Abstract
Objective. To describe the extent to which pharmacy students hold negative attitudes toward people living with HIV/AIDS (PLWHA) and to determine whether background variables, student knowledge, and professional attitudes may affect willingness to care for PLWHA.
Methods. An online survey tool was developed and administered to 150 pharmacy students in their third professional year. Descriptive and stepwise multivariate regressions were performed.
Results. While descriptive results showed a majority of respondents had favorable professional attitudes towards caring for PLWHA, most pharmacy students expressed discomfort with specific attitudes about being in close physical contact and receiving selected services from PLWHA. Multivariate results revealed that: (1) being a minority predicted greater knowledge; (2) having received prior HIV instruction and greater HIV knowledge predicted more positive professional attitudes caring for PLWHA; (3) being more socially liberal, having more positive professional attitudes caring for PLWHA, and having greater empathy towards PLWHA predicted student willingness to provide services.
Conclusion. Future educational interventions specifically targeted toward socially conservative whites may impact greater student willingness to care for PLWHA. Additional research should also explore the generalizability of the present findings and modeling to pharmacy students in other regions of the country.
Keywords: attitudes, stigma, HIV, care, pharmacy students
INTRODUCTION
There are approximately 1.2 million individuals with HIV infection aged 13 and older in the United States, 18.1% of whom remain undiagnosed.1 Despite the availability of effective antiretroviral therapy, only 30% of patients with HIV infection in the United States achieve virologic suppression, with poorer outcomes among minority and younger populations.2 Multiple factors, including access to care, medical mistrust, stigma, race, socioeconomic status, and sexual orientation contribute negatively to the success of people living with HIV/AIDS (PLWHA) to engage and be retained in medical care.3-6
As one of the most accessible health care practitioners, pharmacists are in a position to engage with patients who may feel disconnected from the community. Such opportunities may enhance adherence to care and antiretroviral therapy among PLWHA.7 It is unclear, however, to what extent negative attitudes toward PLWHA among pharmacists and pharmacy students impact their willingness to provide care to these patients. Schools and colleges of pharmacy can assess pharmacy student attitudes toward PLWHA and address barriers that may affect future pharmacists’ willingness to serve this population at a time when engagement and retention in care is essential.
In 1994, researchers described attitudes toward PLWHA among pharmacy students in the Boston metropolitan area using the previously validated AIDS Attitude Scale (AAS).8 These authors found that 66.7% of pharmacy students were afraid of contracting the virus in their everyday practice and, if given a choice, 52.5% of students would not work with PLWHA. Furthermore, the authors cited negative attitudes among pharmacy students toward sexual orientation, which served as a driving factor in professional resistance. When compared to nursing and medical students, pharmacy students’ scores were similar with respect to fear of contagion, professional resistance, and negative emotions.8
In 2009, Seacat et al attempted to determine whether there was an association between attribution of HIV infection, personal and professional attitudes toward PLWHA, and knowledge.9 The authors concluded that negative attitudes were predicted by dental students who attributed HIV infection to personal responsibility and who had less HIV knowledge. In 2012, Nyberg et al described the extent by which 184 pharmacy students at schools of pharmacy in Missouri, Indiana, and Oklahoma held stigmatizing beliefs toward PLWHA by using a survey adapted from Herek et al.10,11 While the results were limited by a low survey response rate (12%), the authors reported that 50-60% of students had generally positive attitudes toward PLWHA. More stigmatizing attitudes toward PLWHA were demonstrated by students younger than 22 compared to students who attended college for at least four years prior to entry into pharmacy school.10
Shifts in attitudes and knowledge among health professions students toward PLWHA may have occurred as a result of improvements in antiretroviral therapy and how such therapy has led to substantial reductions in morbidity, mortality, and transmission of HIV infection.9,10,12,13 However, to explore these shifts more closely, there is need to ensure measures are consistent with current language (ie, removing language specifying only AIDS and including persons living with HIV) and avoid as much as possible social desirability bias (ie, tendency to respond in a more favorable way to researchers). Further, to examine attitudinal and behavioral shifts, it is important to develop theoretical models for how factors contribute to the formation of the attitudes and behaviors. For example, we know from prior work that age and HIV knowledge are associated with negative attitudes toward PLWHA.8-10,13-16
However, no known multivariate models control for multiple factors contributing to negative attitudes or explore how background variables, HIV knowledge, and different attitudes relate to student willingness to care for PLWHA. Prior research did not attempt to differentiate between professional and personal attitudes toward PLWHA or how professional attitudes and empathy relate to willingness to provide care to PLWHA. Further, most prior research used the attitudes as study endpoints vs using student willingness to care for PLWHA (ie, behavioral intention to care for PLWHA) as the endpoint, which seems more proximal to the behavior of providing direct care to PLWHA. The Theory of Reasoned Action posits that behavioral intention is a better predictor of behavior than attitudes.17
Moreover, previous survey instruments such as the AAS and other adapted scales18,19 did not explore the role of the student’s political and social conservativeness as possible predictors of negative attitudes. Intuitively, one might suspect political and social conservativeness would impact attitudes and behavioral intentions of interacting with individuals who are associated with an illness potentially contracted by behaviors conflicting with conservative morals and values. However, political conservativeness and social conservatism do not necessarily overlap, as politically conservative individuals may have more liberal orientation towards social issues, and politically liberal individuals may possess more conservative social attitudes. Understanding the role of a students’ political and social orientations in attitudes towards providing care to PLWHA may help inform and target educational interventions to those in most need of the interventions.
The advent of antiretroviral therapy in conjunction with improved educational efforts among the public and in health professions curricula may have resulted in shifts in pharmacy student knowledge and attitudes toward PLWHA over the last decade. Therefore, we sought to describe the extent to which pharmacy students currently hold negative attitudes toward PLWHA. We also sought to expand the literature in this area by exploring regression models that examine the relationship between background variables (adding social conservativeness), HIV knowledge, different attitudes toward PLWHA, and pharmacy students’ willingness to provide services to PLWHA.
