Abstract
Background:
In most countries, one of the main reasons for developing more advanced roles for nurses is to improve access to care in the context of limited number of doctors. It is considered that the introduction of major policy initiatives, such as nurse prescribing, requires high-level discussion and policy development to ensure successful implementation. This study aimed to identify the barriers and facilitators of nurse prescribing based on policymakers' views in Iran.
Materials and Methods:
This qualitative study was based on conventional content analysis approach. A purposeful sample of 14 participants were recruited, including 6 members of the Nursing Board, 6 members of the Iranian Nursing Organization, and 2 senior employees of Iran's Ministry of Health and Medical Education. Data were gathered through in-depth semi-structured interviews. Interviews were audio-recorded and transcribed verbatim.
Results:
The four emerged categories as facilitators of nurse prescribing were labeled “positive views of health policymakers,” “human resources capabilities,” “non-medical prescribing experiences,” and “governmental and non-governmental organizational activities.” The four extracted categories as barriers of nurse prescribing were “socio-cultural factors,” “organizational factors,” “educational barriers,” and “human barriers.”
Conclusions:
Barriers and facilitating factors should be considered in order to bring about organizational policy changes and improve perspectives. Nurse prescribing requires the efforts of involved managers and authorities for development and modernization. The results of this study can serve as a compressed resource for policymakers and managers to identify the effective issues on nurse prescribing and can help them to plan for the implementation of nurse prescribing.
Keywords: Barriers, drug prescriptions, facilitators, Iran, nurse, nurse administrators, nurse prescribing, policymakers
INTRODUCTION
Health policymakers and health care managers in many countries are seeking opportunities to increase efficiency in health care delivery by modernizing the roles and mix of health professionals, including the roles of nurses, in response to growing demands for care, limited supply, and tight budget constraints.[1] One example of role expansion to improve patient access to medicines is nurse prescribing.[2] One of the main reasons for developing more advanced roles for nurses is to improve access and promote higher quality of care.[1] A quicker service, saving patients' time, and improved quality of care are among the benefits cited most frequently.[2] In addition, the development of more advanced roles for nurses is often seen as a way to increase attraction of nursing profession and retention rates by enhancing career prospects. In many countries (such as Australia, the United States of America, the United Kingdom, Canada, Ireland, and so on), certain nurses are now authorized to prescribe pharmaceutical drugs.[1,3,4,5,6,7,8,9]
The World Health Organization in the fifth meeting of the regional advisory panel in the Eastern Mediterranean Nursing Convention (Islamabad, Pakistan, 2001) recommended the nurses as first-line health care providers to be empowered and prepared to prescribe properly.[10]
Non-medical prescribing in Iran is done by Behvarzes in health homes. The role of Behvarzes in Iran health system is manifested as one of the Islamic revolution outcomes with the primary health care network in rural population.[11,12,13] They work in rural health clinics called “health house.”[14]
However, there is no appropriate evidence that shows its implementation by nurses. According to the special cultural and social background in Iran, compared to other countries, and the context-based nature of nurse prescribing as well as complexities in its implementation, the necessity of a study in order to explore and describe barriers and facilitators of nurse prescribing is evident. On the other hand, introduction of major policy initiatives, such as nurse prescribing, requires high-level discussion and policy development to ensure successful implementation.[15] Therefore, this study aimed to identify the barriers and facilitators of nurse prescribing based on the policymakers' views.
MATERIALS AND METHODS
A conventional content analysis approach was employed. Content analysis is a research method for making replicable and valid inferences from data.[16] This study aimed to explore the perspectives of Iran health system policymakers on nurse prescribing.
A total of 14 participants were interviewed, including 6 members of the Iranian Nursing Board, 6 members of the Iranian Nursing Organization who serve at various universities of medical sciences, and 2 senior employees of Iran Ministry of Health and Medical Education.
Participants were selected purposefully and entered the study voluntarily. Sampling adequacy was decided using data saturation criteria.
Semi-structured interviews were conducted through coordination with the participants and by assignation in their workplace. The researcher met each participant to briefly explain the study goals and participant's role in the study.
Data collection was carried out from February to May 2013 and through face-to-face in-depth interviews using a few leading questions. Samples of leading questions used were:
What is your overall view about nurse prescribing?
What do you think about the necessity of nurse prescribing in Iran?
What are the barriers and facilitators for its implementation?
The interviews lasted 20–60 min (average duration of 40 min) and were digitally recorded using MP3 voice recorder. Data were analyzed using conventional content analysis which includes open coding, categories creating, and abstraction.[17]
Recorded interviews were listened several times and transcribed to verbatim.
