Abstract
Background:
Nausea and vomiting are the worst and the most prevalent complications experienced by 70–80% of patients. Complementary treatments including therapeutic touch are cost-effective and low-risk, independent nursing interventions. Present research aims at investigating the effect of therapeutic touch on the intensity of acute chemotherapy-induced vomiting in these patients.
Materials and Methods:
As a single-blind, randomized clinical trial, the present research was carried out on women with breast cancer undergoing chemotherapy in Isfahan, Iran. The subjects were divided into three groups of control, placebo, and intervention. The intervention was applied to each patient once for 20 min on the aura (human energy field) focusing on solar chakra. Data gathering instruments included demographic questionnaire and acute vomiting intensity scale.
Results:
There was a significant difference among the three groups (and also after the intervention) (P < 0.0001). Paired comparisons among the groups using Mann–Whitney test showed that there was a statistically significant difference between the control group and the intervention group and between the control group and the placebo group (P < 0.0001). However, there was no significant difference between the placebo and intervention groups (P = 0.07).
Conclusions:
Therapeutic touch was effective in reducing vomiting in the intervention group. However, the patients experienced lower-intensity vomiting which may be because of presence of a therapist and probably the reduced anxiety related to an additional intervention. So, further research is recommended considering the placebo group and employing another person in addition to the therapist, who is not skilled for this technique.
Keywords: Breast cancer, chemotherapy, nursing, therapeutic touch, vomiting
INTRODUCTION
Cancer is among the diseases always associated with fear and suffering for humans. Human beings have long been trying to cope cancer, but statistics show that cancer is still affecting people of all age groups, especially those older than 65, and mostly men and those belonging to industrial communities.[1]
In Iran, cancer is the third leading cause of death by 12%, as reported by the World Health Organization in 2011.[1] It has been reported that of all types of cancers, breast cancer ranks first among women in the country.[2,3] Different studies agree that women of age one decade lower than that in other countries are being affected by this type of cancer in Iran.[4,5,6,7] According to the national report of cancer cases in 2009 (the latest available statistics), Isfahan with 39.67% is in the second rank after Tehran (43.36%) in the incidence of breast cancer. Breast cancer ranks second in incidence after acute lymphocytic leukemia (ALL) in this province.[8]
Various treatments are used to control and treat cancer, among which chemotherapy is one of the oldest and the most common treatments (besides radiotherapy, surgery, gene therapy, etc.).[7,9] Due to systemic complication of treatment through chemotherapy, multiple complications are observed in patients, among which nausea and vomiting are the worst, the most prevalent, and the most troublesome ones that are experienced by 70–80% of patients. So, the success of this treatment has been challenged to a large extent.[9,10] Recent studies have suggested that about 70% of the patients undergoing chemotherapy experience anticipatory, acute, and delayed vomiting even after taking antiemetic and anti-nausea drugs.[11,12] In addition, patients with cancer may postpone chemotherapy due to the fear of this undesired complication or avoid completing the treatment or be unable to complete the treatment and even be dissatisfied of the treatment followed.[9]
The symptom of vomiting generally increases with an increase in the number of chemotherapy sessions and most patients who had nausea and vomiting in the first treatment session will also experience these conditions up to 90.9% in the following sessions.[9] As one of the elements of the caring team, the role of nurses is preventing and alleviating the complications induced by chemotherapy (in the form of primary and secondary prevention) is important.[7]
Given the limited effectiveness and dangerous complications of common antiemetic and anti-nausea drugs, one of the fundamental and low-risk measures is using complementary and alternative medicine.[13] Nurses have long been using complementary and alternative medicine and have been among the pioneers in this area.[14] On the other hand, nursing is a holistic profession wherein nurses are expected to be familiar with non-pharmacological approaches in addition to common treatments and apply them to patients.[15]
Among the different complementary and alternative medicine methods, therapeutic touch enjoys a unique position,[16] as this method was primarily developed in 1972 by the nurses Dora Kunz and Dolores Krieger based on “energy transmission” through “laying on of hands.”[17] This treatment is cheap, applicable in any time and place, not invasive, has no special contraindication, and needs only healthy, strong, and experienced hands.[18,19,20,21] On the other hand, it is an independent nursing intervention which has been used for 25 years both in research and clinics.[19,22,23,24,25,26] According to Krieger, the primary effect of therapeutic touch is on autonomic nervous system, as it increases the parasympathetic power in the patient while reducing the activity of the sympathetic system.[24] Krieger describes these changes as a quick tranquillity response that is usually created in the first minutes due to activation of autonomic nervous system, and is characterized by reduced blood pressure, reduced respiratory rate, reduced pulse rate, and relax peripheral nervous system. This technique is a concentration treating art in which the therapist uses her hands by concentrating on consciousness as a focus for creating balance and coordination in mutual energy fields of the patient and the environment.[13]