METHODS
Using a cross-sectional design, a convenience sample of 150 pharmacy students in their third professional year were invited to complete an online survey (as a Google document) prior to a required module providing first-time exposure on HIV pharmacotherapy and following a module covering asthma. The survey was administered in fall 2012. Students were given the survey to complete as extra credit. The survey was anonymous—students were assigned a study identification number and the link between study identification number and survey responses were kept in a separate location. Researchers did a pilot test of their survey instrument in spring 2012 to explore acceptability and understanding of question wording and instrument validation. The survey developed had four main sections: (1) student background, (2) attitudes toward PLWHA, (3) HIV knowledge, and (4) willingness to engage PLWHA.
The student background section included items on gender, age, race, educational background on HIV, political and social orientation, and previous engagement in high risk behaviors (alcohol use, use of recreational substances, and unprotected sex). Respondents indicated their political and social orientation using Likert scales from extremely liberal to extremely conservative. These scales also gave respondents the choice to indicate they didn’t know their political or social orientation or indicate “other.” The “don’t know” and “other” respondents were removed from the regression analyses noted below. Respondents rated the frequency of each of these high-risk behaviors as: 0=never, 1=sometimes, 2=often, and 3= very often. A sum was computed across the three latter behaviors.
The second section on attitudes toward PLWHA was based on previously validated HIV stigma scales.1,12,13 These scales were revised to adjust for language and phrasing to be less restrictive to AIDS and consider more broadly HIV, maximize student understanding of questions, limit social desirability bias, and attempt to elicit more subtle stigmatizing attitudes. For example, previously validated scales from the 1980s used “AIDS” and were developed prior to effective antiretroviral therapy. These items were adjusted to “HIV” to include appropriate present-day terminology and treatment availability and to minimize student selection of inappropriate responses. For example, “All pregnant women infected with HIV will have babies born with AIDS” was changed to “A pregnant woman with HIV can take drugs to reduce the risk of her baby being infected.” This change was also made to minimize social desirability bias. While previously validated scales did address the lack of achievable cure, they did not address any potential benefits of antiretroviral therapy. Therefore, we added an item addressing the reduction of mortality and increased life expectancy among patients with HIV on antiretroviral therapy.
Factor analyses identified three primary sets of attitudes: (1) five statements measuring general attitudes toward personal interactions with persons with HIV for which students were asked to compare their attitudes to those of what they thought pharmacy or nursing students would think (Cronbach alpha:0.82), (2) seven statements reflecting empathic orientation towards persons with HIV (Cronbach alpha:0.81), and (3) six statements about professional interaction with persons with HIV or others at high risk of HIV (Cronbach alpha: 0.82). There were four other attitudes assessed that did not fit into these scales: HIV is not a sign of personal failure; a person with HIV is as productive as a person without HIV; it is uncomfortable working with persons with HIV; and if a person with HIV approached me, I might be uncomfortable and back away a little. All attitudes in this second section were measured using the Likert scale of 1=strongly disagree, 2=disagree, 3=neither agree nor disagree, 4=agree, and 5=strongly agree. Higher scores meant more positive attitudes of personal interaction with persons with HIV and student empathic orientation toward persons with HIV. Conversely, the higher the score, the more negative the attitudes were in professional interactions with persons with HIV and at risk of HIV.
The third section of the survey included 24 knowledge statements in which students indicated if the statement was true or not. These items were based on previously published HIV knowledge questionnaires and wording amended for understanding and reduction in potential social desirability bias.2,4 A validated scoring methodology was based on correct responses, with higher scores indicating greater knowledge.4 Respondents in the present study were given three choices for responses: true, false, and don’t know. Questions answered “don’t know” were included as an incorrect response in the analysis.
The final section of the survey explored student willingness to provide services to PLWHA. This was a newly developed section but modeled after the methodology used in a previous pharmacy stigma study.20 This section included six statements about willingness to counsel PLWHA and those with asthma. Respondents used the same Likert scale as used in the attitude section of the survey. A higher score in this section meant greater willingness to provide services to PLWHA vs patients with asthma. The Cronbach alpha of willingness to provide services to PLWHA was 0.87.
The analytic plan involved conducting: descriptive statistics on all study variables; bivariate tests to detect differences between willingness to provide services to PLWHA and those with asthma; and multivariate statistics to identify significant relationships between how background variables, HIV knowledge, and attitudes toward PLWHA affect pharmacy students’ willingness to provide services to PLWHA. While many items were based on previously validated scales, attitudes were presented in tables according to how they were thematically connected and not organized according to a specific scale. A repeated-measures analysis of variance was conducted to determine differences among the three perspectives regarding respondents’ reported attitudes about personal interactions with persons with HIV and what they thought other pharmacy students and nursing students thought about the same attitudes. Additional tests for pairwise comparisons were conducted to discern within-group differences between the three perspectives. Mann-Whitney U test was performed comparing responses on items of willingness to provide different services to patients with HIV vs asthma. Significance was set a priori at p≤0.05. The project received approval from the university’s institutional review board.
