Abstract
Objective. To assess and improve student adherence to hand hygiene indications using radio frequency identification (RFID) enabled hand hygiene stations and performance report cards.
Design. Students volunteered to wear RFID-enabled hospital employee nametags to monitor their adherence to hand-hygiene indications. After training in World Health Organization (WHO) hand hygiene methods and indications, student were instructed to treat the classroom as a patient care area. Report cards illustrating individual performance were distributed via e-mail to students at the middle and end of each 5-day observation period. Students were eligible for individual and team prizes consisting of Starbucks gift cards in $5 increments.
Assessment. A hand hygiene station with an RFID reader and dispensing sensor recorded the nametag nearest to the station at the time of use. Mean frequency of use per student was 5.41 (range: 2-10). Distance between the student’s seat and the dispenser was the only variable significantly associated with adherence. Student satisfaction with the system was assessed by a self-administered survey at the end of the study. Most students reported that the system increased their motivation to perform hand hygiene as indicated.
Conclusion. The RFID-enabled hand hygiene system and benchmarking reports with performance incentives was feasible, reliable, and affordable. Future studies should record video to monitor adherence to the WHO 8-step technique.
Keywords: Infection control, radio frequency identification, architectural intentional design, pharmacy practice, hand hygiene, benchmarking, pay for performance, World Health Organization
INTRODUCTION
Hand hygiene is the single most effective method for preventing transmission of health care associated infections, a top-10 cause of death in the United States.1,2 Yet, fewer than half of providers comply with hand-hygiene indications and methods.3 Pharmacy students on practice experiences may be exposed to pathogens in health care settings through touching patient bedrails, curtains and tables in health systems or handling credit cards and shaking hands with patients in community settings. Despite the relevance to pharmacy practice and education, to the best of our knowledge, few studies have shed light on instruction and assessment methods for formal hand hygiene instruction in colleges and schools of pharmacy.
Thirteen federal agencies, including the Food and Drug Administration (FDA), US Centers for Disease Control (CDC), and the National Institutes of Health (NIH), compose the Interagency Task Force on Antimicrobial Resistance. The task force endorses the World Health Organization (WHO) hand hygiene indications and methods for hand rubbing with alcohol-based products and has partnered with more than 2500 health care systems to implement these standards, including the use of “innovative and inexpensive wireless technologies to monitor healthcare worker movement and approximate hand hygiene adherence.”1
One of these technologies is radio frequency identification (RFID), which is increasingly used in health systems for a range of applications including tracking patients and resources.2 Concerns over hand hygiene adherence rates as low as 39% among health care providers has led to increased interest in expanding hand hygiene as a measurable outcome in accreditation standards of the Joint Commission.1,3 Several studies compared direct live observation to passive RFID systems for this purpose. Study designs varied widely, resulting in comparative efficacy rates of 52.4 to 100% compared to direct observation.4-7 This range may be attributable to study design factors, such as adherence to wearing the RFID tags and radio interference from other equipment.
Community settings such as private practices and community pharmacies are typically excluded from these efforts, although the prevalence of community-based nasal colonization by Staphylococcus aureus is estimated at 33% and methicillin-resistant Staphylococcus aureus (MRSA) at 1.5%.8 About 14 million outpatient visits per year are attributed to MRSA-related care and screening.9 These estimates are the most recent available but are now at least five years old and may therefore be low. Bacterial contamination of at least one large health system pharmacy robot is documented.10 Indoctrinating pharmacy students in the proper technique and potential impact of proper hand hygiene in all practice settings may help to reduce the transmission of harmful pathogens in all areas of pharmacy practice.
In previous work, we implemented and assessed new curricula for teaching pharmacy students WHO hand hygiene indications and hand rubbing using alcohol-based products.11 We later reinforced these lessons by having students screen themselves for MRSA nasal colonization and calculating the classroom prevalence of nasal colonization.12 Students reported greater motivation to perform hand hygiene, among other outcomes, after this exercise. In this paper, we describe our effort to monitor hand hygiene adherence in the semester following hand hygiene instruction and the MRSA self-screening exercise. Students use the same classroom for every class in the PharmD program, with instructors coming to them. We used the classroom as a proxy for a patient room. Students volunteered to wear hospital nametags that included RFID tracking labels and to use the alcohol-based product hand hygiene stations located at the doorways when entering and exiting the room. The stations included passive RFID monitoring and active dispensing monitoring and recorded the time of each student’s use of the dispenser.