Therapeutic touch has been proved to have positive effects on many symptoms and conditions, including reducing stress and anxiety, relieving different kinds of pain (acute, chronic pain with nervous origin) such as arthritis pain and tension headache, reducing or controlling cardiac arrhythmia, controlling the blood pressure, reducing fatigue, improving the behavioral symptoms in dementia, increasing blood hemoglobin, reducing intensity of carpal tunnel syndrome, improving stomach cramps, controlling fever, increasing the healing rate of wounds and fractures, improving the symptoms in patients with spinal damages (increasing concentration, performance level, and survival rate), enhancing the feeling of being good, decrease intensity of pre menstruation syndrome, improving the immune system, etc. In addition to these, nausea is another symptom for which therapeutic touch is effective.[18,19,22,24,27,28,29]
Literature review reveals that the effect of therapeutic touch on nausea has been generally proved, although nausea is of various types and is due to different causes such as pregnancy, increased intracranial pressure, motion sickness, chemotherapy, etc. On the other hand, no study was found to investigate the effect of therapeutic touch on vomiting, especially chemotherapy-induced vomiting. Therefore, the present research aimed at investigating the effect of therapeutic touch on acute chemotherapy-induced vomiting, based on a pre-determined and specific program. This study was carried out in order to determine the effect of therapeutic touch program on the intensity of chemotherapy-induced vomiting in women treated for breast cancer.
MATERIALS AND METHODS
This research is a single-blind clinical trial registered in IRCT 2013080311136N2 consisting of three groups of control, placebo, and intervention. The intended intervention was applying therapeutic touch to women with breast cancer undergoing chemotherapy and following an identical medication regimen [Cyclophosphamide (Endoxan), Epirubicin (Pharmorubicin), Dexamethasone (Decadron), Plasil (Metoclopramide) and Kytril (Granisetron), and Emend (Aprepitant); the first two drugs are chemotherapy drugs causing nausea and vomiting and the other three drugs are those used to reduce nausea and vomiting as chemotherapy complications].
Data collection instruments in this research included demographic questionnaire and the four-item vomiting intensity scale used in acute phase of vomiting in the form of a checklist. This checklist represents the intensity of vomiting in a scale from 0 to 3, with 0 representing no vomiting or retching, 1 indicating successive retching with or without vomiting less than 3 times, 2 indicating successive retching with or without vomiting for 4–5 times, and 3 representing uncontrollable vomiting (successive vomiting more than 5 times). Validity and reliability of this instrument was considered as acceptable in the study by Bakhshi (validity has been reported as 0.86).[2] Both the questionnaire and the checklist were filled before the intervention and the patients were asked to fill the checklist again 24 h after the intervention and also after chemotherapy.
The research was carried out in a specialized center for cancer affiliated to one of the educational hospitals of Isfahan University of Medical Sciences and the subjects were patients with breast cancer with or without metastasis (except metastasis to central nervous and digestive systems, as it leads to nausea and vomiting) within the age range of 18–55 years. The inclusion criteria were not being simultaneously under radiotherapy and chemotherapy, and following an identical chemotherapy medication regimen (as different chemotherapy drugs cause different intensities of nausea and vomiting). The exclusion criteria were unwillingness to continue in the study and not returning the checklists in the next chemotherapy session. The sample size was determined to be 36 for each group and 108 as the total number, based on Altman's nomogram and using standard deviation of a similar study[7] and considering a statistical power of 0.7. Sampling was performed as nonprobability purposive sampling with random assignment of the subjects into the three groups of control, intervention, and placebo. Random assignment into these three groups was done as follows. Numbers from 1 to 108 were written on cards and the cards were kept in a spherical container; the numbers taken out of the container were then assigned to the three groups of control, intervention, and placebo, respectively, so that each patient's group was determined in advance based on their order of registering in the study. For example, number 4 was put in the intervention group; therefore, the fourth woman registering to participate in the study was assigned to the intervention group. The placebo group was used to control the effect of inculcation. The study was single blind, so that the subjects in both intervention and placebo groups were unaware whether intervention was really performed on them or the therapist was only moving her hands around their body without transmitting energy.