Transcripts were read line by line several times in order to get an overall sense of data. The statements that fitted into the study questions were identified as a “meaning unit” and were coded. Multiple codes were compared based on the differences and similarities, and divided into categories and subcategories. The MAX-QDA software (version 2007) was used to support the coding process. The last step of content analysis was interpretation of the transcribed information as a whole, through which the understandings gained from separate interviews were blended to shape a comprehensive understanding.[18]
The trustworthiness of the study was assessed to confirm data accuracy in terms of the four criteria suggested by Lincoln and Guba: Credibility, dependability, transferability, and confirmability.[19] Credibility was established through careful selection of key informants, combination of data collection methods such as interviews, field notes, and memo writing, integrating different groups of health care policymakers, and rechecking the results with the participants. Dependability was obtained using an interview guide, and through constant comparison of data and classes of similarities and differences, devoting enough time to do interviews and submitting the results to the participants (member-checking), and peer-checking to obtain high agreement. To achieve confirmability, the findings and interpretations of this study were reviewed by expert researchers. Results were also checked with some qualitative researchers who did not participate in this research and they confirmed the fittingness of results. Transferability was determined with a rich description of the context and characteristics of participants and a clear description of the context and restrictions.
Ethical considerations
This study was approved by the Ethics Committee of Tehran University of Medical Sciences (Approval No. 1929). All subjects were informed about the purpose of the study before their participation. They were also provided informed consents. The anonymity was definitely warranted. The raw data, including transcripts, was stored securely and was accessible only for the research team.
FINDINGS
Based on the purpose of study, two headings were identified as barriers and facilitators.
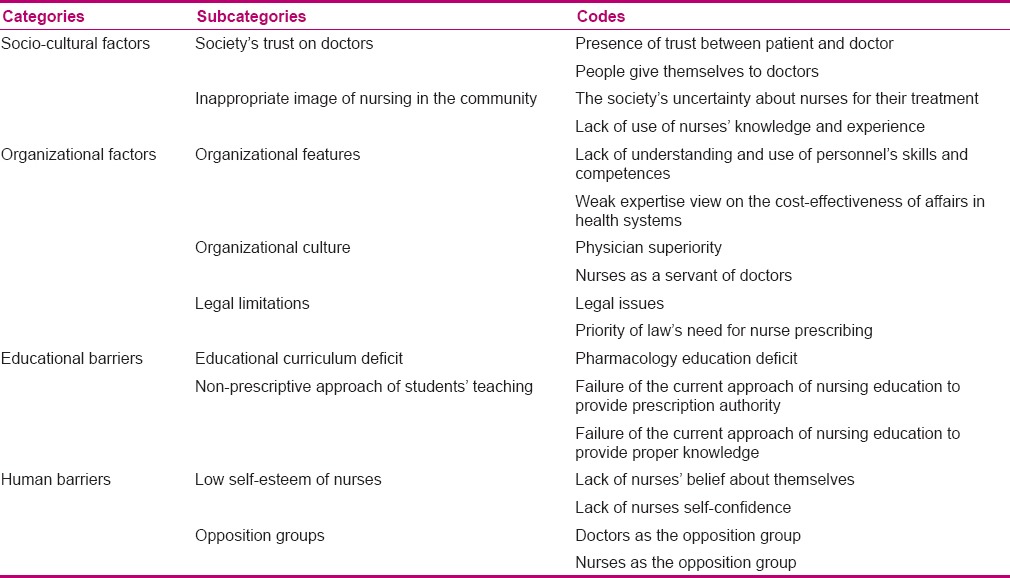
The four categories extractedas facilitators were labeled “positive views of health policymakers,” “human resources capabilities,” “non-medical prescribing experiences,”and “governmental and non-governmental organizational activities.” Also, the four categories extracted as barriers of nurse prescribing were “socio-cultural factors,” “organizational factors,“ educational barriers,” and “human barriers.” Tables 1 and 2 show the summary of categories and related subcategories.
Table 1.