DESIGN
We used the RFID system developed specifically for use in patient rooms in a teaching hospital in our area.7,13,14 A pilot study in an occupied patient room in this hospital over a one-month period demonstrated that this low-cost, automated monitoring system successfully tracked hand-hygiene adherence.7 The system relied on passive RFID tags (stickers) placed under the photo and name plate of ID tags. The stickers did not require recharging and were inexpensive. Each RFID sticker was unique and assigned to an individual. Two sensors on the hand hygiene station capture the date and time of each use and the RFID tags by distance from the dispenser in near continuous time. The data were automatically transferred via secure Internet connection to a server. We then correlated the RFID with the closest proximity to the station at the time of dispensing to identify the student.
Among the WHO indications for hand hygiene with alcohol-based products is moving between patient zones, for example leaving or entering a patient room. Students use the same classroom everyday and sit in the same seats for their entire first (P1) year, with instructors coming to the room to teach. The classroom became our proxy for a patient room, and students were expected to perform hand hygiene upon entry and exit. The spring P1 class schedule consists of 50-minute periods with 10-minute breaks. We used this schedule to predict the approximate time when students should be entering and leaving the room. The expected frequency of hand hygiene station use was twice per break between classes (once to leave and once to return), once in the morning and once at the end of the last class, or up to six times per day on Mondays and Fridays and eight times per day on Tuesdays, Wednesdays, and Thursdays.
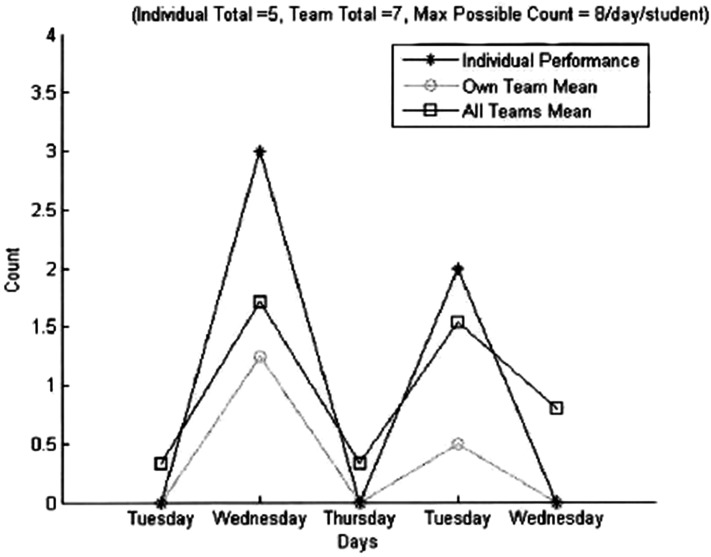
Student volunteers participated for five consecutive days at a time, wearing their assigned ID tags daily. Tags were allocated on a first-come, first-served basis during the study window until all students participated. Students received “report cards” consisting of graphs displaying their hand hygiene adherence next to that of the mean class performance (Figure 1).
Figure 1.
