Abstract
Background:
Migraine is a primary headache disorder that affects the neurovascular system. Recent studies have shown that migraine patients with general obesity have higher characteristics of migraine attacks compared with normal weight patients, but data on central obesity are scarce. This study was done to assess the relationship between central obesity and the characteristics of migraine attacks in migraine patients.
Materials and Methods:
This cross-sectional study was conducted on 129 migraine patients (28 men and 101 women), aged 15–67 years, in Isfahan, Iran. Anthropometric measurements such as waist circumference (WC), hip circumference (HC), waist–hip ratio (WHR) and waist–height ratio (WHtR), as well as characteristics of migraine attacks such as severity, frequency, duration, and headache diary result (HDR) was determined for each participant. Linear regression was used to examine the association between anthropometric measurements and characteristics of migraine attacks. P value less than 0.05 was considered significant.
Results:
WC, WHR, and WHtR were positively associated with the severity (P-value: WC: 0.002, WHR: 0.002, WHtR: 0.001) and frequency (P-value: WC: 0.006, WHR: 0.01, WHtR: 0.002) of migraine attacks. Moreover, we found a significant association between WC (P = 0.001), WHR (P = 0.004), and WHtR (P < 0.001) with HDR. No significant relationship was observed between central obesity indicators and duration of migraine attacks.
Conclusions:
Central obesity indicators were positively associated with the severity and frequency of migraine attacks as well as HDR, but not with duration of attacks. Based on our findings, it can be concluded that weight loss may decrease the characteristics of migraine attacks.
Keywords: Abdominal obesity, central obesity, duration, frequency, headache diary result, migraine, severity, waist circumference
INTRODUCTION
Migraine is a neurovascular disorder that affects 10–20% of the general population worldwide.[1] Migraine patients experience severe, recurrent headache[2] that is accompanied with some symptoms such as nausea, vomiting, photophobia, phonophobia, neck pain, and muscle tension.[3,4] Migraine headaches are one-sided and pulsating that last usually 2–3 h.[5] Other related symptoms are alteration in sensory sensitivity, autonomic dysfunction, dysregulation of mood, and focal neurological symptoms.[6] Migraine mostly occurs in middle age and is more prevalent in women than men.[7,8] One of four migraine patients has visual disturbances in every attack that is known as aura.[9] Migraine is prevalent in around 14.7% of the European population[10] and affects 3% of men and 10% of women in Asian countries.[5] In Iran, several studies have shown a prevalence of 9.5%, which is considered to be high.[11]
The etiology of migraine is still unknown, but several theories about the cause of this disease have been proposed. These include genetic defects and environmental factors.[12,13] Among environmental factors, alcohol and coffee consumption,[14] smoking, low physical activity,[15] nutritional deficiencies,[16] and psychological difficulties[17] are known to worsen the clinical symptoms of migraine. It seems that obesity might also contribute to migraine etiology.[18,19] Obesity is a growing problem in the world, especially in Iran.[20,21] Several studies have shown a significant positive association between obesity and migraine incidence.[18,19] In addition, some evidences reported that obese migraine patients have higher severity and frequency of migraine attacks compared with normal weight patients.[22,23] Earlier studies have mainly considered the effects of general obesity on the characteristics of migraine attacks and the effects of central obesity has been paid less attention. One study showed that central obesity increases the frequency of migraine attacks but does not have any effect on the severity and duration of migraine.[24] If the mentioned relation is confirmed, medical team members can use it as a proper approach in managing migraine attacks and nursing care processes.
Given the few studies in this regard and the high prevalence of migraine and central obesity in the Iranian population, this study was performed to assess the relationship between central obesity and characteristics of migraine attacks among migraine patients in Isfahan, Iran.