Categories, subcategories, and codes that emerged from the data as facilitator factors of nurse prescribing
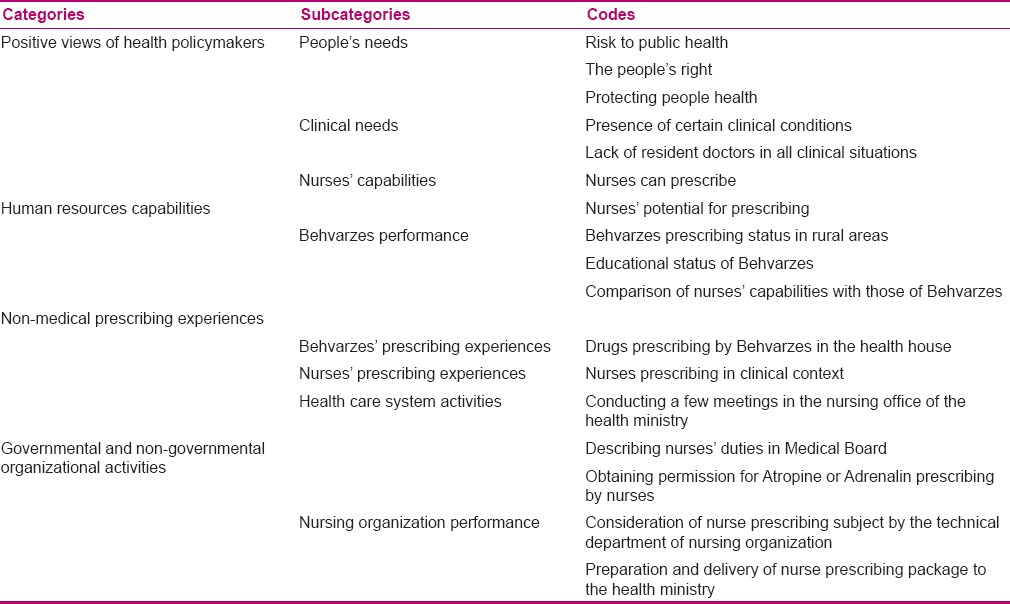
Table 2.
Categories, subcategories, and codes that emerged from the data as barriers of nurse prescribing
Facilitator factors
Positive views of health policymakers
Positive perspective of managers and those involved is essential for implementation of any program because having such a positive view about some issue provides useful support for its implementation. In this study, all participants (health policymakers) agreed on the need and necessity of nursing prescribing in the country; however, they presented this necessity with different statements, often as “people's needs” and occasionally as “clinical needs.” Thus, this category emerged from two subcategories, namely, “people's needs” and “clinical needs.” Following is a selected statement of one of the participants in this regard:
“Nurse prescribing is necessary because its basis is logic, people's health and needs.”
Human resources capabilities
“Human resource capabilities” was the second category that emerged in this study as a facilitator factor of nurse prescribing. This category emerged from two subcategories, namely, “nurses' capabilities” and “Behvarzes' performance.” “Capabilities” means having special skills in each area and participants' statements showed that these capabilities are characteristics of nursing profession. One participant expressed:
“It's true that nurses can prescribe and they have the potential for its doing. If we improve their educational program, they can prescribe drugs. Our nurses are capable. We only should provide the context for them.”
Previous experience of non-medical prescribing
Two subcategories emerged under this category during data analysis: “Behvarzes prescribing experiences” and “nurses prescribing experiences.”
Behvarz prescribing was noted by most participants. They believed that in spite of the positive results of this project, using more educated persons, better results can be expected in hospitals than health houses. This matter was described by a participant as follows:
“Now we see that a Behvarz is prescribing in lower facilities and doing well. Nurse prescribing will answer even better because they are more educated and work in higher facilities.”
Majority of the participants had prescribing experience in hospitals or knew nurses doing so. One of the participants stated:
“Nurse prescribing is being done in our hospitals. I work in a private hospital and the general doctor working there would tell the nurses to take necessary actions including prescribing medicine and he would write the prescription next morning.”
Governmental and non-governmental interventions
Governmental and non-governmental interventions means formal (or even informal) activities conducted to make grounds for their implementation. Two subcategories emerged during analysis under this main category: “Health care system activities” and “nursing organization performance.”
Some participants believed that certain steps were taken by the Health Ministry in relation to nurse prescribing. The following excerpt is part of one of the participants' statements in this regard:
“In my opinion, drug prescription started two years ago when Medical Board permitted nurses to prescribe Atropine or Adrenalin, but needs more work.”
Apart from the interventions done by Treatment Deputy of Ministry, Nursing Board in Iran, as a non-governmental professional organization, was not passive in this case and showed considerable effort, so that according to a participant, a codified program was provided and sent to the Ministry of Health.
Barriers
In this study, on the basis of participants' statements, barriers are classified into four categories as “socio-cultural factors,” “organizational factors,” “educational barriers,” and “human barriers.”
Socio-cultural factors
“Socio-cultural factors” was the first category that emerged in this study as a barrier of nurse prescribing. This category emerged from two subcategories, namely, “society trusts physicians” and “inappropriate image of nursing in the community.” Some of the participants discussed the socio-cultural factors as a barrier for prescribing and stated that people do not trust nurses like they trust doctors. A participant stated:
“In our society, trust between patient and physician exists, but are patients willing to be treated by a nurse?”