Sample Student Report Card.
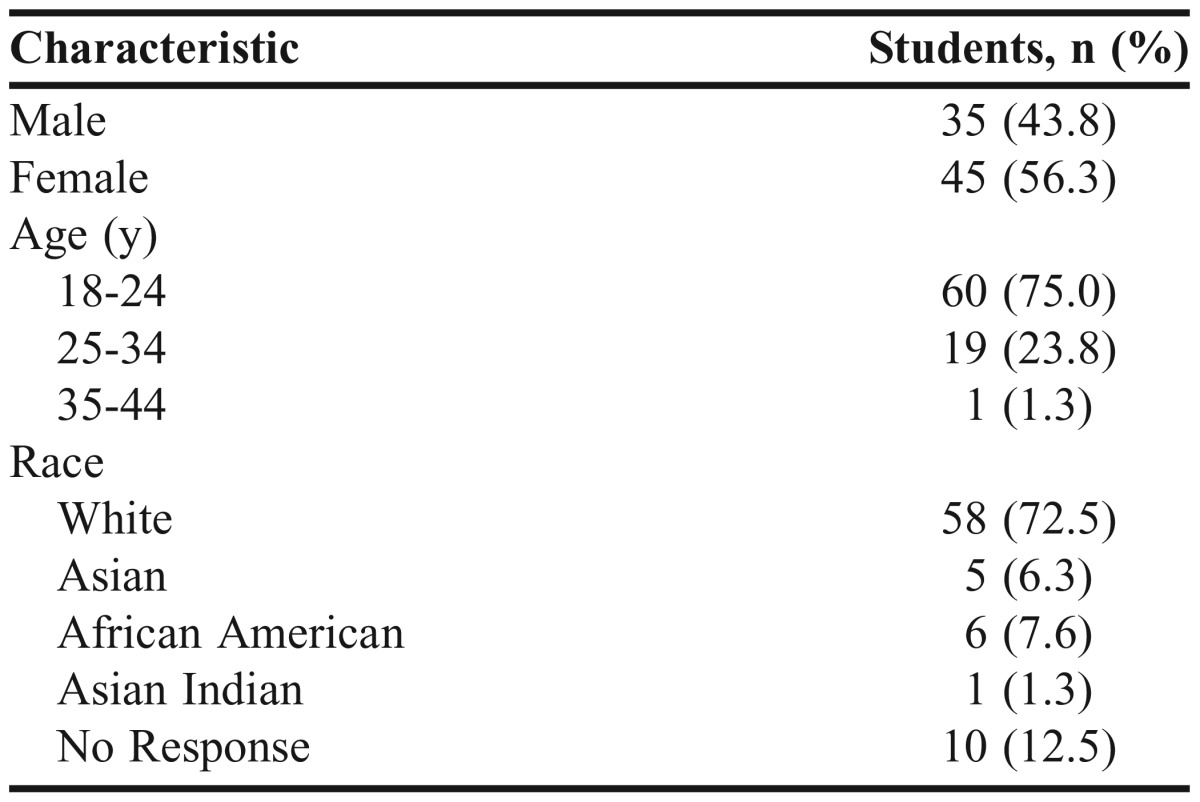
Subjects were volunteers from the PharmD class of 2016 who were then in their P1 year (Table 1). The class was largely white and under age 25. (The investigators were not responsible for any grading in this group of students during this semester, thereby ensuring unbiased treatment of volunteers and those who chose not to participate.) To encourage participation, all volunteers received $5 gift cards for the Starbucks on campus. Individual prizes of up to $50 were given to the top three performers in the class during the study period. Performance was based on the number of uses compared to the number of opportunities (before and after each class). This study was reviewed and approved by the St. John Fisher College Institutional Review Board.
Table 1.
Demographics of the Class of 2016 at Admission (N=80)
Ordinary least squares (OLS) regression was used to determine the association between gender and distance from seat to hand hygiene station, respectively. Wilcoxon rank sum test was used to determine significant changes in pre/postsurvey items. All analyses were performed using SPSS, v22 (IBM, Armonk, New York).
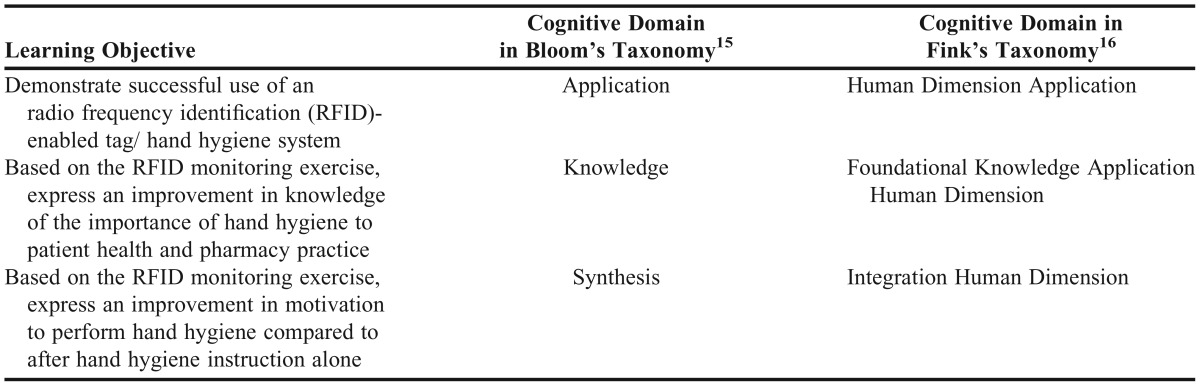
The first learning objective was for students to successfully demonstrate use of the system over a five consecutive day performance period. This objective falls under Application in Bloom’s15 and Fink’s16 Taxonomies (Table 2). Students experienced the system first-hand and observed their peers as they experienced the system (Fink’s human dimension).16 Based on the RFID monitoring exercise, students were also expected to express an improvement in knowledge of the importance of hand hygiene to patient health and pharmacy practice, and an improvement in their motivation to perform hand hygiene. Improvements in knowledge were expected to be a reaction to the formalization and integration of hand hygiene assessment into a classroom in a semester distant from the one in which the material was first introduced, thus reinforcing their knowledge that hand hygiene is considered important by the faculty members and school (Fink’s knowledge, foundational knowledge, human dimension, application).