MATERIALS AND METHODS
This cross-sectional study was performed on migraine patients who referred to Khorshid and Emam Mosa Sadr clinics in Isfahan city, Iran. Patients with migraine for a long time and a 1-year history of severe, recurrent attacks (at least one attack per month) were selected. Migraine diagnosis was carried out by a qualified clinical neurologist using the International Headache Society (IHS) criteria.[9] Patients with tension-type headache and chronic pain were excluded from the study. One hundred and thirty-six migraine patients meeting the inclusion criteria were selected. They were 31 men and 105 women with the age range of 15–67 years. We collected data on age, medical history [chronic diseases such as diabetes mellitus (DM), cardiovascular diseases (CVD), hypertension (HTN), and kidney disease], anti-migraine drug consumption (corticosteroids and analgesics drugs), anthropometric measurements, and family history of migraine from each patient. Informed consent was obtained from all subjects.
Migraine assessment
We determined characteristics of migraine attacks such as headache severity, frequency, duration, and headache diary result (HDR) for each participant. Visual analog scale (VAS) was used for measurement of severity.[25] The number of migraine attacks per month was considered as frequency. Moreover, HDR was defined as the frequency of attack × duration of headache.[25,26]
Anthropometric measurements
Waist circumference (WC), waist–hip ratio (WHR), and waist–height ratio (WHtR) as the indicators of central obesity were determined for each participant. WC was measured at the midpoint between the top of the iliac crest and the last floating rib in the midaxillary line using an inelastic tape. Moreover, hip circumference (HC) was measured at the widest part of the buttocks or hip. Height was taken by tape measure without shoes. WHR was determined as WC (cm) divided by HC (cm). We also calculated WHtR by the formula: WC/height. Central obesity was defined based on WHO classification: WC more than 102 and 88 cm in men and women, respectively, was defined as abdominal obesity.
Statistical analysis
Quantitative and qualitative variables are presented as mean (SD) and number (percent), respectively. We evaluated the differences between men and women with respect to age, anthropometric measurements, and characteristics of migraine attacks using independent sample t-test. To assess the proportion of chronic diseases, intake of anti-migraine drugs for a long term, and family history of migraine between both genders, we used Chi-square test. We examined the association between anthropometric measurements with the severity, frequency, duration of migraine attacks, as well as HDR by multiple linear regression tests in crude and adjusted models. In the first model, we adjusted age (continuous) as a confounding variable which can affect the mentioned associations. In the second model, we additionally adjusted intake of anti-migraine drugs for a long term and history of chronic diseases including CVD, HTN, DM type 2, and kidney disorders. Further adjustment was done for family history of migraine in the final model. All analyses were conducted using SPSS statistical software (version 18.0; SPSS, Inc., Chicago, IL, USA). P value less than 0.05 was considered significant.
Ethical considerations
The study was approved by the Ethics Committee of Isfahan University of Medical Sciences, Isfahan, Iran.
RESULTS
In this study, out of the 136 migraine patients, we had incomplete data on 7 patients which were not considered for statistical analysis. Of the remaining 129 participants, 28 were men and 101 were women with a mean age of 34.00 ± 11.11 and 34.07 ± 10.68 years, respectively. Central obesity was prevalent in 7.1% of men and 23.8% of women.
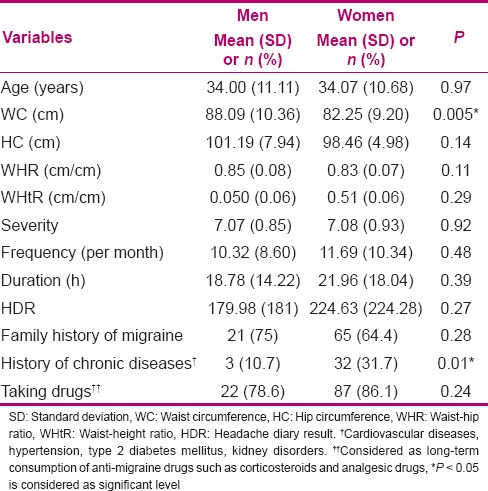
Differences between men and women in age, central obesity indicators, and characteristics of migraine attacks are shown in Table 1. Men had higher WC compared to women. Prevalence of chronic disorders such as CVD, HTN, DM (type 2), and kidney diseases was higher in women than men. There was no difference between men and women in age, HC, WHR, WHtR, features of migraine attacks, family history of migraine, and intake of anti-migraine drugs for a long term.
