNAs that regulate the expression of multiple genes at the posttranscriptional level35. Numerous studies have established that dysregulation of miRNA expression is present in various human tumors36. In particular, the association between miR-21 overexpression and human malignancy has been well established37. miR-21 plays a role in modulating cell proliferation, apoptosis and epithelial to mesenchymal transition in tumor development38,39. As for OSCC, clinical evidence has shown that elevated miR-21 expression is a predictor of a poorer prognosis for patients with tongue squamous cell carcinomas, and miR-21 has been identified as an apoptosis inhibitor40. In vitro and in vivo studies have also demonstrated that targeting miR-21 with an antisense oligonucleotide markedly inhibits proliferation, promotes apoptosis and suppresses migration and invasion41,42. Consistently with these previous findings, the results of the present study showed that the apoptosis-inducing effect of PG was associated with suppression of miR-21 expression, further supporting the involvement of miR-21 in OSCC development. An early study has noted that miR-21 modulates the chemosensitivity of tongue squamous cell carcinoma cells to cisplatin43, and a recent study by Zhou et al has shown that WP1066 (STAT3 inhibitor) sensitizes oral squamous cell carcinoma cells to cisplatin by targeting the STAT3/miR-21 axis44. Given the suppressive effect of PG on miR-21, PG also has the potential to be used as a sensitizing agent for cisplatin treatment in OSCC.
Several tumor suppressors, including PDCD4, PTEN, TPM1 and SPRY2, have been identified as mRNA targets of miR-21 in various cancer cell lines41. Among these mRNA targets, PTEN is an important regulator connecting miR-21 to downstream signaling. In this study, our results also showed that PG modulated survivin expression by targeting the miR-21/PTEN/Akt axis. However, PTEN/Akt acts as an upstream signaling component that regulates the expression of miR-21 in prostate cancer45. Moreover, silencing survivin causes a partial mesenchymal-epithelial transition in human pancreatic cancer cells via the PTEN/PI3K/Akt pathway46. These studies, combined with our results, suggest that it is highly possible that the regulatory mechanism between miR-21 and survivin is different and specific in various cancer cells.
In summary, our study indicated that PG induces cell apoptosis in OSCC cells, at least in part by suppressing survivin expression by targeting the miR-21/PTEN/Akt/GSK3β axis, suggesting the possibility that PG might be used as an anti-cancer agent. However, further studies, including clinical trials, are warranted to make a comprehensive evaluation on the clinical value of PG as a novel anti-neoplastic agent.
Author contribution
Meng-dong LIU and Shi-jiang XIONG initiated the project and participated in the design of the study. Meng-dong LIU, Shi-jiang XIONG, Fei TAN, and Yi LIU contributed to the study design and performed the experiments. Meng-dong LIU and Shi-jiang XIONG wrote the paper.
References
- Hamada T, Wakamatsu T, Miyahara M, Nagata S, Nomura M, Kamikawa Y, et al. MUC4: a novel prognostic factor of oral squamous cell carcinoma. Int J Cancer 2012; 130: 1768–76. [DOI] [PubMed] [Google Scholar]
- Petersen PE. Oral cancer prevention and control--the approach of the World Health Organization. Oral Oncol 2009; 45: 454–60. [DOI] [PubMed] [Google Scholar]
- Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol 2009; 45: 309–16. [DOI] [PubMed] [Google Scholar]
- Ambrosini G, Adida C, Altieri DC. A novel anti-apoptosis gene, survivin, expressed in cancer and lymphoma. Nat Med 1997; 3: 917–21. [DOI] [PubMed] [Google Scholar]
- Tamm I, Wang Y, Sausville E, Scudiero DA, Vigna N, Oltersdorf T, et al. IAP-family protein survivin inhibits caspase activity and apoptosis induced by Fas (CD95), Bax, caspases, and anticancer drugs. Cancer Res 1998; 58: 5315–20. [PubMed] [Google Scholar]
- Tanaka C, Uzawa K, Shibahara T, Yokoe H, Noma H, Tanzawa H. Expression of an inhibitor of apoptosis, survivin, in oral carcinogenesis. J Dent Res 2003; 82: 607–11. [DOI] [PubMed] [Google Scholar]