In order perform therapeutic touch, the researcher first started to learn different steps of therapeutic touch technique theoretically (philosophy of therapeutic touch, seven layers of energy, and body chakras) and practically (the practical process is explained below) simultaneously under the supervision of an instructor. Practical exercises included several meditation sessions (concentration and yoga exercises on a daily basis), giving energy to plant seed and making comparisons with the control seed, scanning and estimating the thickness of the first layer of the body in different parts of a healthy person, and finally scanning and estimating the thickness of the first layer of the body in different parts of a patient, which lasted 1 year. The exercises were performed in a private and individual way by the therapist in the university and the researcher repeated them several times on seed, healthy person, and the patient after that. After finishing the exercise sessions and confirmation by the instructor of the researcher's ability to accurately apply the technique, she started her intervention in the hospital on the patients. The researcher was in the hospital every morning from 8 a.m. to 2 p.m. and started sampling from the patients who met the inclusion criteria of the study, introducing herself and the content of the study and its purpose, obtaining their informed written consent forms (emphasizing that their information will be confidential), and explaining the way they should fill the vomiting scale. The intervention of therapeutic touch was performed in four steps of preparation and concentration (the patient and the therapist), studying and scanning, intervention, and assessment. In the control group, the patients received routine treatment and filled the questionnaire and checklist in their beds. In the intervention group, the patient was taken to a quiet room (along with her relative if they were willing to be present in the room). The patient was asked to sit on a chair, close her eyes, and start taking deep breaths slowly without thinking of anything. After concentration ( first step of the intervention), the researcher started investigating the first layer of energy of the body (as even before the physical problems are being physically revealed, they express themselves in this layer and if not treated, they show as physical symptoms) using her hands at a distance of 12–15 cm from the body from top to bottom, with more emphasis on solar plexus chakra (lower than heart chakra) due to the effect of this chakra on the digestive system, especially stomach[22](second step of the intervention), balancing any disturbances in energy (which are expressed in the form of decrease or increase in the thickness of first layer in this area/changes in sensation in the therapist hands, including feeling coldness/heat/stabbing) through sweeping or energy transmission from the environment (third step of the intervention), and again investigating energy modification and balance (fourth step of the intervention). These steps lasted 15–20 min. These steps were performed once before chemotherapy and vomiting scales were filled 24 h after chemotherapy by the patients; so, the vomiting intensity was once measured immediately before the intervention (and chemotherapy) and again 24 h after chemotherapy (acute vomiting). In the placebo group, the researcher moved her hands around the body maintaining more distance and not considering the order of energy therapy from top to down or vice versa, pretending an act of performing therapeutic touch. Then, the patients were given the vomiting intensity checklists to fill and return them in the next chemotherapy session. In case of not returning the checklists, the researcher called the patients to follow the matter; so, there was no sample loss. Sampling lasted 5 months in total.
Ethical consideration
This research project was approved by the local ethics committee of Tarbiat Modares University and written informed consent forms were obtained from all participants. After intervention, if the control group participants were willing to have TT, they were provided.
Statistical analysis
The data were analyzed through SPSS v. 16 using Kruskal–Wallis test.
RESULTS
One hundred and eight women with breast cancer with or without metastasis (except metastasis to central nervous and digestive systems) participated in the present study and were divided into three groups of control (n = 36), intervention (n = 36), and placebo (n = 36). Based on the demographic information, the three groups were homogenous and had no significant statistical difference (P > 0.05). Demographic characteristics of the patients are presented in Table 1.
Table 1.
Distribution of demographic variables in the three groups of control, intervention, and placebo
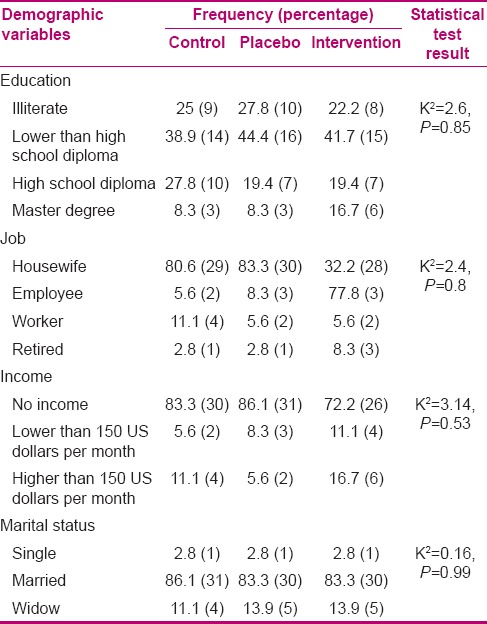
The average age of the patients was 49.7 years with a standard deviation of 9.2 (most of the patients were in the age range of 40–49 years). Most of the subjects in all three groups were married, housewives, without independent income, and with education levels lower than high school. Most of them had no background of digestive diseases and had not been affected by metastasis [Table 1].