Table 1.
Anthropometric measurements and characteristics of migraine attacks in men and women
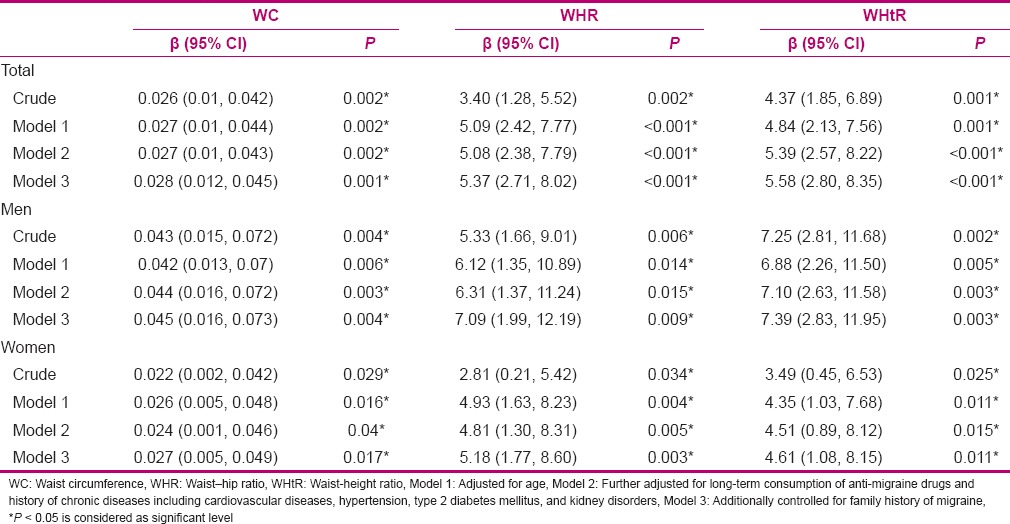
Results of multiple linear regression test for the association between central obesity indicators and severity of migraine attacks are presented in Table 2. There was a significant positive association between WC, WHR, and WHtR with the severity of migraine attacks. This relationship remained significant even after adjustment for potential confounding variables such as age, history of chronic disorders, taking anti-migraine drugs for a long term, and family history of migraine. We observed that one unit increase in WC, WHR, and WHtR was accompanied with 0.028, 5.36, and 5.70 units increase in the severity of migraine attacks. Sex-stratified analysis revealed similar association both in men and women.
Table 2.
Multiple linear regression analysis for the association between central obesity indicators and severity of migraine attacks
The association between central obesity indicators and the frequency of migraine attacks is presented in Table 3. High WC, WHR, and WHtR values were significantly associated with high frequency of migraine attacks. No change was observed in this association after controlling the potential confounders, such that one unit increase in WC, WHR, and WHtR was associated with 0.211, 31.81, and 36 units increase in the frequency of attacks. Moreover, such relationship was found among men for WC and WHtR, but it was not significant for WHR; however, adjustment for potential confounders made it significant. Among women, a significant positive association was found between WC, WHR, and WHtR with the frequency of attacks; however, adjustment for potential confounding variables attenuated this relationship.
Table 3.