Organizational factors
This category is classified into three subcategories of “organizational features,” “organizational culture,” and “legal limitations.” They are discussed below.
“Organizational features” means the characteristics, conditions, and situations that are the basis of performance and guidance of organizational purposes. Majority of the participants believed that conditions of the health care system itself act as a barrier in most of the programs such as nurse prescribing. This leads them to believe that most of the skills and competences of personnel are unknown and unusable.
Another organizational feature noted by the participants included a weak expertise view on the cost-effectiveness of affairs in health systems. One of the participants expressed in relation to this matter as follows:
“We're a little behind in expertise works. We didn't estimate the costs and benefits of physician prescribing and compare it to nurse prescribing.”
“Organizational culture” was also a subcategory defined in organizational factors category. Participants believed that the inter-organizational current culture of our health system only values physicians.
So, the physician superiority attitude has spread in all dimensions of the organization, including health and treatment management and policy making. One participant said:
“System that prevents nurse prescribing is the idea of physicians' superiority.”
“Legal limitations” was also one of the problems that emerged in some statements of the participants. In some participants' views, need for a law on nurse prescribing was a priority, whereas other participants viewed it as unnecessary. A participant stated:
“I believe the first barrier that exists in nurse prescribing is the lack of its description as legal and a documented duty. It should be included as a nursing duty and the law must support its implementation.”
Educational barrier
Two subcategories emerged during data analysis under this main category. The following are the tales that emerged under this category: “Educational curriculum deficit” and “non-prescriptive approach of students' teaching.”
Based on the participants' view, reformation of educational curriculum is a basic necessity for nurse prescribing. One of the participants said:
“If nurse prescribing is going to happen, a proper curriculum should be designed and nurse who can prescribe should have license.”
In most of the participants' statements, educational curriculum deficits, especially in Pharmacology education, were noted. They believed that the current approach of nursing education neither gives prescription authority to students nor provides proper knowledge. This matter gradually caused the feeling that taking orders and executing them is better than having prescriptive authority. The following is a selected statement of a participant:
“'Our nursing education approach is not prescriptive. In fact, nurses do not have the power, they do not know it. In addition, nursing education leads the nurses toward receiving physician order and that way, they will be less responsive.”
Human barriers
Participants introduced human factors as a barrier for nurse prescribing which is classified into two subcategories (nurses' self-esteem and opposition groups). Lack of self-esteem and self-confidence in nurses is a part of human barriers repeatedly mentioned by participants. One of the participants commented on the matter as:
“Nurses don't believe themselves. They have the skill, but don't have the self-confidence to prescribe even if they be granted the authority.”
“Opposition groups” was another subcategory of human barrier stated by some participants. According to some participants, doctors are the main opposed group for nurse prescribing and others, on the contrary, not only know them as the opposed group, but also introduce them as assistant and facilitator. There were several reasons stated by the participants who didn't know physicians as the opposed group. For example, some believed doctors' benefits may be in danger with nurse prescribing, so they disagree, while some participants stated interference of roles and acquiring their professional position as the reason for disagreement.
Unlike some participants who considered doctors as the opposed group, some believed that not only doctors agree with this matter, but also can have assistant role. In this relation, one of the participants said:
“Despite the possible images that might exist, I don't feel doctors' opposition, in fact they can assist us. When our physicians are not present, we can prescribe. PRN, prescription by nurses, is worthful evidence and we can develop PRN.”
An interesting point noted by participants was that most problems and resistance on nurse prescribing were related to the nurses themselves, as stated by one of the participants:
“I think the biggest problem is resistance from our side and nursing experts should present and defend this issue in nursing associations.”
DISCUSSION
Findings of this study reflect the views and perspectives of health policymakers on two headings identified as barriers and facilitator factors of nurse prescribing. At first, the facilitating factors consist of four categories that will be discussed below.
Positive views of health policymakers
The first category of facilitator factors indicated that generally, the perspective of health policymakers in relation to nurse prescribing was positive. Presentation of new models and programs requires preparation and implementation context. Also, may be one of the most important preparations is positive vision of health leaders,[15] because they can plan and support this program. Development of nurses' prescription role roots in modernization of the health system,[20] and positive views of country policymakers showed that they are seeking to modernize the health system aligned with other leading countries (including Canada, the United States of America, and England). Positive views toward nurse prescribing is also mentioned in other studies,[21,22,23,24] and they are consistent with the results of this study.
Human resources capabilities
Human resources have been described as “heart of health system in any country,” “the most important aspect of health care systems,” and “a critical component in health policies.”[25] There is a consensus that despite their importance, human resources have been a neglected component of health system development in low-income countries.[26] It cannot be stated that human resources capabilities have not been used correctly in our country, because Behvarzes with low education are working in villages very well, but the ability of nurses has not been used efficiently.