- Lo Muzio L, Pannone G, Staibano S, Mignogna MD, Rubini C, Mariggio MA, et al. Survivin expression in oral squamous cell carcinoma. Br J Cancer 2003; 89: 2244–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu JH, Wang AX, Huang HZ, Wang JG, Pan CB, Zhang B. Survivin shRNA induces caspase-3-dependent apoptosis and enhances cisplatin sensitivity in squamous cell carcinoma of the tongue. Oncol Res 2010; 18: 377–85. [DOI] [PubMed] [Google Scholar]
- Altieri DC. Survivin, cancer networks and pathway-directed drug discovery. Nat Rev Cancer 2008; 8: 61–70. [DOI] [PubMed] [Google Scholar]
- Jiang L, Zhang S, Xuan L. Oxanthrone C-glycosides and epoxynaphthoquinol from the roots of Rumex japonicus. Phytochemistry 2007; 68: 2444–9. [DOI] [PubMed] [Google Scholar]
- Zhou X, Xuan L, Zhang S. Study on the chemical constituents from Rumex japonicus Houtt. Zhong Yao Cai 2005; 28: 104–5. [PubMed] [Google Scholar]
- Belkin M, Fitzgerald DB. Tumor-damaging capacity of plant materials. I. Plants used as cathartics. J Natl Cancer Inst 1952; 13: 139–55. [PubMed] [Google Scholar]
- Xie QC, Yang YP. Anti-proliferative of physcion 8-O-beta-glucopyranoside isolated from Rumex japonicus Houtt. on A549 cell lines via inducing apoptosis and cell cycle arrest. BMC Complement Altern Med 2014; 14: 377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang CH, Yue J, Fan M, Pfeffer LM. IFN induces miR-21 through a signal transducer and activator of transcription 3-dependent pathway as a suppressive negative feedback on IFN-induced apoptosis. Cancer Res 2010; 70: 8108–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okamoto K, Okamoto I, Okamoto W, Tanaka K, Takezawa K, Kuwata K, et al. Role of survivin in EGFR inhibitor-induced apoptosis in non-small cell lung cancers positive for EGFR mutations. Cancer Res 2010; 70: 10402–10. [DOI] [PubMed] [Google Scholar]
- Zhou H, Xu M, Gao Y, Deng Z, Cao H, Zhang W, et al. Matrine induces caspase-independent program cell death in hepatocellular carcinoma through bid-mediated nuclear translocation of apoptosis inducing factor. Mol Cancer 2014; 13: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elmore S. Apoptosis: a review of programmed cell death. Toxicol Pathol 2007; 35: 495–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennati M, Folini M, Zaffaroni N. Targeting survivin in cancer therapy. Expert Opin Ther Targets 2008; 12: 463–76. [DOI] [PubMed] [Google Scholar]
- Tseng PC, Huang WC, Chen CL, Sheu BS, Shan YS, Tsai CC, et al. Regulation of SHP2 by PTEN/AKT/GSK-3beta signaling facilitates IFN-gamma resistance in hyperproliferating gastric cancer. Immunobiology 2012; 217: 926–34. [DOI] [PubMed] [Google Scholar]
- Huang HC, Tang D, Xu K, Jiang ZF. Curcumin attenuates amyloid-beta-induced tau hyperphosphorylation in human neuroblastoma SH-SY5Y cells involving PTEN/Akt/GSK-3beta signaling pathway. J Recept Signal Transduct Res 2014; 34: 26–37. [DOI] [PubMed] [Google Scholar]
- Wang X, Tan T, Mao ZG, Lei N, Wang ZM, Hu B, et al. The marine metabolite SZ-685C induces apoptosis in primary human nonfunctioning pituitary adenoma cells by inhibition of the Akt pathway in vitro. Mar Drugs 2015; 13: 1569–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Jiang K, Zhao F. Icariin regulates the proliferation and apoptosis of human ovarian cancer cells through microRNA-21 by targeting PTEN, RECK and Bcl-2. Oncol Rep 2015; 33: 2829–36. [DOI] [PubMed] [Google Scholar]
- Zhou X, Ren Y, Liu A, Han L, Zhang K, Li S, et al. STAT3 inhibitor WP1066 attenuates miRNA-21 to suppress human oral squamous cell carcinoma growth in vitro and in vivo. Oncol Rep 2014; 31: 2173–80. [DOI] [PubMed] [Google Scholar]
- Ou HC, Lee WJ, Lee SD, Huang CY, Chiu TH, Tsai KL, et al. Ellagic acid protects endothelial cells from oxidized low-density lipoprotein-induced apoptosis by modulating the PI3K/Akt/eNOS pathway. Toxicol Appl Pharmacol 2010; 248: 134–43. [DOI] [PubMed] [Google Scholar]
- Chen X, Zhong Z, Xu Z, Chen L, Wang Y. No protective effect of curcumin on hydrogen peroxide-induced cytotoxicity in HepG2 cells. Pharmacol Rep 2011; 63: 724–32. [DOI] [PubMed] [Google Scholar]
- Dias N, Bailly C. Drugs targeting mitochondrial functions to control tumor cell growth. Biochem Pharmacol 2005; 70: 1–12. [DOI] [PubMed] [Google Scholar]