Multiple linear regression analysis for the association between central obesity indicators and frequency of migraine attacks
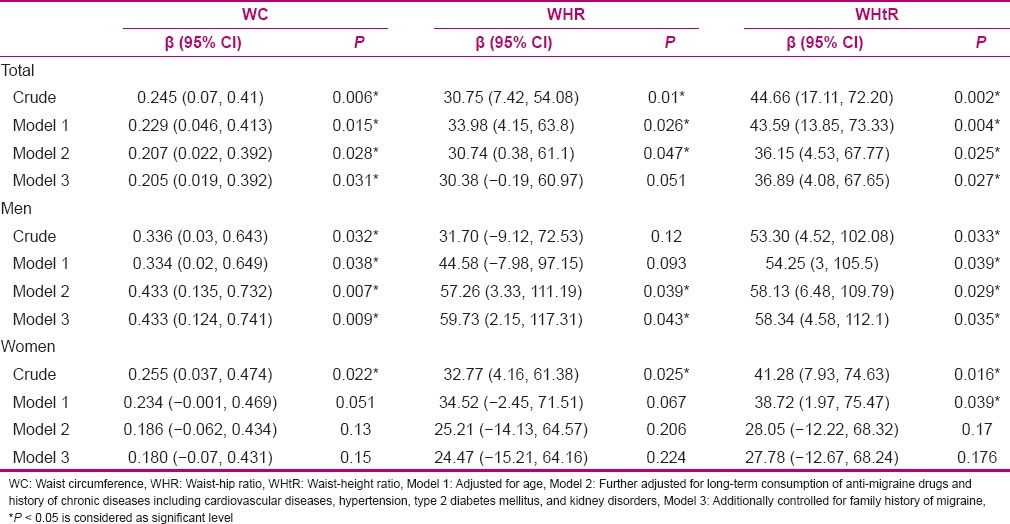
Multiple linear regression analyses revealed no significant association between central obesity indicators and duration of migraine attacks either in crude or adjusted models. In addition, WC, WHR, and WHtR were not significantly associated with duration of attacks either in men or women [Table 4].
Table 4.
Multiple linear regression analysis for the association between central obesity indicators and frequency of migraine attacks
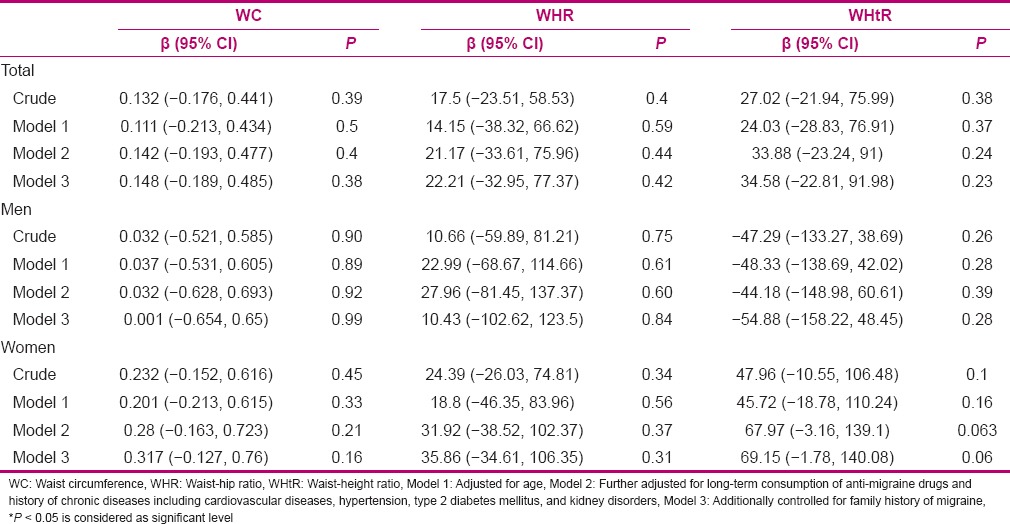
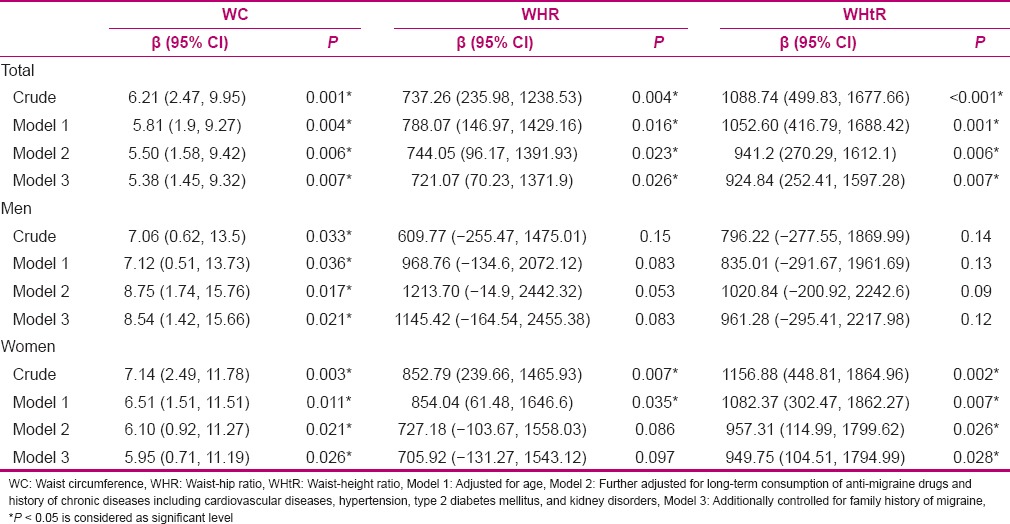
The relationship between central obesity indicators and HDR is shown in Table 5. There was a significant positive association between central obesity indicators and HDR. This relationship was significant even after adjustment for potential confounders. Sex-stratified analysis revealed a significant positive relationship between WC and HDR in both sexes. Among men, no significant association was found between WHR and WHtR with HDR, but after adjustment for potential confounders, this relationship was marginally significant for WHR. Among women, there was a significant positive association between WHR and WHtR with HDR; however, controlling for potential confounding variables attenuated this relationship for WHR.
Table 5.
Multiple linear regression analysis for the association between central obesity indicators and HDR
DISCUSSION
In this study, we found a significant positive association between central obesity indicators with the severity and frequency of migraine attacks in the total population and in both sexes, separately. Moreover, high WC, WHR, and WHtR values were associated with high HDR. Sex-stratified analysis revealed a significant positive association between WC and HDR in both sexes. No significant relationship was observed between central obesity indicators and duration of migraine attacks, and this association remained non-significant in sex-stratified analysis also. This is one of the few studies that examined the association between central obesity and characteristics of migraine attacks.
Evidences have indicated a positive association between obesity and incidence of migraine.[18,19] In addition, some studies have demonstrated that obesity may worsen the features of migraine attacks.[22,23] Recent studies have mainly assessed the association between general obesity and characteristics of migraine attacks, and data about central obesity are scarce. Also, the studies conducted have just focused on WC[24] and there is no evidence on the association between WHR and WHtR with the features of migraine attacks. In addition, to our knowledge, no studies have examined the association between obesity and HDR and the present study is the first one to examine this relationship. We found a significant positive association between WC, WHR, and WHtR with the severity of migraine attacks, frequency of migraine attacks, and HDR, but not with duration of migraine attacks. In addition, among men, the association between WHR and WHtR with HDR was non-significant or partially significant and it can be due to the less number of men with central obesity.