Non-medical prescribing experiences
Previous experience was another category known to be effective in implementation of nurse prescribing. Having previous experience about anything justifies its reuse, because its advantages, disadvantages, barriers, and facilitators are identified and can also act as a guide for development and taking bigger steps in this field. In other words, the existence of established nursing roles may have helped ensure some of these factors were already in place and, hence, smoothed the way for nurse prescribing.[27] Thus, prescription by Behvarzes can be considered as a facilitator for other health care team members such as nurses.
Governmental and non-governmental organizational activities
Governmental and non-governmental interventions means activities conducted formally (or even informally) for making the grounds for their implementation. The role of non-governmental organizations in development and operation of infrastructure is known.[28]
Study participants also noted the role of nursing board as a non-governmental professional organization.
As mentioned above, based on the health policymarkers' views, some barriers and challenges are essential in nurse prescribing. Reviewing the studies around the world also shows that they also encounter many problems for implementation of nurse prescribing. In the US, with a 30-year history of nurse prescribing in some states, barriers still exist.[29] In our study, four categories were extracted as barriers of nurse prescribing that will be discussed below.
Socio-cultural factors
The first category of barriers (socio-cultural factors) showed that people do not trust nurses as they trust doctors for their cure and do not feel the need. This could be due to the lack of public awareness. Shoqirat and Cameron pointed to poor public image and nurses' low social prestige of the nursing profession. They mentioned that in order to provide a positive image of nursing, both nursing organizations and media should work together to reform the professional position of nurses in the society.[30]
Organizational factors
Organizational barrier was another category that emerged in participants' statements. This category is classified into three subcategories which are “organizational features,” “organizational culture,” and “legal limitations.”
Stenner et al. quoted Latter et al. (2005) and Courtenay et al. (2007), who mentioned that the barriers include lack of organizational preparedness (such as organizing access to prescription pads), difficulty implementing, and restrictions imposed by the legislation, regulation, or funding.[27]
In the present study, “organizational features” category indicates current conditions of our country's health care system which do not use individuals' abilities and competences. Of course, specialized use of people's abilities is meant here and not as Miles et al stated. They reported that in low-income countries, due to staff shortage, they use nurses' abilities completely and nurses in these countries play different roles such as prescribing medication and perform these activities without adequate training and often without legislation and regulation.[31]
“Organizational culture” was also a subcategory discussed in organizational factors category. Statements of participants indicated that our current inter-organizational culture in health care system only supports and values doctors (superiority of physicians).
Unfortunately, the culture of most health care institutions in Iran is such that the position of nurses is lower than managers who are mostly doctors. However, organizational culture is influenced by the social culture of Iran. Iranians traditionally respected doctors and saw nurses as doctors' assistants or followers. These socio-cultural factors have played an important role in power, and decreased self-esteem prevented them from using their innate power and self-reliance.[32] Historically, a hierarchical relationship existed between nurses and physicians in the health care arena. Physician often viewed others as subordinates or followers.[33] Stenner et al. stated that good inter-professional relationships can help promote a supportive culture for acceptance of the nurse prescribing role.[27] They quoted Otway (2002) and Bradley and Nolan (2007) as saying that the physicians support ongoing training and supervision as being of principal importance in nurse prescribing.[27]
On the other hand, Bowskill quoted in his study from Jordan, Knight and Pointon (2004) and Jones et al.(2007) as saying that nurse prescribing will reduce professional distance.[34]
So, it seems that there is mutual relationship between nurse prescribing and professional relations. As professional relations get better, the implementation of nurse prescribing becomes easier and with nurse prescribing, professional relationship will get better.
“Legal limitation” was one of the subcategories in organizational factors category that emerged from the statements of many participants. Prescribing error is potentially the most serious type of medication error. Therefore, prescribing is strictly regulated by numerous pieces of legislation.[35]
In resource-rich countries, legal and regulatory frameworks exist which enable nurses to prescribe medicines legally and effectively. However, such models may not be immediately replicable in low-resource nations that have significant financial, human, and physical infrastructure constraints, as well as those with political instability and, consequently, poorly developed governance systems.[31]
Educational barriers
Educational context and training during nursing education period was also a main factor for implementation of nurse prescribing. Education could be regarded as a potential barrier or as an enabling factor, depending on how well it addresses the needs of nurse prescribers.[36] Training is essential in order to protect nursing practice and, ultimately, the patients being cared for. Appropriate training to extend nurses' skills is considered in leading countries.