Table 2.
Cognitive Domains of Learning Objectives According to Taxonomies of Learning
Similarly, improvements in motivation were expected to arise from students’ anticipation of being monitored during future classes or employment. The latter falls under synthesis in Bloom’s Taxonomy and integration in Fink’s Taxonomy, as students must consider facts, experiences, and expectations to develop that increased motivation. Fink’s human dimension is present in all three learning objectives as students learn by first-hand experience and observation about their own and their classmates’ experience with the RFID system and degree of adherence over time to hand hygiene indications. Overall, the exercise was designed to provide an opportunity for students to synthesize and reinforce previous training in hand hygiene indications, skills, and knowledge.11,12
To assess progress towards the learning outcomes, we measured the number and percentage of students who volunteered to participate in the RFID-monitored hand hygiene exercise, the number and percentage of students who participated for all five consecutive days, and the mean frequency of hand hygiene use per day. We also analyzed factors that we hypothesized may have affected adherence, such as distance from the student’s seat to the station. Finally, we assessed student self-reported changes in knowledge and motivation to perform hand hygiene at the end of the semester when the study ended. This survey was based on our previous work in surveying students about learning outcomes associated with educational quality improvement.17-20
EVALUATION AND ASSESSMENT
Sixty-three students (73.2%) volunteered for the study. Of those, 32 (50.8%) completed all five consecutive days, meaning that at least once on each day the RFID nametag assigned to them registered as the closest to the hand hygiene station simultaneously with a squeeze of the hand hygiene station. Mean frequency of hand hygiene station use per student over the 5-day study window was 5.41 (range: 2-10). We did not find a significant difference in mean rates of adherence before and after report cards were issued. However, the distance between the student’s typical seat in the classroom and the dispenser was significantly associated with hand hygiene adherence. The classroom was approximately 40 feet wide by 35 feet deep and had nine rows of seats with one door at the