In line with our findings, Rossoni de Oliveira et al. reported that migraine patients with high WC have higher frequency of migraine attacks, compared to patients with normal WC. Moreover, they reported no significant association between WC with the severity and duration of migraine attacks.[24] In another similar study, both kinds of obesity were associated with migraine symptoms in patients between 22 and 55 years of age.[27] In a clinical trial, Verrotti et al. assessed the effect of weight loss on the characteristics of migraine attacks. Weight loss decreased abdominal fat as well as the severity and frequency of migraine attacks.[28] Winter et al. reported that women with body mass index (BMI) ≥35 had increased incidence of active migraine, compared to women with BMI ≤ 23. Moreover, obese migraine women had higher attacks frequency, photophobia, and phonophobia than non-obese migraine women.[29] In contrast, some evidences showed no significant association between obesity and characteristics of migraine attacks.[19] In addition, Mattsson showed no significant relationship between obesity and the incidence of migraine. The author reported that obesity cannot affect the migraine symptoms.[30] It should be mentioned that several factors including genetic polymorphisms, diet, physical activity, and health status can affect characteristics of migraine attacks;[12,14] therefore, different results obtained in previous studies may be due to changes in these effective factors.
The main mechanism explaining the association between obesity and characteristics of migraine attacks is unknown. There are some hypotheses about this association. First, several inflammatory factors that are secreted from adipose tissue, especially in visceral adipose tissue, are involved in the pathogenesis of migraine and may affect the symptoms of migraine.[31] Calcitonin-related peptide and some interleukins as inflammatory factors can increase the frequency of migraine attacks and central nervous system sensitivity. Second, adipose tissue secretes some hormones that affect the functioning of hypothalamus as an important center for regulation of body weight, food intake, and initiation of migraine attacks.[32] Therefore, alteration in hypothalamus function due to obesity status may change the incidence of migraine attacks. It seems that controlling body weight can be a useful strategy in reducing migraine attacks and its outcomes, and nursing care can use that in this regard.
This study has several limitations. The present study was performed in a cross-sectional design and we cannot confer a causal link between central obesity and characteristics of migraine attacks. Moreover, sample size of our study was small and more studies with a larger number of participants are required to confirm the associations. Although we controlled some potential confounders, further adjustment made for other confounding variables such as dietary pattern, physical activity, and psychological factors will be effective in reaching an independent association between central obesity and characteristics of migraine attacks. However, strength of this study is that for the first time, the relationship between WHR and WHtR with migraine attack features such as its severity and frequency has been assessed. In addition, we evaluated the relationship between central obesity and characteristics of migraine attacks in Iran for the first time.
CONCLUSION
From the findings of the present study, it can be concluded that obesity, especially abdominal obesity, aggravates the migraine symptoms and the severity and frequency of migraine attacks. Therefore, we suggest prevention of obesity, especially abdominal obesity, in migraine patients and weight loss need to be taken by obese migraine patients.
Financial support and sponsorship
Food Security Research Center and Department of Community Nutrition, School of Nutrition and Food Sciences, Isfahan University of Medical Sciences, Isfahan, Iran. This study was extracted from an MSc dissertation which was approved by the School of Nutrition and Food Sciences, Isfahan University of Medical Sciences, code 392363.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We thank all the participants of the study. It should be mentioned that this study has been taken from an MSc dissertation of Food Security Research Center and Department of Community Nutrition, School of Nutrition and Food Sciences, Isfahan University of Medical Sciences, Isfahan, Iran. This study was approved by the School of Nutrition and Food Sciences, Isfahan University of Medical Sciences, code 392363.