However, one of the problems highlighted with regard to training programs is that many academic programs to educate nurses are not always feasible, affordable, or attainable.[31]
The issue of the content of nurses' training background and whether it is sufficient for prescribing activities has not only been raised by other health care professions as a potential weakness in their ability to prescribe, but has also been raised by the nursing professionals themselves. In a literature review, adequacy of nurses' knowledge base in pharmacology was identified as a concern, together with the need for further pharmacology training.[37] It may be appropriate to incorporate management of medicines into the curriculum for pre-registration student nurses, in order to encourage and facilitate the uptake of nurse prescribing training. It could also help to encourage the change in culture that is needed to make nurse prescribing the norm.[36] In order to implement nurse prescription, education should move toward enabling students and personnel through educational courses and continuing education; however, training people to become skilled health workers is costly[38] and managers and policymakers should consider it.
Human barriers
Human factors as a barrier for implementation of nurse prescribing were cited in two subcategories (low self-esteem of nurses and opposition groups). Based on Blanchflower et al., the attitudes of the nurse prescribers themselves and other health professionals are an important factor in the success of nurse prescribing. Confidence in the ability of the nurse to prescribe independently and safely is an important issue for everyone involved. Nurses should feel they have had sufficient training and have adequate understanding to manage medicines effectively.[36] Confidence and competence would develop through prescribing experience over time.[39]
Another significant barrier to nursing autonomy is related to the attitudes of health care practitioners.[40] Support from other professions is needed for nurse prescribing to flourish.[36] Unfortunately, evidence shows the nurses not being supported by organizational systems.[2] Blanchflower et al quoted Rana et al. (2009) about the importance of trust with all professions to make the transition toward new roles for prescribers, concluding that without careful consideration, changes could increase conflict between the professions.[36] The role of doctors' support in nurse prescribing is more essential than that of other health care team personnel. But unfortunately, the conflict between nurses and doctors sometimes acts as a barrier. Much of the conflict between the nurses and physicians is rooted in the historically dominant role of physicians and the subservient role of nurses.[41] Doctors are traditionally considered to be at the top of a hierarchy and are notoriously protective of their power and prestige.[36]
Unfortunately, educational programs offer little or no education about communicating with other clinicians.[42] It is suggested that physicians should learn how to communicate in a way that satisfies the nurses.[43] In other words, physicians should be oriented to the benefits of working with nurses.[44] Finally, some participants mentioned that most of the problems and resistance on nurse prescribing made by the nurses themselves. So, in order to bring change in nursing, nurses must first begin with themselves and create changes within their own.
CONCLUSION
In our country, despite the legal and training deficiency in nurse prescribing, fortunately, the policymakers' view is positive, which could facilitate its implementation. Overall, the results of this study indicate that the current condition is neither so weak that it leads to disappointment nor so desired to remove all the future necessary attempts. The results of this study can be a compressed resource and useful instrument for policymakers and managers, and can help them to identify and describe the effective issues on nurse prescribing, policy formation, and proper planning for the implementation of nurse prescribing.
Financial support and sponsorship
This study is part of a PhD thesis which was financially supported by Tehran University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This study is part of a PhD thesis which was financially supported by Tehran University of Medical Sciences.
REFERENCES
- 1.Delamaire ML, Lafortune G. Nurses in advanced roles: A description and evaluation of experiences in 12 developed countries. OECD Health Working Papers. 2010;54:1–107. [Google Scholar]
- 2.Harris J, Taylor J, Mackie C. Research Literature Review on Prescribing. Scottish Executive Social Research School of Nursing and Midwifery. 2004. [Last accessed on 2013 May 30]. Available from: http://www.scotland.gov.uk/Resource/Doc/17002/0012866.pdf .
- 3.Van Ruth LM, Francke AL, Mistiaen P. Effects of nurse prescribing of medication: A systematic review. Internet J Healthc Adm. 2008;5:1–13. [Google Scholar]
- 4.Kroezen M, van Dijk L, Groenewegen PP, Francke AL. Nurse prescribing of medicines in Western European and Anglo-Saxon countries: A systematic review of the literature. BMC Health Serv Res. 2011;11:127. doi: 10.1186/1472-6963-11-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Courtenay M, Carey N, Stenner K. An overiew of non medical prescribing across one strategic health authority: A questionnaire survey. BMC Health Serv Res. 2012;12:138. doi: 10.1186/1472-6963-12-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhanbhro S, Drennan VM, Grant R, Harris R. Assessing the contribution of prescribing in primary care by nurses and professionals allied to medicine: A systematic review of literature. BMC Health Serv Res. 2011;11:330. doi: 10.1186/1472-6963-11-330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carey N, Stenner K. Does non-medical prescribing make a difference to patients? Nurs Times. 2011;107:14–6. [PubMed] [Google Scholar]
- 8.James J. An overview of non-medical prescribing: Past, present and future. Diabetes voice. 2006;51:26–9. [Google Scholar]
- 9.Kroezen M. Nurse prescribing: A study on task substitution and professional jurisdictions. Utrecht; NIVEL. 2014. [Last accessed on 2015 May 07]. Available from: http://www.nivel.nl/sites/default/files/bestanden/Proefschrift-Marieke-Kroezen-2014.pdf .