RESULTS
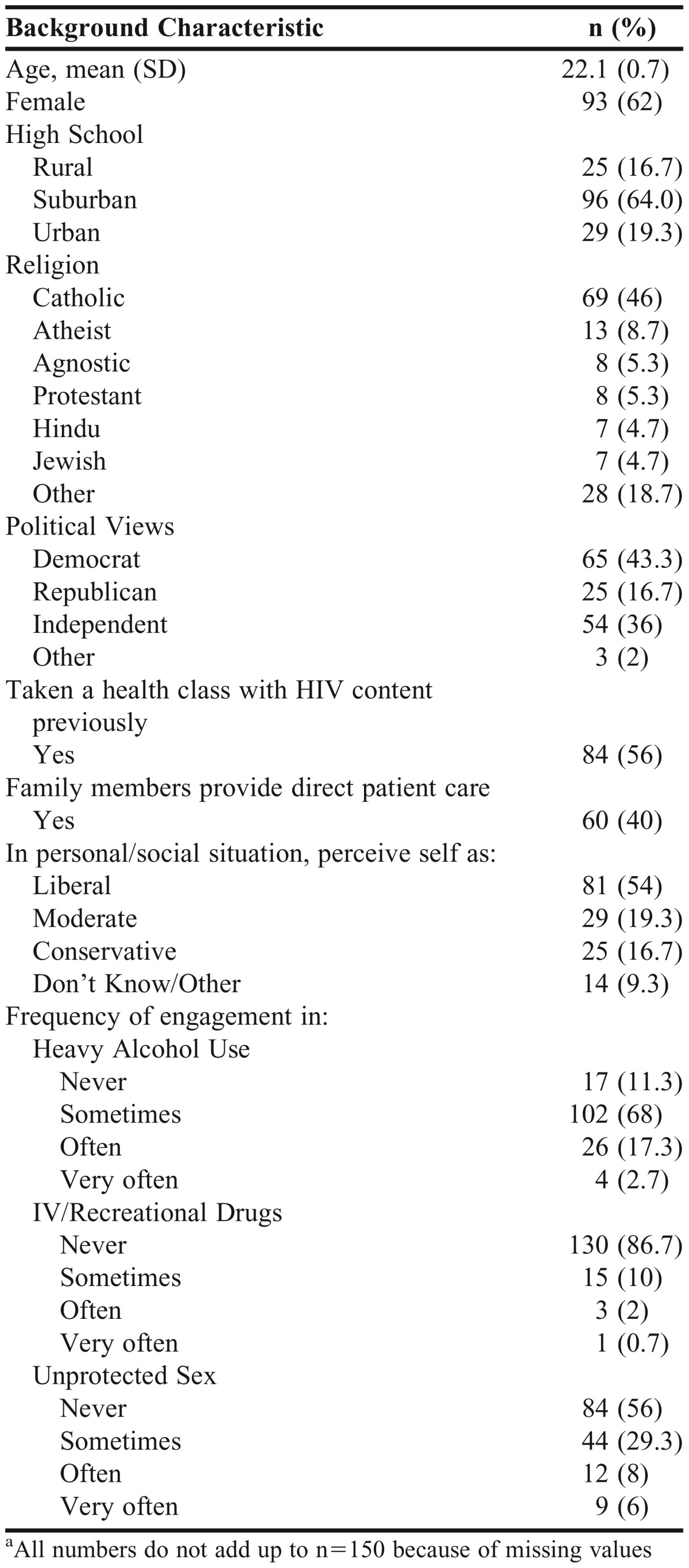
All 150 students enrolled in the fall 2012 pharmacotherapy course participated in the survey. Background characteristics of the sample are provided in Table 1. As typical with many pharmacy classes, 62% were female and 64% were from suburban settings. There was 46% of the sample that self-identified being Catholic. Being democrat or independent was reported by 79.3% of the respondents; 16.7% indicated being republican. Fifty-four percent of the respondents viewed themselves as socially liberal and 16.7% socially conservative. Fifty-six percent of the class had some HIV content prior to the class. Twenty percent and 14% of the class, respectively, self-reported they engaged in heavy alcohol use and unprotected sex often or very often. Only 2.7% of the sample indicated often to very often use of IV/recreational drugs.
Table 1.
Pharmacy Student Characteristics (N=150)a
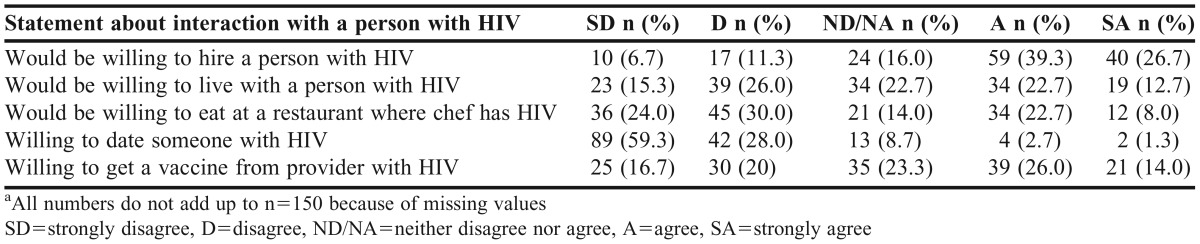
Tables 2 and 3 highlight general attitudes of respondents toward personal interaction with persons with HIV and what they thought other pharmacy and nursing students would say to each of the statements. A majority of the students responded strongly agreed or agreed to statements that HIV does not affect chances of being hired, is not a sign of personal failure, or does not affect productivity (latter two items not presented in tables). On average, students rated themselves as having more agreement (less negative attitudes) on these items than other pharmacy and nursing students (Table 3). Most students strongly disagreed or disagreed with statements about willingness to eat in a restaurant where the chef has HIV or dating a PLWHA.
Table 2.