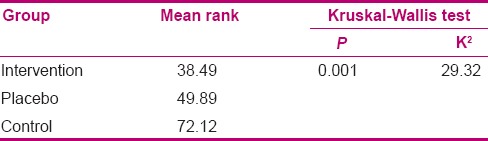
Kruskal–Wallis test also showed that 24 h after chemotherapy (after the intervention), intensity of vomiting among the three groups was different (P < 0.001). Paired comparisons of the groups using Mann–Whitney test showed that there was a statistically significant difference between the control group and the intervention group and between the control group and the placebo group (P < 0.0001). However, there was no significant difference between the placebo group and the intervention group (P = 0.07). That is, while the intervention in the intervention group was significant compared to the control group, it was as well significant in the placebo [Table 2].
Table 2.
Vomiting intensity in breast cancer patients among the three groups of control, intervention, and placebo at 24 h after chemotherapy
Findings related to the intervention group showed that the intervention duration (the whole process) was on an average 21.38 min with a standard deviation of 6.04. Duration of intervention in patients with a digestive disease background was more than in those with no digestive problem background (25 min vs 20 min). On the other hand, the time for performing the intervention in patients with a history of background of digestive diseases was more than in those with no history of background of digestive diseases (30 min vs 20 min). Also, there was a need for repeated intervention after the last step of therapeutic touch (assessment) in 69.4% of cases.
DISCUSSION
This research aimed at determining the effect of therapeutic touch program on chemotherapy-induced vomiting in women treated for breast cancer. The results of the study showed that therapeutic touch significantly reduced the intensity of vomiting compared to the control group, while the placebo group had no significant difference with the intervention group (P = 0.07), that is, the intervention applied to the placebo group (pretending to perform therapeutic touch) reduced the intensity of vomiting after chemotherapy (in acute phase) as well. However, in the study of Matory et al. on the effect of therapeutic touch on the intensity of vomiting in women treated for breast cancer, it was found that the intervention was significantly effective in the intervention group compared to the control and placebo groups (P < 0.05).[30] Also, it was revealed in the study of Matory et al. that therapeutic touch was effective on the number of occurrences and duration of vomiting in the intervention group compared to both control and placebo groups.[31] In the study of Basak et al. on the effect of massage therapy on the number of occurrences of vomiting, the results showed that massage therapy reduced vomiting as a complementary treatment, but this reduction was not statistically significant (P > 0.05).[32] In their study, Molassiotis et al. suggested the positive effect of acupressure on reducing the intensity of chemotherapy-induced vomiting and nausea.[33] In 2010, Ghanbari et al. did not find ginger effective on reducing the number of occurrences of vomiting;[34] as the number of occurrences of vomiting was used for determining the intensity of vomiting in this study, the same conclusion can be made about the intensity of vomiting. In 2000, Marchioro et al. found hypnosis effective for chemotherapy-induced conditional vomiting.[35]
Limitation of the present study was not investigating the delayed phase of the intervention as it was not possible to repeat the intervention for delayed phase because the patients were referring to the hospital from far-away cities and it was impossible for most of them to have another appointment. Fatigue and weakness of these patients was another reason for this. To prevent sample loss in this phase as a result of bias, the intervention and its investigation were ignored. In addition to the mentioned limitation, the intervention was done only once as it was time consuming, and also, increasing number of interventions would not be tolerated by the patients and their relatives. However, increasing the number of interventions can produce more effects of the intervention, which should be considered in further studies.
CONCLUSION
The results of the study showed that therapeutic touch as a complementary treatment was effective on chemotherapy-induced vomiting. However, as this technique was effective in the placebo group as well, no definite conclusion can be made on its effectiveness and further studies with larger sample size and with other cancers, considering the placebo group (for controlling inculcation or indoctrination) and delayed phase are recommended.