REFERENCES
- 1.Lipton RB, Bigal ME. The epidemiology of migraine. Am J Med. 2005;118(Suppl 1):3–10S. doi: 10.1016/j.amjmed.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 2.Goadsby PJ, Lipton RB, Ferrari MD. Migraine-current understanding and treatment. N Engl J Med. 2002;346:257–70. doi: 10.1056/NEJMra010917. [DOI] [PubMed] [Google Scholar]
- 3.Unalp A, Dirik E, Kurul S. Prevalence and clinical findings of migraine and tension-type headache in adolescents. Pediatr Int. 2007;49:943–9. doi: 10.1111/j.1442-200X.2007.02484.x. [DOI] [PubMed] [Google Scholar]
- 4.Steiner TJ, Paemeleire K, Jensen R, Valade D, Savi L, Lainez MJ, et al. European Headache Federation; Lifting The Burden: The Global Campaign to Reduce the Burden of Headache Worldwide; World Health Organization. European principles of management of common headache disorders in primary care. J Headache Pain. 2007;8(Suppl 1):S3–47. doi: 10.1007/s10194-007-0366-y. [DOI] [PubMed] [Google Scholar]
- 5.Sadeghi O, Askari G, Maghsoudi Z, Nasiri M, Khorvash F. Migraine and risk of stroke: Review of current evidence. Jundishapur J Chronic Dis Care. 2014;3:e21707. [Google Scholar]
- 6.Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Headache Classification Committee of the International Headache Society. Cephalalgia. 1988;8(Suppl 7):1–96. [PubMed] [Google Scholar]
- 7.Stewart WF, Lipton RB, Celentano DD, Reed ML. Prevalence of migraine headache in the United States. Relation to age, income, race, and other sociodemographic factors. JAMA. 1992;267:64–9. [PubMed] [Google Scholar]
- 8.Haut SR, Bigal ME, Lipton RB. Chronic disorders with episodic manifestations: Focus on epilepsy and migraine. Lancet Neurol. 2006;5:148–57. doi: 10.1016/S1474-4422(06)70348-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004;24(Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 10.Stovner LJ, Andree C. Prevalence of headache in Europe: A review for the Eurolight project. J Headache Pain. 2010;11:289–99. doi: 10.1007/s10194-010-0217-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zarei S, Bigizadeh S, Pourahmadi M, Ghobadifar MA. Chronic pain and its determinants: A population-based study in southern Iran. Korean J Pain. 2012;25:245–53. doi: 10.3344/kjp.2012.25.4.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kowa H, Yasui K, Takeshima T, Urakami K, Sakai F, Nakashima K. The homozygous C677T mutation in the methylenetetrahydrofolate reductase gene is a genetic risk factor for migraine. Am J Med Genet. 2000;96:762–4. doi: 10.1002/1096-8628(20001204)96:6<762::aid-ajmg12>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 13.Mauskop A. Nonmedication, alternative, and complementary treatments for migraine. Continuum (Minneap Minn) 2012;18:796–806. doi: 10.1212/01.CON.0000418643.24408.40. [DOI] [PubMed] [Google Scholar]
- 14.Panconesi A. Alcohol and migraine: Trigger factor, consumption, mechanisms. A review. J Headache Pain. 2008;9:19–27. doi: 10.1007/s10194-008-0006-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spierings EL, Ranke AH, Honkoop PC. Precipitating and aggravating factors of migraine versus tension-type headache. Headache. 2001;41:554–8. doi: 10.1046/j.1526-4610.2001.041006554.x. [DOI] [PubMed] [Google Scholar]
- 16.Camboim Rockett F, Castro K, Rossoni de Oliveira V, da Silveira Perla A, Fagundes Chaves ML, Schweigert Perry ID. Perceived migraine triggers: Do dietary factors play a role? Nutr Hosp. 2012;27:483–9. doi: 10.1590/S0212-16112012000200020. [DOI] [PubMed] [Google Scholar]