- 10.Report on the fifth meeting of the Regional Advisory Panel on Nursing and consultation on advanced practice nursing and nurse prescribing: Implications for regulation, nursing education and practice in the Eastern Mediterranean. Islamabad, Pakistan, 24-26 June 2001. Cairo, WHO Regional Office for the Eastern Mediterranean. 2002. [Last accessed on 10/31/2011 Oct 31]. Available from: http://whqlibdoc.who.int/emro/2002/WHO-EM_NUR_348_E_L.pdf.
- 11.Rostamigooran N, Esmailzadeh H, Rajabi F, Majdzadeh R, Larijani B, Dastgerdi MV. Health system vision of Iran in 2025. Iran J Public Health. 2013;42(Suppl 1):18–22. [PMC free article] [PubMed] [Google Scholar]
- 12.Moghadam MN, Khanjani N. Assessing health worker's duties from the viewpoint of principals and pupils concerning healthcare of students in the rural areas of Iran. J Pak Med Assoc. 2012;62:558–61. [PubMed] [Google Scholar]
- 13.Shokouhi M, Rezapur-Shahkolai F, Naghavi M, Laflamme L. Fall safety promotion in rural communities. Inj Prev. 2010;16:A262–3. [Google Scholar]
- 14.Malakouti SK, Nojomi M, Salehi M, Bijari B. Job stress and burnout syndrome in a sample of rural health workers, behvarzes, in Tehran, Iran. Iran J Psychiatry. 2011;6:70–4. [PMC free article] [PubMed] [Google Scholar]
- 15.Barrowman LM. Review of the Implementation of the Nurse Prescribing Role. On behalf of the Trust Nurses Association in Northern Ireland. 2007. [Last accessed on 2014 Jan 02]. Available from: http://www.nipec.hscni.net/pub/NursePrescribingFinalRpt.pdf .
- 16.Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62:107–15. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- 17.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–88. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 18.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achievetrustworthiness. Nurse Educ Today. 2004;24:105–12. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 19.Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. EDUC INFORM. 2004;22:63–75. [Google Scholar]
- 20.Latter S, Maben J, Myall M, Courtenay M, Young A, Dunn N. An Evaluation of Extended Formulary Independent Nurse Prescribing. Executive Summary of Final Report. School of Nursing and Midwifery, University of Southampton. 2005. [Last accessed on 2012 Mar 04]. Available from: http://www.dsr.dk/Documents/NHS%20Evaluation%20of%20extended%20formulary%20independent%20nurse%20prescribing.pdf .
- 21.Lloyd F, Hughes C. Pharmacists' and mentors' views on the introduction of pharmacist supplementary prescribing: A qualitative evaluation of views and context. Int J Pharm Pract. 2005;15:31–7. doi: 10.1211/ijpp.18.01.0006. [DOI] [PubMed] [Google Scholar]
- 22.Latter S, Smith A, Blenkinsopp A, Nicholls P, Little P, Chapman S. Are nurse and pharmacist independent prescribers making clinically appropriate prescribing decisions. An analysis of consultations? J Health Serv Res Policy. 2012;17:149–56. doi: 10.1258/JHSRP.2012.011090. [DOI] [PubMed] [Google Scholar]
- 23.Latter S, Maben J, Myall M, Young A. Perceptions and practice of concordance in nurses' prescribing consultations: Findings from a national questionnaire survey and case studies of practice in England. Int J Nurs Stud. 2007;44:9–18. doi: 10.1016/j.ijnurstu.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 24.Cooper RJ, Anderson C, Avery T, Bissell P, Guillaume L, Hutchinson A, et al. Nurse and pharmacist supplementary prescribing in the UK - A thematic review of the literature. Health Policy. 2008;85:277–92. doi: 10.1016/j.healthpol.2007.07.016. [DOI] [PubMed] [Google Scholar]
- 25.Kotzee TJ, Couper ID. What interventions do South African qualified doctors think will retain them in rural hospitals of the Limpopo province of South Africa? Rural Remote Health. 2006;6:581. [PubMed] [Google Scholar]
- 26.Hongoro C, McPake B. How to bridge the gap in human resources for health. Lancet. 2004;364:1451–6. doi: 10.1016/S0140-6736(04)17229-2. [DOI] [PubMed] [Google Scholar]
- 27.Stenner K, Carey N, Courtenay M. Implementing nurse prescribing: A case study in diabetes. J Adv Nurs. 2010;66:522–31. doi: 10.1111/j.1365-2648.2009.05212.x. [DOI] [PubMed] [Google Scholar]
- 28.Uwhejevwe-Togbolo S. The Role of Non Governmental Organizations (NGOs) in Development. Prepared for Coalition of NGOs in Delta State, Nigeria. 2005. [Last accessed on 7/4/2012 2012 Jul 04]. Available from: http://www.nigeriavillagesquare.com/articles/samuel-uwhejevwetogbolo/the-role-of-non-governmental-organizations-ngosin-development.html#moreposts .