front and back. Mean distance from each seat to the closest dispenser was 21.3 feet (range: 2.5 to 42.2 feet). To determine if frequency of use was associated with the distance from the hand hygiene station, we used ordinary least squares regression with frequency of use the dependent variable and independent variables defined as gender and distance between the dispenser and the seat. Distance was inversely associated with adherence with a coefficient of -0.31 (p=0.02). Specifically, for every additional foot away from the station, the number of hand hygiene station uses dropped by 0.31. So, for every additional three feet from the station, the number of hand hygiene uses dropped by one. Male gender was not significantly associated with adherence (coefficient 1.83, p=0.16). Because of the limited number of RFID tags, students completed the study in different weeks and sometimes the weekend divided the week.
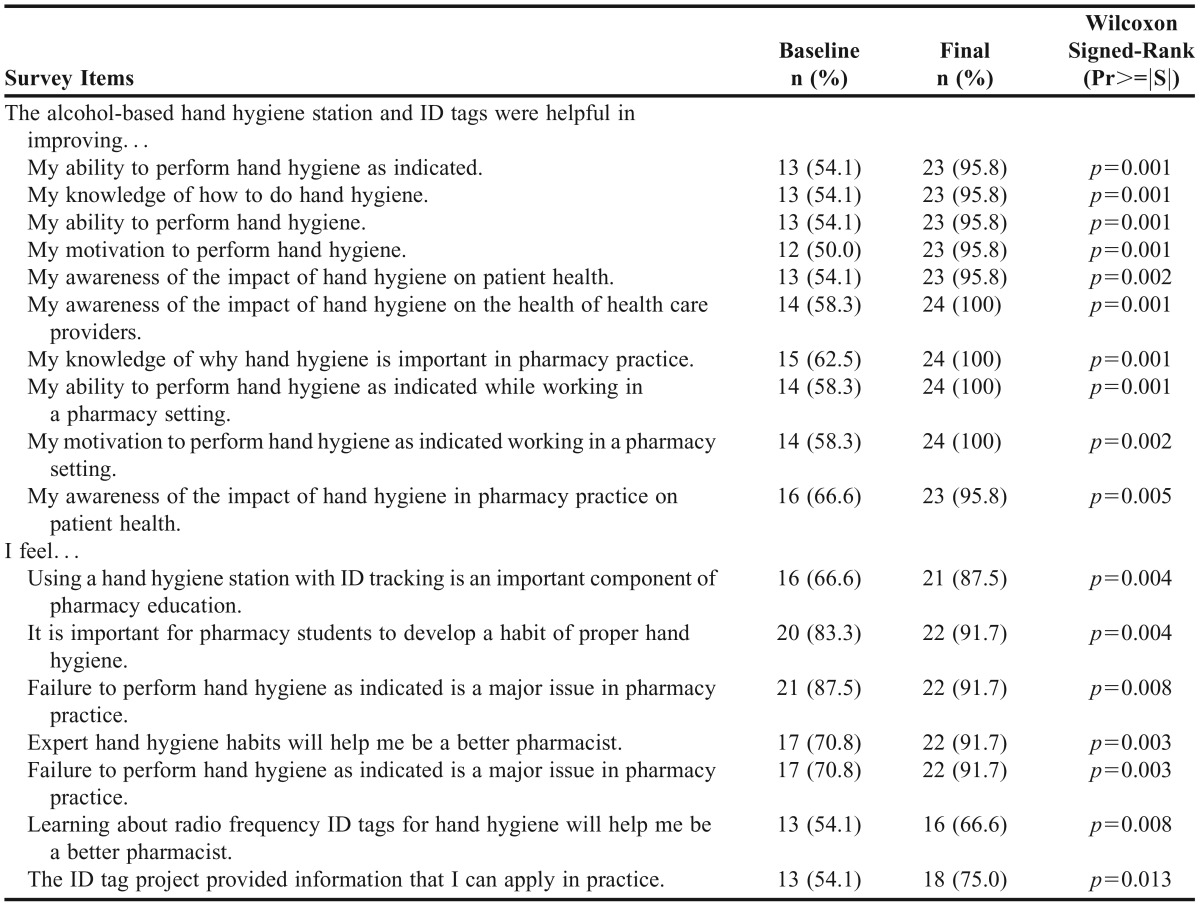
Of the 63 students who volunteered, 24 (38.1%) completed the pre/post survey of motivation, attitudes, and knowledge about hand hygiene following use of the RFID monitoring system. We summarize our results as dichotomous by defining a “strong positive response” as a response of “good” or “very good” on the survey. Otherwise, it was not a strong positive response.
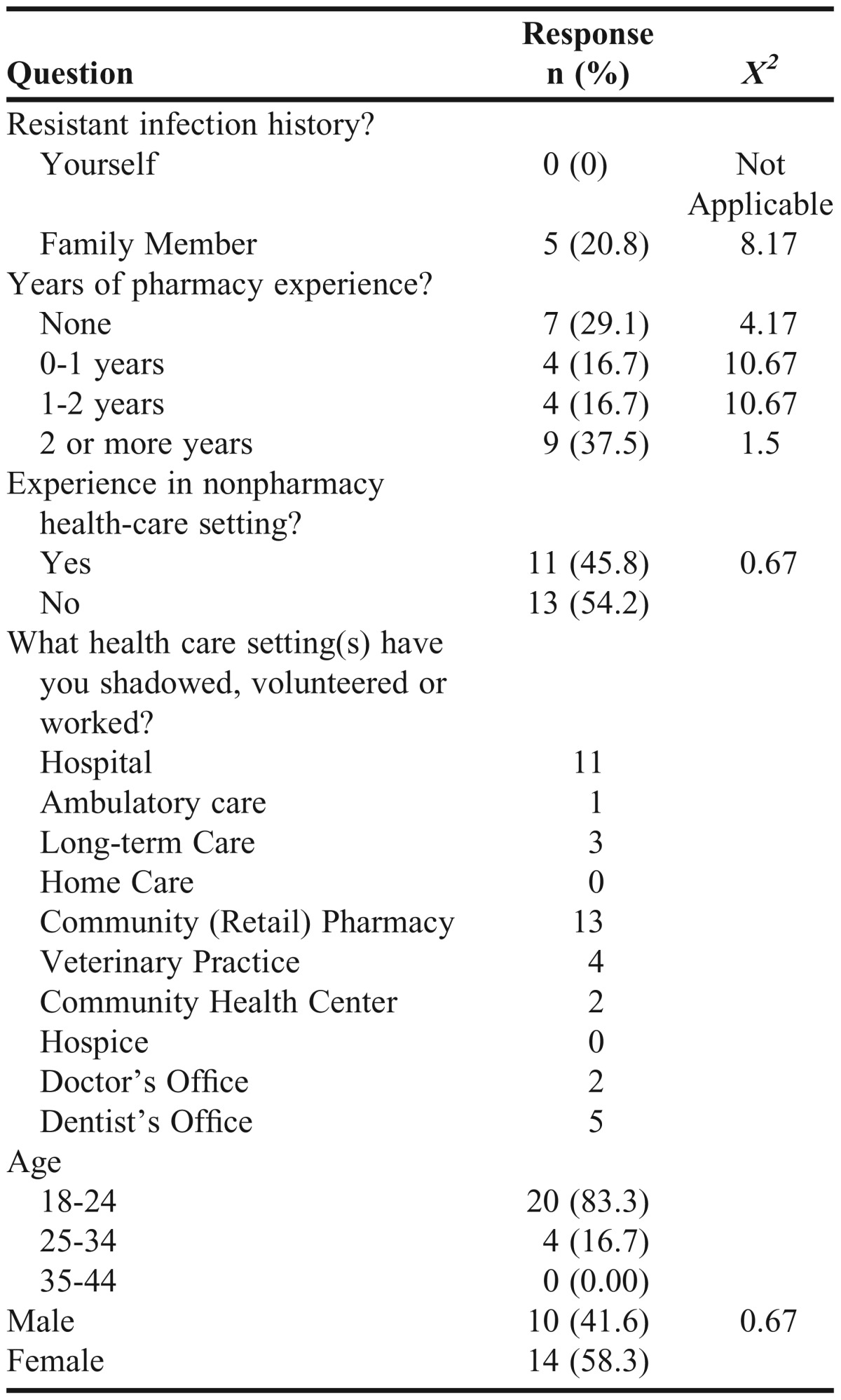
Overall, the majority of respondents demonstrated a confident positive response to the system’s effect on their motivation to perform hand hygiene; a confident response was considered a response of good or very good (Table 3). Students also reported feeling that the experience was not only beneficial to their education but also an important part of pharmacy practice. Of the students who completed the survey, many had hospital and/or community pharmacy experience prior to the trial (45.8% and 54.1%, respectively) and 62.5% had some previous pharmacy experience (Table 4).
Table 3.
Confident Positive Student Response about Attitudes and Motivation to perform Hand Hygiene Before and After Radio Frequency Identification (RFID) Monitoring of Hand Hygiene Adherence
Table 4.
Characteristics of Survey Respondents
DISCUSSION
To the best of our knowledge, our institution is the first to use RFID technology to support hand hygiene behaviors among pharmacy students. The design and implementation was feasible and student respondents demonstrated increased knowledge and motivation to perform hand hygiene at the completion of the study.