Financial support and sponsorship
This article is part of MS nursing thesis and supported by Tarbiat Modares University (Tehran, Iran).
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This article was extracted from the thesis for accomplishing the requirements in nursing (M.S.) in Tarbiat Modares University with registration number 2013080311136 in the Center of Clinical Trial registration. The researchers express their gratitude to all subjects who participated in the study and the personnel and managers of the chemotherapy ward of the hospital for their kind cooperation.
REFERENCES
- 1.Smeltzer SC, Hinke JL, Cheere KH, Kluwer W. Brunner and Sudarth's Textbook of Medical-Surgical Nursing. 12th ed. New York: Lippincott Williams & Wilkins; 2010. pp. 337, 1460–700. [Google Scholar]
- 2.Bakhshi M. Effect of Progressive Muscle Relaxation on Acute and Delayed Emesis in Cancer Patients under Chemotherapy in Institute Cancer of Tehran at 2001. Tehran: Tarbiat Modares University; 2002. pp. 10–28. [Google Scholar]
- 3.Gajizade SE, Najme ET. Investigation breast cancer risk factors by branch grapies. Iran J Nurs Vision. 2010;77:61–8. [Google Scholar]
- 4.Shahkhodabandeh S, Piri Z, Biglo MH, Asasdi M. Breast cancer in Iran: Iranian scientists approach to breast cancer researchers in Medline database. Iranian J Breast Dis. 2009;2:49–59. [Google Scholar]
- 5.Norizadeh R, Bakhtari Aghdam F, Sahebi L. Invstigation insight health behavioure of women about cancer and screening at community health services. J Breast Dis. 2010;3:43–51. [Google Scholar]
- 6.Salimi S, Karimian N, Sheikhan Z, Alavi H. Performance of screening test and effecting factors on women in community health service in Ardebil 2010. J Ardabil Univ Med Sci. 2010;10:310–8. [Google Scholar]
- 7.Ebrahimi SM. Investigation Effect of Ginger on Nausea and Vomiting of Cancer Patients Receiving Chemotherapy. Tehran: Tarbiat Modares University; 2010. p. 12. [Google Scholar]
- 8.The Cancer Organ. Tehran: Center of Disease Control and Preventation; 2009. National Report of Cancer Records. Ministry of Health and Medical Education. Non-contagious Deputy Cancer Organ; p. 12, 40. [Google Scholar]
- 9.Matory P. Breast cancer: Clinical Guideline for Nurses and Nursing Students. Tehran: Heidari Publication; 2014. pp. 5–15. [Google Scholar]
- 10.Sontakke S, Thawani V, Naik MS. Ginger as an antiemetic in nausea and vomiting induced by chemotherapy: A randomized, cross-over, double blind study. Indian J Pharmacol. 2003;35:32–6. [Google Scholar]
- 11.Movafaghi Z. Teherapeutic touch and its role in nursing. N J Mashad Faculty Nurs Midwifery. 2005;17:66–9. [Google Scholar]
- 12.Zolfaghari M. Compariance of Progressive Muscle Relaxation and Therapeutic Touch on Anxiety, Vital Science and Dysrhythmia under Heart Cathethrism. Tehran: Tehran Medical Scientific University; 1999. p. 43. [Google Scholar]
- 13.Hickok JT, Roscoe JA, Morrow GR, Ryan JL. A phase II/III randomized, placebo-controlled, double-blind clinical trial of ginger (Zingiber officinale) for nausea caused by chemotherapy for cancer: A currently accruing URCC CCOP Cancer Control Study. Support Cancer Ther. 2007;4:247–50. doi: 10.3816/SCT.2007.n.022. [DOI] [PubMed] [Google Scholar]
- 14.Adams J. An exploratory study of complementary and alternative medicine in hospital midwifery: Models of care and professional struggle. Complement Ther Clin Pract practice. 2006;12:40–7. doi: 10.1016/j.ctcp.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 15.Cherry B., Jr . Contemporary Nursing. 5th ed. Texas: Mosby; 2001. pp. 36–52. [Google Scholar]
- 16.Ranvanipour M. Master Thesis. Tehran, Iran: Tarbiat Modares University; 1999. Investigation Effect of Therapeutic Touch Before IV Injection on Anxiety Level of School Age in Medical Centers of Boshehr 1998-99; pp. 24–54. [Google Scholar]