General Attitudes Toward Personal Interactions with Persons with HIV (n=150)a
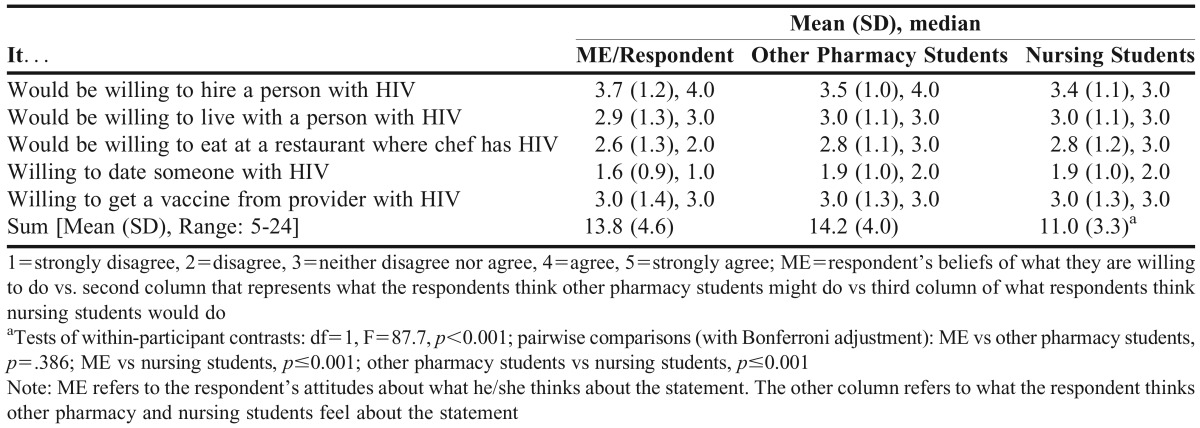
Table 3.
Comparative Attitudes Toward Personal Interactions with Persons with HIV (n=150)
The class was fairly mixed with 41.3% reporting discomfort with living with a person with HIV and 36.7% uncomfortable getting a vaccine from a provider with HIV, 35.4% and 40% respectively reporting comfort under these situations, and the remaining group was neutral. Respondents reported less agreement (more negative attitudes) than they thought other pharmacy and nursing students would have on items related to willingness to live with someone infected with HIV, eat at a restaurant where the chef has HIV, and date a person with HIV (Table 3). On average, respondents reported that they thought other pharmacy and nursing students would have similar agreement on the statement regarding willingness to receive a vaccine from a provider with HIV (Table 3). The repeated-measures analysis of variance of the overall sums indicate respondents thought their attitudes were similar to that of their peers but felt their attitudes and those of fellow pharmacy students were significantly higher than those of nursing students (p≤0.001).
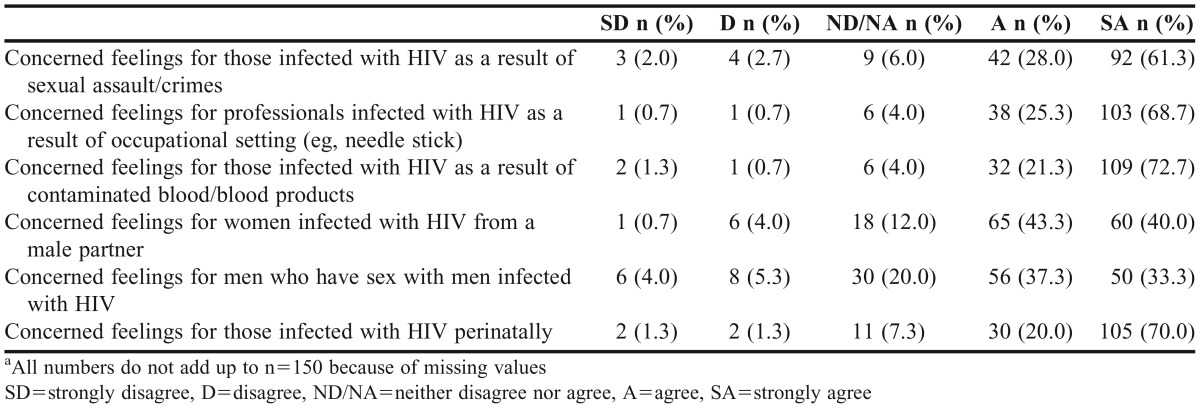
Table 4 shows the extent of empathy expressed by the pharmacy students toward persons with HIV. A majority (70.6-94.0%) of students reported on nearly every statement about agreeing that they had concerned feelings for different populations of HIV-infected persons. The greatest empathy expressed (94% agree/strongly agree) was for those infected with HIV because of contaminated blood/blood products, and the lowest number of students expressed empathy (70.6%) for men who have sex with men infected with HIV.
Table 4.
Empathic Orientation Towards Persons with HIV (n=150)a
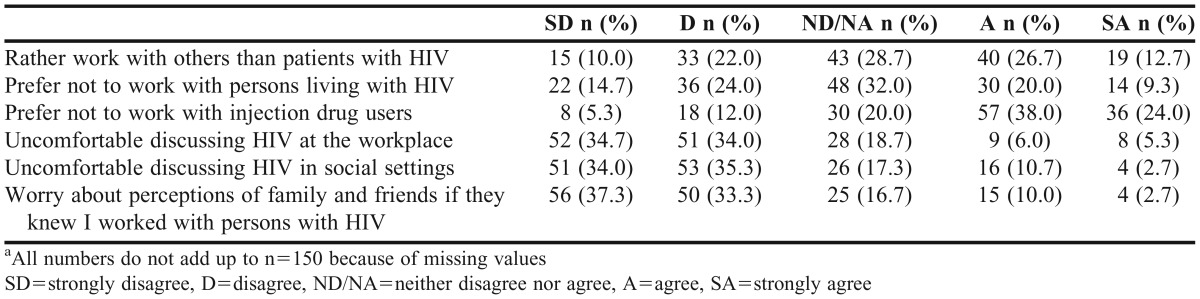
We further identified discomfort students have in being professionally engaged with PLWHA or discussing the topic of HIV (Table 5). Relatively similar number of students disagreed, agreed, or were neutral in their attitudes toward statements about preference working with others than those with HIV and working with persons living with HIV. Results indicate 62% of the students responded they agreed/strongly agreed about preferring not to work with injection drug users. Regarding discussing HIV at the workplace and social settings, 68.7% and 69.3% of the respondents reported disagreement, respectively. Data indicated that 70.6% reported disagreement of having any worry about family and friends knowing that they worked with persons with HIV.