- Schulze-Osthoff K, Ferrari D, Los M, Wesselborg S, Peter ME. Apoptosis signaling by death receptors. Eur J Biochem 1998; 254: 439–59. [DOI] [PubMed] [Google Scholar]
- Zaffaroni N, Daidone MG. Survivin expression and resistance to anticancer treatments: perspectives for new therapeutic interventions. Drug Resist Updat 2002; 5: 65–72. [DOI] [PubMed] [Google Scholar]
- Coumar MS, Tsai FY, Kanwar JR, Sarvagalla S, Cheung CH. Treat cancers by targeting survivin: just a dream or future reality? Cancer Treat Rev 2013; 39: 802–11. [DOI] [PubMed] [Google Scholar]
- Thomas S, Shah G. Calcitonin induces apoptosis resistance in prostate cancer cell lines against cytotoxic drugs via the Akt/survivin pathway. Cancer Biol Ther 2005; 4: 1226–33. [DOI] [PubMed] [Google Scholar]
- Kogo R, How C, Chaudary N, Bruce J, Shi W, Hill RP, et al. The microRNA-218∼Survivin axis regulates migration, invasion, and lymph node metastasis in cervical cancer. Oncotarget 2015; 6: 1090–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Liang H, Cao W, Xu R, Ju XL. Downregulation of survivin by siRNA inhibits invasion and promotes apoptosis in neuroblastoma SH-SY5Y cells. Braz J Med Biol Res 2014; 47: 548–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang M, Coen JJ, Suzuki Y, Siedow MR, Niemierko A, Khor LY, et al. Survivin is a potential mediator of prostate cancer metastasis. Int J Radiat Oncol Biol Phys 2010; 78: 1095–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dogan M, Cagli S, Yuce I, Bayram A, Somdas MA, Karatas D, et al. Survivin expression correlates with nodal metastasis in T1-T2 squamous cell carcinoma of the tongue. Eur Arch Otorhinolaryngol 2015; 272: 689–94. [DOI] [PubMed] [Google Scholar]
- Yang CH, Yue J, Sims M, Pfeffer LM. The curcumin analog EF24 targets NF-kappaB and miRNA-21, and has potent anticancer activity in vitro and in vivo. PLoS One 2013; 8: e71130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calin GA, Croce CM. MicroRNA signatures in human cancers. Nat Rev Cancer 2006; 6: 857–66. [DOI] [PubMed] [Google Scholar]
- Bartel DP. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell 2004; 116: 281–97. [DOI] [PubMed] [Google Scholar]
- Hermansen SK, Dahlrot RH, Nielsen BS, Hansen S, Kristensen BW. MiR-21 expression in the tumor cell compartment holds unfavorable prognostic value in gliomas. J Neurooncol 2013; 111: 71–81. [DOI] [PubMed] [Google Scholar]
- Wang Y, Li J, Tong L, Zhang J, Zhai A, Xu K, et al. The prognostic value of miR-21 and miR-155 in non-small-cell lung cancer: a meta-analysis. Jpn J Clin Oncol 2013; 43: 813–20. [DOI] [PubMed] [Google Scholar]
- Li J, Huang H, Sun L, Yang M, Pan C, Chen W, et al. MiR-21 indicates poor prognosis in tongue squamous cell carcinomas as an apoptosis inhibitor. Clin Cancer Res 2009; 15: 3998–4008. [DOI] [PubMed] [Google Scholar]
- Wang Y, Zhu Y, Lv P, Li L. Targeting miR-21 with AS-miR-21 suppresses aggressive growth of human tongue squamous cell carcinoma in vivo. Int J Clin Exp Pathol 2015; 8: 4773–81. [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Zhu Y, Lv P, Li L. The role of miR-21 in proliferation and invasion capacity of human tongue squamous cell carcinoma in vitro. Int J Clin Exp Pathol 2015; 8: 4555–63. [PMC free article] [PubMed] [Google Scholar]
- Ren W, Wang X, Gao L, Li S, Yan X, Zhang J, et al. MiR-21 modulates chemosensitivity of tongue squamous cell carcinoma cells to cisplatin by targeting PDCD4. Mol Cell Biochem 2014; 390: 253–62. [DOI] [PubMed] [Google Scholar]
- Zhou X, Ren Y, Liu A, Jin R, Jiang Q, Huang Y, et al. WP1066 sensitizes oral squamous cell carcinoma cells to cisplatin by targeting STAT3/miR-21 axis. Sci Rep 2014; 4: 7461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheth S, Jajoo S, Kaur T, Mukherjea D, Sheehan K, Rybak LP, et al. Resveratrol reduces prostate cancer growth and metastasis by inhibiting the Akt/MicroRNA-21 pathway. PLoS One 2012; 7: e51655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi XP, Han T, Li YX, Long XY, Li WZ. Simultaneous silencing of XIAP and survivin causes partial mesenchymal-epithelial transition of human pancreatic cancer cells via the PTEN/PI3K/Akt pathway. Mol Med Rep 2015; 12: 601–8. [DOI] [PubMed] [Google Scholar]