The 2013 National Quality Strategy to reduce hospital-acquired complications (including infections) by 40% by the end of 2014 drew increased attention to hand hygiene practice, yet we found little published information about hand hygiene practice and instruction in pharmacy education.14 The use of RFID technology is relatively new in pharmacy education; however, it is widely used as a method of tracking health care providers in a variety of ways, including hand hygiene. Boudjema and colleagues investigated the accuracy and feasibility of hand hygiene monitoring in patient care areas using RFID. They determined that the use of RFID was feasible for this purpose, with an accuracy rate of 98.1%, sensitivity of 90.6%, and specificity of 100%.4
In addition to monitoring hand hygiene, RFID was investigated for its use on monitoring personnel and equipment in the operating room by Kranzfelder and colleagues. Their system was able to determine the relative location on all personnel in the room (in patient care zone or not), and had between 60%-100% accuracy in determining the number of surgical sponges in use depending on their location.6 Although this may seem to have a small impact on pharmacists directly; RFID systems may be potentially implemented to determine the location of personnel (including pharmacists) in patient care areas to determine proximity in the event of a medical/medication error.6
Students volunteered to participate over a consecutive 5-day period, but performance varied widely and was generally below what we expected based on the WHO indications and the number of class periods. We did not account for student attendance in class, so it is possible that some of the demonstrated nonadherence to hand hygiene may actually be attributable to absence from class. The study did present a significant burden to students. Unlike our previous work on hand hygiene and MRSA screening, this study required students to remember their badge daily for five consecutive days (which may have spanned a weekend), be willing to display it, and use the dispensers. The hand hygiene system recorded uses for which there were no associated ID tags, suggesting that students who forgot their tags (or were not participating in that study period) were performing hand hygiene.