Table 5.
Professional Interaction with Persons with HIV & other High Risk of HIV (n=150)a
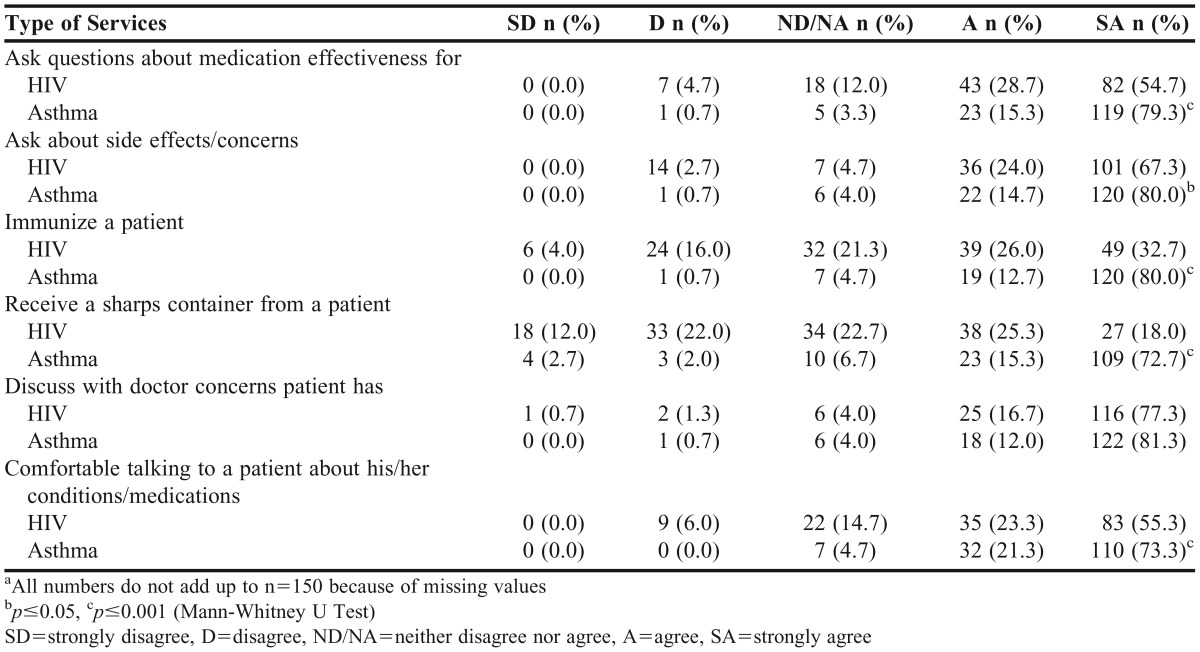
Although not presented in Table 5, a majority of the students responded with disagreement to two statements about being uncomfortable working with persons with HIV and being uncomfortable if a person with HIV approached them to the degree that they would back a way a little. The discomfort reflected in responses in Table 5 are also found in the results in Table 6 regarding student willingness to provide different services to patients with HIV than to patients with asthma. Students reported being significantly more willing to do tasks with patients with asthma than with those who have HIV (eg, ask questions about medication effectiveness or vaccinate, receive a sharps container from a patient, and talk to patients about their conditions/medications, p≤0.001). Students also reported being significantly more willing to counsel patients with asthma than those with HIV on medication side effects/concerns (p≤0.05). There was no significant difference between responses on willingness to talk to the doctor about concerns for HIV or asthma.
Table 6.
Willingness to Provide Services for Patients with HIV vs Patients with Asthma (n=150)a
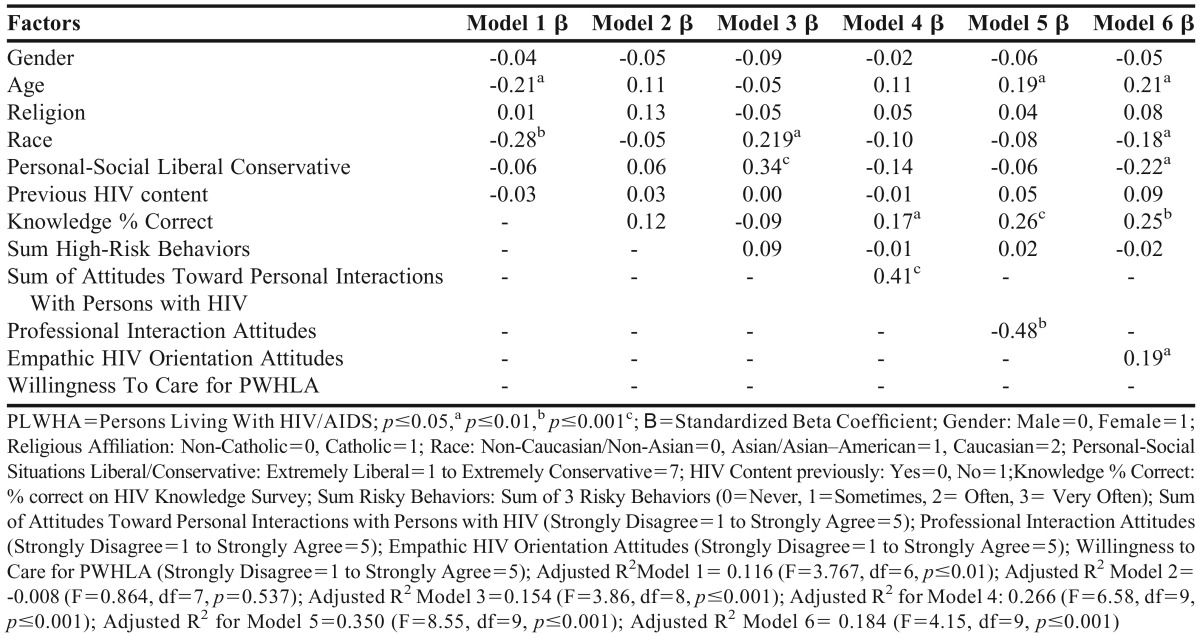
In Table 7, stepwise regressions are presented predicting student knowledge, attitudes, and intentions to provide services to PLWHA. We removed 15 cases where respondents did not specify their level of liberal/conservative attitudes of social situations. In the first model, age and race were the only significant factors influencing percent correct on HIV knowledge assessment (from third section of survey). Younger and minority students were significantly more likely to respond correctly to the 24 knowledge items than older and white students (p≤0.001). There were no significant factors in model 2 predicting extent of high-risk behaviors. Race and social orientation were significant factors predicting student attitudes toward professionally interacting with PLWHA (model 3).