- 29.An Bord Altranais and National Council for the Professional Development of Nursing and Midwifery. The Review of Nurses and Midwives in the Prescribing and Administration of Medicinal Products. Final Report. Dublin: An Bord Altranais. 2005. [Last accessed on 2014 Jan 02]. Available from: http://www.nursingboard.ie/GetAttachment.aspx?id=94ab8ff6-dd58-465d-89a7-437e593e624c .
- 30.Shoqirat N, Cameron S. Promoting hospital patients' health in Jordan: Rhetoric and reality of nurses' roles. Int J Nursing. 2012;1:28–37. [Google Scholar]
- 31.Miles K, Seitio O, McGilvray M. Nurse prescribing in low-resource settings: Professional considerations. Int Nurs Rev. 2006;53:290–6. doi: 10.1111/j.1466-7657.2006.00491.x. [DOI] [PubMed] [Google Scholar]
- 32.Adib Hagbaghery M, Salsali M, Ahmadi F. A qualitative study of Iranian nurses' understanding and experiences of professional power. Hum Resour Health. 2004;2:9. doi: 10.1186/1478-4491-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brancato VC. Improving nurse–physician collaboration: A health care imperative. Pa Nurse. 2005;60:23. [PubMed] [Google Scholar]
- 34.Bowskill D. The Integration of Nurse Prescribing: Case Studies in Primary and Secondary Care. Thesis for the degree of Doctor of Health Science. University of Nottingham. 2009:1–250. [Google Scholar]
- 35.Culley F. Understanding developments in non-medical prescribing. Nurs Times. 2005;101:30–3. [PubMed] [Google Scholar]
- 36.Blanchflower J, Greene L, Thorp C. Breaking through the barriers to nurse prescribing. Nurs Times. 2013;109:12–3. [Google Scholar]
- 37.Hobson RJ. Investigation into early implementation of non medical prescribing in the UK. Thesis for the degree of Doctor of Philosophy. University of Bath. Department of Pharmacy and Pharmacology. 2008:1–534. [Google Scholar]
- 38.Dussault G, Franceschini MC. Not enough there, too many here: Understanding geographical imbalances in the distribution of the health workforce. Hum Resour Health. 2006;4:12. doi: 10.1186/1478-4491-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Watterson A, Turner F, Coull A, Murray I, Boreham N. An evaluation of the expansion of nurse prescribing in Scotland. Health and Community Care, Scottish Government Social Research. Scottish Government Social Research. 2009. [Last accessed on 2013 Dec 31]. Available from: http://hdl.handle.net/1893/2109 .
- 40.Sterchi LS. Perceptions that affect physician-nurse collaboration in the perioperative setting. AORN J. 2007;86:45–57. doi: 10.1016/j.aorn.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 41.Foster JP. A history of the early development of the nurse practitioner role in New South Wales, Australia, PhD thesis. Sydney: University of Technology; 2010. pp. 1–376. [Google Scholar]
- 42.Beyea SC. Patient safety first: Improving verbal communication in clinical care. AORN J. 2004;79:1053–7. doi: 10.1016/s0001-2092(06)60736-9. [DOI] [PubMed] [Google Scholar]
- 43.Manojlovich M, Antonakos C. Satisfaction of intensive care unit nurses with nurse-physician communication. J Nurs Adm. 2008;38:237–43. doi: 10.1097/01.NNA.0000312769.19481.18. [DOI] [PubMed] [Google Scholar]
- 44.Schmalenberg C, Kramer M, King CR, Krugman M, Lund C, Poduska D, et al. Excellence through evidence: Securing collegial/collaboration nurse physician relationships, Part 1. J Nurs Adm. 2005;35:450–8. doi: 10.1097/00005110-200510000-00006. [DOI] [PubMed] [Google Scholar]