Another potential reason for apparent nonadherence may have been the lack of direct faculty oversight. Students mastered hand hygiene techniques in the fall semester as part of a required course. Yet, this study took place in the spring semester and outside of any course. Students have only 10 minutes between classes and we had only one station for about 70 students. Those farthest from the station demonstrated significantly lower rates of use, suggesting that the wait to use the machine at entry and exit inside of 10 minutes may have been a barrier to adherence.
The RFID system came with only 23 ID tags for our 63 volunteers, and so the dates of participation varied by student. It is possible that adherence may have varied systematically by study dates. Students were instructed on the importance of consistently wearing their RFID equipped name tags throughout the duration of the trial. Also first year students may have felt uncomfortable wearing the badges around other classes not participating in the study. This may have caused compliance to be lower then expected as the user could not be identified. Finally, measured adherence was dependent on the RFID tag being closest to the dispenser at the time of use. If a student forgot his or her tag and used the station, then the station would record the closest student with an RFID tag as having used the station.
In future studies, the RFID tag could either be placed on an object more consistently carried, such as cell phones or bags, or all students could be asked to wear nametags as a school-wide policy. Requiring students to wear ID badges early on in the curriculum would prepare them for the practice experiences and employment since the majority of locations require a ID badge of some sort to be worn at all times. Also, students may have had reservations about being passively tracked using the RFID system. Yet, in this classroom, permanent signage notes that audio and video recording may happen as part of the lecture capturing system. The impact of this reservation may have been minimized because of this constant recording in the classroom.
The addition of a camera and vapor sensor may be useful for observing WHO hand hygiene technique, which includes covering eight surfaces in a specific order in about 23 seconds. The addition of a camera may also help to determine the user of the system in situations where no signal was detected. Vapor sensors are able to detect the vapor that is released when the gel is rubbed in one’s hands. By determining the concentration of the vapor, the duration and intensity of the hand rubbing can be estimated.5
Implementation should be tested beyond the classroom in a variety of pharmacy settings. Pharmacists and technicians in community pharmacies often use hand-sanitizing gel after interacting with customers. To many, this is already incorporated in their workday. Community pharmacists are also accustomed to passive monitoring by video cameras and computer systems with password access that track pharmacy inventories and pharmacist actions. Therefore, implementation in pharmacy settings may be more readily accepted by pharmacists than by first year pharmacy students. Future research may improve upon our design by having all of the students complete the study in the same time period and by increasing the number of stations (and decreasing the distance to from seat to station).
SUMMARY
Overall, the RFID-enabled hand hygiene station and monitoring system was feasible in the classroom setting and students reported positive effects on their motivation to perform hand hygiene. However, because of the increased burden on students, participation was lower then expected.
ACKNOWLEDGMENTS
Nikhil Argade, MS, set up and monitored the data collection equipment. Lynn Fine, PhD, MPH, infection control specialist at the University of Rochester Medical Center in New York, provided insightful comments for the development of this paper.
The authors report no previous job titles while working on this paper and no conflicts of interest. This project was funded through a faculty development seed grant from the Wegmans School of Pharmacy, St. John Fisher College. The RFID system was originally developed with funding from the Rochester General Health System (RGH) & RIT for the grant, RFID Monitoring in Healthcare Environments ($20K) (2009) Gill R. Tsouri (PI and Edward Walsh, MD (PI).
REFERENCES
- 1.Interagency Task Force on Antimicrobial Resistance. Public Health Action Plan to Combat Antimicrobial Resistance. 2012 Action Plan. http://www.cdc.gov/drugresistance/actionplan/actionPlan.html. Appendix A: 36.
- 2.Pittet D, Allegranzi B, Sax H, Dharan S, Pessoa-Silva CL, Donaldson LJ. Evidence-based model for hand transmission during patient care and the role of improved practices. Lancet Infect Dis. 2006;6:641–652. doi: 10.1016/S1473-3099(06)70600-4. [DOI] [PubMed] [Google Scholar]
- 3.Interagency Task Force on Antimicrobial Resistance. A Public Health Action Plan to Combat Antimicrobial Resistance: 2012 Update. http://www.cdc.gov/drugresistance/actionplan/actionPlan.html. 2012:31.
- 4.Walther B, Wieler LH, Vincze S, Antão E-M, Brandenburg A, Stamm I. MRSA variant in companion animals. Emerg Infect Dis. 2012;18(12). http://dx.doi.org/10.3201/eid1812.120238. Accessed October 29, 2012.