- 17.Freeman L. Mosbys Complementary and Alternative Medicine: A Research Base Aproach. Mosby: Elsevier; 2001. p. 456. [Google Scholar]
- 18.DiNucci EM. Energy healing: A complementary treatment for orthopaedic and other conditions. Orthop Nurs. 2005;24:259–69. doi: 10.1097/00006416-200507000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Rankin D. The Nurse Handbook of Complementary Therapies. Sussex: Bailliere Tindall; 2001. pp. 267–72. [Google Scholar]
- 20.Carpenter DS, Ambrose M, Holmes N. Professional Guide to Complementary and Alternative Therapy. Spring House. 2002:475–7. [Google Scholar]
- 21.McCabe PN., Jr Complementary Therapy in Nursing and Midwifery: From Vision to Practice. Ausmed. 2001:497–504. [Google Scholar]
- 22.Zare Z. Investigation Effect of Therapeutic Touch on Level of Anxiety before Coronary Artery Bypass Graft in Shiraz Namazi Hospital 2005-06. Isfahan, Iran: Isfahan Medical Science University; 2006. pp. 4–38. [Google Scholar]
- 23.Brown D, Edwards H. Lewis Medical Surgical Nursing Assessment and Management of Clinical Problems. 3rd ed. New Zealand: Elsevier Health Science; 2013. p. 232. [Google Scholar]
- 24.Aghebati N. Investigation Effect of Herapeutic Touch on Pain Intensity and Psychologic Symptom (Anxiety, Depression, Fear) in Cancer Patients Hospitalized. Tehran, Iran: Tarbiat Modares University; 2005. pp. 25–35. [Google Scholar]
- 25.Gleeson M, Timmins F. A review of the use and clinical effectiveness of touch as a nursing intervention. Clin Eff Nurs. 2005;9:69–77. [Google Scholar]
- 26.Coakley AB, Barron AM. Energy therapies in oncology nursing. Semin Oncol Nurs. 2012;28:55–63. doi: 10.1016/j.soncn.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 27.Carpenito LJ. Nursing Diagnosis: Application to Clinical Practice. 12th ed. Philadelphia: Lippincott Williams & Wilkins; 2008. p. 242. [Google Scholar]
- 28.Authers Go. Nurse's Handbook of Alternative and Complementary Therapies. 8th ed. Lippincott Williams & Wilkins; 2003. p. 58. [Google Scholar]
- 29.Wanchai A, Armer JM, Stewart BR. Complementary and alternative medicine use among women with breast cancer: A systematic review. Clin J Oncol Nurs. 2010;14:E45–55. doi: 10.1188/10.CJON.E45-E55. [DOI] [PubMed] [Google Scholar]
- 30.Matory P, Vanaki Z, Zare Z, Mehrzad V, Dehghan M. Investigation of the effects of therapeutic touch on intensity of anticipatory and acute induced-nausea in breast cancer women undergoing chemotherapy in Isfahan. J Complementary Ther. 2013;3:594–85. [Google Scholar]
- 31.Matory P, Vanaki Z, Zare Z, Mehrzad V, Dehghan M. Investigation effects of therapeutic touch plan on acute chemotherapy induced-nausea in breast cancer women in Isfahan 2012-13. J Res Development Nursing Midwifery. 2013;3:56–61. [Google Scholar]
- 32.Basak S, Dasht Bozorgi B, Hosseini S, Latifi S. Investigation effect of massage therapy on vomiting induced chemotherapy in breast cancer patients. J Breast Cancer Dis. 2010;3:14–8. [Google Scholar]
- 33.Molassiotis A, Russell W, Hughes J, Breckons M, Lloyd-Williams M, Richardson J, et al. The effectiveness of acupressure for the control and management of chemotherapy-related acute and delayed nausea: A randomized controlled trial. J Pain Symptom Manage. 2014;47:12–25. doi: 10.1016/j.jpainsymman.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 34.Ghanbari A, Montazeri A, Niknami M, Atrkar Z, Sobhani A, Najafi B. Effect of using ginger beside routine treatment on nausea and vomiting of cancer patients in Razi hospital dependent to Medical scientific university of Rasht. Ardebil J. 2011;10:352–61. [Google Scholar]
- 35.Marchioro G, Azzarello G, Viviani F, Barbato F, Pavanetto M, Rosetti F, et al. Hypnosis in the treatment of anticipatory nausea and vomiting in patients receiving cancer chemotherapy. Oncology. 2000;59:100–4. doi: 10.1159/000012144. [DOI] [PubMed] [Google Scholar]