- 17.Raggi A, Giovannetti AM, Quintas R, D'Amico D, Cieza A, Sabariego C, et al. A systematic review of the psychosocial difficulties relevant to patients with migraine. J Headache Pain. 2012;13:595–606. doi: 10.1007/s10194-012-0482-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Keith SW, Wang C, Fontaine KR, Cowan CD, Allison DB. BMI and headache among women: Results from 11 epidemiologic datasets. Obesity (Silver Spring) 2008;16:377–83. doi: 10.1038/oby.2007.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yu S, Liu R, Yang X, Zhao G, Qiao X, Feng J, et al. Body mass index and migraine: A survey of the Chinese adult population. J Headache Pain. 2012;13:531–6. doi: 10.1007/s10194-012-0470-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Janghorbani M, Amini M, Willett WC, Mehdi Gouya M, Delavari A, Alikhani S, et al. First nationwide survey of prevalence of overweight, underweight, and abdominal obesity in Iranian adults. Obesity (Silver Spring) 2007;15:2797–808. doi: 10.1038/oby.2007.332. [DOI] [PubMed] [Google Scholar]
- 21.Wang Y, Monteiro C, Popkin BM. Trends of obesity and underweight in older children and adolescents in the United States, Brazil, China, and Russia. Am J Clin Nutr. 2002;75:971–7. doi: 10.1093/ajcn/75.6.971. [DOI] [PubMed] [Google Scholar]
- 22.Bigal ME, Liberman JN, Lipton RB. Obesity and migraine: A population study. Neurology. 2006;66:545–50. doi: 10.1212/01.wnl.0000197218.05284.82. [DOI] [PubMed] [Google Scholar]
- 23.Bigal ME, Tsang A, Loder E, Serrano D, Reed ML, Lipton RB. Body mass index and episodic headaches: A population-based study. Arch Intern Med. 2007;167:1964–70. doi: 10.1001/archinte.167.18.1964. [DOI] [PubMed] [Google Scholar]
- 24.Rossoni de Oliveira V, Camboim Rockett F, Castro K, da Silveira Perla A, Chaves ML, Schweigert Perry ID. Body mass index, abdominal obesity, body fat and migraine features in women. Nutr Hosp. 2013;28:1115–20. doi: 10.3305/nh.2013.28.4.6504. [DOI] [PubMed] [Google Scholar]
- 25.Asadi B, Khorvash F, Najaran A, Khorvash F. Cyproheptadine versus propranolol in the prevention of migraine headaches in children. Pak J Med Sci. 2012;28:309–11. [Google Scholar]
- 26.Mottaghi T, Khorvash F, Askari G, Maracy MR, Ghiasvand R, Maghsoudi Z, et al. The relationship between serum levels of vitamin D and migraine. J Res Med Sci. 2013;18(Suppl 1):S66–70. [PMC free article] [PubMed] [Google Scholar]
- 27.Peterlin BL, Rosso AL, Rapoport AM, Scher AI. Obesity and migraine: The effect of age, gender and adipose tissue distribution. Headache. 2010;50:52–62. doi: 10.1111/j.1526-4610.2009.01459.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Verrotti A, Agostinelli S, D'Egidio C, Di Fonzo A, Carotenuto M, Parisi P, et al. Impact of a weight loss program on migraine in obese adolescents. Eur J Neurol. 2013;20:394–7. doi: 10.1111/j.1468-1331.2012.03771.x. [DOI] [PubMed] [Google Scholar]
- 29.Winter AC, Berger K, Buring JE, Kurth T. Body mass index, migraine, migraine frequency and migraine features in women. Cephalalgia. 2009;29:269–78. doi: 10.1111/j.1468-2982.2008.01716.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mattsson P. Migraine headache and obesity in women aged 40-74 years: A population-based study. Cephalalgia. 2007;27:877–80. doi: 10.1111/j.1468-2982.2007.01360.x. [DOI] [PubMed] [Google Scholar]
- 31.Bigal ME, Lipton RB, Holland PR, Goadsby PJ. Obesity, migraine, and chronic migraine: Possible mechanisms of interaction. Neurology. 2007;68:1851–61. doi: 10.1212/01.wnl.0000262045.11646.b1. [DOI] [PubMed] [Google Scholar]
- 32.Overeem S, van Vliet JA, Lammers GJ, Zitman FG, Swaab DF, Ferrari MD. The hypothalamus in episodic brain disorders. Lancet Neurol. 2002;1:437–44. doi: 10.1016/s1474-4422(02)00191-6. [DOI] [PubMed] [Google Scholar]