- 5.Boudjema S, Dufour JC, Aladro AS, Desquerres I, Brouqui P. MediHandTrace®: a tool for measuring and understanding hand hygiene adherence. Clin Microbiol Infect. 2014;20(1):22–28. doi: 10.1111/1469-0691.12471. [DOI] [PubMed] [Google Scholar]
- 6.Pleteršek A, Sok M, Trontelj J. Monitoring, control and diagnostics using RFID infrastructure. J Med Syst. 2012;36(6):3733–3739. doi: 10.1007/s10916-012-9846-y. [DOI] [PubMed] [Google Scholar]
- 7.Kranzfelder M, Zywitza D, Jell T, et al. Real-time monitoring for detection of retained surgical sponges and team motion in the surgical operation room using radio-frequency-identification (RFID) technology: a practical evaluation. J Surg Res. 2012;175(2):191–198. doi: 10.1016/j.jss.2011.03.029. [DOI] [PubMed] [Google Scholar]
- 8.Johnson R, Tsouri GR, Walsh E. Continuous and automated measuring of compliance of hand hygiene procedures using finite state machines and RFID. IEEE Instrument Meas Mag. 2012;15(2):8–12. [Google Scholar]
- 9.Gorwitz RJ, Kruszon-Moran D, McAllister SK, et al. Changes in the prevalence of nasal colonization with staphylococcus aureus in the United States, 2001-2004. J Infect Dis. 2008;197(9):1226–1234. doi: 10.1086/533494. [DOI] [PubMed] [Google Scholar]
- 10.Cluck D, Williamson JC, Glasgo M, Diekema D, Sherertz R.Bacterial contamination of an automated pharmacy robot used for intravenous medication preparation Infect Control Hosp Epidemiol 2012. May335517–520. [DOI] [PubMed] [Google Scholar]
- 11.Hersch AL, Chambers HF, Maselli JH, Gonzales R. National trends in ambulatory visits and antibiotic prescribing for skin and soft-tissue infections. Arch Intern Med. 2008;168(14):1585–1591. doi: 10.1001/archinte.168.14.1585. [DOI] [PubMed] [Google Scholar]
- 12.Curran K, Lavigne JE.Teaching the World Health Organization’s how to handrub and 5 moments of hand hygiene in a healthcare delivery course at a New School of Pharmacy Curr Pharm Teach LearnIn press [Google Scholar]
- 13.Lum T, Picardo K, Westbay T, Barnello A, Fine L, Lavigne J. Student self-screening for methicillin-resistant staphylococcus aureus (MRSA) nasal colonization in hand hygiene education. Am J Pharm Educ. 2014;78(7):Article 138. doi: 10.5688/ajpe787138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The RIT-Rochester General Hospital Alliance. http://www.rit.edu/affiliate/rghs/. Accessed October 26, 2012.
- 15.Bloom BS, editor. Taxonomy of Educational Objectives. The Classification of Educational Goals. Handbook I: Cognitive Domain. New York, NY: McKay; 1956. [Google Scholar]
- 16.Fink LD. Creating Significant Learning Experiences. An Integrated Approach to Designing College Courses. San Francisco, CA: Jossey-Bass; 2003. [Google Scholar]
- 17.Gilligan AM, Myers J, Nash JD, et al. Educating pharmacists to improve quality (EPIQ) in colleges and schools of pharmacy. Am J Pharm Educ. 2012;76(6):Article 109. doi: 10.5688/ajpe766109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lavigne JE. Educating pharmacy students to improve quality in a new school of pharmacy. Currents in Pharmacy Teaching and Learning. Currents in Pharmacy Teaching and Learning. 2012;4:212-216. [Google Scholar]
- 19.Lavigne JE, Curran K. Teaching the World Health Organization's How to Handrub and 5 Moments of Hand Hygiene in a Healthcare Delivery course at a New School of Pharmacy. Currents in Pharmacy Teaching and Learning 7 (2015):207-213. [Google Scholar]
- 20.Lum T, Picardo K, Westbay T, Barnello A, Fine L, Lavigne JE. Student Self-Screening for Methicillin-Resistant Staphylococcus Aureus (MRSA) Nasal Colonization in Hand Hygiene Education.American Journal of Pharmaceutical Education Volume 78, Issue 7, 2014. [DOI] [PMC free article] [PubMed]
- 21.2013. Annual Progress Report to Congress: National Strategy for Quality Improvement in Health Care. Accessed.