Table 7.
Stepwise Regression Predicting Willingness to Provide Care to PLWHA (n=135)
Specifically, students were significantly more likely to have negative professional interaction attitudes if they were white (p≤0.05) and socially conservative (p≤0.001). Models 5-7 predict willingness to care for PLWHA. Because of multicollinearity concerns, we decided not to run attitudes toward personal interactions with persons with HIV, professional interaction attitudes, and empathic orientation into the same model. In model 4, we found having greater HIV knowledge (p≤0.05) and more positive attitudes toward personal interactions with persons with HIV (p≤0.001) were significantly related to willingness to care for PLWHA. Model 5 showed that being older (p≤0.05), having greater HIV knowledge, and having more positive professional interaction attitudes (p≤0.001) significantly influenced willingness to care for PLWHA.
When attitudes toward personal interactions with persons with HIV and professional interaction attitudes were removed from the model (model 6), being socially liberal and having a positive empathic orientation significantly influenced willingness to care for PLWHA (p≤0.05). Although not presented, we replaced social orientation with political orientation and found nearly identical regression results as in Table 7.
DISCUSSION
The present study investigated pharmacy student knowledge, attitudes, and willingness to engage in services for PLWHA. We found five important themes regarding pharmacy student comfort level communicating with patients with HIV/AIDS: (1) pharmacy students still had negative general attitudes toward HIV; (2) pharmacy students had positive attitudes about being concerned for those infected with HIV; (3) pharmacy students perceived themselves as having greater negative attitudes on specific aspects of interacting with persons with HIV than other pharmacy or nursing students; (4) students possessed significantly greater willingness to provide services to patients with asthma than those with HIV/AIDS; and (5) several background factors, HIV knowledge, empathic and attitudes toward professional interaction with PLWA were significant predictors of willingness to provide services to PLWHA.
A majority of students were favorable to the general concept that having HIV/AIDS is not associated with negative attributes about the person or his or her abilities to be worthy of work. However, there were mixed feelings about living with a person with HIV and getting a vaccine from a provider with HIV. Reported feelings were even more negative regarding willingness to eat in a restaurant with a chef who had HIV and dating a person with HIV. The negative attitude regarding dating a person with HIV most likely reflects a significant concern over risk for potential exposure to HIV. It is not entirely clear why students seemed comparatively more willing to get a vaccine from a provider with HIV than eat at a restaurant with a chef who had HIV. It is possible that students were overestimating the risk of exposure to HIV as a result of an injury in the kitchen, which reflects the need for more training to clarify the likelihood of HIV exposure under such circumstances.
More evidence suggesting students were misinformed about risk was seen in almost 70% of them reporting a person is at risk of HIV through saliva, sweat, tears, and urine, and 40% thinking HIV is transmitted through mosquitos. Some of our results almost 20 years later are similar to what Krupat et al found previously with regard to negative attitudes towards HIV/AIDS.8 In fact, for the item regarding willingness to eat at a restaurant with a chef who has HIV/AIDS, 68% of the pharmacy student population in Krupat et al’s study indicated disagreement, and 68% in our study indicated disagreement or neutral to this statement.
The second finding was that most pharmacy students in our study possessed positive attitudes toward persons with HIV. Krupat et al also reported many positive attitudes among pharmacy students.8 While a majority of students expressed empathy towards persons with HIV, it is interesting to note that the greatest empathy was for those persons with HIV who were exposed because of contaminated blood or blood products and the least empathy was expressed for men engaging in sex with men with HIV.
It is encouraging that most students had empathy for persons with HIV and showed significant capacity to engage sensitively with PLWHA. It is interesting to note that several manuscripts reported students from different professions having negative general attitudes but also positive specific attitudes toward caring for PLWHA.16,21-23 Thus, students in the health professions seem to have a generalized concern for PLWHA. However, it seems that empathy in itself does not mean a student will have fewer negative attitudes toward PLWHA and discomforts in personal contact with those who have HIV/AIDS.
One of the common criticisms of survey research of stigma is the degree to which individuals bias their answers in a way that appears socially desirable to researchers.24 Critics will state that this social desirability bias can overestimate the actual extent of positive attitudes. Krupat et al used the Crowne-Marlowe Social Desirability Scale to explore relationships between selected demographic factors and social desirability.8 We wanted to explore how allowing respondents to consider their attitudes relative to others might help reduce the social desirability bias. Rickles et al found this approach did better identify negative attitudes.20
Our third finding similarly revealed that students self-identified having more negative attitudes toward interacting personally with persons with HIV than they thought other pharmacy students and nursing students would. Pharmacy students felt, on average, they were less willing to live with someone with HIV, date someone with HIV, and eat at a restaurant where the chef has HIV than they perceived other pharmacy students and nursing students might be. When these attitudes of personal interaction with persons with HIV were summed as a scale, pharmacy students perceived themselves as having similar attitudes as other pharmacy students but significantly fewer negative attitudes than nursing students. While not conclusive yet, we find this approach of contextualizing one’s feelings with that of one’s peers useful in reducing potential social desirability bias.
As has been shown in past research with another stigmatized condition, mental illness, pharmacists expressed significantly greater willingness to provide services to those with a nonstigmatized condition like asthma than those with the stigmatized conditions.20,25 Our results support these findings. Thus, despite some positive general attitudes toward persons with HIV and empathy, pharmacy students were significantly more willing to provide services to those with asthma than to PLWHA. Pickles et al also found similar reluctance to provide care to persons with HIV among nursing students throughout several regions of the world.14 This data is concerning since it is the first pharmacy student study in the United States to indicate that negative attitudes toward persons with HIV are associated with decreased willingness to provide services to PLWHA. This finding could have a significant implication on the number of pharmacist providers available to care for PLWHA and subsequently influence the potential impact pharmacists can have in the treatment of PLWHA.
The fifth finding of our study highlights underlying factors that contribute to student willingness to provide services to PLWHA. Being older, a minority, being socially and politically liberal, and having greater HIV knowledge were factors associated with greater willingness to provide services to PLWHA. Older students may have more mature and accepting attitudes toward stigmatized conditions. This finding has also been reported in other studies involving nursing and pharmacy students.8,22 However, given that we didn’t have a wide distribution of age, these results should be interpreted with caution.
We were intrigued by the finding that minorities were more likely to be willing to provide services to PLHWA. Cultural variability was reported among nursing students from different countries and their negative attitudes toward those with PLWHA.14 Nationality differences in attitudes about HIV/AIDS was found in a pharmacy sample.8 Marginalization and the consequences of such stigma may be more prevalent in minority populations, which may predispose students to a greater willingness to care for similarly marginalized groups. More research is needed to further investigate the robustness of this finding and implications for education and practice.
While somewhat expected, we believe our study is the first to describe how social and political viewpoints are significantly related to the willingness to provide care to a patient population associated with stigma. Liberal social and political orientations were associated with more willingness to provide services to PLWHA. We often think professional socialization should help students move past their biases and be more open to caring for all types of patients. Our study suggests that such socialization may not have occurred for many students or that students had difficulty moving past their biases, which may impact their comfort in providing care to PLWHA.
Krupat et al did find a significant relationship between high homonegativism and attitudes toward AIDS.8 It is possible that our significant finding relating social and political orientation with willingness to provide services to PLWHA is mediated by prevailing social and political liberal/conservative viewpoints of homosexuality and societal norms. Thus, our findings may highlight that attitudes toward PLWHA may stem from earlier moral development about what constitutes model human behavior and may explain why such attitudes may be resistant to change.
We also anticipated that having more HIV knowledge contributed significantly to more willingness to provide services to PLWHA. Students knowledgeable about HIV/AIDS may be more comfortable in wanting to reach out to those that could benefit from the support. Seacat et al also found that dental students with less HIV knowledge were significantly more likely to have negative attitudes toward treatment.9 We found across models 4 to 6 that having positive attitudes and empathy toward HIV was associated with greater willingness to provide services to PLWHA. Valimaki et al found similar results of positive attitudes as a predictor of willingness to provide care among nursing students across a couple countries in their multi-national study.22
Based on the above findings, there seems to be an opportunity for educational interventions to help identify students at greatest risk for negative attitudes toward PLWHA and facilitate conversations about ways to mitigate the impact of those attitudes on willingness to provide services to PLWHA. A brief assessment survey could be administered early in the pharmacy curriculum asking items regarding age, race, social/political orientation, attitudes toward PLWHA and willingness to provide services to PLWHA, and brief questions assessing HIV knowledge. Faculty members could then use the aggregate descriptive data as a tipping point for conversations around why the negative attitudes exist and how to reconcile or resolve them so they might be more comfortable in providing services to PLWHA.
Some of the reconciliation of issues may require HIV education and correction of any misbeliefs and incorrect information. As discussed previously, educators may need to focus on clarifying risks of exposure to HIV under different conditions of personal contact. Other aspects may involve students hearing from PLWHA and hearing their stories of how pharmacists had an impact on their care. Our findings suggest less curricular time may need to be spent with empathy development since most pharmacy students seem to have adequate empathy for PLWHA.
As with most studies of this nature, there are a few limitations. First, we are unable to generalize our findings to other pharmacy students across the country. A national study might help determine the generalizability of our data to other pharmacy students throughout the country. It would be especially interesting to explore attitudes toward HIV and willingness to provide services to PLWHA in regions of the country where there are strong divides in social/political orientation. Second, while we addressed social desirability bias using a different methodological approach, it is likely social desirability still occurred with some items. We also want to explore what other pharmacy and nursing students actually think about the attitudes and not just what respondents perceive their attitudes might be. Third, we need to further validate the thematic organization of attitudes for reliability and other psychometric properties and how they compare to previously used attitude scales on the topic. Fourth, the present study was a cross-sectional study of a student population at one point in time. We are, therefore, unable to suggest causation of any of the predictor variables of willingness to provide services to PLWHA. Future prospective studies might attempt to sort out temporal effects of pharmacy student socialization and its relationship to attitude development toward PLWHA. Fifth, our study did not look at interaction effects between the study variables and their association with willingness to provide services to PLWHA. For example, there may be an interaction between race and social/political orientation that shows minorities have a more liberal social/political orientation and subsequently more willingness to provide services to PLWHA. An interaction might exist between knowledge and empathy. Such interactions should be explored in future research.
CONCLUSION
We examined different factors associated with pharmacy student willingness to provide services to persons living with HIV/AIDS. The results highlight areas pharmacy educators can consider as potential targets for classroom and experiential intervention. Such interventions are critical for pharmacy students to better care for patients with HIV/AIDS. More educational research can help determine the most effective ways to deliver such interventions and measure the impact of the efforts on the outcomes of patients with HIV.
REFERENCES
- 1.Centers for Disease Control and Prevention. Prevalence of Diagnosed and Undiagnosed HIV Infection — United States, 2008-2012. MMWR 2015; 64:657-662. [PMC free article] [PubMed]
- 2.Centers for Disease Control and Prevention. CDC fact sheet: HIV in the United States: the stages of care. 2014. http://www.cdc.gov/nchhstp/newsroom/docs/HIV-Stages-of-Care-Factsheet-508.pdf. Accessed 7 April 2016.
- 3.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24(6):518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- 4.Carey MP, Morrison-Beedy D, Johnson BT. The HIV-knowledge questionnaire: development and evaluation of a reliable, valid, and practical self-administered questionnaire. AIDS and Behavior. 1997;1(1):61–74. [Google Scholar]
- 5.Herek GM, Capitanio JP, Widaman KF. HIV-related stigma and knowledge in the United States: prevalence and trends, 1991-1999. Am J Public Health. 2002;92(3):371–377. doi: 10.2105/ajph.92.3.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carey MP, Schroder KE. Development and psychometric evaluation of the brief HIV knowledge questionnaire. AIDS Educ Prev. 2002;14(2):172–182. doi: 10.1521/aeap.14.2.172.23902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Society of Health-System Pharmacists. ASHP statement on the pharmacist’s role in the care of patients with HIV infection. Am J Health-Syst Pharm. 2003;60(19):1998–2003. doi: 10.1093/ajhp/60.19.1998. [DOI] [PubMed] [Google Scholar]
- 8.Krupat E, Weston CM, Messier MA. Attitudes towards AIDS among pharmacy students. Am J Pharm Educ. 1994;58(3):273–278. [Google Scholar]
- 9.Seacat JD, Litt MD, Daniels AS. Dental students treating patients living with HIV/AIDS: the influence of Attitudes and HIV Knowledge. J Dent Educ. 2009;73(4):437–444. [PubMed] [Google Scholar]
- 10.Nyberg CR, Patterson BY, Rasu R. Do pharmacy students have positive attitudes towards persons living with HIV/AIDS? A survey of pharmacy students to evaluate stigmatizing beliefs. Int J Pharm Educ and Pract. 2012;8(2):1–10. [Google Scholar]
- 11.Herek GM, Capitanio JP, Widaman KF. HIV-related stigma and knowledge in the United States: prevalence and trends, 1991-1999. Am J of Public Health. 2002;92(3):371–377. doi: 10.2105/ajph.92.3.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rutledge SE, Whyte J, Abell N, Brown KM, Cesnales NI. Measuring stigma among health care and social service providers: The HIV/AIDS provider stigma inventory. AIDS Patient Care STDs. 2011;25(11):673–682. doi: 10.1089/apc.2011.0008. [DOI] [PubMed] [Google Scholar]
- 13.Ivens D, Sabin C. Medical student attitudes toward HIV. Int J STD AIDS. 2006;17(8):513–516. doi: 10.1258/095646206778145631. [DOI] [PubMed] [Google Scholar]
- 14.Pickles D, King L, Belan I. Attitudes of nursing students towards caring for people with HIV/AIDS: thematic literature review. J Adv Nurs. 2009;65(11):2262–2273. doi: 10.1111/j.1365-2648.2009.05128.x. [DOI] [PubMed] [Google Scholar]
- 15.Talley A, Ritzdorf K, Muma RD. Attitudes of US physician assistants toward persons with HIV/AIDS. JAAPA. 2010;23(12):44–46,48. doi: 10.1097/01720610-201012000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Ivens D, Sabin C. Medical student attitudes towards HIV. Int J STD AIDS. 2006;17(8):513–516. doi: 10.1258/095646206778145631. [DOI] [PubMed] [Google Scholar]
- 17.Fishbein M, Ajzen I. Belief, Attitude, Intention, and Behavior: An Introduction to Theory and Research. Boston: Addison-Wesley; 1975. [Google Scholar]
- 18.Froman RD, Owen SV. Measuring attitudes toward persons with AIDS: the AAS-G as an alternate form of the AAS. Sch Ing Nurs Pract. 2001;15(2):161–174. discussion 175-177. [PubMed] [Google Scholar]
- 19.Froman RD, Owen SV. Further validation of the AIDS Attitude Scale. Res Nurs Health. 1997;20(2):161–167. doi: 10.1002/(sici)1098-240x(199704)20:2<161::aid-nur8>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 20.Rickles NM, Dube GL, McCarter A, Olshan JS. Relationship between attitudes toward mental illness and the provision of pharmacy services. J Am Pharm Assoc. 2010;50(6):704–713. doi: 10.1331/JAPhA.2010.09042. [DOI] [PubMed] [Google Scholar]
- 21.Pickles D, King L, Belan I. Undergraduate nursing student’s attitudes toward caring for people with HIV/AIDs. Nurse Educ Today. 2012;32(1):15–20. doi: 10.1016/j.nedt.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 22.Välimäki M, Makkonen P, Mockiene V, et al. Nursing and midwife students’ willingness to provide care to patients with HIV/AIDS-a comparative study in Finland, Estonia and Lithuania. Nurse Educ Today. 2010;30(7):674–679. doi: 10.1016/j.nedt.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 23.Choy KK, Rene TJ, Khan SA. Beliefs and attitudes of medical students from public and private universities in Malaysia towards individuals with HIV/AIDS. The Scientific World Journal. 2013;2013:Article 462826. http://dx.doi.org/10.1155/2013/462826. [DOI] [PMC free article] [PubMed]
- 24.Tan JA, Hall RJ. The effects of social desirability bias on applied measures of goal orientation. Personal Indiv Diff. 2005;38(8):1891–1902. [Google Scholar]
- 25.Phokeo V, Sproule B, Raman-Wilms L. Community pharmacists’ attitudes toward and professional interactions with users of psychiatric medication. Psychiatr Serv. 2004;55(12):1434–1436. doi: 10.1176/appi.ps.55.12.1434. [DOI] [PubMed] [Google Scholar]